Wound, Sinus, and Fistula
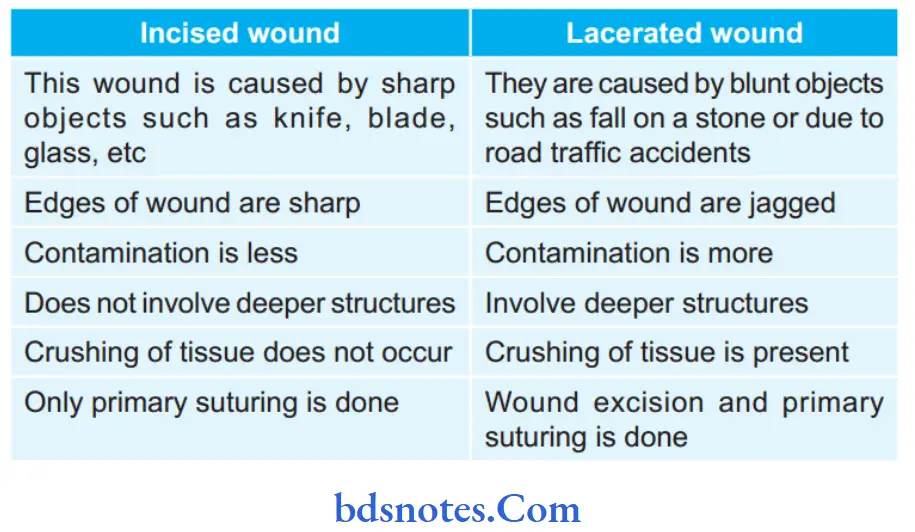
Question.1. Write short note on lacerated wound.
Answer.
Lacerated wound is an open wound.
- Lacerated wounds are caused by the blunt objects like fall on the stone or due to road traffic accidents.
- Edges of lacerated wound are *jagged.
- Injury involves skin or subcutaneous tissue or sometimes-deeper structures also.
- In the lacerated wound, there is crushing of tissue due to blunt nature of the object, which results in hematoma, bruising, or even necrosis of tissue.
Management Of Lacerated Wound
Ideal form of management of incised or lacerated wound is surgical inspection, cleaning, excision and closure, under appropriate anesthesia and *tourniquet in case of a limb.
- Wound must be thoroughly inspected to ensure that there is no damage to deep structure, or where encountered,there must be repaired.
- All dirt and foreign material must be removed.
- Excision of damage skin, wound margins and excision of devitalized tissue such as muscle and fascia.
- After excision, wound is irrigated with antiseptic agent and then suturing must be done.
- There are precise suture placement technique for nerves,tendons and blood vessels.
- Muscles can be apposed in layer by mattess suture and fascia and subcutaneous fat should be apposed by interrupted absorbable suture to allow a fim platform for skin closure.
- On the face, fie nylon suture should be placed near to the wound margins, to be removed on the 5th day.
- An alternative to suturing is the application of adhesive tape strips.
- Systemic antibiotics should be given
- Injection tetanus toxoid for prophylaxis against tetanus.
Read And Learn More: General Surgery Question And Answers
Question 2. Enumerate the various types of surgical wounds and describe their management.
Answer.
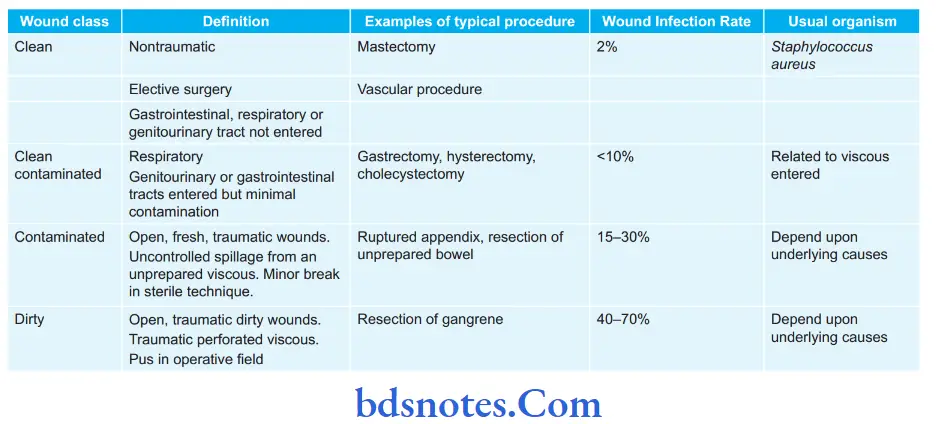
Surgical wounds are classified into four categories according to possibility of infection occurring in them.
Management Of Surgical Wounds
- Airways should be maintained.
- Bleeding of the patient should be controlled.
- IV flids should be started.
- If it is an incised wound, then primary suturing is done after thorough cleaning.
- If it is a lacerated wound, then it is excised and primary suturing is done.
- If it is a crushed wound, there will be edema and tension in wound. In such cases, debridement of wound is done and all the devitalized tissues are excised, edema should subside in 5 to 6 days.
- Afterwards, delayed primary suturing is done.
- If the wound is deep devitalized, debridement of wound is done and it is allowed to granulate completely.
- If wound is small secondary suturing is done.
- If wound is large, split skin graft is used to cover the defect.
- If wound is with tension, then fasciotomy is done.
- Antibiotics, flid and electrolytic balance, blood transfusion, tetanus toxoid or anti-tetanus globulin injection.
Classification of Surgical Wounds
See The Table below
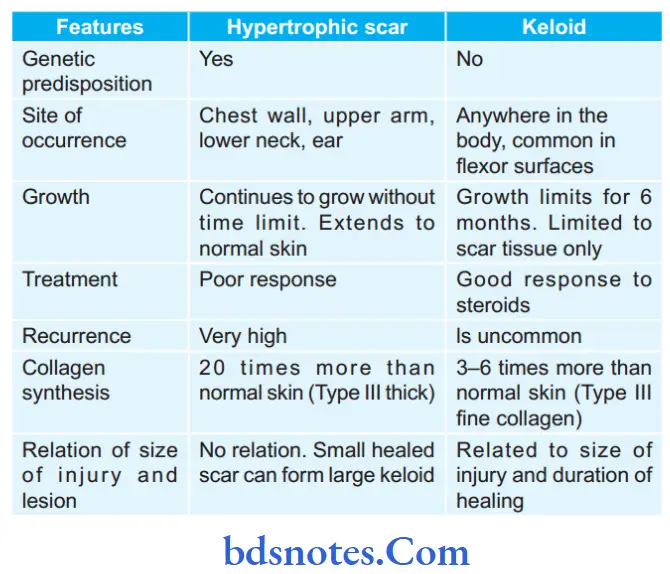
Question 3. Write short note on keloid.
Answer.
Keloid means like a claw.
- In keloid, there is defect in maturation and stabilization of collagen firils. Normal collagen bundles are absent.
- Keloid is common in blacks.
- It is more common in females.
- It is genetically predisposed, often familial and is very rare in Caucasi
- Keloid continues to grow even after 6 months, may be for many years.
- It extends into adjacent normal skin. It is brownish black/pinkish black (due to vascularity) in color, painful, tender and sometimes hyperaesthetic; spreads and causes itching.
- Keloid may be associated with Ehlers-Danlos syndrome or scleroderma.
- When keloid occurs following an unnoticed trauma without scar formation is called as spontaneous keloid, commonly seen in Negroes.
- Some keloids occasionally become non-progressive after initial growth.
- Pathologically, keloid contains proliferating immature firoblasts, proliferating immature blood vessels and type III thick collagen stroma.
- Keloid is common over the sternum. Other sites are upper arm, chest wall, lower neck in front.
Precipitating Factors Of Keloid
- Negro race
- Tuberculosis patient
- Vaccination site.
Complications Of Keloid
- Ulceration
- Infection.
Treatment Of Keloid
- Steroid injection: Intrakeloidal triamcinolone, is injected at regular intervals, may be once in 7–10 days, of 6—8 injections.
Its sequence is Steroid injection—excision—steroid injection. - Methotrexate and vitamin A therapy into the keloid.
- Compressive dressings with silicone gel sheets reduce the tendency of keloid to recurr.
- Laser therapy can be given.
- Vitamin E/palm oil massage.
- Intralesional excision retaining the scar margin may prevent recurrence. It is ideal and bettr than just excision.
- Excision and skin grafting may be done.
Question.4. Classify wound and describes in detail the stage of wound healing.
Answer.
Wound is discontinuity or break in epithelium.
A wound is break in the integrity of skin or tissues often which may be associated with disruption ofthe structure and function.
Classification Of Wound
Rank And Wakefield Classification
Tidy wounds:
- They are wounds such as surgical incisions and wounds caused by sharp objects.
- It is incised, clean, healthy wound without any tissue loss.
- Usually, primary suturing is done. Healing is by primary intention.
Untidy wounds:
- They are due to crushing, tearing, avulsion, devitalised injury, vascular injury, multiple irregular wounds, burns.
- Fracture of the underlying bone may be present.
- Wound dehiscence, infection, delayed healing are common.
- Liberal excision of devitalized tissue and allowing to heal by secondary intention is the management.
- Secondary suturing, skin graft or flp may be needed.
Classification Based On Type Of Wound
- Clean incised wound
- Lacerated wounds
- Bruising and contusion
- Hematoma.
- Closed blunt injury.
- Puncture wounds and bites.
- Abrasion
- Traction and avulsion injury.
- Crush injury
- War wounds and gunshot injuries.
- Injuries to bones and joints, may be open or closed.
- Injuries to nerves, either clean cut or crush.
- Injuries to arteries and veins (major vessels).
- Injury to internal organs, may be of penetrating or
- Non-Penetrating (Blunt) Types.
- Penetrating wounds.
Classification based on Thickness of the Wound
- Superficial wound
- Partial thickness wound
- Full thickness wound
- Deep wounds
- Complicated wounds
- Penetrating wound.
Classification based on Involvement of Structures
- Simple wounds
- Combined wounds.
Classification based on the Time Elapsed
- Acute wound
- Chronic wound.
- Classifiation of surgical wounds
- Clean wound
- Clean contaminated wound
- Contaminated wound
- Dirty infected wound
Stages Of Wound Healing
- Epithelialization: Epithelialization occurs mainly from the edges of wound by process of cell migration and multiplication.
- This is brought about by marginal basal cells.
- Thus within 48 hours entire wound is re-epithelialized.
- Wound contraction: It starts after 4 days and usually complete by 14 days.
- It is brought about by specialized fibroblasts.
- Because of their contractile elements, they are called as myofibroblasts.
- Wound contraction readily occurs when there is loose skin as in back.
- Connective tissue formation: Formation of granulation tissue is most important and fundamental step in wound healing. Injury results in release of mediators of inflmmation.
- This result in increased capillary permeability, later kinins and prostaglandin act and play chemotactic role for white cellsand firoblasts.
- In fist 48 hours, PMN leukocytes dominate. They play role of scavengers by removing dead and necrotic tissue. Between 3rd and 5th day, PMN leukocytes diminished but monocytes increases.
- By 5th or 6th day,firoblasts appear which proliferate and eventually give rise to protocollagen, which is converted in collagen in presence of enzyme protocollagen hydroxylase; O2, ferrous ion and ascorbic acid are necessary. The wound is fier-gel-flid system.
- IV.Scar formation: Following changes takes place during scar formation:
- Fibroplasia and lying of collagen is increased.
- Vascularity becomes less.
- Epithelialization continues.
- Ingrowth of lymphatics and nerve fier takes place.
- Remodeling of collagen takes place with cicatrization result in scar.
Question.5. Write short note on Preauricular sinus. It is a congenital entity occurring due to imperfect fusion of the six tubercles which form ear cartilage.
Answer.
Clinical Features Of Preauricular Sinus
- It is seen since childhood.
- It can be unilateral or bilateral.
- Often swelling appears and apparently disappears repeatedly.
- Pain and discharge is common.
- It causes a cosmetic problem in young individual.
- Sinus opening may be seen at the root of the helix or on the tragus.
- Track is quiet deep running backwards, slightly upwards towards the helix. It usually ends blindly.
- Outer opening of the sinus often closed causing formation of a cystic swelling which contains flid which is often infected.
- Preauricular sinus in no instance will communicate with the external auditory meatus.
- Bursting of this swelling leads into formation of ulcer like lesion.
- Occasionally, multiple sinuses are seen.
- Opening of the sinus occurs in a small triangular area in front of the ear at the level of the tragus.
- Scarring is common around the opening due to repeated infection.
Investigations Of Preauricular Sinus
- Discharge study should be done.
- Sinusogram is done to assess the track.
- MR sinusogram is benefiial.
Differential Diagnosis Of Preauricular Sinus
- Cold abscess
- Sebaceous cyst
Treatment Of Preauricular Sinus
- If sinus infected antibiotics and drainage are required followed by excision when infection passes off
- Under general anesthesia complete excision of tract is only recommended.
Question.6. Write short note on mental sinus.
Answer.
It is a chronic infective acquired condition, wherein there is infection of roots of one or both lower incisor teeth forming root abscess which eventually tracks down between two halves of lower jaw in the midline presenting as discharging sinus on the point of chin at
midline.
Clinical Features Of Mental Sinus
- Usually painless discharging sinus in the midline on the point of chin.
- Often incisor infection may be revealed.
- Osteomyelitis of the mandible is the possible complication.
- Pus discharges through the sinus in center of chin.
- Patient present with recurrent swelling in submental region, which burst open subcutaneously discharging mucus and seropurulent flid at times.
- There is repeated history ofswelling, discharge and healing which are the common presentations.
Investigations Of Mental Sinus
- Dental X-ray is diagnostic.
- Discharge study should be done.
Differential Diagnosis Of Mental Sinus
- Infected sebaceous cyst
- Tuberculous sinus
- Osteomyelitis
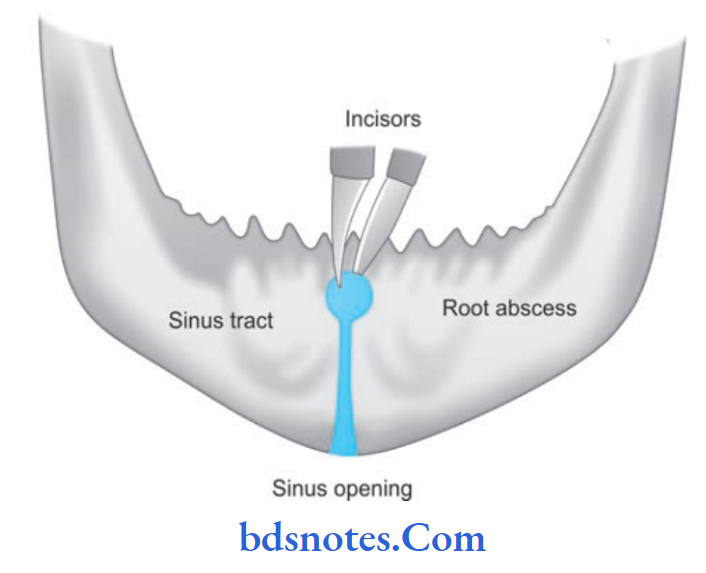
Treatment Of Mental Sinus
- After doing discharge surgery, antibiotics should be given.
- Lay opening and excision of sinus tract with extraction of incisor tooth/teeth.
Question.7. Write short note on crushed lacerated wound.
Answer.
- Crushed lacerated wound is caused by road accidents, or a machinery accidents.
- Crushing of the parts with lacerated skin,devitalization or crushing of the musculature is seen. These devitalized tissues must be excised in order to obtain proper healing.
- Damage to blood vessels and nerves with associated profuse bleeding is also observed. The bone or bones are shattred.
- The wound is highly contaminated.
- There can be loss of soft/hard tissue.
- Treatment of crushed lacerated wound
- Cleaning of wound
- Removal of foreign bodies
- Debridement
- Hemostasis
- Closure in layers, i.e. primary closure
- Dressing
- Prevention of infection
- Pain control
- Follow up.
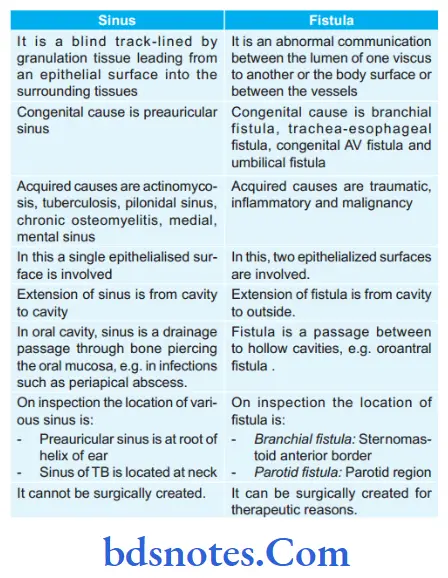
Question.8. Write short note on sinus and fitula.
Or
Write short answer on sinus and fitula.
Answer.
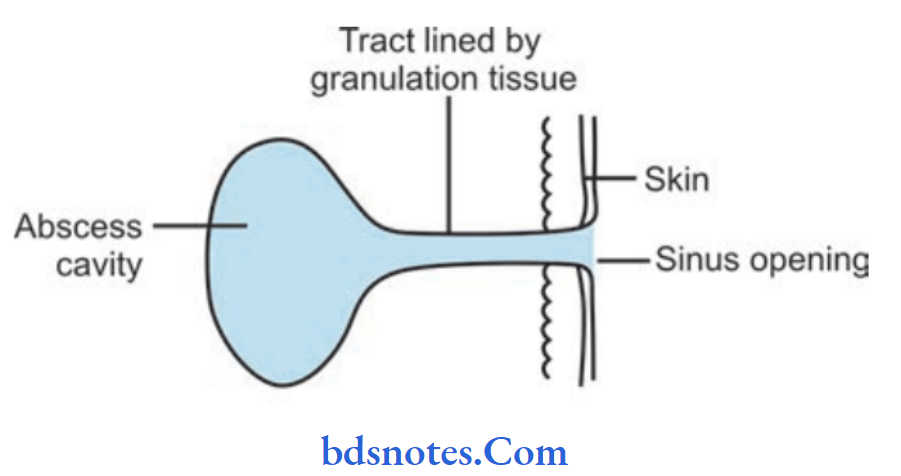
Sinus
- It is a blind tract leading from the surface down into the tissues.
- It is lined with a granulation tissue.
Causes Of Sinus
- Congenital sinus: Preauricular sinus.
- Acquired sinus:
- Median mental sinus: Occurs as a result oftooth abscess.
- Pilonidal sinus: Occurs in the midline in the anal region.
- Osteomyelitis: Gives rise to sinus discharging pus with or without bony spicules.
Fistula
It is an abnormal communication between the lumen of one viscus and the lumen of another (internal) or communication of one hollow viscus withthe exterior, i.e. body surface (external fitula).
- Examples ofinternal fitula:
- Tracheoesophageal fitula
- Colovesical fitula
- Examples of external fitula
- Orocutaneous fitula due to carcinoma of the oral cavity infitrating the skin
- Branchial fitula
- Thyroglossal fitula.
Clinical Features of Sinus/Fistula
- Discharge from the opening of sinus
- No flor is present
- Raised indurated edge, indurated base and non-mobile
- Often sprouting granulation tissue over sinus opening.
- Bone thickening in osteomyelitis
- Surrounding skin may be erythematous and inflmmatory.
- Bluishin tuberculosis, excoriated in fecal fitula, pigmented in chronic sinuses and fitulas.
- Induration is the feature of all chronic fistulas except tuberculosis.
Investigations
- Fistulogram/Sinusogram using ultraflid lipiodol or water soluble iodine dye.
- Biopsy from edge for tuberculosis and malignancy
- X-ray of the involved part.
- Proctoscopy of fistula.
Treatment
- Cause should be treated
- Excision of sinus or fitula and specimen should be sent for histology
- Antibiotics, anti-tubercular drugs, rest and adequate drainage.
Question.9. Write short note on complications of furunculosis.
Answer.
Furunculosis is the reoccurring presence of pus-filed sores, known as boils, on the skin.
Following are the complications of furunculosis:
- Carbuncles
- Cellulitis
- Gangrene
- Necrotizing fasciitis
- Hidradenitis suppurativa (infection in group of hair follicles)
- Lymphadenitis
- Cavernous sinus thrombosis.
Question.10. Describe wounds, their classification, wound healing and its treatment.
Answer.
- Wound is inspected and classified as per the type of wounds.
- If it is in the vital area, then:
- The airway should be maintained.
- The bleeding, if present, should be controlled.
- Intravenous flids are started.
- Oxygen, if required, may be given.
- Deeper communicating injuries and fractures, etc should be looked for.
- If it is an incised wound, then primary suturing is done after thorough cleaning.
- If it is a lacerated wound, then the wound is excised and primary suturing is done.
- If it is a crushed or devitalized wound, then there will be edema and tension in the wound.
- So after wound debridement or wound excision by excising all devitalized tissue,the edema is allowed to subside for 2–6 days.
- Then, delayed primary suturing is done.
- If it is a deep devitalised wound, after wound debridement it is allowed to granulate completely.
- Later, if the wound is small secondary suturing is done.
- In a wound with tension, fasciotomy is done so as to prevent the development of compartment syndrome.
- Antibiotics, flid and electrolyte balance, blood transfusion,tetanus toxoid (0.5 mL intramuscular to deltoid muscle), or anti-tetanus globulin (ATG) injection.
- Wound debridement (wound toilet, or wound excision) is liberal excision of all devitalized tissue at regular intervals.
Question.11. Write short note on complications of wounds.
Answer.
Following are the complications of wounds:
- Infection: Itis the most important complication which is responsible for delay in wound healing.
- Bacteria mainly remain endogenous.
- Based onpus culture and blood report antibiotics should be prescribed.
- Scar: Present due to infection.
- Hypertrophic scar and Keloid formation due to altered collagen synthesis in wound healing process.
- Skin pigmentation
- Marjolin ulcer: As repeated breakdown of hypertrophic scar occur it becomes Marjolin’s ulcer.
Question.12. Write short note on general factors affecting wound healing.
Answer.
General Factors Of Affecting Wound Healing.
General factors affecting wound healing are as follows:
- Age
- Malnutrition
- Vitamin defiiency (Vitamin C, Vitamin A)
- Anemia
- Malignancy
- Uremia
- Jaundice
- Diabetes, metabolic diseases
- HIV and immunosuppressive diseases
- Steroids and cytotoxic drugs
- Age: In younger age group, wound healing is faster and bettr while in elderly healing is delayed due to reduction in collagen synthesis, epithelialization, growth factors and angiogenesis. But facial scar will be excellent in old individuals.
- Malnutrition and vitamin deficiency: Adequate vitamin, trace elements, fatt acids, and proteins are essential for wound healing. Vitamin A deficiency affects monocyte activation, inflammatory phase, collagen synthesis and growth factor actions.
- Vitamin K deficiency affects synthesis of prothrombin (ll), factors VII, IX and X. vitamin E, being an antioxidant stabilizes the cell membrane. Vitamin C deficiency impairs collagen synthesis, firoblast proliferation and angiogenesis; increases the capillary fragility and susceptibility for infection. Zinc is an essential cofactor for RNA and DNA polymerase;magnesium is a co-factor for synthesis of proteins and collagen; copper is a required co-factor for cytochrome oxidase.
- Anemia: Hemoglobin less than 8% causes poor oxygenation of tissues preventing healing of the wounds.
- Diabetes mellitus: In diabetic patients, wound healing is delayed because of several factors such as microangiopathy, atherosclerosis, decreased phagocytic activity, proliferation of bacteria due to high blood sugar etc.
- Metabolic causes: Obesity causes hypoperfusion, reduced microcirculation, increased wound tension, and hence prevents wound healing.
- Jaundice and uremia: Jaundiced and uraemic patients have poor wound healing because firoblastic repair is delayed.
- HIV and immunosuppressive diseases and malignancy: HIV and immunosuppression of varying causes, malignancy leads into poor wound healing.
- Drugs: Steroids interfere with activation of macrophages, fibroblasts, and angiogenesis in the early phase of healing (proliferative).
Nonsteroidal anti-inflammatory drugs (NSAIDs) decrease collagen production. Chemotherapeutic agents used in oncology inhibit cellular proliferation, protein synthesis. Alcohol consumption decreases the phagocyte response and pro-inflammatory cytokine release; diminishes host response and thus increasing the infection rate.
Question.13. Write short note on hypertrophic scar.
Answer.
In hypertrophic scar, there is hypertrophy of mature firoblasts. Blood vessels are minimum in this condition.
- It can occur anywhere in the body.
- Growth limits upto 6 months.
- Hypertrophic scar is limited to scar tissue and does not extend to normal skin.
- It is pale brown in color and is non-tender.
- It is self limiting.
- It is common in wounds crossing tension lines, deep dermal burns, wounds heal by secondary intension.
Complications Of Hypertrophic Scar
- Scar breaks repeatedly and cause infection and pain.
- After repeated breakdown, it may turn into Marjolin’s ulcer.
Treatment Of Hypertrophic Scar
- It is controlled by pressure garments or often revision excision of scar and closure if required with skin graft.
- Triamcinolone injection is second line of therapy.
Question.14. Discuss briefly branchial fistula.
Or
Write in brief on branchial fistula.
Answer.
Branchial fistula is commonly a congenital lesion.
- It is persistent precervical sinus between 2nd branchial cleft and 5th branchial cleft having opening in the skin at lower l/3rd of neck on the inner margin of sternocleidomastoid muscle, often ends as a sinus just proximal to the posterior pillar of fauces behind tonsil which is also the site of inner opening when presents as a fitula.
- Fistula runs between the structures related to second and 3rd branchial arches.
From external opening at skin below,it runs in subcutaneous plane to pierce deep fascia at level of thyroid cartilage; to travel between 2nd arch artery and third arch artery behind posterior digastric belly and stylohyoid; outer to stylopharyngeus, hypoglossal and glossopharyngeal nerves; perforates superior constrictor - to reach the internal opening.
- Occasionally, acquired branchial fitula can occur due to rupture of or after drainage of infected branchial cyst or incomplete excision of the cyst tract.
This type of fitula is located outside at skin at the level of upper third of sternomastoid muscle.
Clinical Features Of Branchial Fistula
- It is a persistent second branchial cleft with a communication outside to the exterior. It is commonly a congenital fitula.
- Occasionally, the condition is secondary to incised infected branchial cyst.
- Often it is bilateral.
- External orifie of the fitula is situated in the lower third of the neckn earth eanterior border of the sternomastoid muscle.
- Internal orifie is located on the anterior aspect of the posterior pillar of the fauces, just behind the tonsils.
- Sometimes fitula ends internally as blind end.
- It is common in children and early adolescent period.
- Equals in both sexes.
- External orifie is very small with a dimple which becomes more prominent on dysphagia with tuck in appearance.
- Discharge is mucoid or mucopurulent.
Treatment Of Branchial Fistula
Only surgical treatment is the choice.
- Under general anesthesia, methylene blue is injected into the tract.
- Probe is passed into the fitulous tract.
- Through circumferential/elliptical incision around the fistula opening, entire length of the tract is dissected until the internal orifie.
- Care should be taken to safeguard carotids,jugular vein, hypoglossal nerve, glossopharyngeal nerve and spinal accessory nerve.
- Entire tract should be excised.
- Step-ladder dissection is done using two parallel incisions one below at lower part another above at upper part of the neck, will make dissection easier and complete.
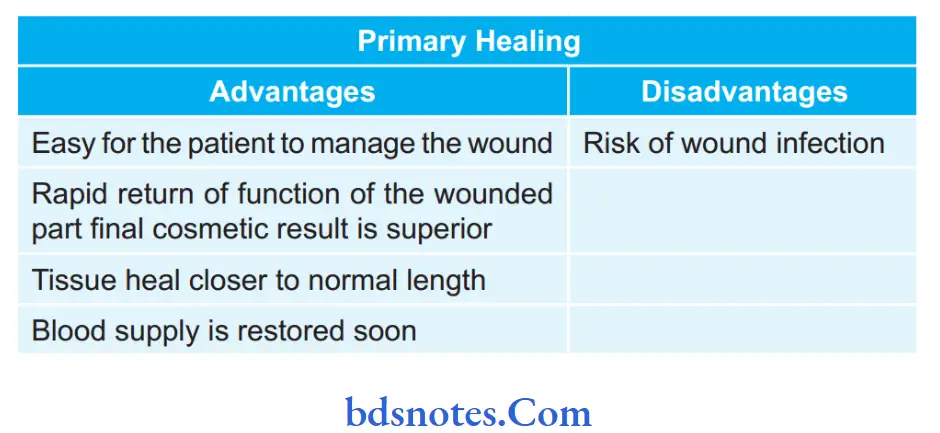
Question.15. Describe briefly primary and secondary healing of wounds.
Answer.
Primary Healing of Wound
- In primary healing of wound edges are approximated by surgical sutures.
- In the initial phase, there will be formation of blood clot, which helps to hold the parts of the wound together.
- The tissue becomes edematous and an inflmmatory process starts, with the infitration of polymor-phonuclear neutrophils (PMN) and lymphocytes into the area.
- The tissue debris collected in the wound are cleared either by the process of phagocytosis or by their lysis with the help of proteolytic enzymes, liberated by the inflammatory cells.
- Once the tissue debris are cleared, granulation tissue forms that replaces the blood clot in the wound, and it usually consists of young blood capillaries, proliferating firoblasts, PMN, and other leukocytes.
- The epithelium at the edge of the wound starts to proliferate and gradually, it covers the entire wound surface.
- Finally, the healing process is complete with progressive increase in the amount of dense collagen bundles and decrease in the number of inflammatory cells in the area.
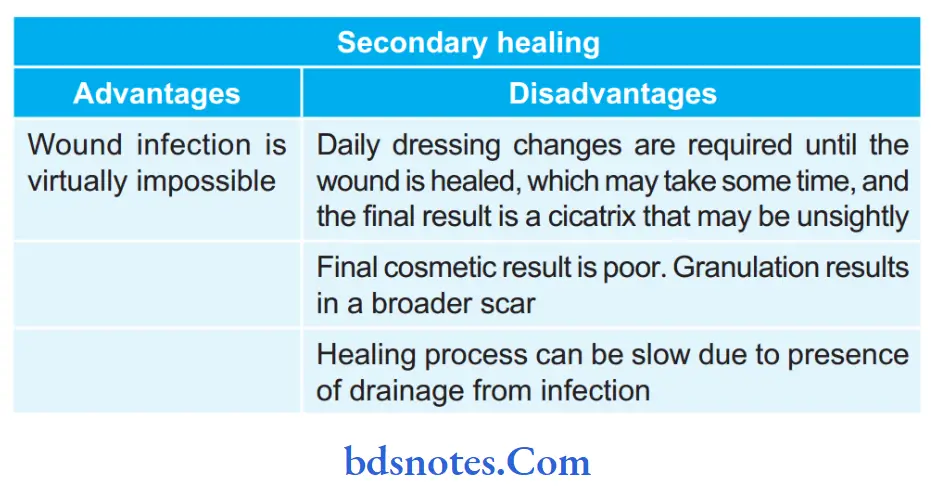
Secondary Healing of Wound
- When the opposing margins of the wound cannot be approximated together by suturing, the wound fils in from the base with the formation of a larger amount of granulation tissue, such type of healing of the open wound is known as healing by “secondary intention” or “secondary healing”.
- The secondary healing occurs essentially by the same process as seen in the primary healing, the only diffrence is that a more severe inflammatory reaction and an exuberant firoblastic and endothelial cell proliferation occur in the later.
- In secondary healing, once the blood clot is removed,the granulation tissue fils up the entire area and the epithelium begins to grow over it, until the wound surface is completely epithelized.
- Later on, the inflmmatory exudates disappear slowly and the firoblasts produce large amounts of collagen.
- Most of the healing processes occurring due to secondary intention, result in scar formation at the healing site.
However, in the oral cavity, these are rare.
Question.16. Write briefly on factors inflencing wound healing.
Answer.
General Factors
General factors affcting wound healing are as follows:
- Age
- Malnutrition
- Vitamin defiiency (Vitamin C, Vitamin A)
- Anemia
- Malignancy
- Uremia
- Jaundice
- Diabetes, metabolic diseases
- HIV and immunosuppressive diseases
- Steroids and cytotoxic drugs
Age: In younger age group, wound healing is faster and better while in elderly healing is delayed due to reduction in collagen synthesis, epithelialization, growth factors and angiogenesis.
But fial scar will be excellent in old individuals.
Malnutrition and Vitamin deficiency: Adequate vitamins,trace elements, fatty acids and proteins are essential for wound healing. Vitamin A deficiency affects monocyte activation, inflammatory phase, collagen synthesis and growth factor actions.
Vitamin K deficiency affects synthesis of prothrombin (ll), factors VII, IX and X. Vitamin E, being an antioxidant stabilizes the cell membrane.
Vitamin C defiiency impairs collagen synthesis, fibroblast proliferation and angiogenesis; increases the capillary fragility and susceptibility for infection.
Vitamin K deficiency affects synthesis of prothrombin (ll), factors VII, IX and X. Vitamin E, being an antioxidant stabilizes the cell membrane.
Vitamin C defiiency impairs collagen synthesis, fibroblast proliferation and angiogenesis; increases the capillary fragility and susceptibility for infection.
Zinc is an essential cofactor for RNA and DNA polymerase;magnesium is a co-factor for synthesis of proteins and collagen;copper is a required co-factor for cytochrome oxidase.
Anemia: Hemoglobin less than 8% causes poor oxygenation of tissues preventing healing of the wounds.
Diabetes mellitus: In diabetic patients, wound healing is delayed because of several factors such as microangiopathy, atherosclerosis, decreased phagocytic activity, proliferation of bacteria due to high blood sugar, etc.
Metabolic causes: Obesity causes hypoperfusion, reduced microcirculation, increased wound tension, and hence prevents wound healing.
Jaundice and uremia: Jaundiced and uremic patients have poor wound healing because firoblastic repair is delayed.
HIV and immunosuppressive diseases and malignancy: HIV and immunosuppression of varying causes, malignancy leads into poor wound healing.
Drugs: Steroids interfere with activation of macrophages,firoblasts and angiogenesis in the early phase of healing (proliferative).
Non-steroidal anti-inflammatory drugs (NSAIDs) decrease collagen production.
Chemotherapeutic agents used in oncology inhibit cellular proliferation, protein synthesis.
Alcohol consumption decreases the phagocyte response and proinflmmatory cytokine release; diminishes host response and thus increasing the infection rate.
Non-steroidal anti-inflammatory drugs (NSAIDs) decrease collagen production.
Chemotherapeutic agents used in oncology inhibit cellular proliferation, protein synthesis.
Alcohol consumption decreases the phagocyte response and proinflmmatory cytokine release; diminishes host response and thus increasing the infection rate.
Local Factors
Local factors affcting wound healing are as follows:
- Infection
- Presence of necrotic tissue and foreign body
- Poor blood supply
- Venous or lymph stasis
- Tissue tension
- Hematoma
- Large defect or poor apposition
- Recurrent trauma
- X-ray irradiated area
- Site of wound
- Underlying diseases such as osteomyelitis and malignancy
- Mechanism and type of wound-incised/lacerated/crush/avulsion
- Tissue hypoxia locally reduces macrophage and firoblast activity
Wound infection: Infection prolongs inflmmatory phase,releases toxins and utilizes vital nutrients thereby prevents wound epithelialization. The β-hemolytic streptococci more than 105 per gram of tissue prevent wound healing. Formation of biofilm on the wound surface by microorganisms prevents wound healing.
Presence of necrotic tissue and foreign body: Necrotic tissue and foreign bodies such as sutures cause intense inflammatory reaction and infection.
Poor blood supply: Improper blood supply to wound delays wound healing.
Tissue tension: It affects quantity, aggregation and orientation of collagen fiers.
Hematoma: It precipitates infection and delays wound healing.
Hypoxia: Hypoxia prevents firoblast proliferation and collagen synthesis; it also promotes bacterial invasion into the wound.
Site of wound: Movement of wound area delays wound healing. e.g. wound over the joints and back has poor healing.
X-ray irradiated area: Both external radiotherapy or ionizing radiation cause endarteritis, fibrosis and delay in wound healing. Radiation may itself cause local tissue necrosis, sepsis and hypoxia.
Poor apposition: Poor apposition leads to the infection in the wound area which delays healing.
Question.17. Define and describe differentiating features of incised wound and lacerated wound.
Answer.
Question.18. Discuss the etiology, clinical features and management of wounds.
Answer.
A wound is the break in the integrity of skin or tissues often which may be associated with disruption of structure and function.
Etiology And Clinical Features
Tidy wounds:
- They are wounds such as surgical incisions and wounds caused by sharp objects.
- It is incised, clean, healthy wound without any tissue loss.
Untidy wounds:
- They are due to crushing, tearing, avulsion,devitalised injury, vascular injury, multiple irregular wounds, burns.
- Fractures of the underlying bone may be present.
- Wound dehiscence, infection, delayed healing are common.
Classification based on Types of Wound
- Clean incised wound: It is a clean cut wound with linear edge.
- Lacerated wounds: The lacerated wounds are caused by the blunt objects such as fall on the stone or due to road traffi accident.
- The edges of lacerated wound are *jagged.
- The injury involves skin or subcutaneous tissue or sometimes-deeper structures also.
- In the lacerated wound there is crushing of tissue due to blunt nature of the object.
- Bruising and contusion: It is a minor soft tissue injury with discoloration and hematoma formation without skin break.
- Hematoma: Caused due to injury. It consist of reddish plasmatic flid which can be aspirated and if it get infected, then pus is formed.
- Closed blunt injury.
- Puncture wounds and bites.
- Abrasion: Occurs due to shearing of skin where surface is rubbed off
- Traction and avulsion injury.
- Crush injury: It is caused in wars, road traff accidents, tourniquet.
- Muscle ischaemia is present.
- Presence of gangrene and loss of tissue.
- War wounds and gunshot injuries.
- Injuries to bones and joints, may be open or closed.
- Injuries to nerves, either clean cut or crush.
- Injuries to arteries and veins (major vessels).
- Injury to internal organs, may be of penetrating or non-penetrating (blunt) types.
- Penetrating wounds.
Classification based on Thickness of the Wound
- Superficial wound
- Partial thickness wound
- Full thickness wound
- Deep wounds
- Complicated wounds
- Penetrating wound.
Classification based on Involvement of Structures
- Simple wounds
- Combined wounds.
Classification based on the Time Elapsed
- Acute wound
- Chronic wound.
Classification of Surgical Wounds.
- Clean wound
- Clean contaminated wound
- Contaminated wound
- Dirty infected wound
Management
- Wound is inspected and classified as per the type of wounds.
- If it is in the vital area, then:
- The airway should be maintained.
- The bleeding, if present, should be controlled.
- Intravenous flids are started.
- Oxygen, if required, may be given.
- Deeper communicating injuries and fractures, etc.Should Be Looked For.
- If it is an incised wound, then primary suturing is done after thorough cleaning.
- If it is a lacerated wound, then the wound is excised and primary suturing is done.
- If it is a crushed or devitalized wound, then there will be edema and tension in the wound.
So after wound debridement or wound excision by excising all devitalised tissue, the oedema is allowed to subside for 2–6 days.
Then delayed primary suturing is done. - If it is a deep devitalised wound, after wound debridement it is allowed to granulate completely.
Later, if the wound is small secondary suturing is done.
If the wound is large a split skin graft (Thiersch graft) is used to cover the defect. - In a wound with tension, fasciotomy is done so as to prevent the development of compartment syndrome.
- Vascular or nerve injuries are dealt with accordingly.
- Vessels are sutured with 6-zero polypropylene nonabsorbable suture material.
If the nerves are having clean-cut wounds then it can be sutured primarily with polypropyl ene 6-zero or 7-zero suture material. If there is diffilty in identifying the nerve ends, or if there are crushed cut ends of nerves, then marker stitches are placed using silk at the site and later secondary repair of the nerve is done. - Internal injuries has to be dealt with accordingly. Fractured bone is also identifid and properly dealt with.
- Antibiotics, flid and electrolyte balance, blood transfusion, tetanus toxoid, antitetanus globulin (ATG) injection.
- Wound debridement is liberal excision of all devitalized tissue at regular intervals until healthy, bleeding, vascular tidy wound is created.
Question.19. Enumerate diffrences between sinus and fitula.
Or
Write differences between sinus and fitula.
Or
Differences between sinus and fitula.
Answer.
Question.20. Describe pathophysiology of primary and secondary healing. Enumerate their clinical advantages and disadvantages in tabular form. List when assault becomes a cognizable offense.
Answer.
Pathophysiology of primary and secondary healing means primary and secondary healing of wounds.
Assault is the act of creating apprehension of an imminent harmful or offnsive contact with a person.
Generally, cognizable offnce means a police offir has the authority to make an arrest without a warrant and the police is also allowed to start an investigation with or without the permission of a court.
Following are the cognizable offenses:
- All grievous hurts
- Simple hurt by dangerous weapon
- Murder
- Culpable homicide
- Causing death by rash or negligence act.
- Dowry death
- Abetment to suicide
- Attmpt to murder
- Attmpt to commit suicide
- Rape.
Question.21. Enumerate causes for chronicity of sinus and fitula.
Answer.
Following are the causes for chronicity of sinus and fitula:
- A foreign body or necrotic tissue underneath. e.g.suture, sequestrum.
- Insuffient or non-dependent drainage
- Persistent obstruction in lumen, e.g. In fecal fitula,biliary fitula
- Lack of rest, persistent infection
- Wall become lined with epithelium and endothelium
- Dense firosis prevents contraction and healing
- Specifi infections: Tuberculosis and actinomycosis
- Presence of malignant disease, post irradiation.
Question.22. What is primary and secondary healing, advantage of one over other. What are the injuries that constitute cognizable offnce in IPC.
Answer.
Primary healing: It occurs in a clean incised or surgical wound. Edges of the wound are approximated by sutures.
Epithelial regeneration is more as compared to firosis.
Wound healing takes place rapidly with complete closure.
Scar will be linear, supple and smooth.
Epithelial regeneration is more as compared to firosis.
Wound healing takes place rapidly with complete closure.
Scar will be linear, supple and smooth.
Secondary healing: It occurs in a wound with extensive soft tissue loss like in major trauma, burn, wound with sepsis.
Healing by secondary intention occur slowly with firosis.
This also leads to the formation of wide scar which is hypertrophied and contracted.
This can also lead to disability.
Healing by secondary intention occur slowly with firosis.
This also leads to the formation of wide scar which is hypertrophied and contracted.
This can also lead to disability.
Injuries that Constitute Cognizable offence in iPC
Cognizable offnce means an offnce for which a police offir may arrest without a warrant.
Following are the cognizable offnces:
- Murder (S.302)
- Causing death by rash or negligent act (S. 304A)
- Dowry death (S.304B)
- Abetment of suicide (S. 306)
- Attmpt to commit suicide (S. 309)
- Causing miscarriage without women’s consent (S. 313)
- Grievous hurt (S. 325, 326)
- Rape (S. 376)
- Theft (S. 379).
Question.23. Write short note on granulation tissue.
Answer.
Granulation tissue is the proliferation ofnewer capillaries along with firoblasts which are intermingled with RBCs and WBCs with thin firin cover over it.
Types Of Granulation Tissue
Following are the types of granulation tissue:
Healthy granulation tissue
- It results in an healing ulcer.
- It has got a sloping edge with serous discharge.
- It bleeds on manipulation.
- Skin graft takes well with healthy granulation tissue.
- Healthy granulation tissue consists of 5Ps i.e. pink,punctuate hemorrhage, pulseful, painless, pinhead
Unhealthy granulation tissue
- This is pale in color with purulent discharge.
- Floor of granulation tissue is covered with slough.
- Its edges are inflmed and edematous.
- It is a type of a spreading ulcer.
Unhealthy, pale, flt, granulation tissue
- It is seen in chronic non-healing ulcer.
- Exuberant granulation tissue
- It occurs in sinus where granulation tissue protrude out of orifie of sinus as proliferating mass.
- Mostly associated with retained foreign body in sinus cavity.
Pyogenic granuloma
- Here granulation tissue protrudes from an infected wound or ulcer bed and presents a well localized, red swelling which bleed on manipulation.
- It is treated by surgical excision.
Question.24. Write briefly on cognizable offense.
Answer.
Generally, cognizable offnce means a police offir has the authority to make an arrest without a warrant and to start an investigation with or without the permission of a court.
- Incognizableoffnce, policehastore cordinformation in writing.
- The police can fie a First Information Report (FIR) only for cognizable offnces.
- In cognizable offnces, police can start investigation without the order of magistrate.
- Cognizable offense is more serious and carry a sentence of 3 years or more.
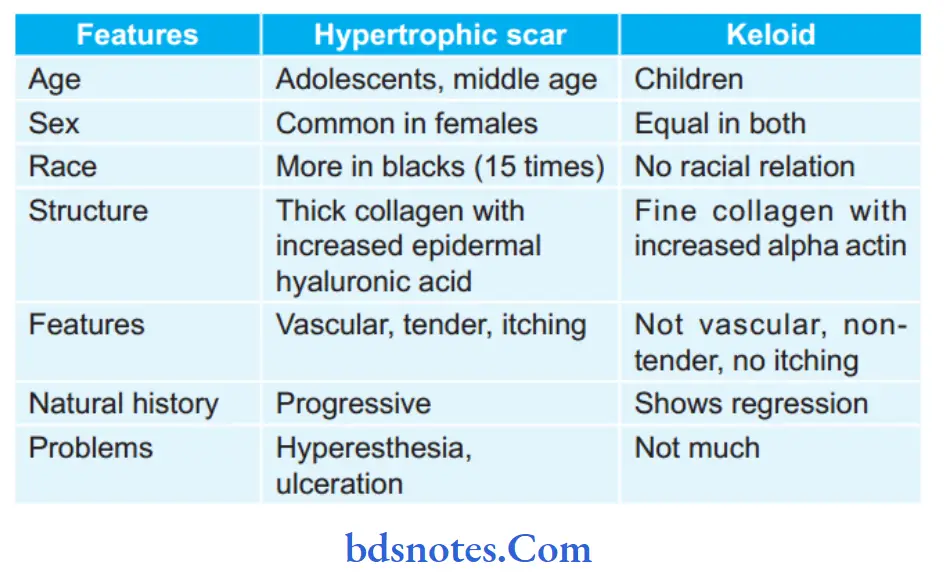
Question.25. Write difference between hypertrophic scar and keloid.
Answer.
Following are diffrences between hypertrophic scar and keloid:
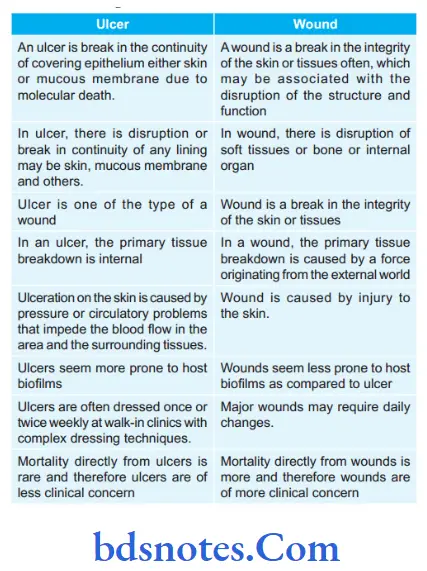
Question.26. Describe differentiating features of ulcer and wound.
Answer.
Following are the diffrences between ulcer and wound
Question.27. Describe primary and secondary wound healing. Discuss mechanism and various phases of wound healing.
Answer.
Primary Wound Healing
- It occurs in a clean Incised wound or surgical wound.
- Wound edges are approximated with sutures. There is more epithelial regeneration than firosis. Wound heals rapidly with complete closure.
- Scar will be linear, smooth and supple.
Secondary Wound Healing
- It occurs in a wound with extensive soft tissue loss like in major trauma, bums and wound with sepsis.
- It heals slowly with firosis.
- It leads into a wide scar, often hypertrophied and contracted.
- It may lead into disability.
- Re-epithelialization occurs from remaining dermal elements or wound margins.
Mechanism of Primary Healing of Wound
- In primary healing of wound, edges are approximated by surgical sutures.
- In the initial phase, there will be formation of blood clot,which helps to hold the parts of the wound together.
- Within 10 to 15 minutes of injury vasodilatation occur and there is increased capillary permeability mediated by vasoactive substances released by damage cells and clot breakdown.
- The tissue becomes edematous and an inflammatory process starts, with the infitration of polymorphonuclear neutrophils (PMN) and lymphocytes into the area.
- The tissue debris collected in the wound are cleared either by the process of phagocytosis or by their lysis with the help of proteolytic enzymes, liberated by the inflmmatory cells.
- Once the tissue debris are cleared, granulation tissue forms that replaces the blood clot in the wound, and it usually consists of young blood capillaries, proliferating firoblasts, PMN and other leukocytes.
- The epithelium at the edge of the wound starts to proliferate and gradually, it covers the entire wound surface.
- Finally, the healing process is complete with invasion of wound area by firoblast on 3rd day, progressive increase in the amount of dense collagen bundles on 5th day and formation of scar tissue with scanty cellular and vascular elements, some inflammatory cells and epithelialized surface by 4th week.
Mechanism of Secondary Healing of Wound
- When the opposing margins of the wound cannot be approximated together by suturing, the wound fils in from the base with the formation of a larger amount of granulation tissue, such type of healing of the open wound is known as healing by “secondary intention” or “secondary healing”.
- The secondary healing occurs essentially by the same process as seen in the primary healing, the only diffrence is that a more severe inflmmatory reaction and an exuberant firoblastic and endothelial cell proliferation occur in the later.
- In secondary healing, once the blood clot is removed, proliferation starts, the granulation tissue fils up the entire area, contraction ofwound occur and the epithelium begins to grow over it, until the wound surface is completely epithelized.
- Later on, the inflmmatory exudates disappear slowly and the firoblasts produce large amounts of collagen.
Most of the healing processes occurring due to secondary intention,result in scar formation at the healing site.
However, in the oral cavity scars are very rare.
Phases of Wound Healing
Following are the phases of wound healing:
Inflammatory Phase
- It begins at the time of injury and lasts 2–4 days.
- This phase is characterized by hemostasis and inflmmation.
- First hemostasis occurs and there is formation of the platelet plug.
- Injury to vascular tissue initiates the extrinsic coagulation pathway by releasing intracellular calcium and tissue factor that activate factor VII. Resulting firin plug leads to hemostasis which is aided by reflx vasoconstriction.
- Now this plug acts as a lattce for aggregation of platelets,this is the indication of early inflmmatory phase.
- In inflammatory phase, both bacteria and debris are phagocytosed and removed, now the factors are released that cause the migration and division of cells involved in the proliferative phase.
- Collagen which were exposed at the time of wound formation causes activation of the clottng cascade (both the intrinsic and extrinsic pathways), initiating the inflmmatory phase.
- Injured tissues, via activated phospholipase A, catalyze arachidonic acids to produce potent vasoconstrictors thromboxane A2 and prostaglandin 2-alpha, which is collectively known as eicosanoids.
This initial response limits hemorrhage. - After a short period of time capillary vasodilatation occurs which is due to local histamine release, and the cells of inflmmation migrate to the wound bed.
- Chemical mediators, i.e. platelets release platelet-derived growth factor (PDGF) and and transforming growth factor beta (TGF-β) from their alpha-granules attact neutrophils and macrophages.
- Now, neutrophils scavenge for bacteria and foreign debris and macrophages continue to release growth factors to attact firoblasts and enter in the next phase of wound healing.
Proliferative Phase
- It starts from day 3 and last for 3 to 6 weeks. It overlaps with the inflammatory phase.
This phase is characterized by angiogenesis, collagen deposition, granulation tissue formation, and epithelialization. - Fibroblasts initiate angiogenesis, epithelialization, and collagen formation. Fibroblasts migrate inside from wound margins over the firinous matrix which is established during this phase.
- During fist week, firoblasts begin secreting glycosaminoglycans and proteoglycans, the ground substance for granulation tissue, as well as collagen, in response to macrophage-synthesized FGF and TGF-β, as well as PDGF.
- Fibroblasts grow and form a new, provisional extracellular matrix (ECM) by excreting collagen and fironectin.
- There is re-epithelialization of the epidermis, in which epithelial cells proliferate and reaches to the wound bed,providing cover for the new tissue.
This process starts from the basement membrane, if the basement membrane remains intact, otherwise the process initiates from the wound edges. - Fibroblasts produce mainly type III collagen in this phase.
- As firin clot and provisional matrix degrades, there is deposition of granulation tissue (ground substance, collagen, capillaries), which continues until the wound is covered.
Granulation tissue formed during this phase, is important in secondary wound healing.
Remodeling Phase
- Remodeling continues for 6–12 months after injury.
- In this, there is maturation of collagen by cross linking and realignment of collagen fiers along the line of tension which is responsible for tensile strength ofscar. Vascularity of wound reduces.
Fibroblast and myofiroblast leads to wound contraction.
Here Type III collagen is replaced by Type I collagen causing maturity of collagen.
Ratio of Type I collagen to Type III collagen is 4:1. - Early extracellular matrix consists of fironectin and collagen Type III; eventually it consists of glycosaminoglycans and proteoglycans; fial matrix consists of Type I collagen.
- Strength of scar is 3% in one week, 20% in 3 weeks, 80% in 12 weeks. Finally, matured scar is acellular and avascular.
Question.29. Classify wounds and discuss management of different types of wounds.
Answer.
Management of different types of Wounds
- Wound is inspected and classified as per the type of wounds.
- If wound is in the vital area, then:
- The airway should be maintained.
- The bleeding, if present, should be controlled.
- Intravenous flids are started.
- Oxygen, if required, may be given.
- Deeper communicating injuries and fractures, etc.should be looked for.
- If it is an incised wound, then primary suturing is done after thorough cleaning.
- If it is a lacerated wound, then the wound is excised and primary suturing is done.
- If it is a crushed or devitalized wound there will be edema and tension in the wound.
- So after wound debridement or wound excision by excising all devitalized tissue, the edema is allowed to subside for 2—6 days.
- Then delayed primary suturing is done.
- If it is a deep devitalized wound, after wound debridement it is allowed to granulate completely.
- Later, if the wound is small secondary suturing is done.
- If the wound is large a split skin graft (Thiersch graft) is used to cover the defect.
- In a wound with tension, fasciotomy is done so as to prevent the development of compartment syndrome.
- Vascular or nerve injuries are dealt with accordingly.
- Vessels are sutured with 6-zero polypropylene nonabsorbable suture material.
- If the nerves are having clean, cut wounds it can be sutured primarily with polypropylene 6-zero or 7-zero suture material. If there is diffilty in identifying the nerve ends or if there are crushed cut ends of nerves then marker stitches are placed using silk at the site and later secondary repair of the nerve is done.
- Internal injuries (intracranial by craniotomy, intrathoracic by intercostal tube drainage, intra-abdominal by laparotomy) has to be dealt with accordingly.
- Fractured bone is also identifid and properly dealt with.
- Antibiotics, flid and electrolyte balance, blood transfusion, tetanus toxoid (0.5 mL intramuscular to deltoid muscle), or antitetanus globulin (ATG) injection.
- Later defiitive management is done with: Wound debridement (wound toilet, or wound excision) is liberal excision of all devitalized tissue at regular intervals (of 48–72 hours) until healthy, bleeding, vascular tidy wound is created.

Leave a Reply