Hypersensitivity
Question 1. Write a short note on hypersensitivity reactions.
Or
Write notes on hypersensitivity reactions.
Or
Write a short note on hypersensitivity.
Or
Write in brief on hypersensitivity reactions.
Answer:
Hypersensitivity refers to a condition in which the immune response results in excessive reactions that lead to tissue damage, disease, or even death in the sensitized host.
Read And Learn More: Microbiology Question And Answers
Classification of Hypersensitivity Reactions: Based on the time required for a sensitized host to develop a clinical reaction on re-exposure to antigen hypersensitivity is classifid as:
- Immediate hypersensitivity (B cell or antibody-mediated)
- Anaphylaxis
- Atopy
- Antibody-mediated cell damage
- Arthus phenomenon
- Serum sickness
- Delayed hypersensitivity (T cell-mediated)
- Infection (tuberculin) type
- Contact dermatitis type
Hypersensitivity reactions are classified into four major types by Coombs and Gel (1963):
- Type I: Immediate
- Type II: Cytotoxic
- Type III: Immune complex
- Type IV: Delayed or cell-mediated.
- Type V: Stimulatory Type Dermatitis:
Type I, II, and III depend on the interaction of antigen with humoral antibodies and are known as immediate-type reactions, while Type IV is mediated by T- T-lymphocytes and is known as delayed hypersensitivity. Later on, Type V hypersensitivity reaction was also described, i.e. stimulatory type.
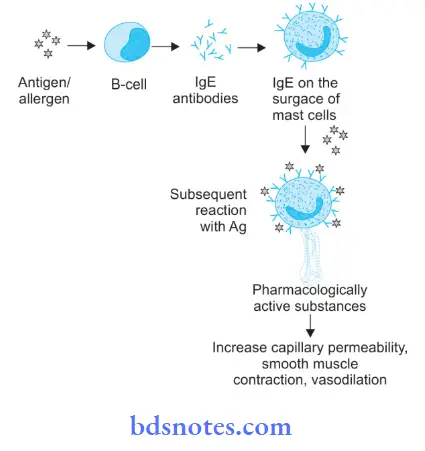
- Type I: Immediate or Anaphylaxis: Antibodies of IgE type fi over the surface of tissue cells, i.e. mast cells and basophils in the sensitized individuals. Antigens combined with cell field antibodies cause the release of chemical mediators which leads to a hypersensitivity reaction, for example. anaphylaxis in man due to insect bite.
- Type II: Cytotoxic:
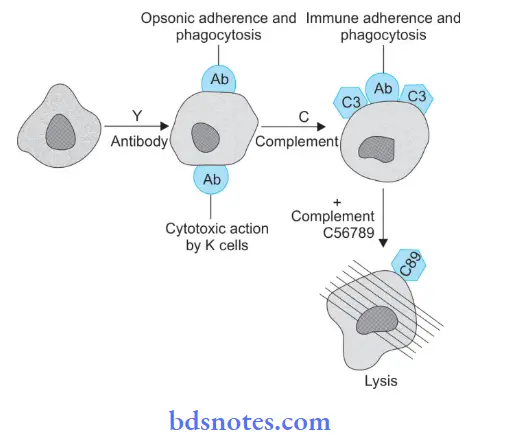
- It is mediated by the antibodies that react with the antigens which are fixed over the surface of a cell or other tissue components which leads to the damage of the cell. Combination with antibodies with IgG or IgM sometimes can lead to cell damage by promoting contact with phagocytic cells or by activating complement components.
- Contact with phagocytic cells is promoted due to a reduction in surface charges by opsonic adherence directly via Fc or immune adherence through bound C3. Cell death can also occur through activation of the full complement pathway till C8 and C9, for example, lysis of RBCs by anti-erythrocyte antibodies.
- Type III: Immune Complex:
- In type III hypersensitivity reaction damage is due to antigen-antibody complexes. Such complexes are deposited inside the tissues leading to immune complex disorders. Formation of the complex in and around blood vessels leads to acute inflammatory reactions. Sometimes the complexes cause mechanical blockage of blood vessels due to platelet aggregation causing interference with blood supply to surrounding tissues.
- Activation of the complement system massive infiltration by polymorphonuclear leukocytes and attraction of platelets lead to inflammation and tissue injury. Type III hypersensitivity reaction is of two types, i.e. Arthus reaction and serum sickness.
- Type IV: Delayed or Cell Mediated:
- Damage to tissue is caused by T-lymphocytes, so no damage is done by the antibody, that is why it is known as cell-mediated hypersensitivity. Antigen present activates sensitized T-lymphocytes which cause secretion of lymphokines along with flid and collection of phagocytes. It is of two types, i.e. tuberculin (infection) type and contact dermatitis type.
- Type V: Stimulatory Type Dermatitis:
- Various IgG antibodies stimulate their target cells rather than killing or inhibiting them. These antibodies react with key surface components and stimulate the functional activity of cell. The best example is thyrotoxicosis in which antibodies react with thyroid cells and stimulate the activity of these cells.
- This leads to excessive secretion of thyroid hormone which can cause thyrotoxicosis.
Question 2. Classify hypersensitivity reaction. Describe in detail about Type IV hypersensitivity reaction.
Answer:
For the classification of a hypersensitivity reaction
Based on the time required for a sensitized host to develop a clinical reaction on re-exposure to antigen hypersensitivity is classified as:
- Immediate hypersensitivity (B cell or antibody-mediated)
- Anaphylaxis
- Atopy
- Antibody-mediated cell damage
- Arthus phenomenon
- Serum sickness
- Delayed hypersensitivity (T cell-mediated)
- Infection (tuberculin) type
- Contact dermatitis type
Hypersensitivity reactions are classified into four major types by Coombs and Gel (1963):
- Type I: Immediate
- Type II: Cytotoxic
- Type III: Immune complex
- Type IV: Delayed or cell-mediated.
- Type V: Stimulatory Type Dermatitis:
Type I, II, and III depend on the interaction of antigen with humoral antibodies and are known as immediate-type reactions, while Type IV is mediated by T- T-lymphocytes and is known as delayed hypersensitivity. Later on, Type V hypersensitivity reaction was also described, i.e. stimulatory type.
- Type I: Immediate or Anaphylaxis: Antibodies of IgE type fi over the surface of tissue cells, i.e. mast cells and basophils in the sensitized individuals. Antigen combined with cell fied antibody causes the release of chemical mediators which leads to a hypersensitivity reaction, for example. anaphylaxis in man due to insect bite.
- Type II: Cytotoxic:
- It is mediated by the antibodies that react with the antigens which are fixed over the surface of a cell or other tissue components which leads to the damage of the cell. Combination with antibodies with IgG or IgM sometimes can lead to cell damage by promoting contact with phagocytic cells or by activating complement components.
- Contact with phagocytic cells is promoted due to a reduction in surface charges by opsonic adherence directly via Fc or immune adherence through bound C3. Cell death can also occur through activation of the full complement pathway till C8 and C9, for example, lysis of RBCs by anti-erythrocyte antibodies.
- Type III: Immune Complex:
- In type III hypersensitivity reaction damage is due to antigen-antibody complexes. Such complexes are deposited inside the tissues leading to immune complex disorders. Formation of the complex in and around blood vessels leads to acute inflammatory reactions. Sometimes the complexes cause mechanical blockage of blood vessels due to platelet aggregation causing interference with blood supply to surrounding tissues.
- Activation of the complement system massive infiltration by polymorphonuclear leukocytes and attraction of platelets lead to inflammation and tissue injury. Type III hypersensitivity reaction is of two types, i.e. Arthus reaction and serum sickness.
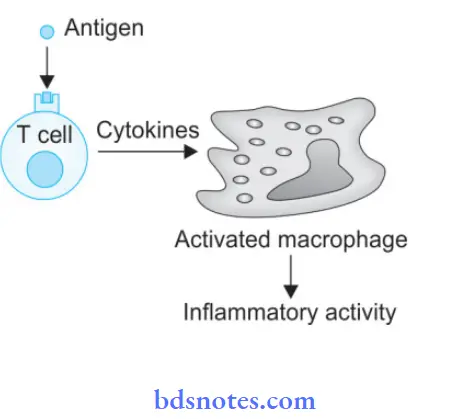
- Type IV: Delayed or Cell Mediated:
- Damage to tissue is caused by T-lymphocytes, so no damage is done by the antibody, that is why it is known as cell-mediated hypersensitivity. Antigen present activates sensitized T-lymphocytes which cause secretion of lymphokines along with flid and collection of phagocytes. It is of two types, i.e. tuberculin (infection) type and contact dermatitis type.
- Type V: Stimulatory Type Dermatitis:
- Various IgG antibodies stimulate their target cells rather than killing or inhibiting them. These antibodies react with key surface components and stimulate the functional activity of the cell.
- The best example is thyrotoxicosis in which antibodies react with thyroid cells and stimulate the activity of these cells. This leads to excessive secretion of thyroid hormone which can cause thyrotoxicosis.
Type IV Hypersensitivity Reaction
- Type IV hypersensitivity reaction is the delay between exposure to antigen and the development of the symptoms.
- This reaction is mediated by sensitized T-lymphocytes which on contact with specific antigens release lymphokines that cause biological effects on macrophages, leukocytes, and tissue cells.
- Type IV or delayed type of hypersensitivity occurs within 48-72 hours of antigen challenge. As it is not antibody-mediated, it cannot be passively transferred by serum but can be transferred by lymphocytes or the transfer factor.
- Two types of delayed hypersensitivity reactions are well recognized, tuberculin (infection) type and contact dermatitis type.
Tuberculin (Infection) Type:
- This reaction develops due to the infection by tuberculous bacillus and is demonstrated by tuberculin reaction.
- When a small dose of tuberculin, i.e. 1 to 5 TU is injected intradermally in an individual sensitized to tuberculoprotein by prior infection or immunization, an erythema and swelling (induration) occurs at the site of injection within 24-72 hours. Purified protein derivative (PPD) which is the active material of tubercle bacilli is used in the tuberculin tests.
- The injection site is infiltrated by a large number of lymphocytes and about 10-12% macrophages. These inflammatory cells are seen around blood vessels and nerves.
- In unsensitized individuals, the tuberculin injection provokes no response.
- The tuberculin test is a useful indicator for delayed hypersensitivity to the bacillus.
- Cell-mediated hypersensitivity reaction develops in many infections with bacteria (M. tuberculosis, M. leprae), fungi, and parasites.
- It occurs when the infection is subacute or chronic and the pathogen is intracellular.
- Various skin tests are performed to detect delayed types of hypersensitivity.
- A positive skin test does not indicate a present infection but implies the person has been infected or immunized by microorganisms in the past.
- Some of these skin tests include:
- Lepromin test: It is positive in tuber cuboid leprosy but negative in the lepromatous type of leprosy.
- Frei test: This test is positive in lymphogranuloma venereum (LGV).
- Histoplasmin test: It is positive in histoplasmosis.
Contact Dermatitis Type:
- Delayed hypersensitivity may sometimes develop as a result of skin contact with a range of sensitizing materials— metals such as nickel and chromium, drugs such as penicillin or other antibiotics in ointments, simple chemicals like hair dyes, picryl chloride, dinitrochlorobenzene, cosmetics, and soaps.
- These substances are not antigens but act as haptens, they combine with skin proteins and become antigenic.
- Cell-mediated immunity is induced in the skin. As most of the antigens involved are fat soluble, their likely portal of entry is along the sebaceous glands.
- Contact with these substances in sensitized individuals leads to contact dermatitis which is characterized by macules and papules to vesicles that break down leaving raw weeping areas of acute eczematous dermatitis.
- The Langerhans cells of the skin carry these antigens to regional lymph nodes where T-lymphocytes are sensitized. On subsequent exposure to the offending agent, sensitized lymphocytes release lymphokines which cause superficial inflammation of the skin characterized by redness, induration, and vesiculation within 24-48 hours.
- It is always possible to identify the substance responsible for sensitivity by patch test. In this test suspected substance is applied to the skin under adherent dressing and observed for itching (after 4–5 hours) and local reaction, i.e. erythema to the vesicle or blister formation (24–48 hours).
Question 3. Write a short note on Type II hypersensitivity reaction.
Answer:
- It is also known as a cytotoxic reaction.
- In cytotoxic reactions, the antigen is either the part of a tissue cell microbial product, or a drug attached to the cell wall.
- So the combination of this antigen with IgG or IgM antibody produces damage to the cell which promotes contact with phagocytic cells or by activating complement components.
- Contact with phagocytes is promoted by a decrease in the surface charges due to opsonic adherence directly via Fc or via immune adherence through bound C3.
- Cell death can occur through activation of the full complement pathway till C8 and C9.
- Various examples of Type II hypersensitivity reactions are:
- Lysis of RBCs by anti-erythrocytic antibodies.
- Platelet gets lysed by autoantibodies causing autoimmune thrombocytopenia.
Question 4. Write a short note on Type III hypersensitivity reaction.
Answer:
It is also known as immune complex-mediated hypersensitivity.
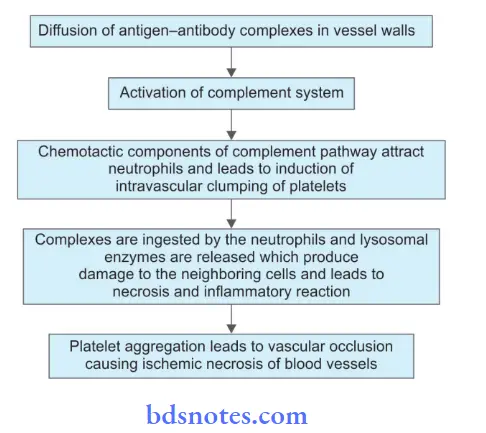
- This reaction is characterized by the deposition of antigen-antibody complexes in tissues mainly on the endothelial surfaces.
- The formation of complexes in and around blood vessels leads to acute inflammatory reactions.
- Sometimes mechanical blockage of vessels occurs due to platelet aggregation causing interference with blood supply to surrounding tissues.
- Activation of complement is done by antigen-antibody complex which leads to the release of anaphylatoxins that causes the release of histamine
which causes vascular permeability changes. - Due to complement activation, there is also the aggregation of PMN leukocytes which engulf antigen-antibody complexes and release proteolytic enzymes and polycationic proteins which causes increased capillary permeability.
- Complement system activation and heavy infiltration by PMN leukocytes and attraction of platelets cause inflammation and tissue injury.
- Type III hypersensitivity is of two types, i.e. Arthus reaction and serum sickness.
Arthus Reaction
- It is given by Arthus in 1903.
- This is a local inflammatory reaction that shows the involvement of blood vessels. This occurs usually after giving the injection of antigen, i.e. horse serum given intradermally in the hyperimmunized animals.
- Arthus reaction presents as erythema, edema, induration, hemorrhagic necrosis, etc.
- It occurs in humans who have received injections of antitoxic serum or insulin.
Inflammatory Mechanism by Arthus Reaction:
Serum Sickness
- It was given by Clemens von Pirquet and Schick in 1905.
- It occurs in humans after the injection of horse serum and sometimes following the injection of drugs, i.e. sulphonamide, penicillin, streptomycin, or organic arsenicals.
- Its single dose is sufficient to produce symptoms.
- Symptoms appear in 1 to 2 weeks. Various symptoms are fever, lymphadenopathy, splenomegaly, arthritis, glomerulonephritis, endocarditis, vasculitis, urticaria, abdominal pain, nausea, and vomiting.
- It is a self-limiting disease. There is an increase in antibody levels.
- Antigen-antibody complexes get bigger in size and are susceptible to phagocytosis as well as there is immune elimination.
- Tissue damage is the same as in the Arthus reaction.
Question 5. Write a short note on Type I hypersensitivity reaction.
Or
Define hypersensitivity, and describe Type I hypersensitivity in detail.
Answer:
- Hypersensitivity refers to a condition in which immune response results in excessive reactions which leads to tissue damage, disease, or even death in the sensitized host.
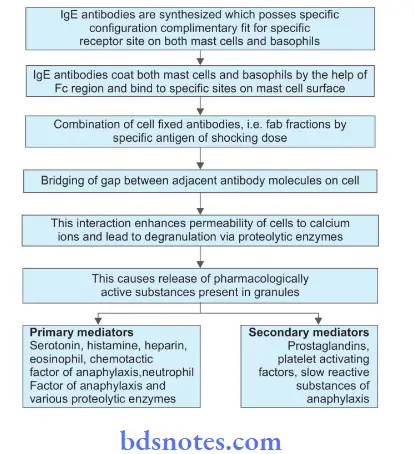
- This is also known as Anaphylaxis or IgE or Reagin dependent hypersensitivity reaction. It is an IgE-mediated immediate hypersensitivity reaction.
- In anaphylaxis when antigen, i.e. egg albumin is injected in the guinea pig no adverse effects are observed but when a second dose of the same antigen is injected intravenously after 2 to 3 weeks. Sensitized guinea pig reacts dramatically which is known as anaphylactic shock.
- In anaphylactic shock animal is restless, cyanosed, develops convulsion, and dies.
- The initial injection of antigen given is known as the sensitizing dose and the second injection is the shocking dose.
- During the interval between two injections, animals form antibodies.
- Anaphylaxis occurs due to the interaction of a shocking dose with newly formed antibodies on the surface of tissue cells.
- This interaction triggers the release of pharmacologically active substances which increase capillary permeability and lead to smooth muscle contraction.
Types of Anaphylaxis
- Local (atopy): It occurs when the antigen is confined to a particular site. It manifests with skin allergy, hives, nasal and conjunctival discharge, etc. It has two distinct phases, i.e. immediate and a late phase.
- Systemic: It mostly follows parenteral administration but can also result from the ingestion of an allergen. It includes itching, erythema, contraction of respiratory bronchioles, diarrhea, pulmonary edema, pulmonary hemorrhage, shock and death.
Mechanism of Anaphylaxis:
Examples of Type I Reaction Based on the types of Type I hypersensitivity reactions, i.e. systemic or local anaphylaxis the examples are:
Systemic Anaphylaxis:
- Administration of antisera, for example. Anti-Tetanus Serum (ATS).
- Administration of drugs, for example. Penicillin.
- Sting by a wasp or bee.
Local Anaphylaxis:
- Hay fever (seasonal allergic rhinitis) due to pollen sensitization of conjunctiva and nasal passages.
- Bronchial asthma a due to an allergy to inhaled allergens like house dust.
- Food allergy to ingested allergens like fish, cow’s milk, eggs, etc.
- Cutaneous anaphylaxis due to contact of antigen with skin characterized by urticaria, wheal, and flare.
- Angioedema is an autosomal dominant inherited disorder characterized by laryngeal edema, edema of eyelids, lips, tongue, and trunk

Leave a Reply