Bacterial Infections Of Oral Cavity Question And Answers
Question 1. Write short note on Cancrum Oris.
Answer. It is also called as NOMA or gangrenous stomatitis.
- It is a rapidly spreading gangrene of oral and facial tissues occurring in deliberated or nutritionally deficient person.
- It is caused by Fusobacterium necrophorum.
Cancrum Oris – Predisposing Factors
- It occurs in undernourished persons.
- Various debilitated infections i.e. diphtheria, dysentery, measles, pneumonia, scarlet fever, syphilis, tuberculosis and blood dyscrasias can predispose to cancrum oris.
- Presence of excessive mechanical injury.
- Poor oral hygiene promotes the growth of bacteria which increases the suseptaibility to infection.
- AIDS leading to immunodeficiency can predispose to cancrum oris.
- Various miscellaneous factors i.e. stress, sickle cell trait and chemotherapeutic agents can cause noma.
Read And Learn More: Oral Medicine Question And Answers
Cancrum Oris – Clinical Features
- It is seen chiefly in children mainly in malnourished children.
- Common sites are areas of stagnation around fixed bridge or crown.
- Commencement of gangrene is denoted by blackening of skin. Small ulcers of gingival mucosa spread rapidly and involve surrounding tissue of jaws, lips and cheeks by gangrenous necrosis.
- Odor is foul. Patient has high temperature during course of disease, suffers secondary infection and may die from toxemia.
- Overlying skin is inflamed, edematous and finally necrotic which results in formation of line of demarcation between healthy and dead tissue.
- In advanced stage, there is blue-black discoloration of skin.
- As gangrenous process advances, slough appears and soon separated, leaving perforating wound in involved area.
- The large masses may be sloughed out leaving jaws exposed.
Cancrum Oris – Management
- Parenteral fluid should be given urgently to correct dehydration and electrolytic balance.
- Blood transfusion helps in improving clinical state of patient who is anemic and toxic.
- Specific drug of choice is penicillin.
- Reconstructive surgery is done to lead normal life.

Question 2. Discuss in detail Cervicofacial Actinomycosis.
Answer. Actinomycosis is a chronic granulomatous suppurative and fibrous type of disease caused by anaerobic, gram- positive, non-acid fast bacteria.
Most common microorganisms are Actinomyces israelii, A. actinomycosis, A. viscosus and A. odontolyticus.
Cervicofacial Actinomycosis Predisposing Factors
- Trauma: Break in the continuity of mucosa due to trauma or by surgery.
- Local factors: Infections leading to cervicofacial actinomycosis are endogenous in origin and occur when dental plaque, calculus or the gingival debris contaminates deep wounds around the mouth. Carious tooth can also cause cervicofacial actinomycosis.
- Others: Hypersensitivity reaction and secondary bacterial invasion may act as predisposing factors.
Cervicofacial Actinomycosis Clinical Features
- It is most common type of actinomycosis and is seen in adult males.
- Submandibular region is most frequent site of infection.
- Trismus is most common feature before formation of pus.
- The first sign of infection is characterized by formation of palpable mass. Mass is painless and indurated.
- There may be associated changes detectable at portal of entry such as non-healing tooth socket, exuberant granulation tissue or periosteal thickening of alveolus.
- Development of fistula is common. Skin surrounding fistula is purplish. Consistency of adjacent tissues is doughy.
- Sulphur granules: Hard circumscribed tumor-like swelling may develop and undergo breakdown, discharging yellow fluid containing submicroscopic sulfur granules.
Cervicofacial Actinomycosis Oral Manifestations
- It produces swelling and induration of tissue.
- It may develop into one or more abscess, which tends to discharge upon the skin surface liberating pus, which contains typical sulphur granules.
- There may be non-healing tooth socket, exuberant granular tissue and periosteal thickening of alveolus.
- It is common for sinus, via which abscess is drained, to heal but due to chronicity, new abscess are formed and perforate through skin surface.
- Disfigurement of face is present as infections involve maxilla and mandible
- On tongue, lesion is painful nodule which eventually ulcerates. In untreated cases tongue may be fixed.
Cervicofacial Actinomycosis Radiographic Features
- Radiographic appearance resemble with apical rarefying osteitis. Scattered area of bone destruction separated from one another by normal or sclerosed bone.
- It appears as an area of bone destruction, which resemble dental cyst, with well-defined area of radiolucency with cortical lining of dense bone.
- Lamina dura is deficient at apex of tooth.
- Persistent radiolucency of tooth socket with increased density of adjacent bone can be the first sign of disease.
Cervicofacial Actinomycosis Diagnosis
- Clinical diagnosis: Sulfur granules with formation of fistula and sinus along with fever provide clue to diagnosis.
- Radiological diagnosis: Scattered area of bone destruction which is separated from one another by normal or sclerosed bone.
- Laboratory diagnosis: On examination, there is presence of round or lobulated colony meshwork of filaments stained by hematoxylin and peripheral club ends of filaments stained by eosin shows typical ray fungus appearance which is characteristic.
Cervicofacial Actinomycosis Management
- Two fold therapy is given, i.e. including antibiotics and surgery.
- Lesion is surgically removed and thorough debridement is required.
- Penicillin should be given, i.e. 3 to 4 million IV, 4 hours till 2 to 4 weeks.
- This should be followed by 0.5 to 12 g of pencillins, four times a day for period of 4 to 6 weeks.
- If patient is allergic to penicillin, tetracycline orally 500 mg QDS for 6 months.
Question 3. Describe oral manifestations of acquired syphilis.
Or
Write short note on oral manifestations of syphilis.
Answer. The acquired form is contracted primarily as a veneral disease. Also, persons such as dentist working on infected patients in a contagious stage may also acquire the disease.
The acquired syphilis comprises of:
- Primary
- Secondary
- Tertiary
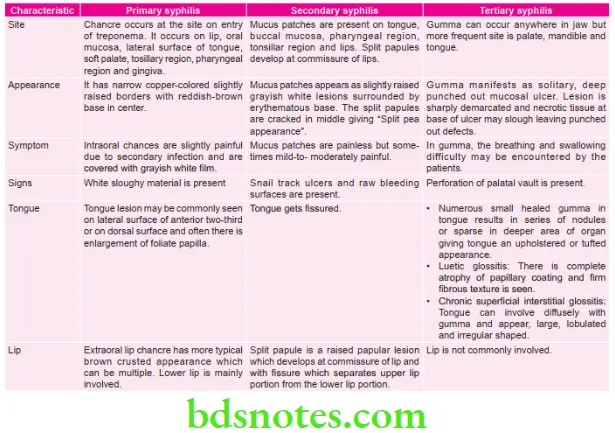
Oral Manifestations of Acquired Syphilis/Syphilis
Question 4. Write short note on causes of cervical lymphadenopathy.
Answer. Following are the causes of Cervical lymphadenopathy:
Cervical lymphadenopathy Inflammation and infection
- Bacterial Infections
- Specific Bacterial Infection
- Tuberculosis
- Syphilis
- Non-Specific Bacterial Infection
- Pericoronitis
- Periodontal disease
- Periapical infections
- Specific Bacterial Infection
- Viral infections
- Infection mononucleosis
- AIDS
- Herpes simplex
- Cat scratch disease
- Fungal infections
- Oral candidiasis
- Histoplasmosis
- Parasitic infections: Rickettsial infection
- Allergic Conditions
- Serum sickness
- Primary Neoplasms
- Lymphoma
- Metastatic Tumors
- Oral squamous cell carcinoma.
- Metastasis of carcinoma of breast.
- Miscellaneous Conditions
- Leukemia
- Collagen diseases
- Sarcoidosis
- Non-tender lymphoid hyperplasia.

Leave a Reply