Orofacial Pain Question And Answers
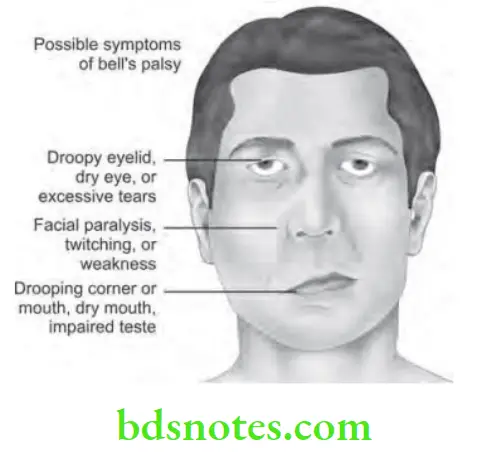
Question 1. Write short note on Bell’s palsy.
Answer. The Bell’s palsy is also called as 7th nerve paralysis or facial palsy.
Bell’s palsy Pathogenesis
- In normal course: Cortical tract communicating with motor nucleus ambiguous of the facial nerve crosses over to get innervated in lower facial musculature. Upper face fibers are ipsilateral proximal to nucleus.
- Lower face palsy: A cortical lesion leads to contralateral lower face palsy.
- Total hemifacial palsy: Lesions of brainstem, main trunk or peripheral fibers leads to total hemifacial palsy.
Bell’s palsy Etiology
- Cold: It occurs after exposure to cold.
- Trauma: Trauma to facial nerve during extraction of teeth or after injection of local anesthetic leads to Bell’s palsy.
- Surgical procedures: Surgical procedures such as removal of parotid gland tumor in which facial nerve is sectioned, may lead to Bell’s palsy.
- Ischemia: It can be caused due to ischemia of nerve near stylomastoid foramen which leads to edema of nerve, compression of nerve in bony canal and finally the paralysis.
- Familial: Hereditary occurrence is seen.
- Facial canal and the middle ear neoplasm: They lead to Sensorineural hear loss in which facial nerve palsy is a feature.
- Tumors: Various tumors of cranial base, parapharyngeal space and infratemporal fossa leads to facial nerve palsy.
- Other factors: Multiple sclerosis, change in atmospheric pressure and pregnancy leads to bell’s palsy.
Read And Learn More: Oral Medicine Question And Answers
Bell’s palsy Clinical Features
- Age and Sex: Women are more commonly affected than man, it occurs in middle age group.
- Prodromal symptoms: It is preceded by pain on the side of face which is ultimately involved, particularly within ear, temple, mastoid area or at angle of jaw.
- Eye on affected side cannot be closed and wrinkles are absent on that side. There is watering of eye.
- When patient smiles, the paralysis become obvious since the corners of the mouth does not rise nor does the skin of forehead wrinkles or the eyebrows raise.
- The patient has mask like or expressionless appearance.
- Corners of mouth: The muscular paralysis manifests itself by drooping in corner of mouth, from which saliva may dribble.
- Food is retained in upper and lower buccal and labial folds.
Bell’s palsy Investigations
- An audiogram should be performed, a CT or MRI and an EMG should be considered.
- A baseline ophthalmologic examination is often helpful to determine further therapy.
- If electroneurography reveals a greater than 90 % loss of compound action potential within first two weeks following onset of paralysis, facial nerve decompression is done.
- If incomplete eye closure is present, artificial lubrication, taping the eye or perhaps the placement of the spring, gold weight or tarsorrhaphy might prevent visual loss from exposure keratitis.
Bell’s palsy Management
There is no universal treatment for the Bell’s palsy.
- Only medical treatment for Bell’s palsy is administration of systemic steroids within the first few days after onset of paralysis, but this should be avoided if Lyme disease is present. Steroids can be combined with antiviral drugs can decrease the severity and duration of paralysis.
- Eye should be protected by lubricating drops or ointment, if closure of eye is not there, patch should be given.
- If paralysis induced eye opening is permanent, intrapalpebral gold weights should be inserted to close the upper eyelid.
- Surgical decompression of infratemporal facial nerve can be done.
- Facial plastic surgery and the surgical anastomosis between facial and hypoglossal nerves occasionally restore partial function and improve the appearance of patients with the permanent damage.
Question 2. Write short note on management of trigeminal neuralgia.
Or
Write short note on clinical features and treatment of trigeminal neuralgia.
Or
Write short note on trigeminal neuralgia.
Or
Write short note on clinical features of trigeminal neuralgia.
Or
Write short answer on trigeminal neuralgia.
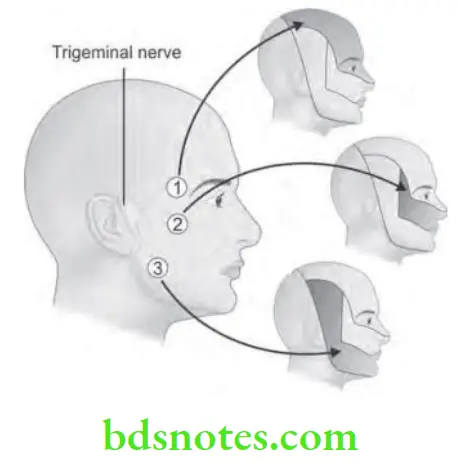
Answer. The trigeminal neuralgia is also called as Tic douloureux, Trifacial neuralgia or Fothergill’s disease.
Trigeminal Neuralgia Etiology
- Dental pathologies at times lead to the trigeminal neuralgia.
- If excessive traction is given on the divisions of trigeminal nerve, it can cause trigeminal neuralgia.
- Allergy or hypersensitivity reactions lead to edema of trigeminal nerve root which causes trigeminal neuralgia.
- According to Wolf, ischemia at various areas of trigeminal pathway leads to paroxysm of pain.
- Intracranial vascular abnormalities:
- Pontine infarcts – compression/distortion at root entry zone of trigeminal nerve at pons by arterial loop.
- Arteriovenous malformation in vicinity
- Compression of the intracranial retrogasserian portion of trigeminal nerve by displaced vein/artery.
- Aneurysm of internal carotid artery
- Intracranial tumors: They can impinge on the nerve. E.g. meningioma of cerebellopontine region and Meckle’s cave, trigeminal neuromas of middle and posterior cranial fossa.
- Inflammatory lesions: Multiple sclerosis and sarcoidosis can lead to trigeminal neuralgia.
- Virus: Postherpetic neuralgia and some other viral lesions of ganglion can lead to trigeminal neuralgia.
Trigeminal Neuralgia Clinical Features
- Age: It usually occurs in middle and old age, disease seldom occurs before 35 years of age.
- Sex: Females are more commonly affected.
- Site: It is most common in right side and lower portion of face is most commonly affected.
- Nature of pain: Pain is paroxysmal, lasting only few seconds to few minutes and is of extreme intensity. It may be described by the patient as resembling to knife-like stablightning electric shock, stabbing or lancinating type of pain.
- Aggravating factors: The pain is provoked by obvious stimuli to face. A touch or a draft of air, any movement of face as in talking, chewing, yawning and swallowing may evoke lancinating attacks.
- Trigger zones: These are the zones which precipitate an attack when touched. The trigger zones are vermilion border of lips, ala of nose, cheeks and around the eyes. The patient avoid touching the skin over trigger zones which makes him go unwashed or unshaven for many days.
- The pain is confined to the trigeminal zone, nearly always unilateral and if bilateral is successive, rather than concomitant.
- During neurological examination, all the findings are normal with no sensory loss along the trigeminal nerve.
- In extreme cases, patient may have mask like or motionless face.
Trigeminal Neuralgia Management
Elimination of all possible sources of infection.
Medical Treatment
- Trichloroethylene inhalation is given.
- Anticholinergic drugs are given.
- Dilantin is given orally, i.e. 300 to 400 mg per day. It is given in single or divided doses.
- Carbamazepine (tegretol) has affected on paroxysmal pain. 100 mg is given twice a day until relief is established. Daily dose should not exceed 1200 mg/day.
- Baclofen as anti-spasmodic drug is also used.
- Clonazepam which is an antiepileptic may also be used.
- Anti-inflammatory agents such as Indomethacin 100mg/ day and short courses of steroids are useful.
Trigeminal Neuralgia Surgical Treatment
- Injection of nerve with anesthetic solution is given in peripheral branches of trigeminal nerve serve as to provide temporary relief.
- Injection of nerve with alcohol leads to neurolysis of affected nerve and patient get relief for 6 to 24 months.
- Peripheral neurectomy, i.e. nerve sectioning and nerve avulsion. This procedure is more lasting and affective than injection with alcohol.
- Electrocoagulation of Gasserian ganglion: Diathermy apparatus is placed in Gasserian ganglion to coagulate and destroy it.
- Percutaneous radiofrequency trigeminal neurolysis: In this, controlled radiofrequency is used. It is performed by insertion of temperature monitoring electrode through foramen ovale in trigeminal ganglion.
- Rhizotomy: Actual cutting of trigeminal sensory root results in permanent anesthesia in more patients.
Trigeminal Neuralgia Newer Technique
The newer technique used is known as gamma knife stereotactic radiosurgery.
- It is the minimal invasive technique for treating trigeminal neuralgia.
- It uses the beam of radiation dose of 70 to 90 Gy units, which converge in three dimensions to focus precisely on small volumes.
- The method relies on accurate MRI sequencing which helps in localization of beam and allows higher dose of radiation to be given with more sparing of nerve tissue.
- Its advantage is that, it is helpful for elderly patients with high surgical risk.
Question 3. Define neuralgia. Describe in detail etiopathogenesis of trigeminal neuralgia with differential diagnosis, clinical features and treatment modalities.
Answer. Neuralgia is defined as severe pain occurring along the course of a nerve.
Treatment Modalities Etiopathogenesis
There is distortion phenomenon which is usually caused by arterial loops of atherosclerotic vessels. Vessels become elongated with advancing age and with atherosclerotic involvement gain abnormal positions by wedging into the space between pons and trigeminal nerve. It is postulated that the progressive material elongation, fascicles of adjacent nerves later suffer myelin injury and pain results.
Treatment Modalities Differential Diagnosis
- Migraine: This is the most common condition which is mistaken for trigeminal neuralgia. This type of periodic headache is persistent, for period of hours and it has no trigger zone.
- Sinusitis: In this pain present is not paroxysmal and trigger zone is absent.
- Toothache: This is identified by examining the oral cavity. It is usually due to severe dental caries.
- Multiple sclerosis: It is autoimmune process. It consists of Charcot’s triad i.e. intentional tremor, nystagmus and dysarthria.
- Nasopharyngeal tumor: They produce same pain which is manifested in lower jaw, tongue, side of the head with associated middle ear deafness. As tumor progresses trismus develops and patient is unable to open the mouth.
- Postherpetic neuralgia: Pain occurs in ophthalmic division. History of skin lesion is present before onset of neuralgia.
For clinical features and treatment modalities refer to Ans 2 of the same chapter.
Question 4. What is pain? Enumerate the causes and give differential diagnosis of orofacial pain.
Answer. Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage.
It is an unpleasant emotional experience initiated by noxious stimuli and transmitted over a specialized neural networks to CNS, where it is interrupted as such.
Orofacial Pain Causes
Orofacial Pain Extracranial Causes
Dental and oral:
- Dental hypersensitivity.
- Pain from disorders of pulp.
- Hyperemia
- Acute pulpitis
- Chronic pulpitis.
- Pain from disorders of periodontium.
- Mucogingival pain.
- Stomatitis
- Gingivitis
- Glossitis
- Glossodynia.
- Osseous and periosteal pain.
- Dry socket
- Periostitis
- Osteomyelitis
- From disorder of ear and eye.
- Enlargement of salivary glands.
- Pain from paranasal sinus:
- Sinusitis
- Tumors of sinus.
Orofacial Pain Musculoskeletal Causes
- Myofacial pain
- TMJ arthropathy
- Cervical spine disorders
- Eagle’s syndrome.
Orofacial Pain Intracranial Causes
- Traction disorders of pain sensory structure of brain.
- Neoplasms, aneurysms, hematoma, hemorrhage or edema.
- Displacement of great venous sinus.
- Distortion and dilation of intracranial vessels.
Orofacial Pain Vascular Pain
- Migraine headache.
- Cluster headache.
- Tension headache.
- Temporal headache.
- Angina pectoris.
Orofacial Pain Neurogenic Pain
- Paroxysmal:
- Trigeminal neuralgia.
- Glossopharyngeal neuralgia.
- Geniculate neuralgia.
- Differential pain syndrome:
- Atypical odontalgia.
- Traumatic neuroma.
- Neuritis.
- Reiter’s sympathetic dystrophy.
Orofacial Pain Psychogenic Pain
- Anxiety and depression.
- Hallucination pain.
Question 5. Write short note on glossopharyngeal neuralgia.
Answer. Glossopharyngeal neuralgia is a typical neuralgia.
Glossopharyngeal neuralgia is a variety of trigeminal neuralgia that can mimic oral pathologic condition in which pain is confined to distribution of ninth cranial nerve.
Glossopharyngeal neuralgia Clinical Features
- Neuralgia occurs without any sex predilection in middle age or older persons.
- It manifest as sharp excoriating electric like, lancinating paroxysm of pain in ear, pharynx, nasopharynx, tonsils or posterior portion of tongue.
- Pain is generally unilateral.
- Glossopharyngeal neuralgia has tendency towards remissions and exacerbations.
- Pain free intervals of seconds, minutes, hours, days and years are common.
- Patient usually has trigger zone in the posterior or pharynx or tonsillar fossa.
- An important and frequent trigger is initiation of act of swallowing.
Glossopharyngeal neuralgia Treatment
Immediate pain relief is present when topical anesthetic agent is applied to the tonsil and pharynx on the side of pain. This is the main diagnostic method and differentiates glossopharyngeal neuralgia from other neuralgias.
No therapy is effective and adequate.
It is less responsive to the treatment with anti-convulsant medications.
If drug therapy fails, surgical intervention should be considered.
Preferred neurosurgical treatment is microvascular decompression or surgical sectioning of glossopharyngeal nerve and upper two rootlets of vagus nerve.
Question 6. Write short note on Eagle’s syndrome.
Answer. It is characterized by elongation of styloid process or ossification of stylohyoid ligament.
- It includes dysphagia, sore throat, otalgia, glossodynia, headache and vague orofacial pain.
- There is presence of pain in lateral pharyngeal wall and side of lower face.
- There are two types of syndrome:
- The classic type occurring after tonsillectomy resulting from surgical exposure of styloid process.
- The carotid artery syndrome type resulting from calcification of stylohyoid ligament and elongated styloid process which encroaches on external or internal carotid vessels producing vascular pain.
- It may mimic glossopharyngeal neuralgia.
- Patients with Eagle’s syndrome will characteristically rotate their head slowly to avoid provoking pain.
- Pain can be demonstrated when pressing pharyngeal wall against the styloid process and when swallowing or opening the mouth wide.
Recently, Eagle’s syndrome is known as DISH syndrome i.e. diffuse interosseous skeletal hypertrophy syndrome. It is also known as stylohyoid syndrome, carotid artery syndrome.
Elongation of the styloid process causes impingement or compression of adjacent nerves causing Eagle’s syndrome.
Eagle’s syndrome Types
- Classic type: It occurs after tonsillectomy resulting from surgical exposure of styloid process. Formation of scar leads to the pressure on nerve leading to pain at the time of swallowing.
- Carotid artery syndrome: It results from calcification of stylohyoid ligament and elongated styloid process which encroaches external or internal carotid vessels producing vascular pain.
- Traumatic Eagle’s syndrome: This develops after fracture of mineralized stylohyoid ligament.
Eagle’s syndrome Clinical Features
- It occurs commonly in adults.
- Sometimes, elongated styloid process is seen in pharyngeal region.
- There is presence of pain in lateral pharyngeal wall as well as over the side of lower face and the neck. It can lead to glossopharyngeal neuralgia.
- There is also presence of dysphagia, sore throat, otalgia, glossodynia, headache and vague orofacial pain.
- Main characteristic sign of Eagle’s syndrome is that, patient will characteristically rotate their head slowly to avoid provoking pain. Pain can be demonstrated while pressing pharyngeal wall against styloid process and at the time of swallowing or opening the mouth wide.
Eagle’s syndrome Radiographic Features
In panoramic radiograph, elongation of styloid process is nicely appreciated.
Eagle’s syndrome Management
- Infiltration of local anesthetic solution around the styloid process provides relief in pain while applying topical anesthesia does not relieve pain.
- In surgical treatment, surgical segmentation or the resection of elongated styloid process is carried out.
- At times the local injection of corticosteroid provides relief.
- It is treated by surgical segmentation or resection of elongated styloid process.
Question 7. Write short note on causes of restricted mouth opening.
Answer. Restricted mouth opening is called as trismus.
Causes of Orofacial Pain.
Extracranial Causes
- Dental and oral:
- Dental hypersensitivity.
- Pain from disorders of pulp:
- Hyperemia.
- Acute pulpitis.
- Chronic pulpitis.
- Pain from disorders of periodontium.
- Mucogingival pain:
- Stomatitis.
- Gingivits.
- Glossitis.
- Glossodynia.
- Osseous and periosteal pain:
- Dry socket.
- Periostitis.
- Osteomyelitis.
- From disorder of ear and eye.
- Enlargement of salivary glands.
- Pain from paranasal sinus:
- Sinusitis.
- Tumors of sinus.
Musculoskeletal Causes
- Myofacial pain.
- TMJ arthropathy.
- Cervical spine disorders.
- Eagle’s syndrome.
Intracranial Causes
- Traction disorders of pain sensory structure of brain.
- Neoplasms, aneurysms, hematoma, hemorrhage or edema.
- Displacement of great venous sinus.
- Distortion and dilation of intracranial vessels.
Vascular Pain
- Migraine headache.
- Cluster headache.
- Tension headache.
- Temporal headache.
- Angina pectoris.
Neurogenic Pain
- Paroxysmal:
- Trigeminal neuralgia.
- Glossopharyngeal neuralgia.
- Geniculate neuralgia.
- Differentiation pain syndrome:
- Atypical odontolgia.
- Traumatic neuroma.
- Neuritis.
- Reiter’s sympathetic dystrophy.
- Psychogenic Pain
- Anxiety and depression.
- Hallucination pain.
- Hypochondriac pain or hysteric pain.
Question 8. Define pain, enumerate various facial neuralgias and write in detail about trigeminal neuralgia.
Answer. Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage.
By IASP (International association of study for pain).
Various Facial Neuralgias
- Trigeminal neuralgia.
- Glossopharyngeal neuralgia.
- Geniculate neuralgia.
- Symptomatic neuralgia.
For trigeminal neuralgia, refer to Ans 2 and Ans 3 of the same chapter.
Question 9. Discuss differential diagnosis of facial pain.
Answer. Following is the differential diagnosis of facial pain
- Pain arising from teeth and supporting structures.
- Pain from neighboring structures such as TMJ, ear, salivary gland, tonsils, eyes, elongated styloid process (Eagle syndrome).
- Neuralgias: Primary neuralgias, e.g. tic douloureux. Secondary neuralgias, e.g. mental nerve compression or entrapment, causalgias, Frey’s syndrome, nasopharyngeal carcinoma (Trotter’s syndrome), post-herpetic neuralgias.
- Vascular pain: Migraine, facial migranous neuralgias, temporal arteritis.
- Psychogenic pain like atypical facial pain, atypical odontalgia. This can be designate as whole orofacial pain of emotional perspective. Pain due to TMJ dysfunction syndrome or myofacial pain dysfunction syndrome and the recent term facial arthomyalgia (FAM).
- Oral dysaesthesia: This group includes burning tongue—glossodynia, dry mouth, denture intolerance, phantombite syndrome, abnormalities of taste, including the obsessional fear of halitosis or a conviction of a ‘discharge’ from a particular corner of the mouth.
- Sinus-related pathologies, i.e. acute or chronic sinusitis
- Primary headache conditions i.e. tension type headache, migraine, cluster headache.
- Carotidynia
- Facial pain secondary to intracranial or extracranial infections or tumors.
- Facial pain secondary to cervical spine disease, i.e. C2-C8 cervical nerve root compression, facial injury or both.
Question 10. Classify neuralgias of maxillofacial region. Write in detail etiopathogenesis, clinical features, importance of imaging and medicinal treatment of trigeminal neuralgia.
Answer.
Classification of Neuralgias of Maxillofacial Region
- Typical neuralgias
- Trigeminal neuralgia
- Glossopharyngeal neuralgia
- Geniculate neuralgia
- Superior laryngeal neuralgia
- Post-herpetic neuralgia
- Atypical neuralgias
- Migrainous neuralgia
- Sphenopalatine neuralgia
- Migraine
- Ciliary neuralgia
- Petrosal neuralgia
- Carotidynia
- Cluster headache
For etiopathogenesis refer to Ans 3 and for clinical features and treatment, refer to Ans 2 of same chapter.
Importance of Imaging in Trigeminal Neuralgia
- Diagnostic imaging, i.e. CT or MRI when multiple sclerosis is suspected should be performed for all patients of trigeminal neuralgia.
- By imaging, tortuous vessel or vascular loop in area of trigeminal nerve root entry zone is detected.
- By MRI, imaging, small compressive vascular structures are detected.
- By imaging, dural arteriovenous fistulae can be detected.
- By imaging neoplasias and demyelinating plaques are detected in root entry zone.
- One of the importance in imaging of trigeminal neuralgia is at root entry zone at times neurovascular compression is seen at cerebellopontine angle cistern, so by MR cisternography in this area trigeminal neuralgia of unknown cause is detected.
Question 11. Define pain. Classify orofacial pain and write in detail on burning mouth syndrome.
Or
Write short answer on burning mouth syndrome.
Answer. Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage. By IASP (International association of study for pain).
Classification of Orofacial Pain
- Superficial Pain
- Mucogingival pain
- Cutaneous pain.
- Deep Pain
- Odontogenic pain:
- Pulpal pain
- Periodontal pain
- Odontogenic pain:
- Musculoskeletal pain:
- Muscle pain
- Neoplastic myofacial pain
- Muscle-splinting pain
- Muscle spasm pain
- Local muscle soarness
- TMJ pain
- Capsule pain
- Disc attachment pain
- Retrodiscal pad pain
- Arthrography pain
- Soft connective tissue pain
- Osseous pain
- Vascular pain
- Atypical facial neuralgia
- Cranial arteritis
- Visceral pain
- True visceral pain
- Reflex sympathetic dystrophy
- Muscle pain
- Neurogenous Pain
Traumatic neuroma pain:
- Neuritis pain
- Peripheral neuritis
- Herpes zoster
- Neuralgia Pain
- Idiopathic neuralgia
- Symptomatic neuralgia
Psychogenic pain:
- Psychogenic intensification pain
- Delusional pain
- Conversion hysteria pain
Burning Mouth Syndrome
Patient describes it as a burning sensation of oral mucosa in absence of apparent mucosal alteration.
Burning Mouth Syndrome Etiology
Local Factors
- Contact allergy: Denture material can cause allergy.
- Chronic mechanical trauma: It occurs due to denture and clasp
- Oral habits: Habits such as clenching, grinding and tongue thrust may lead to burning mouth syndrome.
- Infection: Infections such candidal infection and fusospirochetal infection can cause burning mouth syndrome.
- Xerostomia: It is caused due to irradiation, immunological deficiency and various systemic causes.
- Other factors: Various other factors such as OSMF, esophageal reflex, angioedema, TMJ dysfunction and trauma caused to lingual nerve can cause burning mouth syndrome.
Burning Mouth Syndrome Systemic Factors
- Diabetes mellitus
- Nutritional deficiency: Deficiency of various vitamins and some essential minerals such as vitamin B12, iron, etc. can lead to burning mouth syndrome.
- Psychological distress
- Gastrointestinal problem: Chronic gastritis can lead to burning mouth syndrome.
- Endocrine disorders: Hypothyroidism can lead to burning mouth syndrome.
- Others: Various other factors such as menopause, AIDS, medications, Parkinson’s disease can also lead to burning mouth syndrome.
Burning Mouth Syndrome Clinical Features
- It occurs most commonly in elderly patients mostly during 5th decade of life.
- Females are affected more as compared to males.
- Most frequently affected structure of oral cavity is tongue, denture bearing areas, buccal mucosa and floor of the mouth.
- Pain is present in the morning and its intensity increases to maximum during evening time.
- Patient also complaints of insomnia, lethargy, headache and mood swings.
- Pain increases by tension, hot foods and fatigue and relieves by sleeping, eating and distraction.
- Patient complains of combination of xerostomia and burning is evaluated for the possibility of salivary gland disorder, particularly if thee mucosa is dry and patient has difficulty in swallowing dry foods without sipping the liquids.
Burning Mouth Syndrome Management
- Etiological factor should be removed first.
- Various nutritional supplements should be given such as ferrous sulphate 300 mg TID, Cyanocobalamin 250 mg/day, pyridoxine HCl 25 to 100 mg/day, riboflavin 10 mg/day, thiamin HCl 5 to 30 mg/day, folic acid 0.1 to 34 mg/day.
- Chlordiazepoxide is a mood-altering drug which shows relief in patients.
- Burning of the tongue which results from parafunctional oral habits can be relieved by the use of splint which covers the teeth and the palate.

Leave a Reply