Vesicular Bullous And Ulcerative Lesions Question And Answers
Question 1.
1. Enumerate the ulcerative and vesiculobullous lesions of oral cavity.
2. Describe etiology, clinical features differential diagnosis and treatment plan of recurrent aphthous stomatitis.
Or
Classify ulcerative and vesiculobullous lesions. Describe the etiology, clinical features and treatment plan of recurrent aphthous stomatitis.
Or
Classify oral ulcerative lesions. Discuss in detail about RAS.
Answer.
Classification of Ulcerative Lesions
Classification Of Ulcer
Microbial Origin
- Classification Of Ulcer Bacterial
- Streptococcal
- Tuberculosis
- Syphilis
- Scarlet fever
- Diphtheria
- Typhoid
- Noma
- Classification Of Ulcer Fungal
- Histoplasmosis
- Blastomycosis
- Paracoccidiomycosis
- Coccidiomycosis
- Cryptococcus
- Zygomycosis
- Aspergillosis
- Classification Of Ulcer Viral:
- Herpes
- HIV
- Pox virus
Read And Learn More: Oral Medicine Question And Answers
- Classification Of Ulcer Protozoal
- Entamoeba Histolytica
- Leishmaniasis
- Toxoplasmosis
- Classification Of Ulcer Physical Origin
- Cheek bite (Morsacitio Buccorum)
- Traumatic
- Thermal
- Electrical
- Osteoradionecrosis
- Anesthetic
- Classification Of Ulcer Chemical Origin
- Phenol
- Silver nitrate
- Hydrogen peroxide
- Aspirin
- Classification Of Ulcer Immunological
- BehÇet’s syndrome
- Reiter’s syndrome
- Erythema multiforme
- Erosive lichen planus (Secondary Ulcer)
- Lupus erythematosus
- Sarcoidosis
- Cyclic neutropenia
- Ulcerative colitis
- HIV
- Pemphigus
- Epidermolysis bullosa
- Classification Of Ulcer Metabolic Ulcers
- Diabetes
- Uremia
- Neutropenia
- Sickle cell anemia
- Agranulocytosis
- Crohn’s disease.
- Classification Of Ulcer Non-specific Ulcers
- HIV ulcers
- Graft versus host reaction
- Necrotizing sialometaplasia
- Reynaud’s phenomenon
- Bacterial angiomatosis.
- Classification Of Ulcer Neoplastic
- Squamous cell carcinoma.
Vesiculobullous Lesions
Fitz Patrick Classification
According to Anatomical Plane:
Fitzpatrick Scale
- Intraepidermal blister granular layer:
- Pemphigus foliaceus
- Frictional blisters
- Staphylococcus-scalded syndrome.
- Spinous Layer:
- Eczematous dermatitis
- Secondary to heat and cold
- Herpes virus infection
- Familial benign pemphigus.
- Suprabasal:
- Pemphigus vulgaris
- Pemphigus vegetans
- Darier’s disease.
- Basal layer:
- Erythema multiforme
- Toxic epidermal necrolysis
- Lupus erythematosis
- Lichen planus
- Epidermolysis bullosa simplex.
Dermal-Epidermal Junction Zone
- Lamina lucida:
- Bullous pemphigoid
- Cicatrical pemphigoid
- Epidermolysis bullosa junctional.
- Below basal lamina
- Erythema multiforme
- Epidermolysis bullosa dystrophica.
Fitzpatrick Scale
Vesiculobullous Lesions
- Primary blistering:
- Pemphigus
- Bullous pemphigoid
- Cicatrical pemphigoid
- Epidermolysis bullosa acqusita.
- Secondary blistering:
- Contact
- Erythema mutltiforme
- Toxic-epidermal necrolysis.
- Infection:
- Varicella zoster
- Herpes simplex
- Bullous impetigo.
Systemic Disease:
- Infection: Cutaneous emboli
- Metabolic.
- Diabetic with bullae
- Porphyria cutanea tarda.
Recurrent Aphthous Stomatitis.
Recurrent Aphthous Stomatitis is a common disease characterized by development of painful, recurrent, solitary or multiple ulcerations of oral mucosa.
Recurrent Aphthous Stomatitis Etiology
As per the current concept recurrent aphthous stomatitis is a clinical syndrome with several possible causes out of which major ones are hereditary, hematologic deficiency, immunologic abnormalities and nutritional deficiencies.
- Microbial infection: Due to pleomorphic transitional L form of α hemolytic Streptococcus and Streptococcus sanguis. Various other microbes associated are cytomegalovirus, adenovirus and varicella zoster virus.
- Immunological abnormalities: IgG and IgM binding the epithelial cells of spinous layer of oral mucosa had been observed in recurrent aphthous stomatitis. Mainly mucosal destruction is due to T cell mediated immunological reaction.
- Genetic predisposition: If parent of the child is RAS positive, child has increased susceptibility to develop recurrent aphthous stomatitis. In RAS patient HLA-B51 antigen is identified. So, there is a familial tendency for occurrence of the disease.
- Systemic factors: Patients with recurrent aphthous stomatitis may have nutritional deficiencies such as iron, vitamin B12, folic acid.
- Endocrine factors: Relation between recurrent aphthous stomatitis, pregnancy, menstruation and menopause is observed. Recurrent aphthous stomatitis occurs more commonly at the time of menstruation.
- Stress: Due to psychological stress recurrent aphthous stomatitis occurs. It is seen mainly during exam time or if a person is under work stress.
- Smoking cessation: It increases the incidence of recurrent aphthous stomatitis.
Oral ulcerative lesions Clinical Features
- It occurs between 2nd and 3rd decades of life. It is more common in females.
- It occurs most commonly on buccal and labial mucosa, buccal and lingual sulci, tongue, soft palate, pharynx and gingiva.
- It begins with burning for 24 to 48 hours, before ulcer appears.
- It begins as single or multiple superficial erosion covered by grey membrane.
- Localized area of erythema develops and within hours small white papules form, ulcerate and enlarge over 48 to 72 hours.
- Lesion is painful so interferes with eating for few days.
- Lesion is rounded in shape, shallow and is symmetrical.
- There is presence of multiple lesions. Ulcer persists for 7 to 14 days and may recur after 1 to 4 months.
- Minor aphthae: Their size range from 0.3 to 1 cm. They heal within 10 to 14 days without leaving scar.
- Major aphthae: Their size is larger than 1 cm and may reach to 5 cm in diameter. They are painful. They heal slowly within 10 to 40 days and may leave scars which decrease the mobility of tongue and uvula.
- Herpetiform ulcers: They are seen in older age group females. These are the shallow ulcers with upto 100 in number. It begins as small pin head size erosion which gradually enlarge and coalesce. They can be present for 1 to 3 years with short remission.
oral ulcerative lesions Differential Diagnosis
- Pemphigus: Absence of vesicles and blebs
- Cyclic neutropenia: Appearance with marked period of 3 weeks of compromised general condition.
- Lupus erythematosus: Presence of white component.
- Erosive lichen planus: white changes in border lesion
- Herpetiform gingivostomatitis: Saliva flow, halitosis, papule or vascular lesion.
- Recurrent herpes simplex infection: They are the clusters of small discrete grey or the white vesicles without having red erythematous halo, vesicle rupture quickly and form small punctuate ulcer of 1mm or less in size while in recurrent aphthous stomatitis there is an erythematous macule which undergo central blanching and this is followed by thee necrosis and ulceration.
- Squamous cell carcinoma: This occurs in older age, having indurated edges and base of the ulcer is fixed to underlying structures.
- Herpangina: It affects children in early winters or late summers. They are localized till palate.
- Primary syphilitic lesion: It is mainly painless, exhibit indurated edema and have painless swollen lymphnodes.
Oral ulcerative lesions Treatment Plan
Treatment of recurrent aphthous stomatitis is divided into three parts i.e.
- Topical treatment
- Systemic treatment
- Surgical treatment
Oral ulcerative lesions Topical Treatment
This treatment option decreases the pain or shortens the duration of occurrence, but it does not prevent recurrence
- Topical corticosteroids such as 0.1% triamcinolone acetonide is used 3 to 4 times a day. Other topical medications such as betamethasone in syrup form and 0.01% dexamethasone elixir can be used.
- Topical anesthetics such as 2% lidocaine, benzocaine and benzydamine hydrochloride can alleviate pain.
- Sucralfate application for 4 times a day shows soothing effect on ulcer.
- Tetracycline mouthwash i.e. 250 mg/30 mL used four times a day for period of 5 to 7 days.
- Intralesional triamcinolone acetonide 0.1 to 0.5 mL is also effective.
- Beclomethasone dipropionate spray is used in severe cases where the reach is difficult.
Oral ulcerative lesions Systemic Treatment
- Systemic steroid: Prednisolone or betamethasone syrup is used commonly in swish and swallow method. Prednisolone can also be given as tablet form from 20 to 30 mg per day and betamethasone 2 to 3 mg/day for 4 to 8 days. Systemic therapy is of 15 days duration followed by intralesional injection every 2 week for 2 months which causes decrease in recurrence.
- Other medications: Various other medications used are dapsone 100 mg/day, pentoxifylline 300 mg, azathioprine 50 to 150 mg/day etc.
oral ulcerative lesions Surgical Treatment
- Laser surgery: Laser ablation decreases the duration and associated symptoms. Lasers provide good pain relief but require multiple visits.
- Local cauterization: Application of 0.5% hydrogen peroxide solution, silver nitrate 1 to 2% solution decreases the duration of solitary aphthae.
Question 2. Describe in detail clinical features, differential diagnosis and treatment of erythema multiforme.
Or
Write short note on clinical features and mangement of erythema multiforme.
Or
Write short answer on erythema multiforme.
Or
Write short note on clinical features of erythema multiforme.
Or
Write short note on erythema multiforme.
Answer. Erythema multiforme is an acute self-limiting inflammatory disease which involves skin, mucous membrane and sometimes internal organs.
Erythema Multiforme Treatment
Erythema Multiforme Types
- Erythema multiforme minor: This presents the localized eruptions on skin with mild or no mucosal involvement.
- Erythema multiforme major or Steven Johnson syndrome: It is more severe mucosal and skin disease and is potentially a life threatening disorder.
Erythema Multiforme Treatment
Erythema Multiforme Etiology
- Drugs: Various drugs such as sulfonamides, trimethoprim, phenylbutazone, digitalis, birth control pills can lead to erythema multiforme.
- Microorganisms: Various microorganisms such as herpes simplex virus, mycoplasma pneumonia.
- Some other factors: Radiation therapy, vaccination and some of the diseases such as Crohn’s disease, ulcerative colitis and infectious mononucleosis may predispose to eryhtema multiforme.
- Immune conditions: Graft vs host disease, BCG or hepatitis B immunization, sarcoidosis, systemic lupus erythematosus may predispose to erythema multiforme.
- Food additives or chemicals: These are nitrobenzene, benzoates, terpenes and perfumes.
Erythema Multiforme Treatment
Erythema Multiforme Clinical Features
- It is seen in children and young adults and is rare after age of 50. Males are more affected.
- Most common area involved are hands, feet, extensor surface of elbow and buns.
- It has got acute or explosive onset with generalized symptoms such or fever and malaise. Extremities are involved in symmetric distribution.
- It is characterized by macule, papule, vesicles, bullae and urticarial plaque which are 0.5 to 2 cm in diameter.
- Bull’s eye target or iris or bull’s eye lesion consists of central bulla or pale clearing area, surrounded by edema and band of erythema.
- Palm of the hand shows target like lesions more than any other skin surface.
- Recurrence is common, patient develops tracheobronchial ulceration as well as pneumonia.
- Patients are presented with ‘ocular genital lesions’. Skin lesions consists of necrosis of scrotal skin, penile skin or vulval and the labial surfaces.
- Ocular component is epithelial necrosis of cornea and conjunctiva which develop prominent ulceration and necrosis, at times leading to blindness or visual loss due to secondary infection.
Erythema Multiforme Treatment
Erythema Multiforme Oral Manifestations
- Lip is prominently involved, which is followed by buccal mucosa, palate, tongue and face.
- Starting of oral lesions is with formation of bullae over an erythematous base, they break rapidly into the ulcers varying from aphthous type to multiple superficial widespread ulcers in their major form.
- Patient complains of difficulty in eating and swallowing.
- There is also drooling of blood tinged saliva which causes excessive fluid and electrolyte loss which produces secondary infection and results in cervical lymphadenitis.
- Lesions appear larger, irregular, deeper and bleeds freely. In severe form lips are extensively affected and large areas of oral mucosa get denuded of epithelium.
- There is presence of sloughing of mucosa and diffuse redness along with bright red raw surface.
Erythema Multiforme Differential Diagnosis
- Primary herpetic gingivostomatitis. They are small, round, symmetrical and shallow but erythematic multiforme lesions are large, irregular deeper and often bleed.
- Pemphigus vulgaris: Less inflammation progressive course, immunological autoantibodies against intercellular substance.
- Allergic reactions: Absence of target lesions.
- Erosive lichen planus—white lichen design on border of erosion and skin changes.
- Xerostomia: Mucosa is dry.
- Mucous membrane pemphigoid: This generally shows slow development such as changes in an eye, chronic course and there is quick involvement of gingiva. Gingival involvement is rare in erythema multiforme.
- Recurrent aphthous ulcers: These are the discrete lesions while erythema multiforme is diffuse and severe.
- Herpetic gingivostomatitis: Skin changes are absent and mostly small children are affected. Eryhtema multiforme is seen in young adults and target lesions are hallmark.
- Systemic lupus erythematosus: Polymorphous skin changes are common. Butterfly rash is commonly seen across the malar region. In erythema multiforme target lesions are the hallmark.
Erythema Multiforme Diagnosis or Erythema Multiforme Treatment
- Diagnosis is mainly clinical with presence of Bull’s eye lesion along with hemorrhaging crusting of the lip.
- Positive serology: For HSV antibodies or Mycoplasma pneumoniae when it shows hypersensitive response to HSV or Mycoplasma pneumoniae.
- Biopsy: Perilesional tissue should be biopsied. It shows intracellular edema of spinous layer of epithelium and edema of superficial connective tissue. Liquefaction degeneration is seen in upper layer of epithelium with intraepithelial vesicle formation. There is perivascular infiltration of lymphocytes and macrophages.
Erythema Multiforme Treatment
- Firstly identify the cause and withdraw it.
- Provide supportive care, electrolytes, liquid diet and give nutritional support.
- For oral lesions topical anesthetic agents, antiseptic mouthwash with hydrogen peroxide or chlorhexidine and topical corticosteroids provide some relief in pain.
- In cases having minor erythema multiforme 20 to 40 mg of prednisolone is given for 4 to 6 days and then tapering of the dose should be done. In major erythema multiforme 40 to 80mg of prednisolone should be given with gradual tapering of 2 to 3 weeks.
- In all forms of erythema multiforme symptomatic treatment consists of oral antihistamines, analgesics and local skin care.
- Necrosed skin should be treated by topical antimicrobial creams and eyes are irrigated and patched.
- Erythema multiforme minor is self limiting and improve after 5 to 8 days and it completely resolves in 2 to 4 weeks.
- In major erythema multiforme bed rest and hospital management is required.
Question 3. Classify vesiculobullous lesion in oral mucosa. Describe pemphigus in detail.
Or
Classify vesiculobullous lesions of oral cavity. Write clinical features and management of pemphigus vulgaris.
Or
Write short note on pemphigus.
Or
Write short note on oral manifestations of pemphigus vulgaris.
Or
Classify vesiculobullous lesions of oral cavity and describe in detail etiology, clinical features, diagnosis and treatment of pemphigus.
Or
Classify vesiculobullous lesions. Discuss in detail about etiology, clinical features, differential diagnosis and treatment of pemphigus vulgaris.
Answer. Refer to Ans 1a of same chapter.
Pemphigus
It is an autoimmune disease involving skin and mucosa and is characterized by intraepidermal bulla formation.

Pemphigus Etiology
Presence of circulating antibodies against keratinocyte cell surfaces suggests that pemphigus is an autoimmune disease.
Pemphigus Vulgaris Clinical Features
- It is seen in 5th to 6th decades of life and whites are more commonly affected.
- This is insidious in its onset and can be fatal.
- Both males and females are equally affected.
- Lesions present as thin walled bullae or vesicles varying in diameter from few mm to several cm which arise on normal skin.
- Lesions contain thin watery fluid shortly after development but this may soon become purulent. They rapidly break and continue to extend peripherally, eventually leaving areas of denuded skin.
- Bullae are flaccid, fragile, regular and non-inflammatory. They consist of thin watery fluid initially and it soon becomes purulent and sanguineous.
- Nikolsky’s sign: After application of pressure to an intact bulla, the bulla will enlarge by extension to apparently normal surfaces. Another sign of disease is pressure on apparently normal area will result in formation of new lesion. This is known as Nikolsky’s sign.
- Two types of Nikolsky’s sign are appreciated i.e. Wet Nikolsky’s sign and Dry Nikolsky’s sign.
- In Wet Nikolsky’s sign after the separation of epidermis, base of skin is moist, glistening and is exudative while in Dry Nikolsky’s sign base of the eroded skin is dry. Wet Nikolsky’s sign is indicative of active disease while Dry Nikolsky’s sign is indicative of re-epithelialization beneath remnant blister top.
- If vertical pressure is given on the surface of blister, it extends laterally and this is known as Nikolsky’s sign II or Asboe-Hansen sign.
Pemphigus Vulgaris Oral Manifestations
- Initial lesion occurs on buccal mucosa. Palate and gingiva are other common sites of involvement. Oral mucosa is affected 2 to 3 months before the skin.
- Other lesions begin as classic bullae on non-inflamed base with formation of shallow ulcers as bullae break rapidly.
- Thin layer of epithelium peels away in an irregular pattern leaving denuded base.
- Lesion can have ragged borders and are covered with white or blood tinged exudates. Edges of the lesion can extend peripherally.
- Nikolsky’s phenomenon is present.
- Lesions bleed easily and are tender on palpation. Pain is so severe that patient is unable to eat.
Pemphigus Vulgaris Differential Diagnosis
- Erosive lichen planus: It has similar presentation but lichen planus targets the dorsum of tongue, buccal mucosa and attached gingiva.
- Pemphigoid: Mild form of pemphigus vulgaris resembles like pemphigoid but it does not produce conjunctivitis which is present in pemphigoid.
- Bullous pemphigoid: If oral lesions are not painful and are more prominent than the skin lesions and if individual is older than 50 years, pemphigoid should be considered.
- Erythema multiforme: It has acute onset, polymorphus appearance and shows systemic symptoms. It is seen in older patients.
- Herpetic gingivostomatitis: It shows acute onset and the primary lesions are associated with high fever, malaise, cervical lymphadenopathy, headache and subsides after 10 to 14 days.
- Linear IgA disease: Under immunofluorescence it shows linear homogeneous deposition of IgA antibodies at basement membrane zone.
- Drug induced stomatitis: It shows negative tzanck test as well as negative Nikolsky’s sign.
Pemphigus Vulgaris Diagnosis
- Clinical examination: Patients having pemphigus vulgaris and active blistering, firm sliding pressure by the finger separates normal looking epithelium, this is Nikolsky’s sign. Nikolsky’s sign is positive in pemphigus vulgaris.
- Biopsy: On histopathological examination, there is presence of vesicle or bulla intraepithelially above the basal cell layer producing suprabasilar split. Disappearance of intercellular bridges leads to acantholysis due to which clump of epithelial cells are found lying free in vesicular space. These are known as Tzanck cells which are the diagnostic feature for the condition.
- Tzanck smear: In this, base of the blister is scrapped and is examined for the acantholytic cells. These acantholytic cells or Tzanck cells are free floating, round or ovoid in shape and their nucleus is enlarged, hyperchromatic and is centrally or eccentrically situated.
- Compressed air test: Compressed air stream is applied to oral mucous membrane of gingival tissues which can lead to shimmering of outer tissues followed by formation of bleb or blister.
- Immunofluorescent testing: Direct immunofluorescence testing is done to demonstrate the presence of immunoglobulins, predominantly IgG but sometimes in combination with C3, IgA and IgM, in the intercellular spaces or intercellular substance in either oral epithelium or clincally normal epithelium adjacent to lesion.
- Indirect immunofluorescence: This is accomplished basically by incubating normal animal or human mucosa with serum from the patient suspected of having the disease and adding the fluorescein-conjugated human antiglobulin. A positive reaction in the tissue indicates presence of circulating immunoglobulin antibodies.
Pemphigus Vulgaris Treatment
- Mainstay of the treatment is administration of high dosages of systemic corticosteroids given in dosages of 1 to 2 mg/kg/day.
- When the substantial doses of steroids are used for long periods, adjuvant therapy is recommended to decrease the dose of steroid and its potential serious complications.
- Other adjuvants used are immunosuppressive drugs,parenteral gold therapy, dapsone, plasmapheresis and administration of 8-methoxypsoralen.
- Disease activity gets mild under optimal treatment.
- When steroids are used for long term, adjuvants such as azathioprine or cyclophosphamide are added to decrease the complications of long term steroid therapy.
- Rituximab is presently used and evaluated as the first line treatment.
Question 4. What do you understand by acantholysis. Write clinical features, histopathology and diagnosis of oral pemphigus.
Answer. Acantholysis is defined as any disease of the skin accompanied by degeneration of cohesive elements of the cells of outer or horny layer of skin which causes seperation of cells.
For clinical features and diagnosis refer to Ans 4 of the same chapter.
Oral Pemphigus Histopathology
- On histopathological examination, there is presence of vesicle or bulla intraepithelially above the basal cell layer producing suprabasilar split.
- Disappearance of intercellular bridges leads to acantholysis or loss of cohesiveness due to which clump of epithelial cells are found lying free in vesicular space. These are known as Tzanck cells which are the diagnostic feature for the condition. Tzanck cells have large nuclei and hyperchromatic staining.
- Small number of PMNs and lymphocytes may be found.
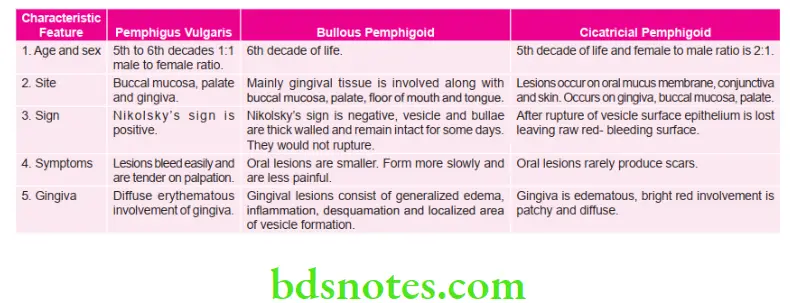
Question 5. Differentiate between pemphigus vulgaris, bullous pemphigoid and cicatricial pemphigoid (Benign mucous membrane pemphigoid).
Answer.
Question 6. Write short note on Nikolsky’s sign.
Answer. Nikolsky’s sign is a clinical dermatological sign, named after Pyotr Nikolsky.
- Nikolsky’s sign is almost always present in toxic epidermal necrolysis and is associated with pemphigus vulgaris.
- It is useful in differentiating between pemphigus vulgaris (where it is present) and bullous pemphigoid (where it is absent).
- Also present in scalded skin syndrome caused by the exfoliative toxin of S. aureus.
- When pressure is applied to the normal area or normal skin this will results in the formation of new lesion. This is called as Nikolsky’s sign.
- Nikolsky’s sign results due to the pulling of upper layer of skin from the basal layer which results in perivesicular edema which brakes the epidermal-dermal junction.
- Two types of Nikolsky’s sign are appreciated, i.e. Wet Nikolsky’s sign and Dry Nikolsky’s sign.
- In Wet Nikolsky’s sign after the separation of epidermis, base of skin is moist, glistening and is exudative while in Dry Nikolsky’s sign base of the eroded skin is dry. Wet Nikolsky’s sign is indicative of active disease while Dry Nikolsky’s sign is indicative of re-epithelialization beneath remnant blister top.
- If vertical pressure is given on the surface of blister, it extends laterally and this is known as Nikolsky’s sign II or Asboe-Hansen sign.
Question 7. Enumerate multiple recurrent oral ulcers. Discuss aphthous ulcers in detail.
Or
Classify ulcerative and vesiculobullous lesions. Describe in detail the etiology clinical features, differential diagnosis and management of recurrent aphthous ulcers.
Or
Write short note on aphthous ulcerations.
Or
Write short note on clinical features of aphthous ulcer.
Answer. For multiple recurrent aphthous ulcers refer to Ans 1a of same chapter.
For classification of ulcerative and vesiculobullous lesions refer to Ans 1 of same chapter.
Aphthous Ulcers
Aphthous ulcer is the most common type of non-traumatic, ulcerative condition of the oral mucosa.
Aphthous Ulcers Etiology
- The exact etiology is not known and only the probable factors have been identified which are as follows:
- Genetic predisposition: The disease often affects several members of the same family and moreover identical twins are most frequently affected.
- Exaggerated response to trauma: The ulcer develops in those mucosal sites which are subjected to trauma in the past. e.g. tooth prick injury.
- Immunological factors: The disease may occur due to some autoimmune reactions, or in patients with immunosuppression, e. g. AIDS. Some investigators believe, then it is an immune complex-mediated Type III or cellmediated type IV reaction.
- Microbiologic factors: The disease may be caused by herpes simplex virus Type I or S. sanguinis.
- Nutritional factors: Deficiency of vitamin B12, folate and iron, etc. often reported in patients with aphthous ulcer; moreover supplementation of these elements may cause rapid recovery.
- Systemic conditions: Behcet’s syndrome, Crohn’s disease and celiac disease are associated with increased incidences of aphthous ulcer.
- Hormonal imbalance: Hormonal change during menstrual cycle may be associated with higher incidence of aphthous ulcer.
- Non-smoking: The disease almost exclusively occurs in non-smokers or the people those who have given up smoke recently.
- Allergy and chronic asthma: Allergic manifestations to any medicines or foods (e.g. Nuts and chocolates, etc.) may lead to the development of aphthous ulcer.
- Miscellaneous factors: Stress and anxiety.
Aphthous Ulcers Clinical Features multiple recurrent
- Aphthous ulcers usually develop over the movable, non keratinized oral mucosa such as the tongue (lateral borders), vestibule, lips, buccal mucosa, soft palate and floor of the mouth, etc.
- Highest incidence of the disease is reported during early adult life.
- Before the appearance of the ulcer, the involved area produces a burning or tingling sensation, but the ulcers are never preceded by vesiculations.
- These ulcers recur in an interval of about 3 to 4 weeks.
- Clinically, aphthous ulcers present three recognizable forms, namely:
- Minor aphthous ulcers
- Major aphthous ulcers
- Herpetiform ulcers.
Aphthous Ulcers Minor
- It is the most common type of aphthous ulcer of the oral cavity and it appears episodically either as single lesion or in clusters of l to 5 lesions.
- The ulcers are very painful, shallow, round or elliptical in shape and they measure about 0.5 cm in diameter with a crateriform margin.
- The lesion is usually surrounded by an erythematous “halo” and is covered by a yellowish, fibrinous membrane.46 Mastering the BDS IVth Year-I (Last 25 Years Solved Questions)
- Minor aphthous ulcers mostly develop over the nonkeratinized mucosa, e.g. lips, soft palate, anterior fauces, floor of the mouth and ventral surface of the tongue (gland bearing mucosa), etc.
- The ulcer lasts for about 7–10 days and then heals up without scarring but recurrence is common.
- New lesions may continue to appear during an attack for about 3–4 weeks period.
- Few lesions may be present in the mouth almost continuously.
Aphthous Ulcers Major
- Major aphthous ulcers are less common than the minor form of the disease.
- These are larger, 0.5 cm in diameter and can be as big as several centimeters in diameter.
- Major aphthous ulcers are more painful lesions than the minor variety; and they persist in the mouth for longer durations as they take more time to heal.
- These lesions are considered to be the most severe among all types of aphthae and they often make the patients ill.
- Only one or two lesions develop at a time and are mostly seen over the lips, soft palate and fauces, etc. Besides involving the non-keratinzed mucosa, major aphthous ulcers can involve the masticatory mucosa as well, such as the dorsum of the tongue and gingiva, etc.
- The ulcer appears crateriform (owing to its increased depth), and it heals with scar formation in about 6 weeks time.
- Few lesions may look like malignant ulcers, moreover sometimes these lesions occur in association with HIV infections.
- Major aphthous ulcers often become secondarily infected and in such cases, the healing process is further delayed.
Aphthous Ulcers Herpetiform
- Herpetiform type of aphthous ulcers produce recurrent crops of extremely painful, small ulcers in the oral mucosa, which resemble herpetic ulcers. However, these ulcers do not develop following vesiculations and exhibit no virus infected cells.
- Their numbers vary from few dozens to several hundreds and each ulcer is surrounded by a wide zone of erythema.
- Size of these ulcers ranges between l to 2 mm in diameter only. However on few occasions, small ulcers coalesce together to form large irregular ulcers.
- The ulcers last for several weeks or months.
- Children in their late teens often suffer from this disease and the lesions occur in both gland bearing mucosa as well as over keratinized mucosa.
- The lesions usually heal up within l to 2 week time.
Differential Diagnosis multiple recurrent oral ulcers
- Pemphigus: Absence of vesicles and blebs
- Cyclic neutropenia: Appearance with marked period of 3 weeks of compromised general condition.
- Lupus erythematosus: Presence of white component.
- Erosive lichen planus: White changes in border lesion
- Herpetiform gingivostomatitis: Saliva flow, halitosis, papule or vascular lesion.
- Recurrent herpes simplex infection: They are the clusters of small discrete grey or the white vesicles without having red erythematous halo, vesicle rupture quickly and form small punctuate ulcer of 1mm or less in size while in recurrent aphthous stomatitis there is an erythematous macule which undergo central blanching and this is followed by the necrosis and ulceration.
- Squamous cell carcinoma: This occurs in older age, having indurated edges and base of the ulcer is fixed to underlying structures.
- Herpangina: It affects children in early winters or late summers. They are localized till palate.
- Primary syphilitic lesion: It is mainly painless, exhibit indurated edema and have painless swollen lymph nodes.
Aphthous Ulcers Treatment
Treatment of recurrent aphthous stomatitis is divided into three parts i.e.
- Topical treatment
- Systemic treatment
- Surgical treatment
Aphthous Ulcers Topical Treatment
This treatment option decreases the pain or shortens the duration of occurrence, but it does not prevent recurrence
- Topical corticosteroids such as 0.1% triamcinolone acetonide is used 3 to 4 times a day. Other topical medications such as betamethasone in syrup form and 0.01% dexamethasone elixir can be used.
- Topical anesthetics such as 2% lidocaine, benzocaine and benzydamine hydrochloride can alleviate pain.
- Sucralfate application for 4 times a day shows soothing effect on ulcer.
- Tetracycline mouthwash i.e. 250 mg/30 mL used four times a day for period of 5 to 7 days.
- Intralesional triamcinolone acetonide 0.1 to 0.5 mL is also effective.
- Beclomethasone dipropionate spray is used in severe cases where the reach is difficult.
Aphthous Ulcers Systemic Treatment
- Systemic steroid: Prednisolone or betamethasone syrup is used commonly in swish and swallow method. Prednisolone can also be given as tablet form from 20 to 30 mg per day and betamethasone 2 to 3 mg/day for 4 to 8 days. Systemic therapy is of 15 days duration followed by intralesional injection every 2 week for 2 months which causes decrease in recurrence.
- Other medications: Various other medications used are dapsone 100 mg/day, pentoxifylline 300 mg, azathioprine 50 to 150 mg/day etc.
Aphthous Ulcers Surgical Treatment
- Laser surgery: Laser ablation decreases the duration and associated symptoms. Lasers provide good pain relief but require multiple visits.
- Local cauterization: Application of 0.5% hydrogen peroxide solution, silver nitrate 1 to 2% solution decreases the duration of solitary aphthae.
Question 8. Write in brief clinical features of BehÇet’s syndrome.
Answer. Behçet’s disease was initially described by Turbish dermatologist Hulusi Behçet’s.
Behçet’s syndrome is characterized by oral and genital lesions, ocular lesions and skin lesions
Etiology and Pathogenesis
- Behçet’s disease is a systemic vasculitis which is characterized by hyperactivity of neutrophils with enhanced chemotaxis and elevated proinflammatory cytokines IL-8, IL-17, with TNF-α playing major role in pathogenesis.
- HLA-B51 genotype is frequently linked to Behçet’s disease.
BehÇet’s syndrome Clinical Features
BehÇet’s syndrome Oral Lesions
- Painful oral ulcers are present which occur in crops and their size varies from mm to cm.
- In oral cavity, any of the site is involved.
- Border of the ulcer is erythematous and are covered by grey or yellow exudates.
- Recurrence is present with the ulcers.
- All the three form of oral aphthous ulcers may be seen.
BehÇet’s syndrome Genital Lesions
- There is presence of recurrent genital aphthae, which are deep and heals by scarring.
- In males, ulcers are present in penis and scrotum while in females ulcers are seen in labia.
BehÇet’s syndrome Cutaneous Lesions
Cutaneous lesions consist of erythematous papules, vesicles, pustules, folliculitis and erythema nodosum like lesions.
BehÇet’s syndrome Ocular Lesions
- It consists of uveitis, retinal vasculitis, vascular occlusion, optic atrophy and conjunctivitis.
- Blindness is the common complication of the disease.
BehÇet’s syndrome Other Diseases
- Arthritis is present
- Paralysis and severe dementia can occur.
BehÇet’s syndrome Management
- Azathioprine and other immunosuppressive drugs combined with prednisolone shown to reduce ocular disease as well as oral and genital involvement.
- Dapsone, colchicine and thalidomide are used effectively to treat mucosal lesions of Behçet syndrome.
- Therapy with the monoclonal antibodies such as infliximab and etanercept play important role in Behçet syndrome mainly in the patients who does not respond to anti–inflammatory and immunosuppressive drugs.
Question 9. Describe biological features, clinical features, types and treatment of recurrent aphthous stomatitis.
Or
Write short answer on recurrent aphthous stomatitis.
Answer.
Biological Features of Recurrent Aphthous Stomatitis
A transitional L-form of α-hemolytic Streptococcus and S. sanguinis are the etiological factors of the disease. Various other microorganisms associated are varicella zoster virus, adenovirus and cytomegalovirus.
For clinical features and treatment in detail refer to Ans 1 of same chapter.
Types of Recurrent Aphthous Stomatitis
Following are the types of recurrent aphthous stomatitis:
- Minor aphthous ulcers.
- Major aphthous ulcers.
- Herpetiform ulcers.
For details refer to Ans 8 of same chapter.
Question 10. Classify vesiculobullous lesions of jaw. Discuss aphthous ulcers in detail.
Answer.
Classification of Vesiculobullous Lesions of Jaw
Vesiculo Bullous Lesions
Fitz Patrick Classification
According to Anatomical Plane:
- Intra epidermal blister granular layer
- Pemphigus foliaceous
- Frictional blisters
- Staphylococcus scalded syndrome
- Spinous layer
- Eczematous dermatitis
- Secondary to heat and cold
- Herpes virus infection
- Familial benign pemphigus
- Suprabasal
- Pemphigus vulgaris
- Pemphigus vegetans
- Darier’s disease
- Basal layer
- Erythema multiforme
- Toxic epidermal necrolysis
- Lupus erythematosis
- Lichen planus
- Epidermolysis bullosa simplex
Dermal-epidermal junction zone:
- Lamina lucida
- Bullous pemphigoid
- Cicatrical pemphigoid
- Epidermolysis bullosa junctional
- Below basal lamina
- Erythema multiforme
- Epidermolysis bullosa dystrophica
Vesiculobullous Lesions
- Primary blistering:
- Pemphigus
- Bullous pemphigoid
- Cicatrical pemphigoid
- Epidermolysis bullosa acqusita
- Secondary blistering:
- Contact
- Erythema mutltiforme
- Toxic epidermal necrolysis
- Infection:
- Varicella zoster
- Herpes simplex
- Bullous impetigo
- Systemic disease:
- Infection-cutaneous emboli
- Metabolic:
- Diabetic with bullae
- Porphyria cutanea tarda
For aphthous ulcers in detail refer to Ans 8 of same chapter.
Question 11. Define a vesicle and a bulla. Classify vesiculobullous lesions and discuss in detail etiopathogenesis, clinical features, diagnosis and management of pemphigus vulgaris.
Or
Classify vesiculobullous lesions of oral cavity. Discuss in detail the etiopathogenesis, clinical features, diagnosis and management of pemphigus vulgaris.
Answer. Vesicle: These are small blisters consisting of clear fluid and are less than 1 cm in diameter.
Bullae: These are elevated blisters which consist of clear fluid and are greater than 1 cm in diameter.
For classification of vesiculobullous lesions, refer to Ans 1 of same chapter.
For clinical features, diagnosis and management refer, to Ans 4 of same chapter.
Etiopathogenesis
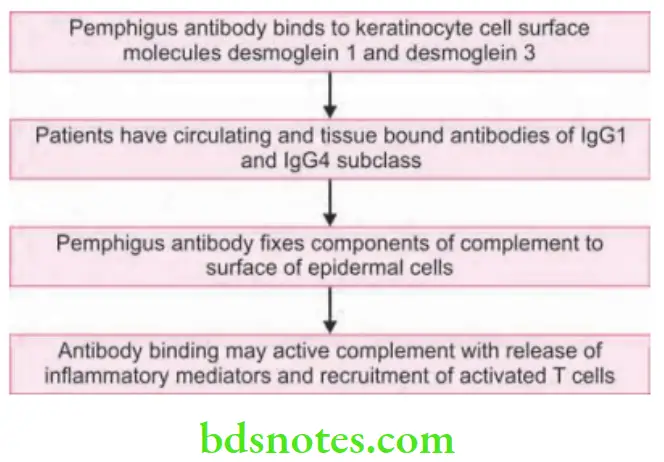
According to protease theory, deposition of autoantibody within the epithelium induces the proteolytic activity by activating tissue plasminogen. This inturn generate proteolytic enzyme called plasmin which destroy desmosomes.

Leave a Reply