Varicose Veins And Deep Vein Thrombosis
Varicosity is the penalty for verticality against gravity. This is the common statement made in lecture classes. The blood has to flow from the lower limbs into the heart against gravity because of the upright posture of human beings. In many cases, varicose veins are asymptomatic.
Read And Learn More: Clinical Medicine And Surgery Notes
- The raised intra-abdominal pressure also precipitates varicose veins, more commonly in females due to repeated pregnancy. Varicose veins and their complications cause significant morbidity to the patient.
- Many of them will have debilitating illnesses, ulcers, itching and bleeding. The complications of varicose veins are responsible for hospitalisation of the patient.
Definition
Dilated, tortuous and elongated superficial veins of the limb are called varicose veins.
Following are examples of varicosity
- Long saphenous varicosity
- Short saphenous varicosity
- Oesophageal varices and fundal varices
- Haemorrhoids
- Varicocele
- Vulval varix and ovarian varix
- In this chapter varicosity of the leg is discussed
Primary Varicose Veins
- They occur as a result of congenital weakness in the vessel wall.
- It can also be due to muscular weakness or due to congenital absence of valves.
- Very often, the valve at the saphenofemoral (SF) junction is incompetent/absent. The valves can also be absent where the superficial veins join the deep veins.
- Klippel-Trenaunay syndrome is a congenital venous abnormality wherein superficial and deep veins do not have any valves. It is also called valveless syndrome.
- Primary varicosity can also be familial. These factors, in addition to prolonged standing (agriculturists, hotel workers), help in the development of the varicose veins.
Secondary Varicose Veins
- Women are more prone to varicose veins because of the following reasons:
- Pregnancy and pelvic tumours cause proximal obstruction to the blood flow.
- Pills (oral contraceptive pills) alter the viscosity of blood.
- Progesterones dilate vessel wall
- Congenital arteriovenous (AV) fistula increases blood flow and increases venous pressure.
- Deep vein thrombosis can occur as a result of road traffic accidents, postoperatively, etc., and can result in the destruction of valves resulting in varicose veins.
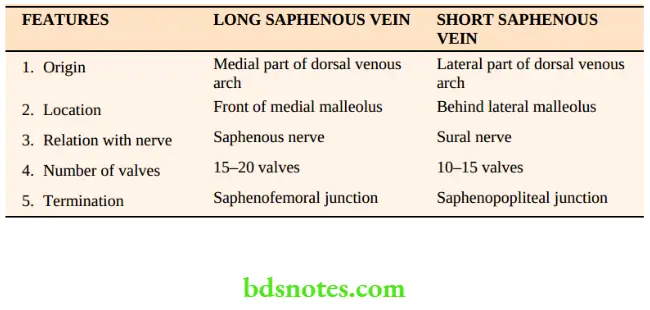
Surgical Anatomy Of The Venous System Of Leg
It can be discussed under the following headings
- Superficial system—long and short saphenous veins and their tributaries
- Perforators
- Deep system of veins.
Superficial Venous System Silent Features
- As the name suggests, they are in the superficial fascia, and often visible (saphenous means easily seen)
- They are low-pressure and poorly supported system
- They are provided with numerous valves
- The middle coat of these veins consists mostly of smooth muscles.
- The middle coat is also thicker than that of other veins
- Normal blood flow is from the superficial to the deep system of veins.
Anatomy Of The Long Saphenous Vein
It starts in the foot from the tributaries of the dorsal venous arch, permits reverse flow through its competent valves ascends in front of the medial malleolus and runs along the medial side of the leg. It then ascends in the thigh and ends at the saphenofemoral junction (SF) by joining the femoral vein, which is 1½ inches (4 cm) below and lateral to the pubic tubercle. It has 15 to 20 valves. Absence of valves results in varicose veins.
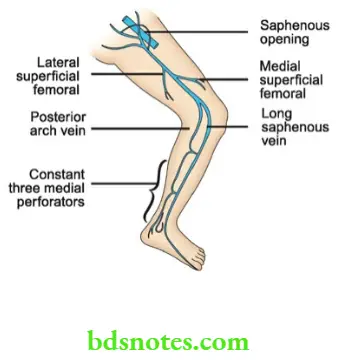
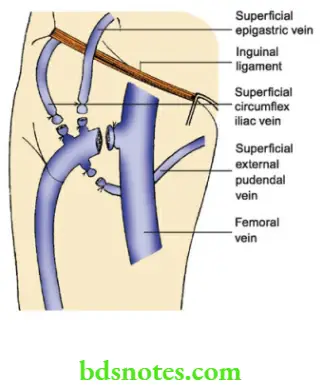
Tributaries
Tributaries near the termination
- Superficial circumflex iliac vein
- Superficial epigastric vein
- Superficial external pudendal vein
Tributaries in the leg
- Anterior vein of the leg.
- The posterior arch vein lies parallel to and behind the main trunk of the long saphenous vein. It anastomoses with small venous arches connecting the medial perforating veins.
Tributaries in the lower thigh
- Lateral superficial femoral
- Medial superficial femoral
- Transverse suprapatellar
- Transverse infrapatellar
These tributaries connect the long saphenous with short saphenous veins. They are also called communicators.
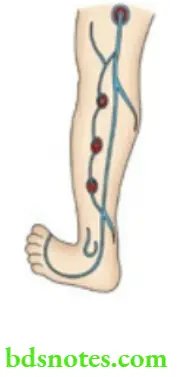
Perforators
These are the veins which connect long saphenous veins with a deep system of veins. Since they perforate deep fascia, they are called perforators. There are 5 constant perforators in the lower limb on the medial side.
- Leg perforators: They are 3 in number. The lowest perforator is situated below and behind the medial malleolus. The middle perforator is 10 cm above the tip of the medial malleolus. The upper perforator is 15 cm above the medial malleolus.
- Knee perforator: It is situated just below the knee.
- Thigh perforator: It is situated palm breadth above the knee.
The knowledge of perforators forms the basis behind multiple tourniquet tests. Most of the perforators are provided with valves. Weakness of these valves or damage to valves results in varicosity.
Deep Venous System
This comprises the femoral and the popliteal veins, or venae comitantes accompanying anterior tibial, posterior tibial and peroneal arteries and valveless veins draining the calf muscles (solely venous sinus).
Salient features of the deep venous system
- They are well-supported systems with powerful muscles and high pressure.
- They are connected to superficial veins by means of perforators.
- It is the powerful calf muscle contraction that returns the blood to the heart.
- The deep veins are also provided with valves.
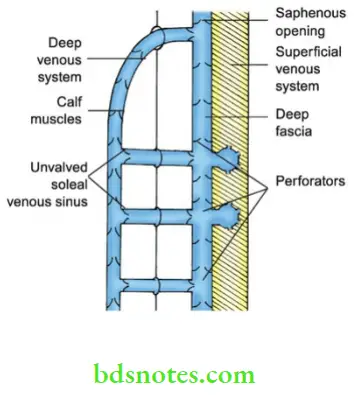
Surgical Physiology
Blood is returned to the heart from the lower limbs by the following mechanism:
- Calf muscle pump: It is the alternate contraction and relaxation of the muscles of the leg (the major factor). The pressure within the calf compartment rises to 200–300 mm Hg during walking.
- Competent valves (unidirectional) in the leg. When these valves are absent or weak, perforator incompetence develops resulting in varicose veins.
- Vis-á-tergo of the circulation, that is the pressure transmitted from the arterial tree passes the capillary bed to the venous side. This helps in the return of blood to the heart at the resting position.
- Negative intrathoracic pressure
- Venae comitantes
Distribution Of Valves
- Inferior vena cava :No valve
- Common Iliac vein :No valve
- Long saphenous vein:10–14 valves
- Short saphenous vein :1 valve
Investigations
- Doppler ultrasound is the most important, minimum-level investigation to be done before treating a patient with venous disease.
- Duplex ultrasound imaging: In this investigation, high-resolution B-mode ultrasound imaging and Doppler ultrasound are used.
- It helps in getting images of veins.
- It can also measure flow in these vessels
- All lower limb veins can be imaged
- The origin of venous ulcers and varicose veins can also be assessed.
- Importantly, it can detect a thrombus.
- Venography: Both ascending and descending venography can be done as in the case of deep vein thrombosis. Duplex ultrasonography has largely replaced this investigation (rarely done nowadays)
Doppler Ultrasound
- This investigation is carried out with the patient Standing.
- The incompetence of SFJ and saphenopopliteal junction (SFJ) can be assessed by this method.
- The gentle squeezing of calf muscles helps in detecting incompetence.
- It also helps to rule out arterial diseases.
- It can detect the patency of veins.
Treatment
Varicose veins can be treated by the following three methods:
- Conservative line of treatment
- Injection line of treatment
- Surgery.
Conservative treatment
Elastic crepe bandage and elevation of the leg form the fundamental steps in treating varicose veins. This can be advised in asymptomatic cases of varicose veins and in secondary varicose veins.
Indications
- Pregnancy
- Pelvic tumour
- When the Perthes test is positive
- AV fistula.
Injection Line Of Management (Compression Sclerotherapy)
Indications
- Below knee varicosity.
- Recurrent varicosity after surgery.
Varicose veins are marked in the standing position. The veins are punctured with a needle attached to a syringe containing sclerosant agent and the patient is asked to lie down. 3% sodium tetradecyl sulphate or 1–2 ml of ethanolamine oleate or hypertonic saline is injected into the column of the vein. Aseptic thrombosis occurs and when fibrosis occurs, the vein shrinks. A tight elastic compression bandage is applied. The success of sclerotherapy depends upon effective sclerosant, injection into an empty vein and compression with exercise.
Surgery1
1. Trendelenburg’s operation
- An inguinal incision is made, a long saphenous vein is identified and the 3 tributaries are ligated. The long saphenous vein is ligated close to the femoral vein juxta femoral flush ligation.
- An incision is given about 5 cm below the knee joint and long saphenous is isolated. The lower end is ligated and the vein is incised. A long metallic stripper is introduced within the vein and brought out from the long saphenous vein in the inguinal incision. A metallic head is connected to the stripper and the vein is avulsed. A tight crepe bandage is applied, an inguinal incision is sutured and the limb is elevated.
1Only when there are complications, surgery is advisable.
During the procedure, the perforators get avulsed from the long saphenous vein and get thrombosed. Hence, this procedure is called Ligation with stripping operation. It is indicated in cases of saphenofemoral incompetency.
2. Subfascial ligation of Cockett and Dodd
In this operation, perforators are identified deep to deep fascia and they are ligated subfascially. This is indicated in cases of perforator incompetence with saphenofemoral competence. This is also done by an endoscope.
3. Subfascial endoscopic perforator surgery (SEPS)
- Small port incisions are made in the skin of the calf region, deepened through the fascia.
- Carbon dioxide insufflation is done otherwise balloon expander is used to distend the subfascial plane.
- 2–6 perforators are identified and ligated
- The procedure is simple, quick with the least morbidity and is becoming popular.
- Indicated for below-knee perforators
Recent Techniques For The Management Of Varicose Veins
Venus closure
By using an ultrasound control, an ablation catheter is inserted into the saphenofemoral junction and slowly withdrawn.

- In this process, veins are destroyed.
- This procedure has the advantage of lesser incidence of thigh haematoma and pain.
- Complications include—deep vein thrombosis, recurrence and damage to overlying skin.
Trivex
- In this method, veins are identified by subcutaneous illumination, followed by injection of large quantities of fluid.
- Then superficial veins are sucked.
- Complications include induration, bruising and subcutaneous grooves.
Complications Of Varicose Veins
- Eczema and dermatitis: It occurs due to extravasation and breakdown of RBCs in the lower leg. It gives rise to itching which precipitates varicose ulcers. It is treated by application of zinc oxide cream or silver sulfadiazine cream (stasis dermatitis).
- Lipodermatosclerosis refers to various skin changes in the lower leg associated with varicose veins such as thickening of subcutaneous tissue, indurated feel like wood, pigmentation, etc. It is due to increased venous pressure resulting in capillary leakage with extravasation of blood and fibrin into surrounding tissues. Blood is broken down and the game is released. This combines with iron giving rise to haemosiderin which is responsible for pigmentation. Classically this affects the gaiter area of the leg just above the malleoli.
- Haemorrhage: It occurs due to trauma or eczema. It can be controlled by elevation of the leg and crepe bandage.
- Thrombophlebitis: It refers to inflammation of a superficial vein. The vein is tender, hard and cord-like. The skin is inflamed and pyrexia is usually present. It is treated by bed rest, elevation, crepe bandage, antibiotics and anti-inflammatory drugs.
- Venous ulcer: It is also called gravitational ulcer. Precipitating factors are venous stasis and tissue anoxia. Deep vein thrombosis is also an important cause of venous ulcers where in valves are either destroyed or incompetent due to damage. Sustained venous pressure results in extravasation of cells, and activation of capillary endothelium resulting in the release of free radicals. These free radicals cause tissue destruction and ulceration —Lipodermatosclerosis and tissue anoxia are the other factors. The following hypothesis may explain the genesis of varicose ulcers.

Thrombophlebitis—Causes
- Spontaneous—TAO, malignancy
- Trauma
- Blood transfusion
- 4 fluids, chemotherapeutic drugs
- Varicose veins
Fibrin cuff hypothesis
The combination of capillary proliferation and inflammation in the form of the presence of macrophages is a major factor in the development of venous ulcers. As a result of chronic inflammation, the perivascular cuff develops around the capillaries. This perivascular cuff is made up of many connective tissue proteins including fibrin, collagen IV and fibronectin. Slowly venous ulcer results.
White cell trapping hypothesis
Venous hypertension causes the trapping of leucocytes. These leucocytes become activated and release proteolytic enzymes thus causing damage to capillary endothelium.



Features of venous ulcer
- Typically, ulcers are situated just above the medial malleolus
- The ulcers are oval, small, painless, and superficial with pigmentation all around.
- Dilated veins above the ulcer give the clue to the diagnosis.
Treatment of varicose ulcer: Bisgaard’s method
- Rest with the elevated limb.
- Elastic crepe bandage helps in venous return
- Active exercises should be taught to the patients (to contract calf muscles).
Passive exercises
- Correct way of walking with the heel down first
- If the ulcer is infected, antibiotics are given and dressing of the ulcer is done. Once the ulcer heals, Trendelenburg’s operation is done.

6. Calcification can be seen in the walls of the vein
7. Periostitis of the tibia can occur due to the ulcer situated on the medial surface of the leg. Due to the involvement of the periosteum, the ulcer gives rise to severe pain.
8. Equinovarus deformity results in the improper habit of walking on the toes which results in the shortening of the tendon Achilles.
9. Marjolin’s ulcer is a squamous cell carcinoma arising from a healed varicose ulcer with scarring.
Short Saphenous Varicosity
They are uncommon causes of varicosity in the leg. The short saphenous vein originates from the lateral part of the dorsal venous arch and ends in the popliteal vein in the popliteal fossa. The incompetence of the saphenopopliteal valve results in short saphenous varicosity. It produces prominent veins on the lateral aspect of the leg with or without ulceration. They are treated by ligation of the short saphenous vein in the popliteal fossa.
Ligation Of Saphenopopliteal Junction
- Preoperative ultrasonographic marking is essential.
- The vein should be ligated deep to deep fascia.
- Branches —Giacomini vein and gastrocnemius veins may be seen—to be ligated.
- It can be stripped up to mid-calf so as to avoid injury to the sural nerve.
- It is important to close the deep fascia to avoid unsightly cosmetic bulge behind the knee.
Deep Vein Thrombosis (Dvt)
It is also called phlebothrombosis. It is an acute thrombosis of deep veins. Deep vein thrombosis is very common in Western countries, the exact cause of which is not known. Post-operative immobilisation, pressure on the calf muscles, sluggish blood flow and prolonged bed rest are the various factors which precipitate deep vein thrombosis. Commonly, it affects venous sinuses in the sole muscles. It is a common starting place. It can also involve pelvic veins. Various factors responsible for deep vein thrombosis can be remembered as THROMBOSIS.
Clinical Features
- The maximum incidence occurs on 2nd day and 5th–6th days in the postoperative period.
- The first complaint is usually oedema, erythema, or dilated veins of the leg.
Thrombosis—Virchow’s Triad
- Endothelial injury
- Stasis
- Increased coagulability
Causes Of Deep Vein ThrombosiS1
- Trauma—Injury to the vessel wall
- Hormones—Increased coagulability
- Road traffic accidents
- Operations—Cholecystectomy, prolonged surgery
- Malignancy—Sluggish blood flow
- Blood disorders—Polycythemia
- Orthopaedic surgery, obesity, old age
- Serious illness—Stroke, M.I.
- Immobilisation
- Splenectomy
1You can remember Thrombosis
- Dull aching or nagging pain in the calf muscles is present.
- Superficial blebs in the skin.
- Low-grade fever with increased pulse rate is characteristic.
- Phlegmasia alba dolens refers to the white leg. It occurs when the thrombus extends from the calf region to the iliofemoral vein.
- Phlegmasia coerulea dolens refers to a blue leg with loss of superficial tissues of the toes.
Signs (acute DVT)
- Homan’s test: Forcible dorsiflexion of the foot results in severe pain in the calf region.
- Moses test (Ideally should not be done for fear of embolism): Tenderness over calf muscle on squeezing the muscle from side to side.
Investigations
1. Doppler study: It is ideal for femoral vein thrombosis or when a thrombus extends into the popliteal vein. The normal femoral vein gives a wind storm sound which completely disappears at the end of inspiration. No sound is heard if there is femoral thrombosis

2. Contrast venography is done by injecting radio-opaque dye into the dorsal venous arch with an inflatable cuff both above the ankle and above the knee. The clot appears as a filling defect. However, venography is not routinely done because it is expensive and invasive.
Treatment
- Bed rest and elevation of limbs
- Injection heparin 10,000 units IV bolus with continuous infusion of 30,000 to 45,000 units per day. During heparin therapy activated partial thromboplastin time should be double the normal value. International Normalized Ratio (INR) should be between 2.0 and 3.0. Heparin is given for a period of 7–10 days.
-
- Warfarin, as oral anticoagulant is started 2–3 days before heparin is withdrawn because of the slow onset time of warfarin. Treatment with warfarin should continue for 6–12 months. A repeat duplex scan should be done to see for recanalisation of the veins. The dose of warfarin is 10 mg twice a day.
3. Inferior vena cava filters: They can be inserted percutaneously via the femoral vein in patients where in lytic therapy is contraindicated.
4. Surgery is not done regularly. However, in chronic cases, venous bypass has been attempted with moderate success.
- Palma operation is done in iliofemoral thrombosis wherein the common femoral vein below the block is anastomosed to the opposite femoral vein through an opposite long saphenous vein.
- May-Husni operation wherein popliteal vein is connected to long saphenous vein above.

Complications
- Permanent oedema of the limb. The limb has an inverted beer bottle appearance.
- Pulmonary embolism because the thrombus is not attached to the vessel wall.
- Secondary varicosity and nonhealing ulcer—postphlebitic limb.
Prophylaxis Of Dvt
- Decrease obesity and exercise before surgery
- Low dose heparin of 5,000 units subcutaneously, 2 hours before surgery and 24 hours after surgery, and then every 12 hours for 5 days is given, during major surgeries like cholecystectomy, abdominoperineal resection, etc.
- Intermittent pneumatic compression of the calf throughout the operation maintains the blood flow in the lower limbs. Inflation pressure is around 30–50 mmHg.
- Dextran 70 inhibits sludging of red blood cells and platelet aggregation.
- Aspirin along with dipyridamole has been used (antiplatelet agents).
- Early mobilisation, walking, adequate hydration
- Low molecular weight heparin decreases the chances of bleeding.
Please note: In some universities, varicose veins can be kept in the clinical examination, hence it has been discussed in detail in this book.
Prophylaxis Risk Groups
- Low risk: Young patients Minor illness Operation < 30 minutes
- Moderate risk : > 40 years Debilitating illness Major surgery
- High risk : > 50 years, medical conditions MI, stroke, major surgery, malignancy, obesity
Clinical Examination Of A Case Of Varicosity Of The Leg Patient Data
- Name and age: Varicose veins are common in middle age group patients.
- Sex: Women (10 times more common) are affected more than men.
- Occupation: Hotel workers, traffic police, and agriculturists who stand for a long time are vulnerable.
- Body build: Tall individuals are more susceptible.
Presenting Complaints
- When did you notice these veins? The majority of the patients present with dilated veins in the leg of a few years duration. They are minimal to start with and at the end of the day, they are sufficiently large because of the venous engorgement. Enquire in females–Did you see these veins during or after delivery? Most of the time you will get the answer yes.
- Do you have any pain? Generally, pain is not a serious complaint in the vast majority of cases. Some may complain of dragging pain in the leg or dull ache. It is due to heaviness. Night cramps occur due to changes in the diameter of veins. Aching pain is relieved at night with rest or elevation of limbs.
- Did you have sudden pain and swelling of the limb? If present it suggests deep vein thrombosis.
- Sudden pain in the calf region with fever and oedema of the ankle region suggests deep vein thrombosis (DVT). Often pain in DVT has been described as a bursting type of pain. Some patients with DVT may be asymptomatic.
- The vast majority of patients in our country present with ulceration, eczema, dermatitis and bleeding. Hence enquire about bleeding, pruritus/itching.
Pearls Of Wisdom
- Interestingly, pain due to varicose veins is on standing for a long time, relieved on exercise in contrast to pain due to arterial diseases, which get worse on exercise.
- Pain in the legs can be due to arthritis, ischaemia or due to sciatica and patient, may attribute the pain to their varicose veins. It is important to keep in mind these possibilities.
Past History
- Any surgical procedures in the past for varicosity—not uncommon.
- Any trauma to the leg such as road traffic accidents and later development of DVT.
Personal History
- In men, a history of smoking should be asked for. Smokers have an increased incidence of varicose veins.
- In women, obstetric history in the form of the number of pregnancies, usage of contraceptive pills, when did she notice the veins–is it during pregnancy or after the first child birth? (They are safe today.)





Family History
Family history can be present in a few patients. They have an early onset of varicose veins. Congenital absence of valves or weakness of the wall of the vein is responsible in such cases.
Signs
Inspection (should be done in a standing position)
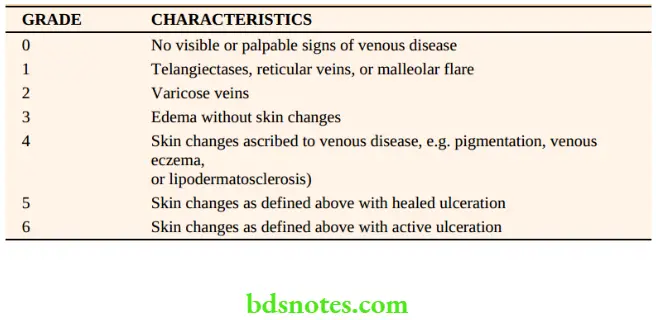
- Dilated veins are present in the medial aspect of the leg and the knee. Sometimes they are visible in the thigh also (refer to next page for clinical classification).
- A single dilated varix at the SF junction is called saphena varix. It is due to saccular dilatation of the upper end of the long saphenous vein at the saphenous opening.
- Veins are tortuous and dilated.
- A localised, dilated segment of the vein, if present, is an indication of a BLOWOUT. It signifies the underlying perforator.
- Ankle flare is a group of veins nearer the medial malleolus.
- Complications such as ulceration, bleeding, eczema, and dermatitis may be present
- A healed scar indicates previous ulceration.
Palpation
1. Cough impulse test (Morrissey’s test): This test should be done in the standing position. The examiner keeps the finger at the SF junction and the patient is asked to cough. Fluid thrill, an impulse felt by the fingers is indicative of “saphenofemoral incompetence”.
2. Trendelenburg test: This test is done in 2 parts.
Method: The patient is asked to lie on the couch in the supine position. The leg is elevated above the level of the heart and the vein emptied. SF junction is occluded with the help of the thumb (or a tourniquet) and the patient is asked to stand. In Trendelenburg, I, release the thumb or tourniquet immediately. A rapid gush of blood from above downwards indicates saphenofemoral incompetence.


- Trendelenburg 2: The pressure at the SF junction is maintained without releasing the thumb or tourniquet. The patient is then asked to stand. Slow filling of the long saphenous is seen. It is due to perforator incompetence (retrograde flow of blood).
3. Multiple tourniquet test is done to find out the exact site of perforators.
- Method: The patient is asked to lie supine on the couch. The vein is emptied by elevation. As the name suggests, 3–5 tourniquets (multiple) can be applied. However, if more tourniquets are applied the exact localisation of the perforators can be made out. It is not practical. There are mainly ankle, knee and thigh perforators. Hence, four tourniquets can be applied at various levels as mentioned below.
- 1st Tourniquet: At the level of saphenofemoral junction (SF junction).
- 2nd Tourniquet: At the level of the middle of the thigh, to occlude perforator in the Hunter’s canal.
- 3rd Tourniquet: Just below the knee.
- 4th Tourniquet: Palm breadth (lower third of the leg) above medial malleolus/ ankle.
The patient is asked to stand and observe his lower limbs for the appearance of veins.
Inference: The appearance of veins between the first and second tourniquets indicates incompetence of thigh perforators, between the second and third indicates incompetence of knee perforators and below the fourth tourniquet indicates incompetence of ankle perforators. Usually, below-knee and ankle perforators will be incompetent.

On releasing the tourniquets one by one from below upwards, sudden retrograde filling of the veins occurs.
4. Modified Perthes1 test is done to rule out deep vein thrombosis. The patient is asked to stand the tourniquet is applied at the SF junction and he is asked to walk briskly.
Inference: If the patient complains of severe pain in the calf region or if superficial veins become more prominent, it is an indication of deep vein thrombosis and it is a contraindication for surgery.
Please note: Vein is not emptied in this test
5. Schwartz test: It is done with the patient in a standing position. Place the fingers of the left hand over a dilated segment of the vein and with the right index finger tap the vein below. A palpable impulse suggests a superficial column of blood in the vein and it also suggests incompetence of the valves in between the segment of the vein.
6. Fegan’s method (test): It is done to detect the site of perforators. The patient is asked to stand. Varicosity is marked with methylene blue and he is asked to lie down. The leg is elevated to empty the vein and the vein is palpated throughout its course. The defects in the deep fascia have a circular, button-hole consistency.

Tests For Varicose Veins
- Cough impulse test—SF incompetence
- Trendelenburg 1—SF incompetence Trendelenburg 2—Perforator incompetence
- Multiple tourniquet test—Site of perforator incompetence
- Schwartz test—Superficial column of blood
- Modified Perthes test—Deep vein thrombosis
- Fegan’s test—To locate the perforators in the deep fascia
Examination of varicose ulcer: In the form of inspection and palpation should be done.
Evidence of deep vein thrombosis: Homan’s test and Moses’s test.
Examination of the abdomen: To rule out pelvic tumours and inferior vena cava obstruction evidenced by dilated veins in the lateral abdominal wall.

Leave a Reply