Describe the Thyroid Gland under the following headings:
- Gross anatomy,
- Parts and relations,
- Blood supply,
- Development and
- Applied anatomy.
Answer.
Thyroid Gland Gross anatomy
- It is a large endocrine gland situated on the front (and side) of the lower part of the neck.
- It consists of right and left lobes, joined by an isthmus. Sometimes, a third small pyramidal lobe may project upwards from the isthmus.
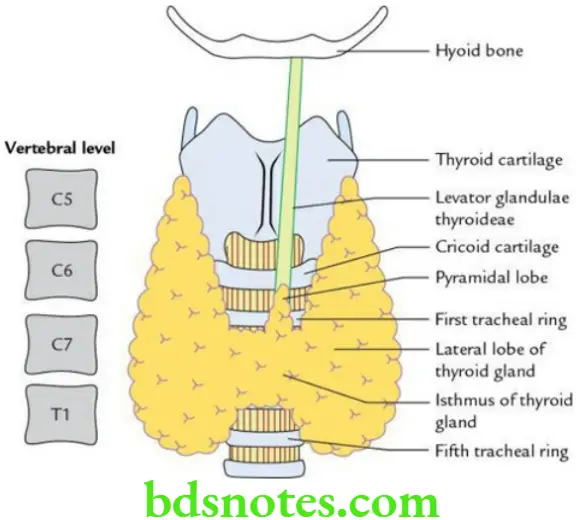
Thyroid Gland Situation and extent
- The thyroid gland is situated in front of the C5 to C7 and T1 vertebrae.
- Each lobe extends from the oblique line of the thyroid cartilage to the 4th or 5th tracheal ring.
- The isthmus extends from the 2nd to the 4th tracheal ring.
Thyroid Gland Weight: 25 g (larger in females)
Thyroid Gland Dimensions
- Each lobe measures 5 × 2.5 × 2.5 cm
- Isthmus measures 1.25 × 1.25 cm
Thyroid Gland Capsules/coverings
The thyroid gland is enclosed into two capsules: true and false.
- True capsule: It is formed by the condensation of the connective tissue of the gland itself at its periphery.
- False capsule: It is formed by the pre-tracheal layer of the deep cervical fascia. It is thin along the posterior border but thick on the medial surface of the gland, where it thickens to form a suspensory ligament of Berry connecting the gland to the cricoid cartilage.
Thyroid Gland Parts and Relations
Thyroid Gland Thyroid lobe
Each lobe is conical in shape and presents the following features:
- Apex
- Base
- Three surfaces: lateral, medial and posterolateral
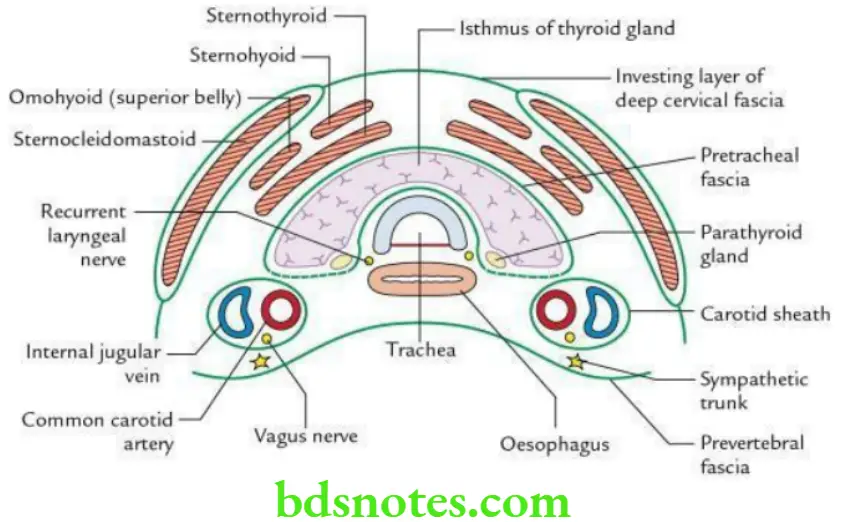
- The lateral/superficial surface is covered from deep to superficial by:
- Sternothyroid
- Sternohyoid, and superior belly of omohyoid
- Anterior border of sternocleidomastoid
- The medial surface is related to:
- Two tubes: Trachea and oesophagus
- Two muscles: Inferior constrictor and cricothyroid
- Two nerves: External laryngeal and internal laryngeal
- The posterolateral/posterior surface is related to the carotid sheath.
- The lateral/superficial surface is covered from deep to superficial by:
- Two borders: Anterior and posterior
- The anterior border is related to the anterior branch of the superior thyroid artery.
- The posterior border is related to:
- Longitudinal anastomosis between superior and inferior thyroid arteries
- Superior and inferior parathyroid glands
- Inferior thyroid artery
- Thoracic duct (on left side only)
Read And Learn More: Selective Anatomy Notes And Question And Answers
Thyroid Gland Isthmus The isthmus presents:
- Two surfaces: Anterior and posterior
- Anterior surface is related to:
- Right and left sternothyroid and sternohyoid muscles
- Anterior jugular veins
- The posterior surface is related to the 2nd, 3rd and 4th tracheal rings.
- Anterior surface is related to:
- Two borders: Superior and inferior
- The upper border is related to anastomosis between the anterior branches of the right and left superior thyroid arteries.
- The inferior border is related to the inferior thyroid veins.
Thyroid Gland Blood supply
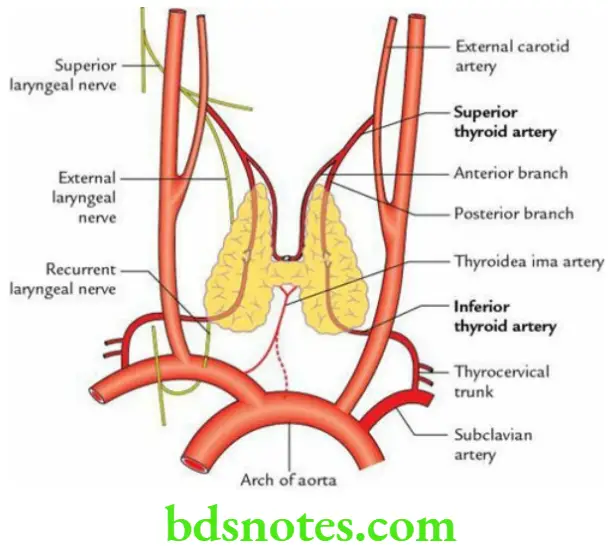
Thyroid Gland Arterial supply
- The superior thyroid artery is a branch of the external carotid artery. It supplies the upper two-thirds of the thyroid lobe and the upper half of the isthmus. The superior thyroid artery is accompanied by an external laryngeal nerve which leaves it near the upper pole of the gland.
- The inferior thyroid artery is a branch of the thyrocervical trunk. It supplies the lower one-third of the thyroid lobe and the lower half of the isthmus. The inferior thyroid artery is closely related to the recurrent laryngeal nerve near the lower pole of the thyroid gland.
- Arteria thyroid ima (if present) is a branch of the brachiocephalic trunk or arch of the aorta. It supplies the isthmus.
- Small accessory arteries are derived from the oesophageal and tracheal arteries.
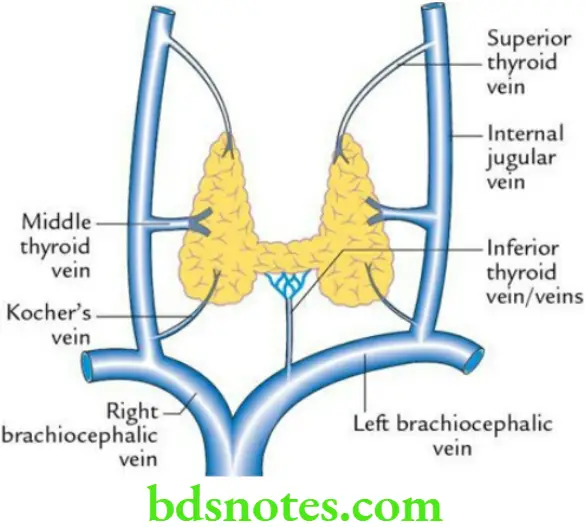
Thyroid Gland Venous drainage
- Superior thyroid vein: It emerges from the upper pole and drains into the internal jugular vein.
- Middle thyroid vein (a short wide venous trunk): It emerges from the middle of the thyroid lobe and drains into the internal jugular vein.
- Inferior thyroid vein: It emerges from the lower border of the isthmus and drains into the left brachiocephalic vein.
- A fourth vein (of Kocher), if present, emerges between the middle and inferior thyroid veins and drains into the internal jugular vein.
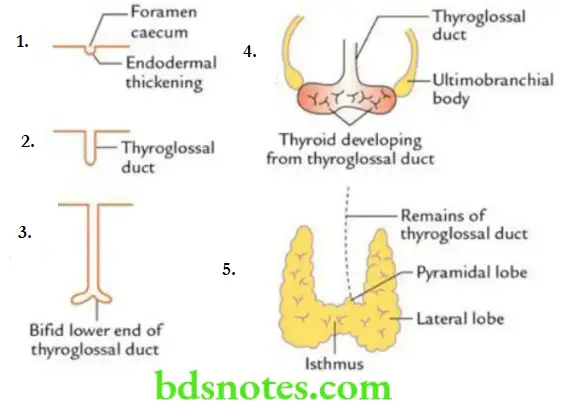
Thyroid Gland Development
- The thyroid gland develops from a median endodermal diverticulum – the thyroglossal duct, which grows downwards in front of the neck from the floor of the primitive pharynx.
- The distal end of the thyroglossal duct bifurcates and then differentiates to form the thyroid gland. The remaining part of the duct is obliterated.
Thyroid Gland Applied Anatomy
- Enlargement of the thyroid gland is called goitre.
- During thyroidectomy (removal of the thyroid gland), the superior thyroid artery should be ligated as near to the superior pole of the gland as possible, while the inferior thyroid artery should be ligated as away from the gland as possible to avoid injuries to external laryngeal and recurrent laryngeal nerves, respectively.
- Swellings arising from the thyroid gland move up and down during swallowing because the thyroid capsule is attached to the laryngeal skeleton.
- Partial thyroidectomy is preferred to total thyroidectomy to avoid postoperative hypothyroidism due to inadvertent removal of parathyroid glands.
- Compression of structures by large goitre leads to characteristic symptoms of:
- Dyspnoea, due to compression of the trachea.
- Dysphagia, due to compression of the oesophagus.
- Dysphonia, due to compression of recurrent laryngeal nerves.
Thyroid Gland Mnemonic: 3D
- Thyroglossal cyst
- It results from the persistence of a portion of the thyroglossal duct.
- It is a commonest congenital anomaly of the thyroid gland.
- It is usually located below the hyoid bone (subhyoid).
Histological Features of the Thyroid Gland
Microscopically, the thyroid gland consists of parenchyma and stroma.
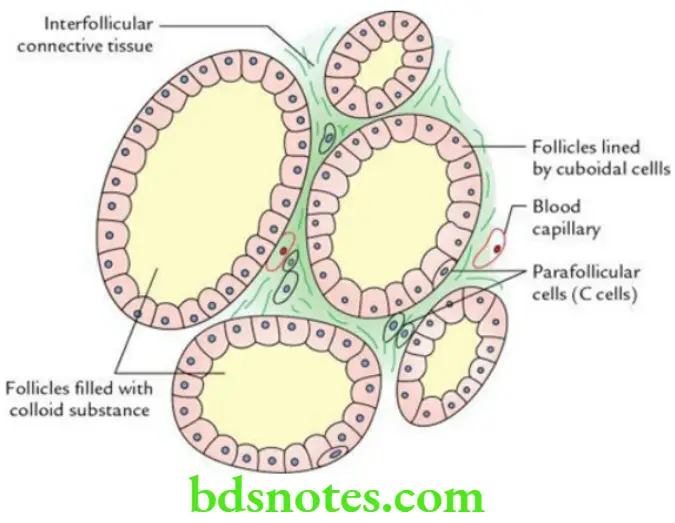
Histological features of the Thyroid Gland Parenchyma
- Presence of spheroidal thyroid follicles (about 0.9 mm in diameter).
- Thyroid follicles are lined by simple cuboidal epithelium and filled with eosinophilic colloid material (thyroglobulin).
- Simple cuboidal epithelium lining the thyroid follicles is made up of follicular cells.
- Presence of parafollicular cells (C cells) in between the thyroid follicles in the connective tissue or sometimes within the follicles close to the basement membrane.
Histological features of the Thyroid Gland Stroma
- It forms the connective tissue framework of the gland.
- Stroma includes the capsule and sparse intralobular connective tissue rich in capillaries.
Parathyroid Glands in Brief
Parathyroid Glands General Features
- These are two pairs (superior and inferior) of small endocrine glands.
- The superior and inferior parathyroid glands are located on the posterior border of each thyroid lobe within the capsule of the thyroid gland.
Each parathyroid gland is a small, yellowish-brown, oval or lentiform body measuring 6 × 4 × 2 and weighing about 50 mg (about the size of a split pea).
The superior and inferior parathyroid glands lie on the posterior aspect of the thyroid lobe along the anastomotic artery between the superior and inferior thyroid arteries, which is used as a guide to locate them during surgery.
Parathyroid Glands Position/location
Parathyroid Glands Superior parathyroid It is more constant in position and usually lies at the middle of the posterior border of the lateral lobe of the thyroid gland at the level of the cricoid cartilage. It usually lies between the true and false capsules of the thyroid gland and dorsal to the recurrent laryngeal nerve.
Parathyroid Glands Inferior parathyroid It is more variable in position. It may lie:
- Within the thyroid capsule below the loop of the inferior thyroid artery, near the lower pole of the thyroid gland.
- Outside the thyroid capsule, immediately above the loop of the inferior thyroid artery.
- Within the substance of the thyroid gland near its posterior border.
Parathyroid Glands Function The parathyroid glands secrete a hormone called parathormone, which plays an important role in calcium metabolism.
Parathyroid Glands Development
- Superior parathyroid develops from the 4th pharyngeal pouch; hence, it is also called parathyroid 4.
- Inferior parathyroid develops from 3rd pharyngeal pouch; hence, it is also called parathyroid 3.
Parathyroid Glands Applied anatomy
- Hypoparathyroidism: It may occur due to inadvertent removal of the parathyroid glands during thyroidectomy. It leads to tetany due to low blood calcium levels. Clinically, it presents as a carpopedal spasm.
- Hyperparathyroidism: It occurs due to tumours of the parathyroid glands. It leads to the decalcification of bones and the formation of renal stones due to high blood calcium levels.

Leave a Reply