The Normal Periodontium
Question 1. Write notes on attached gingiva.
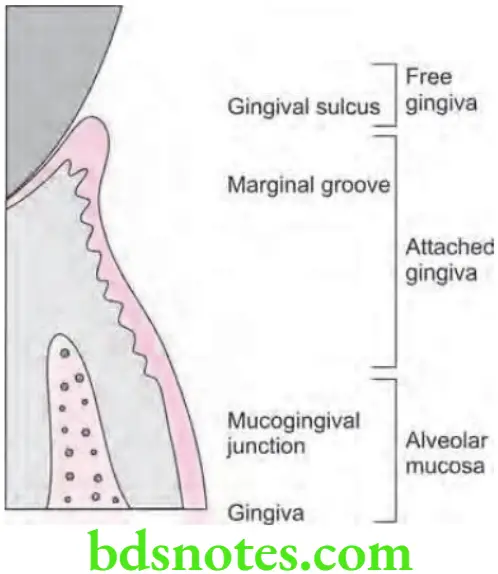
Answer. Attached gingiva is the distance between mucogingival junction and projection on the external surface of the bottom of gingival sulcus or periodontal pocket. attached gingiva is continuous with marginal gingiva.
- Attached gingiva is the part of the gingiva which is tightly attached to the underlying periosteum of alveolar bone and cementum by connective tissue fibers.
- Attached gingiva is firm, resilient and hence immovable portion of the gingiva.
- It is thus, firmly entrenched between two movable structures: the marginal gingiva coronally and the alveolar mucosa apically.
- Attached gingiva is different from keratinized gingiva and should not be confused with it.
- Width of the attached gingiva is measured as the distance between mucogingival junction and the projection on the external surface of the bottom of gingival sulcus/periodontal pocket. The dimensions of the attached gingiva vary from the anterior to the posterior teeth.
- Width of the attached gingiva is generally wider in the maxilla than in the mandible. The narrowest zone of the gingiva is found in the region of the maxillary and mandibular 1st premolars and usually in connection with frenum and muscle attachments. The pattern of variation is approximately the same in deciduous and permanent teeth.
- Width of the attached gingiva is wider in the supraerupted teeth. It also increases with age. This increase in dimension occurs as a result of an increase in the height of the alveolar process, which in turn, is the result of passive eruption.
- Width of attached gingiva is greater in incisor region that is 3.5 to 4.5 mm in maxilla and 3.3 to 3.9 mm in mandible and is less in posterior segments that is there is least width in premolar region which is 1.9 mm in maxilla and 1.8 mm in mandible.
Read And Learn More: Periodontics Question And Answers
Significance of Attached Gingiva
- It gives support to the marginal gingiva.
- It provides attachment or a solid base for the movable alveolar mucosa for the action of lips, cheeks and tongue.
- It can withstand frictional and functional stresses of mastication and toothbrushing. When the marginal tissue is the alveolar mucosa, it does not resist the functional stresses of toothbrush trauma imposed on it. Frequently, the result is apical shiftng of the marginal tissue and additional recession. attached gingiva is tightly attached to underlying periosteum and the alveolar bone with the densely organized connective tissue.
- It acts as a barrier for passage of inflmmation. In the presence of microbial flra, tooth having alveolar mucosa at its margin shows more clinical signs of inflmmation than corresponding tooth that has a suffient band of the attached gingiva. Such marginal tissue appears to be more susceptible to the products of inflmmation that may result in pocket formation or apical migration of both attachment apparatus and marginal tissues.
- It provides resistance to tensional stresses. Attached gingiva serves as a buffer between the mobile free gingival margin and mobile alveolar mucosa. There are skeletal muscle fibers within the alveolar mucosa that exert a force in an apical direction on the attached gingiva. This force is dissipated by bound down keratinized tissue.
Measurement of Attached Gingiva
There are four different methods used to measure width of attached gingiva.
- Measurement approach: In this method pocket depth or the sulcus depth is measured then the total width of gingiva is measured i.e. from gingival margin to mucogingival line. Thus by subtracting these two measurements width of attached gingiva is achieved. Total gingival width – Pocket depth = Width of attached gingiva.
- By using Schiller’s potassium iodide solution: after application of this solution total width of gingiva is measured i.e. from gingival margin to mucogingival line and later the sulcus depth or pocket depth is measured. Then by subtracting the total gingival width from pocket depth, we get the width of attached gingiva. Stained total gingival width – pocket depth = width of attached gingiva.
- Tension test: This is done by stretching the lip or cheek to demarcate the mucogingival line and to see for any movement of the free gingival margin. And if the free gingival margin moves during stretching of lips then the attached gingiva is considered to be inadequate.
- Roll test: It is done by pushing the adjacent mucosa coronally with a dull instrument. If the gingiva moves with the instrument then the width of attached gingiva is considered inadequate. In adequate width, the gingiva does not move because the attached gingiva is filmly attached to the underlying bone.
Question 2. Define periodontal ligament, its structure and function in detail.
Or
Explain functions of periodontal ligament.
Or
Write short note on physical function of periodontal ligament.
Or
Write short note on function of periodontal ligament
Or
Describe functions o periodontal ligament.
Or
Define periodontal ligament. Enumerate the functions of it and describe physical functions in detail.
Or
Define periodontal ligament. Enumerate the principle fibers of periodontal ligament and describe any one in detail.
Or
Describe principle fibers of PDL. Write functions of periodontal ligament.
Or
Define periodontal ligament. Enumerate the principle fibers of periodontal ligament and describe any one function of periodontal ligament in detail.
Or
Write short note on principle fibers of periodontal ligament.
Answer. The periodontal ligament is composed of a complex vascular and highly cellular connective tissue that surrounds the tooth root and connects it to the inner wall of the alveolar bone.
The periodontal ligament is the soft richly vascular and cellular connective tissue which surrounds the root of the teeth and joins the root cementum with the lamina dura or the alveolar bone proper or the socket wall.
Structure of Periodontal Ligament
- Periodontal ligament is continuous with the connective tissue of the gingiva, and it communicates with the marrow spaces via vascular channels present inside the bone.
- Average width of periodontal ligament space is 0.2 mm, considerable variation exists.
- Periodontal space is diminished around teeth which are not in function and in unerupted teeth, but it get increased in teeth which have been subjected to hyperfunction.
- Periodontal ligament consists of the following:
- Periodontal fibers
- Principal fibers
- Secondary fibers
- Cellular elements
- Ground substance
- Periodontal fibers
Periodontal Fibers
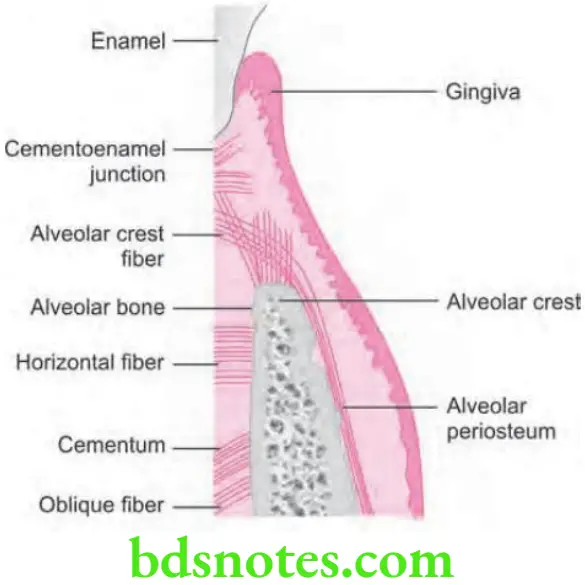
Principal Fibers of Periodontal Ligament
- Most important elements of the periodontal ligament are principal fibers, which are collagenous and arranged in bundles and follow a wavy course when viewed in longitudinal section.
- Terminal portions of the principal fibers which are inserted into cementum and bone are known as Sharpey fibers.
- Principal fiber bundles consist of individual fibers which form a continuous anastomosing network between tooth and bone.
- The principal fibers of the periodontal ligament are arranged in six groups that develop sequentially in the developing root i.e.
- Transseptal group
- Alveolar crest group
- Horizontal group
- Oblique group
- Apical group
- Interradicular group
Transseptal group
- Transseptal fibers extend interproximally over the alveolar bone crest and get embedded in the cementum of adjacent teeth.
- These fibers are reconstructed even after destruction of the alveolar bone which results from periodontal disease.
- Transseptal fibers may be considered as belonging to the gingiva, because they do not have osseous attachment.
- These fibers lead to the maintenance of the teeth in the arch.
Alveolar crest group
- They extend obliquely from cementum just beneath the junctional epithelium to the alveolar crest.
- These fibers also run from the cementum over the alveolar crest and to firous layer of the periosteum which covers the alveolar bone.
- Alveolar crest fibers prevent extrusion of tooth and resist lateral tooth movements.
- Incision of these fibers at the time of periodontal surgery does not increase tooth mobility unless significant attachment loss has occurred.
- These fibers secure teeth inside the socket by resisting the lateral forces which are applied to the tooth.
Horizontal group
- These fibers extend at right angles to the long axis of tooth from cementum to the alveolar bone.
- These fibers mainly prevent the lateral tooth movement.
Oblique group
- Oblique fibers constitute the largest group in periodontal ligament and they extend from the cementum in a coronal direction obliquely to the bone.
- They absorb the chewing forces over the tooth and are the main support of the tooth.
- They resist the apically directed masticatory forces.
Apical group
- Apical fibers radiate in irregular manner from the cementum to the bone at the apical region of the socket.
- They do not occur on incompletely formed roots.
- They prevent the tooth tipping and resist the forces of luxation.
Interradicular group
- These fibers fan out from the cementum to the tooth in the furcation areas of multirooted teeth.
- They prevent tipping of tooth, forces of luxation and rotation.
Secondary Fibers of Periodontal Ligament
- Periodontal ligament has two immature forms are found: oxytalan and elaunin.
- The so-called oxytalan fibers run parallel to the root surface in a vertical direction and bend to attach cementum in cervical third of root. They are thought to regulate vascular low.
- Oxytalan fibers have been shown to develop de novo in the regenerated periodontal ligament.
- In addition to these fiber types, small collagen fibers associated with the larger principal collagen fibers have been described. Such fibers run in all directions and form a plexus called the indifferent fiber plexus.
Cellular Elements of the Periodontal Ligament
Four types of cells have been identified in the periodontal ligament:
- Connective tissue cells
- Epithelial rest cells
- Immune system cells
- Cells associated with neurovascular elements.
Connective Tissue Cells
- Connective tissue cells consist of firoblasts, cementoblasts and osteoblasts.
- Fibroblasts are most common cells in periodontal ligament and they appear as ovoid or elongated cells which are oriented along the principal fibers and exhibit pseudopodia-like processes.
- Fibroblasts synthesize collagen and have the capacity to phagocytose “old” collagen fibers and degrade them be the enzyme hydrolysis. So collagen turnover appears to be regulated by firoblasts.
- Osteoblasts, cementoblasts, osteoclasts, and odontoclasts are also seen in the cemental and osseous surfaces of the periodontal ligament.
Epithelial Rests of Malassez
- These cells form a latticework in periodontal ligament and appear as either isolated clusters of cells or interlacing strands which depends on the plane in which the microscopic section is cut.
- Epithelial rests are considered to be the remnants of the Hertwig root sheath, which disintegrates during root development.
- Epithelial rests are distributed close to the cementum throughout the periodontal ligament of most teeth; they are most numerous in the apical area and cervical area.
- These cells diminish in number with age by degenerating and disappearing or by undergoing calcifiation to become cementicles.
- The cells are surrounded by a distinct basal lamina, they are interconnected by hemidesmosomes and they contain tonofiaments.
- Although the functional properties of these cells are still considered to be unclear but they are reported to contain keratinocyte growth factors, and they have been shown to be positive for tyrosine kinase A neurotrophin receptor. In addition, epithelial rests proliferate when stimulated and they participate in the formation of periapical cysts and lateral root cysts.
Defense Cells
- They are neutrophils, lymphocytes, macrophages, mast cells, and eosinophils.
- These cells and the cells which are associated with neurovascular elements, are similar to the cells which are found in other connective tissues.
Ground Substance
- Periodontal ligament consists of a large proportion of ground substance that fills the spaces between fibers and cells.
- Ground substance consists of two main components i.e.
- Glycosaminoglycans, which are hyaluronic acid and proteoglycans
- Glycoproteins which are fironectin and laminin.
- Ground substance consists of high water content i.e.70%.
- Cell surface proteoglycans participate in several biologic functions, including cell adhesion, cell–cell and cell–matrix interactions, binding to various growth factors as coreceptors, and cell repair.
Functions of Periodontal Ligament
Physical functions
- Provision of soft tissue casing: For protecting the vessels as well as nerves from injury by the mechanical forces, periodontal ligament provides the soft tissue casing around them.
- Transmission of occlusal forces to bone:
- Axial force when applied to tooth, it causes stretching of oblique fibers of periodontal ligament. Transmission of this tensional force to the alveolar bone encourages bone formation rather than bone resorption.
- But when horizontal or tipping force is applied the tooth rotates around the axis, at fist the tooth movement is within the confies of the periodontal ligament. When a greater force is applied, displacement of facial and lingual plates may occur.
- Apical portion of root moves in the in direction opposite to coronal portion. In areas of tension, principle fibers of bundle are taut rather than wavy. In areas of pressure, fibers get compressed, tooth gets displaced and corresponding distortion of bone occur in direction of root movement.
- The axis of rotation, in single-rooted teeth is located in the area between the apical and middle third of the root. Root apex and coronal half of the clinical root are suggested as other locations of axis of rotation.
- In multirooted teeth, the axis of rotation is located at the furcation area.
- Resistant to impact of occlusal forces: Two Theories have been explained for the mechanism of tooth support:
- Tensional theory: According to it, the principal fibers of periodontal ligament plays a major role in supporting the tooth and transmittng forces to the bone. When forces are applied to the tooth, principal fibers unfold and straighten and then transmit the forces to the alveolar bone, causing elastic deformation of the socket. Finally when the alveolar bone has reached its limit, the load is transmittd to basal bone.
- Viscoelastic theory is based on the fact that, the fluid movement largely controls the displacement of the tooth, with fibers playing a secondary role. When the forces are transmittd to the tooth, the extracellular fluid is pushed from the periodontal ligament into the marrow spaces through the cribriform plate. after the depletion of tissue fluids, the bundle fibers absorb the shock and tighten. This leads to blood vessel stenosis followed by arterial back pressure followed by ballooning of the vessels and replenishing with tissue fluids.
- Maintains the gingival tissues in their proper relationship to the teeth.
- Shock absorption resists the impact of occlusal forces.
Formative and Remodeling Function
- Periodontal ligament and alveolar bone cells are exposed to physical forces in response to mastication, parafunction, speech, and the orthodontic tooth movement.
- Cells of periodontal ligament participate in formation and resorption of cementum and the bone, which occur at the time of physiologic tooth movement, during the accommodation of periodontium to occlusal forces, and during the repair of injuries.
- Periodontal ligament shows variations in cellular enzyme activity which are correlated with the remodeling process. Although applied loads may induce vascular and inflammatory reactive changes in periodontal ligament cells.
- The periodontal ligament is constantly undergoing remodeling. Old cells and fibers are broken down and replaced by new ones, and mitotic activity may be observed in the firoblasts and endothelial cells.
- Fibroblasts form the collagen fibers, and the residual Mesenchymal cells develop into osteoblasts and cementoblasts. Therefore the rate of formation and the differentiation of osteoblasts, cementoblasts, and fibroblasts affect the rate of formation of collagen, cementum, and bone.
Nutritional and Sensory Functions
- Periodontal ligament supplies nutrients to the cementum, bone and gingiva via blood vessels, and it also provides lymphatic drainage. As compared to other ligaments and tendons, the periodontal ligament is highly vascularized tissue. High blood vessel content may provide hydrodynamic damping to applied forces as well as high perfusion rates to the periodontal ligament.
- Periodontal ligament is richly supplied with sensory nerve fibers which are capable of transmittng tactile, pressure, and pain sensations through trigeminal pathways. Nerve bundles pass in the periodontal ligament from the periapical area and through channels from the alveolar bone that follows the course of the blood vessels.
- The bundles divide into single myelinated fibers, which loose their myelin sheaths and end in one of four types of neural termination i.e.
- Free endings, which have a treelike confiuration and carry pain sensation
- Ruffini-like mechanoreceptors, which are located primarily in the apical area
- Coiled Meissner’s corpuscles and mechanoreceptors, which are found in mid – root region
- Spindle-like pressure and vibration endings, which are surrounded by a fibrous capsule and located mainly in apex.
Question 3. Write short note on fenestration and dehiscence.
Or
Describe fenestration and dehiscence.
Answer. Isolated areas in which root is denuded of bone and the root surface is covered only by periosteum and overlying gingiva is known as fenestration. In these, instances marginal bone is intact.
- When denuded areas extend through the marginal bone, the defect is called as dehiscence.
- Such defects occur approximately in 20% of teeth and they occur more on facial bone than on lingual, are more common on anterior teeth than on posterior teeth, and are frequently bilateral.
- Prominent root contour, malposition and labial protrusion of root combined with a thin bony plate are predisposing factors.
- Fenestration and dehiscence are important because they may complicate the outcome of periodontal surgery.
- Both fenestration and dehiscence are seen at the time of disease in relation to alveolar bone proper.
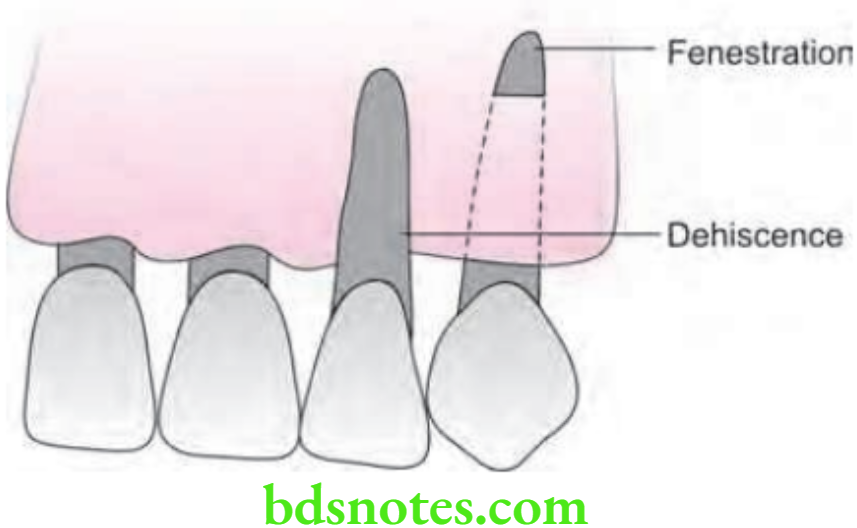
Methods to Detect
- Tactile method: Run finger over the prominent root in apicocoronal and mesiodistal directions. The crest of the bone at the apical extent of the defect may be felt, as may the lateral border. As the figer is moved coronally, the bridge of the bone may be felt at the coronal part of a fenestration but not in dehiscence.
- Bone sounding/transgingival probing: It is done by anesthetizing the tissue locally and inserting the probe horizontally and walking along the tissue tooth interface so that the operator can feel the bony topography. It may be used to differentiate between two types of defects. The sensation transmittd through the probe on touching the tooth is solid and sharp one whereas bone gives softr and mushy sensation. If the sensation is like touching tooth, the probe is moved halfway to the free margin and is pressed through the sof tissue. If the bone is touched the defect is a fenestration and if not, then it is dehiscence.
- Radiography: Cone-beam computed tomography (CBCT) images can show bone dehiscences and fenestrations.
Clinical Importance
- The defects are very important clinically because where they occur the root is covered only by the periosteum and overlying gingiva, which may atrophy under irritation and expose the root.
- Before any mucogingival surgical procedure, especially lateral pedicle existence of osseous dehiscence or fenestration should be ruled out.
- In case of gingival grafting procedure, if the receptor site has fenestration defect, soft tissue is capable of reattaching to the exposed surface with higher predictability than dehiscence.
- If the abutment tooth has dehiscence or fenestration, the partial denture will damage the abutment and abutment loss will occur in a short period.
Question 4. Write short note on gingival col.
Answer.
- Gingival col is valley like depression of interproximal contact areas which connect lingual and buccal interdental papilla.
- In the area of gingival col, gingival epithelium is nonkeratinized which is replaced by continuous cell division.
- Morphology of col differs between anterior and posterior teeth. Anteriorly col is pyramid shaped and posteriorly it is flattened.
- When gingiva is inflamed or hyperemic, col is exaggerated.
- Epithelium of col sends numerous extensions in underlying connective tissue.
- Gingival col is the site where oral hygiene accessibility is not possible. It is the area of food entrapment.
- As col consists of non-keratinized epithelium, so it is prone to inflammation and represent the frequent site for initiation of disease.
- Col confirms the shape of interproximal contact areas.
Question 5. Define gingiva and describe in detail about its microscopic and macroscopic features.
Or
Define gingiva. Write in detail about its microscopic features.
Or
Define gingiva. Discuss in detail about microscopic features of gingiva.
Or
Describe gingiva. Write its microscopic features in detail.
Answer.
Definition
Gingiva is the part of the oral mucosa that covers the alveolar process of the jaws and surrounds the neck of the teeth.
It is masticatory mucosa.
Macroscopic Features
Marginal Gingiva (Unattached Gingiva)
- It is the terminal edge or border of the gingiva surrounding the teeth in collar-like fashion.
- It is usually 1 mm wide.
- It forms the soft tissue wall of the gingival sulcus.
Gingival Sulcus
- The gingival sulcus is the shallow crevice or space around the tooth bonded by the surface of the tooth on one side and marginal gingiva and the epithelium, lining the free margin of the gingiva on other side.
- It is ‘V’ shaped.
- Under ideal conditions, the depth of the gingival sulcus is about ‘0’.
- Clinically, healthy gingiva in human, the normal gingival sulcus depth is 2 to 3 mm.
Attached Gingiva
- Attached gingiva is the part of the gingiva which is tightly attached to the underlying periosteum of alveolar bone and cementum by connective tissue fibers.
- Attached gingiva is fim, resilient and hence immovable portion of the gingiva.
- It is thus, firmly entrenched between two movable structures: the marginal gingiva coronally and the alveolar mucosa apically.
- Attached gingiva is different from keratinized gingiva and should not be confused with it.
- Width of the attached gingiva is measured as the distance between mucogingival junction and the projection on the external surface of the bottm of gingival sulcus/periodontal pocket. The dimensions of the attached gingiva vary from the anterior to the posterior teeth.
- Width of the attached gingiva is generally wider in the maxilla than in the mandible. The narrowest zone of the gingiva is found in the region of the maxillary and mandibular 1st premolars and usually in connection with frenum and muscle attachments. The pattern of variation is approximately the same in deciduous and permanent teeth.
- Width of the attached gingiva is wider in the supraerupted teeth. It also increases with age. This increase in dimension occurs as a result of an increase in the height of the alveolar process, which in turn, is the result of passive eruption.
- Width of attached gingiva is greater in incisor region that is 3.5 to 4.5 mm in maxilla and 3.3 to 3.9 mm in mandible and is less in posterior segments that is there is least width in premolar region which is 1.9 mm in maxilla and 1.8 mm in mandible.
Interdental Gingiva/Papilla
- Part of the gingiva which fils the inter-dental space between two adjacent teeth is known as inter-dental papilla.
- It appears pyramidal or triangular from the facial and lingual aspect along with its lateral borders. Tip of the pyramid is formed by continuation of marginal gingiva of adjacent teeth.
- In the posterior region, interdental gingiva has a ‘tent’ shape.
Gingival Col
- Facial as well as lingual portions of interdental papillae forms the concave or valley like area which fits below the contact area. The valley like area is known as Col.
- Col or Gingival col is lined by non-keratinized epithelium.
- It confirms the shape of interproximal contact areas.
- Because of the non-keratinized epithelium, col is prone to inflammation and lead to disease.
- In this area oral hygiene accessibility is not possible.
Microscopic Features
Gingiva consists of an area of connective tissue covered by stratified squamous epithelium.
Gingival Epithelium is divided into three types i.e. outer epithelium, sulcular epithelium and junctional epithelium.
Outer/Oral Epithelium
- Oral epithelium, also called as an outer epithelium, is a keratinized stratifid squamous type of epithelium.
- It covers the crest and outer surface of marginal gingiva and surface of attached gingiva.
- Oral epithelium consists of following types of cellular layers:
- Stratum basale: Cells of stratum basale are either cylindrical or cuboid. Basal cells are found immediately next to the connective tissue and are separated from connective tissue by a basement membrane. It is the germinative layer and hence can divide. When two daughter cells have been formed by cell division, an adjacent older basal cell is pushed into the spinous cell layer and starts as a keratinocyte to traverse the epithelium. It takes approximately 1 month for a keratinocyte to reach the outer epithelial surface, where it is shed from the stratum corneum.
- Stratum spinosum: It is a prickle cell layer in which large polyhedral cells with short cytoplasmic processes are present. The uppermost cells from this layer contain granules called as keratinosomes or Odland bodies. These are modified lysosomes, which contain a large amount of enzymes acid phosphatase that is involved in the destruction of organelle membranes.
- Stratum granulosum: Cells of this layer are flattned in plane parallel to the gingival surface. Keratohyalin granules, which are associated with keratin formation, are round in shape and appear within the cytoplasm of the cell.
- Stratum corneum: It consists of closely packed, flattened cells that have lost nuclei and the most other organelles as they become keratinized. The cells are densely packed with tonofiaments. Clear, rounded bodies probably representing lipid droplets appear within the cytoplasm of the cell.
Sulcular Epithelium
- It lines the gingival sulcus.
- It is a thin, non-keratinized stratifid squamous epithelium without rete pegs.
- It extends from coronal limit of the junctional epithelium to the crest of the gingival margin.
- It usually shows many cells with hydropic degeneration.
- It is devoid of granulosum and corneum strata.
- The sulcular epithelium has the potential to keratinize, if
- It is reflected and exposed to oral cavity.
- The bacterial flora of the sulcus is totally eliminated.
- It is extremely important because it may act as a semipermeable membrane through which infectious bacterial products pass into the gingiva and tissue fluid from the gingiva seeps into the sulcus.
Junctional Epithelium
- Junctional epithelium consists of a collar-like band of stratified squamous non-keratinized epithelium.
- It is 3-4 layer thick in early life but increases with age upto 10 to 20 layer.
- The length of junctional epithelium ranges from 0.25 to 1.35 mm.
- These cells can be grouped in two strata: the basal layer that faces the connective tissue and the suprabasal layer that extends to the tooth surface.
- The proliferative layer which leads to most of the cell divisions is located in contact with the connective tissue. Shedding surface of junctional epithelium is located at the coronal end which forms bottm of gingival sulcus.
- Junctional epithelium is formed by conflence of the oral epithelium and the reduced enamel epithelium at the time of eruption.
- Junctional epithelial cells are interconnected by few desmosomes and occasionally by gap junctions.
- Junctional epithelium, mainly at its basal cell layers is innervated by the sensory nerve fibers.
- Division of junctional epithelium is there in three zones i.e. coronal, middle and apical.
- Junctional epithelium is attached to the tooth surface by means of an internal basal lamina and to the gingival connective tissue by an external basal lamina which has the same structure as other epithelial–connective tissue attachments elsewhere in the body.
- External basal lamina consists of same structure and the composition as other basement membranes, elsewhere in the body while the internal basal lamina has different structural and molecular characteristics. This lacks the common basement membrane components i.e. collagen Type 4 and 7, most laminins forms.
- The internal basal lamina consists of a lamina densa (adjacent to the enamel) and a lamina lucida to which hemidesmosomes are attached. Hemidesmosomes have a decisive role in the fim attachment of the cells to the internal basal lamina on the tooth surface.
- Junctional epithelial cells migrate in the coronal direction to free surface where they desquamate. As the surface area occupied by basal cells is more than bottm of sulcus, exfoliation occurs at extremely high rate.
- Attachment of the junctional epithelium to the tooth is reinforced by the gingival fibers, which brace the marginal gingiva against the tooth surface. So, the junctional epithelium and gingival fibers are considered as functional unit. Dentogingival unit: Dentogingival unit = junctional epithelium + gingival fibers.
- Intercellular spaces of junctional epithelium give a pathway for fluid and transmigrating the leukocytes. In absence of clinical signs of inflammation, approximately 30,000 PMNs migrate per minute via junctional epithelium of all human teeth in the oral cavity.
Principal Cells of the Gingival Epithelium
- Keratinocytes
- Non-keratinocytes
- Langerhans cells
- Merkel cells
- Melanocytes
The main function of the gingival epithelium, is to protect the deep structure by proliferation and differentiation of the keratinocytes.
Keratinocytes
- They are the principal cells of gingival epithelium.
- Keratinocytes form the keratinized layer outer epithelium by proliferation and differentiation.
- Proliferation of keratinocytes take place by mitosis in basal layer these proliferated cells begin to migrate to the surface.
- Differentiation involves the process of keratinization, which consists of a sequence of biochemical and morphologic events that occur in the cell as it migrates from basal layer.
- Main morphologic change: Flattning of cells with long tonofiaments. Prevention of keratohyaline granule and disappearance of nucleus.
- Complete keratinization process leads to formation of orthokeratin.
- In parakeratin layer the stratum cornea retains pyknotic nuclei and the keratohyaline granules are dispersed.
- The uppermost cells of the stratum spinosum contains dense granules, i.e. keratinosome or Odland bodies which are modified lysosome.
Non-keratinocytes
- Melanocytes: These are dendritic cells located in the basal and spinous layers of the gingival epithelium.
- They synthesize melanin organelles called premelanosome/melanosome.
-
- Melanin are found or phagocytosed within the melanophages or melanophors.
- Langerhans cells: Dendritic cells located among the keratinocytes at all suprabasal level.
- These are modified monocytes derived from bone marrow.
- They have important role in immune reaction.
- They contain g-specific granules (Birbeck’s granule).
- They found in oral epithelium of normal gingiva, less in sulcular epithelium and absent in junctional epithelium.
- Merkel cells:
- Located in deeper layer of epithelium.
- Harbor the nerve endings and are connected to the adjacent epithelium by desmosome.
- They contain tactile receptors.
Gingival Fluid (Sulcular Fluid)
- Gingival fluid can be represented as either a transudate or an exudate.
- Gingival fluid consists of vast array of biochemical factors, thereby offring its potential use as a diagnostic or prognostic biomarker of the biologic state of the periodontium in health and disease.
- It also consists of components of connective tissue, epithelium, inflmmatory cells, serum, and microbial flora that inhabit the gingival margin or the sulcus.
- In healthy sulcus, the amount of gingival fluid is very small.
- During inflammation, the gingival fluid flow increases, and its composition starts to resemble that of an inflammatory exudate.
- The main route of the gingival fluid diffusion is via the basement membrane, through the relatively wide intercellular spaces of the junctional epithelium, and then into the sulcus.
- The gingival fluid is believed to do the following:
- Cleanse material from the sulcus
- It contain plasma proteins that may improve adhesion of the epithelium to the tooth
- It possess antimicrobial properties
- It exerts antibody activity to defend the gingiva.
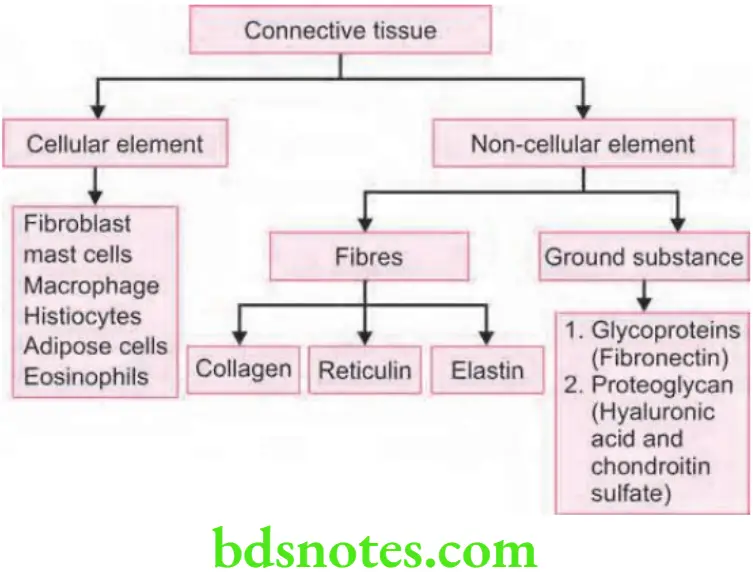
Gingival Connective Tissue
- The major components of the gingival connective tissue are collagen fibers i.e. about 60% by volume, fibroblasts i.e. 5%, vessels, nerves, and matrix i.e. about 35%.
- The connective tissue of the gingiva is called as lamina propria and it consists of two layers i.e.
- A papillary layer subjacent to the epithelium that consists of papillary projections between the epithelial rete pegs
- A reticular layer that is contiguous with the periosteum of the alveolar bone.
- Connective tissue has a cellular compartment and an extracellular compartment composed of fibers and ground substance.
- The ground substance fils the space between fibers and cells; it is amorphous, and it has a high water content. It is composed of proteoglycans (mainly hyaluronic acid and chondroitin sulfate) and glycoproteins (mainly fironectin).
- The three types of connective tissue fibers are collagen, reticular and elastic.
- Collagen type 1 forms the bulk of the lamina propria and provides the tensile strength to the gingival tissue. Type 4 collagen branches between the collagen type 1 bundles, and it is continuous with fibers of the basement membrane and the blood vessel walls.
Gingival Fibers
The gingival fibers are arranged in three groups:
Gingivodental
- The gingivodental fibers are those on the facial, lingual and interproximal surfaces.
- They are embedded in the cementum just beneath the epithelium at the base of gingival sulcus.
- On the facial and lingual surfaces, they project from cementum in fan-like confirmation towards the crest of alveolar ridge and the outer surface of marginal gingiva.
- They terminate on periosteum of bone or in the attached gingiva.
Circular Group
Circular group of fiber are course through connective tissue of the marginal and interdental gingiva and encircle the tooth in ring like fashion.
Transseptal Group
- They are located interproximally.
- It is formed by horizontal bundles that extend between the cementum of approximating teeth into which they are embedded.
- They lie in the area between epithelium at base of gingival sulcus and crest of interdental bone.
Other
Semicircular Fibers
Semicircular fibers are attached to the proximal surface of tooth just below the CEJ and go around facial or lingual marginal gingiva of the tooth, and attach on the other proximal surface of same tooth.
Transgingival Fibers
Attach in the proximal surface of one tooth, transverse interdental space and go around the facial/lingual surface of adjacent tooth, again traverse the interdental space and attach in proximal surface of next tooth.
Question 6. Write short note on gingival fibers.
Answer. Connective tissue of marginal gingiva is densely collagenous and consist a prominent system of collagen fiber bundles known as gingival fiber bundles.
Arrangement of Gingival Fibers
Arrangement of gingival fibers is described as principal group of five bundles and secondary group of minor fibers consisting of six sets.
Principal Group Fibers
- Dentogingival fibers: They project from the cementum in a fan-like conformation towards the crest and outer surface of the marginal gingiva. They provide support to the gingiva by attaching it to the tooth.
- Alveolar gingival fibers: They extend from the periosteum of the alveolar crest coronally into the lamina propria. Their function is to attach the gingiva to the alveolar bone.
- Dentoperiosteal fibers: They arise from the cementum near the cementoenamel junction and insert into the periosteum of the alveolar bone and protect the periodontal ligament.
- Circular fibers: They surround the tooth in a cuff or ring-like fashion and course through the connective tissue of the marginal and attached gingiva.
- Trans-septal fibers: They are located interproximally, they extend from cementum of one tooth to the cementum of the neighboring tooth. Their function is to protect the interproximal bone and maintain tooth-to-tooth contact.
Fibers of the Secondary Group
- Periosteogingival fibers: They extend from the periosteum of the alveolar bone to the attached gingiva. They help to attach the gingiva to the alveolar bone.
- Inter-papillary fibers: They are seen in the interdental gingiva extending in a faciolingual direction and support the gingival papilla.
- Transgingival fibers: These are seen in and around the teeth with in the attached gingiva. They maintain the alignment of teeth in the arch.
- Intercircular fibers: They extend from the cementum on distal surface of a tooth splaying buccally and lingually around the next tooth and are inserted on the mesial surface.
- Intergingival fibers: They are seen within the attached gingiva adjacent to the basement membrane extending mesiodistally. They provide support and contour for the attached gingiva.
- Semicircular fibers: They extend from the mesial surface of a tooth to the distal surface of same tooth in a half circle.
- Oxytalin fibers: They are present in all connective tissue structures of the periodontium. The function of these fibers is yet unknown.
- Elastin fibers: Elastin fibers are only present in connective tissue of the gingiva and periodontal ligament. They are also seen in the connective tissue of alveolar mucosa in large numbers.
Functions of Gingival Fibers
- To brace the marginal gingiva fimly against the tooth.
- These fibers provide rigidity to withstand the forces of mastication without being deflcted away from the tooth surface.
- To stabilize attached gingival to alveolar process and tooth.
- Helps to maintain epithelial seal to tooth.
- To provide stability to tooth.
Question 7. Discuss active and passive tooth eruption.
Or
Write short note on passive eruption.
Or
Write short note on Active and passive eruption.
Answer.
Active Tooth Eruption
- Active eruption is the movement of teeth in the direction of the occlusal plane.
- When the teeth reach their functional antagonists, the gingival sulcus and junctional epithelium are still on the enamel, and the clinical crown is approximately two-thirds of the anatomic crown.
- Active eruption is coordinated with attrition; the teeth erupt to compensate for tooth substance worn away by attition.
- Attrition reduces the clinical crown and prevents it from becoming disproportionately long in relation to the clinical root, thus avoiding excessive leverage on the periodontal tissues,
- Ideally, the rate of active eruption keeps pace with tooth wear, preserving the vertical dimension of the dentition.
- As teeth erupt, cementum is deposited at the apices and furcations of the roots, and bone is formed along the fundus of the alveolus and at the crest of the alveolar bone.
- In this way, part of the tooth substance lost by attrition is replaced by lengthening of the root, and socket depth is maintained to support the root.
Passive Tooth Eruption
- Passive eruption is the exposure of teeth by apical migration of gingiva.
- Passive eruption is now considered as pathologic process.
- Passive eruption is divided into the following four stages:
- Stage 1: The teeth reach the line of occlusion. The junctional epithelium and base of the gingival sulcus are on the enamel.
- Stage 2: The junctional epithelium proliferates so that part is on the cementum and part is on the enamel. The base of the sulcus is still on the enamel.
- Stage 3: The entire junctional epithelium is on the cementum, and the base of the sulcus is at the cementoenamel junction. As the junctional epithelium proliferates from the crown onto the root, it does not remain at the cementoenamel junction any longer than at any other area of the tooth.
- Stage 4: The junctional epithelium has proliferated farther on the cementum. The base of the sulcus is on the cementum, a portion of which is exposed. Proliferation of the junctional epithelium onto the root is accompanied by degeneration of gingival and periodontal ligament fibers and their detachment from the tooth. The cause of this degeneration is not understood. At present, it is believed to be the result of chronic inflammation and therefore a pathologic process.
Question 8. Write short note on mast cells.
Answer. Mast cells are the defense cells of PDL along with macrophages and eosinophills.
Shape of cell: Round or oval
Shape of nucleus: Round
Diameter: 12 to 15 µm.
- Mast cells are often associated with blood vessels and are characterized by numerous cytoplasmic granules. Granules are dense membrane bound vesicles of varying sizes.
- When cell is stimulated, it degranulates. Granules consist of heparin and histamine
- Physiologic role of heparin in mast cells is not clear.
- Histamine plays a role in inflmmatory reaction.
- Mast cells have been shown to degranulate in response to antigen-antibody reactions.
- Mast cells may play an important role in regulating endothelial and fibroblast cell population.
Question 9. What is stippling and its importance? Is stippling present since birth till the death of a person? Justify.
Answer. The surface of normal gingiva has a pitted or textured appearance characterized by numerous small depressions and elevations giving the tissue an orange-peel appearance known as stippling.
Importance
- It is a feature of healthy gingiva and reduction or loss of stippling is a common sign of gingival disease. It is restored after treatment.
- Microscopically, it represents the contours of epithelial connective tissue interface where bottom of the pit corresponds to the deep ridges or rete pegs of the epithelium in the lamina propria of connective tissue. The elevations of stippling correspond to the projection of papillae of connective tissue.
- Both elevations and depressions are covered by an overlying layer of keratinized stratified squamous epithelium.
- It is a form of adaptive specialization or reinforcement for function as the rete pegs arrangement between the epithelium and connective tissue provides an excellent mechanical stability and increased surface area, that can bear more masticatory forces.
- The degree of keratinization appears to be related to stippling. Hyperkeratosis results in a leathery texture, and drug-induced gingival overgrowth produces a nodular surface.
Criteria of Presence of Stippling from Birth till Death of Person
The pattern and extent of stippling vary among individuals or in different areas of same mouth according to age and sex. It is absent in infancy, appears at about 5 years of age, increases until adulthood and begins to disappear in old age.
Question 10. Discuss the distribution and clinical importance of gingival and periodontal group of fibers.
Answer.
Distribution and Clinical Importance of Gingival Fibers
- The connective tissue of marginal gingiva is densely collagenous containing a prominent system of collagen fiber bundles called as gingival fibers.
- The arrangement of gingival fibers is described as principal group of fie bundles and secondary group of minor fibers consisting of six sets.
Principal Group Fibers
- Dentogingival fibers: They project from cementum in a fanlike conformation towards the crest and outer surface of the marginal gingiva. They provide support to the gingiva by attaching it to the tooth.
- Alveolar gingival fibers: They extend from the periosteum of the alveolar crest coronally into the lamina propria. Their function is to attach the gingiva to the alveolar bone.
- Dentoperiosteal fibers: They arise from the cementum near the cementoenamel junction and insert into the periosteum of the alveolar bone and protect the periodontal ligament.
- Circular fibers: They surround the tooth in a cuf or ring like fashion and course through the connective tissue of the marginal and attached gingiva.
- Trans-septal fibers: They are located interproximally, they extend from cementum of one tooth to the cementum of the neighboring tooth. Their function is to protect the interproximal bone and maintain tooth-to-tooth contact.
Fibers of the Secondary Group
- Periosteogingival fibers: They extend from the periosteum of the alveolar bone to the attached gingiva. They help to attach the gingiva to the alveolar bone.
- Inter-papillary fibers: They are seen in the interdental gingiva extending in a faciolingual direction and support the gingival papilla.
- Transgingival fibers: These are seen in and around the teeth with in the attached gingiva. They maintain the alignment of teeth in the arch.
- Inter-circular fibers: They extend from the cementum on distal surface of a tooth splaying buccally and lingually around the next tooth and are inserted on the mesial surface.
- Intergingival fibers: They are seen within the attached gingiva adjacent to the basement membrane extending mesiodistally. They provide support and contour for the attached gingiva.
- Semicircular fibers: They extend from the mesial surface of a tooth to the distal surface of same tooth in a half circle.
- Oxytalin fibers: They are present in all connective tissue structures of the periodontium. The function of these fibers is yet unknown.
- Elastin fibers: Elastin fibers are only present in connective tissue of the gingiva and periodontal ligament. They are also seen in the connective tissue of alveolar mucosa in large numbers.
Distribution of PDL Fibers and Clinical Importance
- Most important elements of the periodontal ligament are principal fibers, which are collagenous and arranged in bundles and follow a wavy course when viewed in longitudinal section.
- Terminal portions of the principal fibers which are inserted into cementum and bone are known as Sharpey fibers.
- Principal fiber bundles consist of individual fibers which form a continuous anastomosing network between tooth and bone.
Principal Fiber
The principal fibers of the periodontal ligament are arranged in six groups that develop sequentially in the developing root i.e.
- Transseptal group
- Alveolar crest group
- Horizontal group
- Oblique group
- Apical group
- Interradicular group
Transseptal Group
- Transseptal fibers extend interproximally over the alveolar bone crest and get embedded in the cementum of adjacent teeth.
- These fibers are reconstructed even after destruction of the alveolar bone which results from periodontal disease.
- Transseptal fibers may be considered as belonging to the gingiva, because they do not have osseous attachment.
- These fibers lead to the maintenance of the teeth in the arch.
Alveolar Crest Group
- They extend obliquely from cementum just beneath the junctional epithelium to the alveolar crest.
- These fibers also run from the cementum over the alveolar crest and to firous layer of the periosteum which covers the alveolar bone.
- Alveolar crest fibers prevent extrusion of tooth and resist lateral tooth movements.
- Incision of these fibers at the time of periodontal surgery does not increase tooth mobility unless significant attachment loss has occurred.
- These fibers secure teeth inside the socket by resisting the lateral forces which are applied to the tooth.
Horizontal Group
- These fibers extend at right angles to the long axis of tooth from cementum to the alveolar bone.
- These fibers mainly prevent the lateral tooth movement.
Oblique Group
- Oblique fibers constitute the largest group in periodontal ligament and they extend from the cementum in a coronal direction obliquely to the bone.
- They absorb the chewing forces over the tooth and are the main support of the tooth.
- They resist the apically directed masticatory forces.
Apical Group
- Apical fibers radiate in irregular manner from the cementum to the bone at the apical region of the socket.
- They do not occur on incompletely formed roots.
- They prevent the tooth tipping and resist the forces of luxation.
Interradicular Group
- These fibers fan out from the cementum to the tooth in the furcation areas of multirooted teeth.
- They prevent tipping of tooth, forces of luxation and rotation.
Secondary Fibers of Periodontal Ligament
- Periodontal ligament has two immature forms are found: oxytalan and elaunin.
- The so-called oxytalan fibers run parallel to the root surface in a vertical direction and bend to attach cementum in cervical third of root. They are thought to regulate vascular low.
- Oxytalan fibers have been shown to develop de novo in the regenerated periodontal ligament.
- In addition to these fiber types, small collagen fibers associated with the larger principal collagen fibers have been described. Such fibers run in all directions and form a plexus called the indifferent fiber plexus.
Question 11. Define cementum. What are different types of cementum according to Schroder’s Classification. Enumerate different causes of cemental hypertrophy?
Or
Classify cementum.
Or
Write short note on Classification of cementum.
Answer. Cementum is Defined as a calcified avascular mesenchymal tissue that forms the outer covering of the anatomic root. It provides anchorage mainly to the principal fibers of periodontal ligament.
Schroder’s Classification
Depending on location, morphology and histological appearance, Shroeder and Page have classifid cementum as:
- Acellular afirillar cementum (AAC): It contains only the mineralized ground substance. It does not contain collagen fibers nor does it exhibit entrapped cementocytes. It is a product of cementoblasts and is found almost exclusively on the enamel near the cementoenamel junction with a thickness of 1 to 15 µm.
- Acellular extrinsic fier cementum (AEFC): By definition it is composed primarily of Sharpey’s fibers of periodontal, ligament but does not contain cementocytes. Developmentally they come to occupy the coronal one half of the root surface. Its thickness is between 30 and 230 µm.
- Cellular mixed stratifid cementum (CMSC): It harbors both intrinsic (cementoblasts derived) and extrinsic (firoblast derived) fibers and may contain cells. In humans, it is seen in the apical third of the roots, apices and furcation areas. Its thickness varies from 100 to 1000 µm.
- Cellular intrinsic fier cementum (CIFC): It contains only intrinsic fibers secreted by cementoblasts and not by the periodontal ligament firoblasts. In humans it fills the resorption lacunae.
- Intermediate cementum (or) the hyaline layer of Hopewell Smith: It is an ill-Defined zone extending from precementoenamel junction to the apical 1/3rd of the root. It appears to contain cellular remnants of Hertwigs sheath embedded in calcified ground substance. The significance of this layer is that, it contains enamel like proteins, which helps in attachment of cementum to dentin. It has been observed by many that, when this layer is removed during root planning procedure, the resultant reparative cementum that is formed will not be attached firmly on the dentin.
Causes of Cemental Hypertrophy
- Accelerated elongation of tooth: This owes to the loss of an antagonist and accompanied by cemental hypertrophy as a result of inherent tendency to maintain normal width of PDL.
- Inflmmation of a tooth: Inflmmation at the apex of tooth root usually occurring as a result of pulpal infection sometime leads to cemental hypertrophy.
- Tooth repair: On an occasion, occlusal trauma results in mild root resorption. Such resorption is repaired by cemental hypertrophy.
- Paget’s disease of bone: This is a disease of bones characterized by excessive cemental hypertrophy over the roots of teeth.
Question 12. Write short note on salivary antibacterial factors and its role in periodontology.
Answer. Saliva contains numerous inorganic and organic factors that influence bacteria and their products in the oral environment. Inorganic factors include ions and gases, bicarbonate, sodium, potassium, phosphates, calcium, florides, ammonium, and carbon dioxide. Organic factors include lysozyme, lactoferrin, myeloperoxidase, lactoperoxidase, and agglutinins such as glycoproteins, mucins, b2-macroglobulins, fironectins and antibodies.
- Lysozyme is a hydrolytic enzyme that cleaves the linkage between structural components of the glycopeptides muramic acid-containing region of the cell wall of certain bacteria in vitro.
- Lysozyme works on both gram-negative and gram-positive organisms; its targets include Veillonella species and Actinobacillus actinomycetemcomitans. lt probably repels certain transient bacterial invaders of the mouth.
- The lactoperoxidase-thiocyanate system in saliva has been shown to be bactericidal to some strains of Lactobacillus and Streptococcus by preventing the accumulation of lysine and glutamic acid, both of which are essential for bacterial growth.
- Another antibacterial finding is lactoferrin, which is effective against Actinobacillus Species.
- Myeloperoxidase, an enzyme similar to salivary peroxidase, is released by leukocytes and is bactericidal for
- Actinobacillus but has the added effect of inhibiting the attachment of Actinomyces strains to hydroxyapatite.
Question 13. Write short note on tooth ankylosis.
Answer. Fusion of alveolar bone and cementum with obliteration of periodontal ligament is known as tooth ankylosis.
- Ankylosis occurs more frequently in the deciduous dentition.
- Ankylosis generally occurs in teeth with cemental resorption.
- It represents a form of abnormal repair.
- Ankylosis occurs after reimplantation, trauma to a tooth, etc.
- Ankylosis results in resorption of root and its replacement by bone.
- Clinically ankylosed tooth lacks physiologic abnormality of normal tooth which is the diagnostic sign for ankylotic resorption.
- Ankylosed tooth have a metallic percussion sound.
- As periodontal ligament is replaced with bone in ankylosis, proprioception is lost because pressure receptors in periodontal ligament are vanished away or do not function correctly.
Question 14. Write key features and structural constituents of the periodontal ligament. Write about cellular part of the periodontal ligament.
Answer.
Key Features
- Periodontal ligament is a connective tissue structure which surrounds the root and connects it with the bone.
- Periodontal ligament is continuous with lamina propria of gingiva.
- It communicates with marrow spaces of alveolar bone.
- Its average width is 0.2 mm and with ranges from 0.15 to 0.38 mm.
- It remains in form of hourglass with narrow portion around middle third of root.
- PDL diminish around the teeth which are not functional and increases in width in hyperfunctional teeth.
- Turnover of fibers and ground substance of tooth is high while turnover of cells is slow.
- Previously PDL was also known as gomphosis, desmodont, pericementum, alveolodental ligament and periodontal membrane.
Question 15. Write short note on junctional epithelium.
Or
Describe junctional epithelium.
Answer.
- Junctional epithelium consists of a collar-like band of stratified squamous non-keratinized epithelium.
- It is 3–4 layer thick in early life but increases with age upto 10 to 20 layer.
- The length of junctional epithelium ranges from 0.25 to 1.35 mm.
- These cells can be grouped in two strata: the basal layer that faces the connective tissue and the suprabasal layer that extends to the tooth surface.
- The proliferative layer which leads to most of the cell divisions is located in contact with the connective tissue. Shedding surface of junctional epithelium is located at the coronal end which forms bottm of gingival sulcus.
- Junctional epithelium is formed by conflence of the oral epithelium and the reduced enamel epithelium at the time of eruption.
- Junctional epithelial cells are interconnected by few desmosomes and occasionally by gap junctions.
- Junctional epithelium, mainly at its basal cell layers is innervated by the sensory nerve fibers.
- Division of junctional epithelium is there in three zones i.e. coronal, middle and apical.
- Junctional epithelium is attached to the tooth surface by means of an internal basal lamina and to the gingival connective tissue by an external basal lamina which has the same structure as other epithelial–connective tissue attachments elsewhere in the body.
- External basal lamina consists of same structure and the composition as other basement membranes, elsewhere in the body while the internal basal lamina has different structural and molecular characteristics. This lacks the common basement membrane components i.e. collagen Type 4 and 7, most laminins forms.
- The internal basal lamina consists of a lamina densa (adjacent to the enamel) and a lamina lucida to which hemidesmosomes are attached. Hemidesmosomes have a decisive role in the fim attachment of the cells to the internal basal lamina on the tooth surface.
- Junctional epithelial cells migrate in the coronal direction to free surface where they desquamate. As the surface area occupied by basal cells is more than bottm of sulcus, exfoliation occurs at extremely high rate.
- Attachment of the junctional epithelium to the tooth is reinforced by the gingival fibers, which brace the marginal gingiva against the tooth surface. So, the junctional epithelium and gingival fibers are considered as functional unit.
- Dentogingival unit: Dentogingival unit = junctional epithelium + gingival fibers.
- Intercellular spaces of junctional epithelium give a pathway for fluid and transmigrating the leukocytes. In absence of clinical signs of inflmmation, approximately 30,000 PMNs migrate per minute via junctional epithelium of all human teeth in the oral cavity.
Question 16. Define gingiva. Write in detail about the structural and metabolic characteristics of oral epithelium, sulcular epithelium and junctional epithelium.
Answer. Gingiva is the part of oral mucosa that covers the alveolar process of the jaws and surrounds the neck of teeth.
Structural and Metabolic Characteristics of Oral Epithelium
- Oral epithelium covers the crest and outer surface of the marginal gingiva and the surface of the attached gingiva.
- On an average, the oral epithelium is 0.2 to 0.3 mm in thickness.
- It is keratinized or parakeratinized or presents various combinations of these conditions. The prevalent surface, however, is parakeratinized.
- Oral epithelium is composed of four layers: stratum basale, stratum spinosum, stratum granulosum and stratum corneum.
- Keratinization of the oral mucosa varies in different areas in the following order: palate (most keratinized), gingiva, ventral aspect of the tongue, and cheek (least keratinized).
- Keratins K1, K2, and K10 to K12, which are specific to epidermal-type differentiation, are immunohistochemically expressed with high intensity in orthokeratinized areas and with less intensity in parakeratinized areas.
- K6 and K16, characteristic of highly proliferative epithelia and K5 and K14, stratifiation-specifi cytokeratins also are present.
- Parakeratinized areas express K19, which is usually absent from orthokeratinized normal epithelia.
- In keeping with the complete or almost-complete maturation, histoenzyme reactions for acid phosphatase and pentose-shunt enzymes are very strong.
- Glycogen can accumulate intracellularly when it is not completely degraded by any of the glycolytic pathways. Thus, its concentration in normal gingiva is inversely related to the degree of keratinization and inflammation.
Structural and Metabolic Characteristics of Sulcular Epithelium
- Sulcular epithelium lines the gingival sulcus.
- It is a thin, non-keratinized stratifid squamous epithelium without rete pegs, and it extends from the coronal limit of the junctional epithelium to the crest of the gingival margin.
- It usually shows many cells with hydropic degeneration.
- As with other nonkeratinized epithelia, the sulcular epithelium lacks granulosum and corneum strata and K1, K2, and K10 to K12 cytokeratins, but it contains K4 and K13, the so-called esophageal-type cytokeratins.
- It also expresses K19 and normally does not contain Merkel cells.
- Histochemical studies of enzymes have consistently revealed a lower degree of activity in the sulcular than in the outer epithelium, particularly in the case of enzymes related to keratinization.
- Glucose 6 phosphate dehydrogenase expressed a faint and homogeneous reaction in all strata, unlike the increasing gradient toward the surface observed in cornified epithelia.
- Acid phosphatase staining is negative, although lysosomes have been described in exfoliated cells.
Structural and Metabolic Characteristics of Junctional Epithelium
- Junctional epithelium consists of a collar-like band of stratified squamous non-keratinizing epithelium.
- It is three to four layers thick in early life, but the number of layers increases with age to 10 or even 20 layers.
- Junctional epithelium tapers from its coronal end, which may be 10 to 29 cells wide to one or two cells at its apical termination, located at the cementoenamel junction in healthy tissue. These cells can be grouped in two strata: the basal layer facing the connective tissue and the suprabasal layer extending to the tooth surface.
- The length of the junctional epithelium ranges from 0.25 to 1.35 mm.
- The junctional epithelium is formed by the confluence of the oral epithelium and the reduced enamel epithelium during tooth eruption. However, the reduced enamel epithelium is not essential for its formation; in fact, the junctional epithelium is completely restored after pocket instrumentation or surgery, and it forms around an implant.
- Cell layers that are not juxtaposed to the tooth, exhibits numerous free ribosomes and prominent membrane bound structures, such as Golgi complexes, and cytoplasmic vacuoles, presumably phagocytic.
- Lysosome-like bodies also are present, but the absence of keratinosomes (Odland bodies) and histochemically demonstrable acid phosphatase, correlated with the low degree of differentiation, may reflct a low defense power against microbial plaque accumulation in the gingival sulcus.
- Junctional epithelium expresses Kl9, which is absent from keratinized epithelia, and the stratifiation-specifi cytokeratins K5 and Kl4.
- Another particular behavior of junctional epithelium is the lack of expression of K6 and Kl 6, which is usually linked to highly proliferative epithelia, although the turnover of the cells is very high.
- Junctional epithelium exhibits lower glycolytic enzyme activity than outer epithelium, and it lacks acid phosphatase activity.
- Junctional epithelium is attached to the tooth surface (epithelial attachment) by means of an internal basallamina. lt is attached to the gingival connective tissue by an external basal lamina that has the same structure as other epithelial—connective tissue attachments elsewhere in the body.
- Internal basal lamina consists of a lamina densa (adjacent to the enamel) and a lamina lucida to which hemidesmosomes are attached. Hemidesmosomes have a decisive role in the firm attachment of the cells to the internal basal lamina on the tooth surface.
- Histochemical evidence for the presence of neutral polysaccharides in the zone of the epithelial attachment has been reported.
- The attachment of the junctional epithelium to the tooth is reinforced by the gingival fibers, which brace the marginal gingiva against the tooth surface.
Question 17. Write short note on types of cementoenamel junction.
Answer. The relation between cementum and enamel at cervical region of teeth is called as cementoenamel junction.
Types of Cementoenamel Junction
- End-to-end approximating junction (But Junction):
- In approximately 30% of all teeth cementum meets the cervical end of enamel in a relatively sharp line.
- Overlapping junction:
- The cementum overlapping the enamel:
- In approximately 60% of teeth, cementum overlaps the cervical end of enamel for short distance.
- This occurs when the enamel epithelium degenerates at its cervical termination permittng connective tissue to come in direct contact with enamel surface which produce a laminated, electron dense, reticular material termed as a fibrillar cementum.
- Enamel overlapping cementum junction:
- Recent observations by researchers by optical microscopy showed fourth type of junction known as enamel-overlapping cementum junction.
- The cementum overlapping the enamel:
- Gap junction:
- The absence of connecting enamel and cementum:
- In about 10% of teeth enamel and cementum do not meet. In such cases, there is no cemento enamel junction. This occurs when enamel epithelium in cervical portion of roots delayed in the separation from dentin. In this case, dentin is an external part of the surface of the root.
- The absence of connecting enamel and cementum:
Question 18. Write short note on dentogingival unit.
Answer. Dentogingival unit was first discovered by Listgarten in 1970.
- Attachment of junctional epithelium to the tooth is reinforced by the gingival fibers which brace marginal gingiva against the tooth surface, due to this junctional epithelium and gingival fibers are considered as a functional unit known as dentogingival unit.
- Dentogingival unit is of importance because of its anatomical location.
- Both the components of dentogingival unit afford biological protection.
Question 19. Write short note on gingival crevicular fluid.
Or
Write short note on functions of gingival crevicular fluid.
Or
Write short note on GCF.
Or
Discuss gingival crevicular fluid (GCF).
Answer. Gingival sulcus consists of fluid known as gingival crevicular fluid or sulcular fluid.
- Gingival crevicular fluid is an important diagnostic marker.
- Gingival crevicular fluid is an inflmmatory exudate.
- Gingival crevicular fluid is composed mainly of blood electrolytes and organic molecules, i.e. albumins, globulins, lipoproteins or fibrinogen and cellular components as well as peptides, bacteria and enzymes.
Production of Gingival Crevicular Fluid
It is obtained from gingival plexus of blood vessels in gingival connective tissue subjacent to epithelial lining of dentogingival space. GCF production is governed by passage of fluid from capillaries into tissues and removal of this fluid by lymphatic system. When the rate of capillary fitrate exceeds lymphatic uptake, fluid collects as edema and get expressed as gingival crevicular fluid.
Clinical Signifiance
Following is the clinical signifiance:
- Circadian periodicity: Increase in the amount of gingival crevicular fluid is from 6 am to 10 pm and decreases afterwards.
- Sex hormones: Female sex hormones increase the gingival crevicular fluid flow as these hormones lead to the vascular permeability.
- Mechanical stimulation: Chewing and gingival brushing stimulates flow of gingival crevicular fluid.
- Smoking: It causes too much increase in gingival crevicular fluid flow.
- Periodontal therapy: There is increase in gingival crevicular fluid production at the time of healing after periodontal therapy.
Composition of GCF
It is composed of following:
- Epithelial cells: Presence of intense mitotic activity in both junctional and sulcular epithelium attibute to presence of desquamated epithelial cells in gingival crevicular fluid. Remnants of epithelial cells along with adhered microorganisms are found in gingival crevicular fluid.
- Leucocytes: PMN is predominant inflmmatory cell in gingival crevicular fluid. Most of crevicular polymorphoneutrophils are viable cells capable of protecting dentogingival junction and prevents apical extension of subgingival plaque in spite of decreased efficiency. Crevicular PMNs in diseased areas show decrease in phagocytic activity and decreased migration when compared to healthy sites.
- Bacteria: Microorganisms are found free floating or attached to epithelial cells in gingival crevicular fluid.
- Products of microbial plaque:
- Endotoxin such as bacterial LPS.
- Enzymes such as proteinases, MMPs, hyalurodinases
- End products of microbial metabolism, i.e. short chain fatty acids, ammonia, etc.
- Tissue breakdown products: Collagens, proteoglycans, hyaluronic acid, ECM components and enzymes.
- Product of host cells: Collagenases, Aspartate aminotransferase, Alkaline phosphatase, elastase, cathepsin, lysozyme, lactoferrin.
- Product of host immunity: Immunoglobulins, complements, Cytokines, Arachidonic acid metabolites.
Signifiance of Gingival Crevicular Fluid in Health and Disease
- Gingival crevicular fluid consists of multiple biochemical factors which act as diagnostic and prognostic markers of biologic state of periodontium in health and disease.
- In healthy sulcus quantity of crevicular fluid is very small while during inflmmation flw of crevicular fluid increases and its composition is of inflmmatory exudate.
- In healthy it cleans material from the sulcus.
- It improves adhesion of epithelium to tooth since it consists of plasma proteins.
- GCF flow decreases progressively in parallel with clinical changes postperiodontal treatment.
- GCF flow follows circadian rhythm. There is increase in flow of GCF early in morning and it decreases afterwards.
- GCF flow increases during pregnancy, puberty and menstruation.
- Smoking produces immediate transient but marked increase in GCF flw.
- Systemically administered drugs were found to expressed in GCF especially drugs such as tetracycline and metronidazole. Concentration of these drugs in GCF is found to be higher than saliva.
Functions of GCF
Following are the functions of gingival crevicular fluid:
- Gingival crevicular fluid consists of many biochemical factors which offr it as a diagnostic or prognostic biomarker of biologic state of periodontium in health and disease.
- Gingival crevicular fluid consists of components of connective tissue, epithelium and inflmmatory cells, serum and microbial flra inhabiting gingival margin or sulcus.
- Gingival crevicular fluid clean material from the sulcus.
- It consists of plasma proteins which improve adhesion of epithelium to the tooth.
- Gingival crevicular fluid possess anti-microbial properties.
- It exerts antibody activity for defending the gingiva.
- PMN activity releases granules which disengages plaque adherence to tooth.
Question 20. Define cementum. Classify cementum according to Schroeder. Write about features of cellular and acellular cementum.
Answer. Cementum is a calcified avascular mesenchymal tissue that forms the outer covering of anatomic root.
Features of Acellular Cementum
- It is the fist cementum formed and covers the cervical third of root.
- Acellular cementum is devoid of cells.
- It is seen at the coronal portion of root.
- Formation of acellular cementum is slow.
- Acellular cementum forms before teeth reaches the occlusal plane, its thickness ranges from 30 to 230 µm.
- Sharpey’s fibers form the most structure of acellular cementum.
- Most of the Sharpey’s fibers are inserted at right angles to root surface and penetrate inside the cementum while other enter at different directions.
- Arrangement of collagen fibers is more organized in acellular cementum.
- Cementoid is absent in this cementum.
- Main function of acellular cementum is anchorage.
- Under light microscope, it appears structureless, incremental lines are closer and there is mineralization of Sharpey’s fibers.
Features of Cellular Cementum
- Cellular cementum forms after tooth reaches the occlusal plane.
- It is seen in the apical half of root surface.
- Formation of cellular cementum is rapid.
- Cellular cementum is irregular and consists of cells known as cementocytes which reside in lacunae and communicate with each other by anastomoting canaliculi.
- Cellular cementum is less calcified.
- Sharpey’s fibers occupy the small portion of cellular cementum.
- Sharpey’s fibers here are completely or partially calcified.
- Cementoid formation is seen over its surface.
- Main function of cellular cementum is repair and adaptation.
- Under light microscope, it shows cementocytes, incremental lines are further apart, intrinsic fibers are densely packed and run parallel to surface, extrinsic fibers are large and haphazardly arranged.
Question 21. Write short note on stippling.
Or
Explain stippling of gingiva.
Answer. The surface of normal gingiva has a pitted or textured appearance characterized by numerous small depressions and elevations giving the tissue an orange- peel appearance known as stippling.
- Stippling should be best viewed by drying the gingiva.
- Stippling is a form of adaptive specialization or reinforcement for function.
- Attached gingiva is stippled while marginal gingiva is not stippled.
- Central portion of interdental papillae is stippled.
- Stippling vary among the individuals and in various areas of same mouth.
- Stippling is less prominent on lingual surfaces as compared to facial surfaces.
- Microscopically stippling is produced by alternate round protuberances and depressions on gingival surface. Papillary layer of connective tissue project in elevation and the elevated and depressed areas covered by stratified squamous epithelium.
- Stippling is the feature of healthy gingiva and reduction or loss of stippling is the sign of gingival disease. As gingiva become healthy stippling again regains after the disease.
- Stippling varies with age, it is absent in infancy, appear in children at 5 years of age, increases till adulthood and disappear in old age.
Question 22. Write short note on cementum.
Answer. Cementum is calcified avascular mesenchymal tissue which forms the outer covering of anatomic root.
Composition of Cementum
- Cementum consists of 46% inorganic and 54% organic matter.
- Inorganic portion consists of calcium and phosphate in form of hydroxyapatite. Trace elements are also present in the cementum. It consists of highest floride content of all the mineralized tissue.
- Organic portion consists of 90% of Type I collagen, 5% of Type 3 collagen and 5% non – collagenous proteins such as enamel proteins, adhesion molecules like tenascin and fironectin, glycosaminoglycans like chondroitin sulphate, dermatan sulphate and heparin sulphate which constitutes the remaining organic matrix.
- Two of the main sources of collagen fibers in cementum are:
- Sharpey’s fibers which are the embedded portion of principle fibers of periodontal ligament and are formed by firoblasts.
- Intrinsic fibers which are the fibers belonging to cementum matrix and are produced by cementoblasts.
- Non-collagenous components of interfibrillar ground substance are proteoglycans, glycoproteins and phosphoproteins.
Functions of Cementum
- Primary function of the cementum is to provide anchorage to tooth in its alveolus. It is achieved via collagen fiber bundles of periodontal ligament whose ends are embedded inside the cementum.
- It plays an important role in maintaining the occlusal relationships whenever the incisal and occlusal surfaces are abraded because of attition, tooth supraerupt in order to compensate for loss and the deposition of new cementum occur at apical root area.
- It act as major reparative tissue for the root surfaces and maintains integrity of root surface.
Question 23. Write short note on non-keratinocytes.
Answer. The various non-keratinocytes or clear cells are Langerhans cells, Merkel cells and melanocytes.
- Langerhans cells: They are dendritic cells located among keratinocytes at all suprabasal levels. They belong to the mononuclear phagocyte system (reticuloendothelial system) as modified monocytes derived from the bone marrow. They contain elongated granules, and they are considered macrophages with possible antigenic properties. Langerhans cells have an important role in the immune reaction as antigen-presenting cells for lymphocytes. They contain gspecifi granules (Birbeck granules), and they have marked adenosine triphosphatase activity. They are found in the oral epithelium of normal gingiva and in smaller amounts in the sulcular epithelium; they are probably absent from the junctional epithelium of normal gingiva.
- Merkel cells: They are usually found in the basal cell layer of the gingival epithelium. These cells either appear individually or in clusters. These are not dendritic cells as melanocytes and Langerhans cells. These cells possess keratin tonofiaments and occasional desmosomes, which link them to adjacent cells. These cells are sensory in nature and respond to touch.
- Melanocytes: They origin from neural crest cells located in the stratum basale and spinous cell layers of the oral gingival epithelium. Oral mucosal melanocytes were identified in the gingiva by Laidlaw and Cahn in 1932. Long dendritic processes from these cells are interposed between the keratinocytes of the epithelium. They lack tonofiaments and desmosomal connection to adjacent keratinocytes. Melanocytes are responsible for the barrier to ultraviolet (UV) damage and synthesize melanin, which is accountable for providing color to the gingiva. Melanin is synthesized in organelle called premelanosomes or melanosomes in melanocytes. Melanosomes consists of tyrosinase which hydroxylate tyrosine to dihydroxyphenylalanine which in turn is progressively converted to melanin. Melanin granules are phagocytosed and contained within other cells of epithelium and connective tissue known as melanophages or melanophores.

Leave a Reply