Tetanus and Gas Gangrene Tetanus
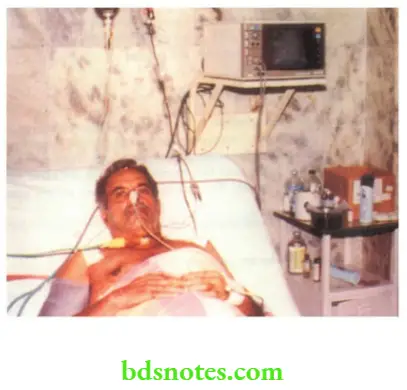
A nonimmunised, eighteen-year-old girl was admitted with moderate tetanus following a nail prick in her foot. In the hospital, she developed convulsions, laryngeal oedema and cardiac arrest from which she was resuscitated and shifted to the intensive care unit under anaesthesiologist’s care.
Tracheostomy and mechanical ventilation along with sedation were used. Unlike others, she was lucky. She walked home after two months of stay in the intensive care unit after a lot of suffering and spending a large amount of money. The case history has been written here to impress upon the students.
Read And Learn More: Clinical Medicine And Surgery Notes
Aetiopathogenesis
Tetanus is a serious disorder with very high mortality even with treatment. The disease is caused by Clostridium tetani, an anaerobic spore-forming bacillus with a terminal spore which has a drumstick-like appearance.
Possible Routes Of Infection Are
- Umbilical cord—in neonates, seen in communities that practise cow dung application on the umbilical stump.
- Wound—a complication of road traffic accidents where aerobic organisms reduce oxygen tension in the wound and thereby facilitate the growth of anaerobic Clostridium tetani.
- Minor injuries with rusted nails, piercing of the ear lobes, tattooing, injections, etc.
- Endogenous infection after septic abortion or surgical operations on the gastrointestinal tract.
- Tetanus due to infection acquired in the operation theatre.
- Thus, tetanus is a wound infection. “NO WOUND, NO TETANUS” is true. Having entered the wound, the organisms multiply and produce powerful exotoxins which produce the disease. Thus, the organisms by themselves, do not produce the disease. The toxins produced by the organisms are tetanospasmin (neurotoxin) and tetanolysin (haemolysin).
- Tetanospasmin has an affinity towards nervous tissues. It reaches the central nervous system along the axons of motor nerve trunks. The toxin gets fixed to the motor cells of the anterior horn cells. The toxin, which is fixed to the motor end plate, acts in the following ways.
- It inhibits the release of Cholinesterase which causes accumulation of acetylcholine at the motor end plate which is responsible for tonic rigidity of the limb, trunk, abdominal and neck muscles.
- It acts at the spinal level and causes reflex contraction of muscles due to minor stimuli.
- The toxin which is fixed to the nervous tissue cannot be neutralised. However, the circulating toxin can be neutralised. The incubation period may vary from a few days to months or years. Hence, it is not important. The interval between the first symptom (dysphagia and stiffness of the jaw) to a reflex spasm is called the period of onset. If this is less than 48 hours, the prognosis is poor and if more than 48 hours, the prognosis is better.
Tetanus Causes
Favourable Conditions For The Development Of Tetanus
- No immunisation
- Foreign body
- Injury
- Improper sterilisation
- Devitalised tissues
- Anaerobic conditions.
Special Types Of Tetanus
- Tetanus Neonatorum: It occurs due to contamination of the umbilical cord in children born to non-immunised mothers. It manifests usually around 6–8 days of birth and is called an Eighth-day disease. It carries almost 100% mortality.
- Local tetanus: In this, contraction of muscles occurs in the neighbourhood of the wound.
- Cephalic tetanus: Usually occurs after a wound of the head and face. Cranial nerves like the facial nerve and oculomotor nerve can get paralysed. It carries a poor prognosis.
- Bulbar tetanus: It is a condition wherein muscles of deglutition and respiration are involved. It is fatal.
- Latent tetanus: It develops after a few months to years following a wound which might have been forgotten.
- Puerperal tetanus: It occurs as a complication of abortion or puerperal sepsis.
- Postoperative tetanus: Occurs due to improper sterilisation of instruments and carries 100% mortality. In an ideal operation theatre, this type of tetanus should not occur.
- Otitis tetanus: It is due to chronic suppurative otitis media. In these cases, the wound is a tear in the tympanic membrane. It can occur in any age group, but commonly in children and young adults.
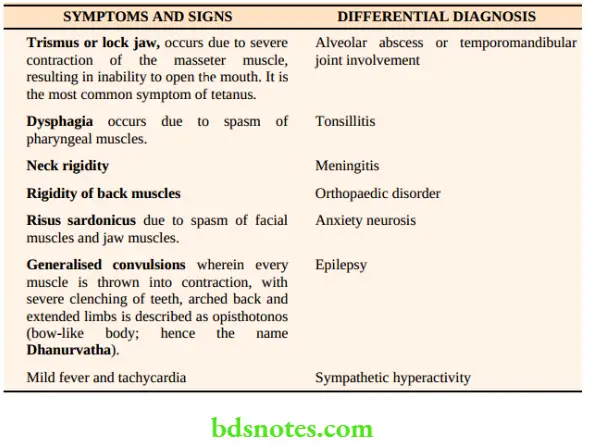
Clinical Features
- Autonomic dysfunction: Increased basal sympathetic tone manifesting as tachycardia and bladder, bowel dysfunction, labile hypertension, pyrexia, pallor, sweating and cyanosis of the digits can occur.
- Episodes of bradycardia, low central venous pressure (CVP) and even cardiac arrest. have been reported due to parasympathetic dysfunction.
- They can develop complications such as pneumonia, urinary tract infection, etc.
Treatment Of Established Tetanus
- General management
- Specific management.
General Management
- Admission and isolation in a quiet room, to avoid minor stimuli which precipitate spasms.
- Wound care which includes drainage of pus, excision of necrotic tissue, removal of foreign body and proper dressing.
- Inj. Tetanus toxoid 0.5 ml to be given IM
Isolation for tetanus has been misunderstood by surgeons. It is a fact that in the majority of hospitals, tetanus patients are isolated in a remote comer of the hospital, well away from the reach of a skilled person. Many cases die due to convulsions and laryngeal spasms before they are intubated and resuscitated. Critically ill patients are admitted to an intensive care unit under the supervision of anaesthesiologist’s care in our institution. Tetanus is NOT COMMUNICABLE from person to person.
Tetanus Causes
- Antitetanus serum (ATS) is 50,000 units intramuscular (IM) and 50,000 units intravenous (IV). This should be given only after giving a test dose which consists of diluting a small dose of serum with ten times saline and injecting a small amount in the subcutaneous tissue. It has become less popular due to the availability of human antitetanus globulin.
- Instead of ATS, human antitetanus globulin is better and safer. It does not cause anaphylaxis. It is given in a dose of 3000 to 4000 units IV. No test dose is required.
- Inj. crystalline penicillin 10 lakh units every 6 hours is the drug of choice against Clostridium tetani. It may have to be given for a period of 7–10 days.
- Metronidazole 500 mg IV 8th hourly for 10 days. It has been shown to be more effective than penicillin.
- After recovery, full immunisation with tetanus toxoid is a must.
Tetanus Causes
Specific Management
1. Mild Cases
- There is only tonic rigidity without spasm or dysphagia. These patients are managed by heavy sedation by using a combination of drugs so as to avoid spasms or convulsions. An example of the method of treatment followed in our hospital.
- Benzodiazepines and morphine act centrally to minimise the effects of tetanospasmin.
- Chlorpromazine being a —receptor blocker, can decrease sympathetic activity, other blockers such as phenoxybenzamine, phentolamine also been used. These drugs are repeated in such a way that every two hours the patient receives some
- Sedative. The dosage of the drugs is adjusted once in 2 or 3 days so as to get the maximum effect of sedation or relaxation.
- Injection of diazepam 10 mg, tracheostomy set, and resuscitation set which includes laryngoscope and endotracheal tube should be kept ready by the side of the patient.
Drug
- Chlorpromazine
- Phenobarbitone
- Diazepam
Dosage
- 50–100 mg
- 30–60 mg
- 10–20 mg
Time
- 8 AM-2 PM–8 PM-2 AM
- 10 AM-4 PM–10 PM-4 AM
- 12 Noon-6 PM–12 MN-6 AM
2. Seriously Ill Cases
- They have dysphagia and reflex spasms
- A nasogastric tube is introduced for feeding purposes and to administer the drugs.
- Tracheostomy, if breathing difficulty arises.
3. Dangerously Ill Cases
This group includes patients with major cyanotic convulsions. In addition to continuing sedatives, these patients are paralysed with muscle relaxants (neuromuscular blocking agents) and positive pressure ventilation is given till they recover. One cannot predict exactly how many days a patient requires ventilatory support. During this period adequate nutrition, care of the urinary bladder, care of the bowel, and frequent change of position to avoid bed sore, have to be taken care of.
Prophylaxis
- Tetanus neonatorum can be prevented by immunisation of the mother with two tetanus toxoid injections, half ml IM given in the third trimester of pregnancy.
- Infants and children are immunised with tetanus toxoid, diphtheria and pertussis vaccine (DPT) in three doses at 6, 10, and 14 weeks of age. This is called a triple antigen. A booster dose is given at 18 months and school-going time (5 years), and once in five years 1 ml of tetanus toxoid is given to achieve active immunity.
- An immunised individual who receives a provocative injury is administered a booster dose if he has not been given in the previous 5 years.
- Tetanus can be prevented by giving tetanus antitoxin in the following situations.
-
- Wounds of head and face, penetrating wounds
- Wounds with contused and devitalised tissues
- War wounds and road traffic accidents
In such patients, a dose of 250 units of human antitetanus globulin will give adequate protection.
Causes Of Death
- Aspiration of pharyngeal contents into the lungs resulting in aspiration pneumonia
- Laryngeal spasm and respiratory arrest resulting in cardiac arrest
- Autonomic disturbances resulting in cardiac arrhythmia.
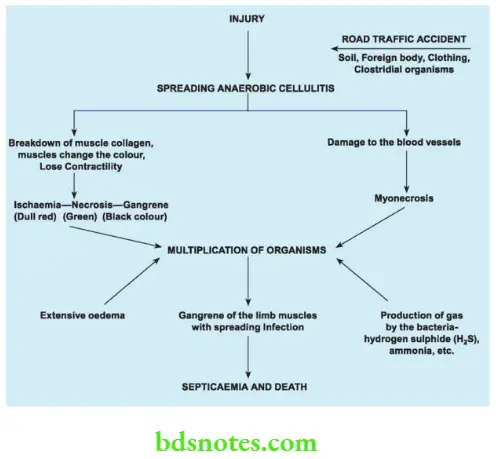
Gas Gangrene
It is a highly fatal spreading infection caused by clostridial organisms which results in myonecrosis.
Other Names For Gas Gangrene Are
Clostridial myositis, clostridial myonecrosis, infective gangrene of the muscles.
Tetanus Causes
Aetiology
The disease is caused by Clostridium perfringens (Clostridium welchii)—the most common organism (60%). Other organisms are Clostridium septicum, Clostridium redemptions, and Clostridium histolyticum.
Source Of Infection
Manured soil or cultivated soil, normal intestines.
Risk Group: Lower limb amputations performed for ischaemic gangrene of limb infection from patient’s own bowel organisms. High-velocity gunshot wounds with perforation of hollow viscus are also associated with the risk of developing gas gangrene.
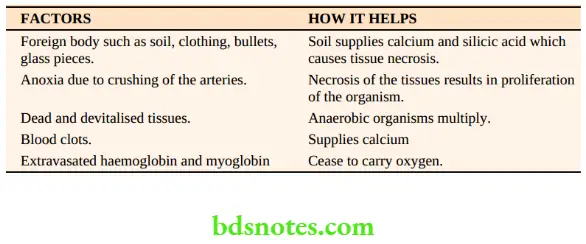
Pathogenesis
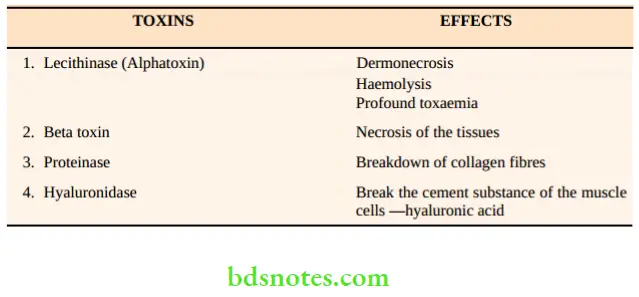
- Gas gangrene develops in wounds where there is heavy contamination with soil or a foreign body or which is associated with laceration and devitalised muscle mass. This type of situation is common today following road traffic accidents. Endogenous infection from a patient’s faecal matter may be responsible for gas gangrene, in certain cases of contamination of a surgical wound such as below-knee amputation done for some other cause. Having entered the wound, Clostridia multiply and produce powerful toxins.
- All these factors contribute to creating a low oxygen tension. Under these favourable conditions,
clostridial organisms multiply and produce toxins which cause further tissue damage. The
toxins produced by the organisms and their effects are given in Table 5.3. - Once powerful toxins start acting, various pathological events occur such as inflammation, oedema, muscle necrosis and gangrene of the muscles. These events are summarised below.
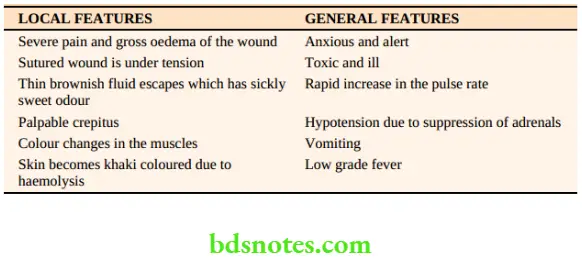
Clinical Features
In untreated cases, the necrotic process continues, and septicaemia, renal failure, peripheral circulatory failure and death occur. Foaming liver is the condition wherein gas is produced in the liver, as a part of septicaemia.
Prophylaxis
A highly fatal disease, gas gangrene can be prevented by following principles while managing the wound.
Palpable Crepitus—Conditions
- Anaerobic infections
- Streptococcal infections
- Surgical emphysema due to oesophageal, tracheal rupture
- Gas gangrene
- Debridement: All dead, necrotic tissue, bone pieces and foreign material are removed. Pus is evacuated. The wound is thoroughly irrigated with antiseptic agents. If there is a fracture, it has to be managed by orthopaedicians following the principles of fracture management.
When in doubt do not suture the wound. - Prophylactic antibiotics: Penicillin is the drug of choice. Injection Crystalline Penicillin 10– 20 lakh units, 4–6 hourly is given for a period of seven days.
- Judicious and minimal use of tourniquet. If possible, avoid a tourniquet while managing such a wound in the leg.
- Gentle but effective application of a plaster cast with or without treatment of associated fractures to avoid compression on the blood vessel.
Tetanus Causes
Crepitus Diagnosis
- In addition to clinical suspicion one of the easy methods of confirming the diagnosis is to examine the pus under microscopy after staining with Giemsa stain.
- These organisms are gram-positive spore-bearing.
Treatment of Established Gas Gangrene
- Emergency surgery which includes excision of all dead muscles and necrotic tissues by using generous, long incisions.
- Penicillin is to be continued.
- Blood transfusions before, during and after surgery.
- Polyvalent antigas gangrene serum
- Hyperbaric oxygen will reduce the amount of toxins produced by the organisms.
- Do not hesitate to amputate if it is life-saving, because this is the only possible measure in late cases.
Summary
- Correct hypotension
- Control infection
- Treat dehydration
- Conduct operation
- Administer hyperbaric oxygen
- Give blood transfusion
- Passive immunisation
- To save lives, amputate
Type Of Gas Infections
- Clostridial cellulitis: In this condition, healthy muscle is not involved. It involves necrotic tissue and produces features of cellulitis such as tense, swollen parts with palpable crepitus. However, it is a mild infection, which can be managed by antibiotics without surgery.
- Local Type: It Refers To Infection Confined To A Single Muscle.
- Group type: It refers to infection confined to one group of muscles in the compartment. Such cases get benefits after a compartmental excision.
Infections By Clostridium Welchii
- Gas gangrene of the limb
- Gas gangrene of the abdominal wall
- Gangrenous appendicitis, cholangitis
- Necrotising enteritis, food poisoning
- Infection of the uterus following septic abortion
4. Massive type: Gas gangrene involving the entire limb, needs to be treated by amputation.


Leave a Reply