Drugs Used In Periodontal Therapy
Question 1. Write short note on local drug delivery system.
Or
Write short note on local drug delivery (LDD).
Or
Write short note on LDD.
Or
Write short answer on local drug delivery.
Answer. Local drug delivery systems are developed due to the limited efficacy of mouthrinsing and irrigation in deep pockets.
Main aim of the drug delivery system is to direct antimicrobials to the infection sites and maintaining effective level of drugs for sufficient period of time without producing any major side effects.
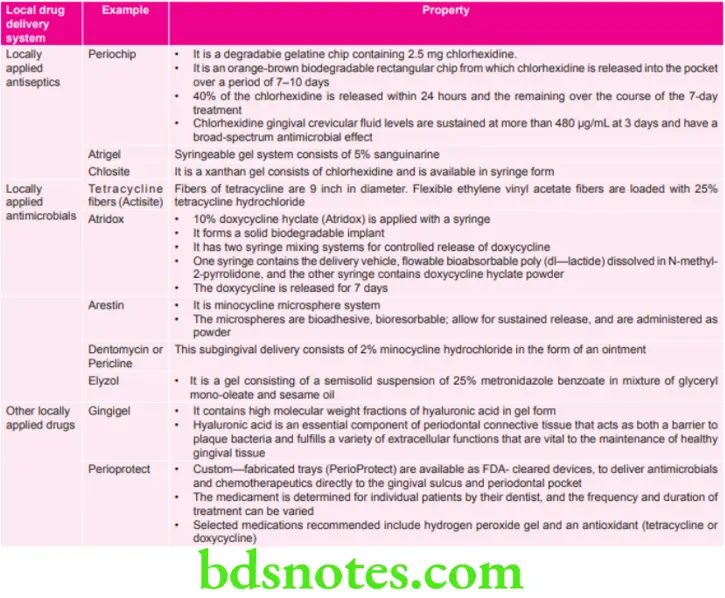
Various Local Drug Delivery Systems Used in Periodontics are:
Local Drug Delivery Indications
- As an adjunct in the treatment of few localized nonresponding sites in an otherwise controlled patient.
- In failing implant cases.
- In medically compromised patients in whom surgical procedures are not recommended.
- In cases with periodontal abscess.
- In cases with periodontal maintenance therapy.
- In patient with gastrointestinal intolerance to systemic drug medication.
Local Drug Delivery Contraindications
- Patients having history of allergy to any particular antimicrobial agent.
- During pregnancy and lactating periods.
- In the children under the age of 12 years.
- Subjects with complete renal failure.
- Subjects susceptible to infective endocarditis.
Local Drug Delivery Advantages
- Presence of high concentration of drug in subgingival sites.
- Patient compliance is absent.
- Does not affect symbiotic microflora of gastrointestinal tract.
- Systemic intolerance gets bypassed.
Local Drug Delivery Disadvantages
- It is difficult to place therapeutic concentrations of the antimicrobial agents in deeper areas.
- Professional application is mandatory, if used manually requires undergo dexterity and patient compliance.
- Complete drug penetration is impossible and extra pocket sites remain unaffected.
Read And Learn More: Periodontics Question And Answers
Question 2. Write short note on datun.
Answer. Datun is used by the people from the past when there were no synthetic toothpaste and toothbrushes.
- Usage of datun in the dentition is the exercise of the whole dentition.
- It increases the blood flow of the gums.
- Datun should be fresh and free of bacteria and other microorganisms.
- Datun can be made from following trees, i.e. Neem, babool, kher, mhaua, oak, imli, keekar, arjan, maulsiri, etc.
Dental Effects of Datun
- Datun of neem
- It is a powerful antiseptic
- Pyorrhea and tooth loss is prevented
- Teeth become strong and shining
- Beneficial in injuries and pus in gums.
- Datun of babool
- Stop bleeding gums
- Prevents shrinking of gums
- Makes grasp of gums on teeth better
- Prevent halitosis.
- Datun of khair
- Beneficial for swelling gums.
- Make teeth-immune to caries.
- Datun of karanz
- It is anti-bacterial
- Datun of keekar
- Antiseptic qualities
- Halitosis is destroyed
- Keeps teeth and gums healthy.
Question 3. Write short note on tetracycline in periodontics.
Answer. Tetracycline is widely used in treating periodontal disease.
- Tetracyclines are mainly used in treatment of refractory periodontitis including localized aggressive periodontitis.
- Tetracyclines have ability to concentrate in periodontal tissues and inhibit growth of A. actinomycetemcomitans. Tetracyclines exert an anticollagenase effect which inhibits tissue destruction and can aid in regeneration of bone.
Pharmacology
- Tetracyclines are bacteriostatic and are effective against rapid multiplying bacteria. They are more effective against gram-positive bacteria as compared to gram-negative bacteria.
- Concentration of tetracycline in gingival crevicular fluid is 2 to 10 times more than serum.
Tetracycline In Periodontics Clinical Use
- They are used as adjuncts in treatment of localized aggressive periodontitis.
- Systemic tetracycline eliminates tissue bacteria arrest bone loss and suppress growth of A. actinomycetemcomitans in combination with scaling and root planning.
- Tetracycline should be given 250 mg four times a day.
Properties of tetracycline which are to value in management of periodontal diseases are:
- Tetracycline and collagenase inhibition: These enzymes are derived from fibroblasts, epithelial cells, macrophages and neutrophils.
- Tetracycline and bone resorption: The antiproteolytic properties together with anticollagenase activity has been resulted in the use of these drugs to inhibit bone resorption.
- Anti-inflammatory effect of tetracycline: Potential antiinflammatory properties include the ability of tetracycline to suppress polymorphonuclear leukocyte activity.
- Tetracycline and fibroblast attachment: Pretreatment of dentin with tetracyclines enhances fibroblast attachment and colonization. The drug also enhances fibronectin binding.
- There effect is maximum in patient with localized juvenile periodontitis and refractory periodontitis.
Question 4. Write short note on antimicrobial agents in periodontal therapy.
Answer.
Classification of Antibiotics
According to the type of action, antibiotics are classified in the following ways:
- Bacteriostatic: For example, tetracyclines, sulfonamides, erythromycin, etc.
- Bactericidal: For example, penicillins, cephalosporins, etc.
Bacteriostatic antibiotics inhibit the growth and multiplication of microorganisms, whereas bactericidal antibiotics kill microorganisms.
Following are the antibiotics used commonly in the periodontal therapy:
- The drugs more extensively investigated for systemic use include tetracycline, minocycline and doxycycline, erythromycin, clindamycin, ampicillin, amoxicillin and the nitroimidazole compounds, metronidazole and ornidazole.
- The drugs investigated for local application include tetracycline, minocycline, doxycycline, metronidazole and chlorhexidine.
Penicillins
- Penicillins were the first group of antimicrobials used in periodontal therapy.
- Penicillins are bactericidal but induce allergic reactions.
Tetracyclines
- Tetracycline HCl became a popular choice during 1970s due to its broader spectrum of activity than penicillins, ability to inhibit collagenase activity, which is thought to interfere with the breakdown of periodontal tissues, firm adsorption to tooth surfaces and slow release over time.
- Most of subgingival microorganisms are susceptible to tetracyclines at a minimum inhibitory concentration of 1-2 mg/ mL.
Doxycyclines
- Doxycyclines are the semisynthetic tetracyclines.
- Doxycycline as compared to tetracyclines does not absorbed by calcium, milk and antacids and show better compliance.
- It is recommended in a 100 mg dosage twice daily for first day and then 100 mg four times a day.
Metronidazole
- Metronidazole is a powerful amebicide.
- The drug has selective antimicrobial features against the obligate anaerobes.
- It should be given 200 mg for four times a day for one week or 400 mg three times a day for one week.
- It is the first choice of drug to treat ANUG and aggressive periodontitis.
Azithromycin
- It is taken up by gingival epithelial cells and penetrates fibroblasts and phagocytes. It is transported and released directly into site of inflammation through phagocytosis.
- Its initial loading dose is 500 mg followed by 250 mg/day for 5 days.
Question 5. Write short note on metronidazole.
Answer. Metronidazole is a nitroimidazole compound.
- Metronidazole is used to treat protozoal infections.
- Metronidazole is bactericidal to anaerobic organisms.
Metronidazole Clinical Indications
- Metronidazole is not the drug for treating A. actinomycetemcomitans infections, but it can be effective at therapeutic levels due to its hydroxyl metabolite. So metronidazole when used in combination with other antibiotics, it becomes effective against A. actinomycetemcomitans.
- It is also effective against anaerobes such as Porphyromonas gingivalis and Prevotella intermedia.
- It has been used to treat gingivitis, ANUG, chronic periodontitis and aggressive periodontitis.
- Single dose of metronidazole (250 mg orally) appears in both serum and gingival crevicular fluid in sufficient quantities to inhibit a wide range of suspected periodontal pathogens.
- When metronidazole is administered systemically (750-1000 mg/ day for two weeks), it decreases the growth of anaerobic microorganisms, including spirochetes, and decreases the clinical as well as histopathological signs of periodontitis.
- Most common regimen for metronidazole is 250 mg three times daily for a week.
- It used as a supplement to rigorous scaling and root planning which result in a significantly reduced need for surgery compared with root planning alone.
Subgingival Metronidazole
- A topical medication containing an oil-based metronidazole 25% dental gel (glyceryl monooleate and sesame oil) has been tested in a number of studies.
- As a precursor, the preparation contains metronidazole benzoate, which is converted into the active substance by esterases in the gingival crevicular fluid.
- Two times the 25% gel applications at a one week interval have been used.
Side Effects of Metronidazole
- The drug has an anti-abuse effect when alcohol is ingested, resulting in severe cramps, nausea and vomiting. Hence, products containing alcohol should be avoided at the time of metronidazole therapy and for at least 1 day after therapy is discontinued.
- Metronidazole inhibits warfarin metabolism.
- Patients undergoing anticoagulant therapy should avoid metronidazole as it prolongs prothrombin time.
- It also should be avoided in patients who are taking lithium.
Question 6. What are the guidelines for use of antibiotics in periodontal therapy? Describe various types of antibiotics in detail used in treatment of periodontal diseases.
Answer. Following are the guidelines for use of antibiotics in periodontal therapy:
- The clinical diagnosis and situation dictate the need for possible antibiotic therapy as an adjunct in controlling active periodontal disease. The patient’s diagnosis can change over time.
- Continuing disease activity, as measured by continuing attachment loss, purulent exudate, and continuing periodontal pockets of 5 mm or greater that bleed on probing, is an indication for periodontal intervention and possible microbial analysis through plaque sampling. Also cases of refractory or aggressive periodontitis may indicate the need for antimicrobial therapy.
- When used to treat periodontal disease, antibiotics are selected based on the patient’s medical and dental status. Current medications and results of microbial analysis, if performed.
- Microbiologic plaque sampling may be performed according to the instructions of the reference laboratory. The samples usually are taken at the beginning of an appointment before instrumentation of the pocket. Supragingival plaque is removed, and an endodontic paper point is inserted subgingivally into the deepest pockets present to absorb bacteria in the loosely associated plaque. This endodontic point is placed in reduced transfer fluid and sent overnight to the laboratory. The laboratory will then send the referring dentist a report that includes the pathogens present and any appropriate antibiotic regimen.
- Plaque sampling can be performed at the initial examination, root planning, reevaluation, or supportive periodontal therapy appointment. Clinical indications for microbial plaque testing include aggressive forms of periodontal disease, diseases refractory to standard mechanical therapy, and periodontitis associated with systemic conditions.
- Antibiotics have also been shown to have value in reducing the need for periodontal surgery in patients with chronic periodontitis.
- Some studies have shown attachment gain with antibiotics given as monotherapy. However, the evidence is insufficient at present to recommend systemic antimicrobial therapy as monotherapy. Therefore, systemic antimicrobial therapy should be an adjunct to a comprehensive periodontal treatment plan. Debridement of root surfaces, optimal oral hygiene, and frequent supportive periodontal therapy are important parts of comprehensive periodontal therapy. Chemotherapeutic adjuncts include locally placed subgingival anti-infective agents, chlorhexidine rinse after debridement, and home intraoral irrigation with or without chemotherapeutic agents. Chlorhexidine gluconate is effective as an antiplaque rinse to reduce gingivitis but not as a subgingival irrigant to reduce periodontal pocketing. Chlorhexidine gluconate anti-infective activity is greatly reduced in the presence of organic matter in the subgingival periodontal pocket. Some evidence suggest that povidone-iodine (Betadine) may be an effective antibacterial agent when used directly into the periodontal pocket, even at low concentrations, but further studies are needed to substantiate these data. Povidone-iodine must be used with caution in patients sensitive to iodine, although the sensitization rate is low. It also should be used with caution in patients who are pregnant or lactating.
- Slots et al. described a series of steps using antiinfective agents for enhancing regenerative healing. They recommend starting antibiotics 1 to 2 days before surgery and continuing for a total of at least 8 days. However, the value of this regimen has not been well documented, and further studies are encouraged.
- Using evidence-based techniques, meta-analysis has shown statistically significant improvements in attachment loss when tetracycline and metronidazole are used as adjuncts to scaling and root planning.
Antibiotics in Treatment of Periodontal Diseases
Following are the antibiotics are used commonly in the periodontal diseases:
- The drugs more extensively investigated for systemic use include tetracycline, minocycline and doxycycline, erythromycin, clindamycin, ampicillin, amoxicillin and the nitroimidazole compounds, metronidazole and ornidazole.
- The drugs investigated for local application include tetracycline, minocycline, doxycycline, metronidazole and chlorhexidine.
Penicillins
- Penicillins were the first group of antimicrobials used in periodontal therapy.
- Penicillins are bactericidal but induce allergic reactions.
Tetracyclines
- Tetracycline HCl became a popular choice during 1970s due to its broader spectrum of activity than penicillins, ability to inhibit collagenase activity, which is thought to interfere with the breakdown of periodontal tissues, firm adsorption to tooth surfaces and slow release over time.
- Most of subgingival microorganisms are susceptible to tetracyclines at a minimum inhibitory concentration of 1-2 mg/ mL.
Doxycyclines
- Doxycyclines are the semisynthetic tetracyclines.
- Doxycycline as compared to tetracyclines does not absorbed by calcium, milk and antacids and show better compliance.
- It is recommended in a 100 mg dosage twice daily for first day and then 100 mg four times a day.
Metronidazole
- Metronidazole is a powerful amebicide.
- The drug has selective antimicrobial features against the obligate anaerobes.
- It should be given 200 mg for four times a day for one week or 400 mg three times a day for one week.
- It is the first choice of drug to treat ANUG and aggressive periodontitis.
Azithromycin
- It is taken up by gingival epithelial cells and penetrates fibroblasts and phagocytes. It is transported and released directly into site of inflammation through phagocytosis.
- Its initial loading dose is 500 mg followed by 250 mg/day for 5 days.
Question 7. Write short note on subantimicrobial dose of doxycycline.
Or
Write short note on SDD.
Answer. Subantimicrobial-Dose doxycycline (SDD) is a 20-mg dose of doxycycline (Periostat) that is approved and indicated as an adjunct to scaling and root planning in the treatment of chronic periodontitis.
- It is taken twice daily for 3 months, up to a maximum of 9 months of continuous dosing.
- The 20 mg dose exerts its therapeutic effect by enzyme, cytokine and osteoclast inhibition rather than by any antibiotic effect.
- Subantimicrobial dose doxycycline may help to prevent the destruction of periodontal attachment by controlling the activation of matrix metalloproteinases, primary collagenase and gelatins, from both infiltrating cells and resident cells of periodontium, primary neutrophils.
- Subantimicrobial dose doxycycline consisting of doxycycline cyclate 20 mg two times a day provide significant additional benefit to scaling and root planning in the treatment of periodontitis. At this dosage benefits obtained are derived from anti-collagenase and antiinflammatory property of doxycyline.
- Research studies have found no detectable antimicrobial effect on the oral flora or the bacterial flora and other regions of the body and have identified clinical benefit when used as an adjunct to scaling and root planning.
- At present, SDD is the only host modulation therapy specifically indicated for the treatment of chronic periodontitis.
Question 8. Write short note on saliva substitutes.
Answer. Saliva substitutes, which are intended to match the chemical and physical traits of saliva, are available to relieve the symptoms of dry mouth.
- Their composition is varied; however, they usually contain salt ions, a flavoring agent, paraben (preservative), cellulose derivative or animal mucins, and fluoride.
- Most saliva substitutes can be used as desired by patients and are dispensed in spray bottle, rinse/swish bottle, or oral swab stick. In addition, products such as dry-mouth toothpastes and moisturizing gels are also available.
- Biotene products are marketed to relieve the symptoms of Xerostomia.
- Patients with dry mouth may also benefit by stimulating saliva flow with sugarless candies and sugarless gum.
- Xylitol chewing gum has been shown to have anticariogenic properties in children.
- Medicated chewing gum with xylitol and chlorhexidine or Xylitol alone has the added benefits of reducing oral plaque scores and gingivitis in elderly persons who live in residential facilities.
- Salivary substitutes and stimulants are only effective in the short-term.
Question 9. Write short note on drugs used in treatment of periodontal diseases.
Answer. Drugs used in periodontal therapy are
- Antiplaque and anticalculus agents
- Antibiotics used to treat periodontal diseases
- Anti-inflammatory drugs.
Classification of Drugs Depending on AntimicrobialEfficacy and Substantivity
- First generation agents: Reduce plaque score by 20 to 50%, efficacy is limited due to poor substantivity. For example, quaternary ammonium compounds and antibiotics.
- Second generation agents: Retained longer in tissues and their slow release property provide overall reduction in plaque score up to 79–90%. For example, chlorhexidine, triclosan.
- Third generation agents: Effective against specific periodontopathic organisms. For example, delmopinol.
Drugs for Supragingival Plaque Control
- Phenol: They have non-specific antibacterial action which depends on ability of the drug to penetrate its lipid content of cell wall of gram-negative organism.
- Quaternary ammonium compounds: Quaternary ammonium compounds are cationic antiseptics and surface-active agents. Quaternary ammonium compounds tend to be more effective against gram-positive than gram-negative organisms. This may suggest that these compounds are most effective as antiplaque agents when used against early developing plaque, which predominantly contains gram-positive bacteria.
Quaternary ammonium compounds include:
- Benzethonium chloride.
- Benzalkonium chloride.
- Cetylpyridinium chloride—CPC.
- Domiphen bromide.
Mechanism of Action
They have some similarities in their mechanism of action to chlorhexidine; the molecules possess both hydrophobic and hydrophilic groups allowing for ionic and hydrophobic interactions. It is assumed that the interaction with bacteria occurs with cationic binding, to the phosphate groups in the cell wall, teichoic acid in the gram-positive bacteria and to the phosphate groups of the cell wall and in general to the membrane lipopolysaccharide of gram-negative bacteria.
The membrane integrity may subsequently be disrupted by interaction with the lipophilic portion of the molecule, causing disturbance of membrane functions and leakage of cytoplasmic material.
Antibiotics in Periodontal Therapy
Following are the antibiotics are used commonly in the periodontal therapy:
- The drugs more extensively investigated for systemic use include tetracycline, minocycline and doxycycline, erythromycin, clindamycin, ampicillin, amoxicillin and the nitroimidazole compounds, metronidazole and ornidazole.
The drugs investigated for local application include tetracycline, minocycline, doxycycline, metronidazole and chlorhexidine.
Penicillins
- The penicillins were the first group of antimicrobials used in periodontal therapy.
- Penicillins are bactericidal but induce allergic reactions.
Tetracyclines
- Tetracycline HCl became a popular choice during 1970s due to its broader spectrum of activity than penicillins, ability to inhibit collagenase activity, which is thought to interfere with the breakdown of periodontal tissues, firm adsorption to tooth surfaces and slow release over time.
- Most of subgingival microorganisms are susceptible to tetracyclines at a minimum inhibitory concentration of 1-2 mg/ mL.
Doxycyclines
- Doxycyclines are the semisynthetic tetracyclines.
- Doxycycline as compared to tetracyclines does not absorbed by calcium, milk and antacids and show better compliance.
- It is recommended in a 100 mg dosage twice daily for first day and then 100 mg four times a day.
Metronidazole
- Metronidazole is a powerful amoebicide.
- The drug has selective antimicrobial features against the obligate anaerobes.
- It should be given 200 mg for four times a day for one week or 400mg three times a day for one week.
- It is the first choice of drug to treat ANUG and aggressive periodontitis.
Azithromycin
- It is taken up by gingival epithelial cells and penetrates fibroblasts and phagocytes. It is transported and released directly into site of inflammation through phagocytosis.
- Its initial loading dose is 500 mg followed by 250 mg/day for 5 days.
Chlorhexidine
It has most positive antibacterial result.
Two daily rinses with 10 mL of 0.2% aqueous solution of chlorhexidine digluconate almost completely inhibited the development of dental plaque, calculus and gingivitis.
Periodontal Diseases Disadvantages
- Locally reversible side effects to chlorhexidine use may occur, primarily brown staining of the teeth, tongue and silicate as well as resin restorations.
- Transient impairment of taste perception
- Painful, desquamative lesions on the oral mucosa may be associated with burning sensation.
Mechanism of Action
It has a broad spectrum of antibacterial activity.
- Gram-positive bacteria are more susceptible than gramnegative.
- In relatively high concentration it is bacteriocidal but in low concentration it may be bacteriostatic.
- Cationic molecules of chlorhexidine bind readily to the oppositely charged cell wall and interfere with the membrane transport initiating a leakage of low molecular weight substances.
- In high concentration chlorhexidine penetrates the cell and causes precipitation of cytoplasm (Bactericidal action).
Triclosan
- Triclosan is a phenol derivative, it is synthetic and is nonionic.
- It has a broad spectrum of activity against gram positive and gram negative bacteria.
Mechanism of Action
- It acts over the microbial cytoplasmic membrane and it induces leakage of cellular constituents and leads to bacteriolysis.
- It also delays plaque maturation and inhibit formation of prostaglandin and leukotrienes which are the mediators of inflammation.
Metallic Ions
Salts of zinc and copper are most commonly used metal ions.
Mechanism of Action
They reduce glycolytic activity in microorganisms and inhibit bacterial as well as crystal growth.
Sanguinarine
- It is effective against wide variety of gram-negative microorganisms.
- It undergoes retention with plaque when used as mouthwash.
Enzymes
- These are mucinase, dehydrated pancreas, dextranase and thiocynate synthetase.
- Various proteolytic enzymes are bactericidal and are effective when applied in the mouth.
- Enzymes act as active agents and they breakdown already formed matrix of plaque and calculus.
Povidone Iodine
- It does not show significant plaque inhibition activity when used as 1% mouthwash.
- Various studies show that it reduces inflammation and progression of periodontal disease.
Delmopinol
- It is a low molecular weight amino alcohol.
- Inhibit growth of plaque and reduce the chances of gingivitis.
Mechanism of Action
- It target dextran in extracellular matrix by blocking the synthesis, reducing the viscosity and selectively inhibiting dextran producing streptococci.
- It also undergoes interference with plaque matrix formation and reduces bacterial adherence. It causes weak binding of plaque to tooth surface and aid in easy removal of plaque.

Leave a Reply