Staphylococcus
Question 1. Write a short note on staphylococcus.
Or
Write notes on staphylococci.
Or
Write briefly on laboratory identification of staphylococci.
Answer:
Staphylococcus are gram-positive cocci which occur in grapes-like cluster. Sir Alexander Ogston in 1880 discover Staphylococci.
Morphology of Staphylococcus
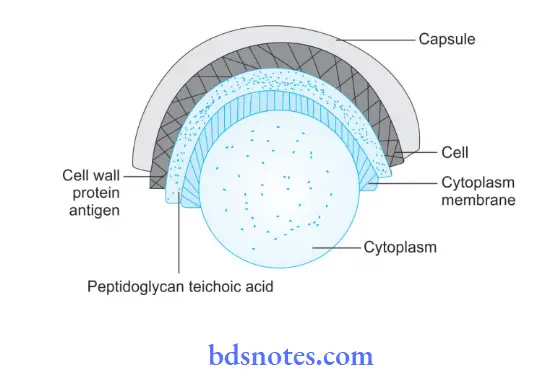
Spherical cocci are arranged characteristically in grapes-like cluster. Staphylococcus are non-motile and non-sporing. A few strains possess visible capsules, else they are noncapsulated. Stain readily with aniline dyes are uniformly gram-positive and about 1 m in diameter.
Read And Learn More: Microbiology Question And Answers
Types of Staphylococcus
Staphylococci contain multiple species but species of medical importance are as follows:
- Staphylococcus aureus: It is a pathogenic staphylococcus which leads to suppurative infections in man.
- Staphylococcus epidermidis: It leads to skin infections.
- Staphylococcus saprophyticus: It is an opportunistic pathogen.
Cultural Characteristics
Aerobes and facultative anaerobes: Optimum pH is 7.4–7.6. The optimum temperature is 37°C.
- Colony characteristics in different media are:
- Nutrient Agar: Smooth, shiny convex, opaque, golden yellow some may be white, orange, or yellow. They are large and 2 to 4 mm in diameter especially on sheep and rabbit blood agar
- Nutrient Agar Slope: Oil paint appearance.
- Blood Agar: Produces β type of hemolysis.
- Mac-Conkey medium: Small lactose-forming colonies (pink).
- Selective media: Various selective media are used for isolating S. aureus from different specimens. Selective media are:
- Salt milk agar or salt broth
- Ludlam’s medium: It has lithium chloride and tellurite
- Mannitol salt agar: Acts as both selective and indicator media. Mannitol-fermented staphylococcal colonies are surrounded by a yellow zone.
- Polymyxin agar: It is the selective media that favor the growth of coagulase-positive S. aureus.
Laboratory Diagnosis of Staphylococcus Aureus
Specimen collected is pus, sputum, blood, urine, CSF, feces, and vomit.
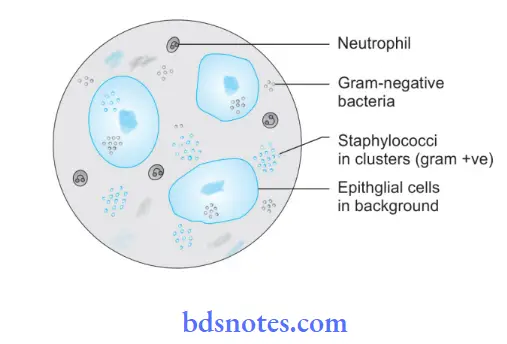
- Microscopy: Gram-stained smears of pus or wound exudate is useful. Gram-positive cocci in the cluster are seen. On Gram staining, gram-positive cocci are arranged in grape-like clusters. Non-motile cocci in clusters are seen in hanging drop preparation.
- Culture: Specimens are inoculated on blood agar and peptone water. Specimens, where staphylococci are expected to be scanty or outnumbered by other bacteria, are inoculated in selective media such as salt agar, salt milk agar, and Robertson’s cooked meat medium. Inoculated media is incubated at 37°C for 18-24 hours. The next day culture plates are examined for the morphology of bacterial colonies. Uniform turbidity is produced on peptone water.
- Biochemical Reactions:
- Catalase test: All staphylococci are catalase positive.
- Coagulase test: Positive in S. aureus but negative in other staphylococcal species.
- Mannitol fermentation: There is the production of acid without gas.
- Gelatin liquefication is positive.
- Tellurite reduction is positive.
- Bacteriophage Typing: It is done to ascertain epidemiological purposes to trace the source of S. aureus infection. Other typing methods are antibiogram pattern, plasmid typing, ribotyping, and DNA fingerprinting.
Question 2. Draw a labeled diagram of Staphylococcus
Answer:
Question 3. Enumerate suppurative diseases caused by Staphylococcus aureus. How will you identify this organism in the laboratory?
Or
Enumerate suppurative diseases caused by Staphylococcus aureus. Describe laboratory diagnosis of this organism.
Answer:
Enumeration of suppurative diseases caused by Staphylococcus aureus:
- Skin and soft tissue infections:
- Impetigo
- Folliculitis
- Furuncle
- Carbuncle
- Staphylococcal scalded skin syndrome
- Hidredenitits suppurativa
- Mastitis.
- Organ infection and disseminated infections:
- Pneumonia
- Endocarditis
- Suppurative osteomyelitis.
For identification of Staphylococcus aureus in the laboratory:
Laboratory Diagnosis of Staphylococcus Aureus
Specimen collected is pus, sputum, blood, urine, CSF, feces, and vomit.
- Microscopy: Gram-stained smears of pus or wound exudate is useful. Gram-positive cocci in a cluster is seen. On Gram staining, gram-positive cocci are arranged in grape-like clusters. Non-motile cocci in clusters are seen in hanging drop preparation.
- Culture: Specimens are inoculated on blood agar and peptone water. Specimens, where staphylococci are expected to be scanty or outnumbered by other bacteria, are inoculated in selective media such as salt agar, salt milk agar, and Robertson’s cooked meat medium. Inoculated media is incubated at 37°C for 18-24 hours. The next day culture plates are examined for the morphology of bacterial colonies. Uniform turbidity is produced on peptone water.
- Biochemical Reactions:
- Catalase test: All staphylococci are catalase positive.
- Coagulase test: Positive in S. aureus but negative in other staphylococcal species.
- Mannitol fermentation: There is the production of acid without gas.
- Gelatin liquefaction is positive.
- Tellurite reduction is positive.
- Bacteriophage Typing: It is done to ascertain epidemiological purposes to trace the source of S. aureus infection. Other typing methods are antibiogram pattern, plasmid typing, ribotyping, and DNA fingerprinting.
Question 4. Write a short note on coagulase test—procedure and precaution.
Or
Write short note on the coagulase test.
Answer:
- The coagulase test is carried out by slide and tube methods.
- Coagulase test is done to differentiate pathogenic S. aureus from non-pathogenic strain.
Principle: To determine the ability of Staphylococcus aureus to produce an enzyme coagulase which is responsible for clotting of human or rabbit plasma.
Slide Coagulase Test: It detects clumping factors.
- Procedure:
- Some of the colonies of bacteria should be emulsified by adding a drop of normal saline over a clean glass slide.
- These are now mixed with drops of undiluted rabbit or human plasma.
- If coagulase strains are present clumping of suspension occurs which is indicative of a positive test.
- Precautions:
- False positive results are seen in cases of citrate-utilizing bacteria.
- Some of the strains which are negative for bound coagulase but are positive for free coagulase give false negative results.
Tube Coagulase Test: It detects real coagulase.
- Procedure:
- 0.1 mL of an overnight broth culture or an agar culture suspension of an organism is mixed with 0.5 mL of 1:5 dilution of human or rabbit plasma.
- Diluted plasma in the second tube act as a control.
- Tubes should be incubated in a water bath at 37°C for 4 to 6 hours.
- If the result comes positive clotting of plasma occurs and it does not flow if tube is inverted.
- If clotting does not occur, it should be left for overnight and is re-examined.
- Precautions:
- The use of citrated plasma should be avoided since this can lead to false positive results.
Mechanism
Staphylococcus aureus produces an enzyme coagulase which acts along with the coagulase reacting factor present in human or rabbit plasma and binds to prothrombin and converts fibrinogen to fibrin which results in clotting
Examples of positive and negative bacteria
- Coagulase positive: Staphylococcus aureus
- Coagulase-negative: Staphylococcus albus, Staphylococcus citrus, and all other bacteria

Leave a Reply