Shock
Question.1.Discuss shock.
Or
Discuss briefly shock.
Or
What is shock? Describe its classification, causes, clinical features, and management.
Or
Write on classification, causes, clinical features, and management of shock.
Answer. Shock is defined as an acute clinical syndrome characterized by a significant, systemic reduction in tissue perfusion, resulting in decreased tissue oxygen delivery and insufficient removal of cellular metabolic products, resulting in tissue injury and severe dysfunction of vital organs.
Read And Learn More: General Surgery Question And Answers
Classification of Shock
Following is the classification of shock:
- Hypovolemic shock
- Cardiogenic shock
- Distributive shock:
- Septic shock
- Anaphylactic shock
- Neurogenic shock
Obstructive shock.
Hypovolemic Shock
- Hypovolemic shock occurs due to loss of blood plasma or body flid and electrolytes, usually caused by massive hemorrhage, vomiting, diarrhea, and dehydration.
- Hypovolemic shock is the most common type of shock which is characterized by a loss in circulatory volume,which leads to decreased venous return, decreased filing of the cardiac chambers, and so there is decrease in cardiac output which leads to increase in the systemic vascular resistance.
Cardiogenic Shock
- Cardiogenic shock occurs due to the dysfunction of one ventricle or other.
- This type of shock is seen in myocardial infarction, chronic congestive cardiac failure, cardiac arrhythmias, pulmonary embolism, etc.
resulting in inability of the heart to pump the adequate amount of blood into the lungs and decreased
cardiac output. - Myocardial infarction is the most common cause of cardiogenic shock.
Distributive Shock
Distributive shock occurs when the afterload is excessively reduced due to extensive vasodilatation and is associated not
only with poor vascular tone in the peripheral circulation but maldistribution of blood flow to organs within the body also.
- Septic shock: This type of shock is mostly due to release of endotoxins in blood, which causes wide spread vasodilation of blood vessels resulting in fall in the cardiac output.
Bacteria responsible for release of endotoxins are E. coli, Pseudomonas proteus, etc. It is most common shock among
all the distributive shocks. - Neurogenic shock: This type of distributive shock is caused by the suppression or loss of sympathetic tone caused any disruption of the sympathetic nervous system like spinal injury, spinal anesthesia, and drugs.
- Anaphylactic shock: This type of shock is a result of type I hypersensitivity reaction and is caused when the body’s antibody-antigen response is triggered by something the person is allergic to drugs, like penicillin, cephalosporins, iodinated contrast media, serum, etc., are common causes of this type of shock.
Obstructive Shock
- This type of shock is associated with physical obstruction of the great vessels or the heart itself.
- Most commonly obstructive shock is due to cardiac tamponade, due to tension pneumothorax and pulmonary embolus.
Causes of Shock
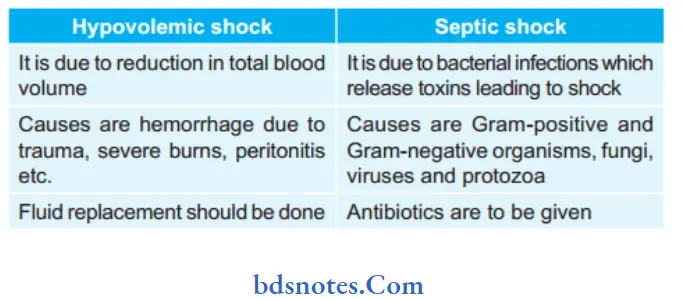
Hypovolemic shock—due to reduction in total blood volume.
It may be due to:
- Hemorrhage:
- External from wounds, open fractures
- Internal from injury to spleen, liver, mesentery or pelvis.
- Severe burns, which results in loss of plasma
- Peritonitis, intestinal obstruction
- Vomiting and diarrhea of any cause
Shock Cardiac causes:
- Acute myocardial infarction, acute carditis
- Acute pulmonary embolism wherein embolus blocks the pulmonary artery at bifurcation or one of the major branches
- Drug-induced
- Toxemia of any causes
- Cardiac surgical conditions like valvular diseases,congenital heart diseases
- Cardiac compression causes:
- Cardiac tamponade due to collection of blood,pus, flid in the pericardial space which prevents the heart to expand leading to shock.
- Trauma to heart.
- Septic shock—is due to bacterial infections which release toxins leading to shock.
- Neurogenic shock—due to sudden anxious or painful stimuli causing severe splanchnic vessel vasodilatation.
Here patient either goes for cardiac arrest and dies or recovers fully spontaneously—spinal cord injury/ anaesthesia
can cause neurogenic shock. - Anaphylactic shock—is due to type I hypersensitivity reaction
Shock Respiratory causes:
- Atelectasis (collapse) of lung
- Thoracic injuries
- Tension pneumothorax
- Anesthetic complications.
Shock Other causes:
- Acute adrenal insufficiency (Addison’s disease)
- Myxedema.
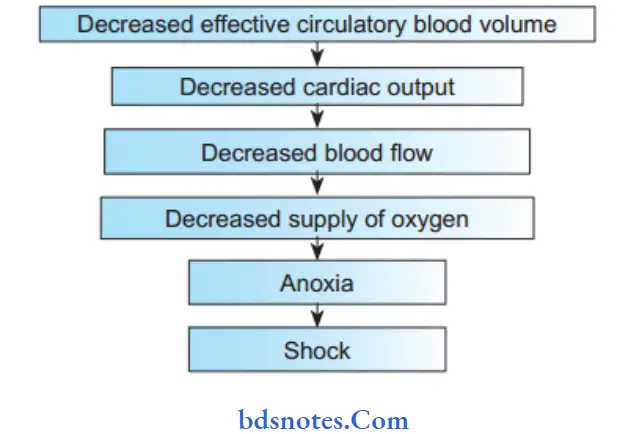
Pathophysiology of Shock
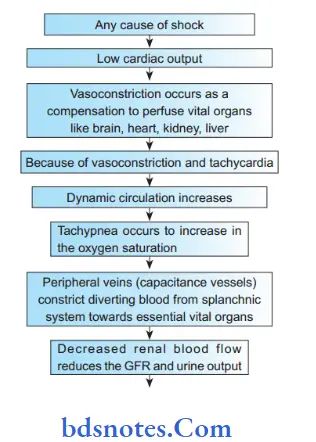

Stages of Shock
Stage l: Stage of compensatory shock—by neuroendocrine response to maintain the perfusion of the vital organs like brain, heart, kidney, liver.
Stage 2: Stage of decompensatory shock—where there is progressive shock causing persistent shock with severe hypotension (with mean arterial pressure <65 mm Hg); oliguria, tachycardia.
Stage 3: Stage of irreversible shock – with severe hypoxia and Multi-organ dysfunction syndrome (MODS).
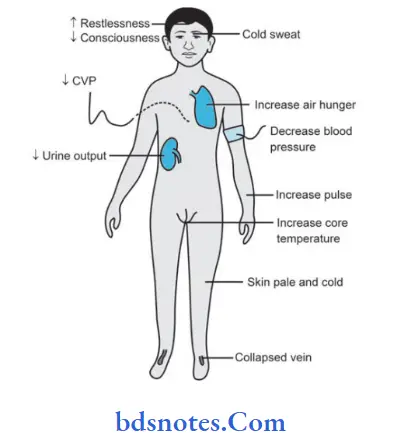
Clinical Features of Shock
- Presence of anxiety, restlessness, altered mental state due to decreased cerebral perfusion and subsequent hypoxia.
- Hypotension because of decrease in circulatory volume.
- Due to decreased blood flw there is tachycardia and weak thready pulse.
- Cold and clammy skin due to vasoconstriction and stimulation of vasoconstriction.
- Rapid and shallow respirations (tachypnea) due to sympathetic nervous system stimulation and acidosis.
- Hypothermia due to decreased perfusion and evaporation of sweat.
- Thirst and dry mouth due to flid depletion.
- Fatigue due to inadequate oxygenation.
- Cold and motted skin, especially extremities, due to insuffiient perfusion of the skin.
- Pallor is present
- Fainting
- Oliguria/anuria due to decreased renal perfusion and afferent arteriolar vasoconstriction.
Investigations and Monitoring of Shock
- Regular monitoring with blood pressure, pulse, heart rate, respiratory rate, urine output measurement (hourly) should be done.
Urine output should be more than 0.5 ml/kg/hour.
Pulse oximetry should be used. - Central venous pressure (CVP), pulmonary capillary wedge pressure (PCWP—an accurate assessment of left ventricular/function) monitoring should be done.
ICU care is needed during monitor period.
But both CVP and PCWP are not accurate method of assessing tissue perfusion. - Complete blood count, ESR, pH assessment, serum electrolyte estimation, chest X-ray (to rule out acute respiratory distress syndrome/pulmonary problems).
- Pus/urine/blood/bile/sputum cultures depending on the focus and need in sepsis.
- Serum lactate estimation is an important prognostic factor.
Level >2 mEq/L suggest tissue ischemia. - USG of a part, CT/MRI of the location of pathology of standard focus should be done; often may require repetition of this imaging to assess progress.
- Blood urea, serum creatinine, liver function tests, prothrombin time (PT), activated partial thromboplastin time (APTT), ECG monitoring are also should be done.
- All these tests including platelet count and arterial blood gas (ABG) should be repeated at regular intervals.
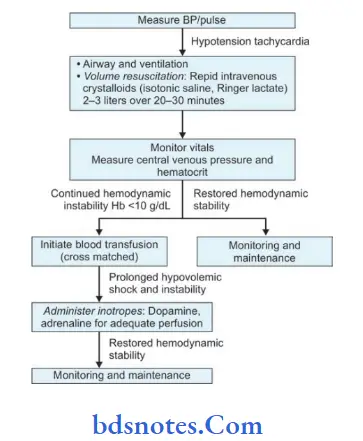
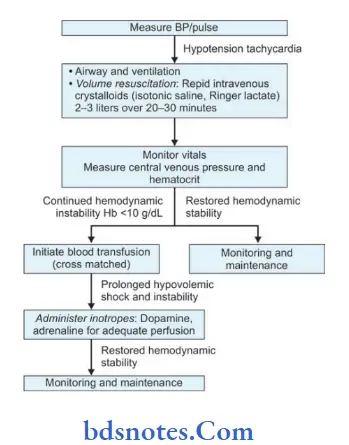
Treatment Of Shock
- Treat the cause, e.g. arrest hemorrhage, drain pus.
- Fluid replacement: Plasma, normal saline, dextrose, Ringer’s lactate, plasma expander (haemaccel).
Dosage is maximum l liter can be given in 24 hours.
Initially crystalloids then colloids are given.
Blood transfusion is done whenever required. - Ionotropic agents: Dopamine, dobutamine, adrenaline infusions—mainly in distributive shock like septic shock.
- Correction of acid-base balance: Acidosis is corrected by using 8.4% sodium bicarbonate intravenously.
- Steroid is often lifesaving. 500–l000 mg of hydrocortisone can be given. It improves the perfusion, reduces the capil- lary leakage and systemic inflammatory effects.
- Antibiotics in patients with sepsis; proper control of blood sugar and ketosis in diabetic patients.
- Catheterization to measure urine output (30–50 mL/hour or > 0.5 mL/kg/hour should be maintained).
- Nasal oxygen to improve oxygenation or ventilator support with intensive care unit monitoring has to be done.
- Central venous pressure line to perfuse adequately and to monitor flid balance. Total parentral nutrition is given
when required. - Pulmonary capillary wedge pressure to monitor very critical patient.
- Hemodialysis may be necessary when kidneys are not functioning.
- Control pain—using morphine (4 mg IV).
- Ventilator and ICU/critical care management.
- Injection ranitidine IV or omeprazole IV or pantoprazole IV.
- Activated protein even though costly is beneficial as it prevents the release and action of inflammatory response.
- MAST(MilitaryAnti-shock Trouser) provides circumferential external pressure of 40 mm Hg.
lt is wrapped around lower limbs and abdomen, and inflted with required pressure. It redistributes the existing blood and flid towards center.
It should be deflted carefully and gradually.
Question.2. Describe briefly hypovolemic shock.
Or
Describe clinical feature and management of hypovolemic shock.
Or
Write a short note on hypovolemic shock.
Answer.
It occurs due to loss of blood plasma or body fluid and electrolytes, usually caused by massive hemorrhage, vomiting,diarrhea and dehydration.
Hypovolemic shock is most common type of shock which is characterized by loss in circulatory volume which leads to decrease in venous return, decrease in filing of cardiac chambers, so there is decreased cardiac output which causes increase in systemic vascular resistance.
Types Of Hypovolemia
- Covert-compensated hypovolemia (Mild <15%): When blood volume is reduced by 10–15%, there will not be signifiant change in heart rate, cardiac output and splanchnic blood compensates for the same.
- Overt compensated hypovolemia (Moderate 15–40%): Here patient has cold periphery, tachycardia, a wide arterial pressure, tachypnea, confusion, hyponatremia, metabolic acidosis, but systolic pressure is well—maintained but postural hypotension.
- Decompensated hypovolemia (Severe >40%): Here all features of hypovolemia are present like hypotension, tachycardia, sweating, tachypnea, oliguria, drowsiness, and eventually features of systemic inflammatory response syndrome is seen, and often if not treated on time leads to multiorgan dysfunction syndrome, i.e. irreversible shock
Hypovolemic Shock Causes
Loss of extracellular fluid:
- Deviation of normal exchange pattrn: As in vomiting,diarrhea, intestinal obstruction, peritonitis, and acute pancreatitis.
- Increased sweating without replacement in a non acclimatized individual.
- Third space shift to sodium from extracellular to intracellular compartment due to failure of sodium pump caused by hypoxia.
Plasma loss: Due to burn.
Hemorrhage: Due to whole blood loss like.
- Surgical: During and following any major surgery especially cardiopulmonary bypass, pelvic surgery or major abdominal surgery.
- Traumatic: As a result of any type of major accident, warfare injuries, homicidal or following suicidal injury as by knife, bullet, etc.
- GI bleeding: Bleeding from peptic ulcer, perforation of intestine, bleeding from esophageal varices, etc.
- Obstructive bleeding: Incomplete abortion, placenta previa, etc.
Hypovolemic Shock Clinical Features
- Anxiety, restless, excitation and disorientation.
- Pallor
- Thirst and hunger
- Cold and clammy skin
- Faint in upright position
- Tachycardia with rapid, thready pulse
- Hypotension
- Oligouria or anuria.
Hypovolemic Shock Management
Question.3. Enumerate different types of shock and discuss management of hypovolemic shock.
Answer.
Hypovolemic Shock Enumeration of types of Shock
- Vasovagal shock
- Neurogenic shock
- Hypovolemic shock
- Cardiogenic shock
- Cardiac compression shock
- Septic shock
- Anaphylactic shock.
Question.4. Write short note on vasovagal shock.
Answer.
- This is a response to sudden fear or severe pain and the effects from slight fainting fi to death.
- This type of shock is also known as neurogenic or psychogenic shock.
- There is sudden pooling of blood in the capacitance vessels of legs and splanchnic arterial bed.
This causes reduced cardiac output and shock. It can be life-threatening due to hypoxia.
Vasovagal Shock Pathophysiology
- Nucleus tractus solitarius of the brainstem is activated directly or indirectly by the triggering stimulus.
- Simultaneous enhancement of parasympathetic nervous system, i.e. vagal tone and withdrawal of sympathetic nervous system tone, which causes either cardioinhibitory response or vasodepressor response
- The cardioinhibitory response is characterized by a drop in heart rate, i.e. negative chronotropic effct and in contrac-
tility, i.e. negative ianotropic effct which causes decrease in cardiac output. - Unconsciousness or vasodepressor response is caused by a drop in blood pressure as low as 80/20 without much change in heart rate.
Vasovagal Shock Clinical Features
- History of emotional stress or pain of a sudden nature.
- Bradycardia or pallor.
- Tachypnea
- Fainting
- Reflexes are usually intact.
Vasovagal Shock Management
- Place the patient flt or in head low position.
- Ensure potency of airway
- IV atropine may be needed for persistent or increasing
bradycardia.
Question.5. Describe briefl anaphylactic shock.
Answer. This type of shock is a result of type I hypersensitivity reaction.
- Anaphylactic shock can occur when a previously sensitized individual is exposed to a specifi antigen, IV. Drugs, especially penicillin, cephalosporins, and iodinated contrast media are common offenders.
Anaphylactic shock Pathophysiology
Injections—penicillins, anesthetics, stings, venom, shellfih may be having antigens which will combine with IgE of mast
cells and basophils, releasing histamine and large amount of SRS—A (Slow releasing substance of anaphylaxis). They cause bronchospasm, laryngeal edema, respiratory distress, hypotension and shock. Mortality is 10%.
Anaphylactic shock Clinical Features
- Due to reduced cerebral perfusion, there is change in mental status.
- Due to reduced preload and cardiac contractility, there is hypotension.
- Due to release of histamine and other chemical mediators there is urticaria.
- Due to hypoxia the cyanosis is caused.
- Due to anaerobic metabolism and hepatic dysfunction the lactic acidosis is caused.
- Due to coronary ischemia other dysrhythmias are caused.
Anaphylactic shock Treatment
- Summon ambulance
- Always check whether respiratory distress is due to other causes.
- Assess the degree of cardiovascular collapse by checking pulse and blood pressure.
- Assess the degree of airway obstruction
- Stop administration of drug
- Patient should be kept supine
- Assess breathing diffilty by checking for stridor, wheeze
- Administer oxygen to patient by face mask
- Give antihistamine chlorpheniramine maleate 10 mg
- Administer hydrocortisone 20 mg
- Monitor consciousness, airway, breathing, circulation,
pulse, blood pressure - Raise legs if blood pressure is low
- Adrenaline 1:1000, 0.5 mL IM is given immediately.
- Repeat IM adrenaline every 5 minutes while waiting for ambulance
- Administer 100% oxygen.
- CPR if cardiac arrest occurs.
- If BP fall is rapid, 1:10,000 adrenalin may be infused IV slowly.
Question.6. Describe management of a patient in state of shock.
Answer. Shock is defined as an acute clinical syndrome characterized by a significant, systemic reduction in tissue perfusion, resulting in decreased tissue oxygen delivery and insufficient removal of cellular metabolic products, resulting in tissue injury and severe dysfunction of vital organs.
State of Shock Management
- Treat the cause, e.g. arrest hemorrhage, drain pus.
- Fluid replacement: Plasma, normal saline, dextrose, Ringer’s lactate, plasma expander (haemaccel).
Dosage is maximum l liter can be given in 24 hours. Initially crystalloids then colloids are given. Blood transfusion is done whenever required. - Ionotropic agents: Dopamine, dobutamine, adrenaline infusions—mainly in distributive shock like septic shock.
- Correction of acid-base balance: Acidosis is corrected by using 8.4% sodium bicarbonate intravenously.
- Steroid is often lifesaving. 500–l000 mg of hydrocortisone can be given. It improves the perfusion, reduces the capillary leakage and systemic inflammatory effects.
- Antibiotics in patients with sepsis; proper control of blood sugar and ketosis in diabetic patients.
- Catheterization to measure urine output (30–50 mL/hour or > 0.5 ml/kg/hour should be maintained).
- Nasal oxygen to improve oxygenation or ventilator support with intensive care unit monitoring has to be done.
- Central venous pressure line to perfuse adequately and to monitor flid balance. Total parentral nutrition is given when required.
- Pulmonary capillary wedge pressure to monitor very critical patient.
- Hemodialysis may be necessary when kidneys are not functioning.
- Control pain-using morphine (4 mg IV).
- Ventilator and ICU/critical care management.
- Injectionranitidine IV or omeprazole IV or pantoprazole IV.
- Activated C protein even though costly is benefiial as it prevents the release and action of inflmmatory response.
- MAST(MilitaryAnti-shockTrouser)provides circumferential external pressure of 40 mm Hg. lt is wrapped around lower limbs and abdomen, and inflted with required pressure.
It redistributes the existing blood and flid towards center. It should be deflted carefully and gradually.
Question.7. Discuss the etiopathology, clinical feature,s and management of hemorrhage shock.
Or
Describe hemorrhagic shock and management.
Answer.
Hemorrhagic Shock
Etiopathology: Due to whole blood loss like.
- Surgical: During and following any major surgery especially cardiopulmonary bypass, pelvic surgery or major abdominal surgery.
- Traumatic: As a result of any type of major accident,warfare injuries, homicidal or following suicidal injury as by knife, bullet, etc.
- GI bleeding: Bleeding from peptic ulcer, perforation of intestine, bleeding from esophageal varices, etc.
- Obstructive bleeding: Incomplete abortion, placenta previa, etc.
Hemorrhagic Shock Clinical Features
- Anxiety, restless, excitation and disorientation.
- Pallor
- Thirst and hunger
- Cold and clammy skin
- Faint in upright position
- Tachycardia with rapid, thready pulse
- Hypotension
- Oligouria or anuria.
Hemorrhagic Shock Management of Hemorrhage Shock
- The primary treatment of hemorrhagic shock is to control the source of bleeding as soon as possible and to replace flid.
- In controlled hemorrhagic shock, where the source of bleeding has been occluded, fluid replacement is aimed toward normalization of hemodynamic parameters.
- In uncontrolled hemorrhagic shock, in which the bleeding has temporarily stopped because of hypotension, vasoconstriction, and clot formation, fluid treatment is aimed at restoration of radial pulse or restoration of sensorium or obtaining a blood pressure of 80 mm Hg by aliquots of 250 mL of lactated Ringer’s solution (hypotensive re-suscitation).
- When evacuation time is shorter than 1 hour (usually ur-ban trauma), immediate evacuation to a surgical facility is indicated after airway and breathing have been secured.
- When expected evacuation time exceeds 1 hour, an intra-venous line is introduced and flid treatment is started before evacuation.
The resuscitation should occur before,or concurrently with, any diagnostic studies. - Crystalloid is the fist flid of choice for resuscitation.
Immediately administer 2 L of isotonic sodium chloride solution or lactated Ringer’s solution in response to shock from blood loss. - Fluid administration should continue until the patient’s hemodynamics become stabilized.
- Because crystalloids quickly leak from the vascular space,each liter of flid expands the blood volume by 20–30%; therefore, 3 L of flid need to be administered to raise the intravascular volume by 1 L.
- Alternatively, colloids restore volume in a 1:1 ratio. Currently available colloids include human albumin, hydroxyethyl starch products (mixed in either 0.9% isotonic sodium chloride solution or lactated Ringer’s solution), or hypertonic saline-dextran combinations.
- Packed red blood cells (PRBCs) should be transfused if the patient remains unstable after 2000 mL of crystalloid
resuscitation.
For acute situations, O-negative noncross-matched blood should be administered.
Administer 2 U rapidly, and note the response.
For patients with active bleeding, several units of blood may be necessary.
Question.8. Write short note on syncope.
Answer. Syncope may be defied as transient loss of consciousness which comes suddenly, lasts for a short time and is due to diminished blood supply to the brain.
The symptoms are fainting and vasovagal attack.
Syncope Etiology
- Simple faint
- Decreased cardiac output in various heart diseases.
- Fear and sudden anxiety.
- Trauma to the deep lying structures.
- Hypoglycemia
- Bouts of coughing, etc.
Syncope Clinical Features
- Syncopal attck is sudden.
- Prodromal symptoms: Tingling or numbness in limbs, sudden darkness before eyes and patient may have a feeling blacking out.
- Person is cold and sweating fall in ground suddenly becoming unconscious.
Syncope Treatment
- All the dental procedure or treatment is stopped.
- Remove instruments from oral cavity such as rubber dam,guaze, cottn, etc.
- Patient is kept in Trendelenburg position, i.e. patient is kept in a head low and feet up position.
- Loose tighten clothing of patient.
- Aromatic fumes inhalation is given or sprinkle cold water on face of patient for reflx stimulation.
- If recovery is gained escort patient home.
- If recovery is not gained Injection atropine 0.6 mg IM or IV is given.
- If still recovery is not gained look for hypoglycemia and
- Addison’s crisis.
- Start basic life support
- Summon medical help.
Question.9. Write in short on septic shock.
Or
Write short note on septic shock.
Or
Write short note on septicemic shock.
Answer. Septic shock is a vasodilator shock wherein there is peripheral vasodilation causing hypotension which is resistant to vasopressors.
Septic Shock Etiology
Septic shock may be due to Gram-positive organisms, Gram negative organisms, fungi, viruses or protozoal origin.
Pathophysiology of Septic Shock
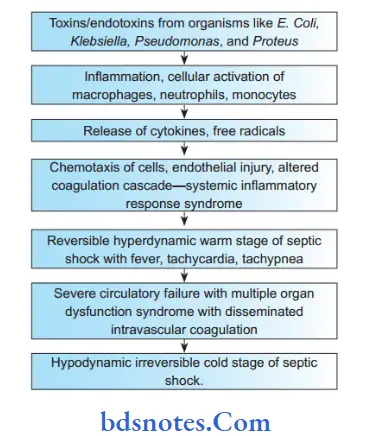
Septic Shock Clinical Features
Based on stages of septic shock.
Hyperdynamic or warm shock:
- It is a reversible stage.
- Patient has fever, tachycardia and tachypnea
- Pyogenic response is intact
Hypodynamic or cold septic shock:
- Pyogenic response is lost.
- Patient is in decompensated shock.
- Presence of anuria, cyanosis, jaundice, cardiac depression, pulmonary edema, hypoxia, drowsiness,coma and death.
Septic Shock Treatment/Management
- Correction of flid and electrolyte by crystalloids, blood transfusion. Perfusion is very/most important.
- Appropriate antibiotics-third generation cephalosporins and aminoglycosides.
- Treat the cause or focus—drainage of an abscess; lapa-rotomy for peritonitis; resection of gangrenous bowel;wound excision.
- Pus/urine/discharge/bile/blood culture and sensitivity for antibiotics.
- Critical care, oxygen, ventilator support, dobutamine dopamine/noradrenaline to maintain blood pressure and urine output.
- Activated C protein prevents the release of inflmmatory mediators and blocks the effcts of these mediators on cellular function.
- Monitoring the patient by pulse oximetry, cardiac status,urine output, arterial blood gas analysis.
- Short-term (one or two doses) high-dose steroid therapy to control and protect cells from effects of endotoxemia.
It improves cardiac, renal, and lung functions. Single dose of methylprednisolone or dexamethasone which often may be repeated again after 4 hours is said to be effective in endotoxic shock.
Question.10. Enumerate the complications of blood transfusion and describe the management of hypovolemic shock.
Answer.
Enumeration Of Complications Of Blood Transfusion
Congestive cardiac failure
Transfusion reactions HBV, HCV:
- Incompatibility. Major and minor reactions with fever,rigors, pain, hypotension
- Pyrexial reactions due to pyrogenic ingredients in the blood.
- Allergic reactions
- Sensitisation to leukocytes and platelets
- Immunological sensitization.
Blood Transfusion Infections:
- Serum hepatitis
- HIV infection
- Bacterial infection
- Malaria transmission
- Epstein-Barr virus infection
- Cytomegalovirus infection
- SyphiIis,Yersinia
- Babesia microti infection
- Trypanosoma cruzi infection.
Air embolism
Thrombophlebitis
Coagulation failure:
- Dilution of clotting factors
- Disseminated intravascular coagulation
- Dilutional thrombocytopenia occurs in patients with massive blood transfusion.
Circulatory overload causing heart failure
Hemochromatosis in patients with CRF receiving repeated blood transfusions
Citrate intoxication causes bradycardia and hypocalcemia.
Iron overload.
Question.11. Define and classify shock. In your practice local anesthetic is used, which type of shock it can produce.
How will you recognize and treat. What precautions should be taken to prevent.
Answer. Shock is a clinical condition characterized by inadequate tissue perfusion and hence cellular hypoxia.
Classification of Shock
- Hypovolemic shock
- Cardiogenic shock
- Distributive shock
- Septic shock
- Anaphylactic shock
- Neurogenic shock.
- Obstructive shock.
In clinical practice local anesthetic leads to anaphylactic shock.
Recognition of anaphylactic Shock
- Patient has asthma-like symptoms, i.e. sneezing and breathing.
- Urticaria and angioedema are present.
- Presence of bronchospasm and tachycardia
- Patient can undergo circulatory collapse.
- Due to rapid fall in blood pressure cardiac arrest may occur.
Treatment Of Anaphylactic Shock
- Summon ambulance
- Always check whether respiratory distress is due to other causes.
- Assess the degree of cardiovascular collapse by checking pulse and blood pressure.
- Assess the degree of airway obstruction
- Stop administration of drug
- Patient should be kept supine
- Assess breathing diffilty by checking for stridor, wheeze
- Administer oxygen to patient by face mask
- Give antihistamine chlorpheniramine maleate 10 mg
- Administer hydrocortisone 20 mg
- Monitor consciousness, airway, breathing, circulation, pulse, blood pressure
- Raise legs if blood pressure is low
- Adrenaline 1:1000, 0.5 mL IM is given immediately.
- Repeat IM adrenaline every 5 minutes while waiting for ambulance
- Administer 100% oxygen.
- CPR if cardiac arrest occurs.
- If BP fall is rapid, 1:10,000 adrenalin may be infused IV slowly.
Precautions taken to Prevent the anaphylactic Shock
- Intradermal test should be done before administering local anesthetic solution.
- Proper medical history of the patient is taken, if patient gives history of allergy from local anesthetic solution, drug should not be administered.
Question.12. Write in brief about complications of blood transfusion.
Answer. Following are the complications of blood transfusion:
- Febrile reactions: Itis the most common complication due to impurities like pyrogens in the blood or in infusion set.
- Headaches, fever, chills and rigors, tachycardia, nausea are the features.
- Transfusion is temporarily stopped or the flow is slowed down with administration of antipyretic drug to reduce fever.
- Often transfusion of that unit needs to be discontinued.
- Allergic reaction: Utrticaria and allergy to specifi proteins inthe donor’s plasma canoccur.
- Usually, itis mild and is treated with steroid and antihistaminics.
- In severe urticaria that unit of blood is discarded; new washed RBC’s and platelets are used.
- Acute hemolytic reactions: It is the most dangerous complication. It is due to ABO incompatibility.
- Usually it is nonfatal but occasionally can be fatal.
- It is commonly due to technical error at diffrent levels.
- It amounts for criminal negligence in court of law.
- Transfusion-related graft versus host disease:
- This very serious, very rare complication occurs due to recognition and reaction against host tissues by infused donor lymphocytes.
- lt is common in immunosuppressed, lymphoma, leukemic patients.
- Any type of blood products including leukocyte-reduced blood can cause the condition.
- Features are pancytopenia, toxic epidermal necrosis, liver dysfunction with more than 90% mortality. It is difficult to treat.
- Congestive cardiac failure: It occurs if especially large quantities of whole blood are transfused in chronic severe anemia, pregnancy, elderly patients, in patients who have cardiac problems.
Question.13. Enumerate differences between hypovolemic and septic shock.
Or
Write the difference between septic and hypovolemic shock.
Answer.
Question.14. Describe etiopathogenesis and classification of shock. How will you manage hemorrhagic shock.
Answer. Etiopathogenesis
Shock Classification
- Hypovolemic shock
- Cardiogenic shock
- Distributive shock:
- Septic shock
- Anaphylactic shock
- Neurogenic shock.
- Obstructive shock.
Management of Hemorrhagic Shock
- The primary treatment of hemorrhagic shock is to control the source of bleeding as soon as possible and to replace flid.
- In controlled hemorrhagic shock, where the source of bleeding has been occluded, fluid replacement is aimed toward normalization of hemodynamic parameters.
- In uncontrolled hemorrhagic shock, in which the bleeding has temporarily stopped because of hypotension, vasoconstriction, and clot formation, fluid treatment is aimed at restoration of radial pulse or restoration of sensorium or obtaining
- a blood pressure of 80 mm Hg by aliquots of 250 mL of lactated Ringer’s solution (hypotensive resuscitation).
- When evacuation time is shorter than 1 hour (usually urban trauma), immediate evacuation to a surgical facility is indicated after airway and breathing have been secured.
- When expected evacuation time exceeds 1 hour, an intravenous line is introduced and fluid treatment is started before evacuation. The resuscitation should occur before, or concurrently with, any diagnostic studies.
- Crystalloid is the fist flid of choice for resuscitation.
- Immediately administer 2 L of isotonic sodium chloride solution or lactated Ringer’s solution in response to shock from blood loss.
- Fluid administration should continue until the patient’s hemodynamics become stabilized.
- Because crystalloids quickly leak from the vascular space,each liter of flid expands the blood volume by 20–30%;therefore, 3 L of flid need to be administered to raise theintravascular volume by 1 L.
- Alternatively, colloids restore volume in a 1:1 ratio.
- Currently available colloids include human albumin,hydroxyethyl starch products (mixed in either 0.9% isotonic sodium chloride solution or lactated Ringer’s solution), or hypertonic saline-dextran combinations.
- Packed red blood cells (PRBCs) should be transfused if the patient remains unstable after 2000 mL of crystalloid resuscitation.
- For acute situations, O-negative non crossmatched blood should be administered.
- Administer 2 U rapidly, and note the response.
- For patients with active bleeding, several units of blood may be necessary.
Question.15. Describe different types of shock. How to manage hemorrhagic shock?
Or
Define shock, clinical feature and managment of various type of shock?
Answer. Shock is defined as an acute clinical syndrome characterized by a significant, systemic reduction in tissue perfusion, resulting in decreased tissue oxygen delivery and insuffient removal of cellular metabolic products, resulting in tissue injury and severe dysfunction of vital organs.
Description Of Different Types Of Shock
Classification of Shock
- Hypovolemic shock
- Cardiogenic shock
- Distributive shock:
- Septic shock
- Anaphylactic shock
- Neurogenic shock
- Obstructive shock
Hypovolemic shock
- It occurs due to loss of blood plasma or body flid and electrolytes, usually caused by massive hemorrhage,vomiting, diarrhea and dehydration.
- Hypovolemic shock is most common type of shock which is characterized by loss in circulatory volume which leads to decrease in venous return, decrease in filing of cardiac chambers, so there is decreased cardiac output which causes increase in systemic vascular resistance.
Hypovolemic shock Causes
Loss of extracellular fluid:
- Deviation of normal exchange pattern: As in vomiting, diarrhea, intestinal obstruction, peritonitis, and acute pancreatitis.
- Increased sweating without replacement in a non acclimatized individual.
- Third space shifts to sodium from extracellular to intracellular compartment due to failure of sodium pump caused by hypoxia.
Plasma loss: Due to burn.
Hemorrhage: Due to whole blood loss like.
- Surgical: During and following any major surgery especially cardiopulmonary bypass, pelvic surgery or major abdominal surgery.
- Traumatic: As a result of any type of major accident,warfare injuries, homicidal or following suicidal injury as by knife, bullet, etc.
- GI bleeding: Bleeding from peptic ulcer, perforation of intestine, bleeding from esophageal varices, etc.
- Obstructive bleeding: Incomplete abortion, placenta previa, etc.
Hypovolemic shock Clinical Features
- Anxiety, restless, excitation and disorientation.
- Pallor
- Thirst and hunger
- Cold and clammy skin
- Faint in upright position
- Tachycardia with rapid, thready pulse
- Hypotension
- Oligouria or anuria.
Hypovolemic shock Management
Cardiogenic shock
- Myocardial infection is the most common cause of cardiogenic shock.
- Cardiogenic shock occurs if more than 40% of left ventricle is involved in acute infection.
- Elevated cardiac chamber filing procedure is hallmark of cardiogenic shock.
Cardiogenic shock Clinical Features of Cardiogenic Shock
- The primary problem is decrease in contractility of heart,due to decrease contractility, there is decrease in stroke volume.
- Patient present with tachycardia, low blood pressure and decrease urinary output.
- Jugular venous pressure may be raised.
- Peripheries are cold and patient may be confuse or*moribund.
Cardiogenic shock Treatment
- Proper oxygenation with intubation, ventilator support,cardiac version, pacing, antiarrhythmic drugs, correction of electrolytes, avoiding flid overload and prevention of pulmonary edema as immediate measures.
- Dobutamine is used to raise cardiac output provided there is adequate preload and intravascular volume. Dopamine is preferred in patients with hypotension.
- But it may increase peripheral resistance and heart rate worsening cardiac ischemia.
- Often both dopamine and dobutamine combination may be required.
- Careful judicial use of epinephrine. norepinephrine, phosphodiesterase inhibitors (amrinone, milrinone) are often needed.
- Anticoagulants and aspirin are given.
- Thrombolytics can be used β blockers, nitrates(nitroglycerine causes coronary arterial dilatation).
- ACE inhibitors are also used.
- Intra-aortic balloon pump: May need to be introduced;transfemorally as a mechanical circulatory support to raise cardiac output and coronary blood flow.
- Relief of pain, preserving of remaining myocardium and its function, maintaining adequate preload, oxygenation, minimizing sympathetic stimulation, correction of electrolytes should be the priorities.
- Percutaneous transluminal coronary angioplasty (PTCA) and coronary artery bypass graft (CABG) are the fial choices.
Distributive Shock
This occurs when the after load is excessively reduced.
Distributive shock occurs in following situations:
- Septic shock
- Anaphylactic shock
- Neurogenic shock
Septic shock
- This type of shock is mostly due to release of endotoxins in blood, which causes widespread vasodilation of blood vessels resulting in fall in the cardiac output.
- Fall in the cardiac output is not initial feature and vasoconstriction is not observed.
- Bacteria responsible for release of endotoxins are E. coli,Pseudomonas, Proteus, etc.
Septic shock Clinical features
- Restlessness, anxiety
- Cyanosis
- Cold and clammy skin
- Tachycardia
- Oligouria or anuria
- Acidotic breathing.
Septic Shock Management
- Sedation with diazepam
- IV fluids
- Blood culture and sensitivity
- Antimicrobial agents: Combination of penicillin or cephalosporins and aminoglycosides and metronidazole.
- Injection hydrocortisone
Anaphylactic Shock
Anaphylactic shock can occur when a previously sensitized individual is exposed to a specifi antigen, IV drug, specially
penicillin, cephalosporins and iodinated contrast media are common offnders.
Anaphylactic Shock Clinical Features
- Due to reduced cerebral perfusion, there is change in mental status.
- Due to reduced preload and cardiac contractility, there is hypotension.
- Due to release of histamine and other chemical mediators there is urticaria.
- Due to hypoxia the cyanosis is caused.
- Due to anaerobic metabolism and hepatic dysfunction the lactic acidosis is caused.
- Due to coronary ischemia other dysrhythmias are caused.
Anaphylactic Shock Treatment
- Summon ambulance
- Always check whether respiratory distress is due to other causes.
- Assess the degree of cardiovascular collapse by checking pulse and blood pressure.
- Assess the degree of airway obstruction
- Stop administration of drug
- Patient should be kept supine
- Assess breathing diffilty by checking for stridor, wheeze
- Administer oxygen to patient by face mask
- Give antihistamine chlorpheniramine maleate 10 mg
- Administer hydrocortisone 20 mg
- Monitor consciousness, airway, breathing, circulation,pulse, blood pressure
- Raise legs if blood pressure is low
- Adrenaline 1:1000, 0.5 mL IM is given immediately.
- Repeat IM adrenaline every 5 minutes while waiting for ambulance
- Administer 100% oxygen
- CPR if cardiac arrest occurs
- If BP fall is rapid, 1:10,000 adrenalin may be infused IV slowly.
Neurogenic Shock
- It occurs due to spinal cord injury which leads to dilatation of splanchnic vessels
- There will be bradycardia, hypotension, arrhythmias and decreased cardiac output.
Neurogenic Shock Clinical Features
- History of emotional stress or pain of a sudden nature.
- Bradycardia or pallor
- Tachypenea
- Fainting
- Reflexes are usually intact.
Neurogenic Shock Treatment
- Blood pressure should be controlled by giving vasoconstrictors.
- Oxygen is administered
- Hemodynamics should be maintained.
- Airways are cleared.
- Fluid therapy should be given
- Intravenous methylprednisolone therapy is done.
- Dopamine and phenylephrine can be used.
Obstructive Shock
- The obstructive shock is due to cardiac temponade, due to tension pneumothorax and pulmonary embolus.
- In cardiac temponade, there is compression ofall chambers of heart with reduce cardiac output. The filing pressure of left- and right-sided chambers equalizes. The central venous pressure is high and the BP is low.
Obstructive Shock Treatment
- To maintain preload with flid or blood.
- Relief of obstructions, drain pericardial cavity as early as possible.
Question.16. Define shock. Name types of shock which can be met within your practice. How will you manage them?
Answer. Shock is defined as an acute clinical syndrome characterized by a significant, systemic reduction in tissue perfusion, resulting in decreased tissue oxygen delivery and insuffient removal of cellular metabolic products, resulting in tissue injury and severe dysfunction of vital organs.
Types of shock which can be met in my dental practice and management of the same
Following are the shocks which can be in my dental practice:
- Anaphylactic shock: It occurs due to the allergy caused by local anesthetic agent.
- Hypovolemic shock: It occur during and following any major dental surgery.
Question.17. Hazards of blood transfusion.
Answer. The following are the hazards of blood transfusion:
Transfusion Reactions—Incompatibility
Blood Transfusion Causes
- Mistake in crossmatching: This is a technical error, if the serum is old or labeling is wrong.
- Due to transfusion of blood which is already hemolysed by warming, over freezing or shaking.
- Due to transfusion of blood after expiry date.
Clinical Features of Mismatched Blood Transfusion
- Presence of rigors and fever. Patient may complain of nausea, vomiting, headache, pain in the loins, tingling sensation in the extremities.
- There can be chest pain and dyspnea.
- If the patient is already in shock, it may become more pronounced instead of curing it. Gradually, he will lose consciousness.
- Urine output decreases and hemoglobinuria may occur within 2 to 3 hours.
- Jaundice may appear within 24–36 hours, this is the confimatory evidence of mismatching.
- Ultimately renal failure sets in due to the blockage of renal tubules by hematin pigment.
Blood Transfusion Treatment
- Transfusion should be stopped immediately.
- Fresh blood specimen of venous blood and urine from the patient should be sent to laboratory for rechecking along with the rejected blood pack.
- IV flids should be started instead of blood.
- Alkalization of blood to be done by isotonic solution of sodium lactate and 10 mL of sodium bicarbonate to facilitate precipitation of hematin pigments.
- Frusemide 80–120 mgIVshould be givenfor forced diuresis.
This maybe repeated, ifurine outputis increased to 30 mL/h. - Antihistamine and hydrocortisones should be given.
- In very severe cases. hemodialysis should be undertaken.
Pyrexial reactions
It is common to see simple reactions like pyrexia, chills, rigors, restlessness, headache, tachycardia, nausea and vomiting.
Pyrexial reactions Causes
- Improperly sterilized drip sets.
- Presence of pyrogens in the donor set.
- Transfusion of infected blood.
- Very rapid transfusion
Pyrexial reactions Prevention
These reactions can be prevented by using sterilized plastic disposable sets.
Pyrexial reactions Treatment
Transfusions should be stopped immediately though temporarily.
Antihistaminics and antipyretics should be given.
After his condition returns to normal, blood transfusion can be restarted.
Allergic Reactions
Usually, within few hours of transfusion, patients may get mild urticaria, tachycardia, fever and dyspnea.
He may even go into severe anaphylactic shock.
Allergic Reactions Treatment
Transfusion should be stopped. Antihistamines and cortisones should be given. Shock should be treated.
Allergic Reactions Transmission Of Diseases
- Serum hepatitis: Hepatitis B is a common disease which can be transmittd during blood transfusion.
The symptoms usually appear within 3 months. - AIDS: HIV can be transmittd from the donor’s blood to the recipient.
- Bacterial infection: This occurs due to faulty storage technique.
This should be treated with higher antibiotics otherwise patient may go into septicemia.
Reaction Due To Massive Blood Transfusion
“Massive blood transfusion implies single transfusion of 8-10 units of blood in 24 hours.”
- Acid-base imbalance results in significant metabolic alkalosis.
- Hyperkalemia
- Citrate toxicity: After massive blood transfusion, increased citrate level consumes ionized calcium from patient’s body.\The body compensates it by rapidly mobilizing calcium from the bones.
- Rarely when hypocalcemia is recognized calcium can be infused.
- Hypothermia: During massive blood transfusion, cold blood is rapidly infused from the refrigerator to the patient. His temperature may drop by 3 to 4°C.
- Failure of coagulation: After massive blood transfusion, the natural process of coagulation may fail due to dilution of platelets and various clottng factors. .
- Disseminated intravascular coagulation (DIC): This may occur after a massive blood transfusion. Actually, it occurs after mismatched blood transfusion.
Complications of over transfusion
These complications may be seen in patients with chronic anaemia, in children and elderly patients.
They should receive packed cells rather whole blood.
Transfusions should be given slowly for 4–6 hours and after some intervals.
Elderly patients should be given packed cells with diuretics.
Complications of intravenous transfusions
Thrombophlebitis and air embolism.
Pulmonary Complications
Syndrome of transfusion—related acute lung injury is defied as a noncardiogenic pulmonary edema related to transfusion.
Question.18. Write short note on indications of blood transfusion.
Answer. Following are the indications of blood transfusion:
- Acute blood loss following trauma ≥15% of total body volume in otherwise healthy individuals (liver, spleen,kidney, GIT injuries, fractures, hemothorax, perineal injuries).
- During major surgeries—abdominoperineal surgery,thoracic surgery, hepatobiliary surgery.
- Following burns.
- In septicemia.
- As a prophylactic measure prior to surgery.
- Whole blood is given in acute blood loss.
- Packed cells are given in chronic anemia.
- Blood fractions are given in idiopathic thrombocytopenic purpura, hemophilia.

Leave a Reply