Salivary Gland Disorders Question And Answers
Question 1. Classify and enumerate salivary gland diseases.
Answer.
Salivary Gland Tumor Classification by WHO (2017)
Malignant Tumors
- Mucoepidermoid carcinoma 8430/3
- Adenoid cystic carcinoma 8200/3
- Acinic cell carcinoma 8550/3
- Polymorphous adenocarcinoma 8525/3
- Clear cell carcinoma 8310/3
- Basal cell adenocarcinoma 8147/3
- Intraductal carcinoma 8500/2
- Adenocarcinoma, NOS 8140/3
- Salivary duct carcinoma 8500/3
- Myoepithelial carcinoma 8982/3
- Epithelial-myoepithelial carcinoma 8562/3
- Carcinoma ex pleomorphic adenoma 8941/3
- Secretory carcinoma 8502/3*
- Sebaceous adenocarcinoma 8410/3
- Carcinosarcoma 8980/3
- Poorly differentiated carcinoma
- Undifferentiated carcinoma 8020/3
- Large cell neuroendocrine carcinoma 8013/3
- Small cell neuroendocrine carcinoma 8041/3
- Lymphoepithelial carcinoma 8082/3
- Squamous cell carcinoma 8070/3
- Oncocytic carcinoma 8290/3
Read And Learn More: Oral Medicine Question And Answers
Salivary Gland Uncertain Malignant Potential
- Sialoblastoma 8974/1
- Benign tumors
- Pleomorphic adenoma 8940/0
- Myoepithelioma 8982/0
- Basal cell adenoma 8147/0
- Warthin tumor 8561/0
- Oncocytoma 8290/0
- Lymphadenoma 8563/0*
- Cystadenoma 8440/0
- Sialadenoma papilliferum 8406/0
- Ductal papillomas 8503/0
- Sebaceous adenoma 8410/0
- Canalicular adenoma and other ductal adenomas 8149/0
- Non-neoplastic epithelial lesions
- Sclerosing polycystic adenosis
- Nodular oncocytic hyperplasia
- Lymphoepithelial sialadenitis
- Intercalated duct hyperplasia
Benign Soft Tissue Lesions
- Haemangioma 9120/0
- Lipoma/sialolipoma 8850/0
- Nodular fasciitis 8828/0
Hematolymphoid Tumors
Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) 9699/3
Question 2. Write short answer note on xerostomia.
Or
Classify salivary gland disorders. Write in detail about causes and management of patients with xerostomia.
Answer. For classification of salivary gland disorders refer to Ans 1 of same chapter.
It is dryness of mouth, which is a clinical manifestation of salivary gland dysfunction.
Xerostomia Etiology
- Radiation induced: Ionizing radiation to head and neck region for treatment of cancer results in pronounced changes in salivary glands located within primary beam.
- Pharmacologically induced xerostomia: The drugs causes decreased salivary flow are anticonvulsants, antiemetics, antihistamines, antihypertensives and antispasmodics.
- Systemic alterations resulting in xerostomia:
- Certain deficiency states such as pernicious anemia, iron deficiency anemia and deficiency of vitamin A and hormone can cause xerostomia.
- Fluid loss associated with hemorrhage, sweating, diarrhea, vomiting and diabetes insipidus.
- Developmental abnormalities of salivary gland.
- Systemic disease accompanied by high temperature and dehydration.
- Local factors: Local factors such as smoking, mouth breathing and decrease in the mastication leads to xerostomia.
- Developmental: Various developmental abnormalities such as salivary gland tumors, autoimmune conditions and some of the diseases which affect efferent or afferent portion of the neural transmission reflex.
Xerostomia Clinical Features
- Effect of xerostomia on oral functions:
- Increased thirst, increased uptake of fluid while eating.
- Frequent use of chewing gums and consumption of sour candy.
- Burning and tingling sensations in mouth.
- Painful salivary gland enlargement.
- Oral infections, intolerance to dental appliances.
- Effect of xerostomia on normal functions:
- Blurred vision and ocular dryness, itching, burning in the eyes.
- Dryness of pharynx and skin. Itching and burning sensation of vagina.
- Clinical signs of xerostomia:
- Dryness of lining of oral mucosa.
- Tongue blade may adhere to soft tissues.
- Increase incidence of dental caries.
- Candidiasis—Pseudomembranous.
- Angular cheilitis.
- Candidiasis: Due to xerostomia, pseudomembranous and hyperplastic forms of candidiasis occur.
- Residual: The residual saliva which remains is foamy, thick and ropey.
Xerostomia Management
Stimulation of Salivary Production:
Local stimulation: By chewing gums, mints, paraffin and citric acid containing lozenges and rinses.
- Systemic stimulation.
- Bromhexine 1/m/4-8 mg TDS.
- Anethole trithionate 1/m/25 mg TDS.
- Pilocarpine 1/m/5 mg TDS.
Symptomatic Treatment:
Salivary substitutes are given: Most commonly it consists of carboxymethyl cellulose or hydroxyethyl cellulose as lubricants, artificial sweeteners, preservative and chloride as well as fluoride ions.
Suggestion to Patient Having Xerostomia
- Try very sweet or tart foods and beverages such as lemonade.
- Try sucking ice cubes.
- Use soft and liquid foods.
- Avoid dry foods, chocolate, pastry.
- Avoid over salty foods.
- Have a sip of water in every few minutes which helps in swallowing.
Question 3. Write short note on sialolithiasis.
Or
Classify salivary gland disorders. Describe clinical features, investigations and treatment of sialolithiasis.
Answer.
- It is a type of a obstructive disorder.
- It is the formation of calcific concentrates within parenchyma or ductal system of major and minor salivary glands.
Etiopathogenesis
- Neurohumoral mechanism: A neurohumoral condition causes salivary stagnation which causes nidus and matrix formation.
- Metabolic mechanism: In presence of the coexisting inflammation, metabolic mechanism favors precipitation on salivary salts into the matrix.
Sialolithiasis Clinical Features
- The sialolith is present in middle-aged patients with slight predilection for males.
- It occurs as solitary concretion varying in size from few millimeters up to several centimeters.
Sialolithiasis Symptoms
- Patient complains of moderately severe pain and intermittent transient swelling during meals, which resolve after meals.
- The occlusion of duct prevents the free flow of saliva and this accumulation of saliva under pressure produces pain.
Sialolithiasis Signs
- Pus may exude from duct orifice.
- Soft tissues surrounding the duct shows severe inflammatory reaction, which may appear as swelling, redness and tenderness.
- Stones in more peripheral portion of the duct may often palpate, if they are of sufficient size.
- Sometimes, overlying mucosa may ulcerate allowing calculus to extend into the oral floor.
- No saliva is seen to be coming out from duct orifice.
Radiographic Features/Investigations
- Radiograph: For submandibular duct stone, mandibular occlusal view is standard and for parotid gland periapical view in the buccal vestibule is standard.
- Sialography: It is to be done when sialoliths are radiolucent. Ductal dilatation is present. Film shows contrast medium which is present behind the stone.
- Radiodensity: Sialoliths are radiopaque, are oval in shape and cylindrical along with the presence of multiple layers of calcification. Borders of sialolith are smooth and have even radiodensity.
- CT scan: During contrast study, it shows the dense radiopaque area.
- Sonography: It demonstrates presence of calculi.
Sialolithiasis Diagnosis
- Clinical diagnosis: On palpation of the suspected gland, it reveals that its size is large and firm as compared to normal gland of contralateral side. During the digital manipulation, flow of saliva is produced via ductal orifice and allows visual inspection of saliva. At the time of examination soft tissues overlying the duct get manually stretched, physical distortion can be caused by the calculus will be apparent. At times yellow color of the calcific deposit is seen via the thin and distended mucous membrane.
- Metallic duct probe: When duct is carefully probed by metallic probe, this indicates existence and location of the calculus.
- Swab test: It stone is present in single duct only, saliva will not come out of that. This is tested by placing the two dry swabs over each of the orifice and some of the drops of lemon juice should be dropped on dorsum of the tongue. After a minute, patient is asked to move tongue up. Swab over the orifice of duct where the stone is impacted remains dry while the other swab gets wet.
- Radiographic examination: It shows calcific deposits.
- Sialography: It demonstrates contrast medium behind the stone.
Sialolithiasis Management
- Manual manipulation of stone within the duct. It moves the stone towards the orifice of duct.
- Stone in submandibular duct: If stone is palpated near the orifice of duct, it can be removed by incision made directly over it through the mucus membrane of mouth.
- Stone in submandibular gland: Excision of gland is advised.
- If infection is present, then antibiotics are given.
- Salivary gland endoscopy: This is the advance modern method to remove the sialoliths.
- Lithotripsy: It leads to the fragmentation of stone inside the gland.
Question 4. Write short note on mucocele.
Or
Write short note on clinical features of mucocele.
Or
Classify cysts of orofacial region. Write in detail about clinical features, etiopathogenesis of mucocele and its management
Answer. For Classification refer to Ans 1 of chapter CYSTS OF JAW.
Mucocele is the term used to describe the swelling caused by pooling of saliva at the site of injured minor salivary gland.
Etiopathogenesis
Trauma is the main cause. Trauma leads to the laceration of minor salivary gland duct which causes extravasation of mucus inside the connective tissue. Mucus accumulates in the connective tissue and due to the continuous pooling of saliva a cavity develops which does not consists of a epithelial lining.
Mucocele Clinical Features
- Mucocele is present as a discrete, painless, smooth surface swelling which ranges from few centimeters to few millimeters in diameter.
- Mucocele occur commonly in younger patients and there is equal predilection for both males and females.
- Superficial mucoceles have a blue hue while the deeper lesions are more diffuse and are covered by normal mucosa without presence of blue hue.
- Superficial mucoceles get frequently traumatized and can develop surface ulceration.
- When superficial cysts get inflamed they become fluctuant, soft, nodular and have dome-shaped elevation.
- Patient complains of presence of painless swelling which is often recurrent. Swelling may suddenly develops at meal time and may drain simultaneously at intervals.
- Extravasation mucocele commonly occur over the lower lip. Other sites of its occurrence are buccal mucosa, floor of mouth and retromolar region.
- Extravasated mucoceles are most commonly seen in children and teenagers.
- Mucus retention cysts are commonly seen on the upper lip, palate, buccal mucosa, floor of mouth and rarely the lower lip.
- Consistency of mucocele is either soft or hard which depends on the tension of fluid. Cyst cannot be emptied by the digital pressure.
Mucocele Types
- Mucus extravasation: It is caused by laceration of minor salivary gland duct by trauma resulting in extravasation of mucus in connective tissue. It is not lined by epithelium.
- Mucus retention: It is caused by obstruction of minor salivary gland duct which causes backup of saliva. It is lined by epithelium.
Mucocele Diagnosis
- Clinical diagnosis: On clinical examination there is presence of dome shaped soft swelling which is usually lateral to the midline.
- Laboratory diagnosis:
- In biopsy, the microscopic examination shows vacuolar macrophages which are known as mucinophages.
- On aspiration, there is presence of sticky, viscous color fluid.
Mucocele Differential Diagnosis
- Superficial non-keratin cyst and vascular lesion: Aspiration is characteristic.
- Early mucoepidermoid tumor and adenocarcinoma: Both the lesions show induration but mucocele does not.
Mucocele Management
- Complete surgical excision is carried out along with removal of adjacent minor salivary gland which is feeding the lesion. This is carried out under local anesthesia.
- Surgery with cryoprobe can also be done.
Question 5. Write short note on pleomorphic adenoma.
Answer. Pleomorphic adenoma or benign mixed tumor is most common neoplasm of salivary glands. The parotid gland is mostly affected by the tumor.
Histogenesis/Pathogenesis
- There is presence of myoepithelial cells and reserve cells arranged in intercalated duct. The intercalated duct reserve cells can differentiate into ductal and myoepithelial cells and the later can undergo mesenchymal metaplasia.
- Dardick’s theory: It is the most accepted theory. They state that a neoplastically altered epithelial cell with the potential for multidirectional differentiation may be histologically responsible for the pleomorphic adenoma.
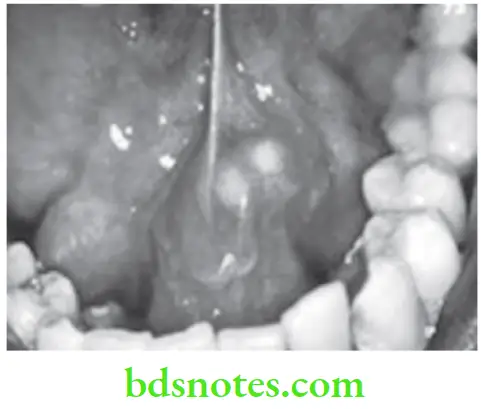
Pleomorphic Adenoma Clinical Features
- Pleomorphic adenoma is most common in 4th to 6th decades of life. Women to men ratio is 6:4.
- Most commonly parotid gland and the intraoral palatal gland on the lip are affected.
- Patient complains of presence of small, painless, quiescent swelling which is slowly began to increase in the size.
- Swelling is round to oval in shape and become lobulated as it get larger.
- In some of the patients, lesion grows towards the medial direction between the ascending ramus and the stylomandibular ligament which produces dumb – bell shaped appearance.
- Generally the surface of the tumor is smooth but sometimes it become bosselated and is occasionally crossed by deep furrows.
- It is firm to rubber y in consistency and sometimes shows cystic degeneration.
- Over the palate, it seen on lateral aspect, it has smooth surface and is of dome shaped.
Pleomorphic Adenoma Diagnosis
- Clinical diagnosis: Presence of smooth surface enlargement in parotid area can provide clue for pleomorphic adenoma.
- Sialography: It demonstrates Ball in hand appearance.
- CT Scan: By help of this, exact extension of tumor should be elicited.
- Laboratory diagnosis: On microscopic examination, neoplasm often exhibits proliferation of glandular epithelial cells in form of diffuse sheet or clusters. Neoplastic cells are polygonal, spindle or stellate shape and form duct like structures. Duct like structures are of varying size, shape, number and are widely distributed within lesion. Each duct like structure exhibits an inner row of cuboidal or columnar cells and outer row of spindle shape myoepithelial cells. Epithelial cells show “squamous metaplasia” and sometimes, there may be formation of keratin pearls by metaplastic epithelial cells. Connective tissue undergoes hyalinization to form structureless homogeneous material. Mucoid materials in myxochondroid are composed of glycosaminoglycAns and consist mainly of chondroitin sulfate. Complete capsule is never present.
Pleomorphic Adenoma Management
- Majority of tumors of salivary glands are radiolucent, so wide surgical excision is the treatment of choice.
- Recurrence is common in parotid tumors.
- In benign condition, superficial parotidectomy is the treatment of choice (Patey’s operation).
- The facial nerve should not be injured during operation. It is preserved by removing the gland in two parts (superficial and deep).
Question 6. Classify various salivary gland diseases and describe in detail about Sjögren’s syndrome.
Or
Write short note on clinical features and management of Sjögren’s syndrome.
Or
Write short note on Sjögren’s syndrome and its management.
Or
Write short note on clinical features of Sjögren’s syndrome.
Or
Describe investigations for Sjögren’s syndrome.
Or
Classify salivary gland disorders. Describe clinical features. Sialographic features and management of Sjögren’s syndrome.
Or
Classify salivary gland disorders. Describe etiology, clinical features, radiographic features, investigations and management of Sjögren’s syndrome.
Or
Write short note on Sjögren’s syndrome.
Or
Write short answer on Sjögren’s syndrome.
Answer. For classification refer to Ans l of the same chapter.
Sjögren’s Syndrome
It is a chronic inflammatory disease that affects salivary, lacrimal and other exocrine glands.
Sjögren’s Syndrome Types
- Primary Sjögren’s syndrome: It is also called as sicca syndrome and it consists of dry eyes and dry mouth.
- Secondary Sjögren’s syndrome: It consists of dry eyes, dry mouth and collagen disorders usually rheumatoid arthritis or systemic lupus erythematosus.
Etiology
- Immunological: Lesion in sjogren’s syndrome is immunologically mediated inflammatory exocrinopathy. This usually starts with the periductal infiltration of the tissue by mononuclear cells.
- Autoantibodies: B cell hyperactivity can occur due to the deficiency of suppressor T lymphocytes or B lymphocytes by secreting antibodies against them. Antinuclear antibodies are seen in patients of Sjogren’s syndrome which are directed most commonly to DNA histone.
- Immune complex: Circulating immune complexes are seen in patients of Sjogren’s syndrome.
- Cell mediated immune response: There is presence of depressed delayed hypersensitivity response to the skin testing in patients of secondary Sjogren’s syndrome as compared to primary Sjogren’s syndrome. Lymphokine production in response to the antigen by normal salivary tissue is increased in patients of Sjogren’s syndrome.
- Natural killer cell activity: This is impaired in patients of sjogren’s syndrome.
- Genetic aspect: The genetic effects of Sjogren’s syndrome depend on HLA linked and non-HLA linked genes. Relations of Sjogren’s syndrome show high incidence of connective tissue diseases.
Xerostomia Clinical Features
Xerostomia Oral Manifestations
- Xerostomia is a major complaint in most of the patients. But many patients do not complaint of dry mouth, but rather of an unpleasant taste, difficulty in eating dry food, soreness or difficulty in controlling dentures.
- Pus may be emitted from the duct. Angular stomatitis and denture stomatitis also occur.
- Dry mouth may be accompanied by the unilateral or bilateral enlargement of parotid gland.
- In early stages, the mouth of patient remain moist but later on there is lack of pooling of saliva in floor of the mouth and frothy saliva can be formed along the lines of contact with oral tissues.
- Tongue becomes lobulated and consists of red surface with partial and complete depapillation. Taste buds also get decreased in numbers.
- In advanced cases, mucosa is glazed, dry and tends to form fine wrinkles.
- In some patients, there may be clicking quality of their speech, caused by sticking of tongue to palate.
- Dental caries is severe and gross accumulation of plaque may be obvious.
- Periodontal disease can also occur.
- Regional lymph nodes may be enlarged and tender.
Xerostomia General Manifestations
- It occurs in middle age persons and females are commonly affected.
- Patient usually complains of dry eyes or continuous irritation in the eyes. Severe lacrimal gland involvement may lead to corneal ulceration as well as conjunctivitis.
- Dryness of pharynx, larynx and nose are noted by some patients. This is accompanied by lack of secretion in upper, respiratory tract and may lead to pneumonia.
- Vaginal dryness may be also complained by some patients.
- Rheumatoid arthritis is long-standing feature in secondary sjogren’s syndrome. Patient can have small joint, ulnar deviation of fingers and rheumatiod nodules.
Radiographic Features
Sialographic Features:
- If salivary flow rate is equivocal, sialography may detect the damage.
- Most typical finding in ‘Sjögren’s syndrome’ is sialectasis, which typically produces snowstorm appearance as a result of leakage of contrast medium.
- There is also presence of atrophy of ductal tree; emptying of duct is typically delayed.
- In some of the cases, it will show cherry blossom appearance of the obstructed ductal system.
- Salivary Scintiscanning: It is done with technetium pertechnetate which shows impaired salivary function in patients of Sjogren’s syndrome.
Sialographic Investigations
- Rose bengal staining test: The keratoconjunctivitis sicca is characterized by corneal keratotic lesions which stain pink when Rose Bengal dye is used.
- Schirmer test: The reduced lacrimal flow rate in Sjögren’s syndrome is measured by this test. A strip of filter paper is placed in between eye and the eyelid to determine the degree of tearing, which should be measured in millimeter. When the flow is reduced to less than 5 mm in a 5 minutes sample period, the patient should be considered positive for Sjögren’s syndrome.
- Biopsy: Changes in minor salivary glands of lower labial mucosa shows correlation with those in major salivary glands.
- Sialometry: Stimulated flow rate in primary and secondary Sjogren’s syndrome is below 0.5 to 1 mL/minute while the normal is 1 to 1.5 mL/min.
- Sialochemistry: The saliva of parotid gland in Sjögren’s syndrome contains double the value of normal lipid and increase in values of phospholipids and glycolipids than normal saliva.
- Immunohistochemistry: Routine antibody profile should be done to detect antinuclear and rheumatoid factor.
- Hematological: This is usually done to look for anemia. Raise in ESR levels and leucopenia can be appreciated.
- Microbiological: Swab from oral mucosa is taken to check for candidiasis, if there is presence of soreness and redness.
Sialographic Management
- Most of the patients are treated symptomatically.
- Keratoconjunctivitis is treated by installation of ocular lubricants, such as artificial tears coating methylcellulose and Xerostomia is treated by salivary substitutes.
- Scrupulous oral hygiene and frequent fluoride application is indicated to reduce these problems.
- Surgery for enlargement of salivary gland is only recommended when the enlargement is causing the discomfort to the patient.
Question 7. Write short note on sialorrhea.
Answer. It is a functional disorder of salivary gland.
- It is also known as ptyalism.
- Sialorrhea is referred to as increased salivary secretion.
Sialorrhea Mechanism
Parasympathetic nervous system controls the secretory innervations of salivary glands. As parasympathetic system gets stimulated, it leads to profuse secretion of watery saliva.
Etiology
- Some drugs which are also known as sialogogues stimulate the salivary flow, e.g. cholinergic antagonists.
- Stomatitis, ANUG, etc. are some of the local factors which leads to increased salivation.
- Parkinson’s disease, epilepsy, Down’s syndrome are some of the systemic diseases which lead to the increased salivation.
- Various miscellaneous factors such as metal poisoning and Bell’s palsy leads to ptyalism.
- Hypersecretion of saliva occur as protective buffering system to neutralize stomach acid in an individual with gastroesophageal reflux disease.
Sialorrhea Clinical Features
- The condition leads to psychological and physical discomfort. Patient use to change numerous handkerchiefs or bibs daily.
- Chances of developing the infection to patient get increased due to drooling of saliva constantly.
- Patient use to suffer social neglect.
Sialorrhea Management
- No treatment is required in children who are less than 4 years of age.
- Oral motor training should be given for 6 months of duration before any of the surgical management should be considered.
- Biofeedback uses conditioning techniques to train the patients to swallow more frequently. It should be used in aware patients with modest drooling problem.
- Various local factors such as nasal airway obstruction, dental disease, inappropriate medicines should be eliminated.
- Anti-cholinergic drug such as atropine sulfate 0.4 mg, 4 to 6 hourly should be given. The drug reduces the amount of resting secretion, intraoral accumulation and pharyngeal-laryngeal pooling of the saliva in more than 50% of patients.
- Surgical therapy: It is carried out in patients with cognitive delay and profuse drooling as well as who fail for nonsurgical therapy. Following surgical treatments can be done:
- Relocation of duct: Mandibular and parotid ducts are relocated to tonsillar fossa which decreases salivary flow and drooling.
- Bilateral tympanic neurectomy: Sectioning the chorda tympani destruct parasympathetic innervations to the gland.
Question 8. Write short note on Stafne’s cyst.
Answer.
- It is also known as latent bone cyst or static bone cyst or lingual cortical mandibular defect.
- It occurs because of inclusion of glandular tissue adjacent to lingual surface of ramus of mandible during development.
Stafne’s cyst Clinical Features
- This is encountered during routine radiography and is asymptomatic
- Seen more commonly in males compared to females.
- It is seen commonly in the posterior area of mandible.
- At times, a depression can be felt during palpation.
Stafne’s cyst Radiographic Features
- On radiographic examination a radiolucency is seen below the mandibular canal in posterior mandible, between the molar teeth and angle of mandible.
- Lesion is well circumscribed and has sclerotic border.
- CT scans and MRI show a well-defined concavity on the lingual surface of mandible.
- Sialograms demonstrate presence of salivary gland tissue in area of defect.

Stafne’s Cyst Differential Diagnosis
- Radicular cyst: It is associated with carious tooth and radiolucency is attached to the roots of teeth.
- Residual cyst: The pre-extraction radiograph reveals tooth with evidence of deep caries.
Treatment
No treatment is required.
Question 9. Write short note on sialadenosis.
Answer. It is also known as sialosis.
Sialadenosis is the non-neoplastic and non-inflammatory enlargement of salivary gland.
Etiopathogenesis
- Sialadenosis is associated with various systemic conditions such as diabetes, cirrhosis of liver, anorexia nervosa and malnutrition.
- It is associated with neurogenic drugs such as sympathomimetic drugs and anti-hypertensive drugs.
- Above mentioned diseases and medications causes dysregulation of autonomic innervations of salivary acini leading to aberrant intercellular secretory cycle.
Sialadenosis Clinical Features
- Females are affected more as compared to males.
- Salivary gland enlargement is bilateral.
- Glands are non tender.
- Parotid gland is more commonly affected.
- Patient complains of swelling of pre-auricular area which is painless.
Radiographic Features
Sialography reveals leafless-tree appearance.
Sialadenosis Diagnosis
- Clinical diagnosis: Presence of bilateral non-inflammatory enlargement of parotid gland provide clinch to diagnosis.
- Radiological diagnosis: Presence of leafless tree appearance.
- Laboratory diagnosis: There is increase in salivary potassium and decrease in salivary sodium levels.
Sialadenosis Management
- Etiological factor should be controlled or eliminated.
- If swelling interferes with aesthetics of patient partial parotidectomy should be done.
Question 10. Classify salivary gland disorders. Write clinical features, complications and treatment plan of mumps.
Or
Classify salivary gland disorders. Describe in detail etiology, clinical features, treatment and complications of mumps.
Answer. For classification of salivary gland disorders refer to Ans 1 of same chapter.
Mumps
Etiology
Mumps spread from human to human by the airborne infection of the infected saliva or urine.
Salivary Gland Clinical Features
- It occurs at 5 to 15 years of age and boys are most commonly affected.
- It lasts for 2 to 3 weeks.
- The onset is by headache, chills, moderate fever, vomiting and pain below ear which last for one week.
- Parotid gland is most commonly involved and is bilateral. One parotid gland swells for 24 to 48 hours one after the other.
- It is followed by onset of salivary gland swelling which is firm somewhat rubbery or elastic and without purulent discharge from salivary gland duct.
- The enlargement of parotid gland causes elevation of ear lobule and produces pain on mastication especially while eating sour food.
- Papilla on opening the parotid duct is often puffy and become reddened.
Salivary Gland Complications
- Orchitis: Orchitis is the inflammation of testis and occur in adult males. It leads to male sterility.
- Pancreatitis: Inflammation of pancreas is present which leads to increase in level of serum lipase.
- Meningitis: Inflammation of meninges
- Mastoiditis
- Deafness
- Meningoencephalitis
- Myocarditis: Inflammation of myocardium
- Epididymitis
Salivary Gland Diagnosis
- Clinical diagnosis: Presence of parotitis and systemic signs of viral infections.
- Laboratory diagnosis: There is increase in salivary amylase levels. Paramyxovirus is isolated from saliva 6 days before and 99 days after the presence of salivary gland swelling.
Salivary Gland Treatment
- Most of the cases are self-limiting, with salivary gland enlargement subsiding within a week.
- Prevention with live-attenuated vaccine is best method for controlling disease.
- Vaccine is given at age of 12 to 15 months and is repeated at age of 4 to 5.
- Symptomatic treatment is given to control pain and swelling.
- Bed rest should be given to patient.
- Patient should not consume sour foods as well as sour drinks.
Question 11. Classify salivary gland diseases. Describe in detail the clinical features, investigations, differential diagnosis and management of chronic bacterial sialadenitis.
Answer. For classification of salivary glands refer to Ans 1 of same chapter.
Chronic Bacterial Sialadenitis
Chronic bacterial sialadenitis occurs due to infection produced by S. viridians, E. coli. or Proteus.
Etiology
- It occurs because of recurrent or the persistent ductal obstruction.
- Congenital stenosis, Sjogren’s syndrome, previous viral infection or allergy.
Salivary Gland Clinical Features
-
- It occurs in early childhood during age of 3 to 5 years.
- Occurrence of disease is unilateral.
- In this disease, patient complains of pain which is dull aching.
- There is presence of swelling which occur unilaterally at the angle of mandible.
- Salivary flow consists of flecks of purulent material. After some recurrences fibrosis occur in glandular parenchyma which causes decrease in salivary flow.
Salivary Gland Investigations
- In clinical examination, a dull aching pain is felt in parotid gland area with pus present at the Stensen’s duct.
- In radiographic investigations, sialogram shows dilation and multiple ectasia.
Salivary Gland Differential Diagnosis
- Viral sialadenitis: Bilateral involvement is present along with self-limiting within a week.
- Allergic sialadenitis: It is bilateral and painless
- Tuberculous lymphadenitis: Swelling is present over the neck which is tender and painful
- Pleomorphic adenoma: It occurs as a small painless nodule which increases in size.
Salivary Gland Management
- In surgical therapy, complete parotidectomy is done.
- Radiation therapy is also beneficial since it causes fibrosis of salivary gland.
- Injection of erythromycin or tetracycline is given intraductally. In this the drug is anesthetized and is cannulated and infusion of antibiotic is done at concentration of 15 mg/mL.
Question 12. Classify non-neoplastic disorders of salivary gland. Discuss chronic bacterial sialadenitis.
Answer.
Classification of Non-neoplastic Disorders of Salivary Gland
Based on Etiology
- Developmental
- Aplasia/hypoplasia
- Agenesis
- Ductal atresia
- Aberrancy
- Accessory ducts/lobes
- Polycystic disease of parotid
- Traumatic/Ischemic
- Cheilitis glandularis
- Mucocele
- Stomatitis nicotina
- Necrotizing sialometaplasia
- Infections
- Bacterial
- Acute sialadenitis
- Chronic sialadenitis
- Subacute necrotizing sialadenitis
- Actinomycosis
- Viral
- Mumps
- Cytomegalovirus
- ECHO
- Influenza
- HIV-SGD
- Fungal: Aspergillosis
- Bacterial
- Autoimmune
- Sjogren’s syndrome
- Mikulicz’s disease
- Chronic sclerosing sialadenitis
- Cysts: Lymphoepithelial cysts
- Functional
- Sialorrhoea
- Xerostomia
- Obstructive
- Sialolithiasis
- Strictures
- Endocrine: Sialosis
- Drug induced
- Chlorhexidine
- Iodine
- Phenylbutazone
- Miscellaneous
- Sarcoidosis
- Radiation damage

Leave a Reply