Diseases Of Respiratory System
Describe the clinical features and management of pulmonary embolism.
Or
Write short note on pulmonary embolism.
Or
Enumerate etiology, clinical features, investigations,complications and management of pulmonary embolism
Answer. Pulmonary embolism is the most common and fatal form of venous thromboembolism in which there is occlusion of pulmonary arterial tree by thromboemboli.
Etiology pulmonary embolism
1. Thrombotic:
- Deep vein thrombosis
- Congestive heart failure
- Rightsided endocarditis
- Atrial firillation.
Respiratory Diseases List
2. Non-thrombotic:
- Fat embolism
- Amniotic flid embolism: Spontaneous delivery and cesarean section
- Tumor embolism: Choriocarcinoma
- Parasitic embolism: Schistosomiasis
- Air embolism: Pulmonary barotraumas generally in the sea divers.
Clinical Features pulmonary embolism
In acute massive embolism, i.e. acute cor pulmonale
- Symptoms are of presence of acute dyspnea, tachypnea,tachycardia, hemoptysis and chest pain.
- Signs are increase in the jugular venous pressure, presence of central cyanosis, Loud P2 and narrow splittng of P2,an ejection systolic murmur in P2 area, right ventricular hypertrophy, signs of shock,
In small- or medium-sized pulmonary vessels embolization
- Symptoms are hemoptysis, pleuritic pain and wheeze which is the triad of pulmonary infarct.
- Signs are of pleural effusion i.e. reduced or absent chest wall movement and expansion of chest on the side involved, activity of extrarespiratory muscles is absent, position of trachea and mediastenum is shifted to opposite side, percussion note is stony dull on the side of involvement, vocal fremitus is reduced or absent on the side involved, breath sounds are absent or diminished over the area involved.
Respiratory Diseases List
In multiple microembolization, i.e. chronic cor pulmonale
- Symptoms are of presence of dyspnea, weakness, fatigue and syncope.
- Signs are increase in the jugular venous pressure, presence of cyanosis, edema, hepatomegaly, presence of loud P2 with the ejection systolic murmur in P2 area, presence of narrow splittng of P2, presence of parasternal heave and right ventricular atrophy.
Diagnosis pulmonary embolism
It is in the patients who had suspicion for underlying cause for emboli formation, development of pulmonary sign and symptoms as well as cardiovascular involvement, presence of thrombophlebitis in deep leg veins, prolonged bed rest, immobilization, cardiac irregularity in form of atrial firillation should be considered while keeping in mind clinical picture of precordial pain, breathlessness and tachycardia in patient who had recently gone for major surgery. Examination of veins is mandatory in the patients who are at high risk for development of deep vein thrombosis.
These features along with investigatory features form the diagnosis. Following are the investigations:
Investigations pulmonary embolism
- Blood examination: If pulmonary infarct is present, there can be leucocytosis or raised ESR.
- Chest X-ray: In massive pulmonary embolism, there is presence of diffse infitrates in the lung with increased bronchovascular markings.
If medium size vessels are involved, there will be triangular pleuropulmonary opacity in peripheral lung filds, there can also be pleural effsion present. - Arterial blood gas analysis: Presence of hypoxemia and hypocapnia.
- D-dimer: It is a fibrin degradation product release in circulation in pulmonary embolism.
Presence of high levels of Ddimer is suggestive of an embolism while presence of low Ddimer exclude pulmonary embolism. - Echocardiography: It shows the right ventricular dilatation and presence of clot in it.
- Spiral CT scan: CT of chest along with the IV contrast diagnose the pulmonary embolism.
It effctively diagnose the large and central pulmonary embolism.
Newer scanners can also detect peripherally present emboli. - Pulmonary angiography: It demonstrates the site of obstruction of all sized blood vessels.
Complications pulmonary embolism
- The foremost complication for pulmonary embolism is pulmonary hypertension.
- Rightsided heart failure
- Peripheral segmental infarctions.
Respiratory Diseases List
Management pulmonary embolism
1. In patient of massive embolism
1. If patient is in state of shock or collapse:
- Vasopressors such as dopamine or dobutamine are to be given.
- Administer oxygen to the patient.
- Correct acidosis
- If there is failure of an initial resuscitation or there is hypotension or right ventricular dysfunction,primary therapy should be administered,i.e. dissociation of clot by thrombolysis or embolectomy.
2. If acute event is survived by the patient,
- Streptokinase 2.5–5 lac unit IV > in dextrose or saline is given for 30 min followed by 1 lac IV for 24 hours.
- Recombinant tissue plasminogen activator tPA, i.e. Alteplase 100mg for 2 hours is a good alternative to thrombolytic therapy.
3. Anti coagulation therapy is an initial and immediate treatment of choice.
- Loading dose of 80–150 units/kg is given which is followed by 15 to 18 units/kg/hr as continuous infusion.
- Warfarin should be added to heparin and is continued for 5 days.
- After 5 days taper the heparin and administer warferin for 6 weeks to 6 months.
- Monitor anticoagulant therapy by PTT or INR ratio or bleeding time which should be 2–3 times than the control.
Respiratory Disease Symptoms
4. In small embolisms
- Analgesics, i.e. NSAIDs should be given to relieve the pain.
- Anticoagulant is given to prevent further embolization.
- Various preventive measures should be undertaken such as calf muscle exercise, elastic stockings, prolong immobilization at bed, respiration exercises should be done.
Write short note on tropical eosinophilia.
Answer. Tropical eosinophilia: A disease of tropical countries (India,Pakistan, Bangladesh, Sri Lanka, etc.) is characterized by chronic cough, attck of breathlessness, lassitude and weight loss with rise in eosinophilic count in blood.
Etiology
The most important cause of tropical eosinophilia is allergic reaction to fiarial worm, e.g. Wuchereria bancrofti.
Pathology
Patients having tropical eosinophilia lack IgG blocking antibodies against the circulating microfilaria. Microfilaria is removed from peripheral circulation and is trapped in various tissue sites by IgG dependent cell-mediated effctor mechanism.
Antigens are released as parasites get destroyed which initiates
Type I hypersensitivity reaction. Peripheral eosinophilia occurs due to a reaction which further progress to granuloma and firosis.
Respiratory Disease Symptoms
Clinical Features tropical eosinophilia.
- Chronic cough of several weeks or months duration is the prominent complaint.
- Cough may be dry or mucoid to mucopurulent
- There is constricting sensation in the chest.
- Patient suffrs from general *debility, weight loss, low grade fever and malaise.
- Presence of lymphadenopathy and splenomegaly
- Nocturnal bronchospasm
Diagnosis tropical eosinophilia.
- Positive history for prolong presence of patient in endemic area.
- Lacking of microfiaria in blood, in both night as well as day samples.
- Presence of high titers of fiarial antibodies.
- IgE levels are 1000 units/mL.
- Peripheral eosinophilia with 3000 cells/mL.
Treatment tropical eosinophilia.
- The drug of choice is diethyl carbamazine given in dose of 5 mg / kg body weight for 2 weeks
- In adult dosage, three tab of 50 mg four times a day for 5 days.
- In addition patient will require bronchodilators to relieve the bronchospasm.
- Corticosteroids and antihistaminics are employed.
- Recovery after therapy is good.
- Repeat course of drug may have to be given after six weeks.
Question. Outline the clinical features of empyema.
Answer. Empyema means the presence of pus in the pleural cavity.
Clinical Features Of Acute Empyema
Symptoms
- Those of primary disease: Imperfect recovery in pneumonic cases, or sudden increase in fever with rigors.
- Those due to mechanical effct: Pleuritic chest pain in early stage, dyspnea, cough and sputum.
- Those due to toxemia: Malaise, anorexia, sweats and loss of weight.
Respiratory Disease Symptoms
Signs clinical features of empyema.
1. Same as pleural effsion, i.e.
1. On inspection:
- Presence of bilaterally symmetrical chest.
- Restrictions of movements of chest on the side of effsion.
2. On palpation:
- Shifting of trachea and mediastinum to opposite side on pushing.
- Diminishing of expansion of chest on involved side.
- Absence of vocal fremitus on involved side.
3. On percussion:
Stony dull percussion note on the involved side.
4. On auscultation:
- Absence of breath sounds or diminishing of breath sounds over area of pleural effsion.
- Amphoric bronchial breathing can be heard at apex of pleural effsion at interscapular region over the involved side.
- Absence of vocal resonance.
5. Sometimes edema of chest wall is present.
6. Finger clubbing can develop within 2 to 3 weeks of onset.
Respiratory Disease Symptoms
Clinical Features of chronic empyema
- Recurrent symptoms of chest pain and fever.
- Loss of weight and anemia.
- Clubbing of figers.
- Chest wall deformity from firosis.
- Chronic sinus tracts into the skin or lungs may develop.
- When bronchopleural fitula is present, air can be heard (or felt) blowing through a patent sinus during coughing.
Question. Write short note on chronic bronchitis.
Answer. Chronic bronchitis may be defied as a “condition where there is persistent productive cough for at least three consecutive months in at least two consecutive years”.
Etiology chronic bronchitis.
- Cigarett smoking
- Air pollution and clinical factors
- Infections, i.e. upper respiratory tract infection in smokers
- Occupation
- Familial and genetic factors
- Alpha-1 antitrypsin defiiency.
clinical Features chronic bronchitis.
Symptoms
- It affcts male more commonly than the females
- Chronic bronchitis is present with recurrent attcks of cough
- Cough may occur in paroxysms or is more in elderly hours of morning.
- Cough is dry when start but later sputum is bringing out which is mucoid to mucopurulent sometimes, it is blood tinged.
- Patient complains sense of tightness in chest, breathlessness and asthmalike picture.
- Fever and toxemia appear when infection supervenes
Signs chronic bronchitis.
- There is increase in respiratory rate.
- Inspiratory and expiratory ronchi and presence of crepitation at the base of lungs.
Investigation chronic bronchitis.
1. X-ray: In early stage, it is normal and later it shows widening of intercostal spaces, ribs placed more horizontally,diaphragm displaced downwards and some patient shows patches of pneumonia.
2. Sputum for culture and sensitivity test is usually sterile.
3. Lung function tests:
- Decrease in FEV1
- Subnormal FEV1/VC
- Decrease in PEF
- Normal lung volumes except with emphysema
- Normal diffsing capacity.
4. Blood gas analysis: In severe cases, there is increase in
hypercapnia and decrease in hypoxaemia.
Management chronic bronchitis.
1. Bronchial irritants should be avoided, i.e.
- Smoking should be strictly stopped.
- Passive smoking is stopped.
- Gas smoke is avoided by housemakers.
- Aerosols such as hair spray, insecticide spray and aerosols should be avoided.
- Polluted atmosphere should be strictly avoided.
2. Treatment ofan infection:
- Ampicillin 250–500 mg every 6 hourly is given for 5 to 7 days.
- Cotrimazole 960 mg can be given as BD dose.
- Antibiotics should be given till purulent mucous become mucoid.
- If necessary modify antibiotics as per culture and sensitivity test.
3. Bronchodilators:
- In mildtomoderate chronic bronchitis oral theophylline 150 mg BD or inhaled salbutamol 200 μg 6 hourly can be given.
- In severe bronchitis, ipratropium bromide 40–80mcg 6 hourly is added.
4. Mucolytic agents: Bromhexine and carbocystein are to be given.
5. Corticosteroids: Prednisolone 30 mg/day for 2 weeks is given. If improvement occur by oral steroids, they are replaced by inhalational steroids.
6. Domiciliary oxygen therapy: Longterm oxygen therapy in low concentration i.e. 2 L/min by nasal cannula is given to reverse or to delay development of pulmonary hypertension.
Causes Of Respiratory Diseases
Question. Write short note on chemotherapy of pulmonary tuberculosis.
Answer.
Chemotherapy of pulmonary tuberculosis.
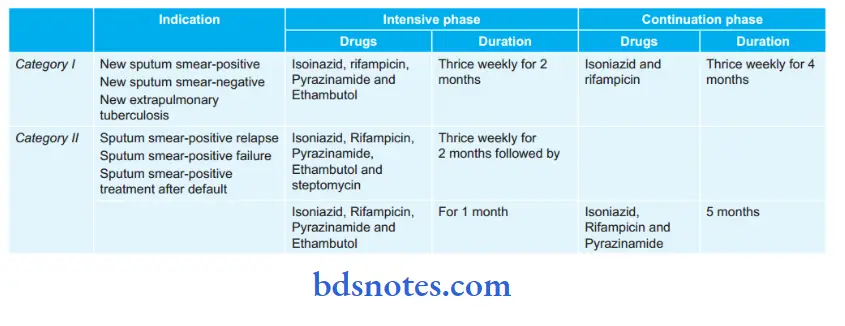
Drugs for primary chemotherapy (First line anti-tubercular drugs)
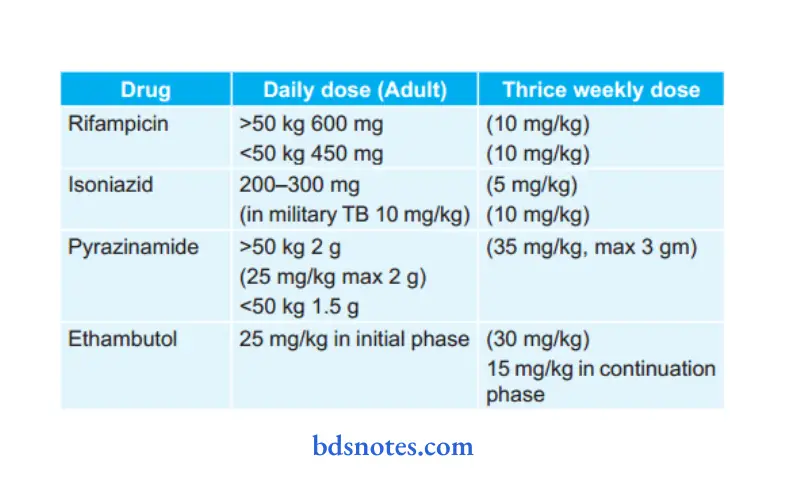
under dots following treatment regimen is used
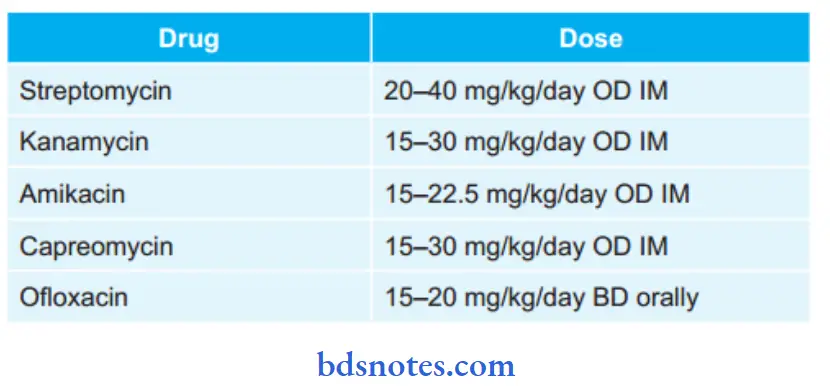
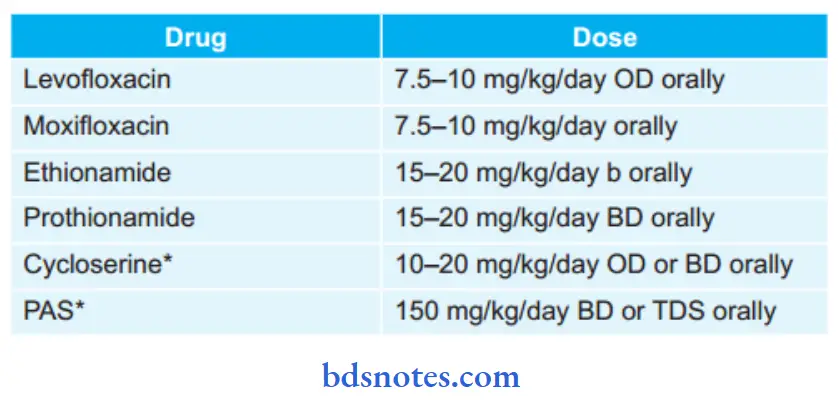
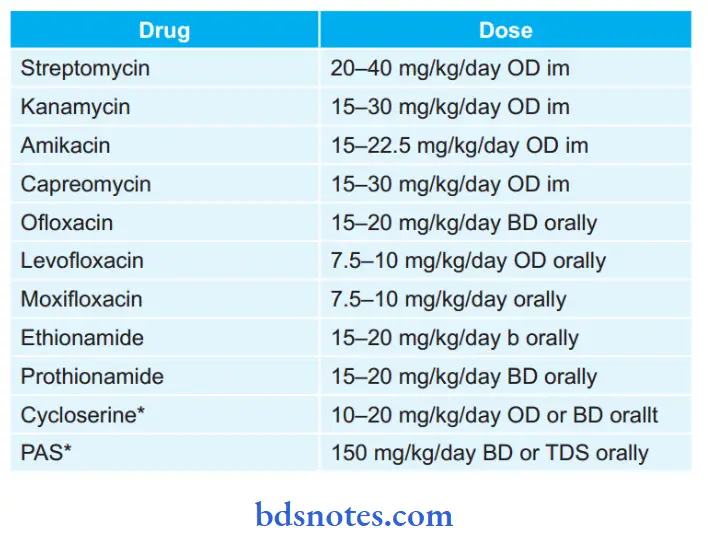
second-line antituberculous drugs
Treatment regimen under rntcP for Mdr-tB (Multidrug-resistant tB) and Xdr—tB (extensively drug
resistant tB)
1. For MDR-TB:
- Six drugs in intensive phase for 6-9 months: Kanamycin,
- Levoflxacin, Ethionamide, Cycloserine, Pyrazinamide and Ethambutol.
- Four drugs in continuation phase for 18 months:
Levofloxacin, Ethionamide, Cycloserine and
Ethambutol. - Reserve drug is paminosalicylic acid.
2. For XDR-TB
- Seven drugs in intensive phase for 6-12 months:
Capreomycin, p-aminosalicylic acid, Moxiflxacin,highdose Isoniazid, Clofazimine, Linezolid,
Amoxicillin and Clavulinic acid. - Six drugs in continuation phase for 18 months:
paminosalicylic acid, Moxifloxacin, high dose lsoniazid, Clofazimine, Linezolid, Amoxicillin and Clavulinic acid. - Reserve drugs: Clarithromycin, Thiacetazone
Causes Of Respiratory Diseases
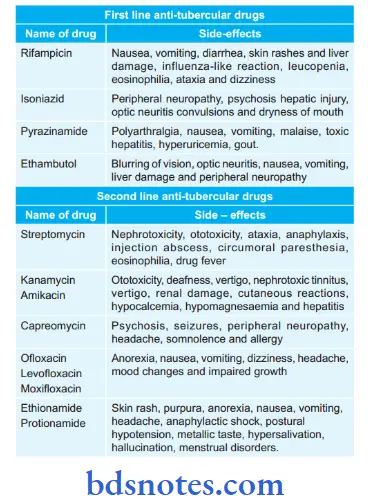
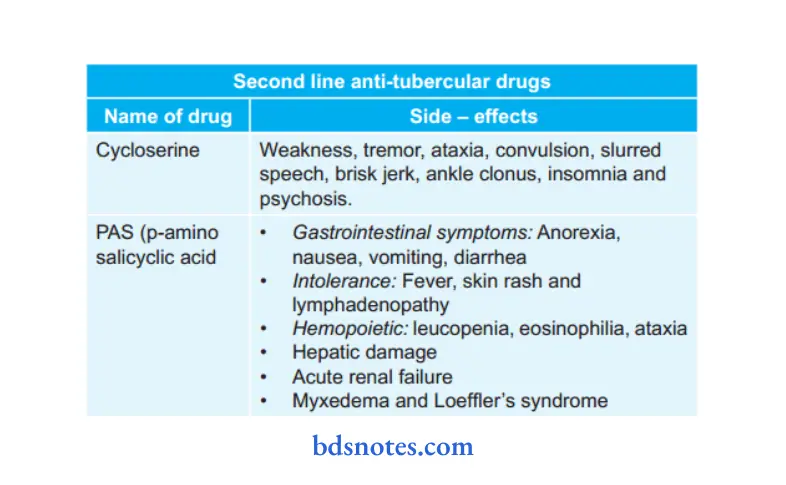
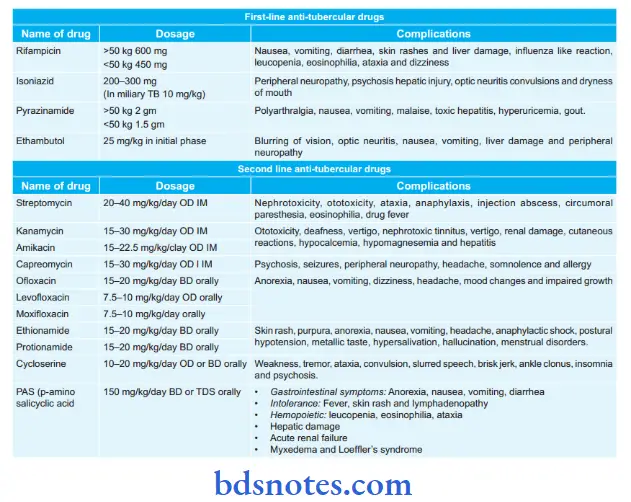
Question. Write short note on side effects of antitubercular drugs.
Answer.
Question. Write short note on rifampicin.
Answer. Rifampicin is a macrolide antimicrobial drug.
It has good sterilizing and resistance preventing actions.
- Rifampicin inhibits DNA dependent RNA polymerase thus stopping the expression of bacterial genes.
- It is bactericidal to M. tuberculosis and many other grampositive and negative bacteria.
Side Effects rifampicin.
- Liver damage
- Inflenza-like reaction
- Intolerance: Fever, skin rash, diarrhea, leucopenia,eosinophilia, ataxia and dizziness.
- Orange to red color of urine, feces and sputum.
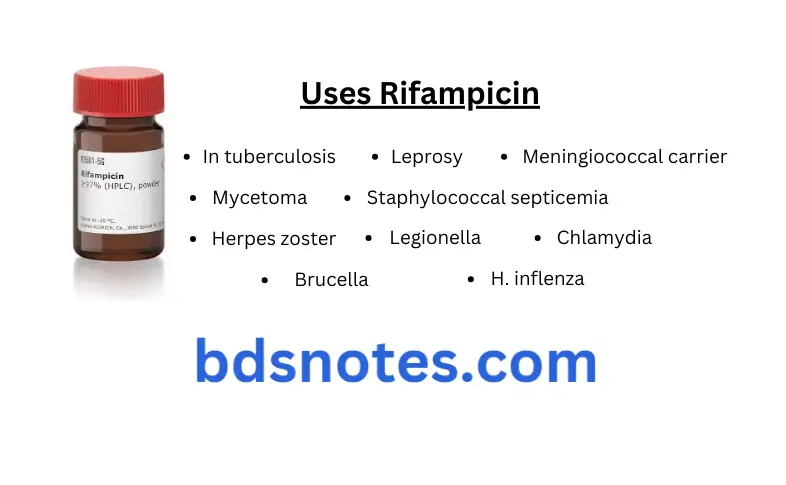
Uses rifampicin.
- In tuberculosis
- Leprosy
- Meningiococcal carrier
- Staphylococcal septicemia
- Herpes zoster
- H. inflenza
- Brucella
- Mycetoma
- Legionella
- Chlamydia
Causes Of Respiratory Diseases
Question. Write short note on nosocomial pneumonia.
Answer. Nosocomial pneumonia is defied as hospital acquired pneumonia.
- It is the secondary pneumonia.
- Pneumonias developing in hospital in a patient who has been admittd for more than 48 hours should be considered to be nosocomial rather than community acquired.
- Because of change of oropharyngeal flra in hospitalized patients, it is caused by anaerobic gramnegative organism like E. coli, Klebsiella pneumoniae, Pseudomonas, more frequent. Staphylococcus aureus, pneumococci and H. influenza are less frequent causative organisms.
Factors Predisposing for nosocomial Pneumonia
1. Reduced host defenses against bacteria:
- Reduced immune defenses (e.g. corticosteroid treatment, diabetes,malignancy)
- Reduced cough reflx (e.g. post-operative)
- Disordered mucociliary clearance (e.g. anesthetic agents)
- Bulbar or vocal cord palsy
2. Aspiration ofnasopharyngeal or gastric secretions:
Immobility or reduced conscious level
Vomiting, dysphagia, achalasia or severe reflx
Nasogastric intubation
3. Bacteria introduced in to lower respiratory tract:
- Endotracheal intubation/tracheostomy
- Infected ventilators/nebulizers/bronchoscopes
- Dental or sinus infection
4. Bacteremia:
- Abdominal sepsis
- Intravenous cannula infection
- Infected emboli
Treatment rifampicin.
- In mild cases amoxicillin with clavulanic acid 500mg TDS is given.
- In severe cases I.V. cefuroxime 750mg every 8 hourly + Clarithromycin 250mg every 8 hourly is given.
- Most of the patients require ventilatory support and also need supplemental oxygen therapy.
Question. Write short note on aspiration pneumonia.
Answer. Aspiration pneumonia is also known as suppurative pneumonia.
Aspiration pneumonia is the consolidation of lung in which there is continued destruction of parenchyma by inflammatory cells which causes formation of microabscess.
Etiology
Aspiration pneumonia is caused by Staphylococcus aureus,Sterptococcal pneumonia, Streptococcus pyogens, Hemophilus inflenza as well as various other anaerobic bacterias.
Clinical Features aspiration pneumonia.
Symptoms aspiration pneumonia.
- Aspiration pneumonia occurs mostly on the right side as compared to left side.
- Patient complaints of high fever, cough and dyspnea.
- During coughing copious foulsmelling sputum is present,which is blood stained too.
- There is presence of tachycardia and restlessness.
- Weight loss is too rapid.
- There is also presence of perspiration.
Signs aspiration pneumonia.
- Signs of lung consolidation are seen.
- If there is formation of lung abscess, cavitation can be felt.
- There is presence of pleural rub.
- Digital clubbing is also well appreciated.
Causes Of Respiratory Diseases
Investigations aspiration pneumonia.
- TLC and DLC should be carried out for checking neutrophilic leucocytosis.
- ESR is high.
- Chest X-ray: It shows a homogeneous opacity. If there is presence of flid in the opacity, this indicates of an abscess.
- Culture ofsputum is carried out to identify microorganisms.
Treatment aspiration pneumonia.
- In aerobic infection ampicillin 500 mg QID or amoxicillin 500 mg TID or cotrimoxazole 960 mg BD orally provides relief.
- In anaerobic infection metronidazole 400 mg TID orally is added.
- Antibiotics should be prescribed based on the culture and sensitivity testing.
- Treatment should be continued for 10 to 15 days.
- NSAIDs should be given for pain relief.
- In subjects with lung abscess physiotherapy and postural drainage is done.
Complications aspiration pneumonia.
- Amyloidosis
- Empyema
- Bronchiectasis
- Septicemia
- Pulmonary firosis.
Question. Mention complications of pulmonary tuberculosis.
Answer. The complications of pulmonary tuberculosis are as follows:
1. Early complications
- Pneumonia
- Empyema
- Hemoptysis
- Laryngitis
- Pneumothorax.
2. Late complications
- Bronchiectasis
- Mycetomas in cavity
- Colonizationoffiroticlungwithnontuberculous
- Mycobacterium
- Nonrespiratory disease, i.e. genitourinary, bone.
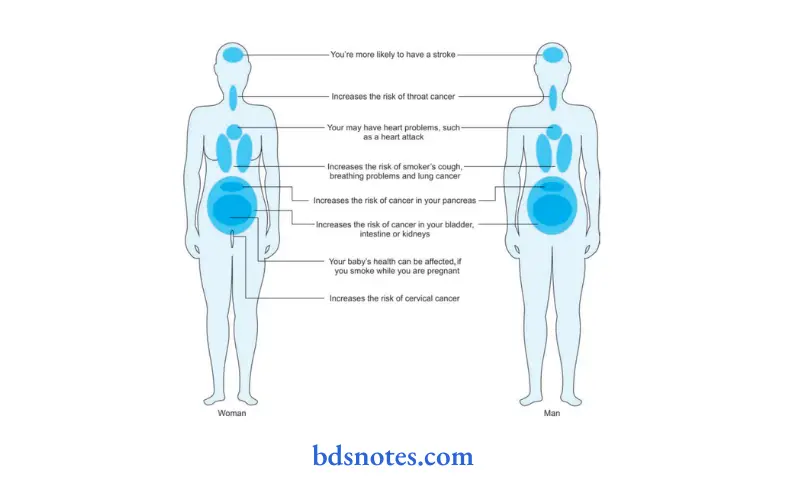
Question. Write short note on smoking-related disorder.
Answer. The incidence of smokingrelated diseases is greater in younger than in older smokers, particularly for coronary artery disease and smokers.
- Cardiovascular disease
- Cigarett smokers are more likely than nonsmokers to develop large vessel atherosclerosis as well as small vessel disease.
- Cigarette smoking also increases likelihood of myocardial infarction and sudden cardiac death.
Smoking-Related Disorder Cancer
Tobacco smoking causes cancer of lung, oral cavity,, nose,oro and hypopharynx, nasal cavity and paranasal sinuses,larynx, esophagus, stomach, pancreas, liver, kidney, ureter,urinary bladder and uterine cervix and also causes myeloid leukemia.
Smoking-Related Disorder Respiratory Disease
Cigarett smoking is responsible for 90% of COPD within 1–2 years of beginning of smoke regularly.
Many smokers will develop inflmmatory changes in small airway due to there is reduced expiratory airflw.
Other Conditions
Smoking delays healing of peptic ulcer, increases risk of
osteoporosis, senile cataract, macular degeneration, premature
menopause, wrinkling in skin, gallstone, male impotence and
cholecystitis in women.
Question. Write short note on bronchitis.
Answer. Bronchitis is the infection of the bronchi.
Types:
1. Acute bronchitis.
2. Chronic bronchitis.
Acute Bronchitis
It is an acute infection of the bronchi and may be caused by the infection with organisms such as Streptococcus, pneumococci, Hemophilus inflenza or primarily viral in origin.
Causes Acute Bronchitis
- Infection: Bacterial or viral, or descending infection from nasal sinus or throat.
- Complicating other diseases such as: measles and whooping cough.
- Physical and chemical irritants: Inhaled dust, steam, gases such as sulphur dioxide and ether.
Symptoms Acute Bronchitis
- Toxemia: Malaise, fever, ill health, tachycardia
- Irritative: Cough with expectoration, at fist scanty viscid sputum is present and later on it become more copious and mucopurulent; substernal pain or raw sensation under sternum.
- Obstructive: Chocked up feeling, paroxysms of dyspnea following spells of coughing relieved with expectoration.
Physical signs Acute Bronchitis
Fever, tachycardia, flshing of face, respiratory rate is slightly increased. Crepitations are heared at the base when secretions collect in the lungs.
Treatment Acute Bronchitis
1. In dry stage:
- Bed rest
- Nutritious diet
- Tincture benzoin inhalation
- Application of vicks vaporub on chest
- Capsule amoxicillin 250 mg 8 hourly for 4 to 5 days.
- Tablet aspirin or paracetamol twice a day.
- Cough sedative mixture like linctus codeine to suppress dry cough.
2. In moist stage:
- Amoxicillin and cloxacillin 500 mg 8 hourly for 4 to 5 days.
- Expectorant mixture with sodium or potassium iodide to bring out the secretions.
Chronic Bronchitis
Chronic bronchitis may be defied as a “condition where there is persistent productive cough for at least three consecutive months in at least two consecutive years”.
Etiology chronic bronchitis.
- Cigarett smoking
- Air pollution and clinical factors
- Infections, i.e. upper respiratory tract infection in smokers
- Occupation
- Familial and genetic factors
- Alpha-1 antitrypsin defiiency.
clinical Features chronic bronchitis.
Symptoms
- It affcts male more commonly than the females
- Chronic bronchitis is present with recurrent attcks of cough
- Cough may occur in paroxysms or is more in elderly hours of morning.
- Cough is dry when start but later sputum is bringing out which is mucoid to mucopurulent sometimes, it is blood tinged.
- Patient complains sense of tightness in chest, breathlessness and asthmalike picture.
- Fever and toxemia appear when infection supervenes
Signs chronic bronchitis.
- There is increase in respiratory rate.
- Inspiratory and expiratory ronchi and presence of crepitation at the base of lungs.
Investigation chronic bronchitis.
1. X-ray: In early stage, it is normal and later it shows widening of intercostal spaces, ribs placed more horizontally,diaphragm displaced downwards and some patient shows patches of pneumonia.
2. Sputum for culture and sensitivity test is usually sterile.
3. Lung function tests:
- Decrease in FEV1
- Subnormal FEV1/VC
- Decrease in PEF
- Normal lung volumes except with emphysema
- Normal diffsing capacity.
4. Blood gas analysis: In severe cases, there is increase in
hypercapnia and decrease in hypoxaemia.
Management chronic bronchitis.
1. Bronchial irritants should be avoided, i.e.
- Smoking should be strictly stopped.
- Passive smoking is stopped.
- Gas smoke is avoided by housemakers.
- Aerosols such as hair spray, insecticide spray and aerosols should be avoided.
- Polluted atmosphere should be strictly avoided.
2. Treatment ofan infection:
- Ampicillin 250–500 mg every 6 hourly is given for 5 to 7 days.
- Cotrimazole 960 mg can be given as BD dose.
- Antibiotics should be given till purulent mucous become mucoid.
- If necessary modify antibiotics as per culture and sensitivity test.
3. Bronchodilators:
- In mildtomoderate chronic bronchitis oral theophylline 150 mg BD or inhaled salbutamol 200 μg 6 hourly can be given.
- In severe bronchitis, ipratropium bromide 40–80mcg 6 hourly is added.
4. Mucolytic agents: Bromhexine and carbocystein are to be given.
5. Corticosteroids: Prednisolone 30 mg/day for 2 weeks is given. If improvement occur by oral steroids, they are replaced by inhalational steroids.
6. Domiciliary oxygen therapy: Longterm oxygen therapy in low concentration i.e. 2 L/min by nasal cannula is given to reverse or to delay development of pulmonary hypertension.
Question. Write short note on pneumococcal pneumonia.
Answer. It is caused by streptococcal pneumonia.
It is characterized by homogeneous consolidation of one lobe or more lobes or segments of a lung, hence, called lobar pneumonia
Clinical Features pneumococcal pneumonia.
- It occurs at all ages but is common in early and adult life. It is most common bacterial pneumonia following an upper respiratory tract infection. It is usually a sporadic disease,common in winter and spreads by droplet infection.
- In children, the onset is sudden often with fever, chills and rigors, vomiting and convulsions. In adults, the onset is with fever, chills, cough, breathlessness and chest pain.
- Shaking chills and rigors
- Loss of apatite body ache and headache
- Hemoptysis and weakness
- The physical signs during an early stage of illness show decreased respiratory movements, impairment of percussion note, diminished breath sounds and often a pleural rub on the affcted side.
- Later on, usually after 3 days, signs of consolidation appear.
- During resolution, numerous coarse crackles crepitations are heard, indicating the liquefaction of alveolar exudate.
pneumococcal pneumonia Investigations
- Blood test: It reveals marked neutrophil leucocytosis.
- Blood culture: It shows the presence of Streptococcus pneumonia.
- Examination of sputum: Gram staining of sputum may demonstrate pneumococci.
- Chest radiograph: In pneumococcal pneumonia, a homogeneous opacity is seen localized to the affcted lobe or segment which appears within 12–18 hours from onset of illness.
- Serological test: It can detect pneumococcal antigen in the serum.
- In some of the cases, fieroptic, bronchoscopic aspiration or transthoracic needle aspiration is required.
Complications pneumococcal pneumonia.
1. Pulmonary:
- Parapneumonic pleural effsion
- Emphysema
- Suppurative pneumonia or lung abscess
- Acute respiratory distress syndrome
- Pneumothorax
2. Extra pulmonary
- Hepatitis, pericarditis, meningioencephalitis
- Multiorgan failure
- Ectopic abscess formation
Management pneumococcal pneumonia.
- Initially, oral amoxicillin should be given 500 mg 8 hourly or erythromycin 500 mg 6 hourly.
- If patient is very ill or gram negative or staphylococcal infection is present IV ampicillin 0.5–1g 6 hourly + flcoxacillin 250–500 mg IV 6 hourly + gentamicin 60–80 mg every 8 hourly IV is given.
- Antibiotic therapy should be given for 7–10 days.
- Choice of antib iotic depends on the causative microorganisms.
- Oxygen therapy is given in seriously ill patients. Oxygen should be delivered at very high rate.
- Analgesics such as mefenamic acid 250–500 mg or pethidine 50–100 mg or morphine 10–15 mg IM or IV injections should be given.
- Physiotherapy is given to patient by encouraging him to cough and to take deep breath as pleuritic pain disappears.
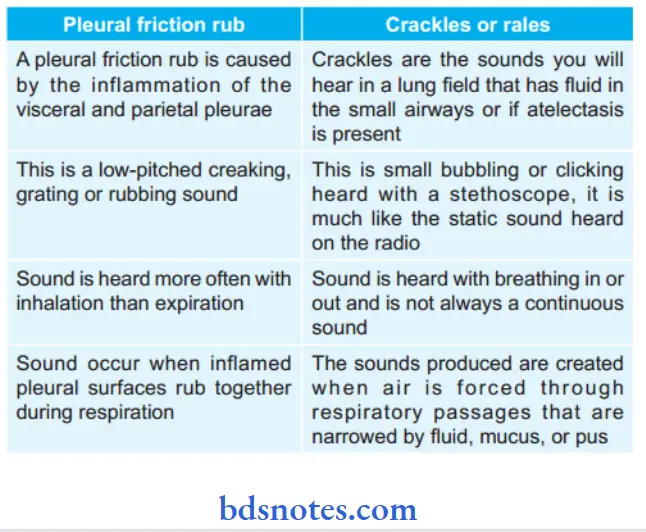
Question .Diffrentiate between pleural friction rub and crackles or rales.
Answer.
Question. Write short note on primary tuberculosis and its investigations.
Answer. Primary tuberculosis is the fist lesion which develops in a previously unexposed nonsensitized individual irrespective of the age.
Pathology
- Reinfection of a sensitized person or reactivation of a primary dormant lesion is called secondary or postprimary tuberculosis.
- The initial lesion after ingestion of tubercle bacilli which mainly occurs in the lungs constitutes primary tuberculosis.
- It commonly involves children and is in the form of subpleural lesion either in the lower part of upper lobe or upper part of lower lobe.
- The initial entry of the bacilli initiates nonspecific inflammatory response which hardly produces any symptoms. Bacilli are transported to regional lymph nodes and parenchymal lesion in the lungs (Ghon Focus) along with enlarged lymph nodes which may calcify over a period of time and this constitutes primary complex (Ghon’s complex).
- A case of primary tuberculosis draws attntion when a child may present with a nonspecifi pneumonia or bronchial obstruction because of enlarged hilar gland or low-grade fever with pleural effsion.
- Primary complex heals leaving a calcifid lesion.
- Bacilli may remain for years and may become reactivated when body’s immunity falls as in malnutrition, debilitating disease and following severe form of measles, whooping cough.
Clinical Features primary tuberculosis
As tuberculosis remains symptomfree and is diagnosed on routine radiography.
Symptoms primary tuberculosis
- Evening rise of temperature
- Night sweats
- Malaise and cachexia
- Irritability and diffilty in concentration.
- Cough and expectoration for more than three weeks.
- Pleuritic chest pain
- Breathlessness is the feature of advanced disease.
- Indigestion and dyspnea
- Amenorrhea often in young women
- Hoarseness of voice.
- Sputum can be mucoid, purulent or blood stained.
- Hemoptysis is a classical feature
- Presence of localized wheeze from local ulcer or narrowing of major bronchus.
- Presence of recurrent cold.
Physical signs primary tuberculosis
- Fever and weight loss
- Tachycardia and tachypnea
- Rapid pulse rate
- Physical signs of collapse, consolidation, cavitation, firosis, bronchiectasis, pleural effsion or pneumothorax.
- In some cases, only localized *rhonchi or rales are present.
- Clubbing of figers is present in chronic disease.
- Most common physical sign of chest is fie crepitation in the upper part of one or both the lungs. This is heard on taking a deep breath after coughing.
- Later on, there can be presence of dullness to percussion or bronchial breathing in upper part of one or both the lungs.
- In chronic cases there is evidence of volume loss and mediastinal shift.
- Hilar, mediastinal and cervical groups lymph nodes are enlarged with splenomegaly.
Investigations primary tuberculosis
- Sputum examination (for acid fast bacilli): By direct smear
examination (ZiehlNeelsen stain). At least, three smears must be examined before fially reaching a conclusion.
When direct smear is negative, sputum examination be done by concentration method using 24 hours collection of sputum. Further confimation is done by sputum culture by animal inoculation which takes 4–8 weeks. If adequate amount of sputum is not available, bronchoscopic
aspiration of secretions be made and submittd for smear and culture examination. - Serology: In this ELISA, technique is used which helpful in diagnosis of tuberculosis in children. PCR technique is more specifi and sensitive serological test than ELISA,but PCR is less used due to its high cost.
- Chest X-ray: Presence of multiple nodular infitrations or ill-defied opacities in one of upper lobes is characteristic for pulmonary tuberculosis. An area of translucency in radiopacities is indicative of cavitation. Presence of cavity is indicative of an active lesion. In some of the patients multiple thickwalled cavities can be seen. At the time of firosis, trachea and mediastinum shift to same side.
Fibrosis can also cause calcifiation - Pathological tests:
- Blood examination: Peripheral blood examination shows monocytosis, i.e. 8 to 12%
- ESR is elevated.
- Tuberculin test: It is a test to recognize prior tubercular infection, and is done by injecting one unit of purifid protein derivative (PPD) on the forearm and readings taken after 48 hours. Induration of more than l5 mm indicates a positive test. The younger is the patient, greater is signifiance of positive test. A negative test does not always exclude tubercular infection since it may be negative in patients of blood malignancies,malnourishment and those on immunosuppressive therapy. Tuberculin test is nonspecific and only indicates prior infection. Its sensitivity wanes with age.
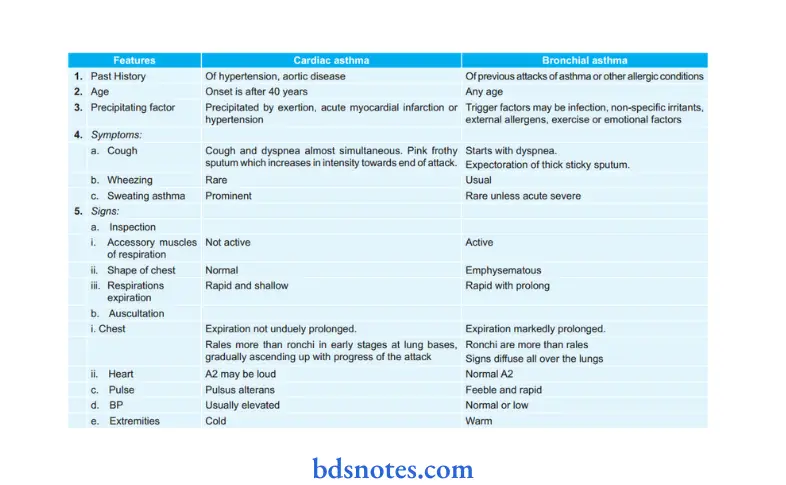
Question. Write diffrence between bronchial and cardiac asthma.
Answer.
Question. Enumerate antitubercular drugs—its dosage and complications.
Answer.
Question. Discuss etiology, clinical features, diagnosis and outline the management of acute pulmonary embolism.
Or
Write short note on acute pulmonary embolism.
Answer.
Etiology pulmonary embolism.
1. Thrombotic:
- Deep vein thrombosis
- Congestive heart failure
- Rightsided endocarditis
- Atrial firillation.
2. Non-thrombotic:
- Fat embolism
- Amniotic flid embolism: spontaneous delivery and caesarean section
- Tumor embolism: Choriocarcinoma
- Parasitic embolism: Schistosomiasis
- Air embolism: Pulmonary barotraumas generally in the sea divers
Clinical Features pulmonary embolism.
- In acute massive embolism, i.e. acute cor pulmonale
- Symptoms are of presence of acute dyspnea, tachypnea,tachycardia, hemoptysis and chest pain.
Signs are increased in the jugular venous pressure, presence of central cyanosis, Loud P2 and narrow splittng of P2,an ejection systolic murmur in P2 area, right ventricular hypertrophy, signs of shock,
In small or mediumsized pulmonary vessels embolization
- Symptoms are hemoptysis, pleuritic pain and wheeze which is the triad of pulmonary infarct.
- Signs are of pleural effusion, i.e. reduced or absent chest wall movement and expansion of chest on the side involved, activity of extrarespiratory muscles is absent, position of trachea and mediastenum is shifted to opposite side, percussion note is stony dull on the side of involvement, vocal fremitus is reduced or absent on the side involved, breath sounds are absent or diminished over the area involved.
Diagnosis pulmonary embolism.
It is in the patients who had suspicion for underlying cause for emboli formation, development of pulmonary sign and symptoms as well as cardiovascular involvement, presence of thrombophlebitis in deep leg veins, prolonged bed rest, immobilization, cardiac irregularity in form of atrial firillation should be considered while keeping in mind clinical picture of precordial pain, breathlessness and tachycardia in patient who had recently gone for major surgery.
Examination of veins is mandatory in the patients who are at high risk for development of deep vein thrombosis.
These features along with investigatory features form the diagnosis. Following are the investigations:
Investigations pulmonary embolism.
- Blood examination: If pulmonary infarct is present there can be leucocytosis or raised ESR.
- Chest X-ray: In massive pulmonary embolism, there is presence of diffse infitrates in the lung with increased bronchovascular markings.
If medium size vessels are involved, there will be triangular pleuropulmonary opacity in peripheral lung filds, there can also be pleural effsion present. - Arterial blood gas analysis: Presence of hypoxemia and hypocapnia.
- D-dimer: It is a fibrin degradation product release in circulation in pulmonary embolism.
Presence of high levels of Ddimer is suggestive of an embolism while presence of low Ddimer exclude pulmonary embolism. - Echocardiography: It shows the right ventricular dilatation and presence of clot in it.
- Spiral CT scan: CT of chest along with the IV contrast diagnose the pulmonary embolism.
It effctively diagnose the large and central pulmonary embolism.
Newer scanners can also detect peripherally present emboli. - Pulmonary angiography: It demonstrates the site of obstruction of all sized blood vessels.
Management pulmonary embolism.
1. In patient of massive embolism
1. If patient is in state ofshock or collapse:
- Vasopressors such as dopamine or dobutamine are to be given.
- Administer oxygen to the patient.
- Correct acidosis
- If there is failure of an initial resuscitation, or there is hypotension or right ventricular dysfunction,primary therapy should be administered,
i.e. dissociation of clot by thrombolysis or embolectomy.
2. If acute event is survived by the patient:
- Streptokinase 2.5–5 lac unit I.V> in dextrose or saline is given for 30 min followed by 1 lac IV for 24 hours.
- Recombinant tissue plasminogen activator tPA i.e.
Alteplase 100 mg for 2 hours is a good alternative to thrombolytic therapy.
3. Anticoagulation therapy is an initial and immediate
Treatment Of Choice:
- Loading dose of 80–150 units/kg is given which is followed by 15–18 units/kg/hr as continuous infusion.
- Warfarin should be added to heparin and is continued for 5 days.
- After 5 days, taper the heparin and administer warfarin for 6 weeks to 6 months.
- Monitor anticoagulant therapy by PTT or INR ratio or bleeding time which should be 2 to 3 times than the control.
2. In small embolisms
- Analgesics, i.e. NSAIDs should be given to relieve the pain.
- Anticoagulant is given to prevent further embolization.
- Various preventive measures should be undertaken such as calf muscle exercise, elastic stockings, prolong immobilization at bed, respiration exercises should be done.
Question. Write on RNTCP classifiation of tuberculosis.
Answer. RNTCP or the Revised National Tuberculosis Control Program is the staterun tuberculosis control initiative of the Government of India. It incorporates the principles of directly observed treatmentshort course (DOTS), the global TB control strategy of the World Health Organization.
The program provides, free of cost, quality antitubercular drugs across the country through the numerous Primary Health Centres and the growing number of privatesector DOTSproviders.
Objectives pulmonary embolism.
- Detecting at least 70% of sputum positive tuberculosis patients in the community.
- Curing at least 85% of the newly detected sputum positive cases.
RNTCP classifis tuberculosis patients into following treatment categories.
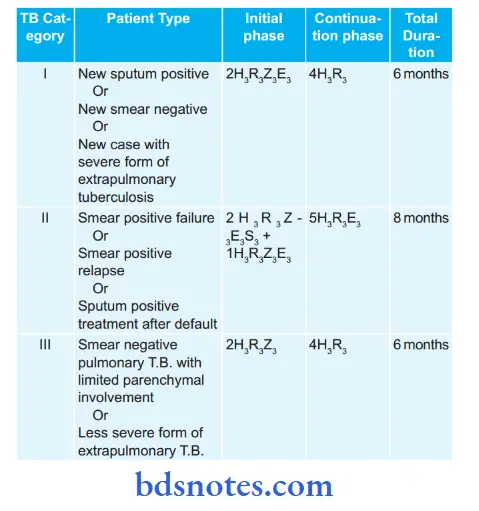
Explanation of standard code pulmonary embolism.
1. Each antitubercular drug has standard abbreviation, i.e.
- Isoniazid (H)
- Rifampicin (R)
- Pyrazinamide (Z)
- Ethambutol (E)
- Streptomycin (S)
- H: Isoniazid (300 mg), R: Rifampicin (450 mg),Z: Pyrazinamide (1500 mg), E: Ethambutol (1200 mg),S: Streptomycin (750 mg).
2. Patients who weigh 60 kg or more receive additional Rifampicin 150 mg.
3. Patients who are more than 50 years old receive
Streptomycin 500 mg. Patients who weigh less than 30 kg
receive drugs as per pediatric weight band boxes according to body weight.
4. Numerical before a phase is the duration of that phase in months.
5. Numerical in subscript is the number of doses of that drug per week. If there is no subscript numerical, then the drug is given daily.
Treatment regimen under rntcP for Mdr-tB (Multidrugresistant tB) and Xdr—tB (extensively drug resistant tB)
1. For MDR-TB:
- Six drugs in intensive phase for 6–9 months: Kanamycin,Levoflxacin, Ethionamide, Cycloserine, Pyrazinamide and Ethambutol.
- Four drugs in continuation phase for 18 months:
Levofloxacin, Ethionamide, Cycloserine and Ethambutol. - Reserve drug is paminosalicylic acid.
2. For XDR—TB:
- Seven drugs in intensive phase for 6-12 months:Capreomycin, p-aminosalicylic acid, Moxiflxacin,high dose Isoniazid, Clofazimine, Linezolid,Amoxicillin and Clavulinic acid.
- Six drugs in continuation phase for 18 months: paminosalicylic acid, Moxifloxacin, high dose lsoniazid, Clofazimine, Linezolid, Amoxicillin and Clavulinic acid.
- Reserve drugs: Clarithromycin, Thiacetazone
Second-line antituberculous drugs
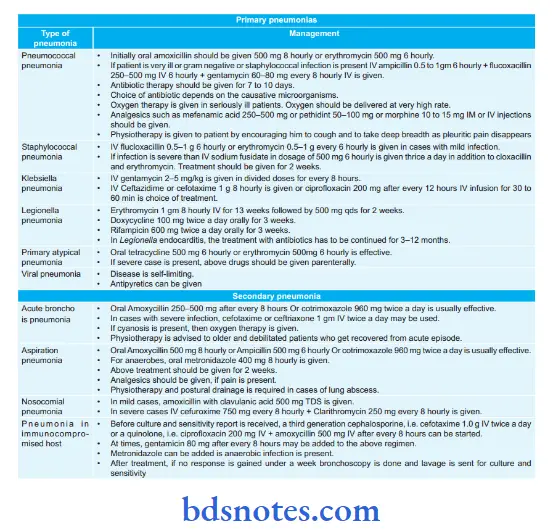
Question. Write in brief clinical features and treatment of pneumonia.
Or
Write sign and symptoms of pneumonia.
Answer. Pneumonia is an accumulation of secretions and inflmmatory cells in alveolar spaces of lungs caused by infection.
Clinical Features pneumonia.
Symptoms
- Malaise, fever, rigors, and night sweats, vomiting in the elderly confusion and disorientation.
- Dyspnea, cough, and sputum which is often bloodstained or rusty and diffilt to expectorate.
- Pain aggravated by cough, deep breath or movement,usually localized to site of inflmmation.
Signs pneumonia.
In early stage:
- Pulse rate and heart rate increases
- Alae nasi are in action
- Presence of herpes on the lip
- Movements of chest are restricted.
- Percussion over the affcted area is diminished.
- Breath sound are harsh with prolong expiration and few crypts.
Signs of pulmonary consolidation:
- Limitation of movement on affcted side.
- Increased vocal fremitus
- Impaired percussion
- Breathing sounds are bronchial, few crypts may be audible.
- Vocal resonance is increased.
- Pleural rub may be heard.
During the period of resolution:
- Bronchial breathing disappear
- Normal breath sound appear
- Coarse crepitations during both phases of respiration.
Treatment pneumonia.
Question. Write in brief sign, symptoms and treatment of pulmonary tuberculosis.
Answer.
Symptoms primary tuberculosis
- Evening rise of temperature
- Night sweats
- Malaise and cachexia
- Irritability and diffilty in concentration.
- Cough and expectoration for more than three weeks.
- Pleuritic chest pain
- Breathlessness is the feature of advanced disease.
- Indigestion and dyspnea
- Amenorrhea often in young women
- Hoarseness of voice.
- Sputum can be mucoid, purulent or blood stained.
- Hemoptysis is a classical feature
- Presence of localized wheeze from local ulcer or narrowing of major bronchus.
- Presence of recurrent cold.
Physical signs primary tuberculosis
- Fever and weight loss
- Tachycardia and tachypnea
- Rapid pulse rate
- Physical signs of collapse, consolidation, cavitation, firosis, bronchiectasis, pleural effsion or pneumothorax.
- In some cases, only localized *rhonchi or rales are present.
- Clubbing of figers is present in chronic disease.
- Most common physical sign of chest is fie crepitation in the upper part of one or both the lungs. This is heard on taking a deep breath after coughing.
- Later on, there can be presence of dullness to percussion or bronchial breathing in upper part of one or both the lungs.
- In chronic cases there is evidence of volume loss and mediastinal shift.
- Hilar, mediastinal and cervical groups lymph nodes are enlarged with splenomegaly.
Treatment regimen under rntcP for Mdr-tB (Multidrug-resistant tB) and Xdr—tB (extensively drug resistant tB)
1. For MDR-TB:
- Six drugs in intensive phase for 6-9 months: Kanamycin,
- Levoflxacin, Ethionamide, Cycloserine, Pyrazinamide and Ethambutol.
- Four drugs in continuation phase for 18 months:
Levofloxacin, Ethionamide, Cycloserine and
Ethambutol. - Reserve drug is paminosalicylic acid.
2. For XDR-TB
- Seven drugs in intensive phase for 6-12 months:
Capreomycin, p-aminosalicylic acid, Moxiflxacin,highdose Isoniazid, Clofazimine, Linezolid,
Amoxicillin and Clavulinic acid. - Six drugs in continuation phase for 18 months:
paminosalicylic acid, Moxifloxacin, high dose lsoniazid, Clofazimine, Linezolid, Amoxicillin and Clavulinic acid. - Reserve drugs: Clarithromycin, Thiacetazone
Question. Write short note on malignancy of lung.
Answer. Malignancy of lung is known as lung cancer.
Predisposing Factors
- Cigarett smoking
- Occupational exposure: This is due to radioactive gases, asbestos, arsenic, nickel, chromates, metallic iron
- Atmospheric pollution: In urban areas
- Lung diseases: Chances of lung cancer increases in patients
- with cryptogenic firosing alveolitis.
Clinical Features malignancy of lung.
Symptoms malignancy of lung.
- Non-specifi: Weakness, tiredness, anorexia, loos of weight
- Respiratory: Presence ofinflenza-like illness or pneumonia distal to obstruction caused by tumor, Increased cough,mild hemoptysis, dyspnea, chest pain which is worst at night, wheeze.
Signs malignancy of lung.
- Clubbing of figers
- Supraclavicular lymphadenopathy
- Mid inspiratory crackles over a lobe, reduction of breadth sounds over a lobe and signs of lobar collapse.
- Wheezing sound is present
- Pleural effsion is present.
Diagnosis malignancy of lung.
It is based on physical examination and investigations.
Investigations malignancy of lung.
- Chest Xray shows peripheral round mass. It is well defined or irregular with pseudopodia or Sunray projection radiating from its surface.
- Sputum cytology: On examination reveals presence of cancer cells.
- Bronchoscopy: Fiberoptic bronchoscopy is done.
- Thoracic CT including upper abdomen is done to see extensions of malignancy.
Management malignancy of lung.
- Surgery can be done.
- Radiotherapy: When resection is not carried out of tumor,radiotherapy is employed.
Continuous hyperfractional accelerated radiotherapy (CHART) three times daily for 2 weeks increases chances of survival. - Chemotherapy: Useful in patients with widespread disease and no local symptoms.
Commonly used combinations are mitomycinifosfamidecisplatin, Mitomycincisplatinvincristine, cisplatingemcitabine and cisplatinvinorelbine.
Three cycles are given.
Question. Write short note on fist-line antitubercular drugs.
Answer. The firstline antitubercular drugs are Isoniazid, Rifampin, Pyrazinamide, Ethambutol and Streptomycin.
These drugs have high antitubercular efficy as well as low toxicity and are used routinely.
Isoniazid
- Isoniazid is a fist line antitubercular drug.
- It acts on extracellular as well as intracellular TB and is equally effctive in alkaline and acidic medium.
- The most possible action of isoniazid is inhibition of synthesis of mycolic acids which are unique fatt acid component of mycobacterial cell wall. The lipid content of Mycobacterium exposed to isoniazid is reduced.
- Isoniazid is completely absorbed orally and penetrates all body tissues, tubercular cavities and placenta.
- It is extensively metabolized in liver by acetylation.
- The metabolites are excreted in urine.
Rifampin
- Rifampin is bactericidal to M. tuberculosis.
- Bactericidal action covers all subpopulations of TB bacilli,but acts best on slowly or intermittntly dividing ones, as well as on many atypical mycobacteria.
- It has good sterilizing and resistance preventing actions.
Rifampin inhibits DNA dependent RNA synthesis. - It is wellabsorbed orally, widely distributed in the body: penetrates cavities, caseous masses, placenta and meninges.
- It is metabolized in liver to an active deacetylated metabolite which is excreted mainly in bile, some in urine also.
Pyrazinamide
- It is weakly tuberculocidal but more active in acidic medium.
- It is more lethal to intracellularly located bacilli and to those at sites showing an inflmmatory response (pH is acidic at both these locations).
- It is highly effctive during the fist 2 months of therapy when inflmmatory changes are present.
- By killing the residual intracellular bacilli, it has good ‘sterilizing’ activity.
- It inhibits mycolic acid synthesis, but by interacting with a diffrent fatt acid synthase encoding gene.
- Pyrazinamide is absorbed orally, widely distributed, has good penetration in CSF, extensively metabolized in liver and excreted in urine.
Ethambutol
- Ethambutol is selectively tuberculostatic and clinically as active as S. Fast multiplying bacilli are more susceptible as are many atypical mycobacteria.
- Ethambutol inhibits arabinosyl transferases involved in arabinogalactan synthesis and to interfere with mycolic acid incorporation in mycobacterial cell wall.
- Patient acceptability of ethambutol is very good and side effcts are few.
Streptomycin
- It was the fist clinically useful antitubercular drug.
- It is tuberculocidal, but less effective than rifampin;acts only on extracellular bacilli. Thus, host defense mechanisms are needed to eradicate the disease.
- It penetrates tubercular cavities, but does not cross to the CSF, and has poor action in acidic medium.
- Resistance developed rapidly when streptomycin was used alone in tuberculosis–most patients had a relapse.
Question. Describe various extra pulmonary tuberculosis and how will you treat a case of tubercular meningitis.
Answer.
Extrapulmonary Tuberculosis
In extrapulmonary tuberculosis which involves all the major organs in body from heart to gastrointestinal tract.
Following are the various types of extrapulmonary tuberculosis:
Tuberculous Pericarditis
- Involvement of pericardium is very common by M. tuberculum bacteria.
- It occurs in form of pericarditis, pericardial effsion and later on there is constrictive pericarditis.
- Its earliest sign is pericardial rub and fever.
- As disease exacerbate, there is formation of effsion and when it is massive cardiac temponade may occur.
Gastrointestinal tract
- There is occurrence of primary lesion due to swallowing of tubercle bacilli which lodges in the ileocecal region and produce primary hypertrophic ileocecal tuberculosis.
- Common manifestations are tuberculous peritonitis, tabes mesenterica, tuberculous enteritis, diarrhea and fitula.
Skeletal Tuberculosis
- Tuberculosis of spine, paravertebral cold abscess, sinus tract formation and involvement of weightbearing joints such as knees and hips.
- When tubercular granuloma extend to the mandible or maxilla via extraction socket by means of hematological spread, this can lead to tuberculous osteomyelitis.
- Early diagnosis by joint aspiration and biopsy is done to prevent disability and to avoid surgery.
Genitourinary Tuberculosis
- It presents as painless hematuria and sterile pyuria.
- In this renal parenchyma, calyces, ureter and bladder are affcted in descending order.
- Testicular and epididymal involvement may be present which causes sterility.
- In females Involvement of fallopian tubes causes female infertility.
Meningeal tuberculosis
- Tuberculoma in brain and tubercular meningitis are very
- common complications and may leave behind number of sequelae.
Adrenal Tuberculosis
- It produces the picture of Addison’s disease.
- It is seen in long standing cases of abdominal tuberculosis.
lupus vulgaris
When tubercle bacilli invade the skin this is known as lupus vulgaris.
Oral Tuberculosis
- When tubercle bacilli directly inoculated in oral tissues of a person who had not acquired the immunity to the tuberculosis.
- In oral cavity, there is involvement of tongue, gingiva, extraction socket and buccal mucosa.
- In oral cavity at above mention sites, there is presence of typical tubercular ulcer.
- Tuberculous gingivitis appears as diffse, hyperemic or nodular papillary proliferation.
Treatment Of A Case Of Tubercular Meningitis
- Antitubercular drugs: Rifampicin 600 mg/day + Isoniazide (600 to 900 mg/day) + Pyrazinamide (1.5 gm) should be given. Treatment with this regimen is given for 2 months.This is followed by rifampicin 600 mg/day + Isoniazide (600 to 900 mg/day) for 12 to 18 months.
- Steroids: Prednisolone 40–60 mg/day to reduce toxicity, piaarachnoid adhesions and feeling of wellbeing.
Question Write etiology, clinical features, investigations and treatment of pneumonia.
Answer. For clinical features ofpneumonia refer toAns 35 of same chapter.
For treatment of pneumonia refer to Ans 6 of same chapter.
Etiology pneumonia.
- Bacterial: Pneumococcus, Staphylococcus, Streptococcus,
- H.inflenza, E.coli, Klebsiella, Pseudomonas, etc.
- Atypical: Viral, Rickettial, mycoplasmal
- Protozoal: E. histolytica
- Fungal: Actinomycosis, aspergillosis, histoplasmosis,nocardiosis
- Allergic: Loeffl’s syndrome
- Radiation
- Collagenosis: Systemic lupus erythematosus, rheumatoid arthritis, polyarteritis nodosa
- Chemical: Aspiration of vomitus, gases and smokes,kerosene, paraff and petroleum.
Investigations pneumonia
- Xray chest is done for assessing the opacity in lung.
- Examination of sputum is done by Gram’s and Ziehl Neelsen stains.
- Sensitivity as well as sputum culture should be carried out for anaerobic and aerobic organisms.
- If sputum is absent, then bronchoscopic aspiration is done for both culture and sensitivity.
- Blood examination is done for assessing leucocytosis.
- Sputum, urine and serum testing should be done for identifying the pneumococcal antigen.
- If empyema is present, then pleural flid aspiration is done.
- Blood gas analysis should be done.
Question. Write etiology, diagnosis and management of pulmonary tuberculosis.
Answer. Involvement of lungs by tuberculosis is known as pulmonary tuberculosis.
Etiology pulmonary tuberculosis.
- Mycobacterium tuberculosis leads to the pulmonary tuberculosis.
- In immunocompromised patients or in children tuberculosis can be caused by atypical Mycobacterium.
Diagnosis pulmonary tuberculosis.
It is based on clinical signs and symptoms as well as investigations.
Symptoms pulmonary tuberculosis.
- Evening rise of temperature
- Night sweats
- Malaise and cachexia
- Irritability and diffilty in concentration.
- Cough and expectoration for more than three weeks.
- Pleuritic chest pain
- Breathlessness is the feature of advanced disease.
- Indigestion and dyspnea
- Amenorrhea often in young women
- Hoarseness of voice.
- Sputum can be mucoid, purulent or blood stained.
- Hemoptysis is a classical feature
- Presence of localized wheeze from local ulcer or narrowing of major bronchus.
- Presence of recurrent cold.
Lung Disease Emphysema
Physical signs pulmonary tuberculosis.
- Fever and weight loss
- Tachycardia and tachypnea
- Rapid pulse rate
- Physical signs of collapse, consolidation, cavitation, firosis, bronchiectasis, pleural effsion or pneumothorax.
- In some cases only localized *rhonchi or rales are present.
- Clubbing of figers is present in chronic disease.
- Most common physical sign of chest is fie crepitation in the upper part of one or both the lungs. This is heard on
taking a deep breath after coughing. - Later on, there can be presence of dullness to percussion or bronchial breathing in upper part of one or both the lungs.
- In chronic cases, there is evidence of volume loss and mediastinal shift.
- Hilar, mediastinal and cervical groups lymph nodes are enlarged with splenomegaly.
Investigations pulmonary tuberculosis.
Serology: In this ELISA, technique is used which helpful in diagnosis of tuberculosis in children. PCR technique is more specifi and sensitive serological test than ELISA, but PCR is less used due to its high cost.
Chest X-ray: Presence of multiple nodular infitrations or ill-defied opacities in one of upper lobes is characteristic for pulmonary tuberculosis. An area of translucency in radiopacities is indicative of cavitation. Presence of cavity is indicative of an active lesion. In some of the patients multiple thickwalled cavities can be seen. At the time of firosis, trachea and mediastinum shift to same side.
Fibrosis can also cause calcifiation.
Pathological tests:
Blood examination: Peripheral blood examination shows monocytosis, i.e. 8 to 12%
ESR is elevated.
Tuberculin test: It is a test to recognize prior tubercular infection, and is done by injecting one unit of purifid protein derivative (PPD) on the forearm and readings taken after 48 hours. Induration of more than l5 mm indicates a positive test. The younger is the patient,greater is signifiance of positive test. A negative test does not always exclude tubercular infection since it may be negative in patients of blood malignancies, malnourishment and those on immunosuppressive therapy. Tuberculin test is nonspecific and only indicates prior infection. Its sensitivity wanes with age.
Management pulmonary tuberculosis.
Chemotherapy: For details, refer to Ans18 of same chapter.
Corticosteroids: They are to be given in the severe cases to enable them to survive till antitubercular drugs become effctive. Oral prednisolone is given in doses of 20 mg orally for 6 to 8 weeks. Steroids produce euphoria and increase appetite in the patients.
Surgery: Surgical resection of infected lobe is feasible.
Symptomatic treatment:
Cough: If it is irritative, linctus codeine is given.
Smoking should be stopped.
Laryngitis: Rest is given to the voice. If pain is present anesthetic powders, spray and lozenges are given.
Lung Disease Emphysema
Question. Describe etiology, clinical features, diagnosis, complications and treatment of chronic obstructive pulmonary disease.
Or
Write etiology, clinical features, diagnosis, and management of chronic obstructive pulmonary disease.
Answer. Chronic obstructive pulmonary disease is characterized by irreversible obstruction to the airflw throughout lungs.
It consists of two important disorders of lungs, i.e. chronic bronchitis and emphysema.
These both diseases coexist in a single patient.
Etiology chronic obstructive pulmonary disease
1. Localized:
- Congenital
- Compensatory due to lung collapse, scarring or resection
- Partial bronchial obstruction due to neoplasm or foreign body
- MacLeod’syndrome
2. Generalized:
- Idiopathic
- Senile
- Familial, i.e. due to alpha-l-anti-trypsin defiiency
- Associated with chronic bronchitis, asthma or
pneumoconiosis.
Clinical Features chronic obstructive pulmonary disease
Lung Disease Emphysema
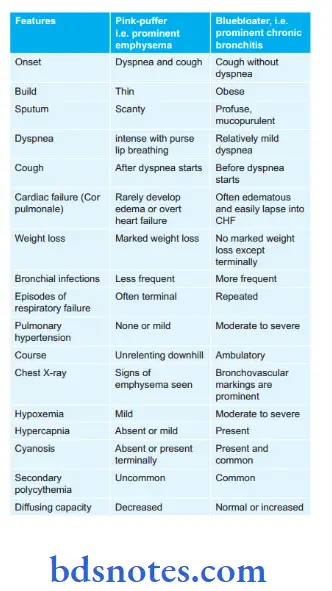
In most of the patients, chronic bronchitis is associated with emphysema so two types clinical syndromes of chronic obstructive pulmonary disease are present i.e.
1. Predominant chronic bronchitis with emphysema, i.e.
Bluebloater type
2. Predominant emphysema with some degree of chronic bronchitis, i.e. pink-puffrs type
Diagnosis chronic obstructive pulmonary disease
1. History of chronic progressive symptoms, i.e. cough orwheeze or breathlessness.
2. General condition: Patient can be emaciated, cyanosed and edematous. Jugular venous pressure may show giant awaves.
3. Chest fidings:
- Chest wall process is barrelshaped.
- Movement of chest is decreased.
- Centrally placed mediastinum
- Percussion is hyperresonant.
- Breath is diminished vesicular with prolong expiration.
- Rhonchi are heared.
- Vocal resonance sounds are diminished.
4. Heart:
- Apex beat may not be visible or palpable.
- Right ventricular heave can be present.
- Heart sounds can be diminished. Second sound can be loud.
- Gallop rhythm can be heared.
- Functional tricuspid regurgitation murmur can be present.
- Hyperkinetic state with warm limb and water hammer
pulse is present.
Lung Disease Emphysema
5. Miscellaneous:
- Hepatomegaly can be present.
- Optic disc can show papilliedema
6. Investigations:
- There is presence of post-bronchodilator FEV1/FVC less than 0.7 which confims the presence of persistent airflw limitation and thus is diagnostic of chronic obstructive pulmonary disease.
- Arterial blood gas show retention of carbon dioxide in emphysema.
- Serum alpha1antitrypsin levels to diagnose alpha1 anti-trypsin defiiency.
- X-ray chest: Presence of hypertranslucency of lung filds, wide intercoastal spaces, diaphragm is low and flt, heart is tubular shaped, presence of large hilar shadows, diminished peripheral vascular pattrn, rounded areas of hypertranslucency with thin hairline shadow forming margins.
Complications chronic obstructive pulmonary disease
In emphysema
- Pneumothorax due to rupture of bullae in pleural space.
- Cor pulmonale, i.e. rightsided heart failure or right ventricular hypertrophy secondary to lung disease.
- Type II respiratory failure.
Lung Disease Emphysema
In chronic Bronchitis
- Type I and type II respiratory failure
- Cor pulmonale
- Pulmonary arterial hypertension
- Secondary infections
- Secondary polycythemia
Treatment chronic obstructive pulmonary disease
1. Bronchial irritants should be avoided, i.e.
- Smoking should be strictly stopped.
- Passive smoking is stopped.
- Gas smoke is avoided by housemakers.
- Aerosols such as hair spray, insecticide spray and aerosols should be avoided.
- Polluted atmosphere should be strictly avoided.
2. Treatment ofan infection:
- Ampicillin 250 to 500 mg every 6 hourly is given for 5–7 days.
- Cotrimazole 960 mg can be given as BD dose.
- Antibiotics should be given till purulent mucous become mucoid.
- If necessary modify antibiotics as per culture and sensitivity test.
3. Bronchodilators:
- In mildtomoderate chronic bronchitis oral theophylline 150 mg
- BD or inhaled salbutamol 200 μg 6 hourly can be given.
- In severe bronchitis, ipratropium bromide 40 to 80 μg 6 hourly is added.
4. Mucolytic agents: Bromhexine and carbocystein are to be given.
5. Corticosteroids: Prednisolone 30mg/day for 2 weeks is given.
If improvement occur by oral steroids they are replaced by inhalational steroids.
6. Domiciliary oxygen therapy: Longterm oxygen therapy in low concentration, i.e. 2L/min by nasal cannula is given to reverse or to delay development of pulmonary hypertension.
7. If cor pulmonale is present diuretics such as furosemide,
digitalis and potassium salts might be given.
8. Chest physiotherapy should be done, and proper exercises should be taught to the patient.
9. Patients with COPD should receive influenza and pneumococcal vaccines.
10. Noninvasive ventilation is useful in those with pronounced daytime hypercapnia.
11. Lung volume reduction surgery can be done. In this parts of lungs are resected to reduce hyperinfltion.

Leave a Reply