Respiration System
Lung functional tests in respiratory diseases:


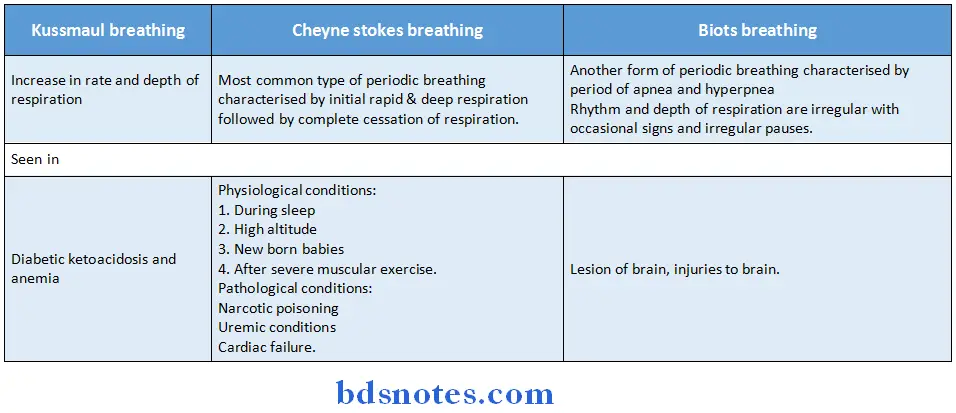
Types of breathing:


Asthma and its management:
- Asthma is a disorder characterised by chronic airway obstruction and increased airway responsiveness.
- This results in wheeze (inspiratory), breathlessness, cough and sensation of chest tightness.
- The symptoms become worse in the mornings.
- Pectus carinatum or pigeon chest or keel breast deformity is caused by severe asthma during childhood.
Other Anomalies of the chest:

- The concept of step-up and step-down is followed in the treatment of asthma.
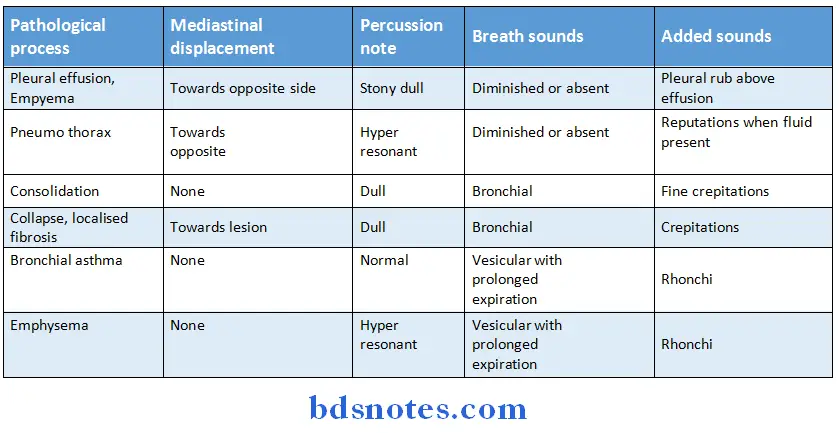
Other respiratory diseases:

- If there has been good symptomatic control a step down schedule should be made.
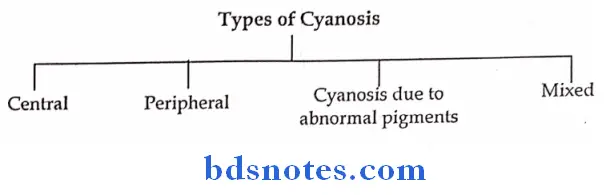
Other clinical findings:


Other clinical findings:
Cardiovascular System
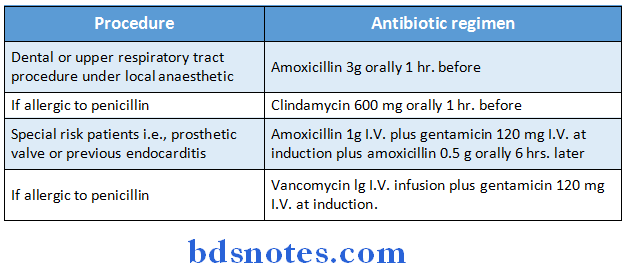
Antibiotic Prophylaxis:
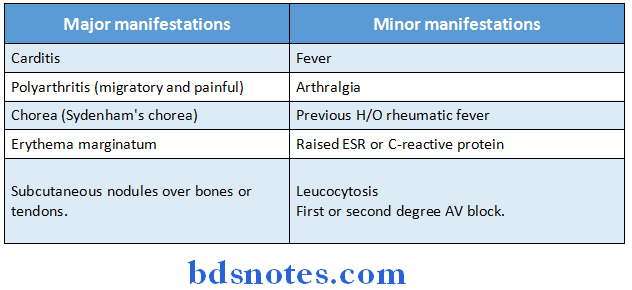
Jones Criteria for the diagnosis of Rheumatic fever:
Infective Endocarditis:
Etiology:

Infective endocarditis is due to microbial infection of a heart valve, the linking of a cardiac chamber or blood vessel or a congenital anomaly (e.g.: septal defect).
If mostly affects jet lesions i.e., areas of endocardial damage caused by high pressure jet of blood such as VSD, MR and AR. Risk of endocarditis is less in low pressure lesions like atrial septal defect.
When the infection is established vegetations composed of organisms, fibrin and platelets grow to become are enough to cause obstruction and also break away as emboli.
Clinical features of infective endocarditis:
- Roth spots in fundi
- Cerebral emboli
- Petechial haemorrhages of ski and mucous membranes
- Splinter haemorrhages and clubbing of nails
- Osler’s nodes which are painful tender swellings at the finger tips
Splenomegaly - Haematuria
- Murmurs, arrhythmias and cardiac failure.
Laboratory investigations in myocardial infection:

Coronary heart diseases:
Stable angina:
Occur whenever there is an imbalance between myocardial oxygen supply and demand. It is characterised by central chest pain, dyspnoea on exertion and is relieved by rest.
Pathology:
Ischemia due to fixed atheromatous stenosis of one or more coronary arteries.
Unstable angina:
It is characterised by rapidly worsening angina (crescendo angina), angina on minimal exertion or angina at rest.
Pathology:
Ischemia caused by dynamic obstruction of a coronary artery due to plaque rupture with superimposed thrombosis and spasm.
Myocardial infarction:
Prolonged cardiac pain, vomiting, breathlessness are the important features of MI.
Pathology:
Myocardial necrosis caused by acute occlusion of a coronary artery.
Heart failure:
Myocardial dysfunction due to infarction or ischemia.
Arrhythmia:
Altered conduction due to ischaemia or infarction.
Sudden death:
Due to ventricular arrhythmia, asystole or massive myocardial infarction.
Pulse and its types:
The normal pulse appears at regular intervals and has a rate between 60-10 per min. The normal pulse has a small Anacrotic wave on the upstroke, which is not felt. This is followed by a big tidal or percussion wave, which is

Other important viva points:
- The first symptom of heart failure – Dyspnoea.
- Both central and peripheral cyanosis occurs in congestive cardiac failure.
- Normal cardiothoracic ratio should be less than 0.5 in radiographic examination.
In jugular venous pressure JVP:
- Absent’a’ wave – atrial fibrillation
- Kussmaul’s sign – constrictive pericarditis
- Large ‘V’ wave – Tricuspid regurgitation
- Steep ‘Y’ descent – constrictive pericarditis
Slow ‘y’ descent – Tricuspid Stenosis:
- A- atrial contraction
- C- onset of ventricular contraction
- V-pressure peak immediately to opening of tricuspid value.
Commonest cause of ventricular tachycardia is acute myocardial infarction. Treatment is by I.V lignocaine.
Blood
Types of Anemias:
Microcyctic hypochromic:
- MCV, MCH, MCHC are reduced
- Example: Iron deficiency anemia, thalassemia, sideroblastic anemia.
Normocytic Normochromic:
- MCV, MCH, MCHC are normal
- Example: Hemolytic, Aplastic anemia, acute blood loss, anaemia of chronic disorders
Macrocytic Normochromic:
- MCV is raised
- Example: Megaloblastic anemia.
Types of leukaemias:

Erythroblastalis foetalis:
When a Rh-ve mother carries in a Rh +ve fetus, usually the first child escapes the complications of the Rh incompatibility.
When the mother conceives for the second time and carries a Rh +ve fetus, the Rh agglutinins enter the fetus and cause agglutination of fetal RBC and hemolysis.
Complications: Hydrops foetalis and kernicterus.
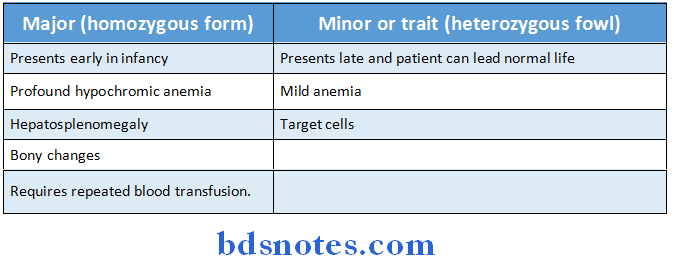
Thalassemia:
Thalassemia is a quantitative defect in hemoglobin characterised by lack of certain types of globin chains and compensatory increase in other globin chains
Failure to synthesize beta chains (beta-thalassemia or Cooley’s anemia) is the most common type of thalassemia.
It is characterised by decrease in HbA (α2 β2) and increase in Fetal hemoglobin HbF (α2 γ2) and HbA2 (α2 δ2).
Spectrum of β thalassemia

Lab investigations in haemophilia:

Classification of Aids:

Herpes virus infection:

Importance of antibodies associated with hepatitis infection
- HbsAg : Its presence in serum indicates infection or previous vaccination with hepatitis B virus
- HbeAg : Its presence in serum indicates relative infectivity (High/low)
- HUCAg : It is a hidden component of the viral core and is not detectable at all
- IgM Anti Hbc: Specific of acute infection
- IgG Anti Hbc: Specific for chronic infection.
Deviation in nerve lesions:

CSF Estimation In Meningitis

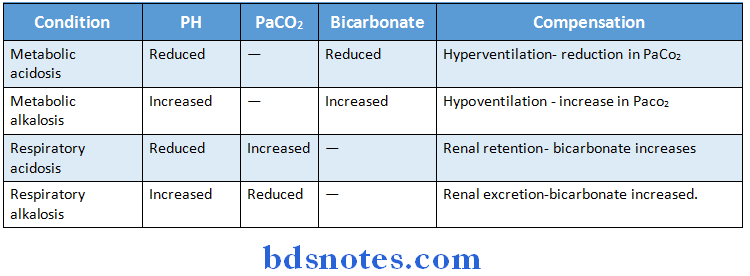
Metabolic acidosis and alkalosis:

Causes of upper GI bleeding:
- Peptic ulcer (most common)
- Gastric erosion (next common)
- Varices
- Oesophagitis
- Cancer of stomach or esophagus.
Peptic ulcer means an ulcer in the wall of stomach or duodenum caused by digestive action of gastric juice.
Two major forms:
- Duodenal
- Gastric
- If peptic ulcer occurs in stomach, it is called gastric ulcer and if found in duodenum it is called duodenal ulcer.
- The recurrent abdominal pain has three notable characteristics:
- Localizations to the epigastrium, relationship to the food and episodic occurrence.
- In gastric ulcer, pain occurs while eating or drinking and is relieved by vomiting.
- Gastric ulcer is associated with anorexia and weight loss.
- In duodenal ulcer, pain is felt 1 or 2 hrs after food intake and during night.
- Pain is relieved by taking food.
- Other symptoms of peptic ulcer are vomiting, heart burn and hematemesis.
Clinical features of hepatic cirrhosis (chronic liver failure) are:
- Jaundice
- Hepatomegaly but gradually liver size decreases due to hepatocyte destruction
- Ascites
- Spider telangiectasia, palmar erythema
- Loss of libido, Gynecomastia
- Bruises, epistaxis
- Portal hypertension features (splenomegaly, collateral vessel, variceal bleeding and fetor hepaticus)
- Clubbing, pigmentation.
Nephritic syndrome:
- Nephrotic syndrome is characterised by protein loss in urine of more than 3.5g proteinuria/day, fluid retention or oedema, hypercoagulability, hyper cholesteremia and infections.
- Albumin is the dominant serum protein.
- Presence of albumin in the urine is a sure sign of Glomerular abnormality.
- The diseases that cause nephritic syndrome always affect the glomerulus.
- Portal hypertension is characterised by prolonged elevation of the portal venous pressure (normally 2-5 mm of Hg).
Etiology:
- In children: Extra hepatic portal vein obstruction
- In adults: Cirrhosis
Clinical features:
- Splenomegaly, Ascites, varices and collateral vessel formation.
Laboratory analysis of jaundice:

Types of Diabetes mellitus:

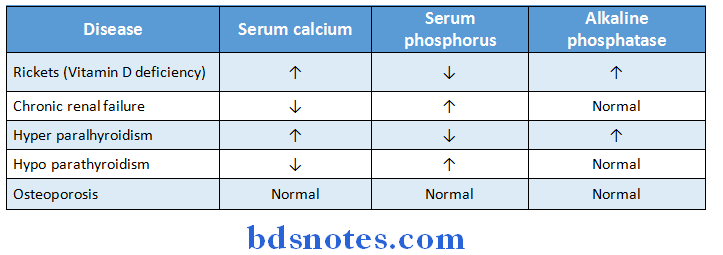
Serum levels of some diseases:
Causes of Clubbing:

Types of murmurs:


Vitamins
- Normal requirements (per day)
Vitamin A (Retinol):
- Children: 500-750 micrograms
- Adults: 750 micrograms
- Pregnancy and lactation: 1200 micrograms.
Vitamin D:
- Children below 5 years: 10 micrograms = 400 units
- Children above 5 years: 2.5 micrograms = 100 units
- Adults: 2.5 micrograms = 100 units
- Pregnancy and lactation: 10 micrograms = 400 units
- Niacin: 6.6 mg/1000 K. cals 18 mg
- Pyridoxin: 1.5 mg
- Pantothenic acid: 10 mg
- Folate Adult: 100 micrograms
- Pregnancy: 300 micrograms
- Cyanocobalamin (B12): 1 microgram.
Incubation periods disease incubation period:
- Anthrax – 1 to 3 days
- Diphtheria – 2 to 5 days
- Typhoid – 5 days
- Tetanus – 3 to 21 days
- Measles -10 days.
- Chicken pox – 2 to 3 weeks
- Rubella – 2 to 3 weeks (18 days)
- Mumps – 2 to 3 weeks (18 days)
- Hepatitis-A – 15 to 50 days
- Hepatitis-B – 50 to 160 days.
Usual complications:
- Mumps: Children – Menningoencephalitis
Adolescents – Orchitis - Rubella : Polyarthritiis
- Measles : Otitis media
- Typhoid : Paralytic fleus
- Tetanus : Airway obstruction and anoxia.
Miscellaneous Important Viva Points
Medicine:
- Human body consists of 40 liters of water approximately.
- The effective osmolality of plasma and interstial fluid determined by sodium ions.
- The extracellular fluid tonicity is maintained by chloride ion.
- The chief ions of intracellular fluid are potassium (K), magnesium (Mg), sulphate etc.
- Hyponatremia: Loss of sodium from the body
Clinical features: are lassitude, hypotension, tachycardia, reduced skin elasticity, apathy, weakness, coma, oliguria etc. - Dehydration is loss of water from body.
Clinical features: thirst, dry mouth, dizziness, dysphagia, muscular weakness, oliguria, mental confusion etc. - Hypokalemia: Depletion of potassium from body
Clinical features: such as generalized muscular weakness, depression of tendon reflexes, confusion, coma, parasthesia, muscle stiffness, polyuria, nocturia - Hyperkalemia: Marked increase in potassium content
Clinical features: cardiac arrest, irregular pulse, flaccid paralysis, abdominal distension etc.
PEM:
- Marasmus
- Kwashiorkor
- Marasmus is a common form of protein energy malnutrition (PEM); occurs, most commonly 6-12 months postnatal (infantile period).
- Clinical features of marasmus are patient presents a large head (relatively), distended abdomen, diarrhea, stick-like limbs, 60% of reduction in normal weight.
- Oral rehydration salts sodium chloride, bicarbonate, and glucose.
- Above 37.8°C, for every 0.5°C rise in temperature 200 mL of extra water is required.
- In total starvation, the body glucose reserves lasts for 24 hrs.
- Kwashiorkor is also a disease of protein-energy malnutrition, which commonly occurs in second year of life.
- Clinical features – generalized edema, change in color of hair (flag sign), diarrhea, palpable liver, pigmentation of skin and ulceration etc.
- pH of blood is 7.3-7.4 (36-44 nanomoles/litre)
- Parenteral diet of the patient with malabsorption syndrome includes fat emulsion, dextrose, amino acids.
- Casein: albumin ratio in human milk is 1:1.
- Commonest autosomal recessive disorder is cystic fibrosis, usually associated with cancrum oris etc
Cardiovascular System:
- Pulse: possesses a characteristic rate, rhythm, volume and quality.
- The rate and rhythm of arterial pulse are best assessed from radial pulse.
- The volume and quality are better assessed from brachial, carotid, femoral pulses. Bradycardia is a resting pulse < 60 beats/min.
- It is commonly seen in athletes, hypothyroidism, vasovagal syncope, sick sinus syndrome and patients taking beta-blockers.
- Tachycardia is a resting pulse >100 beats/min.
- Tachycardia is commonly seen in patients with fever, anxiety, hyperthyroidism, heart failure etc.
- Rhythm of pulse may be regular/irregular.
- Irregular rhythm may be irregular completely (atrial fibrillation) or regular (ectopic beats).
- Rhythm associated with breathing, which speeds up with inspiration and slows with expiration is called as sinus arrhythmia.
- Pulse quality depends upon pulse volume and character of left ventricular impulse, E.g:
- Slow rising pulse-aortic stenosis
- Collapsing pulse-aortic incompetence
- Jerky pulse-hypertrophic obstructive cardiomyopathy.
- Pulsus paradoxus-volume decreases with inspiration and volume increases with expiration-pericardial tamponade.
- Pulsus alterans-alternation of large, and small volume beats-cardiac failure
- Pulsus bisferens-pulse with double peak best felt in brachial artery- aortic stenosis and regurgitation.
- The commonest cause of raised JVP (jugular venous pressure) is cardiac failure.
- Thrills are palpable vibrations caused by turbulent flow and are equivalent to murmur.
- Systolic thrill-mitral regurgitation. Diastolic thrill-mitral stenosis.
- Heart sounds: First heart sound is due to closure of mitral and tricuspid valves (MT).
- First heart sound is loud in mitral stenosis with friable valves.
- Loud first heart sound is present in mitral stenosis, fever, thyrotoxicosis, xc:-cise etc.
- First heart sound is quiet in obesity, emphysema, impaired LVF.
- Second heart sound is due to closure of aortic and pulmonary valves (A2P2).
- Loud P2-mitral stenosis, primary pulmonary hypertension, atrial septal defect.
- Physiological splitting of second heart sound is seen in children and young adults.
- Reversed splitting is seen in LBBB, hypertrophic cardiomyopathy.
- Wide mobile splitting is seen in RBBB, pulmonary stenosis.
- Wide, fixed splitting is seen in ASD.
- Third heart sound is a low-pitched sound heard at end of diastolic left ventricular filling, heard commonly in pregnant women, athletes, children etc,
- Fourth heart sound occurs due to forceful atrial contraction-causes are IHD; long- standing hypertension etc.
- Calcium ions-positive ionotropic effect on myocardium.
- Some clinical conditions producing murmurs

- Pulse pressure is the difference between systolic and diastolic pressure, which is commonly 40mm Hg-more in elders. (Normal: 30-60)
- Cardiac output is the function of preload after load and myocardial contractility.
Heart failure:
- In left sided heart failure, a reduction in left ventricular output and an increase in left atrial/pulmonary pressure occur.
- Left heart failure presents features such as breathlessness, orthopnoea, PND, inspiratory crepitations etc.
- In right-sided heart failure, reduction in right ventricular output occurs. Examples: chronic lung disease, pulmonary stenosis etc.
- Right heart failure presents high JVP, hepatic congestion, edema etc
- Biventricular heart failure is seen in dilated cardiomyopathy of IHD.
- Heart failure due to inadequate cardiac output is called forward heart failure.
- Backward heart failure may have normal cardiac output but with marked salt and water retention and pulmonary, systemic venous congestion.
- High output cardiac failure-conditions that lead to high cardiac output are large A- V shunt, severe anemia, thyrotoxicosis, wet beriberi.
- Haemoptysis-MS
- Sudden death-AS
- In aortic stenosis second aortic sound is diminished, single/paradoxically split and associated with angina.
- Most sensitive diagnosis of myocardial infarction is serial ECG monitoring.
- Ventricular septal defect is the congenital defect associated with SABE.
- Kussmaul sign-rise in the JVP during inspiration-seen in constrictive pericarditis.
- Aortic dissection-ascending part of aorta
- Coarctation-arch of aorta
- Aortic aneurysm-descending aorta.
- Commonest congenital heart disease-ventricular septal defect.
- Hilar dance-atrial septal defect, associated with wide fixed split second heart sound.
- Commonest cyanotic heart disease-tetralogy of Fallot. Associated with pulmonary artery stenosis, ventricular septal defect, overriding of aorta (triology of Fallot) + right ventricular hypertrophy.
- Commonest site of coarctation of aorta-at the junction of arch and descending aorta.
- In JVP:
- a wave-represents atrial contraction. Absent in atrial fibrillation.
- c wave-represents onset of ventricular contraction.
- v wave-represents pressure peak immediate to opening of tricuspid valve.
- Large v wave is seen in tricuspid regurgitation. Large a wave-TS
- Acute rheumatic fever is caused by Streptococcus pyogenes.
- Clinical features of rheumatic fever are:
- Migrating polyarthritis preceded by a history of sore throat.
- Skin lesions such as erythema marginatum, erythema nodosum, and sub cutaneous nodules.
- Carditis-palpitations, chest pain, breathlessness.
- Mid diastolic murmur (Carey Coombs murmur) is present specifically.
- Jerky involuntary movements called Sydenham chorea (St. Vitus dance) are present.
- Duckett Jones proposed criteria in order to diagnose ARF, which consists of major and minor manifestations Duckett Jones major manifestations are carditis, polyarthritis, chorea, erythema marginatum, subcutaneous nodules.
- Minor manifestations are raised ESR, pyrexia, high ASO titre etc.
- Treatment of ARF-benzathaine penicillin 12,00,000 units once a week for 3 weeks and then monthly for first year.
- Infective endocarditis is caused by rnicrobial infection of heart valve or lining of cardiac chamber.
- Subacute endocarditis-Streptococcus sanguis.
- Acute endocarditis-Staphylococcus aureus.
- Post operative endocarditis-Staphylococcus albus.
- Clinical features of S ABE are fever, tiredness, purpura, petechial hemorrhages, finger clubbing, Osier’s nodes, painful swelling at finger tips, Janeway spots, splenomegaly.
- Janeway lesions-seen in acute bacterial endocarditis.
- Commonest cause of angina-coronary atheroma.
- Prinzmetal/variant of angina-pain due to arterial spasm, accompanied by ST elevation in ECG.
- Commonest cause of arterial emboli from heart is postmyocardial infarction.
- Train-in-tunnel murmur-Gibson’s murmur in PDA.
- Musical cooing/seagull effect-AR.
- In MI-LDH, TRANSAMINASES, CPK-MB isoenzymes are raised. CPK-MM increased in muscle, CPK-BB-brain.
- Cause of death in acute state of MI-death in first hour of attack-due to ventricular failure.
- Concentration of methaglobin in blood to cause cyanosis-5 gm%.
- Widow’s artery-left anterior descending coronary artery.
- Wenkenbach’s phenomenon-progressive lengthening of successive PR interval followed by a dropped beat.
- Austin Flint murmur-mid diastolic murmur.
- Carey Coombs murmur-mid diastolic in acute rheumatic fever.
- Graham Steel murmur-early diastolic in pulmonary regurgitation.
- Means murmur-harsh pulmonary systolic murmur.
- Gibson’s murmur-train-in-tunnel murmur in patent ductus arteriosus.
- In hypercalcemia-shortening of QT interval.
- Treatment for ventricular fibrillation-DC shock.
Respiratory system:
- Barrel chest-emphysema
- Pigeon chest-chronic bronchial asthma.
- Eggshell calcification of hilar lymph nodes-silicosis.
- Blue bloaters-chronic bronchitis
- Pink puffers-emphysema.
- Expiratory stridor-bronchial asthma
- Inspiratory stridor/wheeze/ronchi-airway obstruction.
- Colour of sputum and associated conditions:
- Pink frothy
- Black sputum
- Rusty
- Yellow and foul smelling
- Red juicy sputum
- Pulmonary edema
- Aspergillosis and anthracosis
- Pneumonia
- Lung abscess, bronchiectasis
- Bronchial carcinoma
- Bronchial breath sounds-lobar pneumonia, bronchial destruction, fibrosis and cavitations
- Vesicular breath sound-bronchial asthma, emphysema, bronchitis
- Pleural rub-pleural effusion
- Expiratory wheeze-asthma, bronchopneumonia, emphysema.
- Eocalized wheezing-foreign body in lung.
- Type-I respiratory failure-Paco2 and Pao
- Type-II – Paco2↑, Pao2↓
- Pulmonary hypertension involves small pulmonary arteries.
- Prolonged hyperventilation is associated with paraesthesia, tetany and palpitations.
- Sequence of changes in status asthmaticus-respiratory alkalosis; respiratory acidosis; metabolic acidosis.
- Cheyne Stokes breathing:
- Heart failure
- High altitude
- Elderly
- Kussmaul breathing-in lactic acidosis due to increased H”1″ ions.
- Characterized by deep inspiration and prolonged expiration.
- Biot’s breathing-advanced respiratory failure, two or three inspiratory movements on respiration.
- Amphoric breathing-pneumothorax.
- Interstitial lung disease-crackling crepitations unaltered by breathing.
- Pulmonary infarction-caused due to tuberculosis and pneumoconiosis.
- Characterized by pleural pain, hemoptysis, dyspnoea.
- Bovine cough-recurrent laryngeal nerve paralysis.
- Stony dull note on percussion-pleural effusion.
- Foreign body when aspirated is lodged in the right middle and inferior apical lobe.
- Bilateral pleural effusion-nephrotic syndrome, constrictive pericarditis and congestive heart failure.
- Commonest cause of massive hemoptysis-bronchiectasis.
- Ascites: Transudative ascites-cirrhosis, CHF, nephritic syndrome.
Exudative ascites in bronchial carcinoma, tuberculosis. - Earliest manifestation of pulmonary embolism-hemoptysis.
- Clubbing is seen earliest in emphysema.
- Minimum amount of air required in acute massive pulmonary emboHsrn-30 ml.
- Lung abscess is most common in left lower lobe.
Renal system:
- Increase in ADH secretion causes increased permeability to water in distal convoluted tubule and collecting duct.
- Amyloidosis of kidney-associated with retinitis, ulcerative colitis, and hematuria.
- Renal involvement of multiple myeloma is characterized by hematuria.
- Except for sodium, concentrations of creatinine, potassium, and uric acid increase in renal failure.
- Polyurea is seen in hypercalcemia, glycosuria, and hypokalemia:
- Penicillin, gentamycin, vancomycin, erythromycin, doxycycline, INH do not require major change in dose in case of chronic renal failure.
- Increased secretion of aldosterone causes an increase in angiotensin secretion.
- Potassium, hydrogen & creatinine are added to urine by tubular secretion except urea.
- In acute glomerulonephritis erythrocytes and casts are seen in urine.
- In nephritic syndrome edema, proteinuria, hypoalbumenimia are seen.
- GFR ceases when systolic BP falls below 70 mm Hg.
- Green urine-seen in oxalate poisoning.
- Renal calculi calcium oxalate.
CNS:
- Aphasia-lesions in the cerebral cortex.
- Ataxia-lesion in the basal ganglia & Tremors
- Romberg’s sign-posterior column lesion.
- Oxicephaly-associated with early closure of frontal and sagittal sutures.
- Parkinsonism-reduced levels ofdopamine. Due to damage to basal ganglia and associated with lead pipe rigidity.
- Schizophrenia-raised levels of dopamine.
- Treatment-phenothiazine.
- Alzheimer’s disease-deficiency of acetyl choline.
- Treatment-physostigmine.
- Upper motor neuron palsy-cogwheel type spastic paresis.
- Lower motor neuron palsy-flaccid palsy.
Hepatobiliary and GIT:
- Minimum fluid to detect ascites-300 cc.
- Ketone bodies seen in uncontrolled diabetes mellitus and starvation.
- Syndrome associated with impaired hepatic intake of bilirubin-Gilbert’s syndrome.
- Nutmeg liver-CVC liver.
- Jaundice is evident in the sclera when serum bilirubin is more than 0.5 to 1 mg %.
- Alkaline phosphatase-raised levels in obstructive jaundice.
- Kayser-Fleischer ring (K – F ring) is seen in hepatolenticular degeneration and Wilson’s disease (copper poisoning).
- Flapping tremors-carbon dioxide poisoning, uremia, hepatic failure.
- Honeycomb liver-actinomycosis.
- Foaming liver-gas gangrene.
- Liver function test is abnormal when 80% of the liver is damaged.
- Most sensitive liver function-prothrombin.
- Heartburn- reflux oesophagitis.
- Duodenal ulcer-associated with excessive acid secretion
- Pointing sign
- Periodicity
- Rouge pain
- Pain relief on eating
- More chances of occurrence in smokers.
- Kerning’s sign and Brudiznsky’s sign-meningitis->CNS.
- Flag sign-kwashiorkor.
- Acute appendicitis-Rovsing sign, Murphy’s sign and Moymhan signs are seen.
- Phenylketonuria-phenylalanine hydroxylase deficiency.
- Anterior wall of duodenal ulcer has maximum chances for spontaneous regression.
- Old blood-acidic, reduced oxygen carrying capacity, poor red cell definability. Reduced 2, 3 DPG
- CSF glucose levels are normal in viral infections and decreased in all other infections.
- In TB meningitis-CSF sugar is low; unchanged- neoplasms.
- Glycokinase is deficient in diabetes mellitus.
- 1 unit of insulin neutralizes 2.5 g of glucose.
- Addison’s disease-reduced serum sodium
- Best treatment of SLE-corticosteroids.
- Forscheimer spots-rubella.
- Antacids in duodenal ulcers are given 1 hour after meals and at night.
- Glycogen storage disease can cause xanthomas.
- Common cold-rhinovirus.
- Folic acid is best absorbed as monoglutamate.
- Complications of mumps: In children-aseptic meningitis; In adults-orchitis.
- Tersilian sign-reddish appearance of Stenson’s duct in mumps.
General Medicine - Infectious mononucleosis is characterized by antibodies to EB V, heterophile antibodies, and anti I antibodies.
- Massive splenomegaly kala azar, chronic lymphatic leukemia, lipid storage diseases. Dane particle-HBV.
- Engerix B vaccine-vaccine against hepatitis B provides immunity to HBV by active immunity and gamma globulin production; given at 0, land 6th month. Booster doses given at 5 years.
- Tuberculosis of adrenal gland-causes Addison’s disease.
- Primary toxic goiter-Grave’s disease.
- Secondary toxic goiter-Plummers disease.
- Thalassemia-HbA2
- Fever
- Saddle back fever-dengue
- Step ladder fever-typhoid
- Pell Ebstein fever-brucellosis and Hodgkin’s disease
- Double rise of temperature in a day-kala azar.
- INH toxicity-treating by IV pyridoxine + gastric lavage.
- Strongyloides is the only parasite that completes its entire life cycle in man. Seen in immunocompromised individuals.
- AML-characterized by Auer bodies in blast cells.
- Barr body represents genetically inactive X chromosome.
- Sex chromatin can best be studied in cells of buccal mucosa.
- Down’s syndrome-non-disjunction/translocationfrom 13/15 to 21.
- Foetal haemoglobin-A2G2.

Leave a Reply