Resin Based Composites And Bonding Agents
Question 1. Classify anterior restorative materials. Write in detail about the composition and classification of composite resin.
Or
Classify anterior restorative materials. Write in detail about composite restorative material.
Or
Write a short note on composite resin.
Or
Describe briefly composite resins.
Or
Classify composite resin material. Give the composition of composite resin.
Answer:
Tooth-colored restorative materials are:
- Composite resins
- Glass ionomer cement
- Silicate cement
- Ceramics
- Acrylic resins.
Read And Learn More: Dental Materials Question And Answers
Composite Resin:
- It is a tooth-colored restorative system.
- It is basically a resin that has been strengthened by adding silica particles.
Classification of Restorative materials
1. ISO 4049:200:
- Type 1: Polymer-based materials suitable for restorations involving occlusal surfaces
- Type 2: All other polymer-based materials and luting agents
2. Based on the curing mechanism (ISO 4049: 2009):
In this classification Type 1 and Type 2 are classified into 3 subclasses, i.e.
- Class 1: Self-cured materials
- Class 2: Light-cured materials
- Group 1: Energy applied intraorally
- Group 2: Energy applied extraoral
- Class 3: Dual-cured materials
3. Based on filer particle size (Willems, 1993):
- Fine: Particle size > 3 µm
- Ultrafie: Particle size < 3 µm
- Microfie: Average particle size–0.04 µm
- Nano: Nano range—0.005–0.01 µm
4. Based on filer particle size:
- Macro filers: 10 to 100 µm
- Midfielders: 1 to 10 µm
- Minifilers: 0.1 to 1 µm
- Microfilers: 0.01 to 0.1 µm
- Homogeneous: Contain only microfilers
- Heterogeneous: Microfillers combined with prepolymerized filers
- Splintered prepolymerized particles
- Spherical prepolymerized particles.
- Agglomerated: Microfiler sintered to form large filer particles.
- Nanofiler: 0.005 to 0.01 µm
- Hybrid.
5. Based on viscosity:
- Conventional
- Flowable
- Packable.
6. Based on the application and commercial availability:
- Restorative composites: Direct intraoral restorations
- Hybrid composites
- Macrofiled hybrids
- Midfiled hybrids
- Minifiled hybrids
- Nanofiled hybrids.
- Microfiled
- Nanofiled
- Flowable
- Packable
- Core build-up composites.
- Hybrid composites
- Prosthodontic composites
- Provisional composites
- Luting composites
- Repair composites.
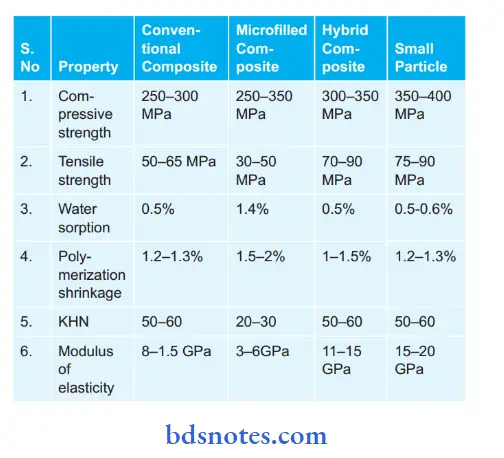
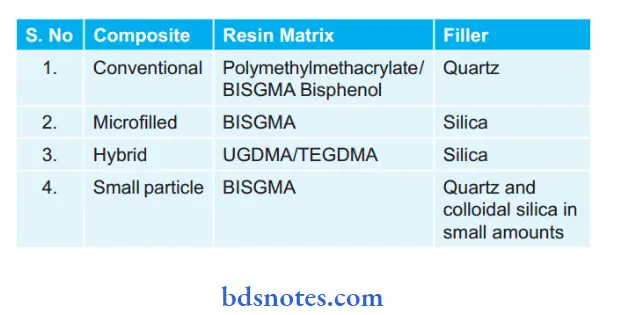
Composition of Restorative Materials
- Matrix: Plastic resin that is continue and binds the filler particles.
- Resin matrix: Commonly used Bis-GMA or urethane dimethyl acrylate.
- Fillers: Quartz colloidal silica on heavy metal glasses.
- Fillers improve the physical properties of composite resin.
- Coupling agent: Organosilanes. The coupling agent bound the filer particle to the resin matrix.
Composite resin also contains:
- Hydroquinone: Inhibitor (to prevent premature polymerization).
- UV absorbers: To improve color stability.
- Opacifirs: Titanium dioxide and aluminum oxide.
- Color pigments: To match the tooth color.
Uses of Composite Resin:
- As direct and indirect restorative material for both anterior and posterior teeth.
To Venner the metal crowns and fixed partial dentures. - As a component of fiber reinforced composites used in fier splints, FRC posts, etc.
- Chemical cures as well as dual cure resins are used as core build-up materials in post-endodontic restorations.
- For direct splinting of mobile teeth with or without glass fiber or metal wire.
- As luting agents and root canal sealers.
- Filled and unfiled composite resins are used as pit and fissure sealants.
- In bonding orthodontic brackets during orthodontic treatment.
- As aesthetic lamination.
- For repair of chipped porcelain restorations.
Question 2. Write a short note on hybrid composite resin.
Answer:
Hybrid Composite Resin:
The latest category of composite is the hybrid. These were to be developed so as to obtain better surface smoothness than that of the small particle, but yet maintain the properties of the latter. The hybrid composites have a surface smoothness and esthetics competitive with microfilmed composites for anterior restoration.
Composition of Hybrid Composite Resin:
- Two kinds of filer particles are employed:
- Colloidal silica: Present in higher concentration.
- Heavy metal glasses: Average particle size is 0.6 to 1 mm.
- Filler content: 75–80 wt% or 60–65 volume%.
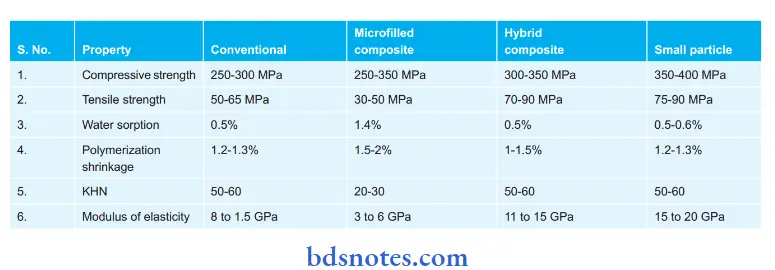
Properties Hybrid Composite Resin:
The properties range between conventional and small particles.
They are gradually superior to microfiler Compressive strength:
- It is slightly less than that of small particle composite (i.e. 240 to 290 MPa).
- Tensile strength: Comparable to small particles (i.e. 30 to 55 MPa).
- Elastic modulus: It ranges between that of conventional and microfiled composites (7 to 12 GPa).
- Coefficient of thermal expansion: Though CTE is high (30-40 × 10-6/°C) it is still less than that of microfiled.
- Water sorption: It corps less water than the microfiled resin (i.e. 5 to 17 mg/mm2).
- Esthetics: The surface smoothness and esthetics is competitive with microfilled composite for anterior restoration.
- Radiopacity: The presence of heavy metal glasses makes the hybrid more radiopaque than enamel. It is 2 to 5 mm, Al.
Clinical Consideration / Indication:
- The hybrid composite is widely used for anterior restorations including class IV because of its smooth surface and good strength.
- The hybrids are also being widely employed for stress-bearing restorations in class II restoration.
Question 3. Write a short note on microfiled resin.
Answer:
They were developed to overcome the problems of surface roughness of conventional composites. The resin achieved the smoothness of unfiled acrylic direct filing resins and yet had the advantage of having filers.
Composition of Microfiled Resin:
- The smooth surface is due to the incorporation of microfilers. Colloidal silica is used as the microfilers.
- The problem with colloidal silica was that it had a large surface area that could not be adequately wetted by the matrix resin.
- Thus addition of even small amounts of microfiled results in the thickening of the resin matrix.
- The colloidal silica size is (0.02 to 0.04 mm)
- Filler content: With the inclusion of pre-polymerized filers, the filer’s content is 80 wt % or 70 vol %.
Properties of Microfiled Resin:
With the exception of compressive strength their mechanical properties are inferior to the other types of composites.
Compressive strength — 250 to 350 MPa
Tensile strength — 30 to 50 MPa (lowest)
Modulus of elasticity — 3 to 6 GPa (lowest)
Hardness — 25 to 30 KHN (lowest)
Thermal expansion
Coeffient — (50 to 60 × 10-6/°C)
Water sorption — 1.4 to 1.7 mg/cm² (highest among composites)
Esthetics — The higher resin content and presence of microfilers is responsible for the increased surfacesmoothness.
Clinical Consideration / Indication:
The microfiled composite is the resin of choice of aesthetic restoration of anterior teeth, especially in non-stress bearing situations.
Question 4. Write a short note on the filers.
Answer:
Fillers are the inert materials that strengthen or improve the physical properties of many materials. Fillers are most commonly used in the composites.
Type of Fillers:
Following are the types of filers used in composite:
- Quart filers: Grinding and milling of quart is done to obtain this. These fillers are mainly indicated in conventional composites. These filers are very hard. Due to these filers restoration are difficult to polish.
- Glasses or ceramics consisting of heavy metals: Such filers provide radiopacity to resin restoration. Due to the increase in the radiopacity composites can be seen on the radiographs and this provides some aid in diagnosis. Examples of these filers are barium, zirconium, zinc, ytterbium fluoride, and strontium glass.
- Fluoride-releasing fillers: Fillers such as ytterbium trifluoride and barium aluminium florosilicate glass provide radiopacity to resin restoration.
- Colloidal Silica: Its composition and refractive index is similar to quart but it is not hard as quartz These are also known as microfilers. In microfiled composites, it is the main filer used.
Functions of Fillers:
- Fillers reinforce the resin and improves the mechanical properties of resin such as strength, hardness, etc.
- Since the resin content is less curing, shrinkage decreases and this leads to a decrease in marginal leakage.
- Fillers decrease the wear of composite resins.
- Fillers enhance the surface smoothness and subsequent esthetics of the composite.
- Fillers reduce the water sorption by resin and reduce the content of resin.
- Fillers have a lower coefficient of thermal expansion so it reduces thermal expansion and contraction.
- Fillers improve the clinical handling of resin.
- Fillers provide radiopacity and aids in diagnosis.
Question 5. Describe the physical properties, and drawbacks of composite resins.
Answer:
Drawbacks/Disadvantages of Composite Resins:
- They have high shrinkage.
- Composites are very technique sensitive.
- Composites stick to the instruments.
- They directly do not bond with tooth structure so require a dentin bonding agent.
- Composites are non-condensable.
- If restoration of composites is improperly done microleakage and recurrent caries may occur.
- Composite resins have low wear resistance as compared to metal restorations.
- The life span of composites is shorter when compared to the life span of metallic restorations.
- Composites get stained with time and can show color instability.
Question 6. Give the ideal requirements for tooth-colored restorative material. Describe the composition, advantages, and disadvantages of light-cure composite restorative materials.
Or
Name all the anterior restorative materials. Describe the composition, advantages, disadvantages, and classification of light-cure composite restorative materials.
Or
Write a brief on the composition of composite resin.
Answer:
Tooth material is often lost as a result of caries and trauma. A restorative material is a material that substitutes the missing tooth structure and restores the form and function of the tooth.
- Restorative materials are aesthetic and non-aesthetic.
- Aesthetic restorative materials are tooth-colored.
Name of Anterior Restorative Materials:
- Glass ionomer cement
- Silicate cement
- Composites
- Dental ceramics
The Ideal Requirements of Tooth-colored Restorative Materials are:
- Biologically compatible.
- Physical property should be good.
- Easily manipulated.
- Aesthetic quality.
- Economic.
- Chemically stable in the mouth.
- Biologically compatible:
- The material should be tasteless, odorless, non-toxic, non-irritating, and nonharmful to the oral tissues.
- The material should be insoluble in saliva and other fluids have been taken.
- The material should impermeable to oral fluid.
- Physical properties should be good:
- Adequate strength
- Resist to biting or chewing force, impact force, and excessive wear that can occur in the oral cavity.
- The material should also be dimensionally stable under all conditions of thermal changes and variation in loading.
- The material should also have low specific gravity and weight.
- Manipulation: Material should not produce toxic fumes.
- It should be easy to mix, insert, shape, and cure.
- It should be insensitive to handling procedures.
- The final product is easy to polish, finish and also repair.
- Aesthetic properties: Material should have the ability to match the appearance of oral tissue.
- Economic: The processing method should be low-cost, and not require complex and expensive equipment.
Light-Cure Composite Restorative Material:
“A particle-filed resin consisting of a single paste that becomes polymerized through the use of photosensitive initiator system (Camphoroquinone and an amine initiator) and light source activator (visible blue light).”
Classification of Light-Cure Composite Restorative Materials: Materials whose setting is affected by the application of energy from an external source such as blue light or heat.
These materials are subdivided as:
- Materials whose use requires the energy to be applied intraorally; this group consists of direct composite materials to be directly applied to teeth.
- Materials whose use requires the energy to be applied extraoral; this group consists of indirect composite materials for the fabrication of inlays and onlays.
Composition of Light-Cure Composite Restorative Materials: The light source activator is a tungsten halogen bulb of blue light with a wavelength between 400 to 500 nm.
These are single-paste systems containing:
- Photoinitiator: Camphoroquinone (0.25 wt%)
- Amine accelerator: dimethylamino ethyl methacrylate (DEAEMA 0.15 wt %).
Advantages of Light-Cure Composite Restorative Materials:
- Mixing is not required therefore less porosity, less staining, and increased strength.
- An aliphatic amine can be used in state of an aromatic amine as required for chemically cured resin, this enhances color stability.
- Control of working time.
- Insertion and contouring is possible before curing.
- Quick cure with no air bubbles.
- Reduction in laboratory procedures.
- Reduction in patient appointments.
Disadvantages of Light-Cure Composite Restorative Materials:
- Limited curing depth (maximum 2 mm thickness).
- Relatively poor accessibility in certain posterior and interproximal locations.
- Variable exposure time because of shade (hue, value, and chroma). Longer exposure time for darker shade.
Question 7. Write a short note on light-cure composite resin.
Or
Write a short note on light-cure composite.
Answer:
“A particle-filed resin consisting of a single paste that becomes polymerized through the use of photosensitive initiator system (Camphoroquinone and an amine initiator) and light source activator (visible blue light).” is known as light-cure composite resin.
Classification of Light-cure Composite Restorative Materials:
Materials whose setting is affected by an application of energy from an external source such as blue light or heat.
These materials are subdivided as:
- Materials whose use requires the energy to be applied intraorally; this group consists of direct composite materials to be directly applied to teeth.
- Materials whose use requires the energy to be applied extra orally; this group consists of indirect composite materials for fabrication of inlays and onlays
Composition of Light-Cure Composite Restorative Materials: The light source activator is a tungsten halogen bulb of blue light with a wavelength between 400 to 500 nm.
These are single-paste systems containing:
- Photoinitiator: Camphoroquinone (0.25 wt%)
- Amine accelerator: dimethylamino ethyl methacrylate (DEAEMA) 0.15 wt %.
Light Activation of Direct Composites:
Initiation:
- Camphoroquinone/amine-photoinitiator/co-initiator system.
- Blue light (400-550 nm wavelength) activates camphor quinone and converts it to an excited state.
- The activated camphor quinone reacts with a co-initiator to form free radicals starting the polymerization process (activation and initiation stages).
- The free radical reacts with a monomer molecule and propagates the polymerization process (propagation).
Propagation and Chain Growth:
- Free radical joins with the monomer molecule and forms a covalent bond with it.
- This complex also releases a free radical which seeks another monomer molecule.
- This process continues till all C=C bonds are converted to C–C bonds.
- During polymerization the molecules group together to form a high molecular weight complex.
- This grouping of molecules results in less intermolecular distance which is seen clinically as volumetric shrinkage.
Properties of Light Activated Resin:
- It is a single-paste system.
- Mixing of pastes is not required in this system and results in less porosity.
- Light-activated resins are less sensitive to oxygen inhibition
- Since the resin does not cure till a light source is shown on it there is ample working time to manipulate the resin.
- The light-activated resin also allows incremental curing and results in a tightly compacted restoration.
- Polymerization is peripheral (towards the light source).
Extraoral Cure or Light Activated Indirect Composite Resins:
- Extraoral cure refers to light-activated composite resin restorations made in the laboratory and cured using a special curing unit.
- Extraoral heat or light results in a higher level of cure of the material since all portions of the restoration is cured in a uniform manner.
- It is used with the indirect technique, i.e. fabricated in the laboratory—inlays, crowns, and veneers.
Procedure or Light Activated Indirect Composite Resins:
- Chemical or light-cured composite is used to fill the cavity contours in the model.
- The model with the resin is transferred to an oven for light curing.
- The cured restoration is removed from the model and is finished and polished.
- The restoration is cemented with resin-based composite cement.
Advantages of Light Activated Resins:
- Mixing is not required therefore less porosity, less staining, and increased strength.
- An aliphatic amine can be used in the state of an aromatic amine as required for chemically cured resin, this enhances color stability.
- Control of working time.
- Insertion and contouring is possible before curing.
- Quick cure with no air bubbles.
- Reduction in laboratory procedures.
- Reduction in patient appointments.
Disadvantages of Light Activated Resins:
- Limited curing depth (maximum 2 mm thickness).
- Relatively poor accessibility in certain posterior and interproximal locations.
- Variable exposure time because of shade (hue, value, and chroma). Longer exposure time for darker shades.
Precautions or Light Activated Indirect Composite Resins:
- Resin paste should not be dispensed until it is to be used. Exposure to operatory lights for any appreciable time can initiate the polymerization of material.
- Exposure to sunlight should be avoided.
- Unused composite should never be returned to the syringe or kept for future use.
- Storage should be in a cool and dry environment to maintain the shelf-life of all composites.
- High-intensity light can cause retinal damage if one looks directly. Use protective eyeglasses.
Question 8. Describe briefly acid-etching.
Or
Write a short note on acid-etching in composite resin.
Or
Write a short note on the acid-etch technique.
Or
Write in brief about the acid-etch technique.
Answer:
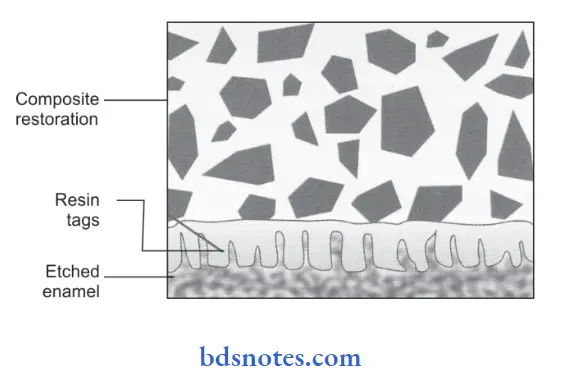
The acid-etch technique is one of the most effective ways of improving the bond and marginal seal between resin and enamel.
Mode of Action
- It creates microporosities by discrete etching of the enamel rod centers, or peripheries, or both.
- Etching increases the surface area.
- Etching enamel has a high surface energy, allowing the resin to wet the tooth surface better and penetrate into the microporosities.
- When polymerized, it forms resin tags which form a mechanical bond to the enamel.
- These resin tags may penetrate 10 to 20 mm in enamel porosity.
Used of Acid-etching: 37% phosphoric acid is used for etching.
Types of Acid-etching:
- Liquid etchants
- Gel etchants
The Technique of Application for Liquid Etchants:
Liquid etchants are used primarily to etch large surface areas of enamel, such as for veneers or sealants.
- Common types of applicators include small cotton pellets, foam sponges, and brushes.
- Gently apply the acid to the appropriate enamel surfaces to be restored, keeping the excess to a maximum of 0.5 mm past the anticipated extent of restoration.
- For preparations involving the proximal area, a polyester strip is placed before acid-etching to prevent the etching of the adjacent tooth.
- The application of acid is repeated every 10-15 seconds to keep the area moist for 30 seconds.
- A shorter etching time is advised as it yields acceptable bond strength in most cases and it also conserves enamel and saves time.
Care is to be taken not to flood the area with acid or to rub the enamel
- The acid is rinsed of thoroughly with a stream of water for 10-15 seconds after etching the tooth.
- If cotton roles were used for isolation, it should be replaced at this time, ensuring that the cavity preparation does not become contaminated with saliva.
- Now this tooth surface is dried with clean air for 20 seconds.
- Enamel that has been properly air-dried is described as having a ground glass or white frosted appearance.
The Technique of Application for Gel Etchants:
- For the application of a gel etchant, a brush paper point instrument or syringe are used to place the etchant onto the prepared enamel.
- Leave the surface untouched for 30 seconds after the application etchant.
- Rinse for 20 to 30 seconds with water.
- Dry the tooth surface.
Question 9 . Describe briefly the advantages and disadvantages of composite resin.
Answer:
Advantages of Composite Resin:
- Composites are highly esthetic restorative materials.
- Working time is quite good due to the multiple curing system.
- The placement of composites is very easy.
- They are moderately strong and durable.
- Corrosion does not occur in composites.
- Composites are easily repaired
Disadvantages of Composite Resin:
- They have high shrinkage.
- Composites are very technique sensitive.
- Composites stick to the instruments.
- They directly do not bond with tooth structure so require a dentin bonding agent.
- Composites are non-condensable.
- If restoration of composites is improperly done microleakage and recurrent caries may occur.
- Composite resins have low wear resistance as compared to metal restorations.
- The life span of composites is shorter when compared to the life span of metallic restorations.
- Composites get stained with time and can show color instability.
Question 10. Describe tooth-colored materials used in dentistry.
Answer:
The tooth-colored/aesthetic restorative materials give a natural tooth-like appearance.
Examples of aesthetic restorative materials are:
- Composite resin
- Acrylic resin
- Glass ionomer cement
- Silicate cement
- Porcelain
Question 11. Write a short note on flowable composites.
Answer:
Flowable composites are characterized by the presence of filer parties that have particular sizes similar to that of hybrid composites but filer content is reduced which results in a decrease in viscosity.
The following are the features of flowable composites:
- Filler content is 20–25%.
- Because of less filer amount flow is increased.
- The depth of cure is 6 mm.
- Stickiness to the instrument makes it difficult to smoothen the material.
- Mechanical properties of material like compressive strength, diametric tensile strength, biaxial flexural strength, and toughness values are about 60–90% of those of conventional composites.
Application of flowable composites:
- Used as filling material in low-stress bearing areas.
- Useful in areas of difficult access like in repairing amalgam, composite and crown margins, pit and fissure, preventive resin restoration
- Useful for repairing porcelain.
- Resurfacing worn composite or glass ionomer restorations for rebuilding worn contact areas in composite restorations.
- Tunnel restorations
- Core build-up
- Veneer material
- Cementing agents for porcelain restorations.
- As liner in class I and class II restorations.
Contraindication: In classes I, II, and IV restorations because of high stress.
Advantages of Flowable Composites
- It forms a thin layer over a composite over a hybrid layer which eliminates air entrapment.
- Due to high flexibility, it acts as a stress reliever in high-stress concentration areas such as cervical areas.
- Flowable composite increases marginal adaptation in the gingival marginal area in class II restoration and decreases microleakage.
The disadvantage of Flowable Composites:
- Due to the lower filer load flowable composite exhibits high curing shrinkage and low mechanical properties.
Question 12. write in detail about the physical and chemical properties of composite resins.
Answer:
Physical Properties of Composite Resins:
Chemical Properties of Composite Resins:
Question 13. Write a short note on BisGMA and TEGDMA.
Answer:
BisGMA is one of the first multifunctional methacrylates used in dentistry.
- BisGMA was developed by RL Bowen (Bowen resin) in the early 1960s.
- The BisGMA resin is an aromatic ester of a methacrylate, synthesized from an epoxy resin (ethylene glycol of phenol A) and methyl methacrylate.
- Because BisGMA has two-OH groups that form hydrogen bonds between the monomers, it is extremely viscous.
- The high viscosity of BisGMA makes it very difficult to blend and manipulate, thus it is necessary to use lower molecular weight, highly fluid monomers to dilute BisGMA.
- A low-viscosity methacrylate such as trimethylene glycol dimethacrylate (TEGDMA) is blended with it to reduce viscocity.
- TEGDMA also has the advantage of producing extensive cross-linking among polymer chains. This results in a rigid resin matrix that is highly resistant to softening and/or degradation by heat and solvents such as water and alcohol.
Question 14. Discuss in detail anterior restorative materials and setting mechanism.
Answer:
Anterior restorative materials are:
- Composite resins
- Glass ionomer cement
- Silicate cement
- Porcelain
- Acrylic resins.
Thermal Properties:
- Thermal Expansion Coefficient: Thermal expansion can create additional strain on tooth resin bond, in due course of time this can cause material fatigue, bond failure, and also percolation of fluid in gaps. In ideal conditions, the thermal expansion coefficient of a restorative material should be close to the tooth structure.
- Thermal coefficient of tooth structure:
- Enamel: 11.4 × 10-6/0C
- Dentin: 8.3 × 10-6/0C
Thermal coefficients of various composite materials are:
- Conventional composite: 25 × 10-6/0C
- Microfiled composite: 55 to 68 × 10-6/0C
- Hybrid composite: 25 to 38 × 10-6/0C
- Small particle composite: 19 to 26 × 10-6/0C
Composites with high resin components such as microfiled resin show more thermal expansion coefficient.
Thermal Conductivity:
Thermal conductivity is the rate by which either heat or cold is transmitted through restoration. Ideally, restorative materials have low thermal conductivity for decreasing the transfer of excessive thermal stimuli to pulp.
The following are the thermal conductivity of composite materials:
- Microfiled composites: 12 to 15 × 10-4Cal/Sec/cm2.
- Hybrid composite: 25 to 30 × 10-4Cal/Sec/cm2.
Dimensional Stability:
Hygroscopic expansion which starts 15 min after polymerization reaches its equilibrium in 7 days. Microfilmed composites show more expansion as compared to hybrid varieties.
Retention of Thermal Conductivity: Composites adhere to tooth structure by micromechanical retention with the help of bonding agents.
Esthetics of Thermal Conductivity:
Composites are highly aesthetic materials and are supplied in various shades. In nano field and microfiled composites high resin content and the presence of microfibers lead to increased surface smoothness.
Composites with large filers have decreased surface smoothness which produces staining over a period of time.
Biocompatibility of Thermal Conductivity:
Properly polymerized composites are biocompatible till there is a proper thickness of dentin. In some cases where the pulp is exposed, pulp capping along with glass ionomer liner is done.
In proximity to gingival tissues correct technique is employed so that inflammatory responses should be prevented which are associated with overhangs and microleakage.
Solubility of Thermal Conductivity:
The solubility of resin-based composites is of concern as inorganic ions present as filers can leach into the surrounding environment causing the breakdown of restoration.
ADA specification requires that water sorption of all materials be less than or equal to 40 µm g/mm and solubility of all materials be less than or equal to 7.5 µm g/mm. Higher values of water sorption and solubility lead to reduced wear, abrasion resistance, and color instability.
The radiopacity of Thermal Conductivity:
To evaluate the integrity of composite resin radiographically the resin needs to be radiopaque. Radiopacity is provided by filers such as glass ceramics which consist of heavy metals, i.e. barium, strontium, and zirconium.
ADA specification no. 27 requires that composite resins have radiopacity equivalent to 1 mm of aluminum which is equal to dentin.
Setting Mechanism of Composite:
Settling of composite occurs through polymerization, so the method is known as polymerization.
- Chemically Activated Composite Resins: Self-cure resin occurs in a two-paste system, i.e. base paste and catalyst paste. The base paste consists of a benzoyl peroxide initiator and the catalyst paste consists of a tertiary amine activator. When two pastes are spatulated the amine reacts with benzoyl peroxide to form free radicals which starts polymerization.
- Light Activated Composite Resins: Light activation in visible light curing ranges between 460 and 470 nm wavelength. On activation, a photoinitiator, i.e. camphor quinone combines with an amine accelerator and releases free radicals which start the polymerization.
- Dual Cure Resins: A combination of chemical and light curing is used to overcome some of the drawbacks of light curing. Dual cure resins are supplied in two pastes. When they are mixed together a slow reaction is initiated. After the initial light cure, the remainder of the resin cures over a period of time by a chemical process.
Question 15. Write a short note on nanocomposite.
Answer:
- A new type of composite resin based on nanosized filer particles has recently been introduced.
- Nanocomposites are similar to microfilmed composites comprising uniformly sized nanofillers.
- The predominant fillers are zirconium/silica or nano-silica particles measuring approximately 5 to 25 nm and nano aggregates of approximately 75 nm.
- The aggregates are treated with silane so that they bind to the resin.
- Nanocomposites are highly polishable.
- They have tooth-like translucency with excellent esthetic.
- They have good color stability.
- They have high wear resistance.
- They can be used for both anterior and posterior
- restorations and splinting teeth with fiber ribbons.
- Some commercially available nanocomposites are Filtek Supreme Plus and Filtek Z250 XT, tetric N cream, etc.
Advantages of Nanocomposite:
- As the particle size of the nanocomposite is small a better finish and surface texture is achieved.
- Biodegradation of material over time decreases.
- Nanotechnology enhances the mechanical properties of composite resin making it ideal for the restoration of both
anterior and posterior teeth. - As particle size is small it allows more volume of filer particles and decreases polymerization shrinkage.
- Less cuspal deflection and a decrease in the micro-fissures in enamel margins lead to less marginal leakage,
discoloration, and postoperative sensitivity.
Question 16. Write a short note on C-Factor.
Answer:
The magnitude of stress depends on the composition of the composite and its ability to flow before gelation occurs. This is influenced by the shape of the cavity and can be overcome by the way the dentist places the material into the cavity. This has been termed a configuration factor or C-factor.
- It is the ratio of bonded to unbonded surfaces.
C-Factor = \(\frac{\text { Bonded surface area }}{\text { Unbonded surface area }}\)
- The higher the ratio the more stress is potentially incorporated into the situation.
C-Factor in Different Tooth Preparations:
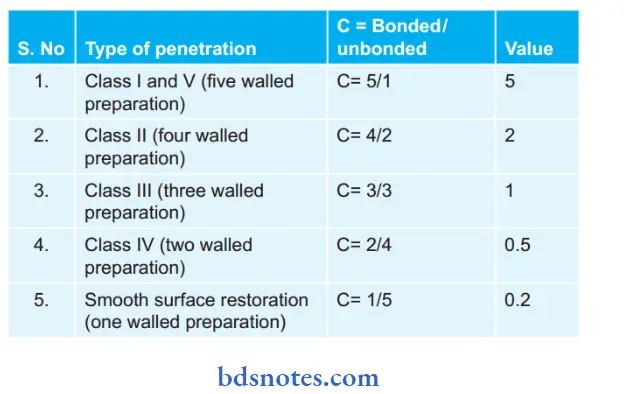
- For example, a Class I cavity with four walls and a pulpal floor will have a larger surface area that is bonded when compared to the occlusal surface area which will be unbounded.
- Similarly, a class V cavity with fixed internal surfaces also has a high C-factor.
- Cervical abrasive class V lesions have a saucer-shaped cavity design which will lower the C-factor significantly as the saucer shape is visualized as a single surface.
- As there is a small ratio of bonded to the free surface area, the flow of composite resin undergoes polymerization that occurs easily over the free area minimizing stress caused during the polymerization shrinkage.
- A relationship occurs between C-factor values and occlusal surface areas, larger is the occlusal surface area of restoration smaller is the C-factor.
- If the C-factor is more than 1, adhesion should not be maintained with conventional adhesives alone.
- In these cases, adhesive linings, different formulations of resin, and curing methods are used.
- The higher the C-value, the greater the polymerization shrinkage.
Question 19. Write a short note on dentin bonding agents.
Answer:
Dentin bonding agents are described under various generations which are as follows:
First generation (1950–1970): Mineral acids were used to etch enamel. Dentin etching was not applicable because of the belief that it may harm pulp. Glycerophosphoric acid methacrylate is used.
It is a bifunctional molecule. Hydrophilic phosphate reacts with calcium ions of hydroxylapatite. Hydrophobic methacrylate groups bonded to acrylic restorative resin. The major disadvantage was their low bond strength, i.e. 2 to 6 MPa.
Second generation (1970s): Developed as adhesive agents for composite resins which had by then replaced acrylic restorations. One system used N-phenyl glycine glycidyl methacrylate (NPGGMA).
It was proposed that the NPG portion bonded to the calcium of the tooth by chelation. Other products included phenyl-P and 2-methacrylate phenyl phosphoric acid. Bond strengths achieved were three times more than the earlier generations.
- Disadvantage: Bond strengths were still low. The adhesion was short-term and the bond eventually
hydrolyzed. - Examples: Prisma, universal bond, clear, scotch bond.
Third generation (1980s): The third-generation bond agents deal with the smear layer which is formed when dentin is cut. It was believed that the smear layer prevented proper bonding to the underlying dentin.
Complete removal by aggressive etching was contraindicated because it was believed that it protect the pulp by preventing direct contact with the monomer.
The third-generation bond agents had bond strengths comparable to that of resin to etched enamel. Thus bond strengths improved to 12 to 15 MPa.
- Examples: Tenure, scotch bond 2, prisma, universal, bond, mirage bond, etc.
Fourth generation (early 1990s): The fourth-generation systems were possible because of some important ideological breakthroughs like the total-etch technique and the development of the hybrid zone.
Research showed that acid-etching of dentin did not significantly harm the pulp as long as bacterial contamination and microleakage were avoided. Thus the total-etch technique was introduced. These bonding agents were applied in multiple steps.
- Examples: All bond 2, scotch bond multipurpose, options, etc.
Fifth generation (the mid-1990s): The fifth generation combined the primer and adhesive into one bottle (self-priming adhesive). Examples of the fifth-generation self-priming adhesives are single bond (SM), one step (Bisco), prime, and bond (Dentsply).
- Advantages:
- Application steps were reduced.
- Less technique is sensitive as it can bond to moist dentin.
- Higher bond strength.
Sixth generation (the mid to late 1990s): In this system, a separate etchant is not required. These are 2 botte systems. Two varieties are seen, i.e. Type I and Type II. Type I—two-botte two-step system. Etchant and primer are combined in one bottle (called self-etching primer). Another bottle contains adhesive.
- Examples are Clearfi SE bond (Curare), Adhese (Ivo-clair), Optibond solo plus (Kerr), Nano-bond (Pentron), etc.
- Type II—two-bottle one-step system. Liquid A contains the primer. Liquid B contains a phosphoric acid-modified resin (self-etching adhesive). Both liquids are mixed just before application. For example Xeno III (Densply), adper prompt L-pop (3M), tenure imbibed (Dent Mat), etc.
Seventh generation (early 2000): Attempts to combine all three (etchant, primer, and adhesive) into a single product. Thus, seventh-generation adhesives may be characterized as – ‘no mix self-etching adhesives, examples include iBond (Heraeus Kulzer), G bond (GC), Xeno IV (Dentsply) (glass ionomer based), Clearfi S3 (Curare). Still, the efficacy of the newer systems is to be determined.
Question 20. Brief on bonding agents.
Or
Write a short note on bonding agents.
Answer:
Current bonding agents bond to enamel and dentin so the terminology dentin bonding agent is not relevant. Usage of the terminology dentin bonding agent is limited till its evolution.
Question 21. Write a short note on composite veneer materials.
Answer:
They are also known as prosthodontic veneer composites or composites for dental indirect restorations.
- The resin may be used as a veneer, i.e. a tooth-colored layer used to hide the underlying metal for crowns and field partial dentures.
- Early materials were heat-cured poly (methyl methacrylate) improved by filers and cross-linking agents.
- Recent veneer materials are hybrid, micro, or nanofiller-reinforced resins such as Bis-GMA, urethane methacrylate or 4,8-di (methacrylic methylene), tricyclo (5.2.1.02,6)decane.
Some are further reinforced.
- The newer resins have superior physical properties and are polymerized by light or heat and pressure.
- Resins are mechanically bonded to the metal using wire loops or retention beads.
- Recent improvements include micromechanical retention created by acid-etching the base alloy and the use of chemical bonding systems such as 4-META, phosphorylated methacrylate, epoxy resin, or silicon dioxide that is flame sprayed to the metal surface followed by the application of a silane coupling agent (silicoating).
Indications of Veneer materials:
- Inlays
- Onlays
- Veneers
- Anterior crowns (metal free)
- As veneer over metal-supported crowns and FPDs.
Advantages of Veneer materials:
- Fabricate easily
- Can be repaired intraorally
- Opposite teeth undergo less wearing.
Disadvantages of Veneer materials:
- Microleakage of oral fluids and staining under the veneers due to thermal cycling and water sorption.
- Surface staining and intrinsic discoloration.
- Susceptibility to toothbrush wear
- Cannot be used in crowns serving as abutments for removable partial dentures.
- Not as durable as ceramics and PFM.
Question 22. Classify anterior restorative materials. Write in detail about step-by-step procedures for composite resins.
Answer:
Anterior restorative materials are:
- Composite resin
- Acrylic resin
- Glass ionomer cement
- Silicate cement
- Dental ceramic.
Step-by-Step Procedure for Composite Resin:
- Placement of rubber dam: Since composite resins are highly technique-sensitive contamination from blood, and saliva is avoided by the use of a rubber dam.
- Cavity preparation: Cavity is prepared and margins are beveled.
- Cleaning: The tooth is cleaned with mild abrasive
- Etching: Enamel at the cavity margin is acid-etched. Acid is rinsed and the area is dried thoroughly.
- Bonding agent: An enamel or dentin bonding agent is applied and polymerized. The cavity is now ready for the composite.
- Insertion of composite: Resins are manipulated with plastic or plastic-coated instruments.
- Metal instruments should be avoided as they may abrade and discolor the composite.
- Composites are tacky and stick to metal instruments. It is inserted into the cavity using a plastic instrument or a special syringe.
- Some manufacturers supply it in the form of a capsule which can be injected directly into the cavity with a special extruding gun.
Chemically Activated Composites:
The correct proportions of base and catalyst pastes are dispensed onto a mixing pad and combined by rapid speculation for 30 seconds. It is inserted while still plastic for better adaptation to cavity walls. Air inclusions can be avoided by swiping the material into one side of the cavity and filing the cavity from the bottom outward. The cavity is slightly overfilled. A matrix strip is used to apply pressure and avoid inhibition by air
Light Activated Composites:
The light-activated composites are single-component pastes and require no mixing. Since ambient light leads to the slow polymerization of composite resin it may lose its ability to flow. Therefore, some precautions to be observed when using light-activated materials are as follows:
- The paste is dispensed just before use.
- Avoid dispensing excessive quantities.
- The depth of cure is limited, so in deep cavities the restorations must be built up in increments, each increment being cured before inserting the next.
- Between cures, any excess material is protected by covering with a lightproof dark or orange-tinted cover
- The material hardens rapidly on exposure to the curing light. To ensure maximum polymerization a high-intensity
light unit should be used. - The light tip should be held as close as possible to the restoration.
- The exposure time should be not less than 40 to 60 seconds.
- The resin should be no greater than 2.0 to 2.5 mm thick. Darker shades require longer exposure times, as do resins that are cured through the enamel.
- Microfilmed resins also require a longer exposure.
- The high-intensity light can cause retinal damage if one looks at it directly. Avoiding looking at the light directly and use of protective eyeglasses is recommended.
Finishing and Polishing:
Finishing is best done after 24 hours during which time the polymerization is complete. However, if a subsequent appointment is not desired, finishing procedures can be started 15 minutes after curing. The initial contouring can be done with a knife or diamond stone. The final finishing is done with rubber-impregnated abrasives or a rubber cup with polishing pastes or aluminum oxide discs. The best fit is obtained when the composite is allowed to be set against a matrix or mylar strip.
Question 23.Classifytooth filling materials. Give ideal requirements for filling materials. Describe the advantages, disadvantages
Answer:
Classification of Tooth Filling Materials:
- According to the Nature of Materials:
- Metallic: Dental amalgam, direct filing gold, miracle mix, casting gold, and base metal alloys.
- Non-metallic: Dental cement, composites, and ceramics.
- According to Life Span:
- Permanent restorative materials: Dental amalgam, direct filing gold, miracle mix, casting gold and base metal alloys, composites, ceramics, and modified glass ionomer cement
- Semipermanent/intermediate: Life span is weeks to months. Modified zinc oxide eugenol cement, zinc
phosphate cement, and zinc polycarboxylate cement. - Temporary: Life span is days to weeks. Acrylic resins, zinc oxide eugenol cement.
- According to Placement:
- Anterior restorations: Glass ionomer cement, silicate cement, composites, and ceramics.
- Posterior restorations: Dental amalgam, posterior composites, metal-modified glass ionomer cement, base
metal alloys, and metal ceramics.
- According to the Technique
- Direct restorations: Dental cement, dental amalgam, direct filing gold, composites.
- Indirect restorations: Ceramics, casting gold, and base metal alloys.
- According to Hardening:
- Acid-base reactions: Dental cement except for resin cement.
- Polymerization: Composites, resin cement, compomers.
- Solidification: Casting gold and base metal alloys, ceramics
Ideal Requirements for Filling Materials:
The ideal requirements of tooth-colored restorative materials are:
- Biologically compatible.
- Physical property should be good.
- Easily manipulated.
- Aesthetic quality.
- Economic.
- Biologically compatible:
- The material should be tasteless, odorless, non-toxic, non-irritating, and non-harmful to the oral tissues.
- The material should be insoluble in saliva and other fluids have been taken.
- The material should be impermeable to oral fluid.
- Physical properties should be good:
- Adequate strength
- Resist biting or chewing force, impact force, and excessive wear that can occur in the oral cavity.
- The material should also be dimensionally stable under all conditions of thermal changes and variation
in loading. - The material should also have low specific gravity and weight.
- Manipulation: Material should not produce toxic fumes.
- It should be easy to mix, insert, shape, and cure.
- It should be insensitive to handling procedures.
- The final product is easy to polish, finish, and also repair.
- Aesthetic properties: Material should have the ability to match the appearance of oral tissue.
- Economic: The processing method should be low-cost, and not require complex and expensive equipment.
Advantages of Composite Resins:
- Composites are highly esthetic restorative materials.
- Working time is quite good due to the multiple curing system.
- The placement of composites is very easy.
- They are moderately strong and durable.
- Corrosion does not occur in composites.
- Composites are easily repaired.
Disadvantages of Composite Resins:
- It is very technique-sensitive.
- It undergoes shrinkage.
- It does not bond directly to tooth structure, it requires dentin bonding agents.
- Composite resins stick to instruments.
- Composite resin is non-condensable.
- If restoration of composites is improperly done microleakage and recurrent caries may occur.
- Composite resins have low wear resistance as compared to metal restorations.
- The life span of composites is shorter when compared to the life span of metallic restorations.
- Composites get stained with time and can show color instability.
Question 24. Classify restorative resin.
Answer:
Classification of Restorative Resin:
- Unfiled resin (no filers), i.e. acrylic resin
- Filled resin, i.e. composites
- Preventive resin, i.e. pit and fissure sealants
Question 25. Write on the uses of restorative resins.
Answer:
Following are the restorative resins, i.e.
- Unfiled resin (no filers), i.e. acrylic resin
- Filled resin, i.e. composites
- Preventive resin, i.e. pit and fissure sealants.
Uses of Unfiled Resin, i.e. Acrylic Resin:
- For making temporary crowns and FPDs.
- For denture repair, relining, and rebates.
- For making removable orthodontic appliances.
- For the construction of special trays.
- For fabrication of temporary and permanent denture bases.
- For fabricating inlay and post-core patterns.
Uses of Filled Resin, i.e. Composite:
As direct and indirect restorative material for both anterior and posterior teeth.
- To Venner the metal crowns and fixed partial dentures
- As a component of fiber-reinforced composites used in fier splints, FRC posts, etc.
- Chemical cures as well as dual cure resins are used as core build-up materials in post-endodontic restorations.
- For direct splinting of mobile teeth with or without glass fiber or metal wire.
- As luting agents and root canal sealers.
- Filled and unfiled composite resins are used as pit and fissure sealants.
- In bonding orthodontic brackets during orthodontic treatment.
- As aesthetic lamination.
- For repair of chipped porcelain restorations.
Uses of Preventive Resin, i.e. Pit and Fissure Sealants:
In newly erupted posterior teeth with deep pits and fissures should be sealed soon after eruption.
- An incipient caries lesion on pit and fisure area.
- In deep lingual pits
- In mentally or physically challenged individuals.
- In children living in non-fluoridated areas.
- Patients with xerostomia
- The margin of Class I amalgam or composite can be sealed with sealant to improve marginal integrity.
- In cases where the contralateral tooth surface becomes carious or previously restored.
Question 26. Classify dental resins.
Answer:
Classification of Dental Resin:
- Unfiled resin (no filers), i.e. acrylic resin
- Filled resin, i.e. composites
- Preventive resin, i.e. pit and fissure sealants
Question 27. Write in brief on the sandwich technique.
Answer:
In the sandwich technique glass ionomer cement is sandwiched between the tooth and composite resin restorative material. Here glass ionomer cement acts as a bonding agent.
As composite resins do not adequately bond to dentin, during polymerization a gap may result if the cavity margin is situated in dentin. This bond to dentin is improved by placing a glass ionomer liner between composite restoration and dentin.
Glass ionomer bonds to dentin via chemical adhesion, while the resin bonds mechanically to porosities and crazing present on the surface of the glass ionomer liner. For improving the retention glass ionomer can be acid-etched.
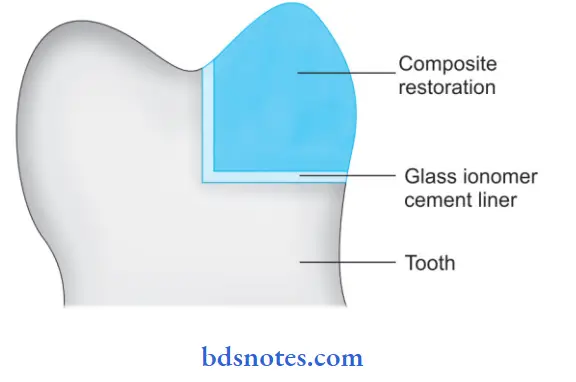
The procedure of the Sandwich technique:
- Condition the dentin and place the thin layer of GIC cement.
- The enamel portion should be etched with phosphoric acid. Some operators also etch the surface of GIC with phosphoric
acid to enhance surface roughness. - Wash the surface for 25 to 30 seconds.
- After adequate drying apply the bonding agent to the surface of the enamel and etched cement surface.
- Insert the composite resin in the usual manner.
Indications of Sandwich technique:
- In Class II composite restorations.
- Lesions where one or more margins are in dentin, i.e. cervical lesions

Leave a Reply