Composite Resins
Essentially, it is a resin that has been strengthened by adding silica particles called fillers. The pioneering research of Bowen together with the development of the acid etching technique and bonding agents, revolutionized restorative dentistry. It largely replaced the earlier silicate and restorative acrylics.
Read And Learn More: Basic Dental Materials Notes
The composite is a system composed of a mixture of two or more macromolecules, which are essentially insoluble in each other and differ in form. The composite material’s properties are superior to those of its components, e.g. fiberglass has a resin matrix that is reinforced by glass fibers.
The resulting composite is harder and stiffer than the resin matrix material, but less brittle than glass. Examples of natural composite materials are tooth enamel and dentin. Matrix is made of collagen, with hydroxyapatite crystals acting as fillers. Though the early composites were developed for restorative purposes their uses subsequently expanded to include provisional restorations, luting, etc.
Composite Resins Uses
- Restoration of anterior and posterior teeth (directly or indirectly).
- To veneer metal crowns and fixed partial dentures (prosthodontic resins).
- To build-up cores (post core).
- Bonding of orthodontic brackets, etched cast restorations, ceramic crowns, posts, inlays, onlays and laminates.
- Pit and fissure sealant.
- Esthetic laminates.
- Repair of chipped porcelain restorations.

Types
Composite resins are difficult to classify because of the wide range of overlapping filler sizes. Therefore, a wide range of classifications exist. No single classification is deemed satisfactory.
ISO 4049:2009
- Type 1 Polymer-based materials suitable for restorations involving occlusal surfaces
- Type 2 All other polymer-based materials and luting agents
Based on the curing mechanism (ISO 4049:2009)
- Type 1 and 2 are further grouped into 3 classes based on curing mechanism.
- Class 1 — Self cured materials
- Class 2 — Light cured materials
- Group 1 — Energy applied intraorally
- Group 2 — Energy applied extraoral
- Class 3 — Dual cured materials
Based on filler particle size (Willems 1993)
Willems developed an extensive classification based on a number of parameters, such as Young’s modulus, the percentage (by volume) of inorganic filler,the size ofthe main particles, surface roughness and compressive stress. Though the classification is not presented, terminology from Willems classification is still used today to describe some commercially available composites. With the inclusion of nanosized particles the particle sizes can be described as
- Fine Particle size > 3 µm
- Ultrafine Particle size < 3 µm
- Microfine Average particle size — 0.04 µm
- Nano Nano range (5–100 nm or 0.005–0.01 µm)
Based on filler particle size
Fillers play an important role in the composite performance. However, a universal system of classifying fillers has not been agreed upon. Differences exist on the nomenclature and the size range of the filler particles.
- Macrofillers (10-100 µm)
- Midifillers (1-10 µm)
- Minifillers (0.1-1 µm)
- Microfillers (0.01-0.1 µm)
- Homogenous — contains only microfilters
- Heterogenous — microfilters combined with pre-polymerized fillers
splintered pre-polymerized particles
spherical pre-polymerized particles - Agglomerated — microfilter sintered to form larger filler complexes
- Nanofillers (0.005–0.01 µm)
- Hybrid (range of sizes which usually includes micro or nanofillers with macro, midi or mini fillers
Based on viscosity
- Conventional
- Flowable
- Packable
Viscosity determines the flow characteristics during placement. A flowable composite flows like liquid or a loose gel. A packable composite is firm and offers some resistance to condensation.
Based on applications and commercial availability
- Restorative composites—direct intraoral restorations
- Hybrid composites
- Macrofilled hybrids
- Midifilled hybrids
- Minifilled hybrids
- Nanofilled hybrids
- Microfilled
- Nanofilled composites
- Flowable
- Packable
- Core build-up composites
- Hybrid composites
- Prosthodontic composites (for fabrication of inlays, veneers, crowns and FDPs)
- Provisional composites (for temporary crowns, FDPs, etc.)
- Luting composites
- Repair composites (intraoral repair of fractured ceramic or acrylic or composite veneer)




Restorative Composite Resins
The first tooth colored restorative system were developed in the late 1950s and early 1960s by Bowen (also known as Bowen’s resin). The early composite resins were generally macrofilled resins and were referred to as conventional composites. These were chemically activated. This was followed by U-V light activated and later visible light activated systems. The early composites had poor wearresistance and stained easily. This was attributed to the large sized (macrofillers) filler particles used. The introduction of the microfilled composites improved wear resistance and better esthetics. However, they had poor mechanical properties. The hybrid composites attempted to combine the esthetics and wearresistance ofthe microfilled with the mechanical properties of the macrofilled composites. The latest entry into the field – the nanocomposites holds the promise of high polishability with further improvement in mechanical properties.
Supplied Us
Composites used for restoring teeth are usually supplied as a kit containing the following
- Composite resin (either chemical or light cured)
- Etching liquid (37% phosphoric acid)
- Bonding agent
- Shade guide.
Chemically activated composite resins are available as
- Two paste (base and catalyst) system Supplied in small jars or syringes.
- Powder-liquid systems Powder (inorganic phase plus the initiator) is supplied in jars. Liquid (BIG-GMA diluted with monomers) in bottles.
Light-activated resins are available as
- Single paste form in dark or light-proof syringes

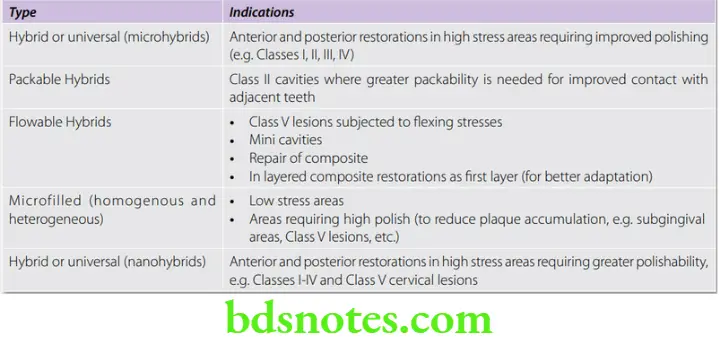
Indications For Various Composite Resins
- The indications for different products.
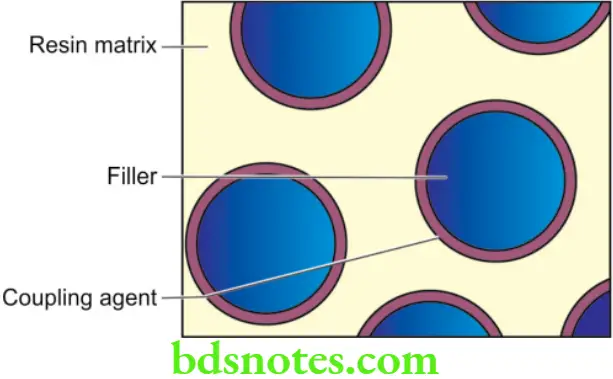
Composition And Structure
The essentials components of a composite resin
- Resin matrix/binder—Bis-GMA or urethane methacrylate
- Filler—Quartz, colloidal silica or heavy metal glasses
- Coupling agent—Organosilanes.
In addition they contain
- A curing system—Chemical or light curing chemicals.
- Inhibitors (0.01%)—Prevents premature polymerization, e.g. butylated hydroxytoluene (BHT).

- UV absorbers—to improve color stability
- Opacifiers—(0.001 to 0.007%) e.g. titanium dioxide and aluminum
- Color pigments—to match tooth color.
Resin Matrix
- Dental composites use a blend of monomers that are aromatic or aliphatic dimethacrylates. Of these, bis-GMA (Bisphenol-A-glycidyl methacrylate), urethane dimethacrylate (UDMA) and bis-EMA (Bisphenol-A-polyethylene glycol diether dimethacrylate) are most commonly used. Triethylene glycol dimethacrylate (TEGDMA) is added to control the viscosity.
- Bis-GMA was developed by RL Bowen (Bowen’s resin) in the early 1960s. Its properties were superior to those of acrylic resins. However, it had a few limitations like
- A high viscosity which required the use of diluent monomers
- Difficulty in synthesizing a pure composition
- Strong air inhibition to polymerization
- High water sorption because of diluents used
- Polymerization shrinkage and thermal dimensional changes still existed
- Like other resins it does not adhere to tooth structure
- To make it clinically acceptable, diluent monomers are added to the resin matrix to reduce the viscosity of the resin. It also allows more fillers to be incorporated.
- Diluents allow extensive cross-linking between chains, thereby increasing the resistance of the matrix to solvents. The commonly used diluent monomer is TEGDMA (triethylene glycol dimethacrylate). Thus composite resins have to be blended with different monomers to optimize their properties.
- Drawbacks of TEGDMA include
- High shrinkage.
- Contributes to reduced shelf-life by migration in to the plastic walls.
- Being hydrophilic it makesthe composite susceptible to moisture leading to thickening or softening of the paste in certain climatic conditions.
(Because ofthese drawbackssome manufacturers have replaced the majority of the TEGDMA with a blend of UDMA and bis-EMA).
The refractive index is an important property for anterior restorative materials. To have acceptable esthetics composite resins must match the translucency of enamel. Bis-GMA and TEGDMA have a refractive index of 1.55 and 1.46 respectively which average to around 1.5 when combined together.
Filler Particles
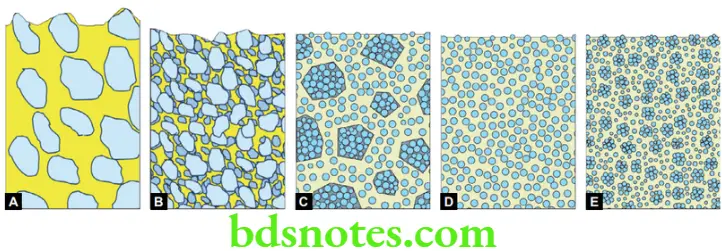
Fillers play a crucial role in the composite resin. Most of the important properties of the resin is determined by its filler content. Composite fillers are classified by material,shape and size.
Many different classifications of fillers have been proposed. They are broadly classified into 3 groups- macrofillers, microfillers and nanofillers. A mixture of different particle sizesisreferred to as a hybrid. For details of fillersize and nomenclature see‘classification of composite resins.’
Functions of fillers
The addition of filler particles into the resin significantly improves its properties.
- Improves strength—Fillers reinforce the resin and improve mechanical properties like strength, stiffness, hardness, etc.
- Reduces shrinkage—As less resin is present, the curing shrinkage is reduced thereby reducing marginal leakage.
- Reduces Wear—Fillers play a crucial role in reducing the wearing of composite resins. The smaller the size and higher the concentration of fillers the better the wear resistance.
- Surface smoothness and esthetics—Fillers affect the surface smoothness and subsequent esthetics of the composite. The smaller the particle size, the greater the polishability. Larger particle sizes in the early composites contributed to surface roughness and staining.
- Reduces water sorption—Resins absorb water and makes it more prone to wear and staining. Filler reduce water sorption by reducing the overall resin content.
- Reduces thermal expansion and contraction—Fillers have a lower CTE in comparison to the resin.
- Improves clinical handling (increased viscosity makes them easier to handle clinically).
- Imparts radiopacity—Radiopaque fillers help improve diagnostics (e.g. caries detection through roentgenograms, etc.).
Important attributes of fillers
Important attributes of fillers, that determine the properties and clinical application of composites are
- Amount of filler added (filler loading)
- Size of particles and their distribution
- Shape of fillers
- Index of refraction
- Radiopacity
- Hardness
Filler size The size of the fillers affect the surface smoothness and the wear resistance. The smaller the fillers the greater the surface smoothness. Microfilled composites have the best surface smoothness and lowest wear. This is because the particles are removed at the same rate as the resin matrix if they are smaller. Larger particles result in a rougher surface. The introduction of the nanoparticles hold great promise of improved smoothness, good wear resistance as well as improved mechanical properties.
Filler loading Filler loading refers to the amount of fillers that can be practically incorporated into the resin. The amount of filler that can be added depends on the type of filler and the purpose for which it is intended. Most hybrid composites have a filler loading ranging from 60 to 70% volume. The introduction of the newer nanofillers allow a greater filler loading of up to 79.5% vol. Microfillers thicken the resin quickly. Thus microfilled resins usually do not have the same filler loading as resins with larger particle sizes such as the hybrids.
Particle size distribution Most modern hybrid composites have particle ranges in size from 0.01 to 10 µm. Microfillers are usually in the range of 0.01 – 0.07 (average 0.04 µm). In order to increase the filler amount in the resin, it is necessary to add the fillersin a range of particle sizes. If a single particle size is used, a space will exist between the particles. Smaller particles can then fill up these spaces, thus increasing the filler content.
Shape of fillers Based on shape 3 types of fillers are used—irregular, spherical, and fibrous. The shape affects the filler loading and the handling characteristics of the composite.
Refractive index For esthetics, the fillers should have a translucency similar to tooth structure. To achieve this, the refractive index ofthe filler should closely match that ofthe resin. Most glass and quartz fillers have a refractive index of 1.5, which matches that of bis-GMA and TEGDMA.
Measurement of filler content—volume versus weight percentage
Filler content is designated in percent volume (vol.%) or percent weight(wt.%).Weight percent is usually higher in value than percent volume. The volume percentage may be a more reliable indicator of filler content than the weight percentage. This is because of differences in density between different fillers. For example, composites can have a similar volume percentage of fillers yet different weight percentages. This is because the composite containing a larger fraction of heavy metal glass fillers will have a higher weight percentage.
Fillers Types
Composite resins may contain a variety of fillers
- Ground quartz
- Glasses or ceramic containing heavy metals
- Boron silicates
- Lithium aluminum silicates
- Ytterbium trifluoride
- Colloidal silica
Quartz filters are obtained by grinding or milling quartz. They were mainly used in conventional composites. They are chemically inert and very hard. This makes the restoration more difficult to polish and can cause abrasion of the opposing teeth and restorations.
Glasses/ceramics containing heavy metals These fillers provide radiopacity to the resin restoration. Increased radiopacity makes composites detectable on radiographs which aid diagnostics. Examples are barium, zirconium, ytterbium fluoride, zinc, and strontium glasses. The most commonly used is barium glass. It is not as inert as quartz. Some barium may leach out with time.
Fluoride releasing fillers Some current composites have fluoride releasing capability. This includes fillers like ytterbium trifluoride and Ba-Al-fluorosilicate glass. In one commercial product (Tetric ceram) the YbF3 content is as high as 17 wt.%. The Ba-Al-fluorosilicate glass content was 5 wt.%.
Colloidal silica They have the same composition and refractive index as quartz but not as hard or abrasive. This is due to their ‘amorphous’ (or noncrystalline) form. They are also referred to as microfilters.
They are obtained by a pyrolytic or precipitation process. Colloidal silica particles have a large surface area (50 to 400 m2/g), thus, even small amounts of microfilters thicken the resin. They are added in small amounts in hybrid composites (5 wt.%) to adjust the paste viscosity.
The hybrid varieties have a microfilter loading of 10 to 15% weight. In microfilled composites, it is the main filler used (20 to 59%volume). Since they cannot be added in large amounts the overall filler loading of microfilled composites is lower than conventional or hybrid varieties.
Methods To Increase Microfiller Loading
Manufacturers are constantly on the lookout for methods to increase the filler content of the microfilled composites.
- One method is to sinter(fuse)the colloidal silica particles, thereby reducing surface area. These are known as agglomerated silica.
- Addition of prepolymerized fillers This is the more common method. Also known as ‘organic fillers’. They are prepared by adding 60 to 70 wt.% of silane-coated colloidal silica to the monomer, which is held at a slightly higher temperature to reduce its viscosity. It is then heat-cured and ground.
The composite is obtained by adding these prepolymerized fillers along with more silane coated microfillers into unpolymerized resin matrix.
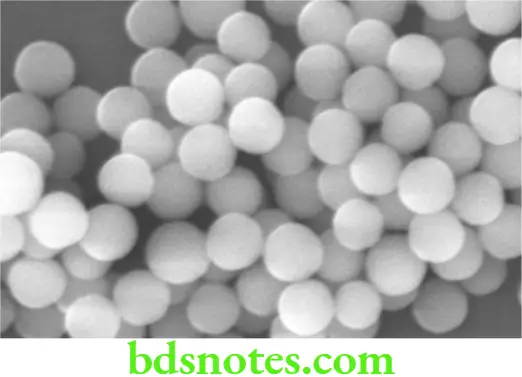
Silica nanoparticles These are currently the smallest filler particles used in dental composites. Nanoparticles are defined as particles between 1 and 100 nanometers in size. Innano technology, a particle is defined as a small object that behaves as a whole unit with respect to its transport and properties.
Adoption of nanoparticle technology have ushered in the next generation of composite resins. Incorporation of silica nanoparticles into the composite resins have improved many of the properties of composite resins, particularly wear resistance and polishability. Nanoparticles in composites can be used in 2 forms.
- Nanoparticle—a single nanoparticle (size ranges from 5-25 nm)
- Nanoclusters—a group of nanoparticles (forms larger-sized particles).
Manufacture of fillers
Filler particles can be generated: (1) by crushing, grinding, and sieving large blocks of ceramic, (2) by condensation of SiO2 from the vapor phase as small droplets of microfiller, or (3) by precipitation of filler particles from solution (sol-gel). The smallest fillers can only be manufactured practically from the vapor phase or by sol-gel processes.
Coupling Agents
Coupling agents bond the filler particles to the resin matrix. The earliest composites did not use coupling agents. This resulted in microscopic defects between the filler and surrounding resin. Microleakage of fluids into these defects led to surface staining and failure. Typically the manufacturer treats the surface of the filler with a coupling agent to bond the filler to the resin matrix.
Functions of coupling agents
- They improve the properties ofthe resin through transfer of stresses from the more plastic resin matrix to the stiffer filler particles.
- They prevent water from penetrating the filler-resin interface.
- They bond the fillers to the resin matrix thereby reducing the wear.
The most commonly used coupling agents are organo silanes (i.e. 3-methacryloxypropyltrimethoxysilane).
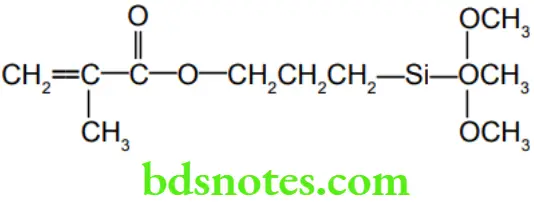
The agent is a molecule with a methacrylate groups on one end and methoxy groups(OCH3) on the other end. In the presence of adsorbed water, the methoxy groups hydrolyze to form silanol groups(-Si-OH)which then form ionic bonds with the silanol groups of the filler forming a siloxane bond (-Si-O-Si-).
The other end has a methacrylate group which forms a covalent bond with the resin when it is polymerized. This completes the coupling process. Zirconates and titanates can also be used as coupling agents.
Polymerization (Setting) Mechanisms
They polymerize by the addition mechanism that is initiated by free radicals as described in resins. The free radicals can be generated by chemical activation or external energy (heat, light or microwave).
Based on the mode of activation of polymerization, there are three main types
- Chemically activated resins
- Light-activated resins
- Combination of the above (dual cure).
Chemically Activated Composite Resins
This is a two-paste system
- The base paste contains—benzoyl peroxide initiator
- Catalyst paste—tertiary amine activator (i.e. N, N-dimethyl-p-toluidine).
Setting
When the two pastes are spatulated, the amine reacts with the benzoyl peroxide to form the free radicals which start the polymerization.
Disadvantages
- No control of curing time.
- No control of curing shrinkage.
- Hand mixing increases the possibility of voids.
Light Activated Composite Resins
Under normal light, they do not interact. However, when exposed to light of the correct wavelength the photoinitiator (camphorquinone) is activated and reacts with the amine to form free radicals which then start the polymerization.
UV light-activated systems
The earliest systems used ultraviolet (UV) light for curing. Light activation puts control of the working time in the hands of the dentist.
Limitations of UV light curing were
- Limited penetration of the light into the resin. Thus, it was difficult to polymerize thick sections.
- Lack of penetration through tooth structure.
Visible-light activated resins
These have replaced UV light systems. They are also more widely used than the chemically activated resins.
These are single-paste systems containing
- Photoinitiator: Camphorquinone 0.2 wt.%
- Amine accelerator: Dimethylaminoethyl-methacrylate (DMAEMA 0.15 wt.%).
Camphorquinone has a light absorption range between 400 and 500 nm. This is in the blue region ofthe visible light spectrum. In some cases, inhibitors are added to enhance its stability to room light or dental operatory light.
Dual Cure Resins
- A combination of chemical and light curing is used to overcome some of the drawbacks of light curing. Dual cure resins are supplied as two pastes. When mixed a slow-setting reaction is initiated. These resins are used for cementing crowns or bulk restorations where there is limited or no light penetration. After the initial light cure, the remainder of the resin cures over some time by the chemical process.
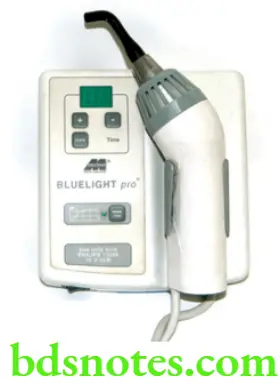
Curing Lamps
- A number of curing lights are manufactured. Most use visible light in the blue spectrum (between 400 and 500 nm). In some units the light source is remote and is transmitted to the site of restoration through a light guide which is a long, flexible fiber-optic cord. There are also hand held light curing devices which transmit the light through shortlight guides.
Important features of curing lamps
- Spectral range Light emitted by curing lamps should fall in the photo absorption spectral range of camphor quinone. This is in the violet-blue region of the spectrum and is between 400-500 nm. Some curing lamps produce light within this spectrum whereas others produce more broad spectrum light which then needs to be filtered to emit only the light in the blue range.
- Light intensity should be high for a shorter curing time and greater depth of cure. The light intensity of lamps varies from 300 to 1200 milliwatts/cm2. For maximum curing, a radiant energy of 16 J/cm2 is needed for a 2 mm thick section of composite.
Types of lamps
Currently, many forms of curing lights are available. These include
- QTH (Quartz-tungsten-halogen) These were the earliest visible light lamps. The light source is a tungsten-halogen-quartz bulb. The white light generated passes through a filter that removes all wavelengths except those in the blue range. Heat is also generated thus requiring a cooling fan. The intensity of light gradually reduces with time (aging) and so calibration is required at intervals.


- LED (Light emitting diodes) LED is increasingly popular as a light source in all spheres including dentistry ever since the discovery of the blue diode in the 1990s. It is similar in power to QTH lamps(700 mW/cm2).
- Research has shown that the curing depth and degree of conversion is significantly better with LEDs than with QTH. It emits light only in the blue part of the spectrum.
- Thus, it does not require filters. Its advantages also include low power consumption (can even be operated by batteries), no heat generation (eliminating cooling fan), and low noise (due to the absence of cooling fan).
- PAC (Plasma arc curing) These lamps generate an intense white light by ionizing xenon gas to produce plasma. Filters are required to remove heat and unwanted wavelengths. Their high power allows faster cures as well as greater depth of cures.
- Argon laser These produce light of the greatest intensity. They emit light of a single wavelength around 490 nm and therefore do not require filters. They do not produce little heat because of the limited infrared.
- However, these lamps are more expensive. They have a narrow light tip (spot size) requiring clinicians to increase the number of overlaps in case of a larger restoration.
- The high-intensity lights like the PAC and the laser provide a faster cure (as short as 5 seconds for a 2 mm section). Besides being expensive the accelerated curing can introduce substantial stresses. Further studies are needed.
Eye Protection
- Staring into the curing lights for prolonged periods can cause retinal damage. It is best to look away while the curing is in progress. Various kinds of eye protection are available and should be used when working with composites.
Degree Of Polymerization And Depth Of Cure
The total amount of resin polymerized depends on several factors.
- Transmission of light through the material This is controlled by the absorption and scattering of light by the filler particles, as well as any tooth structure interposed between the light source and the resin. For this reason, microfilled composites with smaller and more numerous particles will not cure to as great a depth as conventional composites.
- The shade of resin Darker shades require longer exposure time.
- Amount of photoinitiator and inhibitor present For polymerization to take place at any depth, a particular amount of photons must be available. This is directly related to the intensity of light and time of exposure.
- Curing time Manufacturers recommend curing times for each material and shade. This depends on the output of the particular curing device. Thus, 80 to 240 seconds is required with a low-intensity light whereas to achieve the same result, a high-intensity light requires only a 20 to 60-second exposure.
- Intensity of light Light intensity is measured in milliwatts/cm2. The time required for curing a 2 mm depth of resin by a QTH lamp is 40 seconds. The same thickness can be cured in 20 seconds if the light intensity is increased to 800 mW/cm2.
- Type of light High-intensity lights like PAC and LASER cure faster and to a greater depth than the QTH and LED-generated lights.
- Thickness of resin Thickness greater than 2–3 mm is difficult to cure because of the lack of light penetration.
- Distance from light Optimum distance is 1 mm with the light positioned 90 degrees from the surface of the resin.
Microfilled Composite
The microfilmed composites were introduced soon after the traditional composites. They were developed to overcome the problems of surface roughness of traditional composites. The resin achieved the smoothness of unfilled acrylic direct filling resins and yet had the advantage of having fillers.
Unfortunately, they could not achieve high levels of fillerloading and therefore had somewhat inferior mechanical properties when compared to the traditional composites. For this reason, these composites are primarily used for esthetic restorations in stress-free areas and in areas close to the gingiva where a smooth finish is required for reduced plaque accumulation.
Synonyms Also referred to as microfine composites.
Composition
- The smoother surface is due to the incorporation of microfilters. Colloidal silica is used as the microfilter and is the only type of filler present in this type. The problem with colloidal silica was that it had a large surface area that could not be adequately wetted by the matrix resin. Thus, the addition of even small amounts of microfilters resulted in thickening of the resin matrix. Thus, it was not possible to achieve the same filler loading as conventional composites.
- Manufacturers tried to overcome this problem by
- Using prepolymerized or organic fillers (see section on fillers). These composites were referred to as heterogenous.
- Using silica in a cluster or agglomerate form. These were referred to as ‘homogenous’ microfilmed composites.
- Filler size The colloidal silica is 200-300 times smaller than the quartz fillers of conventional composite. Size ranges from 0.04 to 0.4 µm.
- Filler content With the inclusion of prepolymerized (organic) fillers, the filler content is 70wt.% or 60 vol.%. However, the actual inorganic filler content is only 50 wt.%.
Clinical Considerations
Except for compressive strength, their mechanical properties are inferior to the other types of composites. This is because of their higher resin content(50 vol.%). Their biggest advantage is their aesthetics. The microfilmed composite is the resin of choice for esthetic restoration of anterior teeth, especially in non-stress-bearing situations.
For most applications, the decreased physical properties do not create problems. However, in stress-bearing situations like Class 4 and Class 2 restorations, they have a greater potential for fracture. Sometimes, chipping occurs at the margins.
Hybrid Composite Resins
The hybrid type forms the majority of the composites used in dentistry currently. These were developed to obtain better surface smoothness than that of the conventional large particle composites, yet maintain the properties of the latter. Hybrid composites have a surface smoothness and esthetics competitive with microfilmed composites for anterior restorations. The hybrids are generally considered multipurpose composites suitable for both anterior and posterior use.
Filler volume
- The total filler content is 75–80 wt.% or 60–65 vol.%. The overall filler loading is not as high as small particle composites because of the higher microfilter content.
Filler type
Two kinds of filler particles are employed
- Heavy metal glasses Average particle size is 0.4 to 1 µm. 75% of the ground particles are smaller than 1.0 µm.
- Colloidal silica Size—0.04 µm. It is present in higher concentrations (10 to 20 wt.%) and therefore, contributes significantly to its properties.
The hybrids are generally considered multipurpose composites suitable for both anterior and posterior use. They are widely used for anterior restorations, including class IV because of its smooth surface and good strength.
The hybrids are also widely employed for stress-bearing restorations.
Nano And Nanohybrid Composite Resins
Continued interest in the reduction of the size of fillers has led to the adaptation of nanotechnology to the field of composite resins. A new type of composite resin based on nanosized filler particles has been recently introduced.Nanocomposites (Fig. 11.6) are similar to the microfilled, comprising of uniformly sized nanofillers.Nanohybridslike the conventional hybrids, come in a range of filler sizes including nanofillers.
Unfortunately, conflicting reports exist on the efficacy of these relatively new materials. Initial reports indicate that these materials have the mechanical properties of the hybrid composites with the esthetics and polishability of the microfilmed composites.
Thus they can be used for both anterior and posterior restorations. Nanohybrids are generally stronger than nanocomposites. However, nanocomposites have improved polishability.
Continued development along these lines might eventually lead to the phasing out of conventional hybrid and microfilmed composites. However, further research is required to establish the efficacy of the nano and nanohybrid composites.
Filler Volume And Type
The predominant fillers are zirconium/silica or nano-silica particles measuring approximately 5 to 25 nm and nano aggregates of approximately 75 nm. The aggregates are treated with silane so that they bind to the resin.The aggregates and nanoparticles filler distribution gives a high load, up to 79.5%.
Properties Of Composite Resins
- Composite resins were developed after amalgam and therefore it is a useful material with which to compare restorative composite resins. The mechanical properties of these materials have steadily improved over the years.
- However, when compared to amalgam these materials are highly technique-sensitive, and therefore optimal properties can be achieved only if proper techniques of manipulation and insertion are followed.
- The common factor affecting most physical and mechanical properties of the composite is the filler content.
Hardness
Hardness determines the degree of deformation of a material and it is generally accepted as an important property and a valuable parameter for comparison with tooth structure.
To assure an optimized clinical performance of restorations, it is of paramount importance to employ materials with hardness at least similar to that of the dentinal substrate, not only superficially, but also in-depth, since an accentuated decrease in hardness would adversely affect their mechanical properties and marginal integrity.
- Enamel 343 KHN
- Dentin 70 KHN
Composites generally show lower hardness than enamel. The hardness varies between different products and depends on the amount and type of filler used.
- Hybrid 60–117 KHN
- Microfilled 22–80 KHN
- Amalgam 110 KHN
Factors affecting hardness
- Period Composites show an increase in surface hardness with time due to continued polymerization. The best results are seen 7 days after polymerization. For those unable to wait for a subsequent appointment a 15-minute delay is recommended before the start of polishing procedures.
- Polishing Polishing has been shown to increase the surface hardness of composites. Polishing removes the surface organic layer and exposes the harder fillers below. However, polishing is best delayed at least 24 hours after polymerization.
Polymerization Shrinkage
- Polymerization in composite resins is accompanied by a shrinkage that varies between different composites depending on the resin-to-filler ratio. Thus, the polymerization shrinkage ranges from 0.6–1.4% (in composites with higher filler content) to 2–3% (in composites with lower filler content like microfilled composites). This creates tensile stresses as high as 130 kg/cm2 which severely strains the bond and can lead to marginal leakage. Sometimes, it may also cause the enamel at the restoration margin to crack or fracture.
- The total polymerization shrinkage between light-activated and chemically-activated resins does not differ. However, the pattern of shrinkage is different (see differences). The polymerization shrinkage is highest in the case of the microfilmed composites because of the higher resin content.
- Clinical techniques to reduce polymerization shrinkage include
- Ramped curing Polymerizing the composite resin in layers or ramps.
- Soft start In this technique polymerization is initiated slowly. The device automatically begins with a low-intensity light, gradually increasing and ending with high intensity light. This gives time for stress relaxation.
- Delayed curing The restoration is partially cured with a low-intensity light. The operator continues working on the restoration and then follows it with a final high intensity exposure.
- Fabricating and curing the restoration extraorally on a cast (indirect technique) and then cementing on to the tooth, thereby completing the polymerization before cementing.
Air Or Oxygen Inhibition
- Polymerization is inhibited by air or oxygen. To avoid this the surface of the restoration should be protected by a transparent matrix strip or celluloid crown former. If the composite is unprotected during polymerization the surface of the composite remains tacky. This is known as the air or oxygen-inhibited layer (OIL).
Thermal Properties
Thermal expansion coefficient (TEC)
Thermal expansion and contraction are cyclic in the mouth and this can place additional strain on the tooth-resin bond. Over time this can lead to material fatigue, bond failure, and percolation of fluids into the gap. Ideally, the TEC of a restorative material should be close to that of tooth structure.
- Dentin 8.3 × 10-6/°C
- Enamel 11.4 × 10-6/°C
The TEC of composite resins is again related to the proportion of resin. Thus composites with higher resin content like microfilled will show a greater TEC.
- Hybrid 25–38 × 10-6/°C
- Microfilled 55–68 × 10-6/°C
Thermal conductivity
The thermal conductivity influences the rate at which heat or cold is transmitted through the restoration. Ideally, restorative materials should have low thermal conductivity to reduce the transfer of excessive thermal stimuli to the pulp.
- Hybrid 25–30 × 10-4 cal/sec/cm2 (°C/cm)
- Microfilled 12–15 × 10-4 cal/sec/cm2(°C/cm)
Water Sorption
Water sorption is related to the resin content. The water sorption of hybrid composites is comparatively lower than that ofthe microfilled resins. ISO4049 requirements limit the water sorption to a maximum of 40 µg/mm2.
- Hybrid 5–17 µg/mm2
- Microfilled 26–30 µg/mm2
Dimensional Stability
- A slow expansion (hygroscopic expansion) is associated with water sorption. The expansion which starts 15 minutes after polymerization reaches equilibrium in about 7 days. Microfilled resins show more expansion than hybrid varieties.
Retention
- Composite resins do not adhere chemically to tooth structure. Micromechanical retention together with bonding agents have to be used to enhance adhesion to tooth structure.
Esthetics
- Composites are highly esthetic direct restorative materials. Composites are supplied in a variety of shades. Special composite stains and other effects are also available to create lifelike restorations.
- Ideally,with wear the silicafiller should be removeda long with the resin in which it is embedded. This is possible by using smaller fillersizes. In nanofiller and microfilmed composites,the higher resin content and presence of microfillersisresponsible forthe increased surface smoothness. The inorganic filler particles are smaller than the abrasive particles used for finishing the restoration. Composites with larger fillers have a reduced surface smoothness which results in staining over some time. Age related effects also include stress cracks, apartialdebonding of the filler-resin bond. This results in a loss of opacity/and or loss of shade match over time.
Biocompatibility Of Composite Resins
The resin components are cytotoxic in vitro. Composites release some resin components for weeks after insertion. The level of release depends on the type of composite and the efficiency of the cure.
Thus composite resins have biocompatibility issues from three aspects.
- Inherent chemical toxicity of the material on the pulp.
- Pulmonary involvement due to microleakage.
- Allergic potential on contact with the oral mucosa.
- Allergic potential for personnel handling the material.
- Chronic inflammatory response in the periodontium when compared to amalgam in animal studies (monkeys).
- More cytotoxic than amalgam in vitro studies.
- Resin composite components have been shown to cause immunosuppression or immunostimulation and to inhibit DNA and RNA synthesis.
- Concerns over estrogenicity of Bisphenol A and its methacrylate.
Despite the controversies properly polymerized composites appear to be relatively biocompatible as long as there is sufficient thickness of dentin. In cases where the pulp is exposed some form of pulp capping overlayed with a glass ionomer liner is recommended.
When used in proximity to gingival tissues, proper care should be taken to ensure the correct technique of placement to prevent inflammatory responses associated with overhangs and microleakage. Issues concerning estrogenicity have not been proven to be of sufficient concern under intraoral conditions.
Pulp protection
- Glass ionomer liners are applied as pulp protection in deep cavities. Zinc oxide-eugenol is contraindicated as it interferes with polymerization. Bacterial contamination should be avoided by using rubber dam isolation.
Wear Rates And Life Expectancy Of Composites
- Composites are ideal as an anterior restorative material where wear rates are low. For posterior teeth amalgam has long been the standard direct filling material.
- Due to the increasing demand for esthetics, concern about mercury toxicity, and aggressive marketing, there is an increasing interest in the use of composites for class 1 and 2 restorations. The older generation composites showed high attrition rates. Newer formulations have shown improvements in wear resistance.
- All types of composites have been used for posterior restorations. Current guidelines require posterior composites to show less than 50 µm wear over 18 months. For posterior use, the cavity preparation should be conservative, and the manipulation technique meticulous.
Problems In The Use Of Composites For Posterior Restorations
- In Class 5 restorations, when the gingival margin is located in cementum or dentin, the material shrinks away from the margin leading to a gap.
- The placement technique is more time-consuming and demanding.
- Composites wear faster than amalgam. However, the newer materials like hybrids and nanocomposites have less wear (20 µm per year), which approaches that of amalgam (10 µm). In terms of years, the average life expectancy of the composite resin is around 8 years, which is near to that of amalgam (10 years).
The major indications of composites for posterior use are
- When esthetics is the prime consideration.
- When a patient is allergic to mercury.
Adhesion
- Composites do not adhere to tooth structure or any dental-related surface. Acid etch technique and bonding agents have to be used to ensure adhesion.
- Adhesion to instruments Composite adhere to the sculpting and packing instruments which interfere with adaptation to the cavity walls, increase porosity, and reduce operator comfort. Some clinicians use alcohol or the bonding agent as a release agent. However, both these techniques should be avoided as these materials are solvents that can weaken the resin.
Radiopacity
- Radiopacity is a useful feature for any restorative material. Posterior restorations must demonstrate adequate radiopacity to permit the detection of secondary caries, excess or inadequate quantities of material, air bubbles, and other imperfections.
- ISO norm states that the minimum radiopacity of a restorative material should be equal to or greater than that of the 2 mm-thick aluminum step wedge. Composites containing heavy metal glass fillers are radiopaque (2–3 mm/Al).
Manipulation And Placement Of Composite Resins
- Steps in the manipulation of composite resin are illustrated
- Placement of rubber dam Composite resins are highly technique sensitive and contamination from saliva, gingival fluid, or blood is best avoided with rubber dam isolation.
- Cavity preparation The cavity is prepared and margins bevelled. Cleaning The tooth is cleaned with a mild abrasive.
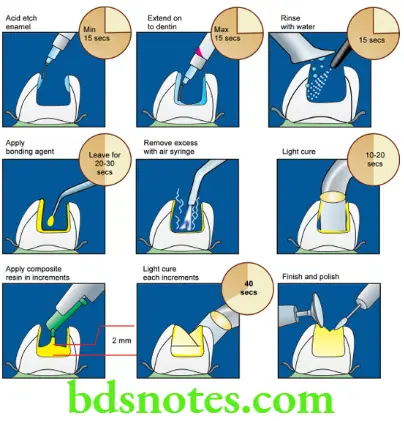

- Etching The enamel at the cavity margins is acid etched. The acid is rinsed off and the area is dried thoroughly.
- Bonding agent An enamel or dentin bond agent is applied and polymerized. (Discussed in detail subsequently). The cavity is now ready for the composite.
Techniques Of Insertion
- Resins are manipulated with plastic or plastic-coated instruments. Metal instruments should be avoided as they may abrade and discolor the composite. Composites are tacky and stick to metal instruments.
- Some operators use alcohol or bonding liquid as a release agent to reduce tackiness. However, this should be avoided as it can interfere with the properties of the resin. This is especially true of the bonding agent as it can dissolve the resin matrix and cause dilution.
- It is inserted into the cavity using a plastic instrument or a special syringe. Some manufacturers supply it in the form of a capsule which can be injected directly into the cavity with a special extruding gun.
Chemically Activated Composites
- The correct proportions of base and catalyst pastes are dispensed onto a mixing pad and combined by rapid spatulation for 30 seconds. It is inserted while still plastic for better adaptation to cavity walls.
- Air inclusions can be avoided by swiping the material into one side of the cavity and filling the cavity from the bottom outward. The cavity is slightly overfilled. A matrix strip is used to apply pressure and to avoid inhibition by air.
Light Activated Composites
The light activated composites are single component pastes and require no mixing. The working time is under the control of the operator.
Effect of ambient light Light-cured composites is vulnerable to prolonged exposure to ambient room light or the operatory light if they are left exposed and unprotected on the mixing pad. The composite begins slow polymerization as soon as it is exposed to ambient light and within 60 to 90 seconds it may lose its ability to flow. Therefore, some precautions are to be observed when using light-activated materials.
- The paste is dispensed just before use
- Avoid dispensing excessive quantities
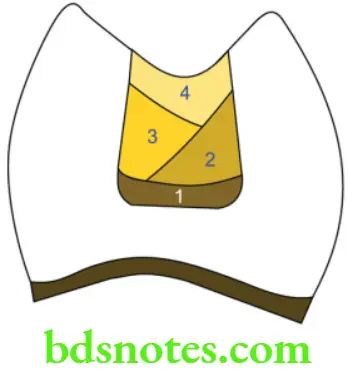
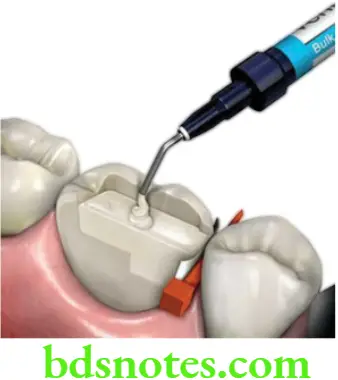
- The depth of cure is limited, so in deep cavities the restorations must be built up in increments, each increment being cured before inserting the next
- Between cures, any excess material is protected by covering it with a light-proof dark or orange-tinted cover
The material hardens rapidly, on exposure to the curing light. To ensure maximal polymerization a high intensity light unitshould be used. The light tip should be held as close as possible to the restoration.
The exposure time should be no lessthan 40 to 60 seconds. The resin should be no greater than 2.0 to 2.5 mm thick. Darker shades require longer exposure times, as do resins that are cured through enamel. Microfilled resins also require a longer exposure.
Retinal damage The high-intensity light can cause retinal damage if one looks at it directly. Avoiding looking at the light directly and using protective eyeglasses is recommended. Even greater care should be exercised when using a laser as even a short exposure can cause damage.
Control of polymerization shrinkage As mentioned earlier composites exhibit polymerization shrinkage and build-up of stresses. This can be controlled by
- Incremental curing The restoration is built-up in increments each increment being cured before inserting the next.
- Soft-start technique The curing is started with low intensity and finished with high intensity. This extends the time and fosters relaxation. Some commercially available lamps have this feature built in. Ramped curing is a variation of this technique.
- Delayed curing In delayed curing the restoration is partially cured at low intensity. The operator then completes the shaping and contouring and follows it with a second exposure for the final cure.
Finishing And Polishing
- Finishing is best done after 24 hours during which time the polymerization is complete. However, if a subsequent appointment is not desired finishing procedures can be started 15 minutes after curing.
- The initial contouring can be done with a knife or diamond stone. The final finishing is done with rubber-impregnated abrasives or a rubber cup with polishing pastes or aluminum oxide disks.
- The best finish is obtained when the composite is allowed to be set against a matrix or mylar strip.
- Special glazes and coatings are available. These are lightly filled resins. They are applied with a brush on the surface of the restoration and cured.
Bonding
One of the initial problems when resin restoratives were introduced was microleakage which resulted from the shrinkage of the resin while curing. The problem was overcome to a great extent by the introduction of the ‘acid etch technique’ by Buonocore in 1955. The acid etch technique used a combination of acid to etch the tooth and a bonding agent to improve the retention of the composite resin to the tooth.
Acid Etch Technique
The acid etch technique wasinitially developed to improve retention to enamel. Initial bond agents did not appear to bond to the dentin.
At the time it was widely believed that
- Dentin could not be etched as well as enamel
- Acid etching of dentin would cause injury to the pulp
One reason for the low bond strength to dentin was because of the hydrophobic nature of the early adhesive resins. In 1979 Fusyama demonstrated that dentin could be etched without causing any significant harm to the pulp. This together the development of hydrophilic bonding agents significantly improved the bond strength to dentin.
The acid etch technique together with the application of current bonding agents is one of the most effective ways of improving the bond and marginal seal between resin and tooth structure.
Etchant/Conditioner
The etchants are acidic. They may be grouped as
- Mineral (e.g. phosphoric, nitric acid, etc
- Organic (e.g. maleic, citric, ethylene-diamine-tetracetic (EDTA), etc.)
- Polymeric (e.g. polyacrylic acid).
The most frequently used etchant is 37% phosphoric acid. The acid in concentrations greater than 50% results in the formation of monocalcium phosphate monohydrate that reduces further dissolution.
It may be supplied as clear or colored gel or liquid. Brushes are used to apply or the acid is supplied in a syringe for direct application to the enamel. Another acid used is 10% maleic acid.

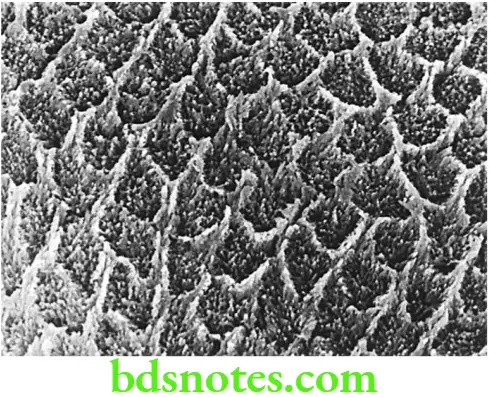
Mode Of Action On Enamel
- It creates microporosities by discrete etching of the enamel, i.e., by selective dissolution of enamel rod centers, peripheries, or both.
- Etching increases the surface area.
- Etched enamel has a high surface energy, allowing the resin to wet the tooth surface better and penetrate the microporosities. When polymerized, it forms resin ‘tags’ which form a mechanical bond to the enamel.
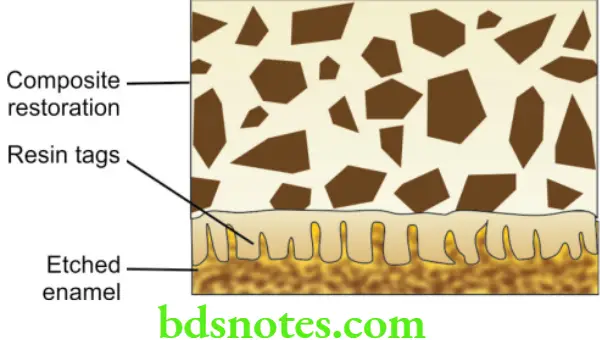
Mode Of Action On Dentin
- Removes the smear layer and partially opens the dentinal tubules.
- Provides modest etching of the intertubular dentin.
Procedure
- The tooth is cleaned and polished with pumice before etching. The phosphoric acid is then applied onto the enamel and then on to the dentin (also known as the total etch technique).
- Originally the length of application was set at 60 seconds but now it has been shown that 15 seconds is sufficient. The etching time also depends on the history of the tooth, e.g. a tooth with high fluoride content and primary teeth require longer etching time (to produce a similar etch pattern and bond strength 10% maleic acid needed at least 60 seconds of etching time).
- The acid along with dissolved minerals should be rinsed off with a stream ofwaterfor 15 seconds and the enamel dried using compressed air. After drying the enamel should have a white, frosted appearance.
- This surface must be kept clean and dry until the resin is placed. Even momentary contact with saliva or blood can prevent effective resin tag formation and severely reduce the bond strength.


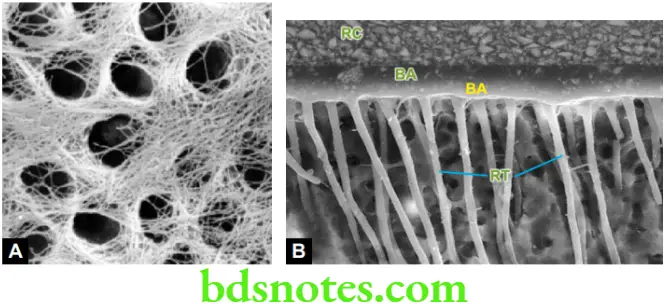
Avoiding desiccation of dentin
- Desiccation (excessive drying) of the dentin should be avoided. Desiccation can result in the collapse of the collagen mesh or network which forms a dense film that is difficult to penetrate by the bond agent.
- The collagen mesh is crucial in the formation of the hybrid layer.The monomers impregnate and become entangled with the collagen fibrils of surface demineralized dentin, creating a hybrid layer after their polymerization.
- The hybrid layer together with the resin tags forms the prime mechanism for the adhesion of the composite restoration in dentin. After drying the tooth the dentin may be lightly remoistened with cotton and then blotted dry.
Enamel Bond Agents
- These were the earliest bond agents. The more viscous composite did not bond well to the etched enamel. The enamel bond agent helped improve the bond by flowing into all the microporosities of the etched enamel and creating a mechanical retention.
Composition
- They are unfilled resins similar to that of the resin matrix of composite resin, diluted by other monomers to lower the viscosity. These materials have been replaced by agents that bond to both enamel and dentin.
Bond Strength
- Bond strengths to etched enamel range from 16 MPa (230 Psi) to 22 MPa (3200 Psi). Drying the enamel with warm air or using an ethanol rinse can increase the bond strength.
Enamel/Dentin Bond Systems
The term dentin bond agent is no longer relevant as current bond agents bond to both enamel and dentin. The usage of the term is relevant only to discuss their evolution.
Due to acid etching, microleakage or loss of retention is no longer a hazard at the resin-enamel interface. The problem lies at the resin-dentin/cementum interface. Thus agents that could bond to dentin were needed. Developing agents that will adhere to dentin was more difficult because
- It is heterogenous.
- The high water content interferes with bonding. Its tubular nature provides a variable area.
- Presence of a smear layer on the cut dentin surface (The smear layer is the layer of debris that adheres tightly to the dentin and fills the tubules after cavity cutting).
Ideally, the bond agent should be hydrophilic to displace the water and thereby wet the surface, permitting it to penetrate the porosities in dentin as well as react with the organic/ inorganic components.
Restorative resins are hydrophobic, therefore, bond agents should contain both hydrophilic and hydrophobic parts. The hydrophilic part bonds with either calcium in the hydroxyapatite crystals or with collagen. The hydrophobic part bonds with the restorative resin.
Supplied As
- Dentin bond systems are supplied in one or more bottles containing conditioners(etchant)/ primers/ and adhesive depending on the generation (see box below and also evolution of dentin bond agents – the various generations).
Evolution Of Dentin Bond Agents – The Various Generations
For ease of description, the evolution of bonding agents for composite resins is described under various generations.
- First-generation (1950 to 1970) Mineral acids were used to etch enamel. Dentin etching was not recommended as it was believed it would harm the pulp. They used glycero phosphoric acid methacrylate to provide a bifunctional molecule.
- The hydrophilic phosphate part reacted with calcium ions of the hydroxyapatite. The hydrophobic methacrylate groups bonded to the acrylic restorative resin. These were generally self-cured.
- The main disadvantage was their low bond strength (2 to 6 MPa) because of their high polymerization shrinkage and the high CTE. Leakage was a concern at the dentin-resin interphase.
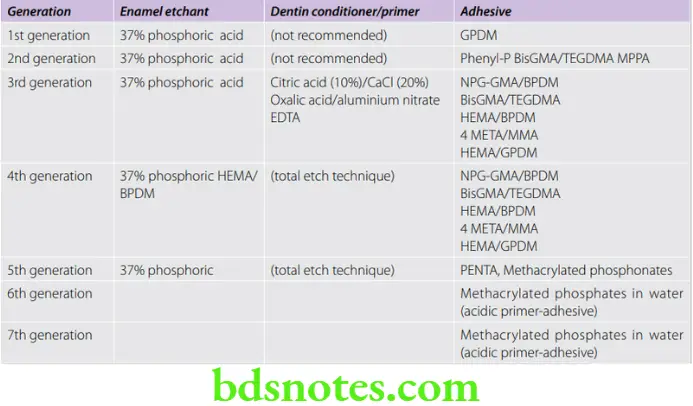
- Second generation (1970s) Developed as adhesive agents for composite resins which had by then replaced acrylic restorations. One system used NPG-GMA. It was proposed that the NPG portion bonded to the calcium of the tooth by chelation.
- Other products included phenyl-P and 2-methacryloxy phenyl phosphoric acid. Bond strengths achieved were three times more than the earlier generations.
- Disadvantage Bond strengths were still low. The adhesion was short term and the bond eventually hydrolyzed, e.g. Prisma, Universal Bond, Clearfil, and Scotch Bond.
- Third generation (1980s) The third-generation bond agents made a serious attempt to deal with the smear layer which is formed when dentin is cut. It was believed that the smear layer prevented proper bonding to the underlying dentin.
- Yet its complete removal by aggressive etching was contraindicated because it was believed that it protected the pulp by preventing direct contact with the monomer.
- The third-generation bond agents had bond strengths comparable to that of resin to etched enamel. Thus bond strengths improved to 12 to 15 MPa. However, their use is more complex and requires two to three application steps.
- Etching of enamel using 37% phosphoric acid
- Conditioning of dentin using mild acids
- Application of separate primer
- Application of polymerizable monomer
- Placement of the resin.
Examples are Tenure, Scotch Bond 2, Prisma, Universal bond, Mirage bond, etc.
- Fourth generation (the early 1990s) The fourth generation systems were possible because of some important ideological break throughs-like the total etch technique and the development of the hybrid zone.
- Research showed that acid etching of dentin did not significantly harm the pulp as long as bacterial contamination and microleakage were avoided. Thus, the total-etch technique was introduced.
- The Hybrid Layer In 1982, Nakabayashi and Fusayama reported the formation of a hybrid layer. The hybrid layer is defined as“the structure formed in dental hard tissues (enamel, dentin, cementum) by demineralization of the surface and subsurface, followed by infiltration of monomers into the collagen mesh and subsequent polymerization.
- However, dealing with the collagen mesh was not easy. It is delicate and can be destroyed by desiccation. Kanca (1991) introduced the idea of wet bonding again breaking with the traditional belief that thorough drying was necessary to improve bonding.
- Examples are All Bond 2, Scotch Bond multipurpose, Optibond, etc.
- The All Bond consists of 2 primers (NPG-GMA and Biphenyl methacrylate (BPDM) and an unfilled resin adhesive (40%BIS-GMA, 30%UDMA, 30%HEMA).
- This system bonds composite not only to dentin but to most dental-related surfaces like enamel, casting alloys, amalgam, porcelain, and composite. Bond strengths were high but as with the earlier system, multiple application steps were required.
- Fifth generation (mid-1990s) Because of the clinical complexity and multiple steps of the fourth generation dentists began asking for more simple adhesives. The fifth generation combined the primer and adhesive into one bottle (self-priming adhesive). Examples of the fifth-generation self-priming adhesives are Single Bond (3M), One Step (BISCO), Prime, and Bond (Dentsply).
The advantages claimed are
- Reduced application steps.
- Less technique-sensitive as it can bond to moist dentin.
- Less volatile liquid.
- Pleasant odor.
- Higher bond strength.
Sixth generation (mid to late 1990s) A separate etchant is not required. These are 2 bottle systems. Two varieties are seen—Type 1 and Type 2.


-
- Type 1 2 bottle 2 step system. Etchant and primer are combined in one bottle (called self-etching primer). The other bottle contains adhesive. Examples are Clearfil SE bond (Curare), Adhese, Optibondsoloplus(Kerr), Nanobond(Pentron), etc.
- Type 2 2 bottle 1 step system. LiquidA contains the primer. Liquid B contains a phosphoric acid-modified resin (self-etching adhesive). Both liquids are mixed just before application. For example, Xeno 3, Adper prompt L-pop (3 M), Tenure Unibond (Dent Mat), etc.
- Seventh generation (early 2000) Attempts to combine all three (etchant, primer, and adhesive) into a single product. Thus, seventh-generation adhesives may be characterized as -‘no mix self-etching adhesives’.
- Examples include iBond, G bond (GC), Xeno 6 (Dentsply) (glass ionomer based), and Clearfil S3 (Curare). Unfortunately, insufficient research exists on the efficacy of the newer systems. Composition and procedure for one such product is presented.
Indications For Use Of Bond Agents
- For bonding composite to the tooth structure.
- Bonding composite to porcelain and various metals like amalgam, base metal, and noble metal alloys.
- Desensitization of exposed dentin or root surfaces.
- Bonding of porcelain veneers.
- Contraindication Bonding should not be done immediately after bleaching a tooth. It is advisable to wait at least a week following the procedure.

Bonding Mechanisms
- Though chemical bonding schemes have been proposed, there is little evidence supporting them. The bonding is more probably micromechanical, due to the penetration of the polymerizable monomer into the finely textured primed dentin.
- A fine collagen mesh exists on the surface of the dentin which current bond agents can infiltrate because of their hydrophilic components.
- One more precaution is that the dentin should not be dried excessively as desiccation can cause the collapse of the fine collagen meshwork thereby reducing the bond strength.
Bond Strength Of Dentin Bond Agents
- Current dentin bond agents generate bond strengths comparable to that of resin to etched enamel. Bond strength is difficult to measure because of the wide variations in the dentin itself, test methods, and other factors. Bond strength reduces with increased depth of dentin. Various studies have shown values ranging from 15 to 35 MPa.
- An increasing number of studies are using the microtensile test methodology. The size of the specimen is smaller (1 mm2 in cross-section). Thus, several specimens can be prepared from the same tooth thereby increasing the uniformity of the study.
Dye Penetration Tests
- These are important tests related to the performance of the bonding system. A test for microleakage is indicative of the success or failure of a bond. These tests are done using tracers and staining to determine the depth of penetration.
Repair Of Composites
Composite resins may be repaired by adding new material over the old. This is useful in correcting defects or altering contours of an existing restoration. The procedure differs depending on whether the restoration is fresh or old.
- Freshly polymerized restoration still has an inhibited layer of resin on the surface. More than 50%of unreacted methacrylate groups are available to copolymerize with the newly added material.
- In older composites, the presence of fewer methacrylate groups and greater cross-linking reduces the ability of fresh monomers to penetrate the matrix.
Method
- Remove contaminated material from the surface and roughen it. Place fresh composite after applying bonding agent.
Sandwich Technique
- Composite does not bond adequately to dentin, therefore during polymerization, a gap may result if the cavity margin is situated in dentin. The bond to dentin can be improved by placing a glass ionomer liner between the composite restoration and dentin.
- The glass ionomer bonds to the dentin through chemical adhesion where as the resin bonds mechanically to porosities and crazing present on the surface of the glass ionomer liner. The glass ionomer can also be etched with the help of phosphoric acid to improve retention.
- In addition, it also provides an anti-cariogenic effect due to its fluoride release. When used in this context it is often referred to as ‘sandwich technique’.
Indications
- Lesions where one or more margins are in dentin, e.g. cervical lesions.
- Class 2 composite restorations.
Procedure
- Dentin is conditioned and a thin layer of GIC cement is placed. The cement must be exposed at the margins to achieve fluoride release. Phosphoric acid is used to etch the enamel portion. Some operators also etch the GIC surface with the same phosphoric acid for 15 to 20 seconds to increase surface roughness (light cured GIC is not etched).
- The surface is then washed for 25 to 30 seconds. After adequate drying, a bond agent is applied to the cement surface and the etched enamel. The composite resin is then inserted in the usual manner.
Specialized Composite Resins
Flowable Composites
As suggested by the name these are hybrid composites modified to have an increased flow. The increased flow is achieved by a reduction in the filler content (30–55 vol % or 40–60 wt.%). When placed in the cavity the material flows readily and intimately adapts to the cavity wall. The reduced filler content affects some of the properties.
Thus these materials
- Are more prone to wear
- Have half the stiffness(more flexible) of regular hybrids (4–8 GPa)
- Greater polymerization shrinkage (3–5 vol%)
These materials are intended for specialized usage
- As a preventive material (fissure sealant and small class I cavity).
- Cervical lesions and Class V restorations.
- As a base or liner.
- Areas of reduced access.
Packable Composites
These are composites that have very high viscosity and low surface tackiness. They have a high filler loading (66–70% vol) with porous or irregularly shaped particles. They are not condensable like classic amalgam, rather they can be compressed and forced to flow using flat-faced instruments, hence the term packable.
They are considered as posterior composites. The distinguishing characteristics of all packable compositions are less stickiness or stiffer viscosity than conventional composites, which allow them to be placed in a manner that somewhat resembles amalgam placement.
They have a higher wear resistance. Claims also include a greater depth of cure and low polymerization shrinkage. In general, the mechanical properties of packable composites are not substantially better than those of most conventional universal composites.
Commercial examples Solitaire (Heraeus), ALERT (Jeneric), and SureFil (Dentsply).
Indications
They are indicated for use in Classes 1 and 2 cavities. In class 2 cavitieswhere improved contacts with adjacent teeth are desired.
Prosthodontic Veneer Composites (Laboratory Composites)
- The resin may be used as a veneer (a tooth-colored layer used to hide the underlying metal) for crowns and fixed partial dentures. They are also known as composites for dental indirect restorations.
- The earliest recorded use was in the Hollywood film industry where they were used to temporarily mask the teeth of actors. The early materials were heat cured poly (methyl methacrylate) improved by fillers and cross-linking agents.
- Current veneer materials are hybrid, micro, or nanofiller-reinforced resins such as bis-GMA, urethane methacrylate, or 4,8-di(methacrylic methylene) tricyclo-(5.2.1.02,6) -decane. Some are fiber reinforced.
- The newer resins have superior physical properties and are polymerized by light or heat and pressure.
- The resins are mechanically bonded to the metal using wire loops or retention beads. Recent improvements, include micromechanical retention created by acid etching the base alloy and the use of chemical bonding systems such as 4-META, phosphorylated methacrylate, epoxy resin, or silicon dioxide that is flame sprayed to the metal surface followed by the application of a silane coupling agent (silicoating).
- Commercial examples are SR Adoro (Ivoclar), GC Gradia (GC), Targis Vectris, etc.
- Available as A kit containing various materials which include—incisal, dentin, and other specialized resins, masking resins.

Indications
- Inlays, on lays, veneers and anterior crowns (metal free).
- As veneer over metal-supported crowns and FDPs.
- Long term temporaries (alone or in combination with Kavo C-temp blanks).
The advantages of resin when compared to porcelain
- Ease of fabrication.
- Easily repairable intraorally.
- Less wear of opposing teeth or restorations.
Disadvantages
- Microleakage of oral fluids and staining under the veneers due to thermal cycling and water sorption.
- Surface staining and intrinsic discoloration.
- Susceptibility to toothbrush wear.
- Cannot be used in crowns serving as abutments for removable partial dentures. The clasp arm will abrade the resin.
- Not as durable as other prosthodontic materials like ceramics and PFM.
Resin Inlay Systems
- These were introduced in an attempt to overcome some of the limitations of traditional posterior composite resin restoration.
- The resin inlay is completely polymerized outside the mouth by light, heat, pressure, or combination and then luted to the tooth using a resin cement. They may be fabricated using the direct method or indirect method.
Direct inlay system (fabricated in the mouth)
- Hybrid or microfilled resins are used. A separating medium (agar solution or glycerine) is applied to the prepared tooth. The restoration is then formed, light-cured, and removed from the tooth.
- The rough inlay is subjected to additional polymerization by light (6 minutes) or heat(100 °C for 7 minutes). After this the prepared tooth is etched and the inlay is luted to place with a dual-cure resin cement and then polished.
Indirect inlay system (fabricated on a die)
- The inlay is fabricated with prosthodontic resin (described earlier) in the laboratory on a die made from an impression of the prepared tooth. Conventional light and heat or heat and pressure may also be used for polymerization.
Advantages of inlays
- Improved physical properties and wear resistance due to the higher degree of polymerization attained.
- Induced stresses and potential for microleakage are reduced as polymerization shrinkage occurs outside the mouth.
- Being resins they do not abrade opposing teeth and are repairable in the mouth.
Preformed Composite Resin Laminates
- Composite resins are used as preformed laminate veneers to mask tooth discoloration or malformation. These shells are adjusted by grinding and are bonded to teeth using the acid-etch technique and resin cement.
Core Build-Up Composite Resins
- Modified highly filled resins are used as core materials in combination with prefabricated posts during the restorations of broken-down teeth. They are highly colored opaque materials. They are usually chemically cured or dual-cured with a longer working time and shorter setting time.
- Some concerns exist regarding the strength of composite cores when compared to cast posts and cores. Failures are often seen when these materials form the bulk of the support for crowns and FDPs.
- The lower stiffness (greater flexibility) can result in slightly more frequent debonding of crowns and other restoration.
- Therefore, when using composite cores shared support from the remaining tooth structure is indicated. MultiCore (Ivoclar Vivadent) is an example of a core build-up composite. The product also contains fluoride.

Resin Cement
- Lower viscosity-filled resins(e.g. Panavia Ex, Infinity) are used for the cementation of laminates, crowns, and orthodontic brackets. Etching and bonding is done before cementing (described in detail in the chapter on cements).
Provisional Composites
- A temporary restoration is necessary to protect the teeth after preparation and in the interim period while the definitive restoration is being constructed. Composite resins are available for making provisional inlays, onlays, crowns and FDPs. E.g. Protemp (ESPE), Structur(VOCO), Integrity (Dentsply), etc.

Advantages
- Can be made directly in the mouth because of its low exothermic heat of 18 to 28 °C.
- It is easily ground and shaped using regular high-speed diamond burs without melting and clogging the burs (unlike the conventional acrylic provisional resins).
- Improved mechanical properties including low wear rates when compared to acrylic provisionals.
- Good radiopacity.
Available as
- Syringe form It comes as base and catalyst. Currently, two shades are available. It is supplied in a syringe form and is dispensed by rotating the plunger until a clicking sound is heard, this represents one unit.
- The catalyst is a two-component system and only a small amount is required. As the plunger is rotated the two components are dispensed simultaneously. The base and catalyst aremixedwitha spatula andused. Setting occurs approximately two to three minutes.
- Cartridge form The material is also available in the cartridge form for use with a static mixing device. It consists of a caulking gun that forces the materials through special static mixing tips. The material comes out mixed and ready to use when expressed through these tips. After curing in the mouth the hardening can be accelerated by placing in hot water.
Precautions
- As with all materials expressed from cartridges, the material that comes initially should be discarded as it may not be in the correct proportions.
- Oxygen-inhibited layer This reaction is strongly inhibited by oxygen diffusing from the atmosphere into the curing resins is responsible for the formation of a soft, sticky, superficial layer on the surface of the prepared tooth. This layer can affect or inhibit the setting of polyvinyl siloxane impression materials In some techniques where a putty impression is used as a template, this layer can prevent the bonding
Composite Resin Blanks For CAD – CAM Systems
- Composite resin blanks are available for the fabrication of long term (up to 1 year) provisional restorations including crowns and fixed partial dentures. They are fabricated by a CAD/CAM process (see the chapter on ceramics for further details of the process).
- One such product is the Everest C-Temp (Kavo). The whole restoration may be fabricated as one piece or it may be fabricated as a framework which is subsequently veneered with conventional prosthodontic resins. These resins are characterized by high flexural strength.

Porcelain Repair Composite Resins
- Composite resins are occasionally used to repair fractured or chipped ceramic restorations. The kit consists of a silane-based bonding agent, and a metal masking agent(opaquer). Conventional composite is then used to carry out the final repair. The material and procedure are discussed in further detail.
Pit And Fissure Sealants
- Deep pits and fissures on posterior teeth are susceptible to decay as they provide shelter for organisms. They are often too narrow making it difficult to clean.
- Various materials have been used to seal these areas, especially in the child patient. The objective is for the resin to penetrate into the pits and fissures, thereby,sealing these areas against oral flora and debris.
Indications
Sealants are most effective in children with high risk of caries. Both deciduous molars and young permanent molars with deep pits and fissures are common candidates. Commonly surfaces that are free of caries should be selected. However, a recent study where the sealant was placed intentionally in pits and fissures having caries showed that the lesion did not progress.
Types
- Based on filler content 2 types are available—Filled and Unfilled.
- Based on curing mechanism—they may be light cured or chemical cured.
- Color—The sealants are available as transparent, tooth-colored, opaque, tinted, or white materials. The color contrast helps to determine the efficacy of the application. Recent products include photosensitive color reversible sealants. These sealants are normally colorless but change to pink or green when exposed to a curing light. The color change which lasts about 5–10 minutes is useful for diagnosis during periodic recalls.
Composition
- The most commonly and successfully used sealant is bis-GMA. It may be cured chemically (amine-peroxide system) or by light. The bis-GMA resin is mixed with a diluent to obtain a low-viscosity sealant that flows readily.
- In filled sealant, small amounts of filler (up to 40%) are added to improve its stiffness and wear resistance. Other resins systems include polyurethanes and cyanoacrylates.
Properties
- Important properties of sealants are flow, wear resistance, fluoride release and long term retention.
- Sealants must have low viscosity so that they will flow readily into the depths of the pits and fissures and wet the tooth. Wettability is also important for proper adaptation and penetration. Acid etching improves the wettability.
- Proper retention of the sealant is important for caries prevention. Acid etching with bonding agents is necessary for the retention of the sealant.
- The sealant must have sufficient mechanical properties like strength, stiffness and wear resistance for effective function and durability. Sealants with fillers usually have better mechanical properties than unfilled resins.

- Current products have been formulated for fluoride release during service. Initial fluoride release is high, especially during the first 24 hours but gradually tapers to low levels which may not be effective for long-term protection.
- Air inhibition during polymerization is also a problem in sealants. The tacky air-inhibited layer is removed using a pumice paste on a cotton pellet rotary cup or brush. The operator must ensure that sufficient thickness of sealant is applied to compensate for this loss.
- The unpolymerized surface layer was once a health concern because of the presence of BPA (bisphenol A) which is chemical similar to estrogen. However, this has since been discredited and is no longer a major concern.
Efficacy of sealant therapy
- Early clinical studies showed a retention rate of 42% and a caries reduction rate of 35% over 5 years. Improvementsin materials and technique overthe years have dramatically improved the success rates.
- Current studies indicate a success rate of over 90% in caries reduction.
Periodic recall
- Evidence has shown that sealant therapy cannot be taken for granted. The sealant should be re-examined every six months. If the sealant is missing it should be reapplied. Improper case selection and application of sealant may actually enhance caries.
Composite Resin Denture Teeth
- Over the years various types of materials have been used for denture teeth. Traditionally conventional acrylic (Biotone), cross-linked acrylics(SR-Postaris, Genios-P, etc.), and porcelain denture teeth are used.
- Since their introduction composite resins too have been tried as denture teeth. Some examples are nano-filled (Veracia) and micro-filled composites(SR-Orthosit, Endura, Duradent, Surpass). In one study.
- The composites and cross-linked acrylic resins did not show significant differences in wear resistance properties. However, both were significantly better than conventional resin acrylic teeth.
Advantages And Disadvantages Of Restorative Composite Resins
Advantages
- Highly esthetic tooth colored restorations possible.
- Multiple curing systems allow choice of working time.
- Relatively ease of placement.
- Moderately strong and durable.
- Does not corrode when compared to amalgam.
- Easy to repair.
Disadvantages
- Highly technique-sensitive.
- High shrinkage.
- Does not bond to tooth structure; requires dentin bonding techniques.
- Sticks to instruments.
- Not condensable like amalgam.
- Possibility of microleakage and recurrent caries if improperly placed.
- Some materials exhibit slumping.
- Not as wear resistant as other metallic restorative materials.
- Shorter life span when compared to other more durable restorative materials like ceramics, DFGs, amalgam, and cast metal restorations.
- Higher allergic, inflammatory response, cytotoxic, and other biologically adverse effects when compared to amalgam.
- Potential for color instability and staining over time.

Leave a Reply