Question. Write short note on urine examination of Renal Failure.
Answer.
Reduction in glomerular filtration rate and rise in nitrogenous and nonnitrogenous substance in blood as a result of degenerated renal function is known as renal failure.
For Acute rRenal Failure
- Volume of urine is less (Oliguria) or absent, i.e. anuria.
- Albumin content in urine depends on the underlying
Causes Renal Failure
- Urine osmolality is more than 600 mOsm/L; urinary sodium excretion is less than 20 mmol/L; urine/plasma urea ratio is more than 10:1
- Dipstick for blood, protein or both is suggestive of renal inflmmatory process.
- Urine microscopy: Presence of red cell cast is suggestive of glomerulonephritis.
For Chronic Renal Failure
- Volume of urine passed daily is in the form of polyuria.
- Appearance and color is normal.
- There is no odor present
- Specifi gravity of urine is low and fied.
- Albuminuria is present
- Microscopically, there are hyaline and broad cell cast in urine
- Serum creatinine increases
Question. How will you diagnose and investigate a case of nephrotic syndrome?
Answer. Diagnosis is based on clinical signs and investigations:
Clinical Signs Nephrotic Syndrome
- Physical examination reveals generalized edematous person.
- Edema may persist for many weeks or months.
- Tachycardia is present while blood pressure is normal.
- Pittng edema is present over legs and feet, abdominal walls and lower eyelids.
- Eyelids become puff
- At places where edema is severe ascites and pleural effsion are seen.
- Kidneys are not palpable.
Investigations Nephrotic Syndrome
1. Urine examiation:
- Oliguria while edema is forming, dieresis or normal amount of urine during period of subsidence of edema.
- Proteinuria: It is massive, usually more than 5 g/day though variable from time to time; urine becomes almost solid on boiling. Daily loss of protein may be 20–50 g.
- 24 hour urine shows excretion of albumin or protein more than 3.5 g/day.
- Red blood cells are absent or few are seen
- Casts: Fatt casts, tubular cells, oval fat bodies, doubly refractile bodies are seen
Nephrotic Syndrome Blood examination: Nephrotic Syndrome
- Anemia: It is slight normochromic.
- Hypoalbuminemia: Serum albumin usually less than 3 g/100 mL. Total serum globulin concentration frequently lowered with often elevation of α2 and β-globulins.
- Serum lipids show increase in LDL levels and cholesterol.
- ESR is raised due to hyperfirinogenemia.
Serum complement level: Serum complement C3 and C4 levels get reduced. - Other biochemical tests, i.e. blood urea, serum creatinine, creatinine clearance and electrolytes are normal.
2. Ultrasound of abdomen: It can show normal small or large kidneys which depends on the underlying cause.
Amyloid and diabetic kidneys are large while kidney in glomerulonephritis is small.
3. Renal biopsy: It is normal on light microscopy but electron microscopy shows typical abnormalities (effcement of epithelial cell foot processes).
Question. Outline the management of Urinary Tract Infection.
Answer.
Infection of kidneys, ureter or bladder by microorganism that either ascends from the urethra or spread to kidney from bloodstream.
Management Urinary Tract Infection
- Rest should be given to the patient.
- Mildtomoderate cases should be treated by giving antibiotics, i.e. nitrofurantoin, ciproflxacin, gentamicin,cotrimoxazole, norflxacin.
- In severe cases, parenteral antibiotics, i.e. inj. carbenicillin is given.
- Fluid intake should be high, alkalization of urine with potassium citrate solution to alleviate symptoms
- To reduce pain, antispasmodic drug is given.
Question. Outline the management of Acute Gout.
Answer.
Gout is an abnormality of metabolism which results in the deposition of monosodium urate crystals in joints and other tissues.
Management Acute Gout
Management of Acute Attack
- NSAIDs: Any of the NSAID should be given except aspirin as it causes uric acid retention. Selective COX2 inhibitors e.g.
Etoricoxib 120 mg OD or Valdecoxib 20–40 mg BD can be given. Colchicine 0.5 mg postoperatively every 2 hours, up to 4–6 mg/day is now reserved for patients without renal, hepatic or marrow disease, in whom the more effctive NSAIDs contraindicated or poorly tolerated. - Corticosteroids: Methyl prednisolone acetate 5–25 mg per joint as Intraarticular injection is given. Systemic oral prednisolone 20 mg/ day tapered of over 4–10 days or IM triamcinolone 60 mg/ day repeated in 1–4 days, are highly effective relatively safe alternatives.
- Restrict allopurinol or uricosuric drugs till the acute attck has setted for 2–3 weeks as they can prolong the acute attack or trigger their episodes. Patients should be advised to avoid diuretics and/ or salicylates.
Long-Term Management Acute Gout
- Diet: It should given low in purine and fats.
- Weight reduction in obese patient, avoid alcohol.
- Anti-hyperuricemic therapy:
- Hypouricemic drug: Allopurinol 300 mg daily with a
NSAID or colchicines 0.5 mg BD. - Febuxostat 40 mg OD to reduce and maintain serum uric acid levels below 6 mg/dL. Ifserum uric acid levels are more than 6 mg/dL after 2 to 4 weeks treatment with the drug 80 mg/day, dose is increased to 120mg/day.
- Probenecid 0.5 to 1gm BD or Sulfipyrazone 100mg
TDS as an alternative to allopurinol with colchicines if renal function is not impaired. - Benzbromarone 100 mg daily in patients with moderate renal impairment where other uricosuric agents are ineffctive.
- If patient do not tolerate or fail the full dose of other treatments IV pegloticase is given 8 mg for every 2 weeks. It dramatically reduces the serum uric acid.
Question. Write the investigation and management of proteinuria.
Answer. Proteinuria is defied as presence of protein usually albumin in the urine, this fiding may be transient and entirely benign or a sign of severe renal disease.
Investigations of Proteinuria
- Heat coagulation method: This is done by heating upper portion of urine in a test tube. White coagulum present at top of the urine is suggestive of proteinuria.
- Dipstick test: This is a bedside test, which patient can perform by himself if his/her color vision is normal. Color change in strip is compared to the color on botte which quantify loss of proteins.
- Electrophoresis ofproteins: It detects the globulins in urine.
- Immunoelectrophoresis: It is carried out to identify fragments of immunoglobulins when there is a monoclonal peak on routine urine paper electrophoresis.
- 24 hours urine for proteinuria: It is done to separate the cases of nephrotic syndrome, i.e. massive proteinuria more than 3.5 g/day from other etiology of proteinuria in which there is mild proteinuria, i.e. 1 to 2 g/day.
- Radioimmunoassay: This test is done for detection of microalbuminuria.
Management of Proteinuria
Proteinuria is not a specifi disease. So its treatment depends on identifying and managing its underlying cause.
- Angiotensinconverting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) reduce intraglomerular pressure by inhibiting angiotensin II mediated effrent arteriolar vasoconstriction. These groups of drugs have a proteinuria-reducing effct independent
of their antihypertensive effct. - When treatment with an ACE inhibitor or ARB does not adequately control proteinuria in a patient with chronic kidney disease (e.g. diabetic nephropathy), a further reduction in proteinuria can be achieved by adding a mineralocorticoid receptor antagonist (MRA) such as
eplerenone or spironolactone. - Immunosuppressants such as cyclophosphamide and azathioprine should be reserved for patients with progressive renal insuffiency or with vasculitic lesions on renal biopsy.
- Patients with moderatetosevere proteinuria are usually flid overloaded and require diuretic therapy along with dietary salt restriction.
- There are recommendations for no restrictions or only mild restriction in protein intake, i.e.0.8–1 g/kg daily.
Question. Write short note on renal failure.
Answer. The deterioration of renal function resulting in decline in GFR and rise in urea and nonnitrogenous substances in blood is called renal failure.
Types:
1. Acute renal failure.
2. Chronic renal failure.
Acute Renal Failure
- There is acute fall in GFR over days or weeks.
- Invariable reversible
- Causes of acute renal failure may be pre renal, renal or postrenal.
- Oligouria and anuria are characteristics.
- Symptoms and signs of uremia are of recent onset.
- Parameters of acute reduction of GFR, i.e. edema,hypertension, salt and water retention are presenting features.
- Broad casts or renal failure casts are absent.
- Specifi gravity of urine is high
- Dialysis is rewarding required for short period.
Chronic Renal Failure
- GFR falls gradually over a period of months or years.
- Invariably irreversible
- Causes are mostly renal but may be extrarenal.
- Polyuria and nocturia are commonly seen.
- Symptoms and signs of uremia are of more than three months of duration.
- Proof of chronicity is present, such as long duration of symptoms and signs of uremia, small sized kidney, anemia, hypertension, renal osteodystrophy.
- Broad casts or renal failure casts present.
- Specifi gravity of urine is low and fied.
- Repeated chronic maintenance and dialysis is required.
- Renal transplantation is fial answer.
Question. Write briefl clinical features and management of nephrotic syndrome.
Answer.
Clinical Features Nephrotic Syndrome
- Age and sex: Nephrotic syndrome is two to three times more common in childhood with peak incidence at 2–3 years.
In this age group, there is a male : female ratio of 2.5 : 1,in adults, sex incidence is equal. - Edema: It is peripheral involving the limbs, particularly lower limbs.
In children, edema may be more obvious in the face and abdomen.
Usually, massive generalized anasarca, the patient almost weighing double his true weight.
Intense edema of the scrotum or vulva may occur.
There may be bilateral hydrothorax.
Edema may persist for many weeks or months.
Spontaneous subsidence with diuresis (nephrotic crisis) may occur, to be followed again by increase of edema. - Gastrointestinal symptoms: Anorexia causes severe malnutrition, Diarrhea and vomiting due to edema of intestinal wall.
- General symptoms: Prolonged protein loss causes anorexia,lethargy, tiredness, frequent infections and muscle wasting.
Dyspnea may occur, if there is flid in the pleural cavity. - Blood pressure: There may be periods of hypertension;ultimately with development of chronic nephritis permanent hypertension may develop.
Management of nephrotic syndrome involves:
- Scientifi treatment of underlying morphology or causative disease
- General measures to control nephritic complications
- Treatment to reduce proteinuria
Non-specifi measures that may reduce proteinuria include ACE and NSAIDs.
ACEI and ARBs (angiotensinreceptor blockers) reduce proteinuria and slows the rate of progression of rate of renal failure by lowering intraglomerular pressure and preventing development of hemodynamically mediated focal segmental *glomerulosclerosis. - Edema: Advice patient to take low sodium diet i.e.1 to 2 g/day. In mild edema thiazide induce gentle diuresis.
In moderate edema frusemide in doses of 80 to 120 mg/day or torsemide 20 to 40mg/day is given.
In patients with severe edema frusemide 20 to 40mg/day is combined with spironolactone 100 to 200mg/day for complete resorption of sodium throughout the nephron. - Hypercholesterolemia: It is treated by the lipid lowering agent specially statins. Atorvastatin 20 mg OD or BD
Anticoagulation is needed for patient with deep vein thrombosis, arterial thrombosis and pulmonary embolism. - Antiplatelet agents and warfarin could be advocated.
- Diet: Restricted protein diet is advised since high protein diet accelerates progression of nephritic syndrome.
- Vitamin D supplementation is advisable.
- Antibiotics: Aggressive antibiotic therapy is given in nephrotic syndrome as chances of sepsis are always present. Mainly cephalexin are given
- Corticosteroids: Produce rapid and complete remission with clearing of proteinuria in 90% cases.
Dose -Prednisolone 1 mg/kg/day, maximum 80 mg/ day. Remission usually occurs between days 7 and 14, though some patients need up to 16 weeks therapy to achieve complete remission.
Prednisolone dose is reduced to 0.5 mg/kg/day and then tapered slowly.
An attmpt to stop treatment should be made after 8 weeks.
In patients who relapse, course of prednisolone should be repeated. - Immunosuppressive drugs: In steroidresistant patients, or in those in whom remission can only be maintained by heavy doses of steroids, cyclophosphamide 1.5–2 mg/kg/ day for 8–12 weeks with concomitant prednisolone 7.5–15 mg/day.
- Levamisole: In corticosteroiddependent children 2.5 mg/ kg to maximum 150 mg on alternate days is useful in maintenance of remission.
Question. Write short note on UTI.
Answer. UTI- Urinary Tract Infection
The urinary tract infection is divided into two general anatomic categories:
1. Lower tract infection (Urethritis and cystitis).
2. Upper tract infections (Acute pyelonephritis,prostatitis, intra renal and perinephric abscess).
Etiology
Gramnegative organisms are mainly responsible, i.e. E.coli,
Proteus, Klebsiella, Enterobacter, etc.
- UTI is more common in females as compared to males.
- Pain is the most common sign. It can be mild, constant or intense and colicky.
- There is also abrupt onset of frequency of micturition and dysuria.
- Patient suffrs from fever with rigors and chills, malaise,loss of apetite and vomiting.
- There is presence of scalding pain in urethra duringmicturition.
- After urinary bladder get empty, there is desire to pass more urine.
- Hematuria can occur.
- In chronic infection, there are periods of acute exacerbation in addition to malaise, lowgrade fever and ill health.
- In acute cases, tachycardia and tenderness develops on deep palpation on renal region.
Investigations
- Urine examination: A mid stream specimen is taken for examination. A heavily infected urine may look hazy to naked eye. It may have a fihy smell in E. coli infection and ammonical in Proteus infection. Reaction of urine usually is acidic. Albumin is present in traces. Microscopic examination will show clumps of pus cells. Urine should be cultured for type of organisms. Colony count done and sensitivity of the organism to various drugs.
- Plain X-ray abdomen is done for renal/bladder/ureteric calculi
- Intravenous pyelography for any congenital anomalies,calculi.
- Ultrasonography for renal size, calculi and any other abnormality.
Management
- Rest should be given to the patient.
- Mildtomoderate cases should be treated by giving antibiotics, i.e. nitrofurantoin, ciproflxacin, gentamicin,cotrimoxazole, norflxacin.
- In severe cases, parenteral antibiotics, i.e. inj. carbenicillinis given.
- Fluid intake should be high. Alkalization of urine with potassium citrate solution to alleviate symptoms.
- To reduce pain, antispasmodic drug is given.
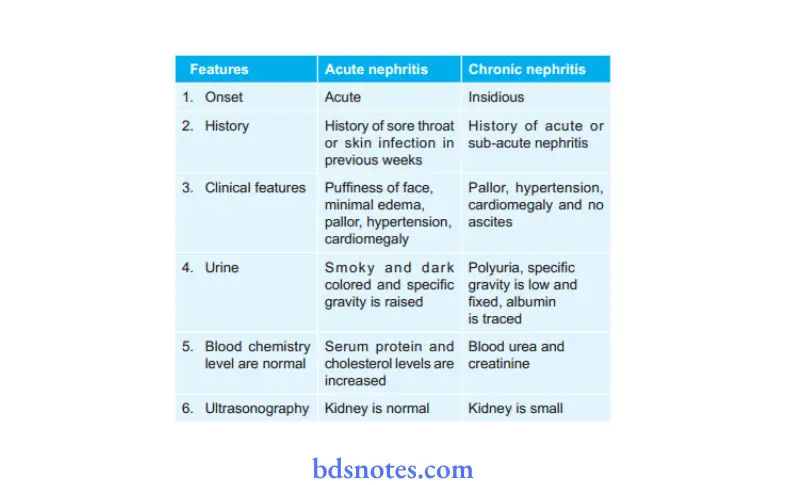
Question. Diffrentiate acute and chronic nephritis.
Answer.
Question. Define nephrotic syndrome its etiology, clinical features, pathological blood and urine fidings and management.
Or
Describe the etiology, clinical features and management of nephrotic syndrome.
Answer. This syndrome refers to massive proteinuria more than 3.5 g/day mainly of albumin, reduced albumin concentration, edema, hyperlipidemia, lipiduria and hypercoagulability.
It is a clinical complex with number of renal and extrarenal features
- Hypoproteinemia
- Hypoalbuminemia
- Generalized edema or anasarca
- Hypercholesterolemia
- Hypercoagulability.
2. Primary glomerular diseases
- Minimal change nephropathy.
- Mesangioproliferative glomerulonephritis.
- Membranous nephropathy.
- Focal and segmental glomerulosclerosis.
- Crescentic glomerulonephritis
- Idiopathic:
3. Secondary to other diseases:
- Infections: Malaria, hepatitis B, herpes zoster,
streptococcal and staphylococcal infections, syphilis,
leprosy, schistosomiasis. - Drugs: NSAIDs, Heavy metals such as gold, anti convulsants, penicillamine, ACE inhibitors, heroin,rifampicin, tolbutamide and probenecid.
- Malignancy: Hodgkin’s disease and other lymphomas.
Systemic diseases: Diabetes mellitus, amyloidosis, systemic lupus erythematosus, HenochSchonlein purpura, cryoglobulinemia, polyarteritis nodosa. - Familial disorders: Congenital (neonatal) nephrotic syndrome, Alport’s syndrome, Fabry’s disease
- Miscellaneous conditions: Reflx nephropathy, renal vein thrombosis, toxemia of pregnancy, allergic reactions to insect bites, pollens and vaccines, renal artery stenosis.
Clinical Features
- Age and sex: Nephrotic syndrome is two to three times more common in childhood with peak incidence at 2–3 years.
In this age group, there is a male : female ratio of 2.5 : 1,in adults, sex incidence is equal. - Edema: It is peripheral involving the limbs, particularly lower limbs. In children, edema may be more obvious in the face and abdomen. Usually, massive generalized anasarca, the patient almost weighing double his true weight. Intense edema of the scrotum or vulva may occur.
There may be bilateral hydrothorax. Edema may persist for many weeks or months. Spontaneous subsidence with diuresis (nephrotic crisis) may occur, to be followed again by increase of edema. - Gastrointestinal symptoms: Anorexia causes severe malnutrition, Diarrhea and vomiting due to edema of intestinal wall.
- General symptoms: Prolonged protein loss causes anorexia,lethargy, tiredness, frequent infections and muscle wasting.
Dyspnea may occur, if there is flid in the pleural cavity. - Blood pressure: There may be periods of hypertension;ultimately with development of chronic nephritis permanent hypertension may develop.
- Urine examiation:
- Oliguria while edema is forming, dieresis or normal amount of urine during period of subsidence of edema.
- Proteinuria: It is massive, usually more than 5 g/day though variable from time to time; urine becomes almost solid on boiling. Daily loss of protein may be 20–50 g.
- 24-hour urine shows excretion of albumin or protein more than 3.5 g/day.
- Red blood cells are absent or few are seen
- Casts: Fatt casts, tubular cells, oval fat bodies, doubly refractile bodies are seen
2. Blood examination:
- Anemia: It is slight normochromic.
- Hypoalbuminemia: Serum albumin usually less than 3 g/100 mL. Total serum globulin concentration frequently lowered with often elevation of α2 and β-globulins.
- Serum lipids show increase in LDL levels and cholesterol.
- ESR is raised due to hyperfirinogenemia.
- Serum complement level: Serum complement C3 and C4 levels get reduced.
- Other biochemical tests, i.e. blood urea, serum creatinine, creatinine clearance and electrolytes are normal.
- Ultrasound of abdomen: It can show normal small or large kidneys which depends on the underlying cause.
Amyloid and diabetic kidneys are large while kidney in glomerulonephritis is small. - Renal biopsy: is normal on light microscopy but electron microscopy shows typical abnormalities (effcement of epithelial cell foot processes).
- Management of nephrotic syndrome involves:
- Scientifi treatment of underlying morphology or causative disease
- General measures to control nephritic complications
Treatment to reduce proteinuria
- Non-specific measures that may reduce proteinuria include ACE and NSAIDs.
- ACEI and ARBs (angiotensinreceptor blockers) reduce proteinuria and slows the rate of progression of rate of renal failure by lowering intraglomerular pressure and preventing development of hemodynamically mediated focal segmental *glomerulosclerosis.
- Edema: Advice patient to take low sodium diet i.e.1 to 2 g/day. In mild edema thiazide induce gentle diuresis. In moderate edema frusemide in doses of 80 to 120 mg/day or torsemide 20 to 40mg/day is given. In patients with severe edema frusemide 20 to 40mg/day is combined with spironolactone 100 to 200mg/day for complete resorption of sodium throughout the nephron.
- Hypercholesterolemia: It is treated by the lipid lowering agent specially statins. Atorvastatin 20 mg OD or BD
Anticoagulation is needed for patient with deep vein thrombosis, arterial thrombosis and pulmonary embolism.
Antiplatelet agents and warfarin could be advocated. - Diet: Restricted protein diet is advised since high protein diet accelerates progression of nephritic syndrome.
Vitamin D supplementation is advisable. - Antibiotics: Aggressive antibiotic therapy is given in nephrotic syndrome as chances of sepsis are always present. Mainly cephalexin are given
- Corticosteroids: Produce rapid and complete remission with clearing of proteinuria in 90% cases.
- Dose -Prednisolone 1 mg/kg/day, maximum 80 mg/ day.
- Remission usually occurs between days 7 and 14, though some patients need up to 16 weeks
therapy to achieve complete remission. - Prednisolone dose is reduced to 0.5 mg/kg/day and then tapered slowly. An attmpt to stop treatment should be made after 8 weeks. In patients who relapse, course of prednisolone should be repeated.
- Immunosuppressive drugs: In steroidresistant patients, or in those in whom remission can only be maintained by heavy doses of steroids,cyclophosphamide 1.5–2 mg/kg/ day for 8–12 weeks with concomitant prednisolone 7.5–15 mg/day.
- Levamisole: In corticosteroiddependent children 2.5 mg/ kg to maximum 150 mg on alternate days is useful in maintenance of remission.
Question. Describe causes, clinical features and management of chronic renal failure.
Answer. Persistent impairment of tubular and glomerular function of gradual onset so that kidneys are unable to maintain their normal physiological functions constitutes chronic renal failure.
Causes
- Congenital or heredofamilial disorders: Polycystic disease of kidney, Alport syndrome
- Vascular diseases ofkidney: Vasculitis, polyarteritis nodosa,systemic lupus erythematosus.
- Glomerular diseases: Proliferative glomerulonephritis,
- Crescentric glomerulonephritis, membranous glomerulonephritis, glomerulosclerosis, diabetic nephropathy.
- Tubulointerstitial diseases: Chronic pyelonephritis,tuberculosis of kidney, analgesic nephropathy
- Obstructive renal diseases: Pelvic tumor, benign enlargement of prostrate, retro-peritoneal firosis
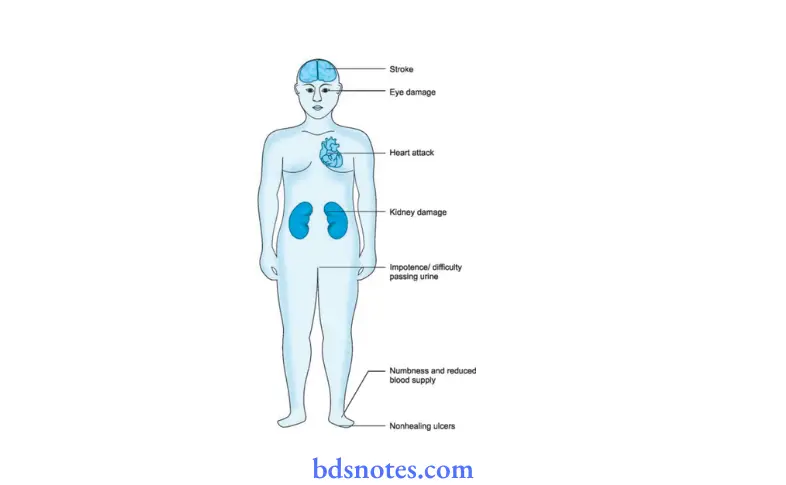
Clinical Features
- Cases of chronic renal failure may remain asymptomatic for a long time and it is often either an intercurrent infection or exacerbation of the disease process or some complications which draw attntion to the patients illness.
- Symptoms are varied and involve all the major systems of body.
- Patient has got marked weakness, lethargy and restlessness.
There is anorexia, nausea and vomiting. - Sleep rhythm is disturbed. Nausea, retching is most marked in the early hours of morning.
- Patient develops revulsion towards food. Dehydration is invariably present.
- Neurological features include headache, lassitude,neuropathy, muscular weakness. In those with severe degree of hypertension, convulsions, muscular twitchings,irritability and in late stages of renal failure, loss of consciousness even leading to coma.
- Hypertension is invariably present in chronic renal failure. Patient may develop hypertensive heart failure,myocarditis or pericarditis.
- Patient has acidotic breathing.
- Repeated chest infections are common. Uremic lung develops soon.
- Skin has a yellowishbrown pigmentation and patient complains of intractable itching.
- Because of disturbances in calcium metabolism (osteomalacia, osteoporosis, renal osteodystrophy) and development of secondary hyperparathyroidism, patient has aches and pains in the bones.
- Cases of chronic renal failure suffr from anaemia which is normocytic normochromic. Bleeding tendency is often present and patient may bleed from various sources.
- Menstrual irregularities in women (amenorrhea, infertility) are common while men may complain of impotence.
- Physical examination reveals generally an ill, looking person, anaemic, pale. Skin is shallow with a peculiar earthy color.
- Tongue is brown, dry and furred.
- Breath has a peculiar ammoniuremic smell (uraemic fetor).
- Hiccough is present.
Management
- The aim is to delay the progression of renal failure and main thought is to correct water and electrolyte disturbances, prevent endogenous breakdown of protein and retention all its end products as well as controlling blood pressure levels and improving the quality of life.
- Diet: Adequate caloric intake by encouraging patient to consume high caloric, carbohydrate foods such as sweetened rice, sugar, sweetened biscuits, cornflour, bread etc.
Restriction of dietary proteins (15-18 g per day) essential to reduce the rate of production of nitrogenous waste products.
High carbohydrate diet gives energy and so it is essential that patient takes adequate amount of calories. - Fluids andelectrolytes: Patients in chronic renal failure have to maintain balance in their salt and water intake.
Fluid intake should be suffientso that patientpasses at least 2–2.5 liters of urine per day.
Overhydration as well as dehydration must be prevented. Salt intake has to be restricted in presence of edema, hypertension and congestive cardiac failure. Intake of potassium has to be restricted. - Anemia: Anemia in chronic renal failure requires fresh blood transfusions. It is bettr to use packed cells.
- Renal bone disease: There is hypocalcemia along with features of hyperparathyroidism.
Calcium orally is given to act as phosphate binder from the gut.
Large doses of vitamin D or D3 are taken to help in the absorption of calcium from the gut. - Hypertension: Control of hypertension is essential, since it shall worsen the renal failure as well as produce various complications.
Angiotensin-converting enzyme (ACE) inhibitors are the one which, are preferred for treating renal hypertension.
Question. Write about diet in renal failure.
Answer. Following is the diet in renal failure:
- Adequate caloric intake by encouraging patient to consume high caloric, carbohydrate foods such as sweetened rice,sugar, sweetened biscuits, corn-flur, bread, etc.
- Restriction of dietary proteins (15–18 g per day) essential to reduce the rate of production of nitrogenous waste products.
- High carbohydrate diet gives energy and so it is essential that patient takes adequate amount of calories.
- Patients in chronic renal failure have to maintain balance in their salt and water intake.
- Fluid intake should be suffient so that patient passes at least 2–2.5 liters of urine per day. Overhydration as well as dehydration must be prevented. Salt intake has to be restricted in presence of edema, hypertension and congestive cardiac failure.
- Intake of potassium has to be restricted if levels of serum potassium are high.
- Diet consists of whole meal bread, marmalade or honey, small quantity of fih, fruits and vegetables.
- Milk about 200 mL per day is permittd.
- Patient can take good quantities of sugar, jam, honey, tea and lemonade.
Question. Write about causes of anasarca and defie and discuss nephrotic syndrome.
Answer. Anasarca is a form of generalized edema. There is massive collection of flid in the subcutaneous interstitial spaces and the various sacs of the body.
The various causes of anasarca are:
Causes Of Anasarca
- Heart disease—right heart failure.
- Kidney disease—nephritis. nephrosis,
- Severe anaemia—tropical diseases (epidemic dropsy)
- Nutritional causes—wet beriberi, hypoproteinemia
- Endocrine disorder—myxedema
- In congenital—general edema.
- Neurological features include headache, lassitude,neuropathy, muscular weakness.
In those with severe degree of hypertension, convulsions, muscular twitchings,irritability and in late stages of renal failure, loss of consciousness even leading to coma. - Hypertension is invariably present in chronic renal failure.
- Patient may develop hypertensive heart failure,myocarditis or pericarditis.
- Patient has acidotic breathing.
- Repeated chest infections are common. Uremic lung develops soon.
- Skin has a yellowishbrown pigmentation and patient complains of intractable itching.
- Because of disturbances in calcium metabolism (osteomalacia, osteoporosis, renal osteodystrophy) and development of secondary hyperparathyroidism, patient has aches and pains in the bones.
- Cases of chronic renal failure suffr from anaemia which is normocytic normochromic. Bleeding tendency is often present and patient may bleed from various sources.
- Menstrual irregularities in women (amenorrhea, infertility) are common while men may complain of impotence.
- Physical examination reveals generally an ill, looking person, anaemic, pale. Skin is shallow with a peculiar earthy color.
- Tongue is brown, dry and furred.
- Breath has a peculiar ammoniuremic smell (uraemic fetor).
- Hiccough is present.
Question. Write in brief on sign, symptoms and treatment of nephrotic syndrome.
Answer. Nephrotic syndrome is a clinical complex with number of renal and extrarenal features
Symptoms
- Gradual onset of generalized edema with puffiss of eyelids.
- Patient complains of loss of appetite, malaise and generalized weakness.
- Swelling over abdomen is present
- Breathlessness is present
- Diarrhea is also present.
- Amount of passing of urination is decreased in 24 hours.
Signs
- Physical examination reveals generalized edematous person.
- Tachycardia is present while blood pressure is normal.
- Pittng edema is present over legs and feet, abdominal walls and lower eyelids.
- Eye lids become puff
- At places where edema is severe ascites and pleural effsion are seen.
- Kidneys are not palpable.
Treatment
Treatment to reduce proteinuria
- Non-specific measures that may reduce proteinuria include ACE and NSAIDs.
- ACEI and ARBs (angiotensinreceptor blockers) reduce proteinuria and slows the rate of progression of rate of renal failure by lowering intraglomerular pressure and preventing development of hemodynamically mediated focal segmental *glomerulosclerosis.
- Edema: Advice patient to take low sodium diet i.e.1 to 2 g/day. In mild edema thiazide induce gentle diuresis. In moderate edema frusemide in doses of 80 to 120 mg/day or torsemide 20 to 40mg/day is given. In patients with severe edema frusemide 20 to 40mg/day is combined with spironolactone 100 to 200mg/day for complete resorption of sodium throughout the nephron.
- Hypercholesterolemia: It is treated by the lipid lowering agent specially statins. Atorvastatin 20 mg OD or BD Anticoagulation is needed for patient with deep vein thrombosis, arterial thrombosis and pulmonary embolism.
Antiplatelet agents and warfarin could be advocated. - Diet: Restricted protein diet is advised since high protein diet accelerates progression of nephritic syndrome.
Vitamin D supplementation is advisable. - Antibiotics: Aggressive antibiotic therapy is given in nephrotic syndrome as chances of sepsis are always present. Mainly cephalexin are given
- Corticosteroids: Produce rapid and complete remission with clearing of proteinuria in 90% cases.
Dose -Prednisolone 1 mg/kg/day, maximum 80 mg/ day. Remission usually occurs between days 7 and 14, though some patients need up to 16 weeks therapy to achieve complete remission.
Prednisolone dose is reduced to 0.5 mg/kg/day and then tapered slowly.
An attmpt to stop treatment should be made after 8 weeks. In patients who relapse, course of prednisolone should be repeated. - Immunosuppressive drugs: In steroidresistant patients, or in those in whom remission can only be maintained by heavy doses of steroids,
cyclophosphamide 1.5–2 mg/kg/ day for 8–12 weeks with concomitant prednisolone 7.5–15 mg/day. - Levamisole: In corticosteroiddependent children 2.5 mg/ kg to maximum 150 mg on alternate days is useful in maintenance of remission.
Question. Write Sign And Symptoms Of Uremia.
Answer. Following are the signs and symptoms of uremia:
Uremia Symptoms
- Malaise, weakness, lethargy and fever.
- Nausea, vomiting, anorexia, diarrhea
- Polyuria and breathlessness when patient gets exerted.
- Headache, confusion and disorientation
- Irregular menstrual cycle and loss of libido.
Uremia Signs
- Presence of flid and electrolyte disturbances.
- Neurological: Cramps, lethargy, myopathy, seizures and coma
- Cardiovascular: hypertension, pulmonary edema,pericarditis
- Gastrointestinal tract: Gastritis and enteritis
- Hematological: Anemia and bleeding diathesis
- Endocrinal: Secondary hyperparathyroidism, amenorrhea,osteodystrophy.
Question. Write Short Note On Acute Nephritis.
Answer. If the kidneys suddenly become inflmed, a condition is developed called acute nephritis. Acute nephritis can lead to kidney failure.
Acute Nephritis Types
There are several types of acute nephritis.
Interstitial nephritis
In interstitial nephritis, the spaces between the renal tubules that form urine become inflmed.
The kidneys swell from the inflmmation.
Pyelonephritis
Pyelonephritis is an infection in the bladder that travels up the ureters and spread into the kidneys.
Glomerulonephritis
This type of acute nephritis produces inflmmation in the glomeruli. Inflmed glomeruli may not fiter the blood properly.
Acute Nephritis Symptoms
- Pain in the pelvis
- Pain or a burning sensation while urinating
- Frequent need to urinate
- Cloudy urine
- Blood or pus may be present in urine
- Pain in the kidney area and/or abdomen
- Swelling in the body, commonly in the face, legs, and feet
- Vomiting
- Fever.
Acute Nephritis Diagnosis
Various diagnostic tests may be needed to confim a case of acute nephritis. These tests include the following:
- A biopsy of the kidneys. A biopsy is a small tissue sample taken from an organ and examined in a laboratory settng.
- Urine and blood testing.
These tests may detect and locate bacteria and signs of infection.
Abnormal blood cells may be present to show signs of infection. - A CT scan may be used to take pictures of your pelvis and abdomen.
Acute Nephritis Treatment
Acute Nephritis Medications:
- Antibiotics and pain relievers may be, used if pyelonephritis is present.
- If high blood pressure is present, calcium channel blockers should be taken.
- Corticosteroids or other immune suppressing medications should also be given.
Acute Nephritis Home Care:
- Drink more and more water: Water helps your kidneys flsh out any waste products that may be hampering the recovery.
- Eat less sodium to prevent flid retention.
Question. Write Short Note On Clinical Features And Treatment Of Post-Streptococcal Glomerulonephritis.
Answer. It follows an acute streptococcal infection of throat or skin by GroupA beta hemolytic streptococci.
Post-Streptococcal Glomerulonephritis Clinical Features
- It is commonly seen in children.
- In morning, there is presence of puffiss over the face and edema over the feet.
- Presence of headache, vomiting and abdominal pain
- Oligouria is present.
- Proteinuria is less, i.e. 1 g/day
- Hypertension is present.
- Circulatory congestion can occur.
Post-Streptococcal Glomerulonephritis Treatment
- Bed rest: Patient should be hospitalized and rest is given till illness is resolved.
In mild cases, bed rest is given for 3 weeks and in severe cases for 3 months. - Fluid restriction: Avoid flid overload.
For fist 24 hours only 500 mL of water or glucose or barley water should be given.
If volume of urine in 24 hours is less than 400 mL teart for acute renal failure and if it is more than 400 mL limit intake of flid to 500 mL + a volume equal to that passed in preceding 24 hours.
Fruit juices rich with potassium are given with caution. - Diet: Restrict dietary protein and restrict sodium and potassium intake.
Monitor potassium and sodium. - Hypertension: Moderatetosevere hypertension is controlled by hydralazine, betablockers such as atenolol or calciumchannel blockers or ACE inhibitors. Salt restriction should be done.
- Antibiotics: Injection benzathine penicillin 500,000 units IM 6 hourly for 7 days.
- Diuretics: It is not indicated unless there is acute LVF or pulmonary edema is present.
Frusemide 40 mg IV daily for few days, followed by oral substitution till diuretic phase is induced. - In patients with progressive renal failure or if fluid overload is present, dialysis may have to be employed.
Question. Write About Acute Renal Failure Under Following Headings.
- Acute Renal Failure Causes
- Acute Renal Failure Management
Answer.
1. Acute Renal Failure Causes:
- Pre-renal causes: The causes for renal hypoperfusion are septicaemia, hypovolemia, hemorrhage, shock,burn, crushing injury, hemolysis inside the vessels,rhabdomyolysis.
- Intra-renal causes: The causes for intrinsic renal disease are renovascular obstruction, glomerulonephritis,vasculitis, tubulointerstitial nephritis, acute tubular necrosis.
- Obstructive causes: Obstruction of the urinary tract at any place.
Acute Renal Failure Management:
Management of acute renal failure is divided into three phase, i.e.
Oligouric phase:
- Water and electrolyte balance should be maintained. One liter of flid should be started and CVP is also maintained. Fluids which are to be replaced should be calculated by loss to urine output of yesterday.
- Proteins should be given, i.e. 20–40 g of proteins per day are given.
- In cases of infections, antibiotics are to be given based on culture and sensitivity test.
- Sodium bicarbonate should be given.
- Dialysis should be done when in oliguria is present, hyperkalemia, metabolic acidosis etc.
Diuretic phase
- Fluid and electrolytes should be replaced.
- IV glucose or glucose saline is given.
- 70–80 g of protein per day is given.
- Patient is told to have plenty of fruit juices.
Recovery phase
After 7–20 days recovery occurs.
Question. Write In Detail About Nephrotic Syndrome Under The Headings:
- Nephrotic Syndrome Defiition
- Nephrotic Syndrome Etiology
- Nephrotic Syndrome Clinical features
- Nephrotic Syndrome Diagnosis
- Nephrotic Syndrome Treatment
Answer.
Nephrotic Syndrome Defiition: Nephrotic syndrome is defied as the presence of heavy proteinuria and hypoalbuminemia in association with varying degrees of edema, lipiduria and hyperlipidemia.
It is a clinical complex with number of renal and extrarenal features
- Hypoproteinemia
- Hypoalbuminemia
- Generalized edema or anasarca
- Hypercholesterolemia
- Hypercoagulability.
- Primary glomerular diseases
- Minimal change nephropathy.
- Mesangioproliferative glomerulonephritis.
- Membranous nephropathy.
- Focal and segmental glomerulosclerosis.
- Crescentic glomerulonephritis
Nephrotic Syndrome Idiopathic:
- Secondary to other diseases:
- Infections: Malaria, hepatitis B, herpes zoster,streptococcal and staphylococcal infections, syphilis,leprosy, schistosomiasis.
- Drugs: NSAIDs, Heavy metals such as gold, anti convulsants, penicillamine, ACE inhibitors, heroin,rifampicin, tolbutamide and probenecid.
- Malignancy: Hodgkin’s disease and other lymphomas.
- Systemic diseases: Diabetes mellitus, amyloidosis, systemic lupus erythematosus, HenochSchonlein purpura, cryoglobulinemia, polyarteritis nodosa.
- Familial disorders: Congenital (neonatal) nephrotic syndrome,
- Alport’s syndrome, Fabry’s disease
- Miscellaneous conditions: Reflx nephropathy, renal vein thrombosis, toxemia of pregnancy, allergic reactions to insect bites, pollens and vaccines, renal artery stenosis.
Nephrotic Syndrome Clinical Features
- Age and sex: Nephrotic syndrome is two to three times more common in childhood with peak incidence at 2–3 years.
In this age group, there is a male : female ratio of 2.5 : 1,in adults, sex incidence is equal. - Edema: It is peripheral involving the limbs, particularly lower limbs.
In children, edema may be more obvious in the face and abdomen.
Usually, massive generalized anasarca, the patient almost weighing double his true weight.
Intense edema of the scrotum or vulva may occur.
There may be bilateral hydrothorax.
Edema may persist for many weeks or months.
Spontaneous subsidence with diuresis (nephrotic crisis) may occur, to be followed again by increase of edema. - Gastrointestinal symptoms: Anorexia causes severe malnutrition, Diarrhea and vomiting due to edema of intestinal wall.
- General symptoms: Prolonged protein loss causes anorexia,lethargy, tiredness, frequent infections and muscle wasting.
Dyspnea may occur, if there is flid in the pleural cavity. - Blood pressure: There may be periods of hypertension;ultimately with development of chronic nephritis permanent hypertension may develop.
Diagnosis is based on clinical signs and investigations:
Nephrotic Syndrome Clinical Signs
- Physical examination reveals generalized edematous person.
- Edema may persist for many weeks or months.
- Tachycardia is present while blood pressure is normal.
- Pittng edema is present over legs and feet, abdominal walls and lower eyelids.
- Eyelids become puff
- At places where edema is severe ascites and pleural effsion are seen.
- Kidneys are not palpable.
Nephrotic Syndrome Investigations
1. Urine examiation:
- Oliguria while edema is forming, dieresis or normal amount of urine during period of subsidence of edema.
- Proteinuria: It is massive, usually more than 5 g/day though variable from time to time; urine becomes almost solid on boiling. Daily loss of protein may be 20–50 g.
- 24 hour urine shows excretion of albumin or protein more than 3.5 g/day.
- Red blood cells are absent or few are seen
- Casts: Fatt casts, tubular cells, oval fat bodies, doubly refractile bodies are seen
2. Blood examination:
- Anemia: It is slight normochromic.
- Hypoalbuminemia: Serum albumin usually less than 3 g/100 mL. Total serum globulin concentration frequently lowered with often elevation of α2 and β-globulins.
- Serum lipids show increase in LDL levels and cholesterol.
- ESR is raised due to hyperfirinogenemia.
- Serum complement level: Serum complement C3 and C4 levels get reduced.
- Other biochemical tests, i.e. blood urea, serum creatinine, creatinine clearance and electrolytes are normal.
3. Ultrasound of abdomen: It can show normal small or large kidneys which depends on the underlying cause.
Amyloid and diabetic kidneys are large while kidney in glomerulonephritis is small.
4. Renal biopsy: It is normal on light microscopy but electron microscopy shows typical abnormalities (effcement of epithelial cell foot processes).
Nephrotic Syndrome Treatment to reduce proteinuria
- Non-specifi measures that may reduce proteinuria include ACE and NSAIDs.
- ACEI and ARBs (angiotensinreceptor blockers) reduce proteinuria and slows the rate of progression of rate of renal failure by lowering intraglomerular pressure and preventing development of hemodynamically mediated focal segmental *glomerulosclerosis.

Leave a Reply