Epidemiology Etiology And Prevention Of Periodontal Disease
Question 1. Define public health dentistry. Write epidemiology of periodontal disease.
Answer.
Definition of Public Health Dentistry
Public health dentistry is defined as “The science and art of preventing and controlling dental diseases and promoting dental health through organized community efforts. It is that form of dental practice which serves the community as the patient rather than individual. It is concerned with the dental health education of the public with applied dental research and with the administration or group dental care programs as well as the prevention and control of dental diseases on community basis.” By American Board of Dental Public Health by Adapting Winslow’s definition (Adopted May 1976).
Epidemiology of Periodontal Disease
Epidemiology of periodontal diseases is studied under three factors
- Host factors
- Agent factors
- Environmental factors
Host Factors in Epidemiology of Periodontal Disease
Following are the host factors in epidemiology of periodontal disease:
Age
Prevalence of periodontal diseases increases with the increasing age. Greater prevalence and severity of periodontal disease in older people is due to cumulative progression of lesions over the time and not due to increased susceptibility in older individuals.
Sex
Males have high prevalence and severity of periodontal diseases as compared to females. As per the latest documentation pathogenesis of periodontal diseases indicates no difference between men and women in susceptibility to periodontitis.
Socioeconomic Status
High income group have lower prevalence of periodontal disease as compared to lower income group because they have means and can afford dental treatment. Lower socioeconomic status have poor diet, poor oral hygiene and lack dental awareness. They cannot afford the high cost of dental services and also the oral hygiene.
Read And Learn More: Public Health Dentistry Question And Answers
Diet and Nutrition
Sticky food adheres to the tooth and is difficult to remove. It interferes with self cleansing process of oral cavity. These foods aggravate already existing periodontal problem. Nutrients associated with periodontal tissues are vitamin A, B complex, C and D, calcium and phosphorus.
Studies have demonstrated that there is high prevalence and severity of periodontal disease in areas where protein calorie malnutrition and vitamin A deficiency is common.
Anatomy
- Health of gingiva and periodontium depends on correct form and position of the teeth in the dental arch. The normal contour of tooth protects the underlying tissues.
- In tooth poor cuspal anatomy, uneven marginal ridges, lack of contact between teeth and crowding can cause food impaction and accumulation causing the underlying gingival tissue to become irritated and inflamed resulting in periodontal disease.
- In soft tissue when frenum is inserted close to themarginal gingiva, pull of this attachment may cause recession of inter-proximal papilla. Proximity of frenum to marginal gingiva interferes with proper use of toothbrush in the area.
Habits
- In unilateral mastication one side of the oral cavity is affected by periodontal disease to a greater degree. Due to tooth extractions, pain and discomfort, patient starts chewing over the healthy side which results in unilateral mastication. Due to this, one side of mouth is healthy, clean and is in proper function while over the neglected side tissue tone get lost, accumulation of food, debris and calculus is seen.
- Abnormal habits such as putting pencil, finger nail, toothpick in the mouth. Opening of bobby pins, lip biting, cheek biting, occupational habits causes trauma to the periodontium.
Systemic Factors
- Uncontrolled diabetes and heavy metal poisoning leads to gingivitis and periodontitis.
- Acute monocytic leukemia may produce gingival enlargement and ulceration.
- AIDS and HIV increase susceptibility for destructive periodontal disease.
Local Irritants
- Mechanical irritants: Faulty toothbrushing can lead to abrasion of teeth and recession of gingiva and also irritates already inflamed tissues.
- Faulty dentistry such as overhanging margins of any restoration or open cavity margins impinge on gingiva or irritate them.
- Faulty orthodontic treatment also results in root resorption as well as alveolar bone loss and mobility.
- Chemical irritants: Alcohol, tobacco and condiments directly lowers tissue and increases gingival susceptibility to gingivitis and periodontal diseases.
- Atmospheric irritants: Because of obstruction in nasal passage, habit, malocclusion, systemic disturbances and psychosomatic factors some patients breathe through the mouth. Dehydration of mucous membrane leads to lowered tissue resistance.
Agent Factors in Epidemiology of Periodontal Disease
Agent factors are dental plaque and calculus.
Dental Plaque
- It is defined as structured, resilient, yellow grayish substance that adheres tenaciously to the intraoral hard surfaces, including removable and fixed restorations.
- Plaque is composed of bacteria in a matrix of salivary glycoproteins and extracellular polysaccharides. It is due to this matrix plaque which cannot be removed by rinsing.
- Dental plaque is classified as supra-gingival and subgingival plaque.
Plaque Biofilm
- It is a well organized co-operating community of microorganisms.
- They are composed of microcolonies of bacterial cells nonrandomly distributed in a matrix.
- Plaque biofilm has open fluid filled channels running through the plaque which permits passage of nutrients and other agents.
- Intercellular matrix consists of organic and inorganicmaterials derived from saliva, gingival crevicular fluid and bacterial products.
- Matrix functions as a barrier to retain and concentrate the substances produced by bacteria.
Calculus
- It is a hard deposit which is formed by mineralization of dental plaque and is covered by a layer of unmineralized plaque.
- Calculus can be classified as sub-gingival and supragingival.
- Supragingival calculus is located coronal to the gingival margin and is white or whitish yellow in color and has hard clay like consistency which can be detached from the tooth.
- Subgingival calculus is located below the crest of marginal gingiva, is dark brown or greenish black in color and is hard and dense which is firmly attached to tooth surface.
- Mineralization of dental plaque leads to formation of calculus.
Environmental Factors in Epidemiology of Periodontal Disease
Geographic Variation
Studies show differences in susceptibility to periodontal disease between the nations. Russell describes population according to whether disease is relatively high, intermediate or relatively low. However the WHO Global Oral Health Data Bank should not implicate any difference between nations and therefore race and ethnicity cannot be considered as risk factors for periodontal disease.
Degree of Urbanization
It is related to periodontal disease. Studies show that people residing in rural areas has significantly higher prevalence of periodontal disease than did urban people.
Psychological and Cultural Factors
Anxiety, fear of dentist, lack of knowledge about diseases and their treatment are some relevant psychological factors. Various culture view dental problems and loss of teeth solely as an extension of aging process.
Question 2. Define epidemiology. What are the host, agent and environmental factors in epidemiology of periodontal diseases. Add the note on prevention of periodontal disease.
Answer.
Definition of Epidemiology
Epidemiology is defined as “the study of the distribution and determinants of health related status for events in specified populations, and the application of this study to the control of health problems.” John M Last (1988)
Prevention of Periodontal Disease
Question 3. Define epidemiology. Discuss the epidemiology of periodontal disease in India with its prevention.
Answer.
Definition of Epidemiology
Epidemiology is defined as “the study of the distribution and determinants of health related status for events in specified populations, and the application of this study to the control of health problems.” John M Last (1988)
Epidemiology of Periodontal Disease in India
- It is widely accepted that periodontal disease affects over 90% of Indian population.
- Majority of Indian population have only mild gingivitis and bleeding from gums which is reversible after proper oral hygiene methods.
- More advanced periodontal disease with pocket formation and bone loss which could ultimately lead to tooth loss if not treated properly may affect 40 to 45% of population.
- Data from national oral health survey (2002-03) suggests that in children of 12 years age, prevalence of periodontal disease was 57%. In 15 years age group it is 67.7%. In 35 to 44 years age group it is 89.6% and 79.9% in 65 to 74 years age group.
- Tabulation of data of various studies regarding epidemiology of periodontitis which were done in India are:

Question 4. What are the various levels of prevalence? Describe various measures in the prevention of periodontal disease in India.
Answer.
Prevalence
It is defined as the efforts, which are made to maintain normal development, physiological function and to prevent disease of the mouth and adjacent parts.
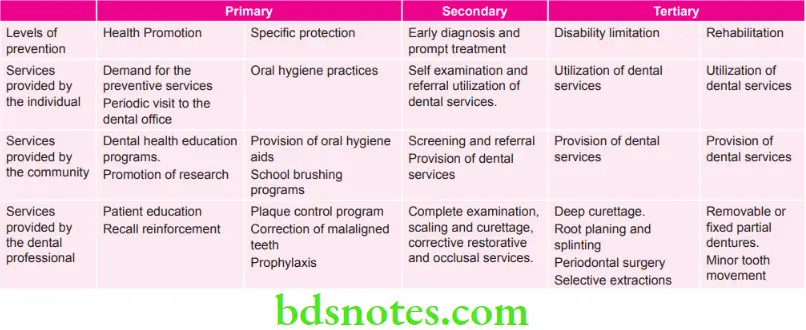
Levels of Prevention
- Primary prevention: It is defined as “action taken prior to the onset of disease, which removes the possibility that a disease will ever occur”.
- Secondary prevention: It is defined as “action, which halts the progress of a disease at its incipient stage and prevents complications”.
- Tertiary prevention: It is defined as “all measures available to reduce or limit impairments and disabilities, minimize suffering caused by existing departures from good health and to promote the patient’s adjustment to irremediable conditions”.
Question 5. Write note on risk factors in periodontal disease.
Answer. The risk factors involved in the susceptibility of periodontal disease are:
- Age: The prevalence of periodontal disease directly with increasing age.
- Sex: In general, males have a higher prevalence and severity of periodontal disease then females.
- Race: Blacks appear consistently to have more severe periodontal disease than whites.
- Education: Periodontal disease is inversely related to increasing levels of education.
- Income: Periodontal disease is inversely related to increasing level of income.
- Place of resistance: In general, the prevalence and severity of periodontal disease are slightly higher in rural area than in urban areas.
- Geographic area: India rates among one of the countries, having the highest prevalence of periodontal disease.
- Psychological and cultural factors: Anxiety, fear of the dentist, lack of knowledge about the disease and their treatment are some of the relevant psychological factors.
- Diet: Decrease in dietary fat content and an increase in sugar consumption increase the prevalence and severity of periodontal disease in India.
- Nutrition: The nutrients that have been specifically associated with periodontal tissue are vitamin A, B complex, C and D, calcium and phosphorus.
- Oral hygiene practice: Poor oral hygiene is an important risk factor in highly susceptible individuals.
- Oral hygiene practices have a major influence on the prevalence of periodontal disease in India.
- Professional dental care: The incidence and severity of periodontal disease are lower in individual who receive regular dental care.
Question 6. Write short note on dental plaque.
Answer. Dental plaque is defined as a structured, resilient, yellow, grayish substance that adheres tenaciously to the intraoral hard surfaces, including removable and fixed restorations.Plaque contains bacteria in a matrix of salivary glycoproteins and extracellular polysaccharides.
Classification of Dental Plaque
- Supragingival plaque: Plaque lies coronal to the gingival margin
- Subgingival plaque: Plaque lies apical to the gingival margin.
Formation of Plaque
- It consists of three stages
- Formation of the pellicle
- Initial adhesion and attachment of bacteria
- Colonization and plaque maturation
- Pellicle is a thin saliva derived layer which forms over tooth surface on exposure to saliva.
- Bacteria are transported to the tooth surface and result in an initial reversible adhesion.
- Firm anchorage occurs between bacteria and tooth surface.
- Microorganisms which are firmly attached start growing and newly formed bacterial clusters form a biofilm.
- A biofilm is well organized and consists of community of microorganisms.
- Biofilm also consists of open fluid filled channels which run through the plaque and permit the passage of nutrients and other agents.
- Intercellular matrix in biofilm acts as a barrier for retention and concentrate the substances produced by bacteria.
- At first 24 hours on a clean tooth, plaque growth is negligible.
- Following three consecutive days plaque growth increases.
- After 4 days 30% of crown is covered with plaque.
- In early phases the plaque consists of gram-positive facultative anaerobes while in later phases those are replaced by gram-negative anaerobes.
Question 7. Discuss the role of bacterial plaque in dental public health. How can you prevent its formation.
Answer.
Role of Bacterial Plaque in Dental Public Health
- Dental caries is a bacterial plaque-dependent disease in dental public health that is characterized by an intermittent demineralization of enamel, dentine and/or cementum.
- Oral microorganisms, when organized in voluminous masses as in dental plaque on tooth surfaces, hydrolyze starches and metabolize sugars to form weak acids (mainly lactic acid) which slowly and intermittently demineralize the hard tissue underneath.
- This utilization of some food components such as sugars by bacteria is a local side effect in the mouth during food passage, in contrast to the systemic effect of carbohydrates as a source of energy for the host.
- Carious demineralization is the result of a side effect namely acid formation from sugars in the bacterial plaque on the teeth in dental public health.
- The sugars and other carbohydrates per se exert no direct damaging effect on the teeth.
- During sleep and when no food is available, the acidogenic plaque bacteria can (slowly) metabolize and survive on a minimum supply of substrate derived from carbohydrate side chains of salivary mucins.
- At these low concentrations, no cariogenic amounts ofacid are formed.
- However oral acidogenic bacteria can handle substrate concentrations of a very large range from very low to very high, and to high concentrations of sugars they react with acid formation immediately.
- For quite sometimes in the early phases of acid attack on our dental tissues, the demineralization is a diffusioncontrolled process resulting in an increase in pore volume only without disintegration of the mineralized tissues; supply and access of saliva are important for remineralization between acid attacks because saliva contains buffering systems and transports mineral and fluoride ions to the tooth-environment interface.
- Both processes, that is, the attacks resulting in demineralization and remineralization resulting in repair, are modified by a number of variables.
- The most important factor on the side of attack is presence of plaque, its thickness and bacterial composition; there is a good reason for not listing carbohydrates such as sugars in the first place: if there is no mature plaque present that is there are no more than thin layers of bacteria, no appreciable amount of acid is formed.
- When the mineralization of plaque occurs it is now known ascalculus which leads to periodontitis in dental public health.
- So the plaque is the biggest factor which leads to the dental caries and periodontitis in dental public health.
Question 8. Write short note on disclosing solution.
Or
Write short note on disclosing agent.
Answer. A disclosing agent is a preparation in liquid, tablet or lozenge form, which contains a dye or other coloring agents, which is used for the identification of bacterial plaque, which might otherwise be invisible to the naked eye.
- When applied to teeth, disclosing agent impart color to soft deposits and is rinsed easily from clean tooth surface.
- So such procedure can demonstrate to patient the presence of deposits and the areas that need special attention during personal oral care.
Uses
- Personalized patient instruction and motivation.
- Self-evaluation by the patient.
- To evaluate the effectiveness of oral hygiene maintenance.
- Preparation of plaque indices.
- In research studies with regard to effectiveness of plaque control devices like toothbrushes and dentifrices, etc.
Ideal Properties
- Intensity of color: Color should contrast with normal color of oral cavity.
- Duration of intensity: Color should not rinse off immediately with ordinary rinsing method or it cannot be removed by saliva.
- Taste: It should be pleasant and encourage cooperation.
- Irritation to the mucous membrane: It should not produce irritation or allergic reaction.
- Diffusibility: A solution should be thin enough so it can be applied readily to the exposed surface of teeth.
- Astringent and antiseptic properties: An antiseptic is applied before scaling.
Technique of Application
- Disclosing solution is applied to tooth surface by using cotton pellet if it is in form of liquid.
- If it is in form of tablets and wafers it can be chewed around the mouth for 30 to 60 seconds and is rinsed.
Question 9. Write short note on toothbrush.
Or
Write in brief on toothbrush.
Answer. Toothbrushes are the most widely used oral hygiene aids.
As per ADA “Toothbrush is designed primarily to promote cleanliness of teeth and oral cavity”.
Types of Toothbrushes
- Manual toothbrushes
- Powered toothbrushes
- Sonic and ultrasonic toothbrushes
- Ionic toothbrushes.
ADA Specifications of a Toothbrush
- 1–1.25 inches in length.
- 5/16 to 3/8 inches in width
- 2 to 4 rows of bristles
- 5-12 tufts/row.
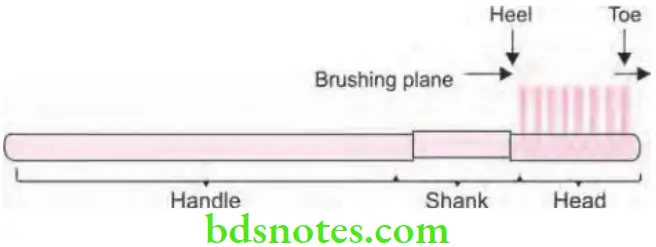
Parts of a Toothbrush
- Handle: The part grasped in hand during toothbrushing.
- Head: The working end of a toothbrush that holds the bristles or filaments.
- Tufts: Clusters or bristles of filaments secure in head.
- Brushing planes: The surface formed by the free ends of the bristles.
- Shank: The section that connects head and handle.
Objectives of Toothbrushing
- To clean teeth and interdental surface of food remnant debris and stains, etc.
- To prevent plaque formation
- To disturb or remove plaque
- To stimulate and massage gingival tissue
- To clean the tongue.
Question 10. Write short note on powered toothbrush.
Answer. Powered tooth-brush is also known as automatic, mechanical or electrical toothbrush.
- Powered tooth brush mimic action of manual toothbrush and also make toothbrushing faster and efficient.
- Heads of these tooth brush oscillate in side to side motion or in a rotary motion.
- Frequency of oscillation is around 40 Hz in an ordinary powered toothbrush.
- Brush heads of powered toothbrushes tend to be more compact than manual toothbrush.
- Bundle of bristles are arranged either in a circular pattern or in a rows which are mounted on a round head.
Types of Powered Toothbrush
Based on type of Brush Head’s shape and movement.
- First generation had a head looking like the one of manual toothbrushes and moving back and forth to simulate manual brushing.
- Rotary toothbrushes: Next generation moved to a design with circular head which is rotating in one direction.
- Counter rotational toothbrushes: Different tufts of brushes rotating in opposite direction.
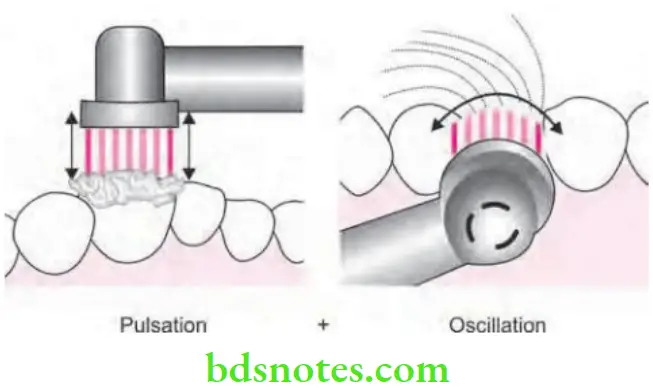
- Rotating-Oscillating: In which a circular head spins back and forth in quick bursts.
- Oscillating-pulsating toothbrushes: They have in addition a pulsating motion to enhance the cleaning action.
Toothbrush Indications
- In young children
- In handicapped patients
- Individuals lacking manual dexterity
- Patients with prosthodontic or endosseous implants.
- Orthodontic patients
- Patients on supportive dental therapy.
Toothbrush Advantages
- It increases patient motivation resulting in better patient compliance.
- Increased accessibility in interproximal and lingual tooth surfaces.
- No specific brushing technique required.
- Use less brushing force than manual tooth brushes.
Maintenance of Toothbrush
- Toothbrushes should be stored in dry areas.
- Toothbrush should be stored in an open air.
- Head of the toothbrush should be upright.
- There should be no contact with other toothbrushes.
Question 11. Write short note on dentifrices.
Answer. “A dentifrice is a substance used with a toothbrush for the purpose of cleaning the accessible surfaces of the teeth”. American Dental Association Council on Dental Therapeutics.
Dentifrices are available in form of toothpaste, toothpowder and gel.
Composition
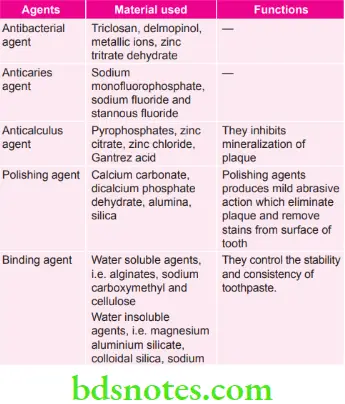
Method of Application
- Toothpaste or gel needed should be pea sized on top half of brush.
- Dentifrice should be dispersed between the bristles and should not be kept on top of bristle.
Question 12. Write short note on modified Bass method for brushing teeth.
Answer.
Technique
- Bristles of the toothbrush should be placed at 450 angle to gingiva.
- Bristles should be vibrated gently by moving the handle of brush in back and forth motion.
- Bristles then swept over the sides of teeth towards the occlusal surfaces in single motion.
Brushing Teeth Indications
- Routine oral hygiene method.
- Cleans inside the sulcus.
Brushing Teeth Advantages
- Cleaning of the sulcus is excellent.
- Interproximal and gingival cleaning is good.
- Gingival stimulation is good.
Brushing Teeth Disadvantages
It is difficult to apply as dexterity of wrist is required.
Question 13. Write short note on interdental cleansing aids.
Answer. Interdental cleansing aids are adjunctive device, which are used to remove plaque from the interproximal tooth surface.
Or
Interdental oral hygiene aids are used to remove plaque and debris that are adherent to the teeth, restorations, and gingiva in interproximal embrasures.
Interdental Cleansing Aids
- Dental floss
- Triangular toothpicks
- Interdental brushes
- Yarn
- Super floss
- Perio-Aids.
Dental Floss
Functions of Dental Floss
- Removal of adherent plaque and food debris from the interproximal embrasure.
- Polishing of tooth surface during removal of the plaque and debris.
- Stimulating and massaging the interdental papillae.
- Improving oral hygiene.
- Reducing gingival bleeding.
Dental Floss may be Available in Various Forms
- Multifilament—twisted or nontwisted
- Bonded or nonbonded
- Thick or thin
- Waxed or nonwaxed
- The waxed floss are generally easier to hold and slide readily between tight contacts.
- The wider ribbon like flosses provide greater surface contact with the enamel surface to help remove plaque.
Unwaxed Dental Floss is Better than Waxed
- It is small in diameter and process more easily through tight interproximal contacts.
- Under tension it flattens out on the tooth surface.
- Unwaxed floss makes a squeaking noise when used on a clean tooth surface.
Methods are Using Dental Floss
- The spool method: Used by adults and teenagers with mental maturity.
- The circle or loop method using by handicapped and mentally retarded patients.
Wooden Tips
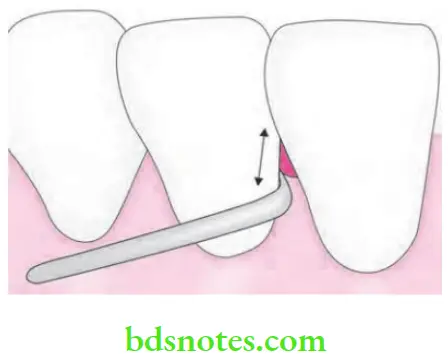
- In type 2 gingival embrasures.
- These devices are manufactured in cross-section.
- Their use is restricted to the facial aspect of anterior teeth.
Interproximal or Interdental Brushes
- In case of type 3 gingival embrasure interdental brushes have proven to be the best choice for plaque removal from interdental tooth surfaces.

Unitufted or Single Tufted Brushes
- Basically used in type 3 gingival embrasures.
- Besides plaque removal these brushes may be used to carry antimicrobial agents (Chlorhexidine) into the interproximal areas.

Question 14. Write in brief chemical means of plaque control.
Or
Write short note on chemical plaque control agents.
Or
Write short note on chemical methods of plaque control.
Or
Write short answer on chemical plaque control.
Answer. As chemical methods of plaque control ADA has accepted two agents, i.e.
- Prescription chlorhexidine rinse.
- Nonprescription essential oil rinse.
Chlorhexidine Gluconate
- It is a cationic bisbiguanide which is effective-against multiple microorganisms, i.e. gram positive, gramnegative microorganisms, fungi, yeasts and viruses.
- Chlorhexidine possess both antiplaque and antibacterial properties.
Mechanism of Action
- Chlorhexidine inhibits plaque formation and leads to the blockage of acidic groups present on salivary glycoprotein and reduces adsorption of glycoprotein on tooth surface.
- It prevents adsorption of bacterial cell wall over tooth surface by binding to bacteria.
- It precipitates agglutination factors in saliva and displace calcium from plaque matrix which prevents binding of mature plaque.
- At low concentration it is bacteriostatic while at high concentration it is bacteriolytic.
Adverse Effects
- Leads to brown staining of teeth and restoration.
- Taste sensation get lost
- In long-term use stenosis of parotid duct may occur.
Nonprescription Essential Oil Rinses
These products have shown relative decrease. The products are:
Triclosan
- Triclosan is a synthetic and nonionic, topical anti-microbial agent.
- It shows broad spectrum activity against both gram-positive and gram-negative microorganisms, mycobacterium spores and candidal activity.
- It acts on the cytoplasmic membrane of microbes and causes leakage of cellular contents and promote bacteriolysis.
Delmopinol
- Delmopinol is a morpholinoethanol derivative.
- It inhibits plaque growth and reduces gingivitis.
- It interferes with plaque formation and reduces bacterial adherence.
- It leads to weak binding of plaque to tooth surface and leads to removal of plaque.
- Its adverse effects are tooth staining, numbness of tongue, mucosal soreness and erosion.
Metallic Ions
- Salts of zinc and copper are commonly used metallic ions.
- They inhibit glycolytic activity in microorganisms and causes delay of bacterial growth.
Quaternary Ammonium Compounds
- Quaternary ammonium compounds are antiseptics and surface active agents.
- Active against the gram-positive and gram-negative organisms.
- Since the compounds consists of positive charged molecule which undergo reaction with negatively charged cell membrane and causes disruption of cell wall of microorganisms.
Sanguinarine
- It is a benzophenanthridine alkaloid.
- It is effective against gram-negative organisms.
Enzymes
- They are used as active agents and are able to break plaque matrix.
- Various proteolytic enzymes are bactericidal.
- They should be used topically in mouth.
Question 15. Write short note on chlorhexidine.
Or
Write short answer on chlorhexidine.
Answer. Chlorhexidine gluconate is a cationic bisbiguanide.
It is effective against an array of microorganisms which includes gram positive and gram negative organisms, fungi, yeasts and viruses.
Chlorhexidine consists of both anti plaque and antibacterial properties.
Mechanism of Action
- The superior anti-plaque activity of Chlorhexidine is because of its property of sustained availability—“Substantivity”. It involves a reservoir of chlorhexidine which slowly dissolve from all the oral surfaces which result in “Bacteriostatic mileu” inside oral cavity Chlorhexidine shows different effects at different concentrations.
- Chlorhexidine is bacteriostatic at its low concentration and is bactericidal at its high concentration. All these concentrations vary between different bacterial species.
- As single rinse is done with chlorhexidine, saliva itself exhibits antibacterial activity for about 5 hours and suppresses salivary bacterial counts for over 12 hours. By several rinses of Chlorhexidine, the number of aerobic and anaerobic species in saliva can be reduced by 80-90%.
- Chlorhexidine causes of inhibition of plaque by:
- It prevents pellicle formation by blocking acidic groups over salivary glycoproteins and so it reduces glycoprotein adsorption over tooth surface.
- It prevents adsorption of bacterial cell wall over the tooth surface by binding to bacteria.
- It prevents binding of mature plaque by precipitatingagglutination factors inside the saliva and displacing calcium from the plaque matrix.
Chlorhexidine Precautions
Avoid using chlorhexidine before/immediately after using a tooth paste because interaction with anionic surfactants which are present inside the chlorhexidine formulation, will decrease effective delivery of chlorhexidine in an active form.
Adverse Effects of Chlorhexidine
- Presence of brownish staining of teeth on the restorations but the staining is reversible.
- Presence of loss of taste sensation.
- There is presence of stenosis of parotid duct.
Question 16. Describe the role and tools of plaque control to achieve oral health.
Or
Write short note on plaque control.
Or
What are the methods of prevention of periodontal disease.
Or
Write short answer on mechanical plaque control.
Answer. Plaque control is the removal of microbial plaque and the prevention of its accumulation on the teeth and adjacent gingival tissue.
- Plaque control is an effective method of treating as well as preventing periodontal disease.
- It is primary level of prevention of periodontal disease.
- Plaque control or oral hygiene aids consists of two types of methods, i.e.
- Mechanical methods.
- Chemical methods.
Mechanical Methods
Following are the mechanical methods:
- Aids for gingival stimulation
- Tongue scrapers.
Aids for Gingival Stimulation
Following are the aids for gingival stimulation, i.e.
- Gingival massage.
- Water irrigation devices.
Gingival Massage
- Gingival massage is the mechanical stimulation of gingiva.
- It is done by toothbrushing or interdental cleaning.
- Gingival massage increase keratinization, increase blood flow and increases the flow of gingival crevicular fluid in gingival sulcus.
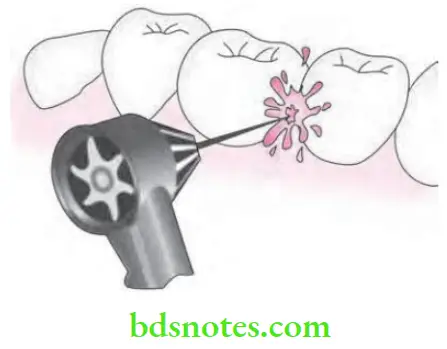
Irrigation Devices (Water Pik) or Hydrotherapy
An irrigating device can be a useful supplement to the toothbrush, particularly where there is fixed bridgework; however, it needs to made clear to the patient that irrigation can remove food debris. This helps in prevention of periodontal disease.
Tongue Scrapers
- It is defined as “process of removing debris from the surface of tongue with some form of scraper designed for this purpose”.
- Many of them are made by soft plastic.
- Metal tongue scrapers are also available in market.
- For scrapping the tongue soft toothbrush can be used.
Question 17. Write short note on prevalent oral hygiene habit in India.
Or
Write short note on oral hygiene habit of Indian people.
Or
Write short note on oral hygiene habit in India.
Answer. According to the consumer usage and attitudes study done in 2010, among the most shocking of revelations is that nearly half of the Indian population does not use a tooth brush and only 51% brushed their teeth using a toothbrush and toothpaste.
- Although brushing was the commonly used method of cleaning.
- Use of “datoon” or tree twig chewing is still very popular in rural India, as an oral hygiene measure and though it is inferior to tooth-brushing.
- Massaging action of tree twig makes it probably the next best option. Its disadvantages include gingival trauma and occlusal wear.
- In some of rural areas in India tobacco is used as a dentifrice. Its name is Gul manjan.
- India is one such country wherein preventive programs have not been completely established.
- Unsurprisingly, standards of oral health are very poor in India, with a large proportion of the population being affected due to poor socio- economic conditions. In addition to this, two-thirds of people have never seen a dentist.
Question 18. Classify plaque control agents used in dentistry. Explain the role of interdental cleaning aids.
Answer. Classification of plaque control agents in dentistry
Mechanical Plaque Control
- Toothbrush
- Manual
- Electrical
- Ionic toothbrushes
- Sonic and ultrasonic
- Inter-dental oral hygiene aids
- Dental floss
- Dental floss holder
- Toothpicks and toothpick holder
- Interproximal brushes
- Single tuft brushes
- Knitting yarn
- Gauze strip
- Pipe cleaner
- Wedge stimulators
- Adjunctive aids
- Irrigation devices (water-pik)
- Tongue cleaner
- Dentifrices
- Mouth rinses (mouthwash)
- Rubber tip stimulator
- Denture brush
Chemical Plaque Control
- Antibiotics
- Enzymes
- Phenolic compounds and essential oils
- Quaternary ammonium compounds
- Bisguanides
- Natural products
- Metal salts
- Amine alcohols
- Oxygenating agents
- Fluorides
Role of Interdental Cleaning Aids
Interdental oral hygiene aids are used to remove plaque and debris that are adherent to the teeth, restorations, and gingiva in interproximal embrasures.
Following are interdental cleaning aids:
- Dental floss
- Dental floss holder
- Toothpicks and toothpick holder
- lnterproximal brushes
- Single tuft brushes
- Knitting yarn
- Gauze strip
- Pipe cleaner
- Wedge stimulators
Dental Floss
Flossing need digit skills and is more time consuming, but there is no alternative for using the floss to clean inter dental space when normal healthy papilla fills interdental space.
Functions of Dental Floss
- Removal of adherent plaque and food debris from the interproximal embrasure.
- Polishing of tooth surface during removal of the plaque and debris.
- Stimulating and massaging the interdental papillae.
- Improving oral hygiene.
- Reducing gingival bleeding.
Disadvantages of Dental Floss
- Not easy to perform specially in posterior areas,
- Requires good manual dexterity.
- Time consuming.
- Risk of frequent shredding when passing through contact point.
- Risk of tissue damage if improperly used.
Types of Dental Floss
- Twisted or nontwisted.
- Bonded or nonbonded.
- Waxed or unwaxed.
- Thin or thick.
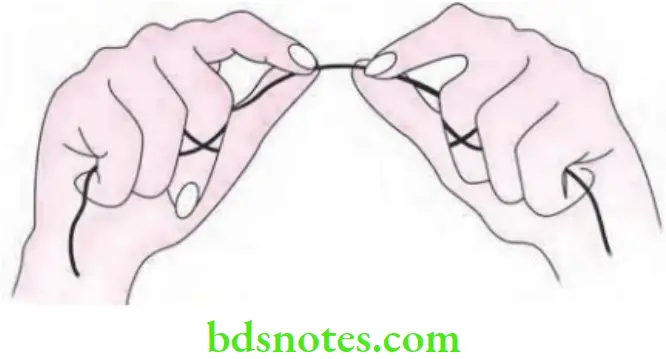
Methods of Using Dental Floss
- Spool method.
- Loop or circle method.
Spool method
It is recommended for teenagers and adults who have acquired the required level of neuromuscular coordination and mental maturity to use floss correctly.
Method
- A piece of floss approximately 18 inch long is taken.
- Bulk of the floss length is lightly wound around the middle finger and the rest of the floss is similarly wound around the same finger of opposite hand.
- Space should be left between wraps to avoid cutting off circulation to the fingers.
- The last three fingers are clenched and both hands are moved apart, pulling the floss taut. The thumb and index finger of each hand are free. The floss is then secured with the index finger and thumb of each hand by grasping a length of 3/4th to 1 inch in each hand.
- The finger of opposite hand can wind the floss as it becomes soiled or frayed to permit access to an unused portion.
Loop Method
This method is particularly suited for children as well as adults with less nimble hands or handicaps such as poor muscular coordination or arthritis.
Method
- A piece of 18 inch long is made into a circle and tied securely with three knots. All fingers except the thumbs are placed within the loop so that fingers or thumbs will be 3/4th to 1 inch apart.
- The floss is guided with the two index fingers for mandibular teeth and with two thumbs or one index finger and one thumb for maxillary teeth. As teeth are flossed, the loop is rotated so that, each proximal area receives unused floss for proper cleaning.
- To be effective the floss should be pulled around the tooth curvature so that, close contact with tooth surface is made
Floss Holder
Floss holder is a flossing aid. The majority of floss holders consist of a device with a handle with two prongs in Y shape or C shape. The floss is tightly secured between the two prongs. The patient holds the handle of the device to guide it during use.
Floss Holder Indications
- Patient with physical disabilities.
- Patient lacking manual dexterity.
- Individuals with large hands.
- Individuals with strong gag reflex.
- Caregivers.
- Type 1 embrasures.
Floss Holder Disadvantages
- More time consuming.
- Unable to maintain tension of floss.
- Must be rethreaded when the floss becomes soiled or frayed.
- Need to set fulcrum to avoid floss cuts.
Toothpicks
Toothpicks are usually made of softwood and have a triangular. A round or rectangular shape. Triangular are said to be superior to the rest as they are ineffective on lingual aspect of proximal surfaces.
Toothpicks Indications
- Type 2 and Type 3 embrasures from facial aspect only.
- Accessible furcations.
- Small root concavities.
- Interproximal open spaces.
Toothpicks Contraindications
- Type 1 embrasures.
- Healthy gingiva.
Toothpicks Disadvantages
- Wearing down of papilla and marginal tissues from incorrect usage.
- Wood ends may cause tissue trauma/ cuts or abrasion.
- Enamel abrasion from incorrect use.
- Can force bacteria or debris into gingival attachment if used improperly.
- May cause opening of the embrasure.
Toothpick Holder
It is also called as periodontal aid. It is an instrument designed to increase patient’s application of the traditional toothpick by holding it securely at the proper angle.
Toothpick Holder Indications
- Plaque removal along the gingival margin.
- Type 2 and Type 3 embrasures from facial or lingual aspect.
- Accessible furcations.
- Concave surfaces in interproximal areas.
- Fixed prosthetic and orthodontic appliances.
- Sulcular cleansing in areas of shallow pocketing.
- Application of fluoride, antimicrobials and desensitizing agents.
Interproximal Brushes
- Also called as interdental brushes, proxa brush.
- They are available in various sizes and shapes.
- The most common are conical or tapered and designed to be inserted into a plastic or metal reusable handle that is angled to facilitate interproximal adaptation. Studies have shown that they are equal to or more effective than floss for plaque removal and for reducing gingival inflammation in Type 2 and Type 3 embrasures and exposed furcations areas.
Interproximal Brushes Indications
- Type 2 and Type 3 embrasures.
- Diastema
- Exposed root furcations.
- Orthodontic and fixed appliances.
- Application of fluoride, antimicrobial or desensitizing agents.
Interproximal Brushes Technique
Inserted interproximally and activated with short back and forth strokes in between the teeth.
Interproximal Brushes Disadvantages
- Different types may be needed to fit different open interproximal spaces.
- Trauma to tooth or gingiva from sharp wire center of some.
Single Tuft Brushes
- Single tuft or end tuft brushes are small brushes with nylon bristles that are attached to a plastic handle.
- There are variations in the shape of the tufts and the width and length of the handles
- Single tuft brushes are indicated in open embrasure areas where there is little or no papilla.
- They are used by placing the brush in the interdental area. The brush is then jiggled in a small circular motion and/or use a sweeping motion away from the gingiva.
Single Tuft Brushes Indications
- The single tuft brush is for patients who prefer a long handle.
- Patients who are not able to change the refills of the interproximal brush.
- Patients who cannot control the interproximal brush due to manual dexterity or disabilities.
Knitting Yarn
- It is used to clean proximal tooth surfaces adjacent to wide embrasure spaces.
- Yarn is used similar to floss.
Knitting Yarn Indications
- Type 2 and Type 3 embrasures.
- Isolated teeth.
- Diastemas.
- Abutments of partial dentures.
- Under sanitary pontics.
- Distal of posterior most teeth in arch.
Knitting Yarn Disadvantage
Yarn may catch on appliances and become stuck on rough appliances and removing a stuck yarn may damage the appliance.
Gauze Strip
It is an effective aid for cleaning the proximal surfaces of teeth specially adjacent to edentulous areas.
Gauze Strip Technique
It is used by positioning the gauze edge length wise with the folds towards the gingiva. Any loose ends are folded inwards to avoid gingival irritation. Gauze is adapted by wrapping it around the exposed proximal surface to the facial and lingual line angles of the tooth. A facial-lingual ‘shoeshine’ stroke is used to loosen plaque and debris.
Gauze Strip Indications
- Type 3 embrasures.
- Diastemas.
- Teeth adjacent to edentulous areas.
- Implant abutments.
Gauze Strip Disadvantage
The patient may damage an appliance while removing stuck gauze.
Pipe Cleaner
They are another useful adjunct to dental flossing for removal of plaque and debris. A pipe cleaner with soft covering and with a minimum exposed wire should be selected. It is used by passing between exposed roots of a furcations and a buccolingual movement is used for cleaning.
Pipe Cleaner Indications
- Type 3 embrasures.
- Exposed root furcations.
- Malpositioned or separated teeth (areas of bone loss and severe loss of tissues).
- Exposed proximal surfaces.
Pipe Cleaner Disadvantages
Sharp wire center can damage the cementum or can cause trauma to gingiva.
Wedge Stimulator
- Wooden and plastic sticks or wedge stimulators reduce bleeding and inflammation when used to reduce plaque. They are wooden or plastic oral hygiene devices designed for interdental cleansing and stimulation. These devices are made of balsa, bass, birch, or linden wood or plastic. Some of the wood stick; are treated with xylitol. They are recommended for use only from the facial aspect, where the proximal surfaces are exposed to avoid traumatizing gingival tissue. Wooden and plastic sticks or wedge stimulators reduce bleeding and inflammation when used to reduce plaque.
- Most wedge stimulators are triangular. They are inserted interdentally, with the base of the triangle resting on the gingival side, the pointing occlusally or incisally and the sides of the triangle against the adjacent tooth surfaces. Such a placement of base of triangle against the tissues prevents damage such as gingival cuts and clefts, to the interdental papilla and gingival margins.
Wedge Stimulator Indications
- Type 2 and Type 3 embrasures from facial aspect only.
- Accessible furcations.
- Application of fluoride, antimicrobial or desensitizing agents.
Wedge Stimulator Disadvantages
- Wearing down of papilla and marginal tissues from incorrect use.
- Enamel abrasion from incorrect use.
- Splaying of wood ends may cause tissue trauma or abrasions.
- Improper use can force bacteria or debris into gingival attachment leading to abscess formation.
Question 19. Write a note on ecological plaque hypothesis.
Answer. This was given by Marsh in 1991.
- In ecological plaque hypothesis, it was proposed that a change in key environmental factor will trigger a shift in the balance of resident plaque microflora and this predispose a site to the disease.
- Occurrence of potentially pathogenic species as the minor members of resident plaque microflora is consistent with this proposal.
- Under the conditions which prevail inside the health, such organisms are only weakly competitive and their growth can also be suppressed by inter-microbial antagonism, now they compromise only a small percentage of plaque microflora and should not be significant clinically.
- Microbial specificity in disease is due to the fact that only some of the species are competitive under new environmental conditions.
- Disease can be prevented not only by inhibiting periodontopathogens directly but also by interfering with factors which drive their transition.

Leave a Reply