Periodontal Microbiology
Question 1. Discuss structure, formation and microbiology of dental plaque.
Answer.
Structure/Morphogenesis
Supragingival Plaque
- It is adherent to tooth structure and consists of gram positive cocci and gram-negative rods and filaments.
- Morphologic arrangement of flora in supragingival plaque is described as corncob formation.
- Corncob formation has a central core which consists of rod shaped bacterial cells which attaches along the surface of the rod-shaped cell.
Subgingival Plaque
- It has many large filaments with flagella and is rich in spirochetes.
- Tooth-associated plaque is same as supraginigival plaque while tissue associated plaque is covered with flagellated bacteria and numerous bristle brush formations. Extracellular matrix is not well Defined. This arrangement is called as test tube brush formation.
- Test-tube brush formation is characterized by large filaments that form long axis and short filaments or gram-negative rods embedded in an amorphous matrix.
Read And Learn More: Periodontics Question And Answers
Formation of Dental Plaque
Formation of Organic Pellicle
- Pellicle is the initial phase of plaque development that forms on all the surface of teeth and artificial prosthesis.
- The first stage of pellicle formation is derived from component of saliva and crevicular fluid as well as bacterial and host tissue cell products and debris. Pellicle consists of glycoproteins, proline rich proteins, phosphoproteins, histidine-rich proteins, enzymes as well as various other molecules which act as adhesion site for the bacteria.
- There is adsorption of the positively charged salivary fluid, crevicular fluid and various other environmental molecules to the negatively charged hydroxyapatite surfaces of teeth via electrostatic, Van der Waals and hydrophobic forces.
- Pellicle functions as a protective barrier providing lubrication for the surface and preventing tissue desiccation. Pellicle is a non-shedding hard surface provides a substrate on which bacteria progressively accumulated to form a dental plaque.
Initial Colonization of Bacteria on Tooth Surface:
- Within a few hours, bacteria are formed on a dental pellicle. The initial bacteria which colonize on pellicle coated tooth surface are predominantly gram positive facultative microorganisms such as S. sanguinis, S. mitis and Actinomyces species.
- Adherence of bacteria via various specific attachments, i.e. extracellular polymeric substances and specific molecules, i.e. adhesions, which attach to receptors at dental pellicle.
- Each of the oral bacteria has different cell surface binding site for attachment and multiplication.
Following are the various sequences which shows the attachment of bacteria to the tooth surface.
First phase: Transport to Surface
This phase consists of initial transport of bacteria to the tooth surface. Various contacts can occur via chemotactic activity, Brownian motion, sedimentation of microorganisms, etc.
Second phase: Initial Adhesion
This phase consists of initial reverse adhesion of bacterial which get initiated by integration of bacteria and tooth surface from a distance through long range or short range forces which consists of Van der Waals forces and electrostatic forces.
Third Phase: Attachment
- As initial adhesion finishes, firm adhesion between bacteria and tooth surface occur via covalent, ionic and hydrogen bonding.
- If there is presence of rough surface, bacteria protect themselves against the shear forces and the bonding becomes irreversible.
Fourth phase: Colonization of surface and biofilm formation
As firmly attached bacteria starts their growth, newly formed bacterial clusters remain attached to microcolonies or there is a development of a biofilm.
Secondary Colonization and Plaque Maturation
- Initial colonizers use the available oxygen which causes decrease in the levels of oxygen as well as redox potential which favors growth of gram-negative anaerobic organisms i.e. Fusobacterium nucleatum and Capnocytophaga species.
- Now these microorganisms adhere to the cell surface receptors of initial colonizers as they vave poor ability of attachment directly to pellicle, so as plaque mature number of gram-negative bacteria increases.
- These microorganisms adhere to cells of bacteria already in the plaque mass by a process known as coaggregation and this play very important role in secondary colonization.
- During early stages of plaque formation interaction between gram-positive and Gram negative bacteria occur which is followed by coaggregation in the later stages between gram-negative organisms.
- Within the plaque matrix nutrients are required so that there is growth of bacteria in plaque matrix. Main source of nutrient is saliva.
- If plaque is established substances produced by various species become nutrients which are essential for growth of other organisms.
- Long-standing supragingival plaque demonstrates corncob as well as test-tube brush arrangement.
- Corncob formation are observed between rod-shaped bacterial cells which forms the inner structure and the coccal cells which attach along the surface of rod-shaped cell while the test-tube brush arrangement consists of filamentous bacteria to which gram-negative rods adhere.
- Early colonizers which lead to plaque formation lie in yellow and purple complex while secondary colonizers lie in green, orange and red complexes.
Microbiology of Dental Plaque
The organisms associated with plaque formation are:
Gram +ve
- Actinomyces viscosus
- Streptococcus sanguinis
Gram –ve
- Actinobacillus actinomycetemcomitans
- Bacteroides forsythus
- Capnocytophaga species
- Porphyromonas gingivalis
- Prevotella intermedia
- Treponema denticola
- Fusobacterium nucleatum
Red Complex
- Porphyromonas gingivalis
- Treponema denticola
- Bacteroides forsythus
Purple Complex
- Veillonella parvula
- Actinomyces odontolyticus
Yellow Complex
- Streptococcus mitis
- Streptococcus oralis
- Streptococcus sanguinis
- Streptococcus gordonii
- Streptococcus intermedius
Green Complex
- Actinobacillus actinomycetemcomitans
- Capnocytophaga species
- Eikenella corrodens
Orange Complex
- Prevotella intermedia
- P. nigrescens
- Peptostreptococcus micros
- Fusobacterium nucleatum
- C. Showae
- E. nodatum
- Early colonizers which lead to plaque formation lie in yellow and purple complex while secondary colonizers lie in green, orange and red complexes.
Question 2. Define dental plaque and give its Classification and composition, describe in detail the role of dental plaque in initiation and progression of periodontal disease.
Or
Define dental plaque. Discuss its role in etiology of periodontal disease.
Or
Define and classify plaque. Write its role in periodontal disease.
Answer. Dental plaque: Dental plaque is Defined as an adherent intercellular matrix consisting primarily of proliferating microorganisms along with a scattring of epithelial cells, leucocytes and macrophages.
Plaque
It is Defined as the sof deposit which forms the biofim adhering to the tooth surface or other hard surfaces in oral cavity including removable and fied restorations.
Classification of Dental Plaque
Based on the relationship to gingival margin
- Supragingival:
- Coronal plaque: Plaque in contact with only tooth surface
- Marginal plaque: Associated with the tooth surface at gingival margin
- Subgingival:
- Attached plaque: It can be tooth, epithelium and/or connective tissue associated.
- Unattached subgingival plaque
Composition of Dental Plaque
- Bacteria along with the intercellular matrix are microbial plaque.
- 1 mg of dental plaque contains up to 250 million bacteria.
- Non-bacterial microorganisms such as yeast, mycoplasma, protozoa as well as some viruses are seen in small amount.
- Various host cells, i.e. epithelial cells, macrophages and leucocytes are also present.
- Intercellular matrix accounts for 25% of plaque volume and have organic and inorganic materials.
- Organic matter has polysaccharide protein complex produced by microorganisms.
- Protein such as albumin present in plaque is derived from gingival crevicular fluid.
- Various carbohydrates are also present, i.e. levans, glucans, galactose and methylpentose. Carbohydrates in form of levans provide mainly energy while glucans not only provide energy but also work as organic skeleton of plaque.
- Lipids are also present in plaque and are derived from disrupted cell wall of gram-negative bacteria.
- Various inorganic material of plaque are calcium, phosphorus with small amount of magnesium, potassium and sodium.
Role of Dental Plaque in Periodontal Disease
- Gingival sulcus and periodontal pocket consists of plenty of gingival crevicular fluid, which flows outward from the base of the pocket. So, to colonize themselves, bacteria must attach to available surfaces for preventing the displacement by fluid flow. So adherence represents a virulence factor. Surfaces which are available for attachment are as follows:
- Tooth or root, e.g. A. viscosus binds to proline-rich proteins which are found on saliva-coated tooth surfaces.
- Tissues, i.e. P. gingivalis bind to connective tissue components i.e. firinogen and fironectin.
- Pre-existing plaque, e.g. A. viscosus bind to polysaccharide receptor present on cells of Streptococcus sanguinis.
- Bacteria present in plaque can lead to periodontal disease directly by injuring the host tissues through toxins, enzymes and toxic metabolic end products or indirectly by stimulating host-mediated responses which leads to tissue injury.
- Process of tissue destruction results from elaboration of bacterial substances that directly or indirectly cause degradation of the periodontal tissues.
- Many of the periodontal pathogens invade the periodontal tissues and evade the host defenses which cause them to infect and as well as damage the periodontal tissues.
- Bacteria may enter host tissues by following:
- Bacteria penetrate directly by widening and rupturing intercellular spaces of stratum spinosum and perforation found in basal lamina.
- Bacteria can also penetrate through the ulcerations in epithelium of sulcus or pocket.
- Bacteria can invade throughout the microholes present in the surface created by transmigrating leucocytes.
- Pathogens such as A. actinomycetemcomitans and P. gingivalis suppress the host defense cells. A. actinomycetemcomitans secrete an exotoxin, i.e. leukotoxin which inhibit the function of polymorphoneutrophils and is also capable of killing mature T and B cells.
- IgA, IgG proteases, firolysin catalase and superoxide dismutase leads to evasion of host defenses.
- Various enzymes are released by these pathogens such as collagenases, aminopeptidases, gelatinase, acid phosphatase, alkaline phosphatase and hyaluronidase causes tissue destruction and periodontal disease manifestations.
- Lipopolysaccharides of gram-negative bacterial cell wall has complex lipid, i.e. lipid A which is attached to a polysaccharide. This lipopolysaccharide is known as endotoxin as it is fimly bound to tooth surface and is released when the cells are lysed.
- As there are many gram-negative bacteria present in periodontal pocket which leads to release of endotoxin which interact with the receptors present on macrophages and monocytes which causes release of cytokines, i.e. Interleukin 1 and tumor necrosis factor. Complements are also activated through alternative pathway. This causes intravascular coagulation and tissue necrosis and also has cytotoxic effects on fibroblasts and various other cells.
- Endotoxins also cause leucopenia and play an important role in pathogenesis of periodontal diseases.
- Peptidoglycan found in many bacteria causes stimulating bone resorption and inducing macrophages to produce prostaglandin and collagenases.
- Capsular substances also lead to tissue destruction. These capsular substances are seen on outermost surface of many bacterial cells.
Question 3. Write short note on subgingival plaque.
Answer. Subgingival plaque is found below the gingival margin between the tooth and gingival circular tissue.
- It is usually thin, contained within the gingival sulcus or periodontal pocket and thus cannot be detected by direct observation.
- Its presence can be identifid only by running the end of probe along gingival margin.
- There are three types of subgingival plaque:
- Tooth-associated subgingival plaque: The structure is similar to the supragingival plaque. The flora is associated with calculus formation, root caries and root resorption.
- Epithelium-associated subgingival plaque: This type of plaque is usually adherent because it lacks the interbacterial matrix and is in direct association with gingival epithelium.
- Connective tissue-associated plaque: It is usually demonstrated in ANUG and localized juvenile periodontitis patient. Its clinical signifiance is unclear.
The tooth-associated subgingival plaque is most important in calculus formation, root caries and slowly progressive periodontal destruction.
Question 4. Write short note on Materia alba.
Answer. Materia alba is a concentration of microorganisms, desquamated epithelial cells, leukocytes and a mixture of salivary proteins and lipids, with few or no food particles and it lacks regular pattern observed in plaque.
- It is a yellowish or grayish white, soft sticky deposit and is less adherent than dental plaque.
- The irritating effct of materia alba on gingiva is caused by bacteria and their products.
- The materia alba is easily displaced with the water spray. Aqueous solutions are typically cleared within 15 minutes whereas sticky foods may adhere for more than one hour.
- Materia alba is the ideal growth medium for bacteria which leads to gingival inflammation.
Question 5. Give defiition and composition of dental plaque. Discuss specific and nonspecific plaque hypothesis.
Or
Write short note on specific plaque hypothesis.
Or
Write short note on specific and non-specific plaque hypothesis.
Answer.
Walter Loesche proposed the nonspecific and specific plaque hypothesis in 1976.
Nonspecific Plaque Hypothesis
- It states that it is the total bulk of plaque, which determines the pathogenicity rather than the individual species within it
- It means all plaque is equally pathogenic
- According to this, when only small amount of plaque are present, the products released by this get ‘neutralized by the host. Large amount of plaque would produce large amount of noxious products, which would overwhelm the host’s defense.
- Inherent concept of non specific plaque hypothesis is that control of periodontal disease depends on control of amount of plaque accumulation.
Specific Plaque Hypothesis
- It states that not all plaque is pathogenic and its pathogenicity depends upon the presence of the certain specific microbial pathogens in plaque. This is based on the fact that the specific microorganisms responsible for periodontal disease release certain damaging factors that mediate the destruction of the host tissue. For example, Actinobacillus actinomycetemcomitans as a possible pathogen responsible for localized juvenile periodontitis.
- This hypothesis was revisited to state that the disease associated with specific strains of given species. Revision was done because there is fiding of multiple strains of any given bacterial species which show diffrence in their virulency.
Question 6. Define dental plaque. Classify plaque. Describe stages of plaque formation.
Or
Define dental plaque. Classify the types of plaque. Discuss the stages of plaque formation.
Or
Write short note on stages of plague formation.
Or
Define dental plaque and give its Classification. Describe the different stages of plaque formation.
Answer.
Dental Plaque
Dental plaque is Defined as an adherent intercellular matrix consisting primarily of proliferating microorganisms along with the scattering of epithelial cells, leucocytes and macrophages.
Classification of Dental Plaque
Based on the relationship to gingival margin
- Supragingival
- Coronal plaque: Plaque in contact with only tooth surface
- Marginal plaque: Associated with the tooth surface at gingival margin
- Subgingival
- Attached plaque: It can be tooth, epithelium and/or connective tissue
- Associated.
- Unattached subgingival plaque
Question 7. Define and classify plaque. Describe in detail the composition, morphogenesis and steps in the formation of dental plaque.
Or
Define dental plaque. Classify types of plaque. Discuss composition and formation of plaque.
Or
Define plaque. Describe the composition, structure and formation of dental plaque.
Or
Define dental plaque. Describe the structure and composition of dental plaque.
Or
Discuss the composition, formation and role of dental plaque in periodontal diseases.
Or
Define plaque. Write about its composition and formation of plaque.
Answer.
Structure/Morphogenesis
Supragingival Plaque
- It is adherent to tooth structure and consists of gram positive cocci and gram-negative rods and filaments.
- Morphologic arrangement of flora in supragingival plaque is described as corncob formation.
- Corncob formation has a central core which consists of rod shaped bacterial cells which attaches along the surface of the rod-shaped cell.
Subgingival Plaque
- It has many large fiaments with flgella and is rich in spirochetes.
- Tooth-associated plaque is same as supraginigival plaque while tissue associated plaque is covered with flgellated bacteria and numerous bristle brush formations. Extracellular matrix is not well Defined. This arrangement is called as test tube brush formation.
- Test-tube brush formation is characterized by large filaments that form long axis and short filaments or gram-negative rods embedded in an amorphous matrix.
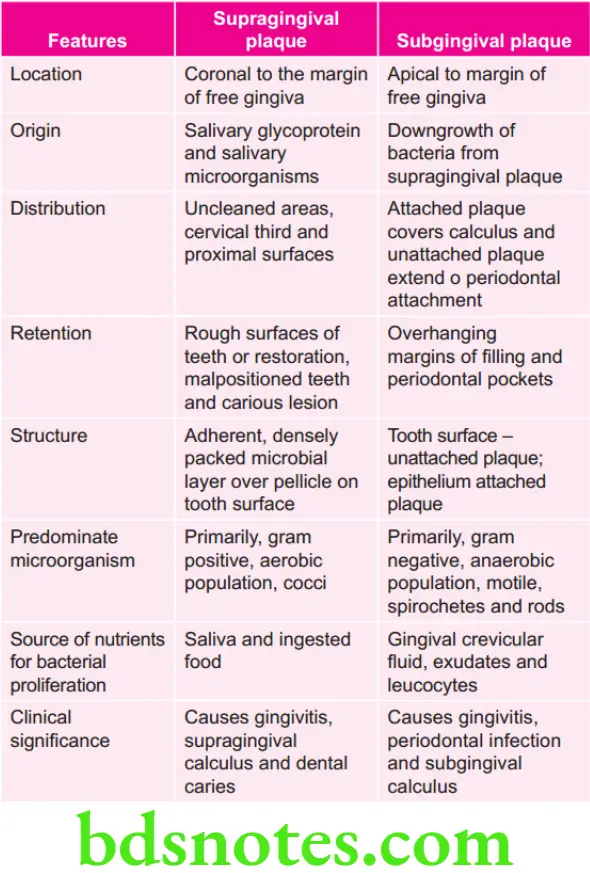
Question 8. Write differences between supragingival and subgingival plaque.
Answer.

Leave a Reply