Bone Loss And Patterns Of Bone Destruction
Question 1. Write short note on patterns of bone destruction in periodontal disease.
Or
Describe various patterns of bone destruction in various diseases.
Answer.
The Patterns of Bone Destruction in Periodontal Disease
- Horizontal bone loss
- Margins gutter
- Irregular bony margins
- Vertical or angular defects
- Osseous craters
- Bulbous bony contours
- Reverse architecture
- Ledges
- Furcation involvement
- Fenestration and dehiscence
Read And Learn More: Periodontics Question And Answers
Horizontal Bone Loss
It is the most common pattern of bone loss in periodontal disease. The bone is reduced in height but the bony margin remains approximately perpendicular to tooth surface. The interdental septa and facial and lingual plates are affected, but not necessarily to an equal degree around the same tooth.
Vertical or Angular Defects
These are those defects occurs in oblique direction, leaving a hollowed out trough in bone alongside the root, the base of defect is located apical to surrounding bone. In most of the situation angular defects are accompanied by infrabony pockets.
Osseous Craters
They are concavities in the crest of the interdental bone confined within the facial and lingual walls. It is found to make up two-thirds of all mandibular defects, can be diagnosed by transgingival probing.
The following reasons have been suggested for the high frequency of interdental craters:
- Interdental areas are more prone to the accumulation of plaque and are more difficult to clean.
- The normal flat or even concave sublingual shape of the interdental septum in lower molars may favor crater formation.
- Vascular patterns from the gingiva to center of the crest may provide a pathway for inflammation.
Bulbous Bony Contours
They are bony enlargements caused by exostoses, adaptation to function or buttressing bone formation. They are found more frequently in the maxilla than mandible.
Reversed Architecture
These defects are produced by loss of interdental bone, including the facial and lingual plates without concomitant of radicular bone, thereby reversing the architecture (more common in maxilla).
Ledges
They are plateau-like bone margins caused by resorption of thickened bony plates.
Furcation Involvement
It refers to the invasion of the bifurcation and trifurcation of multirooted teeth by periodontal disease. Mandibular first molars are most common sites and also common are maxillary premolars.
The role of trauma from occlusion in the effect of furcation involvement is controversial; others include by careful probing with Naber’s probe and radiograph of this area is helpful, but can be obscured by varied factors such as, angulations of the beam and radiopacity of adjacent structures.
Fenestration and Dehiscence
- Fenestrations are the isolated areas in which root is denuded of bone and marginal bone is intact while dehiscence are the denuded areas which extend through marginal bone.
- They are associated with extreme buccal or lingual version of teeth.
- These defects are important clinically because wherever these defects occur root is only covered by periosteum and overlying gingiva.
- These areas become crucial, if periodontal disease occur or if gingival recession takes place since they may complicate therapy and adversely affect area’s prognosis.
Marginal Gutter
It is a shallow linear defect between marginal bone of radical cortical plate or interdental crest, extending the length of one or more root surfaces, usually formed by resorption of socket side of plate and deposition of facial surface.
Irregular Bony Margins
They are the abrupt irregularities in scalloped level of marginal bone and interdental septa.
Question 2. Write short note on bone loss and pattern of bone loss.
Answer. Bone loss in periodontal diseases is determined by the radiograph.
- It shows amount of remaining bone rather than amount of bone lost.
- Amount of bone loss is estimated to be the difference between the physiologic bone level of the patient and height of remaining bone.
- The distribution of bone loss is an important diagnostic sign. It points to the location of destructive local factors in different areas of mouth and in relation to different surfaces of same tooth.
Question 3. Discuss the patterns and pathogenesis of alveolar bone loss in periodontal disease.
Answer.
Pathogenesis of Alveolar Bone Loss in Periodontal Disease
- Bacterial plaque products induce the differentiation of bone progenitor cells into osteoclasts and stimulate gingival cells to release mediators that have the same effect.
- Plaque products and inflammatory mediators can also act directly on osteoblasts or their progenitors, inhibiting their action and reducing their numbers.
- Bacteria induce tissue destruction indirectly by activating host defense cells, which in turn produce and release mediators that stimulate the effectors of connective tissue breakdown.
- Components of microbial plaque have the capacity to induce the initial infiltration of inflammatory cells, including lymphocytes, macrophages and polymorphonuclear leukocytes (PMNs).
- Microbial components, especially lipopolysaccharide (LPS), have the capacity to activate macrophages to synthesize and secrete a wide array of molecules, including the cytokines, Interleukin-1(IL-l) and tumor necrosis factor-alpha (TNF-α), prostaglandins especially PGE2 and hydrolytic enzymes.
- Bacterial substances activate T lymphocytes and produce IL-1 and lymphotoxin (LT), a molecule having properties similar to TNF-α.
- These cytokines manifest potent proinflammatory and catabolic activities, and play key roles in periodontal tissue breakdown.
- Bacteria mediated; LPSs, lipoteichoic acids, peptidoglycan, capsular and surface-associated material, muramyl dipeptide, lipoprotein.
- Host mediated: Prostaglandins, leukotrienes, heparin, thrombin, bradykinin, cytokines, HA and IL-6, TNF, transforming growth factor-β, platelet-derived growth factor.
- Host factors released by inflammatory cells are capable of inducing bone resorption. These include host-produced prostaglandins and their precursors IL-lα and IL-1β and TNF-α.
- Bone destruction in periodontal disease is caused by local and systemic factors.
- Local factors fall into the following groups:
- Those that cause gingival inflammation.
- Those that cause trauma from occlusion
- Reduction in the height of alveolar bone is caused by extension of gingival inflammation, whereas trauma from occlusion causes bone loss lateral to the root surface.
- Systemic Factors
- When generalized tendency towards the bone resorption exists, bone loss initiated by the local factors magnified by the systemic conditions.
- Osteoporosis is a physiological condition in postmenopausal women resulting in loss of bone mineral content and structural bone changes.
- In certain generalized skeletal disturbances like hyperparathyroidism, leukemia and Langerhans cell histiocytosis, periodontal bone loss may occur by mechanisms that are totally unrelated to usual periodontal problem.
- Local factors fall into the following groups:
Question 4. Describe the pathways of inflammation from gingiva to periodontal supporting tissues with appropriate diagrammatic presentation. Enumerate the various patterns of bone destruction in periodontitis and give a note on vertical or angular defects.
Answer.
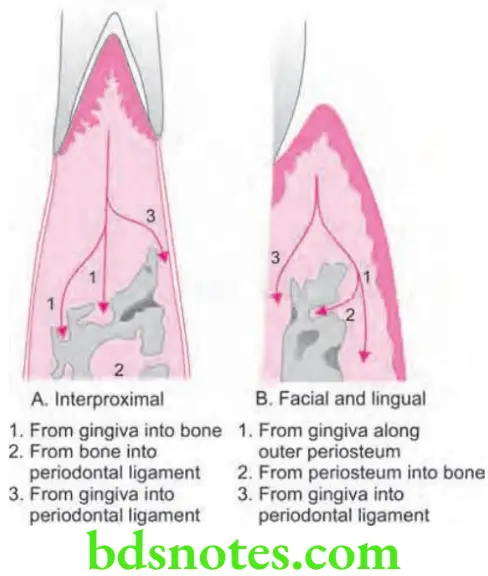
Pathways of Inflammation from Gingiva to Periodontal Supporting Tissues
- Interproximally from gingiva to bone and from bone to periodontal ligament.
- Facially and lingually from gingiva to bone along the outer bone and from gingiva into the periodontal ligament.
- Gingival inflammation can spread through transseptal fibers in the bone along the vessel channel which course throughout the alveolar bone and perforate the crest of interdental septum. The inflammation thus enters the centre of crest or through its side depending upon the course of the vessel channel. After reaching the bone, inflammation may again return to periodontal ligament.
- Gingival inflammation can spread directly from gingiva to periodontal ligament and from there on to interdental septum.
- Outer periosteal surface provides less physical resistance to spread of inflammation and inflammation thus spread lingually or facially along this surface and penetrate into the marrow spaces by coursing along supra periosteal vascular network.
Various Patterns of Bone Destruction in Periodontitis
- Horizontal bone loss
- Vertical or angular defects
- Osseous craters
- Bulbous bony contours
- Reverse architecture
- Ledges
- Furcation involvement.
- Fenestration and dehiscence
- Marginal gutter
- Irregular bony margins
Vertical or Angular Defects
Vertical or angular defects are those which occur in an oblique direction and leave a hollow out trough in bone alongside the root.
- Base of the defect is located apical to surrounding bone.
- Mostly angular defects are accompanied by intrabony periodontal pockets.
- Vertical defects detected radiographically appear most often on distal surfaces and mesial surfaces.
- When inflammation spread directly from gingiva to periodontal ligament and from periodontal ligament to bone it will lead to angular type of bone loss.
- Angular defects can also occur on facial and lingual or palatal surfaces, but these defects are not appreciated on the radiographs.
- Surgical exposure is the only means by which vertical osseous defects are detected.
- Vertical defects increases as the age advances.
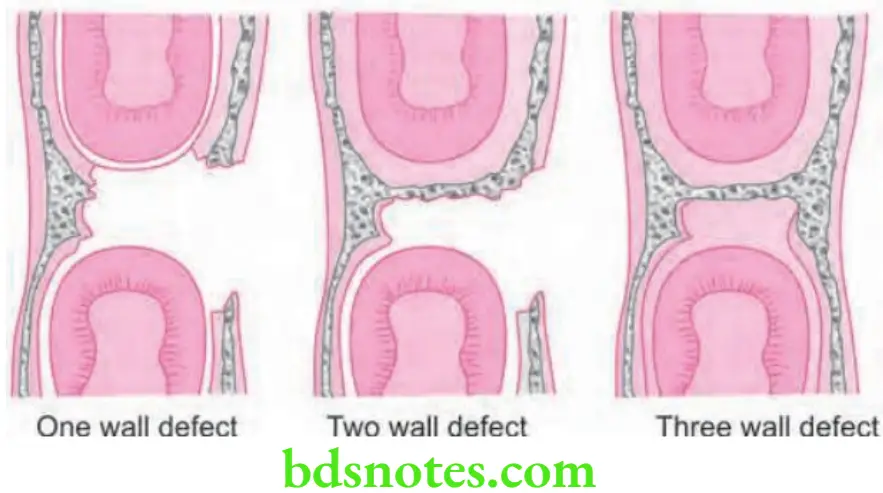
Classification of Vertical or Angular Defects
- One walled or hemiseptal defect: One wall is present
- Two walled defect: Two walls are present
- Three walled or intrabony defect: Three walls are present
- Combined osseous defect: Number of walls in apical portion of defect is greater than that in its occlusal portion. The less the number of walls remaining poor is the prognosis.
Question 5. Write short note on types of osseous defects.
Answer. Osseous defects are those defects which are formed as a result of destruction of alveolar bone due to periodontal disease.
Various Types of Osseous Defects
According to Goldman and Cohen (1958)
- One-walled defect
- Two-walled defect
- Three-walled defect
- Combined defect
According to Glickman (1964)
- Osseous/interdental craters
- Hemiseptal defects
- Infrabony defects
- Bulbous bone contour
- Inconsistent margins and ledges (plateau-like bony margins)
- Reversed architecture
According to Prichard (1967)
- Interproximal crater
- Inconsistent margins
- Hemisepta
- Furcation invasion
- Intrabony defects
- Combination
According to Manson and Nicholson
- Thickened margins
- Interdental crater
- Hemiseptum
- Infrabony defect with 3 osseous walls
- Infrabony defect with 2 osseous walls
- Infrabony defect with one osseous wall other than hemiseptum
- Marginal gutter
- Furcation involvement
- Irregular bony margins
- Dehiscence
- Fenestration
- Exostosis

Leave a Reply