Parotid region
Question 1. What are the boundaries of the parotid region?
Answer.
Parotid Region Boundaries
Anterior: Anterior border of masseter
Posterior: Mastoid process
Parotid Region Above: Zygomatic arch
Parotid Region Below: Line joining the angle of the mandible to the mastoid process
Question 2. What is the parotid bed?
Answer.
It is the retromandibular space where the parotid gland lies.
Parotid Bed Boundaries
Anterior: Posterior border of ramus of mandible
Posterior: Mastoid process
Superior: External acoustic meatus
Medial: Styloid process
Question 3. Describe the parotid gland under the following headings:
- External features,
- Relations,
- Nerve supply and
- Applied anatomy.
Answer.
Parotid Gland External features The parotid gland is the largest salivary gland (weight: 25 g) located in the parotid region. It resembles a three-sided inverted pyramid and presents the following features.
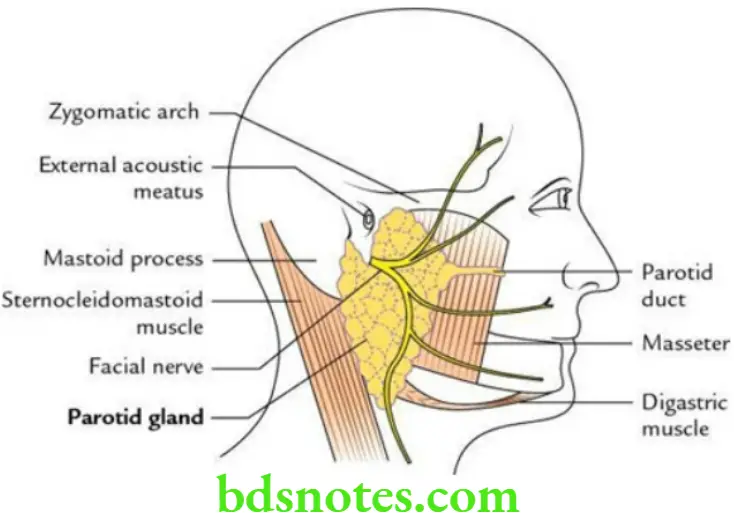
Apex: Directed downwards
Base: Directed upwards
Parotid Gland Three surfaces:
- Superficial (largest)
- Anteromedial
- Posteromedial
Parotid Gland Three borders:
- Anterior
- Posterior
- Medial
Read And Learn More: Selective Anatomy Notes And Question And Answers
Relations
Apex: It is related to the posterior belly of the digastric.
Base: It is related to:
- External acoustic meatus
- Posterior aspect of the temporomandibular joint
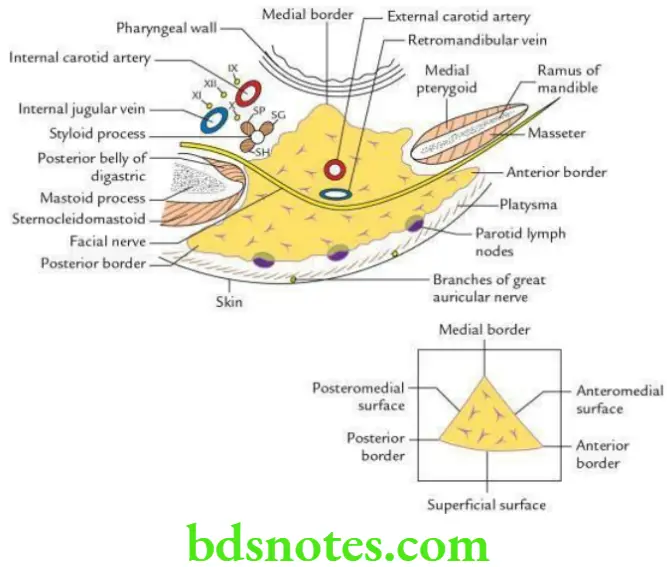
Superficial surface: It is related to:
- Skin
- Superficial fascia containing platysma, branches of great auricular nerve and superficial parotid lymph nodes
- Parotidomasseteric fascia
- Deep parotid lymph nodes embedded in the gland
Anteromedial surface: It is related to:
- Masseter
- Posterior border of ramus of mandible
- Medial pterygoid
Posteromedial surface: It is related to:
- Mastoid process and muscles covering it
- Styloid process and muscles covering it
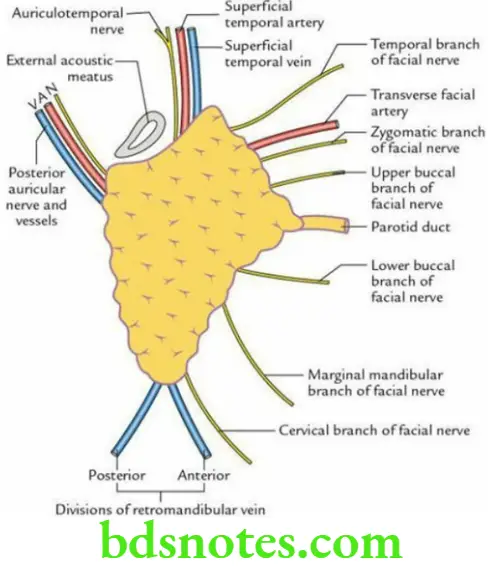
Anterior border: The following structures (from above to downwards) emerge underneath this border:
Posterior border: The following structures emerge from underneath this border:
- Posterior auricular nerve
- Posterior auricular vessels
Medial border: It is related to the lateral wall of the pharynx.
Nerve supply
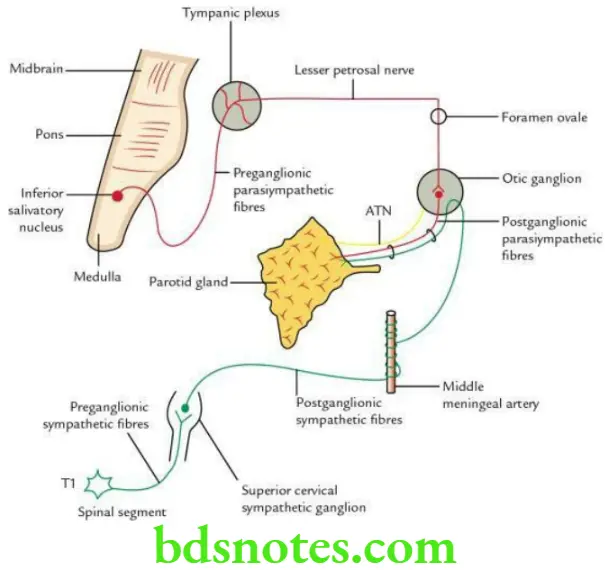
Secretomotor (parasympathetic): Preganglionic fibres arising from the inferior salivatory nucleus and travel to the otic ganglion as follows:
Inferior salivatory nucleus → Glossopharyngeal nerve → Tympanic branch of glossopharyngeal nerve (Jacobson’s nerve) → Tympanic plexus → Lesser petrosal nerve → Relay in otic ganglion
Postganglionic fibres arise from otic ganglion and travel through an auriculotemporal nerve to supply the parotid gland.
Vasomotor (sympathetic):
- Preganglionic fibres arise from the T1 segment of the spinal cord and relay in the superior cervical sympathetic ganglion.
- Postganglionic fibres arise from the superior cervical sympathetic ganglion and run along the arteries (e.g. external carotid artery) to supply the gland.
Vasomotor Sensory:
- Auriculotemporal nerve
- Great auricular nerve
Vasomotor Applied anatomy
Mumps (viral parotitis): It is the inflammation of the parotid gland by the mumps virus. Mumps characteristically do not suppurate. In adults, the mumps may cause complications like orchitis in males, oophoritis in females and pancreatitis in both sexes.
Parotid swellings: These are very painful due to the unyielding nature of parotid fascia, which encloses the gland.
Parotid abscess: It is drained by a transverse incision in the parotid masseteric fascia to avoid injuries to the facial nerve (Hilton’s method).
Frey syndrome: It occurs due to the damage of branches of the auriculotemporal and great auricular nerves by penetrating wounds in the parotid region. During regeneration, secretomotor fibres of the auriculotemporal nerve join the fibres of the great auricular nerve.
As a result, the stimulation of the parotid gland causes stimulation of the great auricular nerve, which leads to sweating and redness (hyperaemia) in the area of distribution of the great auricular nerve (e.g. parotid region).
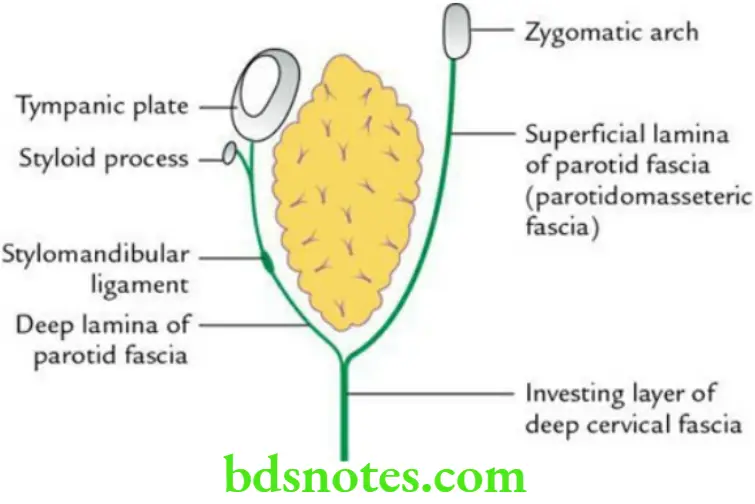
Question 4. Write a short note on the parotid capsule.
Answer.
It is a facial capsule that encloses the parotid gland. It is derived from the investing layer of the deep cervical fascia. At the lower end of the gland, the fascia splits into superficial and deep laminae to enclose the gland.
- The superficial lamina is extremely dense and tough and is attached to the lower border of the zygomatic arch. It blends with the perimysium of the masseter to form the parotid masseteric fascia.
- The deep lamina is relatively thin and is attached to the styloid process, tympanic plate and mandible. It also forms the stylomandibular ligament.
Question 5. Enumerate the structures present within the parotid gland.
Answer.
From superficial to deep, these are as follows:
- Deep parotid lymph nodes
- Facial nerve
- Retromandibular vein
- External carotid artery
Question 6. Write a short note on the parotid duct (Stensen’s duct).
Answer.
Parotid Duct General Features
- It is a 5-cm long and 3-mm wide tube.
- It emerges from the middle of the anterior border of the parotid gland and opens into the vestibule of the mouth opposite the crown of 2nd upper molar tooth on the parotid papilla.
Parotid Duct Course
- Runs forward over masseter muscle.
- Turns medially (1st bend) at the anterior border of the masseter and pierces buccal pad of fat, buccopharyngeal fascia and buccinator muscle in succession.
- Runs forward (2nd bend) between the buccinator and mucous membrane for some distance.
- Turns medially (3rd bend) to open on the summit of the parotid papilla to pour its secretions in the vestibule of mouth.
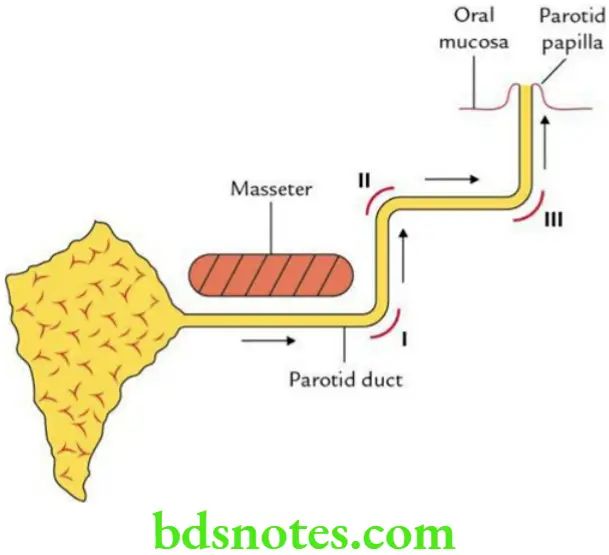
Parotid Duct Applied anatomy
- The parotid duct can be palpated and rolled on the firm anterior edge of the masseter.
- The sinuous course of the parotid duct serves as a valve-like mechanism to prevent the entry of infective agents in the duct from the mouth during violent blowing.
Question 7. Describe the development of the parotid gland in brief.
Answer.
- It develops as a furrow/groove arising from the ectodermal lining of the stomodeum between the mandibular and maxillary arches at the site of the future lateral angle of the mouth.
- The ectodermal groove is converted into a tube.
- The anterior part of the tube forms the parotid duct.
- The posterior part of the tube branches rapidly in the substance of the cheek and forms the parenchyma, i.e. glandular substance.
- Supporting tissue of the gland develops from surrounding mesenchyme.
Question 8. Describe the histological features of the parotid gland in brief.
Answer.
It is a compound tubuloalveolar gland and presents the following histological features.
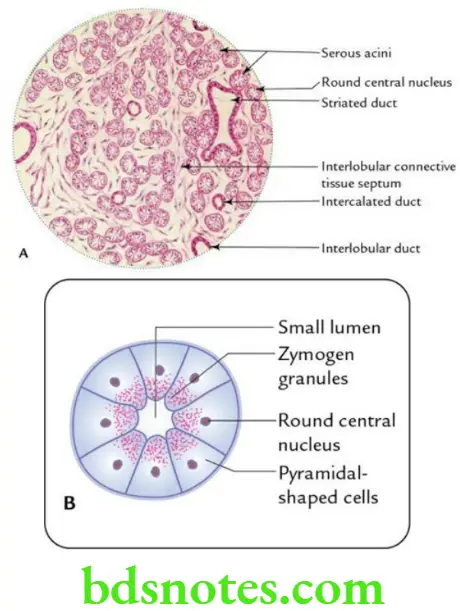
Connective tissue:
The connective tissue (fibrous) septa divide the gland into lobes and lobules.
Acini:
- Presence of a large number of serous acini.
- Acini are round and show biphasic stain with H&E stain, basophilic in basal part and eosinophilic in apical parts. They have very small lumen.
- Acini are lined by pyramidal cells with round nuclei placed near the centre.
Ducts:
- Intercalated ducts are lined by simple squamous epithelium.
- Striated ducts are lined by simple columnar epithelium with basal striations. They are stained dark with eosin.
- Interlobular ducts are present in connective tissue septa between the lobules and are lined by stratified cuboidal/low columnar epithelium.
Submandibular region
Question 1. Write a short note on the digastric muscle.
Answer.
- This muscle lies above the hyoid bone in the submandibular region.
- It has two bellies – anterior and posterior.
Digastric Muscle Origin
Anterior belly: It is unipennate and arises from the digastric fossa of the mandible.
Posterior belly: It is bipennate and arises from the mastoid notch of the occipital bone.
Insertion The two bellies meet to form an intermediate tendon, which is anchored by a fibrous pulley to the hyoid bone.
Nerve supply
Posterior belly: By facial nerve (nerve of the second arch)
Anterior belly: By mandibular nerve through nerve to mylohyoid (nerve of 1st arch)
Action It elevates the floor of the mouth and hyoid bone during the second phase of deglutition.
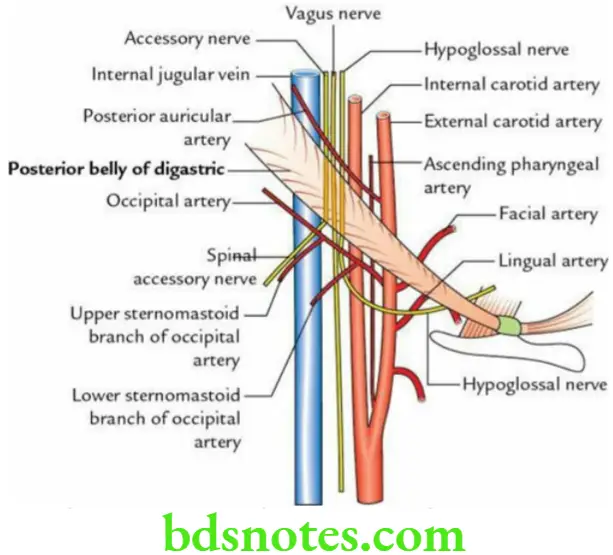
Question 2. List the relations of the posterior belly of the digastric muscle.
Answer.
Digastric Muscle Superficial relations
- Skin
- Superficial fascia
- Deep fascia
- Mastoid process
- Parotid gland
Digastric Muscle Deep relations
- Transverse process of atlas crossed superficially by spinal accessory nerve.
- Both the internal and external carotid arteries.
- Internal jugular vein.
- The Vagus nerve descends between the internal jugular vein and the internal carotid artery.
- Hypoglossal nerve.
- Along its upper border the posterior auricular branch of the external carotid artery and along its lower border the occipital branch of the external carotid artery pass upwards and laterally.
- Lingual and facial arteries.
Question 3. Describe the origin, insertion, nerve supply and actions of the hyoglossus muscle.
Answer.
It is the key muscle of the submandibular region.
Hyoglossus Muscle Origin From the greater cornu and lateral part of the body of the hyoid bone.
Hyoglossus Muscle Insertion Fibres run upwards and forward to be inserted into the side of the tongue. The styloglossus muscle interlaces at its insertion.
The Hyoglossus Muscle Nerve supply the Hypoglossal nerve (CN 7).
Hyoglossus Muscle Action Depresses the tongue to make its dorsum convex.
Question 4. Enumerate the relations of the hyoglossus muscle.
Answer.
Hyoglossus Muscle Superficial relations
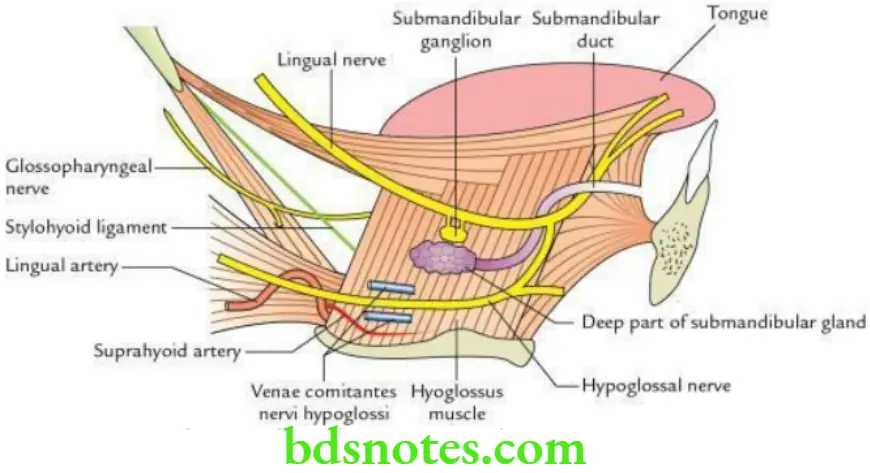
From above to downwards, these are as follows:
- Lingual nerve with the submandibular ganglion suspended from it.
- Deep part of the submandibular gland and submandibular duct.
- Hypoglossal nerve and its venae comitantes.
- Loop of communication between the lingual and the hypoglossal nerves.
- Styloglossus muscle.
Hyoglossus Muscle Deep relations
Two muscles: Middle constrictor and genioglossus
An artery: The lingual artery and its dorsal linguae branches
A nerve: Glossopharyngeal nerve
A ligament: Stylohyoid ligament
Question 7. Enumerate the structures passing deep to the posterior border of the hyoglossus.
Answer.
From above to downwards, these are as follows:
- Glossopharyngeal nerve (CN 9)
- Stylohyoid ligament
- Lingual artery
Question 8. Describe the submandibular gland under the following headings:
- Location and parts,
- External features,
- Relations,
- Nerve supply and
- Applied anatomy.
Answer.
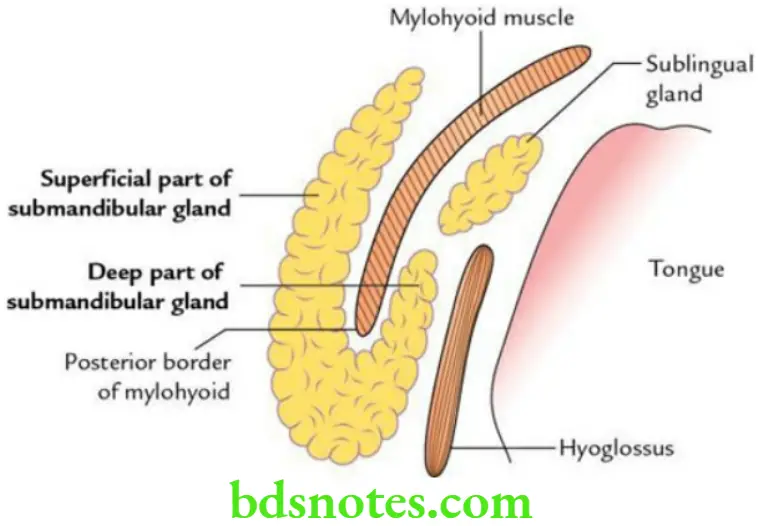
Submandibular Gland Location and Parts The submandibular gland lies in the digastric triangle. It is divided into two parts:
- Superficial
- Deep
The large, superficial part is located below the mylohyoid muscle and almost fills the digastric triangle.
The small, deep part is located above the mylohyoid muscle.
The two parts are continuous with each other around the free posterior margin of the mylohyoid muscle.
The gland is enclosed between the two layers of the investing layer of deep cervical fascia. The superficial layer covers the superficial surface of the gland and is attached to the base of the mandible. The deep layer covers the medial surface of the gland and is attached to the mylohyoid line of the mandible.
Superficial part of submandibular gland External features: It presents:
- Two ends: Anterior and posterior
- Three surfaces: Inferior, lateral and medial
Superficial part of submandibular gland Relations
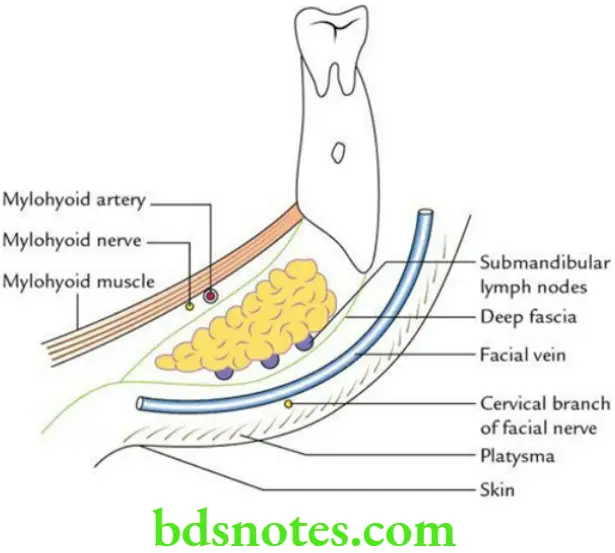
Superficial part of submandibular gland Inferior surface is related to:
- Skin
- Superficial fascia
- Platysma
- Deep fascia
- Common facial vein
- Cervical branch of the facial nerve
- Submandibular lymph nodes
Superficial part of submandibular gland Lateral surface is related to:
- Submandibular fossa of mandible
- Medial pterygoid muscle
- Facial artery
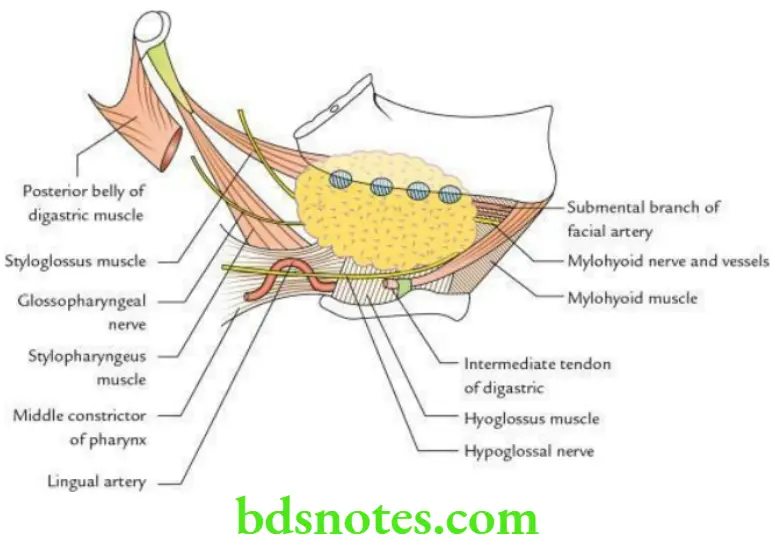
Superficial part of submandibular gland Medial surface: It is extensive and is divided into three parts: anterior, intermediate and posterior.
- Anterior part is related to:
- Mylohyoid muscle
- Mylohyoid nerve and vessels
- Submental artery (a branch of facial artery)
- The intermediate part is related to:
- Hyoglossus muscle
- Lingual nerve
- Submandibular ganglion
- Hypoglossal nerve
- Submandibular duct
- The posterior part is related to:
- Styloglossus muscle
- Stylopharyngeus muscle
- Middle constrictor of the pharynx
- Glossopharyngeal nerve
- Lingual artery
Deep part of the submandibular gland
- It is small and lies on the hyoglossus muscle.
- Posteriorly, it is continuous with a superficial part around the posterior border of the mylohyoid muscle.
- The submandibular duct emerges from its anterior end.
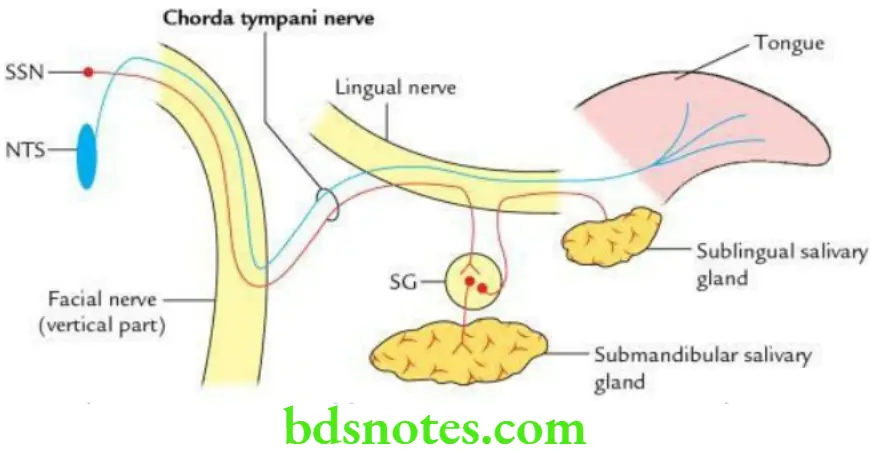
Nerve supply
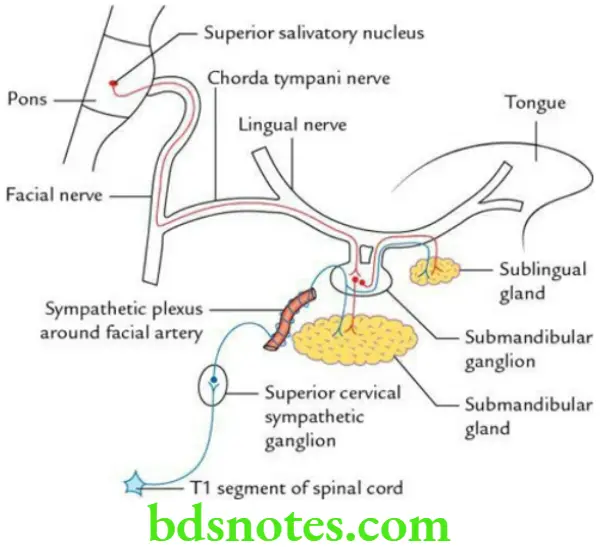
Secretomotor (parasympathetic):
- Preganglionic fibres arise from the superior salivatory nucleus and pass successively through the facial nerve, geniculate ganglion, chorda tympani and the lingual nerves to reach and relay in the submandibular ganglion.
- Postganglionic fibres arise from the submandibular ganglion and enter the submandibular gland to supply it.
Vasomotor (sympathetic):
- Preganglionic fibres arise from the T1 spinal segment and relay in the superior cervical sympathetic ganglion.
- Postganglionic fibres arise from the superior cervical sympathetic ganglion and run along the arteries to supply the gland. These fibres do not relay in the ganglion.
Sensory:
- Lingual nerve.
- Sensory fibres also do not relay in the ganglion.
Superficial part of submandibular gland Applied anatomy
- Formation of calculi is more common in the submandibular gland than in the parotid gland, because of (a) its secretion being more viscous and (b) the tortuous upward course of its duct (i.e. drainage occurs against gravity). This leads to stasis of secretion which leads to the formation of stone.
- To excise the submandibular gland, the skin incision is given at about 4 cm below the angle of the mandible to avoid injury to the marginal mandibular nerve.
- A stone in the submandibular duct can be palpated bimanually on the floor of the mouth and may even be seen if sufficiently large.
- Submandibular gland swelling can be palpated bimanually as it lies on both aspects of the oral diaphragm (i.e. mylohyoid muscle).
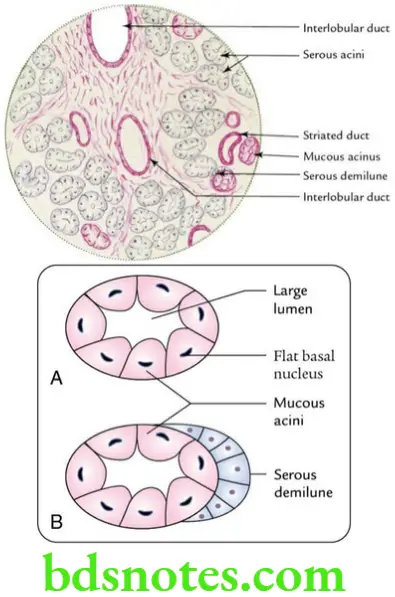
Question 9. Describe the histological features of the submandibular salivary gland in brief.
Answer.
The important histological features of the submandibular salivary gland:
- Presence of both serous and mucous acini.
- Mucous acini are made up of truncated columnar cells with flattened basal nuclei. They are stained light pink with H&E.
- Serous acini are described on p. 120. They stain basophilic in the basal part and pink in the apical part.
- Serous demilunes of Giannuzzi capping some of the mucous acini are seen.
- Moderately developed duct system.
Question 10. Write briefly about the sublingual gland.
Answer.
- It is a small, almond-shaped salivary gland located on the floor of the mouth on the mylohyoid muscle underneath the oral mucosa.
- It weighs about 3–4 g.
- About 15–20 ducts emerge from the gland (ducts of Rivinus) and open directly into the floor of the mouth on the sublingual fold.
- Its nerve supply is similar to that of the submandibular gland.
Sublingual Gland Applied Anatomy The cystic degeneration of the sublingual gland forms a swelling, which resembles the belly of a frog; hence, it is called a ranula.
Question 11. Write a short note on the submandibular ganglion.
Answer.
- The submandibular ganglion is a small parasympathetic ganglion lying on the hyoglossus muscle.
- Topographically, it is connected to the lingual nerve, whereas functionally it is connected to the facial nerve. (Note: The chorda tympani nerve is a branch of the facial nerve.)
Submandibular Ganglion Roots
Parasympathetic root:
- Preganglionic fibres arise from superior salivatory nucleus. These fibres then pass successively through nervus intermedius, facial nerve, chorda tympani and lingual nerves to relay in the ganglion.
- Postganglionic fibres arise from ganglion and supply submandibular and sublingual salivary glands.
Sympathetic root:
- Preganglionic fibres arise from the T1 spinal segment and relay in the superior cervical sympathetic ganglion.
- Postganglionic fibres arise from the superior cervical sympathetic ganglion, form a plexus around the external carotid artery, pass through the ganglion without relay, and supply the submandibular and sublingual glands.
Submandibular Ganglion Sensory:
- Lingual nerve.
- Sensory fibres also do not relay in the ganglion.
Question 12. Describe the chorda tympani nerve in brief.
Answer.
Chorda Tympani Nerve Origin The chorda tympani nerve is a branch of the facial nerve. It arises from the facial nerve at about 6 mm above the stylomastoid foramen.
Chorda Tympani Nerve Functional components
- General visceral ef event (GVE) fibres (i.e. postganglionic parasympathetic fibres), provide secretomotor supply to the submandibular and sublingual salivary glands.
- Special visceral af event (SVA) fibres, which carry taste sensations from the anterior two-thirds of the tongue, except from vallate papillae.
Chorda Tympani Nerve Course
Arises from the vertical part of the facial nerve → enters the middle ear through posterior canaliculus → runs across the lateral wall of middle ear → enters anterior canaliculus → enters infratemporal fossa through petrotympanic fissure → crosses medial aspect of spine of sphenoid → joins lingual nerve.
Chorda Tympani Nerve Applied anatomy The lesions of the chorda tympani nerve lead to:
- Decrease in the production of saliva
- Loss of taste sensations in the anterior two-third of the tongue

Leave a Reply