Oral Premalignant Lesions And Conditions Question And Answers
Question 1. Enumerate white lesions of oral cavity. Describe in detail etiology, signs and symptoms, diagnosis, differential diagnosis, treatment and prognosis of leukoplakia.
Or
Write a short note on leukoplakia
Or
Define leukoplakia. Write in detail about etiology, clinical features, investigations and its management.
Or
Write short note on management of leukoplakia.
Or
Write short note on clinical features of oral leukoplakia.
Or
Write short note on differential diagnosis of oral leukoplakia.
Answer.
White Lesions of Oral Cavity.
- Variation in structure and appearance of normal mucosa.
- Leukoedema.
- Fordyce’s granules.
- Linea alba.
- White lesion with definite precancerous potential
- Leukoplakia
- Erythroplakia
- Tobacco keratosis
- Carcinoma in situ
- Verrucous carcinoma
- Lichen planus
- Lichenoid reaction
- Oral submucous fibrosis (OSMF)
- Lupus erythematosus.
- White lesion without precancerous potential
- Traumatic keratosis
- Focal epithelial hyperplasia
- Psoriasis
- Geographic tongue
- White sponge nevus
- Stomatitis nicotina
- Intraoral skin grafts
- Hairy leukoplakia.
- Non-keratotic white lesion
- White hairy tongue
- Desquamative gingivitis
- Pemphigus
- Pemphigoid
- Diphtheria
- Syphilitic mucous patches.
- Acute necrotizing ulcerative gingivitis (ANUG)
- Koplik spot of measles
- Candidiasis
- Median rhomboid glossitis.
Read And Learn More: Oral Medicine Question And Answers
Leukoplakia Definition
Leukoplakia is defined as “a white patch or plaque that cannot be characterized clinically or pathologically as any other disease and is not associated with any physical or chemical causative agent except use of tobacco”. WHO, [First International Conference on oral Leukoplakia, Malmo, Sweden (1984)].
Leukoplakia Etiology
- Local Factors
- Tobacco: It is used by large number of people in various forms such as smoking of cigarette. Cigar, beedies and pipes. All these types of tobacco habits leads to development of leukoplakia. It is believed that during smoking large amount of tobacco end products are produced in oral cavity. These products in association with heat causes severe irritation to oral mucus membrane and finally result in development of leukoplakia.10 Mastering the BDS IVth Year-I (Last 25 Years Solved Questions)
- Alcohol: Many people who consume alcohol as well as use tobacco in some form develops leukoplakia.
- Sanguinaria: It is the herbal extract which is used in toothpaste and can cause true leukoplakia.
- Candidiasis: Chronic candidal infections are associated with leukoplakia.
- Systemic Factors
- Vitamin deficiency: Deficiency of vitamin A causes metaplasia and hyperkeratinization of epithelium which may result in development of leukoplakia.
- Syphilis: The syphilitic infections play minor role in causation of leukoplakia.
- Hormonal imbalance: Imbalance or dysfunction of both male and female sex hormones causes keratogenic changes in oral epithelium. These changes lead to the development of leukoplakia.
- Nutritional deficiency: Sideropenic anemia as well as some of the other nutritional deficiencies is some of the predisposing factors for occurrence of leukoplakia.
- Xerostomia: Some of the factors i.e. salivary gland diseases, anti – cholinergic drugs and radiation can lead to xerostomia can cause leukoplakia.
- Drug: Various anti – cholinergic, anti – metabolic drugs and systemically administered alcohol may lead to leukoplakia.
- Virus: Mainly, there are two types of viruses associated with leukoplakia i.e. herpes simplex and human papilloma virus. HPV associated antigen is demonstrated in cases of leukoplakia.
- Idiopathic Leukoplakia: In small proportion of cases, none of the underlying causes are seen. Such lesions are known as Idiopathic leukoplakia. Such lesions have high potential for malignant transformation.
Leukoplakia Signs and Symptoms/Clinical Features
-
- Leukoplakia remains asymptomatic and is discovered during routine oral examination.
- This is more common in older age group greater than 35 years and is usually more common in man.
- Most commonly and frequently affected sites are lips, vermilion border, buccal mucosa, tongue, hard palate and floor of the mouth.
- Lesions can vary in size, shape and distribution, borders can either be distinct or indistinct, smoothly contoured or ragged.
- Lesion is whitish or grayish or in some cases, it is brownish yellow in color due to heavy use of tobacco.
- In most of the cases, these lesion are asymptomatic, however, in some cases, they may cause pain, feeling of sickness and burning sensation, etc.
- Typical homogeneous leukoplakia is characterized by white, well demarcated plaque with identical reaction pattern throughout the lesion.
- Surface texture of the lesion vary from smooth thin surface to leathery appearance along with surface fissures which is referred to as cracked mud.
- Non-homogeneous type of leukoplakia or speckled leukoplakia can have white patches or plaque which is intermixed with red tissue elements.
- Verrucous or verruciform leukoplakia are the lesions in which white component is dominated by the papillary projections similar to oral papillomas. This type of leukoplakia is more aggressive.

Leukoplakia Investigations
Investigative procedures include the following:
- Cytobrush technique: This technique is more accurate than any other cytologic technique used in the oral cavity. The cytobrush technique uses a brush with firm bristles that obtains individual cells from the full thickness of the epithelium.
- Oral biopsy: When a suspicious lesion is identified, an incisional biopsy using a scalpel or a biopsy forceps is recommended. When the lesion is very small excisional biopsy is performed as an investigative procedure and as a treatment modality. In homogeneous leukoplakia, the value of histological examination to some extent is questioned. The occurrence of epithelial dysplasia is rather low in this type as is the risk of future malignant transformation.
- Markers of proliferation in leukoplakia: There are markers for determining future cancer development in premalignant lesions. These markers are divided into genomic markers and differentiation markers. The genomic markers include DNA aneuploidy, loss of heterozygosity and changes in expression of oncogene and tumor suppressor genes (p53), whereas the proliferative markers include keratins and carbohydrate antigens.
Leukoplakia Diagnosis
- Clinical: Any of the white patch in oral cavity along with the history of tobacco chewing which cannot be rubbed off is indicative of leukoplakia.
- Laboratory diagnosis: Biopsy is mandatory. On microscopic examination there is presence of either hyperorthokeratosis or parakeratosis along with epithelial dysplasia.
Leukoplakia Differential Diagnosis
- Lichen planus: Distinguished by frequent occurrence of multiple lesions and presence of Wickham’s striae.
- Syphilitic mucus patches: Features such as split papule are present.
- Discoid lupus erythematosus: Central atrophic area with small white dot and slightly elevated borders.
- Psoriasis: Auspitz’s sign is positive.
- Leukoedema: It occurs on buccal mucosa covering most of oral surface of cheek extending on labial mucosa.
- Hairy leukoplakia corrugated leukoplakic lesion: Occurring on lateral and ventral surface of tongue in patient with AIDS.
- Cheek-biting lesion: Careful history elicit cause and promote proper diagnosis.
- Cheek bite lesion: History tells about the cause and proper diagnosis.
- Electrogalvanic white lesion: It disappears when different metal restorations are replaced by composite restoration or GIC.
Leukoplakia Prognosis
- Prognosis is quite fair.
- Rate of regression is higher when tobacco habit is discontinued.
Leukoplakia Treatment
Removal of etiological factors may lead to the reversal or elimination of disease.
Leukoplakia Conservative Treatment
- Vitamin A therapy: Vitamin A is used as topical application after painting the lesion with podophyllin solution. Its therapeutic dosage is 75000 to 300000 IU. Treatment should be given for 3 months.
- Vitamin A along with Vitamin E is used to inhibit the metabolic degeneration.
- 13-cis-retinoic acid is given at high doses of 1.5 to 2 mg/kg body weight for the 3 months.
- Antioxidant therapy: β carotene supplementation is beneficial.
- Nystatin therapy: This is given in candidal leukoplakia. It is given in doses of 500000 IU two times a day.
- Vitamin B complex can be given as supplemental therapy.
Surgical Treatment
Leukoplakia Conventional Surgery
- Incision is made around the lesion including the safe margins.
- Incision is deep and wide.
- Affected area is undermined and is dissected from underlying tissue.
- Sliding mucosal flap should be prepared for covering the wound.
- Fine iris scissors and skin hook is used for decreasing trauma.
- Extensive undermining of mucosal flap should be carried out so that when flap is advanced into its position, amount of tension will be minimum.
- As mobilization of mucosal flap is completed, it is advanced and free edges are approximated by multiple interrupted silk sutures.
Leukoplakia Fulguration
It is a technique in which there is destruction of tissues by high voltage electric current and the action is controlled by movable electrode. This is done by electrocautery and electrosurgery.
Laser
Laser peel: It is used to remove the lesion which involves relatively large surface area.
Procedure
- Beam of laser is highly defocussed and should be kept at distant from the tissue.
- Initially, not any effect is seen on the tissue plane.
- Beam of laser should be gradually brought closer in focus, but remains in defocussed mode until tissue have white appearance and it begins to blister.
- Blistering usually occur at the basement membrane.
- The technique is extended over the rest of the lesion to be peeled.
- White area is then grafted with tissue forcep or hemostat.
Question 2. Enumerate precancerous lesion and describe oral lichen planus.
Or
Write short note on treatment of erosive lichen planus.
Or
Write short note on oral lichen planus.
Or
Write short answer on oral lichen planus.
Or
Write short answer on management of oral lichen planus.
Or
Write short note on clinical features of oral lichen planus.
Answer. Precancerous lesion is defined as “morphologically altered tissue in which cancer is most likely to occur than in its apparently normal counterpart”.
Precancerous Lesion
- Leukoplakia.
- Erythroplakia.
- Mucosal changes associated with smoking habits.
- Carcinoma in situ.
- Bowen disease.
- Actinic keratosis, cheilitis and elastosis.
Oral Lichen Planus
Lichen planus is the most frequently occurring precancerous condition.
It is a relatively common dermatological disorder occurring on skin and oral mucus membrane and refers to lace like pattern.
Lichen Planus Etiology
- Cell mediated immune response: This is associated with the lymphocyte-epidermal interactions which lead to degeneration of basal cell layer. This happens due to alteration of the keratinocytes because of unknown events which causes antigenic alterations of these cells which stimulates the immunological reaction.
- Autoimmunity: Activated T lymphocytes secrete gamma interferons which induce keratinocytes to produce HLA – DR and enhance the rate of differentiation by forming thick surface. Antigenic signals are transferred from Langerhans cells to the lymphocytes when there is mutual expression of HLA-DR. Normally lymphocytes get attracted towards HLA-DR expressing the keratinocytes and can contact the epithelial cell. At the time of this contact, improper epithelial antigenic signal is passed to lymphocytes because of HLA-DR linkage. As per this mechanism, self antigen can be recognized as foreign body which causes destruction of basal cells producing autoimmune response.
- Genetic: Lichen planus occur in families, twins and husband and wife. But it has also suggested that familial cause can be environmental and is related to infection as compared to genetics.
- Psychogenic factor: Patients having severe psychological stress such as a death of close friend or relative. Marital or sexual problems, carrier problems, loss of job and security and exam problems.
- Habits: Lichen planus is associated with tobacco habit. Tobacco and betel chewers have increased tendency of oral lichen planus.
- Miscellaneous: Oral lichen planus also occur due to deficiency of vitamin B1, B6 and C.
Lichen Planus Clinical Features
- It occurs in males from 35 to 44 years and in females from 45 to 54 years. More predilection is toward females.
- Common sites are buccal mucosa and to lesser extent tongue, lips, gingiva, floor of mouth and palate.
- Patient may report with burning sensation of oral mucosa.
- Oral lesion is characterized by radiating white and gray velvety thread-like papules in linear, angular and retiform arrangement.
- Wickham’s striae: Tiny white elevated dots are present on intersection of white lines called Wickham’s striae.
- Six P of lichen planus: P’s characterize lesions of lichen planus, i.e. they are planar, polygonal, purple, pruritic, papules and plaques.
- In some of the cases superimposed candidal infection is present.
- Reticular type: It is most common form and is bilateral. It shows Wickham’s striae.
- Papular: White elevated lesions are present which are 0.5 to 1mm in size and are seen over the keratinized areas of oral mucosa.
- Plaque: These are seen over dorsum of tongue and the buccal mucosa. If plaque is present on tongue, there is disappearance of papilla. Concentric peripheral growth is reported.
- Atrophic form: This is smooth, red, poorly defined area. In this attached gingiva is frequently affected. At the margins of atrophic zones, white keratotic striae are evident which radiate peripherally and bled in the surrounding mucosa.
- Bullous form: It consists of vesicles and bullae which are short lived. On ulceration they leave surface. It occurs on buccal mucosa and the posterior as well as lateral margins of tongue.
- Malignant transformation of oral lichen planus ranges from 0.4 to 12.3%. In India it is 0.4%.
Lichen Planus Diagnosis/Investigations
- Clinical diagnosis: Presence of interlacing white striae which can be seen bilaterally. Wickham’s striae and Koebner phenomenon is perfectly diagnostic.
- Laboratory diagnosis: Incisional biopsy of lesional area is done. When it is seen under microscope, it shows hyperorthokeratosis or hyperparakeratosis, acanthosis of spinal cell layer, saw tooth appearance of rete pegs, presence of liquefaction degeneration of basal cell layer of epithelium, juxta-epithelial band of inflammatory cell infiltrate, presence of civatte bodies and presence of MaxJoseph clefts.
- Immunofluorescent study: Direct immunofluorescent reaction is positive with IgA, IgM and IgG antisera. There is presence of subepithelial shaggy deposit of fibrinogen at basement membrane zone.
Lichen Planus Differential Diagnosis
- Leukoplakia: Men are more commonly affected in leukoplakia. Wickham’s striae are not present.
- Candidiasis: Pseudomembrane is rubbed off.
- Pemphigus: Clinical white striation of lichen planus is evident in cases.
- Lupus erythematosus: Fleeky and feathery appearance of lupus lesion.
- White sponge nevus: It is seen at birth and puberty. Lichen planus is seen over age of 30 years.
- Geographic tongue: Presence of redness in the centre with slightly raised margins which can change their shape.
- Lichenoid drug reaction: Systemic corticosteroids should be given for 2 weeks, if there is no improvement lichenoid reaction is the diagnosis.
Lichen Planus Management
- There is no known cure for oral lichen planus. So the management of symptoms guides the therapeutic approaches.
- Systemic and oral corticosteroids have been the most predictable and successful medications for controlling signs and symptoms associated with lichen planus.
- Topical medications consisting of high-potency corticosteroids, i.e. 0.05% fluocinonide, 0.05% clobetasol and triamcinolone acetonide 0.1 %. Various oral suspension of triamcinolone, high-potency steroid mouthwashes such as betamethasone valerate 0.1%, fluocinolone acetonide 0.1% and clobetasol propionate 0.05% have been used effectively.
- Extensive-erosive lesions of oral lichen planus on gingiva, i.e. desquamative gingivitis may be treated effectively by using occlusive splints as carriers for the topical steroid.
- Topical or systemic anti – fungal should be given to the patient as there is fungal overgrowth present when patient is on steroid therapy.
- Systemic steroids are only indicated for brief treatment of severe exacerbations or for short periods of treatment of recalcitrant cases which fail to respond to the topical steroids.
- Under systemic administration of corticosteroids, prednisone tablets may be given with dosages varying between 40 and 80 mg daily for less than l0 days without tapering. Dosage regimens are determined individually, based on the patient’s medical status, severity of disease and previous treatment responses.
- In patients whom underlying systemic problems are present consultation with the patient’s primary care physician should be done.
- Retinoids are useful, usually in conjunction with topical corticosteroids as adjunctive therapy for oral lichen planus.
- Systemic and topically administered B all-transretinoic acid, vitamin A acid, systemic etretinate, and systemic and topical isotretinoin are all effective, and topical application of a retinoid cream or gel will eliminate reticular and plaque-like lesions in many patients. But following withdrawal of the medication, the majority of lesions recur.
- A new systemically administered retinoid, temarotene, is effective in oral lichen planus and is free of side-effects other than a slight increase in liver enzymes.
- Various other topical and systemic therapies reported to be useful are dapsone, doxycycline and antimalarials which should need additional research.
- Topical application of cyclosporine is helpful in managing recalcitrant extensive and otherwise intractable oral lesions of oral lichen planus. Systemic cyclosporine should also be administered, i.e. 8 mg/kg/day for 8 weeks.
- When there is presence of lesions confined to the mucosa just opposite to amalgam restorations or other metals, complete removal of the amalgam restorations has been curative in most patients.
- Surgical excision is carried out in oral lichen planus cases in whom concomitant dysplasia is present.
Question 3. Enumerate white lesions of oral cavity. Discuss in detail the etiology, clinical picture and management of lichen planus.
Answer. For white lesions of oral cavity refer to Ans l of the same chapter.
For etiology, clinical picture and management of lichen planus refer to Ans 2 of the same chapter.
Question 4. Write short note on clinical features with emphasis on oral manifestations and diagnosis of systemic lupus erythematosus.
Answer. Systemic lupus erythematosus is a premalignant condition.
It is characterized by presence of abnormal antibodies and immune complex.
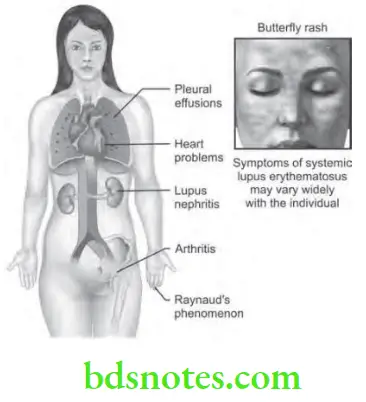
lupus erythematosus Clinical Features
- It occurs in 3rd and 4th decades of life. It has female predilection with ratio of 5:1.
- This is characterized by repeated remissions as well as exacerbations with common sites such as face, neck, upper arm, shoulders and fingers.
- Patient complaints of fever and pain in muscles and joints. Burning or itching can be present along with the area of hyperpigmentation.
- Skin lesions shows erythematous patches over the face, which coalesce to form roughly symmetrical pattern over the cheeks and across bridge of nose which is known as butterfly distribution.
- Lesions are widespread and show the signs of acute inflammation.
- Kidney shows the fibrinoid thickening of glomerular capillaries which produces characteristic wire loop, which causes renal insufficiency.
- Endocarditis can occur in heart, there is also fibrinoid degeneration of epicardium and the myocardium.
lupus erythematosus Oral Manifestations
- Most common site are buccal mucosa, lip and palate.
- Patient complains of burning sensation, xerostomia or soreness of mouth.
- There is presence of hyperemia, edema and pronounced extension of lesion with greater tendency to bleed and petechiae.
- Lip lesions appear with central atrophic area with small white dots surrounded by keratinzed border, which is composed of small radiating white striae.
- Intraoral lesion is composed of central depressed red atrophic area surrounded by 2 to 4 mm elevated keratotic zone, that dissolve in small white lines.
lupus erythematosus Diagnosis
- Clinical diagnosis: Skin lesion or the oral lesion which is atropic and erythematous is suspective of lupus erythematosus. Both oral and the nasopharyngeal ulceration form the major diagnostic criteria for systemic lupus erythematosus.
- Laboratory diagnosis:
- LE inclusion phenomenon with surrounding pale nuclear mass apparently devoid of lymphocytes.
- Anemia, leukopenia and thrombocytopenia, with sedimentation rate increased.
- Serum gamma globulin increased and Coombs test is positive.
- Positive lupus band test: This shows deposition of IgG, IgM or complement component in skin.
Question 5. Describe in detail oral leukoplakia and also differentiate it with oral lichen planus.
Answer. For oral leukoplakia refer to Ans 1 of the same chapter.

Question 6. Discuss differential diagnosis and management of oral lichen planus and leukoplakia.
Answer. For differential diagnosis and management of oral lichen planus refer to Ans 2 of the same chapter.
For differential diagnosis and management of leukoplakia refer to Ans 1 of the same chapter.
Question 7. Write short note on candidal leukoplakia.
Answer. It is also known as chronic hyperplastic candidiasis. Candida albicans is mostly associated with the nodular leukoplakia.
candidal leukoplakia Pathogenesis
- Various etiological factors such as cigarette smoking, denture wearing are associated with the pathogenesis of candidal leukoplakia.
- Tobacco smoking leads to immune defect due to decrease in salivary immunoglobulin-A concentration or PMN leukocyte function while denture wearing causes oral mucosal keratosis, they both lead to oral candidiasis associated with nodular leukoplakia.
candidal leukoplakia Clinical Features
- It is most common in men which are of middle age and are heavy smokers
- Most common sites are tongue, lip and cheeks.
- There is presence of firm and white leathery plaques.
- Lesion is whitish in color, borders are vague. It does not rub while applying lateral pressure.
candidal leukoplakia Differential Diagnosis
- Lichen planus: Wickham’s striae are seen as well as at times involvement of skin is evident.
- Bacterial infection: Microbiological tests should be carried out to confirm the diagnosis.
- Hairy leukoplakia: It does not resolve while taking anti fungal drugs.
candidal leukoplakia Treatment
- Cigarette smoking should be stopped.
- Denture should be replaced.
- Antifungal therapy is given. Drugs such as nystatin, ketoconazole and fluconazole are effective.
Question 8. Enumerate premalignant lesions of oral cavity. Describe clinical features, etiopathogenesis, treatment and differential diagnosis of lichen planus.
Answer.
Lichen Planus Premalignant Lesions
- Leukoplakia
- Erythroplakia
- Mucosal changes associated with smoking habits
- Carcinoma in situ
- Bowen disease
- Actinic keratosis, Actinic chelitis and Actinic elastosis.
For clinical features, treatment and differential diagnosis of lichen planus refer to Ans 2 of same chapter.
Lichen Planus Etiopathogenesis
Oral lichen planus is a T-cell-mediated autoimmune disease in which cytotoxic CD8 + T cells trigger the apoptosis of oral epithelial cells. The CD8 + lesional T- cells may recognize the antigen associated with major histocompatibility complex (MHC) class I on keratinocytes. After antigen recognition and activation, CD8 + cytotoxic T-cells may trigger keratinocyte apoptosis. Activated CD8+ T-cells may release cytokines that attract additional lymphocytes.
As per the recent studies in psychoneuroimmunology psycosomatic stress results in the autoimmunity reactions and this leads to lichen planus.
Question 9. Define premalignant lesion and premalignant condition with examples. Describe in detail clinical features, differential diagnosis and management of leukoplakia.
Answer. Premalignant lesion is defined as a morphologically altered tissue in which cancer is more likely to occur than its apparently normal counterparts. WHO (1972) For example,
- Leukoplakia
- Erythroplakia
- Mucosal changes associated with smoking habits
- Carcinoma in situ
- Bowen disease
- Actinic keratosis, actinic cheilitis and actinic elastosis
Premalignant condition is defined as a “generalized state or condition associated with significantly increased risk for cancer development.” For example,
- Syphilis
- OSMF
- Oral lichen planus
- Sideropenic dysplasia
- Dyskeratosis congenita
- Lupus erythematosus.
Question 10. Write short note on classifications and treatment of leukoplakia.
Answer.
Leukoplakia Classification
Based on Clinical Description
- Homogeneous
- Flat
- Corrugated
- Pumice like
- Wrinkled.
- Non-Homogeneous
- Nodular or speckled
- Verrucous
- Ulcerated
- Erythroleukoplakia.
Based on Etiology
- Tobacco induced
- Non-tobacco induced.
Based on Risk of Future Development of Oral Cancer
- High-risk sites
- Floor of mouth
- Lateral or ventral surface of tongue
- Soft palate.
- Low-risk sites
- Dorsum of tongue
- Hard palate.
- Intermediate Group
All other sites or oral mucosa.
Based on Histology
- Dysplastic
- Non-dysplastic.
Based on Extent
- Localized
- Diffuse.
Classification Given by Benoczy
- Leukoplakia simplex
- Leukoplakia erosive
- Leukoplakia verrucosa.
Question 11. Write short note on clinical features and treatment of OSMF.
Or
Write short note on submucous fibrosis.
or
Write short note on management of OSMF
Or
Write short note on OSMF.
Or
Write short note on management of OSMF.
Or
Write long answer on etiology, clinical features and management of oral submucous fibrosis
Answer. OSMF is defined as “An insidious chronic disease affecting any part of oral cavity and sometime pharynx. Although occasionally preceded by and/or associated with vesicle formation, it is always associated with juxtaepithelial inflammatory reaction followed by fibroelastic changes in lamina propria, with epithelial atrophy leading to stiffness of oral mucosa and causing trismus and inability to eat.”
Submucous fibrosis Etiology
- Chillies: Red chillies are the most important components. Capsaicin is the active ingredient of chilli which is the vanillylamide of 8-methyl-6-nonenoic acid which is the active irritant of chilli.
- Tobacco: It act as local irritant.
- Lime: This is used along with the betel nut. It leads to local irritation and causes damage to oral mucosa.
- Areca nut: It consists of different types of alkaloids such as arecoline, arecadine, arecalidine, guvacoline, guvacine and isoguvacine which lead to OSMF.
- Nutritional deficiency: It is characterized by deficiency of vitamin B complex which leads to repeated vesiculations and ulcerations.
- Collagen disorders: OSMF is thought to be the localized collagen disorder of oral mucosa. It is associated with scleroderma, rheumatoid arthritis and intestinal fibrosis.
- Immunological disorders: Serum immunoglobulin levels of IgA, IgG and IgM get raised in OSMF. It is suggestive of an antigenic stimulus even when infection is absent. Circulating auto – antibodies are seen in some of the cases of OSMF.
- Genetic susceptibility: Familial occurrence of OSMF is also reported.
Submucous fibrosis Clinical Features
- It occurs during 20 to 40 years of age.
- Most commonly involved sites are buccal mucosa, retromolar area, uvula, soft palate, palatal fauces, tongue, lips, pharynx and esophagus.
- Onset of disease is insidious or develop over the period of 2 to 4 years.
- Initially, the patient complains of burning sensation in the mouth, particularly during taking hot and spicy foods.
- It is often accompanied or followed by the formation of multiple vesicles over the palate or ulcers or inflammatory reactions in other parts of oral mucosa.
- There can be either excessive salivation or decreased salivation (xerostomia) along with recurrent stomatitis. Patients also develop defective gustatory sensation.
- In the initial phases of the disease, palpation of the mucosa elicits a “wet-leathery” feeling.
- Petechial spots may also be seen in the early stages of the disease over the mucosal surfaces of tongue, lips and cheek, etc.
- Oral mucous membrane is very painful upon palpation at this stage.
- One of the most important characteristic features of oral submucous fibrosis is the gradual stiffening of the oral mucosa with progressive reduction in the mouth opening.
- The stiffness of the oral mucosa and the subsequent trismus develops gradually within a few years after the development of the initial symptoms.
- In the advanced stage of OSMF, the oral mucosa losses its resiliency to a great extent and it becomes blanched and stiff. Severe trismus develops at this stage.
- Because of stiffness of the lips and the tongue patients are unable to blow whistles or even blow out a candle.
- Oral mucosa is symmetrically affected on both sides of the mouth and it shows extreme pallor.
- Oral submucous fibrosis often causes a blanched opaque (white marble-like) appearance of the mucosa, on which, there may be occasional presence of leukoplakia or erythroplakic patches.
- Palpation of the mucosa often reveals many vertical white fibrous bands on the inner aspect of the cheek.
- Patients of OSMF often develops difficulty in deglutition, referred pain in the ear or deafness and nasal intonation of voice.
- Depapillation of the tongue with recurrent or sometimes persistent glossitis occurs. Later on the tongue becomes stiff and shows restricted movements.
- Uvula become ’bud-like” or hockey-stick shaped or become shrunken.
Submucous fibrosis Treatment
Stop the areca nut and tobacco chewing stricitly.
Submucous fibrosis Supportive Treatment
- Diet rich with the vitamins along with iron preparation should be given to the patient.
- IM injection of Iodine B complex is given to the patient. During early phase low doses are given and later on high doses are effective.
- Local injection of hydrocortisone in the lesional area is of value.
- Intralesional injection of hyalurodinase can be given.
- Systemically 100 mg/day of hydrocortisone is effective in reducing the burning sensation.
- 2 mL injection of placentrex intra lesional is effective.
- Lycopene as an antioxidant should be given to the patient.
- Vitamin E along with hyalurodinase and dexamethasone is effective.
- Intralesional injection of interferon-gamma helps in increment in mouth opening.
Submucous fibrosis Surgical Treatment
Conventional Surgery:
- Tongue mucosa as a graft: Fibrous bands are excisioned and tongue mucosa as a flap is used.
- Implantation of fresh human placenta can be done.
- Fibrotic bands are excisioned and nasolabial flap is taken for reconstruction.
- Bilateral palatal flap is taken for generally covering exposed area.
Laser: Patient should be incorporated with general anesthesia. CO2 LASER incise the buccal mucosa and vaporizes mucosal connective tissue.
Cryosurgery: It helps in providing the relief from the local lesions.
Oral Physiotherapy
Various oral exercises should be advised in early and moderately advanced cases.
Diathermy
Microwave diathermy is effective in early and moderate lesions.
Question 12. Classify red and white lesions of oral cavity. Describe etiology, clinical features and treatment plan of oral submucous fibrosis.
Answer.
Etiologic Classification of Red and White Lesions of Oral Cavity
- Normal mucosal variations:
- Leukoedema
- Fordyce’s granule
- Linea alba buccalis
- Genetically linked white keratotic lesions:
- Oral genodermatoses
- White sponge nevus
- Hereditary benign intraepithelial dyskeratosis
- Pachyonychia congenita
- Post inflammatory white lesions
- Traumatic keratosis
- Mechanical trauma
- Thermal burn
- Chemical burn (aspirin burn, uremic stomatitis)
- Radiation mucositis
- Reactive mucosal hyperplasia (stomatitis nicotina palati)
- White and red lesions due to infections:
- Syphilis
- Measles (Koplik’s spots)
- Candidiasis
- Bacterial stomatitis
- Premalignant Lesions:
- Leukoplakia
- Lichen planus
- Lichenoid reactions-drug induced, graft versus host disease
- Erythroplakia
- Actinic keratoses
- Discoid lupus erythematosus
- Chronic hyperplastic candidiasis
- Premalignant conditions:
- Oral submucous fibrosis
- Oral psoriasiform
- Dyskeratosis congenita
- Sideropenic dysphagia
- Syphilitic glossitis
- Miscellaneous:
Question 13. Write short note on types of oral lichen planus.
Answer. Following are the various types of lichen planus:
Oral Lichen Planus Reticular
- This is the most common form of lichen planus.
- Characteristically, it presents as a series of line, radiant, white striae known as ‘Wickham’s striae’, which may be surrounded by a discrete erythematous border.
- Buccal mucosa is the site most commonly involved.
- Striae are typically bilateral in a symmetrical form on the buccal mucosa.
- They may also be seen on the lateral border of tongue and less often on the gingiva and the lips.
- Reticular lichen planus is likely to resolve in 4l% of cases.
Oral Lichen Planus Papular
- This form presents as small white pinpoint papules about 0.5 mm in size.
- It is rarely seen and being small, it is possible to overlook them during a routine oral examination.
Oral Lichen Planus Plaque
- Lesion resembles oral leukoplakia and occurs as homogeneous white patches.
- Plaque-like form may range from a slightly elevated and smooth to a slightly irregular form and may be multifocal.
- Primary sites are over the dorsum of the tongue and buccal mucosa.
- Plaque-like oral lichen planus resolves in only 7% of cases.
- This form is significantly more common among tobacco smokers.
Oral Lichen Planus Atrophic
- Atrophic type is diffuse, red and there are usually white striae at the lesional area.
- Such striae that radiate peripherally are usually evident at the margins of the atrophic zones of the lesion.
- Attached gingiva is often involved and the condition is commonly referred to as `chronic desquamative gingivitis’.
- Lingual gingiva is usually less severely involved.
- This condition can cause a burning sensation particularly when in contact with certain foods.
- About12% of the atrophic lesions will resolve spontaneously.
Oral Lichen Planus Bullous
- Appear as small bullae or vesicles that tend to rupture easily.
- Bullae or vesicles range from a few millimeters to several centimeters in diameter.
- When they rupture they leave an ulcerated, painful surface.
- This form is rarer than the other forms of oral lichen planus.
- Bullous form is commonly seen on the buccal mucosa, particularly in the posteroinferior areas adjacent to the second or third molar teeth. The next most common site is the lateral margin of the tongue.
- The lesions are rarely seen on the gingiva or inner aspect of the lips.
Oral Lichen Planus Erosive
- This is the second most common type.
- Lesions are usually irregular in shape and covered with a fibrinous plaque or pseudomembrane where there is an erosion.
- Periphery of the lesion is usually surrounded by reticular or finely radiating keratotic striae.
- It is painful when the pseudomembrane or fibrinous plaque is removed.
- It is thought that the erosive oral lichen planus has a greater potential to undergo malignant change.
Question 14. Define leukoplakia. Describe clinical features, investigations and treatment of homogeneous leukoplakia.
Answer. Leukoplakia is defined as “a white patch or plaque that cannot be characterized clinically or pathologically as any other disease and is not associated with any physical or chemical causative agent except use of tobacco”. [WHO First International Conference on oral Leukoplakia, Malmo, Sweden (1984)] (Axell et al. 1984).
Homogeneous Leukoplakia Clinical Features
- It occurs during 3rd and 4th decade of life.
- Males are affected more commonly as compared to females.
- Homogeneous leukoplakia is an extensive white patch, which is consistent throughout.
- Surface of the lesion is corrugated or presence of pattern of fine white lines or wrinkled area.
- Lesion is usually whitish in color. Color can be yellowish white or yellow.
- Margins of lesion are irregular.
Homogeneous Leukoplakia Investigations
Investigative procedures includes the following:
- Cytobrush technique: This technique is more accurate than any other cytologic technique used in the oral cavity. The cytobrush technique uses a brush with firm bristles that obtains individual cells from the full thickness of the epithelium.
- Oral biopsy: When a suspicious lesion is identified, an incisional biopsy using a scalpel or a biopsy forceps is recommended. When the lesion is very small excisional biopsy is performed as an investigative procedure and as a treatment modality. In homogeneous leukoplakia, the value of histological examination to some extent is questioned. The occurrence of epithelial dysplasia is rather low in this type as is the risk of future malignant transformation.
- Markers of proliferation in leukoplakia: There are markers for determining future cancer development in premalignant lesions. These markers are divided into genomic markers and differentiation markers. The genomic markers include DNA aneuploidy, loss of heterozygosity and changes in expression of oncogene and tumor suppressor genes (p53), whereas the proliferative markers include keratins and carbohydrate antigens.
Homogeneous Leukoplakia Treatment
Removal of etiological factors may lead to the reversal or elimination of disease.
Conservative Treatment
- Vitamin therapy is given to patient. Vitamin A should be given to apply topically.
- Along with vitamin A, vitamin E should be given this leads to inhibit metabolic degeneration.
- Nystatin therapy is given to eliminate candidal infection.
- Vitamin B complex can be given as supplemental therapy.
Homogeneous Leukoplakia Surgical Treatment
Conventional Surgery:
- Incision is made around the lesion including the safe margins.
- Incision is deep and wide.
- Affected area is undermined and is dissected from underlying tissue.
- Sliding mucosal flap should be prepared for covering the wound.
- Fine iris scissors and skin hook is used for decreasing trauma.
- Extensive undermining of mucosal flap should be carried out so that when flap is advanced into its position, amount of tension will be minimum.
- As mobilization of mucosal flap is completed, it is advanced and free edges are approximated by multiple interrupted silk sutures.
Fulguration: It is a technique in which there is destruction of tissues by high voltage electric current and the action is controlled by movable electrode. This is done by electrocautery and electrosurgery.
Laser
Laser peel: It is used to remove the lesion which involves relatively large surface area.
Procedure
- Beam of laser is highly defocussed and should be kept at distant from the tissue.
- Initially, not any effect is seen on the tissue plane.
- Beam of laser should be gradually brought closer in focus, but remains in defocussed mode until tissue have white appearance and it begins to blister.
- Blistering usually occur at the basement membrane.
- The technique is extended over the rest of the lesion to be peeled.
- White area is then grafted with tissue forcep or hemostat.
Question 15. Describe in detail differential diagnosis of white patch on palate.
Answer. Following is the differential diagnosis of white patch on the palate:
white patch on palate Chemical Burn
- Acute painful lesion is present.
- Shape of the lesion is irregular with white pseudomembrane covering the lesion.
- While applying the lateral pressure white membrane get removed and leaves painful red area.
white patch on palate Candidiasis
- Presence of white patches which when removed by a normal guaze leaves erythematous area.
- Presence of rapid onset of bad taste.
- There should be presence of burning sensation.
- Lesion appears as curdled milk.
white patch on palate Lichen Planus
- Patient complaints of burning sensation
- There is presence of lacy or reticular pattern as well as rings over the palate.
- At white lines tiny elevated white dots are present at the intersection of these white lines which are known as Wickham’s striae.
- It is bilateral in presentation.
white patch on palate Leukoplakia
- Presence of white plaque-like areas which are present in groups or can occur solitary.
- Margins of the lesions are irregular.
- It cannot be wiped off by the guaze.
- Lesion is asymptomatic.
white patch on palate Frictional Keratosis
- It is caused due to chronic friction.
- Condition is reversible on removing the cause.
white patch on palate Smoker’s Keratosis
- Caused due to chronic tobacco smoking.
- Patient remains asymptomatic.
- Palatal mucosa becomes white with tiny elevated red dots.
- Condition is reversible on cessation of smoking.
white patch on palate Verrucous Carcinoma
- Affected area shows white papillary or pebbly surface.
- Surface is covered by leukoplakic film. Surface also consists of rugae-like folds along with deep clefts.
- Lesion is broad with slight elevation above the mucosa.
- Lesion consists of well-defined margins.
Question 16. Classify red and white lesions of the oral cavity. Describe the etiology, clinical features and treatment plan of oral lichen planus.
Or
Classify red and white lesions and discuss the etiology, clinical features, investigations and management of lichen planus.
Answer. For classification of red and white lesions of oral cavity refer to Ans 12 of same chapter.
For etiology, clinical features, investigations and treatment plan of oral lichen planus refer to Ans 2 of same chapter.
Question 17. Classify red and white lesions of the oral mucosa. Describe etiopathogenesis, clinical features and treatment of oral lichen planus.
Answer. For classification of red and white lesions of oral cavity refer to Ans 12 of same chapter.
For etiopathogenesis refer to Ans 8 of same chapter.
For clinical features and treatment of oral lichen planus refer to Ans 2 of same chapter.
Question 18. Enumerate white lesions of the oral cavity. Define OSMF and describe etiology, clinical features and treatment of oral submucous fibrosis.
Or
Classify white lesions of oral cavity. Describe in detail about the etiology, pathogenesis, clinical features and management of OSMF.
Answer. For enumeration of white lesions refer to Ans 1 of same chapter.
For definition, clinical features, etiology and treatment of oral submucus fibrosis refer to Ans 11 of same chapter.
Pathogenesis/Etiopathogenesis of OSMF
Basically pathogenesis of OSMF consists of disturbance in collagen metabolism via TGF-β. The whole procedure is described as:
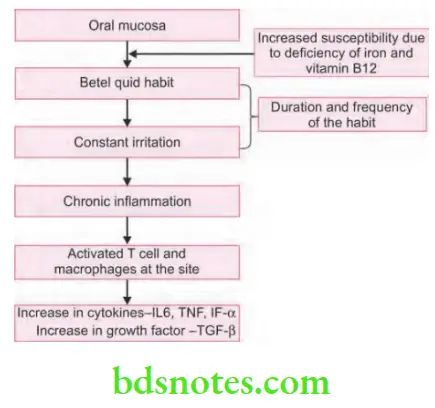
Initial Event of Disease Process
According to P. Rajalitha, S.Vali (2005) initial event of the disease process is, oral mucosa which is in direct contact with betel quid (tobacco + areca nut + slaked lime + catechu and condiments) because of the habit which is the means of constant irritation. Major areca nut alkaloids are arecoline, arecaidine, arecolidine, guyacoline and guacine. Out of all these arecoline is most abundant. These alkaloids undergo nitrosation and give rise to N-nitrosamines which have cytotoxic effects on cells. Important flavonoid components of areca nut are tannins and catechins. So all these alkaloids, flavonoids and microtrauma produced by friction of coarse fibers of areca nut leads to chronic inflammatory process which is characterized by presence of inflammatory cells i.e. T cells and macrophages, these cells release and/or stimulate synthesis of various cytokines and growth factors. Increased susceptibility among individuals who are anemic due to iron or vitamin B12 deficiencies. It is because of increased fragility of mucosa by which there is more betel quid absorption.
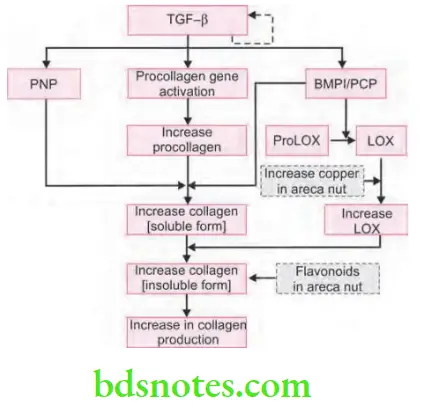
Collagen Production Pathway as Regulated by TGF-β
Transforming growth factor-β (TGF-β) is a growth factor which regulate the collagen production pathway, it has autocrine activity. TGF-β activate procollagen genes which lead to production of more procollagen. TGF-β also increases secretion of procollagen C-proteinase (PCP) and procollagen N-proteinase (PNP) both of these are needed for conversion of procollagen to collagen fibrils. In oral submucous fibrosis, there is increase in cross linking of collagen which results to increase in insoluble form. This is facilitated by increase activity and production of key enzyme lysyl oxidase (LOX). PCP and bone morphogenetic protein1 and increased copper in betel quid stimulate the activity of LOX which produces increase collagen which is insoluble. Flavonoids increases the cross linking of collagen fibers. These all steps lead to increase in collagen production. TGF-β strongly promote the expression of LOX both at mRNA and protein levels in various cell lines. LOX activity is important in formation of insoluble collagen due to cross linking. Process of cross linking provides tensile strength and mechanical properties to fibers as well as makes collagen fibers resistant to proteolysis.
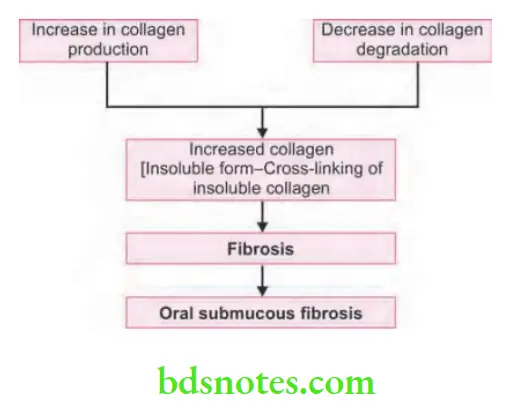
Collagen Degradation Pathway as Regulated by TGF-β

There are also two main events modulated by TGF-β which also decreases collagen degradation i.e. activation of tissue inhibitor of matrix metalloproteinase gene (TIMPs) and activation of plasminogen activator inhibitor (PAI) gene.
Collagen degradation pathway as regulated by TGF-β activate genes for TIMPs and so more TIMP is formed. Now this inhibit activated collagenase enzyme which is necessary for degradation of collagen. It also activate gene for PAI which is the inhibitor of plasminogen activator, so there is no plasmin formation. Plasmin is needed for the conversion of procollagenase to active form of collagenase and absence of plasmin lead to absence of active collagenase. Flavonoids inhibit collagenase activity. Reduction in activity and levels of collagenase result in decrease in collagen degradation.
Overall Effect of TGF-β Pathway
So, overall effect of activated TGF-β pathway is that there is an increase in collagen production and cross-linking (insoluble form) along with decrease in collagen degradation. This produces an increased collagen deposition in subepithelial connective tissue layer of oral mucosa causing oral submucous fibrosis.
Question 19. Enumerate precancerous lesions. Write in detail about OSMF.
Answer. Enumeration of precancerous lesions
Leukoplakia
Erythroplakia
Mucosal changes associated with smoking habits
Carcinoma in situ
Bowen’s disease
Actinic keratosis, cheilitis and elastosis.

Leave a Reply