Oral Pathology Glossary
Abfraction:
Loss of tooth surface at the cervical areas of teeth caused by tensile and compressive forces during tooth flexure; cervical erosive lesions that cannot be attributed to any particular cause.
Abrasion:
Abnormal loss of tooth structure due to non-masticatory physical friction.
Abscess:
A localized acumulation of pus caused by an infection.
Acantholysis:
Dissolution of the intercellular bridges of the prickle cell layer of the epithelium.
Acanthosis:
Excessive thickening of the intermediate cell layer resulting in broadening and elongation of the rete pegs.
Acquired disturbances:
Disturbances in the structure of enamel can occur as a result of environmental or hereditary factors.
Acral lentiginous melanoma:
A melanoma that is a brown irregularly shaped macular lesion of the unexposed skin of the hands and feet that undergoes progression to nodular melanoma.
Acute pulpitis:
A hormonal disorder that results when the pituitary gland produces excess growth hormone (GH).
Addison’s disease:
Having severe symptoms and a short course.
Adenoid squamous cell carcinoma:
A rapidly destructive inflammatory process within bone that consists of granulation tissue, purulent exudate, and islands of non-vital bone (sequestra).
Adenomatoid odontogenic tumor (AOT):
A well-circumscribed lesion derived from odontogenic epithelium that usually occurs around the crowns of unerupted anterior teeth of young patients and consists of epithelium in swirls and ductal patterns interspersed with spherical calcifications.
Adenosquamous carcinoma:
Rare, aggressive carcinoma of the mucosa consisting of a mixture of malignant squamous and glandular cells.
Adult monostotic fibrous dysplasia:
A rare form of fibrous dysplasia occurring spontaneously in adulthood.
Agranulocytosis:
A marked decrease in the number of granulocytes, particularly neutrophils.
Allergen:
A substance capable of inducing hypersensitivity or an allergic reaction.
Allergy:
- A hypersensitive state acquired through exposure to a particular allergen.
- Re-exposure to the same allergen elicits an exaggerated reaction.
Amalgam tattoo:
Oral soft tissue discolorations due to amalgam; most common pigmentation of the oral cavity.
Ameloblastic carcinoma:
An aggressive neoplasm of the mandible or maxilla in which the epithelial cells exhibit cytologic features of common ameloblastoma and malignancy.
Ameloblastic fibroma:
A circumscribed lesion predominantly located over unerupted molars in young patients; the epithelium and connective tissue recapitulate the cap and bell stages of odontogenesis.
Ameloblastic fibro-odontoma:
An expansile growth in young patients that contains the soft tissue components of ameloblasticfibroma and the hard tissue components of complex odontoma.
Ameloblastic odontoma:
An extremely rare odontogenic tumor that contains an ameloblastomatous component and odontoma-like elements.
Ameloblastoma:
A benign and locally aggressive neoplasm of odontogenic epithelium that has a wide spectrum of histologic patterns resembling early odontogenesis.
Amelogenesis:
The formation of the enamel portion of the tooth.
Amelogenesis imperfecta:
A spectrum of hereditary defects in the function of ameloblasts and the mineralization of enamel matrix that results in teeth with multiple generalized abnormalities affecting the enamel layer only.
Amino acid:
An organic compound containing the amino group NH2. Amino acids are the main component of proteins.
Analogous:
Having similar properties.
Anaplastic:
Pertaining to adult cells that have changed irreversibly toward more primitive cell types. Such changes are often malignant.
Anaphylaxis:
A type of hypersensitivity or allergic reaction in which the exaggerated immunologic reaction results from the release of vasoactive substances such as histaminThe reaction occurs on re-exposure to a foreign protein or other substance after sensitization.
Anemia:
Reduction to less than normal of the number of red blood cells, quantity of hemoglobin, to the volume of packed red blood cells in the blood.
Aneurysmal bone cyst:
An uncommon lesion (not a true cystic lesion) located primarily in the posterior mandible and maxilla with clinical features similar to central giant cell lesion; it contains many large blood-filled spaces separated by connective tissue septa containing giant cell tissue.
Angioma:
A tumor made up of blood or lymph vessels.
Angiosarcoma:
Malignant, rare, rapidly growing lesion of endothelial cells that is more common in young patients and has a poor prognosis.
Ankyloglossia:
Extensive adhesion of the tongue to the floor of the mouth or the lingual aspect of the anterior portion of the mandible caused by a short lingual frenum.
Ankylosed teeth:
Teeth that are fused to the alveolar bone; a condition especially common with retained deciduous teeth.
Anodontia:
Congenital condition in which all the teeth fail to develop.
Anomaly:
Deviation from normal.
Antibiotic:
Any substance produced by a microorganism which harms or kills another microorganism.
Antibody:
A protein produced in the body in response to stimulation by an antigen. Antibodies react specifically to antigens in an attempt to neutralize these foreign substances.
Antigen:
A substance, usually a protein that is recognized as foreign by the body’s immune system and stimulates formation of a specific antibody to the antigen.
Aplasia:
Absence of an organ or organ part due to failure of development of the embryonic tissue of origin.
Apical periodontal cyst:
An odontogenic cyst of inflammatory origin that is preceded by a chronic periapical granuloma and stimulation of rests of malassez present in the periodontal membran
Asymptomatic:
A lack of symptoms or complaints by the patient.
Atrophic:
A normally developed tissue that has decreased in size.
Attrition:
Loss of tooth structure due to mechanical action of mastication.
Autoantibody:
An antibody that reacts against an antigenic constituent of the person’s own tissues.
Autoimmune disease:
A disease characterized by tissue injury caused by a humoral or cell-mediated immune response against constituents of the body’s own tissues.
Autoimmunity:
Immune-mediated destruction of the body’s own cells and tissues; immunity against self.
Autosomes:
The non-sex chromosomes that is identical for men and women.
Atypical:
Irregular, not conformable to the type.
Autoinoculation:
To inoculate with a pathogen such as a virus from one’s own body.
Basal cell carcinoma:
Common, locally destructive, non-metastasizing malignancy of the skin composed of medullary patterns of basaloid cells.
Basaloid squamous cell carcinoma:
Rare, aggressive form of poorly differentiated squamous cell carcinoma consisting of medullary patterns of cells with central areas of necrosis.
Benign fibro-osseous lesions:
A collection of non-neoplastic intraosseous lesions that replace normal bone & consist of a cellular fibrous connective tissue within which nonfunctional osseous structures form.
Benign fibrous histiocytoma:
Benign neoplasm of fibroblasts with a propensity to differentiate into histiocytes.
Benign lymphoepithelial cyst:
A lymphoepithelial cyst commonly located intraorally on the posterior lateral tongue and the anterior floor of the mouth.
Benign migratory glossitis:
Multiple sensitive irregularly shaped erythematous patches on the tongue with arcuate white rims that enlarge and change shape daily.
Biopsy:
Excision of living tissue for the purpose of examination by a pathologist.
Blanching:
To take the color out of, and make white.
Blue nevus:
A benign pigmented lesion that presents as a dark blue dome-shaped papule or as a flat macule on the skin or mucosa.
B lymphocyte:
A lymphocyte, also called a b cell that matures without passing through the thymus. It matures into plasma cells that produce antibodies.
Bohn’s nodules:
Uncommon superficial raised nodules occur scattered over the hard palate near the border with the soft palate of infants that resolve without treatment; derived from rests of the dental lamina and consisting of keratin-producing epithelial lining.
Brodie’s abscess:
A chronic abscess walled off in sclerotic bone.
Branchial cleft cyst:
An unusually large lymphoepithelial cyst located on the lateral aspect of the neck.
Bruxism:
A habit related to stress or a sleep disorder, characterized by grinding one’s teeth.
Bony:
Composed of or containing bone.
Botryoid odontogenic cyst:
A slow-growing, non-expansile developmental odontogenic cyst derived from one or more rests of the dental lamina, containing an embryonic lining of 1 to 3 cuboidal cells and distinctive focal thickenings (plaques).
Buccal bifurcation cyst:
A cyst of uncertain origin found primarily on the distal or facial aspect of a vital mandibular third molar, consisting of intensely inflamed connective tissue and epithelial lining.
Bulimia:
An eating and psychiatric compulsive disorder characterized by episodic binge eating of large volumes of food, followed by purging behavior such as self-induced vomiting, vigorous exercise and laxative or diuretic abuse.
Bulla:
A circumscribed elevated lesion that is more than 5 mm in diameter, usually contains serous fluid, and looks like a blister.
Bull’s eye lesion:
Skin lesions which are concentric rings resembling a circle within a circle; with a slightly depressed, dusky purple center, an elevated, surrounding macular erythema pale middle zone, and an erythematous border; usually associated with herpes simplex or mycoplasma infections.
Café au lait spots:
Hyperpigmented lesions that may vary in color from light brown to dark brown. The borders may be smooth or irregular.
Calcifying epithelial odontogenic tumor:
A locally aggressive tumor consisting of strands and medullary patterns of squamous and clear cells that are often accompanied by spherical calcifications and amyloid- staining hyaline deposits.
Calcifying odontogenic cyst:
A rare, well-circumscribed, solid or cystic lesion derived from odontogenic epithelium that resembles follicular ameloblastoma but contains “ghost cells” and spherical calcifications.
Candidiasis:
Encompasses a group of mucosal and cutaneous conditions with a common etiologic agent from the candida genus of fungi; most common oral mycotic infection.
Capsule:
Compressed fibrous connective tissue around a benign neoplasm separating it from surrounding tissues.
Carcinogen:
An agent that induces cancer.
Carcinogenesis:
The train of biological events that underlies development of neoplasia.
Carcinoma:
A malignant growth made up of epithelial cells that are capable of infiltration and metastasis. Carcinoma is a specific form of cancer.
Carcinoma in situ:
The most severe stage of epithelial dysplasia, involving the entire thickness of the epithelium, with the epithelial basement membrane remaining intact.
Caries:
The progressive loss of tooth mineral, followed by bacterial invasion into the demineralized tooth.
Carrier:
In genetics, a heterozygous individual who is clinically normal but who can transmit a recessive trait or characteristic; also, a person who is homozygous for an autosomal dominant condition with low penetrance.
Cellulitis:
A painful swelling of the soft tissue of the mouth and face resulting from a diffuse spreading of purulent exudate along the fascial planes that separate the muscle bundles.
Cell-mediated immunity:
Immunity in which the predominant role is played by t lymphocytes.
Cementoblastoma:
A benign, well-circumscribed neoplasm of cementum-like tissue growing in continuity with the apical cemental layer of a molar or premolar that produce expansion of cortical plates and pain.
Cemento-ossifying fibroma:
A well-demarcated, encapsulated, expansile intraosseous lesion of the jaws composed of cellular fibrous tissue containing spherical calcifications and irregular, randomly oriented bony structures.
Centimeter:
The fundamental unit of distance in the metric system, equal to 0.01 meter. One centimeter is about 0.393 inch.
Central:
In oral pathology, a lesion occurring within bone.
Central calcifying epithelial odontogenic tumor:
A locally aggressive tumor consisting of strands and medullary patterns of squamous and clear cells that are often accompanied by spherical calcifications and amyloid- staining hyaline deposits.
Central giant cell lesion:
An intraosseous destructive lesion of the anterior mandible and maxilla in which larger lesions expand the cortical plates, cause movement of teeth, and produce root resorption; composed of multinucleated giant cells in a background of mononuclear fibro-histiocytic cells and red blood cells.
Central odontogenic fibroma:
An intraosseous benign neoplasm derived from connective tissue of odontogenic origin containing widely scattered islands and strands of embryonic odontogenic epithelium and calcifications.
Centromere:
The constricted portion of the chromosome that divides the short arms from the long arms.
Cervical lymphoepithelial cyst:
An unusually large lymphoepithelial cyst located on the lateral aspect of the neck.
Cervical enamel projection:
Focal apical extensions of the coronal enamel beyond the normally smooth cervical margin and on to the root of the tooth.
Cheesy:
Lesion’s texture is similar to curds of cheese.
Chemotaxis:
Taxis or movement in response to chemical stimulation.
Chemotherapy:
The treatment of cancer with drugs that can destroy cancer cells. These drugs often are called “anticancer” drugs.
Cherubism (Juvenile fibrous dysplasia):
Autosomal dominant fibro-osseous lesion of the jaws involving more than one quadrant that stabilizes after the growth period, usually leaving some facial deformity and malocclusion.
Chondrosarcoma:
Uncommon malignant bone neoplasm in the jaws, usually of the anterior maxilla, consisting of a proliferation of plump chondroblasts or spindle-shaped mesenchymal cells and abnormal cartilage but no osteoid or bonChondrosacomas of the maxillofacial region are extremely rare tumors, accounting for only about 1% of chondrosarcomas of the entire body.
Chromatid:
Either of the two vertical halves of a chromosome that are joined at the centromer
Chromatin:
A general term used to refer to the material (DNthat forms the chromosomes.
Chronic:
Persisting over a long time; when applied to a disease, chronic means that there has been little change or extremely slow progression over a long period.
Chronic apical pulpitis:
A lesion located at the root apex showing the extension of the inflammatory process. from the pulpal chamber.
Chronic hyperplastic pulpitis (Pulp polyp):
An uncommon and specific type of inflammatory hyperplasia reaction to deep caries in a young tooth in which an inflamed pulp extends through a large carious lesion; usually associated with a non-vital tooth.
Chronic osteomyelitis:
Prolonged inflammation of bone marrow, almost invariably due to infection.
Chronic pulpitis:
An inflammation of the pulp caused by injury to the pulp, usually from dental caries or trauma.
Clear cell calcifying epithelial odontogenic tumor:
A locally aggressive tumor consisting of strands and medullary patterns of squamous and clear cells that are often accompanied by spherical calcifications and amyloid- staining hyaline deposits.
Clear cell odontogenic carcinoma:
A rare neoplasm of the jaw with malignant potential and unknown cytogenetic alterations.
Cleft lip:
A developmental defect characterized by the failure of fusion of median nasal process and maxillary process.
Cleft palate:
A developmental defect of the palate characterized by a lack of complete fusion of the two lateral portions of the palate, resulting in a communication with the nasal cavity.
Cleidocranial dysplasia:
A rare condition inherited as an autosomal dominant and characterized by partial or complete absence of the clavicles, defective ossification of the skull, and faulty occlusion due to missing, misplaced, or supernumerary teeth.
Consanguinity:
Blood relationship. In genetics, the term is generally used to describe matings or marriages among close relatives.
Cotton wool:
Confluent radiopacities
Crouzon syndrome:
An uncommon, autosomal dominant craniofacial disorder characterized by craniosynostosis and dysmorphic facial features.
Cyst:
A pathologic epithelium-lined cavity, usually containing fluid or semisolid.
Cystic hygroma:
Anomaly of the lymphatic system characterized by single or multiple cysts within the soft tissues, usually involving the neck.
Cytologic:
Pertaining to the scientific study of cells.
Cytology:
The scientific study of structures within the cell.
Cytopathic:
Pertaining to or characterized by pathologic changes in cells.
Degeneration:
Reversible pathologic changes with cells.
Delayed eruption:
Appearance of deciduous or permanent teeth relative to the normal age rang
Dentinogenesis:
The formation of dentin.
Dens evaginatus:
A developmental anomaly in which a focalarea of the crown projects outward and produces what appears as an extra cusp or an abnormal shape to existing cuspal arrangements (talon cusps).
Dens in dente:
“A tooth within a tooth”; a malformed tooth caused by an invagination of the crown before it is calcified.
Dental fluorosis:
A condition of emamel hypoplasia characterized by white chalky spots or brown staining & pitting of teeth due to an increased level of fluoride affecting enamel matrix formation and calcification by impairment of ameloblastic function.
Dental lamina cyst of the newborn:
Uncommon superficial raised nodules on edentulous alveolar ridges of infants that resolve without treatment; derived from rests of the dental lamina and consisting of keratin-producing epithelial lining.
Denticle:
Sperical calcification within the dental pulp lying free or attached to the pulpal surface of the tooth.
Dentigerous cyst:
An odontogenic cyst, that surrounds the crown f an impacted tooth; caused by fluid accumulation between the reduced enamel epithelium and the enamel surface, resulting in a cyst in which the crown is located within the lumen and root(s) outside.
Dentine dysplasia:
A hereditary defect in dentin formation in which the coronal dentin and tooth color is normal; the root dentin is abnormal with a gnarled pattern and associated shortened and tapered roots.
Dentinogenesis imperfecta:
A hereditary defect consisting of opalescent teeth composed of irregularly formed and undermineralized dentin that obliterates the coronal and root pulpal chambers.
Deoxyribonucleic:
(DNA) substance composed of a double chain of polynucleotides; both chains coiled around a central axis form a double helix. DNA is the basic genetic code or template for amino acid formation.
Dermoid cyst:
A cyst of the midline of the upper neck or the anterior floor of the mouth of young patients, derived from remnants of embryonic skin, consisting of a lumen lined by a keratinizing stratified squamous epithelium & containing one or more skin appendages such as hair, sweat, or sebaceous glands.
Desmoplastic fibroma:
Benign diffuse infiltrative proliferation of fibroblasts and mature collagen occurring primarily within the mandible in young patients.
Differential diagnosis:
A list of possible diseases that fit the information derived from examination of a patient.
Diffentiation:
The distinguishing of one thing from another.
Diffuse:
In the description of a lesion, borders of the lesion are not well defined, and it is not possible to detect the exact parameters of the lesion.
Dilaceration:
An abnormal bend or curve, as in the root of a tooth.
Diploid:
Having two sets of chromosomes; the normal constitution of somatic cells.
Dominant:
In genetics, a trait or characteristic that is manifested when it is carried by only one of a pair of homologous chromosomes.
Dry mouth:
Decreased saliva production.
Dorsal:
Directed toward or situated on the back surface (opposite of ventral).
Double lip:
Anomaly characterized by a horizontal fold of redundant mucosal tissue located on the inner aspect of the upper lip.
Down syndrome:
A common and easily recognizable chromosomal disorder caused by an error in cell division that results in the presence of an additional third chromosome 21 and presents mild to moderate mental retardation and associated medical problems.
Drug induced gingival hyperplasia:
Generalized increase in the fibrous component of the gingiva in patients who have been taking long-term doses of phenytoin (dilantin), cyclosporine and nifedipinPersistent dental plaque, calculus (tartar) and gingival irritation increase the severity of the hyperplasia.
Dry socket:
A condition sometimes occurring after tooth extraction, particularly after traumatic extraction, resulting in a dry appearance of the exposed bone in the socket, due to disintegration or loss of the blood clot.
Dysplasia:
An abnormality of development characterized by the loss of normal cellular architecture.
Dystrophic calcifications:
Ectopic linear calcification within the pulp chamber of a tooth.
Ecchymosis:
Large reddish-blue areas caused by the escape of blood into the tissues, commonly referred to as a bruisEcchymoses do not blanch on diascopy.
Ectodermal:
Pertaining to the outermost of the three primitive germ layers of an embryo. The middle layer is the mesoderm and the innermost layer is the endoderm. Ectodermal structures include the skin, hair, nails, oral mucous membrane, and the enamel of the teeth.
Ectopic sebaceous gland:
Collection of sebaceous glands that occur in various locations within the oral cavity.
Edema:
Abnormal amounts of fluid in the intercellular spaces, resulting in visible swelling.
Edentulous:
The clinical absence of teeth.
Embryonic:
Pertaining to the earliest stage of development of an organism.
Emigration:
The passage or white blood cells through the endothelium and wall of small blood vessels.
Enamel hypoplasia:
A defect in tooth enamel that results in less quantity of enamel than normal.
Enamel pearl:
Ectopic nodular deposits of enamel that primarily occur in the bifurcation or trifurcation areas on the roots of molars.
Epidermoid cyst:
A cyst of skin with a lumen lined by keratinizing stratified squamous epithelium, usually filled with keratin and without skin appendages in the capsule wall.
Epstein’s pearls:
Uncommon superficial raised nodules on the midline of the hard palate of infants that resolve without treatment; derived from rests of the dental lamina and consisting of keratin-producing epithelial lining.
Epulis fissuratum:
Proliferation of fibrous connective tissue with an associated chronic inflammation in response to chronic injury.
Epithelium:
The cellular makeup of skin and mucous membranes.
Endodermal:
Pertaining to the innermost of the three primitive germ layers of an embryo. Endodermal structures include the epithelium of the pharynx, respiratory tract (except the nose), and the digestive tract.
Epithelial dysplasia:
A premalignant change in epithelium characterized by a combination of individual cell and architectural alterations.
Erosion:
The wearing away of teeth through the action of chemical substances, or a denudation of epithelium above the basal cell layer.
Eruption cyst:
An odontogenic cyst with the histologic features of a dentigerous cyst that surrounds a tooth’s crown that has erupted through bone but not soft tissue and is clinically visible as a soft fluctuant mass on the alveolar ridges.
Eruption sequestrum:
A small spicule of calcified tissue that is extruded through the alveolar mucosa that overlies an erupting molar.
Erythema:
An abnormal redness of the mucosa or gingiva.
Erythematous:
Characterized by a redness of the tissue due to engorgement of the capillaries in the region. Erythematous lesions blanch on diascopy.
Erythroplakia:
A chronic red oral mucosal patch usually not attributed to traumatic, vascular or inflammatory causes but frequently caused by epithelial dysplasia, ca in situ, or squamous cell carcinoma.
Erthroplastic:
Characterized by a reddish appearancThis term implies abnormal tissue proliferation in the reddish area.
Esinophilic granuloma:
A probable neoplastic proliferation of langerhans type of histiocytic cells with a wide spectrum of biological behavior ranging from a single lesion of the mandible to diffusely distributed bone lesions in combination with organ and other soft tissue lesions; consists of s-100 positive histiocytes containing birbeck granules and accumulations of eosinophils.
Etiology:
The study or theory of the factors that cause disease and their introduction to the host.
Ewing sarcoma:
Rare malignant bone neoplasm of uncertain cell origin in young patients; The lesion is composed of anaplastic small, dark, round cells containing glycogen granules and intermediate filaments.
Exophytic:
An outwardly growing lesion.
Exostosis:
An exophytic nodular growth of dense cortical bone commonly located on maxillary or mandibular buccal alveolar bone, usually in the bicuspid / molar area.
Expansile:
Capable of being extended or expanded.
Expressivity:
In genetics, the degree of clinical manifestation of a trait or characteristic.
Extrinsic stain:
Stains on the surface of teeth.
Exudate:
Fluid composed of cells, proteins, and solid materials that pass through vessel walls into adjoining tissues; may leak from incisions or sites of infection or inflammation to form a clot.
Facies:
The appearance of the face.
Fever:
An elevation of body temperature to greater than the normal of 98.6°F (37°C).
Fibrin:
An insoluble protein that is essential to the clotting of blood.
Fibroma:
Hyperplasia of fibrous connective tissue that evolves in response to chronic irritation in which there is extensive elaboration of collagen resembling scar tissue.
Fibromatosis:
Benign diffuse infiltrative proliferation of fibroblasts and mature collagen occurring within the soft tissues of the head and neck in young patients.
Fibrosarcoma:
Malignant neoplasm of fibroblastic cells.
Fibrous dysplasia:
An asymptomatic regional alteration of bone in which the normal architecture is replaced by fibrous tissue and nonfunctional trabeculae-like osseous structures; lesions may be monostotic or polyostotic, with or without associated endocrine disturbances.
Firm:
Relatively solid, compact, or unyielding to pressure or touch.
Fissural cyst:
Originally believed to arise from cystic degeneration of epithelium remnants entrapped along lines of fusion of embryonic growth processes; now origin is controversial.
Fissure:
A narrow slit or cleft.
Fissure tongue:
Deep grooves in dorsum of tongue, which cause no adverse consequences other than being a collection site for food debris and colonization site for candida albicans.
Fistula:
A drainage pathway or abnormal communication between two epithelium-lined surfaces due to destruction of the intervening tissue.
Florid osseous dysplasia:
Diffuse asymptomatic radiopaque and radiolucent intraosseous areas of cemento- osseous tissue that involve.
Fluctuant:
A wavelike motion felt on palpating a cavity with nonrigid walls, especially one containing fluid.
Fluoride mottling:
A condition of enamel hypoplasia characterized by white chalky spots or brown staining and pitting of teeth due to an increased level of fluoride affecting enamel matrix formation and calcification by impairment of ameloblastic function.
Focal osteitis:
A condition sometimes occurring after tooth extraction, particularly after traumatic extraction, resulting in a dry appearance of the exposed bone in the socket, due to disintegration or loss of the blood clot.
Follicular cyst:
A unique and rare congenital tumor of the alveolar mucosa of the jaws that occurs only in newborns.
Fordyce granules:
Collection of sebaceous glands that occur in various locations within the oral cavity.
Foreign body granuloma:
A reaction to foreign materials that is too large to be ingested by either microphages (PMNS) or macrophages.
Frenal tag:
A redundant piece of mucosal tissue that projects from the maxillary labial frenum.
Fusion:
The union of two adjoining tooth germs.
Gamete:
Spermatozoon or ovum.
Gardner syndrome:
A rare autosomal dominant disease characterized by GI polyps, multiple osteomas, and soft tissue tumors.
Garrè osteomyelitis:
An unusual hyerplastic reaction of the periosteum to a chronic osteomyelitis of the posterior mandible that is unique to young patients.
Geographic tongue:
Multiple sensitive irregularly shaped erythematous patches on the tongue with arcuate white rims that enlarge and change shape daily.
Gemination:
In dentistry a single tooth germ splits completely or partially, forming separate crowns. The tooth usually has a single root and root canal; also called twinning.
Genetic heterogeneity:
Having more than one inheritance pattern.
Ghost teeth:
A developmental disturbance of several adjacent teeth in which the enamel and dentin are thin and irregular and fail to adequately mineralize; surrounding soft tissue is hyperplastic and contains focal accumulations of spherical calcifications and odontogenic rests.
Gingival cyst of the adult:
A small developmental odontogenic cyst of the gingival soft tissue derived from the rests of the dental lamina, containing a lining of embryonic epithelium of cuboidal cells and distinctive focal thickenings similar to the lateral periodontal cyst.
Gingival cyst of the newborn:
Uncommon superficial raised nodules on edentulous alveolar ridges of infants that resolve without treatment; derived from rests of the dental lamina and consisting of keratin-producing epithelial lining.
Glandular odontogenic cyst:
An unusually large solitary or multilocular odontogenic cyst probably derived from the rests of dental lamina, consisting a stratified squamous epithelium containing numerous mucus-secreting cells.
Globulomaxillary radiolucency:
Radiolucency in the anterior maxilla between the roots of vital maxillary lateral incisor and the adjacent cuspid.
Gorlin cyst:
A rare, well-circumscribed, solid or cystic lesion derived from odontogenic epitheliium that resembles follicular ameloblastoma but contains “ghost cells” and spherical calcifications.
Granular cell tumor:
Submucosal mass consisting of diffuse sheets of large cells of either nerve or muscle origin with a cytoplasm of densely packed eosinophilic granules (lysosomal bodies) and commonly found in the dorsal surface of the tongue.
Granuloma:
A tumor-like mass of inflammatory tissue consisting of a central collection of macrophages, often with multinucleated giant cells, surrounded by lymphocytes.
Granulomatous:
Pertaining to a well-defined area that has developed as a reaction to the presence of living organisms or a foreign body. The tissue consist primarily of histiocytes.
Ground glass:
Fine radiopaque spots in radiolucent background.
Hamartoma:
A tumor-like nodule consisting of a mixture of normal tissue usually present in an organ but existing in an unusual arrangement and/or an unusual site.
Hairy tongue:
Marked accumulation of keratin on the filiform papillae of the dorsum of the tongue resulting in hairy appearance and discoloration of the tongue thought to denote a change in the body’s natural bacterial balance.
Haploid:
A cell with a single set of chromosomes. A gamete is haploid.
Hard:
Tissue having a firm intercellular substance.
Hemangioma:
A proliferation of large (cavernous) or small (capillary) vascular channels occurring commonly in children; individual lesions have variable clinical courses.
Hematocrit:
The volume percentage of red blood cells in whole blood.
Hematoma:
A large ecchymosis or bruise caused by the escape of blood into the tissues. Hematomas are blue on the skin and red on the mucous membranes. As hematomas resolve they may turn brown, green, or yellow.
Hematopoietic bone marrow defect:
Abnormal anatomic variation of bone marrow; asymptomatic radiolucent lesion that contains either hematopoietic or fibrofatty marrow.
Hemifacial atrophy:
A characteristic loss in the soft tissues below the skin, usually on one side of the face; in some severe cases, the underlying bone is also effected.
Hemifacial hypertrophy:
Condition which involves the enlargement of half of the head with enlarged teeth on the involved side.
Hemoglobin:
The iron-containing pigment of the red blood cells.
Its function is to carry oxygen to the tissues. One of the causes of anemia is a deficiency of iron, causing patients to look pale and feel tired.
Hemolysis:
Generally speaking, this term refers to the disintegration of elements in the blooA common form of hemolysis occurs during anemia and involves lysis or the dissolution of red blood cells.
Hemostasis:
The stoppage of blood flow. This can occur naturally by clotting or artificially by the application of pressure or the placement of sutures.
Hepatomegaly:
Enlargement of the liver.
Hereditary:
Transmitted or transmissible from parent to offspring; determined genetically.
Hereditary gingival fibromatosis:
Hereditary form of generalized gingival hyperplasia in which the autosomal dominant form may be associated with hypertrichosis, craniofacial deformities, epilepsy and mental retardation.
Heterotopic oral gastrointestinal cyst:
A rare and unusual developmental cyst commonly found in the tongue or floor of the mouth of infants or young children.
Heterozygote:
An individual with two different genes at the allele loci.
Histiocyte:
Large phagocytic cell from the reticuloendothelial system. The reticuloendothelial system is a network made up of all of the phagocytic cells in the body, which included macrophages, kupffer cells in the liver, microglia of the brain.
Histiocytosis x:
A probable neoplastic proliferation of langerhans type of histiocytic cells with a wide spectrum of biological behavior ranging from a single lesion of the mandible to diffusely distributed bone lesions in combination with organ and other soft tissue lesions; consists of s-100 positive histiocytes containing birbeck granules and accumulations of eosinophils.
Histology:
The microscopic study of the structure and form of the various tissues making up a living organism.
Homozygote:
An individual having identical genes at the allele loci.
Hormone:
A chemical substance produced in the body that has a specific regulatory effect on certain cells or a certain organ or organs.
Humoral immunity:
Immunity in which antibodies play the predominant role.
Hutchinson’s incisors:
Screwdriver-shaped central incisors seen in congenital syphilis.
Hypercementosis:
Excessive deposit of cementum on root surface.
Hyperchromatic:
Staining more intensely than normal.
Hyperdontia:
A condition or circumstance characterized by one or more extra, or supernumerary teeth.
Hyperemia:
The presence of excess blood in a tissue area.
Hyperglycemia:
The presence of excessive sugar or glucose in the bloodstream.
Hyperkeratosis:
Excessively thickened layer of the stratum corneum composed of orthokeratin (hyperorthokeratosis) or parakeratin (hyperparakeratosis).
Hyperorthokeratosis:
Keratin is the outermost layer of epithelium as seen under the microscope and is seen in two forms: orthokeratin and parakeratin. Orthokeratin has no visible nuclei within the outer layer, whereas in parakeratin nuclei are present.
Hyperparakeratosis:
Keratin is the outermost layer of epithelium as seen under the microscope and is seen in two forms: orthokeratin and parakeratin.
Orthokeratin has no visible nuclei within the outer layer, whereas in parakeratin nuclei are present.
Hyperparathyroidism:
Loss of bone mineralization (osteoporosis) because of increased paratharmone secretion (primary) or increased demand for serum calcium (secondary), resulting in multiple systemic complications, loss of alveolar bone architecture, and occasionally giant cell tumor (“brown tumor”).
Hyper pigmentation:
Excessive pigmentation.
Hyperplasia:
An increase in the size of a tissue or organ due to an increase in the number of constituent cells.
Hyperplastic gingivitis:
Focal or generalized fibrous hyperplasia of the marginal gingiva with an associated inflammatory response.
Hypersensitivity:
Generally this term means an abnormal sensitivity to a stimulus of any kinThe term, however is often used with specific reference to some form of allergic response.
Hypertrophy:
An increase in the size of a tissue or organ due to an increase in the size of constituent cells.
Hypocalcification:
Less than normal amount of calcification.
Hypochromic:
Stained less intensely than normal.
Hypodontia:
The congenital absence of one or several teeth as a result of agenesis.
Hypoglycemia:
Less than normal amount of sugar or glucose in the bloodstream.
Hypophosphatasia:
A genetic metabolic disorder of bone mineralization caused by a deficiency in alkaline phosphatase in serum and tissues; characterized by skeletal defects resembling those of rickets.
Hypophosphatemia:
Deficiency of phosphates in the blood.
Hypopigmentation:
Decrease in pigment production.
Hypoplasia:
Incomplete development of a tissue or organ; a tissue reduced in size because of a decreased number of constituent cells.
Immune complex:
A combination of antibody and antigen.
Immune reaction:
Aprotective response to a specific invading pathogen.
Immunodeficiency:
A deficiency of the immune response caused by hypoactivity or decreased numbers of lymphoid cells.
Immunoglobulin:
A protein, also called an antibody, synthesized by plasma cells in response to a specific antigen.
Impacted teeth:
Teeth continue to form within bone but fail to erupt into the oral cavity because of a physical obstruction.
Incisive canal cyst:
An intraosseous developmental cyst of the midline of the anterior palate, derived from the islands of epithelium remaining after closure of the embryonic nasopalatine duct.
Indurated:
Characterized by being hard; an abnormally hard portion of a tissue with respect to the surrounding similar tissue; often used to describe the feel of locally invasive malignant tissue on palpation. An excessive hardening or firmness of any body site. One of the signs of inflammation.
Induration:
Characterized by being hard; an abnormally hard portion of a tissue with respect to the surrounding similar tissue; often used to describe the feel of locally invasive malignant tissue on palpation.
Inflammatory papillary hyperplasia:
A reactive tissue growth that usually develops beneath a denture.
Infection:
Invasion by pathogenic microorganisms which reproduce and multiply, causing disease by local cellular injury, secretion of a toxin, or antigen-antibody reaction in the host.
Inflammatory fibrous hyperplasia:
Proliferation of fibrous connective tissue with an associated chronic inflammation in response to chronic injury.
Inflammatory reaction:
A defense mechanism to an invading pathogen which includes repair and destruction; prepares tissue for healing and controls spread of infection.
Insulin:
A protein hormone secreted by the islands of langerhans of the pancreas; insulin deficiency produces hyperglycemia, otherwise known as diabetes mellitus.
Intramucosal nevus:
The pigmented nevus is characterized by a proliferation of nevus cells microscopically within the underlying connective tissue.
Intrinsic stain:
Stains on the inner layers of the dentin and pulp.
Involucrum:
New bone formed by the periosteum.
Invasive squamous cell carcinoma:
Histological evidence of invasion and presence of malignant cells in the connective tissue.
Invasion:
The infiltration and active destruction of surrounding tissues.
Irreversible pulpitis:
Progresses from reversible pulpitis, a severe inflammation of the pulp.
Irritation fibroma:
Hyperplasia of fibrous connective tissue that evolves in response to chronic irritation in which there is extensive elaboration of collagen resembling scar tissue.
Ischemia:
A deficiency of blood to a body part usually due to constriction or blockage of a blood vessel.
Jaffe-lichtenstein syndrome:
A syndrome characterized by polyostotic fibrous dysplasia of the skeletal system and cafe-au-lait spots
Jaundice:
A diseased condition of the liver due to the presence of bile pigments in the blood and characterized by yellowish staining of the eyes, skin and body fluids.
Junctional nevus:
The pigmented nevus is characterized by a proliferation of nevus cells microscopically within the basal cell layer of the surface epithelium.
Juvenile fibrous dysplasia:
A form of fibrous dysplasia which features slow growing regional distortion that usually enlarges proportionately with the affected bone.
Kaposi sarcoma:
A unique form of angiosarcoma that occurs in elderly and HIV-Positive patients and has a predilection for the palate.
Karyotype:
A photomicrographic representation of a person’s chromosomal constitution arranged according to the denver classification.
Keratinization:
The formation of microscopic fibrils of keratin in the keratinocytes (keratin-forming cells) In the oral cavity the term is used to describe changes in the outer layer of the epithelium.
Keratoacanthoma:
A benign endophytic epithelial growth appearing as a wee circumscribed keratin-filled crateronsun-exposed skin; often mistaken for squamous cell carcinoma.
Keratotic:
A condition of the skin characterized by the presence of horny growths.
On the oral mucous membrane, keratotic tissue usually looks white; the term implies a thickening of the outer layer of the oral epithelium.
Klestadt cyst:
A developmental cyst of the soft tissue of the anterior muco-buccal fold beneath the ala of the nose, most likely derived from remnants of the inferior portion of the nasolacrimal duct.
Langerhans cell histiocytosis:
A probable neoplastic proliferation of langerhans type of histiocytic cells with a wide spectrum of biological behavior ranging from a single lesion of the mandible to diffusely distributed bone lesions in combination with organ and other soft tissue lesions; consists of s-100 positive histiocytes containing birbeck granules and accumulations of eosinophils.
Latent bone cyst:
A slow-growing, non-expansile developmental odontogenic cyst derived from one or more rests of the dental lamina.
Containing an embryonic lining of 1 to3 cuboidal cells and distinctive focal thickenings (plaques).
Lateral:
Pertaining to or situated at the side.
Leukocytosis:
A temporary increase in the number of white blood cells circulating in blood.
Lateral periodontal cyst:
A slow-growing, non-expansile developmental odontogenic cyst derived from one or more rests of the dental lamina, containing an embryonic lining of 1 to 3 cuboidal cells and distinctive focal thickenings (plaques).
Le cell:
A cell that is a characteristic of lupus erythematosus and other autoimmune diseases. It is a mature neutrophil that has phagocytozed a spherical inclusion derived from another neutrophil.
Leiomyoma:
Benign neoplasm of smooth muscle within the oral cavity, usually of the blood vessels, that appears as a firm, movable, submucosal nodule.
Lentigo maligna melanoma:
Slowly evolving melanoma that develops within a pre-existing pigmented macular lesion on the sun-exposed skin of elderly patients.
Lesion:
A site of structural or functional change in body tissues that is produced by disease or injury.
Leukoedema:
Accumulation of fluid within the epithelial cells of the buccal mucosa.
Leukoplakia:
A clinical term used to denote mucosal conditions that produce a whiter than normal coloration of the mucous membranes; a white patch that cannot be rubbed off and that does not clinically represent any other condition.
Lichen planus:
A skin disease common within the oral cavity, where it appears as either white reticular, plaque, or erosive lesions with a prominent t lymphocyte response in the immediate underlying connective tissue.
Linea alba:
A soft linear streak of parakeratinized tissue on the buccal mucosa at the occlusal linThe line may be initiated by irritation from rough buccal cusps, bruxism or habitual clenching of teeth.
Lingual mandibular salivary gland depression:
A developmental concavity of the lingual cortex of the mandible, usually in the third molar area, caused by overextension of an accessory lateral lobe of the submandibular gland, and has the radiographic appearance of a well-circumscribed cystic lesion within the bone, usually below the inferior alveolar canal.
Lingual thyroid nodule:
Accessory accumulation of thyroid tissue that is usually functional within the body of the posterior tongue.
Lingual varicosities:
A normal variant in adults over 60 years of agEnlarged veins usually purple or red on ventral and lateral surface of the tongue.
Lipid:
Fat or fatty; a naturally occurring substance made up of fatty acids.
Lipoma:
Benign neoplasm of normal fat cells that appears as a soft, movable swelling, often with a slight yellowish coloration.
Liposarcoma:
Rare, malignant neoplasm of the oral cavity composed of a wide spectrum of histologic patterns of the fat cells.
Lip pits:
Autosomal dominant trait resulting in developmental defects involving the paramedial portion of the vermilion of the lower and upper lip or the labial commissure area.
Lobulated:
Made up of lobules, which are smaller divisions of lobes. Many structures are divided into lobes and lobules, such as the brain, lung, and salivary glands. Some pathologic lesions are described as lobulated when the lesion is divided into smaller parts.
Local:
Confined to a limited part, not general or systemic.
Ludwig angina:
Cellulitis involving fascial spaces between muscles and other structures of the posterior floor of the mouth that can compromise the airway.
Lymphadenopathy:
Any disease process that affects lymph nodes such that they become enlarged and palpable.
Lymphoid tissue:
Tissue composed of lymphocytes supported by a meshwork of connective tissue.
Lymphangioma:
Benign proliferation of lymphatic vessels that occurs as a focal superficial lesion within the oral cavity and as a massive diffuse lesion of the neck (cystic hygroma).
Lymphocyte:
A variety of leukocyte or white blood cell that is important to the immune response and that arises in the lymph nodes. Lymphocytes can be large or small, and are round, nongranular, and classified as either t- or b-lymphocytes.
Lymphoblastic:
Pertaining to a cell of the lymphocytic series; the term implies proliferation. Lymphoblastic is one of the forms of leukemic cancer of the white blood cells characterized by the presence of malignant lymphoblasts or immature lymphocytes.
Lymphoepithelial cyst:
A cyst with a lumen lined by a keratinizing stratified squamous epithelium and a capsule containing multiple normal lymphoid follicles and a dense accumulation of normal lymphocytes.
Macrodontia:
Teeth that are considerably larger than normal.
Macroglossia:
A congenital disorder where the tongue is larger than normal due to an increase in the amount of tissue.
Macrophage:
A large, mononuclear phagocyte derived from monocytes.
Macrophages become mobile when stimulated by inflammation and interact with lymphocytes in an immune response.
Macrostomia:
Greatly exaggerated width of the mouth, resulting from failure of union of the maxillary and mandibular processes, with extension of the oral orifice toward the ear. The defect may be unilateral or bilateral.
Macule:
An area that is usually distinguished by a color different from that of the surrounding tissuIt is flat and does not protrude above the surface of the normal tissue (e.g. Freckles).
Malaise:
A constitutional symptom that describes a feeling of uneasiness, discomfort, or indisposition.
Malignant:
A neoplastic growth that is not usually encapsulated, grows rapidly, and can readily metastasize.
Malignant ameloblastoma:
A lesion with the histopathologic features of common ameloblastoma in which a metastasis has occurred.
Malignant fibrous histiocytoma:
Malignant neoplasm of fibroblasts with a propensity to differentiate into histiocytic and fibrohistiocytic cells.
Malignant tumor:
Cancer; a tumor that is resistant to treatment and frequently causes death; a tumor that has the potential for uncontrolled growth & dissemination or recurrence or both.
Mandibular infected buccal cyst:
A cyst of uncertain origin found primarily on the distal or facial aspect of a vital mandibular third molar, consisting of intensely inflamed connective tissue and epithelial lining.
Margination:
A phenomenon that occurs during the relatively early phases of inflammation in which white blood cells tend to occupy the periphery of the blood vessels and adhere to endothelial cells that line the vessels.
Mastication:
Chewing.
Mccune-albright syndrome:
A syndrome characterized by polyostotic fibrous dysplasia of the skeletal system, cafe- au-lait spots, and endocrine dysfunction.
Median rhomboid glossitis:
An asymptomatic, elongated, erythematous patch of atrophic mucosa of the mid-dorsal surface of the tongue due to a chronic Albicans infection.
Meiosis:
The two-step cellular division of the original germ cells, which reduces the chromosomes from 4 NDNA to 1 NDNA.
Melanin pigmentation:
A normal variant found predominantly in dark skinned individuals. The melanin produced by melanocytes is deposited extracelluarly. An increase in the number of melanocytes produces melanin resulting in clinically visible pigmentation of skin, eyes, hair, mucosa and gingiva.
Melanoma:
Malignant neoplasm of melanocytes occurring on skin and mucosal surfaces that commonly has a radial and superficial initial growth period before it extends into the deeper underlying tissues and metastasizes.
Melanosis:
Disorder of increased melanin pigmentation that develops without preceding inflammatory disease; condition characterized by abnormal deposits of melanin (especially in the skin).
Melanotic macules:
Physiologic or reactive small, flat, brown areas of the mucosal surfaces caused by an increase in the production of melanin granules but not in the number of melanocytes.
Mesenchymal:
The meshwork of embryonic connective tissue in the mesoderm that gives rise to the connective tissue of the body, blood vessels, and lymph vessels.
Mesial:
Toward the front, anterior, or midlinThe mesial surface of teeth is the side of the tooth closest to the midlinThe five surfaces of teeth are mesial, distal, occlusal or incisal, labial or facial, and lingual or palatal.
Mesiodens:
A supernumerary tooth between the maxillary central incisors.
Metastasize:
To spread or travel from one part of the body to another; a term usually reserved to describe the spread of malignant tumors.
Metastasis:
The transport of neoplastic cells to parts of the body remote from the primary tumor and the establishment of new tumors in those sites.
Metastatic tumor:
A tumor formed by cells that have been transported from the primary tumor to a site not connected to the primary tumor.
Microcyte:
A red blood cell that is smaller than normal.
Microdontia:
Teeth that are considerably smaller than normal.
Millimeter (mm):
A common metric unit of distanc One millimeter equals about 0.039 inch.
Mitosis:
The way in which somatic cells divide so that the two daughter cells receive the same number of identical chromosomes.
Mitotic figure:
Dividing cells caught in the process of mitosis.
Mixed radiolucent and radiopaque:
A radiographic lesion composed of a mixture of radiolucencies and radiopacities; indicates a mixture of soft and hard tissues.
Monocyte:
A mononuclear phagocytic leukocyte with an ovoid or kidney-shaped nucleus, containing lacey, linear chromatin, and abundant gray-blue cytoplasm filled with fine, reddish and azurophilic granules.
Mucopurulent:
Consisting of both mucous and pus.
Mucositis:
Mucosal inflammation.
Mulberry molars:
Berry-like molars seen in congenital syphilis.
Multilocular:
A term used to describe a radiographic appearance of multiple, rounded compartments of locules. These can appear “soap bubble-like” or “honeycomb-like”.
Multiple endocrine neoplasia syndrome:
Autosomal dominant condition involving the parathyroids, pancreas, thyroid and adrenal with one variant (men–IIthat has an oral manifestation consisting of multiple neuromas on the mucosalsurfaces.
Multiple neurofibromatosis:
Autosomal dominant hereditary condition consisting of multiple neurofibromas of the skin and mucosa and associated café au lait spots of the skin with the potential for producing disfigurement and malignant transformation.
Mutagenesis:
The induction of genetic mutation.
Mutation:
A permanent change in the arrangement of genetic material.
Myxoma:
An aggressive intraosseous lesion derived from embryonic connective tissue associated with odontogenesis and primarily consisting of a mucoid ground substance with widely scattered undifferentiated spindled mesenchymal cells.
Nasolabial cyst:
A developmental cyst of the soft tissue of the anterior muco-buccal fold beneath the ala of the nose, most likely derived from remnants of the inferior portion of the nasolacrimal duct.
Nasopalatine duct cyst:
An intraosseous developmental cyst of the midline of the anterior palate, derived from the islands of epithelium remaining after closure of the embryonic nasopalatine duct.
Nasopharyngeal carcinoma:
Aggressive form of squamous cell carcinoma located in the nasopharynx and having varying levels of differentiation; often first discovered as a metastatic lesion in a lateral neck lymph node.
Natal teeth:
Teeth present at birth or shortly after; eruption of permanent teeth after premature loss of preceding deciduous teeth.
Necrosis:
The death of a cell as a result of injury or disease.
Neoplasia:
The process of the formation of tumors characterized by the presence of new and uncontrolled cellular growth.
Neoplastic:
Characterized by the presence of new and uncontrolled cellular growth.
Neoplasm:
A mass of newly formed tissue in which the growth of tissue is uncontrolled and progressive; a tumor.
Nevoid basal cell carcinoma syndrome:
Autosomal dominant disorder characterized by oral, systemic and skeletal anomalies. An inherited group of defects, which involve abnormalities of the skin, eyes, nervous system, endocrine, glands and bones. The condition is characterised by an unusual facial appearance and a predisposition for skin cancer.
Neurilemoma:
Well-demarcated, benign lesion consisting of a fibroblastic proliferation of the nerve sheath cell (Schwann cell) producing distinctive patterns referred to as antoni A and antoni B tissue.
Neuroectodermal tumor of infancy:
Benign, usually pigmented neoplasm commonly of the anterior maxilla and composed of two cell types arranged in alveolar patterns and derived from embryonic neural crest tissue.
Neurofibroma:
Demarcated or diffuse benign proliferation of perineural fibroblasts that are oriented in either a random pattern with a myxoid background or a nodular (plexiform) pattern.
Neurogenic sarcoma:
Malignant neoplasm with a poor prognosis of perineural fibroblasts or schwann cells with a propensity to rapidly extend along the associated nerve trunk.
Neutrophil:
A medium-sized white blood cell with a nucleus consisting of three to five lobes and a cytoplasm containing small granules; one of a group of white blood cells called granulocytes, the others being eosinophils and basophils. Neutrophils make up about 65% of the white blood cells in normal blooAlso known as polymorphonuclear leukocyte, PMN, or “poly”.
Neutropenia:
A diminished number of neutrophils in the blood.
Nevus:
A benign, exophytic, usually pigmented, congenital lesion of the skin or mucosa composed of focal collections of rounded melanocytes; a molIt may be flat or elevated, pigmented or non-pigmented, and may or may not contain hair.
Nicolsky’s sign:
Seen in some bullous diseases, such as pemphigus vulgaris and bullous pemphigoid; the superficial epithelium separates easily from the basal layer on exertion of firm sliding manual pressure.
Nicotine stomatitis:
A diffuse white change of the palate and / or buccal mucosa caused by a combination of hyperkeratosis and acanthosis, frequently containing multiple small dimpled nodules; found in heavy smokers.
Nodule:
A palpable solid lesion up to 1 cm in diameter found in soft tissuIt can occur above, level with, or beneath the skin surface.
Noncaseating:
A tissue-degenerative process that forms a dry, shapeless mass resembling cheese.
Nodular fasciitis:
Localized benign lesion composed of fibroblasts and myofibroblasts that is often clinically mistaken for a malignancy.
Nodular melanoma:
A form of melanoma of the skin and occasionally the mucosa that arises as a raised mass with a limited macular radial-growth phase, quickly invades and metastasizes and consists of a wide variety of cell shapes and sizes.
Nondysjunction:
The result of chromosomes that were crossing over and did not separate; therefore, both migrate to the same cell.
Occluded oral tonsil:
A lymphoepithelial cyst commonly located intraorally on the posterior lateral tongue and the anterior floor of the mouth.
Odontogenic:
Tooth forming.
Odontogenic cyst:
A cyst in which the lining of the lumen is derived from epithelium produced during tooth development.
Odontoma:
A rare, well-circumscribed, solid or cystic lesion derived from odontogenic epitheliium that resembles follicular ameloblastoma but contains “ghost cells” and spherical calcifications.
Odontogenic carcinoma:
An aggressive and destructive intraosseous lesion of the mandible or maxilla that consists of poorly differented epithelial cells and clear cells in a pattern that is reminiscent of early odontogenesis.
Odontogenic fibroma:
A peripheral or intraosseous (central) benign neoplasm derived from connective tissue of odontogenic origin containing widely scattered islands and strands of embryonic odontogenic epithelium and calcifications.
Odontogenic ghost cell tumor:
A rare, well-circumscribed, solid or cystic lesion derived from odontogenic epithelium that resembles follicular ameloblastoma but contains “ghost cells” and spherical calcifications.
Odontogenic keratocyst:
A cyst derived from the remnants (rests) of the dental lamina, with a biologic behavior similar to a benign neoplasm, with a distinctive lining of six to ten cells in thickness, and that exhibits a basal cell layer of palisaded cells and a surface of corrugated parakeratin.
Oligodontia:
Presence of fewer than the normal number of teeth.
Odontogenic tumors:
Lesions derived from epithelial or mesenchymal elements, or both, that are part of the tooth-forming apparatus and are therefore found exclusively in the mandible, maxilla and on rare occasions, the gingiva.
Oncogenic:
Capable of causing tumor formation.
Oncologist:
Physicians who study, diagnose, and treat cancerous tumors.
Oncology:
The study of tumors or neoplasms.
Opportunistic:
A disease caused by a microorganism that does not ordinarily cause disease but becomes pathogenic under certain circumstances.
Oral facial digital syndrome, type I:
An x-linked dominant condition with lethality in males and is characterized by malformations of the face, oral cavity, and digits, and by a highly variable expressivity even within the same family.
Oral lymphoepithelial cyst:
A lymphoepithelial cyst commonly located intraorally on the posterior lateral tongue and the anterior floor of the mouth.
Oral tonsil:
Islands of extra pharyngeal tonsillar tissue; lymphoid aggregates that exhibit germinal centers surfaced by non-keratinized squamous epithelium.
Organism:
An viable life form, such as animals, plants, and microorganisms, including bacteria, fungi, and viruses.
Orthokeratin:
An epithelial component of hyperkeratosis, which is void of nuclei.
Ossifying fibroma:
A well-demarcated, encapsulated, expansile intraosseous lesion of the jaws composed of cellular fibrous tissue containing spherical calcifications and irregular, randomly oriented bony structures.
Osteoblastoma:
A benign neoplasm of bone that arises from osteoblasts with similar clinical, radiographic, and histopathologic features of osteoid osteoma consisting of well- demarcated, rounded intraosseous swellings, each with an active cellular central nidus surrounded by a wide zone of osteoid, with pain upon palpation.
Osteogenesis imperfecta:
A spectrum of diseases of bone due to a basic alteration in the formation of bone connective tissue matrix, resulting in an inability of the matrix to fully mineralize,, a tendency for multiple broken bones, blue sclera of the eyes, and associated dentinogenesis imperfecta.
Osteogenicsarcoma:
Most common of the malignant neoplasms derived from bone cells that in the jaws exhibit radiographic widening of periodontal membrane of teeth and histologically exhibit a wide spectrum of findings, all of which contain atypical osteoblasts and abnormal bone or osteoid formation.
Osteoid osteoma:
A benign neoplasm of bone that arises from osteoblasts with similar clinical, radiographic, and histopathologic features of osteoid osteoma consisting of well- demarcated, rounded intraosseous swellings, each with an active cellular central nidus surrounded by a wide zone of osteoid, with pain upon palpation.
Osteoma:
An exophytic nodular growth of dense cortical bone on or within the mandible or maxilla in locations other than those occupied by tori or exostoses.
Osteoporosis:
A hereditary disease marked by abnormally dense bone.
Osteopetrosis:
Generalized hereditary condition consisting of excessive bone mineralization, resulting in altered stature, frequent fractures, lack of bone marrow hematopoietic function, and a tendency for severe osteomyelitis of the jaws.
Osteoporotic bone marrow defect:
Abnormal anatomic variation of bone marrow; asymptomatic radiolucent lesion that contains either hematopoietic or fibrofatty marrow.
Osteoradionecrosis:
A condition of non-vital bone in a site of radiation injury.
Osteosclerosis:
Abnormal hardening or increased density of bone on radiographs.
Ovum:
The mature female germ cell.
Paget’s disease:
Uncoordinated increase in the osteoclastic and osteoblastic activity of the bone cells of older adults producing larger but weaker bones, extensive pain, high levels of serum alkaline phosphatase and urinary hydroxyproline, and an increased tendency to develop malignant bone neoplasms.
Palpate:
To examine by hand, to feel.
Palpation:
The evaluation of a lesion by feeling it with the fingers to determine the texture of the areThe descriptive terms for palpation are soft, firm, semifirm and fluid filleThese terms also describe the consistency of a lesion.
Papillary:
Describing a small nipple-shaped projection of elevation usually found in clusters. Papillary hyperplasia
A reactive tissue growth that usually develops beneath a denture.
Papilloma:
A benign exophytic papillary growth of stratified squamous epithelium.
Papillon lefevre syndrome:
An autosomal recessive disorder characterized by severe destructive periodontal disease affecting both the primary and permanent dentitions and hyperkeratosis of the palms of the hands and soles of the feet.
Paradental cyst:
A cyst of uncertain origin found primarily on the distal or facial aspect of a vital mandibular third molar, consisting of intensely inflamed connective tissue and epithelial lining.
Parakeratin:
An epithelial component of hyperkeratosis, which has small residual nuclei.
Parry-romberg syndrome:
A characteristic loss in the soft tissues below the skin, usually on one side of the face; in some severe cases, the underlying bone is also effected.
Parulis:
A sessile nodule on the gingiva at the site where draining sinus tact reaches the surface.
Pathogenesis:
Series of events taking place in a disease.
Pathogenic microorganism:
A microorganism that causes disease.
Pathologic:
Pertaining to or caused by disease.
Pathology:
A science that focuses on the mechanisms which cells, tissues, and organs are injured and on the structural changes that underlie disease processes.
Pathosis:
An abnormal state or condition.
Pavementing:
Adherence of white blood cells to the endothelial cells lining an injured blood vessel.
Pedunculated:
Attached by a stem-like or stalk base similar to that of a mushroom.
Penetrance:
The prevalence of individuals with a given genotype that manifest clinically the phenotype associated with that trait.
Periapical abscess:
A progression of an acute pulpitis in which exudate extends into the adjacent soft and hard tissues.
Periapical cemental dysplasia:
Asymptomatic diffuse periapical radiolucent and radiopaque areas, primarily of the anterior mandible, in which cemento-osseous tissue replaces the normal architecture of bone.
Periapical cyst:
An odontogenic cyst of inflammatory origin that is preceded by a chronic periapical granuloma and stimulation of rests of malassez present in the periodontal membrane.
Periapical granuloma:
A mass of chronically inflamed granulation tissue resulting from irritation following pulp disease or endodontic treatment.
Peripheral:
Pertaining to the outer part, such as the edge or margin.
Peripheral calcifying epithelial odontogenic tumor:
A locally aggressive tumor consisting of strands and medullary patterns of squamous and clear cells that are often accompanied by spherical calcifications and amyloid- staining hyaline deposits.
Peripheral odontogenic fibroma:
A peripheral benign neoplasm derived from connective tissue of odontogenic origin containing widely scattered islands and strands of embryonic odontogenic epithelium and calcifications.
Peripheral giant cell lesion:
An uncommon reactive growth of granulation tissue in youngsters appearing as a red- purple mass arising from the gingiva.
Peripheral ossifying fibroma:
A benign reactive lesion that occurs exclusively on the gingiva.
Phagocytosis:
A process of ingestion and digestion by cells.
Petechia:
Little red spots, ranging in size from pinpoint to several millimeters in diameter. Petechiae consist of extravasated blood.
Pigmented:
Colored as the result of a deposit of pigment.
Phenotype:
The physical and clinical visible characteristics of an individual. Genotype is the genetic composition. Phenotype is its observable appearance.
Pindborg tumor:
A locally aggressive tumor consisting of strands and medullary patterns of squamous and clear cells that are often accompanied by spherical calcifications and amyloid- staining hyaline deposits.
Plaque:
An area with a flat surface and raised edges.
Platelet:
One of the elements found in circulating blooA platelet has a circular or disk-like shape is small; hence the term platelet.
Platelets aid in blood coagulation and clot retraction.
Pleomorphic:
Occurs in various forms.
Polycythemia:
An increase in the total red blood cell mass in the blood.
Polyostotic fibrous dysplasia:
Fibrous dysplasia affecting several or many bones.
Port wine stain:
A unique type of hemangioma consisting of superficial and deep dilated capillaries in the skin, which produces reddish to purplish discoloration of the skin.
Postoperative maxillary cyst:
An intrabony cyst located near the floor of the maxillary sinus lined by pseudostratified ciliated columnar epithelium, caused by implantation of normal mucus-secreting sinus epithelium during previous surgery.
Predilection:
A disposition in favor of something; preference.
Premalignant:
Dysplastic lesions that show histologic change in epithelium characterized by a combination of individual cell and architectural alterations.
Premature eruption:
Teeth present at birth or shortly after; eruption of permanent teeth after premature loss of preceding deciduous teeth.
Primary osseous carcinoma:
A squamous cell carcinoma within the mandible or maxilla with no indication that it originated from surface epithelium or that it metastasized from another site.
Primary tumor:
The original tumor; the source of metastasis.
Prolifertion:
The multiplication of cells.
Proliferative verrucous leukoplakia:
Diffuse white and/ or papillary area of the mucosa caused by varying degrees of epithelial hyperplasia; it has the potential to develop into verrucous carcinoma or well- differentiated squamous cell carcinoma.
Pseudoepitheliomatous hyperplasia:
Excessively elongated rete pegs composed of normal keratinocytes that extend into the immediately adjacent connective tissue, giving a false impression of a squamous cell carcinoma.
Pulpal abscess:
An inflammation of the dental pulp, associated with a circumscribed collection of necrotic tissue and pus arising from breakdown of leukocytes and bacteria, sometimes walled off with connective tissue.
Pulpal calcifications:
Calcifications within the dental pulp.
Pulpal necrosis:
A term applied to pulp tissue that is no longer living, may be partial or complete.
Pulpitis:
An inflammation of the pulpal tissue that may be acute or chronic with or without symptoms, and reversible or irreversible.
Pulp stone:
Spherical calcification within the dental pulp lying free or attached to the pulpal surface of the tooth.
Punched out radiolucency:
Small areas of radioluency.
Purpura:
A group of disorders characterized by purplish or brownish-red discolorations caused by bleeding into the skin or tissues.
Purulent:
Containing pus.
Pustule:
Variously sized circumscribed elevations containing pus.
Pyogenic granuloma:
Fast-growing reactive proliferation of endothelial cells commonly on the gingiva and usually in response to chronic irritation.
Radiation therapy:
The careful use of high-energy radiation to treat cancer; one of several treatments used to treat cancer by itself or in combination with other forms of treatment, most often
surgery or chemotherapy.
Radicular cyst:
An odontogenic cyst of inflammatory origin that is preceded by a chronic periapical granuloma and stimulation of rests of malassez present in the periodontal membrane.
Radiolucent:
The black or dark areas in a radiograph that result from the ability of radiant energy to pass through the structurLess dense structures (e.g., the pulp) are radiolucent.
Radiopaque:
The white or clear appearance in a radiograph that results from the inability of radiant energy to pass through a structurThe more dense the structure (i.e., amalgam restorations), the whiter it appears in the radiograph.
Recessive:
In genetics, a trait or characteristic manifested clinically with a double gene dose in autosomic chromosomes or with a single dose in males if the trait is x-linked.
Repair:
The restoration of damaged or diseased tissues.
Regional odontodysplasia:
A developmental-disturbance of several adjacent teeth in which the enamel and dentin are thin and irregular and fail to adequately mineralize; surrounding soft tissue is hyperplastic and contains focal accumulations of spherical calcifications and odontogenic rests.
Residual cyst:
A cyst that remains at the site of a previously extracted tooth.
Rests of dental lamina:
Dental lamina in its post functional period becomes disrupted into a series of small islands and strands of epithelium.
Rests of serres:
Rests of dental lamina epithelium in which the cytoplasm appears clear or transparent due to an accumulation of glycogen.
Retrocuspid papilla:
A sessile nodule on the gingival margin of the lingual aspect of the mandibular cuspids.
Reversible pulpitis:
Mild inflammation of the tooth pulp caused by caries encroaching on the pulp.
Rhabdomyosarcoma:
Rare, rapidly growing malignant neoplasm of striated muscle that occurs in three histologic patterns (embryonal, alveolar, and pleomorphic); all have a poor prognosis.
Rheumatoid factor:
A protein, an immunoglobulin m (IGM), found in serum and detectable on laboratory tests. It is associated with rheumatoid
Ribonucleic acid:
RNA; single strands of polynucleotides found in all cells; different types of RNA have different functions in the production
Ribosome:
The cytoplasmic organelles in which proteins are formed based on the genetic code provided by RNA.
Romberg syndrome:
A characteristic loss in the soft tissues below the skin, usually on one side of the face; in some severe cases, the underlying bone is also effected.
Rootless teeth:
A hereditary defect in dentin formation in which the coronal dentin and tooth color is normal; the root dentin is abnormal with a gnarled pattern and associated shortened and tapered roots.
Root resorption:
Breakdown or destruction of root structure; loss of root structurThe apex of the tooth appears shortened or blunted and irregularly shaped.
Sarcoma:
- A malignant growth of cells of embryonic connective tissue origin.
- This condition is highly capable of infiltration and metastasis.
Scalloping:
A radiolucent lesion that extends between the roots; fluted border.
Sequestrum:
A fragment of dead bone separated from healthy bone as a result of injury or disease.
Serous:
A substance having a watery consistency; relating to serum.
Schwannoma:
Well-demarcated, benign lesion consisting of a fibroblastic proliferation of the nerve sheath cell (schwann cell) producing distinctive patterns referred to as antoni a and antoni b tissue.
Sessile:
Describing the base of a lesion that is flat or broad.
Sialo-odontogenic cyst:
An unusually large solitary or multilocular odontogenic cyst probably derived from the rests of dental lamina, consisting a stratified squamous epithelium containing numerous mucus-secreting cells.
Sinus tract:
A drainage pathway from a deep focus of acute infection through tissue and/or bone to an opening on the surface.
Smoker’s melanosis:
Irregularly shaped brownish macular pigmentations of oral tissue that are associated with prolonged tobacco smoking.
Snuff pouch:
Altered mucosa that resembles a “pouch” due to the chronically stretched tissue in the area of the placement of smokeless tobacco.
Soft tissue:
The nonbony and non-cartilaginous tissues of the body.
Somatic cells:
All the cells of the human body with the exception of the primitive germ cells (oogonia and spermatogonia).
Spermatogenesis:
The process of formation of spermatozoa (sperm).
Spermatozoon:
The mature masculine germ cell.
Spindle cell carcinoma:
Rare, unusual form of poorly differentiated squamous cell carcinoma consisting of elongated (spindleepithelial cells that resemble a sarcoma.
Squamous cell carcinoma:
Malignant neoplasm of stratified squamous epithelium that is capable of locally destructive growth and distant metastasis.
Squamous odontogenic tumor:
A rare, sometimes multifocal, potentially aggressive lesion derived from odontogenic epithelium, consisting of islands of stratified squamous epithelium that commonly contain microcysts and calcifications in a dense fibrous background.
Stafne cyst:
A developmental concavity of the lingual cortex of the mandible, usually in the third molar area, caused by overextension of an accessory lateral lobe of the submandibular gland, and has the radiographic appearance of a well-circumscribed cystic lesion within the bone, usually below the inferior alveolar canal.
Stain:
Color changes in the teeth.
Stomodeum:
The embryonic structure that becomes the oral cavity.
Sturge weber syndrome:
A rare cevelopmental condition characterized by a vascular birthmark and neurological abnormalities.
Submucous fibrosis:
A whitish-yellow lesion that has a chronic insidious biologic course; result of frequent chewing of the areca or betel nut.
Superficial spreading melanoma:
Most common form of malignant melanoma, initially appearing as an irregularly shaped brown-black macular area with jagged borders and satellite lesions in which areas of nodular melanoma eventually develop.
Supernumerary cusps:
Teeth exhibit extra or supernumerary cusps.
Supernumerary roots:
Extra roots; more than the expected number.
Supernumerary teeth:
In excess of the regular number.
Surgical ciliated cyst of maxilla:
An intrabony cyst located near the floor of the maxillary sinus lined by pseudostratified ciliated columnar epithelium, caused by implantation of normal mucus-secreting sinus epithelium during previous surgery.
Symptom:
A manifestation of disease of which the patient is usually aware and frequently complains.
Syndrome:
A combination of signs and symptoms occurring commonly enough to constitute a distinct clinical entity.
Systemic:
Pertaining to or affecting the body as a whole.
Thrombocyte:
A platelet.
Talon cusp:
A form of supernumerary cusp, which arises from the cingulum portion of the tooth and extends to the incisal edge as a prominent projection of enamel that imparts a t shape.
Thrombocytopenia:
Decrease in the number of platelets in circulating blood.
Taurodont:
A malformed multirooted tooth characterized by an altered crown-to-root ratio, the crown being of normal length, the roots being abnormally short, and the pulp chamber being abnormally large.
Telangiectasia:
The formation of capillaries near the surface of a tissuTelangiectasia may be a sign of hereditary disorder, alcohol abuse, or malignancy in the region.
Therapeutic:
Of or pertaining to therapy or treatment; beneficial. Therapy has as its goal the elimination of control of a disease or other abnormal state.
Thymus:
A lymphoid organ that is situated in the chest. It reaches maximal development at about puberty and then undergoes gradual involution.
Thyroglossal tract cyst:
An odontogenic cyst with the histologic features of a dentigerous cyst that surrounds a tooth’s crown that has erupted through bone but not soft tissue and is clinically visible as a soft fluctuant mass on the alveolar ridges.
T lymphocyte:
A lymphocyte that passes through the thymus before migrating to tissues. The t lymphocyte, also called a t cell, is responsible for cell-mediated immunity.
Tobacco pouch:
Altered mucosa that resembles a “pouch” due to the chronically stretched tissue in the area of the placement of smokeless tobacco.
Tooth discoloration:
Color changes in the teeth.
Torus:
A bony nodule on the hard palate or on the lingual aspect of the premolars.
Translucent:
Somewhat penetrable by rays of light.
Trauma:
A wound or injury; damage produced by an external force.
Traumatic bone cyst:
Asymptomatic intraosseous empty cavity of young patients located primarily within the mandible, lined by a thin loose connective tissue membrane and is adequately treated when blood enters the space during an intraosseous biopsy.
Traumatic neuroma:
Painful nodular proliferation of nerve and fibrous tissue of the nerve sheath resulting from the futile attempt of nerve fibers to reunite with their severed distal portion.
Trisomy:
A pair of chromosomes with an identical extra chromosome.
Treacher collins syndrome:
An autosomal dominant disorder characterized by certain facial features including downward slanting palpebral fissures, sunken cheekbones, receding chin, and malformed ears.
Tumor:
A solid, raised mass that is larger than 1 cm. In diameter and has the dimension of depth. This term also describes a mass consisting of neoplastic cells.
Turner’s tooth:
Enamel hypoplasia of a single tooth, most commonly one of the permanent maxillary incisors or a maxillary or mandibular premolar, resulting from local infection or trauma.
Ulcer:
Loss of surface tissue due to a sloughing of necrotic inflammatory tissue; the defect extends into the underlying lamina propria.
Unilocular:
A term used to describe a radiographic appearance of a single, rounded compartment or locule.
Ventral:
Directed toward or situated on the belly surface (opposite of dorsal)
Verrucous carcinoma:
Distinct, diffuse, papillary, superficial, nonmetastasizing form of well-differentiated squamous cell carcinoma.
Vesicle:
A well-defined lesion of the skin and mucous membranes that resembles a sac, contains fluid, and is less than 1 cm in diameter.
Visceral:
Pertaining to body organs.
Von recklinghausen’s disease:
Autosomal dominant hereditary condition consisting of multiple neurofibromas of the skin and mucosa and associated café au lait spots of the skin with the potential for producing disfigurement and malignant transformation.
Well circumscribed:
Term used to describe a lesion whose borders are specifically defined, and in which one can clearly see the exact margins and extent; well defined (well delineateborder.
White:
The color resulting from commingling of all the rays of the spectrum.
White sponge nevus:
Relatively rare autosomal dominant hereditary condition in which the oral mucosa is white, thickened, and folded.
Whitlow:
An infection involving the distal phalanx of a finger.
Xerophthalmia:
Abnormal dryness of the eyes.
Xerostomia:
Dry mouth.
Yellow:
A color occupying a position in the spectrum between green and orangA yellowish staining of the integument, sclerae, and deeper tissues and the excretions with bile pigments, which are increased in the plasma.
Zygomycosis:
Opportunistic, frequently fulminant, fungal infection that is caused by normally saprobic organisms of the class zygomycetes.
Synonyms
Cheilitis granulomatosis : Meischers syndrome
Hereditary intestinal polyposis : Peutz-jeughers syndrome / Intestinal polyposis with melanin pigmentation.
Ephelis : Labial and oral melanotic macule
Ankyloglossia : Tongue tie
Fissured tongue : Scrotal tongue
Benign migratory glossitis : Geographic tongue/ Erythema migrans
Dens invaginatus : Dens in dente/Dilated composite odantome
Dens evaginatus : Leong’s premolar, occlusal enamel pearl
Talen’s cusp : Dens evaginatus of anterior tooth
Taurodontism : Bull teeth
Amelogenesis imperfecta : Hereditary enamel dysplasia
Turner’s teeth/Turners hypoplasia : Enamel hypoplasia due to local infection on trauma.
Huchinson’s teeth : Enamel hypoplasia due to congenial syphilis.
Dentinogenesis imperfecta : Hereditary opalescent dentin
Dentin dysplasia : Root less teeth
Regional odontodysplasia : Odontogenic imperfecta/ Ghost teeth
Ankylosed deciduous teeth : Submerged teeth
Median anterior maxillary cyst : Naso palatine duct cyst/ Incisive canal cyst
Palatal cyst of neonate : Epsteins pearl/ Bohn’s nodules
Keratoanthoma : Self healing carcinoma
Intraepithelial carcinoma : Carcinoma in situ
Basal cell carcinoma : Rodent ulcer
Epidermoid carcinoma : Squamous cell carcinoma
Peripheral ossifying fibroma : Peripheral odontogenic fibroma or calcifying/ossifying fibroid epulis.
Peripheral giant cell granuloma : Giant cells epulis /Osteoclastoma /peripheral giant cell tumor
Hemangioma : Vascular naevus.
Kaposis sarcoma : Multiple idiopathic hemorrhagic sarcoma of Kaposi
Ewing’s sarcoma : Round cell sarcoma
African jaw lymphoma : Burkitts lymphoma
Multiple myeloma : Plasma cell myeloma/ plasmacytoma
Traumatic neuroma : Amputation neuroma
Neurofibroma : Neurofibromatosis/Von Reckling hausens disease of skin/Fibrosa molluscum.
Pleomorphic adenoma : Mixed tumor
Warthins tumor : Papillary cystadenoma lymphomatosum or adeno lymphoma
Sjogren’s syndrome : Sicca syndrome
Adenoid cystic carcinoma : Cylindroma/Baseloid mixed tumor
Dentigerous cyst : Follicular cyst
Radicular cyst : Periapical cyst/Apical periodontal cyst
Calcifying epithelial odontogenic cyst : Gorlin cyst
Enameloma : Enamel drop/Enamel pearl
Ameloblastoma : Adamantinoma.
Calcifiying epithelial odontogenic tumor : Pindborg tumor
Periapical cemental dysplasia : Cementoma/Cementoblastoma / periapical fibrous dysplasia
Internal resorption : Pink tooth of mummery/odontoclastoma
Hypercementosis : Cemental hyperplasia
Hereford’s syndrome : Uveo parotid fever
Leprosy : Hanson’s disease
Tetanus : Lock jaw
Syphilis : Lues
Noma : Cancrum oris/ Gangrenous stomatitis.
Herpes simplex : Acute herpetic gingivostomatitis/ Fever blisters/ Cold sores
Aphthous ulcers : Canker sores
Herpangina : Aphthous pharyngitis/ Vesicular pharyngitis
Measles : Rubeola
Mikulicz’s disease : Benign lymphoepithelial lesion
Actinomycosis : Lumpy jaw
German measles : Rubella
Chicken pox : Varicella
Herpes zoster : Shingles
Mumps : Epidemic parotitis
Poliomyelitis : Infantile paralysis
Candidiasis : Candidosis/Moniliasis
Focal reversiblle pulpitis : Pulp hyperemia
Pulp polyp : Chronic hyperplastic pulpitis
Periapical granuloma : Apical periodontitis
Periapical abscess : Dentoalveolar abscess/Alveolar abscess
Condensing osteitis : Chronic focal sclerosing osteomyelitis
Gare’s osteomyelitis : Chronic osteomyelitis with proliferative periostitis
Cellulites : Phlegmon
Traumatic cyst : Solitary bone cyst/hemorrhagic cyst
Denture sore mouth : Denture stomatitis
Epulis fissuratum : Inflammatory fibrous hyperplasia
Angular cheilitis : Perleche
Mucocele : Mucous retention cyst/ cyst of pregregor
Acrodynia : Pink disease
Angioneurotic edema : Angioedema/bion/urticaria
Contact stomatitis & dermatitis : Stomatitis and dermatitis venenata
Osteomalacia : Adult rickets
Osteogenesis imperfecta : Brittle bones/ Lobsteins disease
Cleidocranial dysplasia : Mariae & sainten’s disease, mutational dysostosis
Marfans syndrome : Arachnodactyly
Downs syndrome : Mongolism
Osteoporosis : Marble bone disease
Paget’s disease : Osteitis deformans
Cherubism : Familial fibrous dysplasia of the jaws
Ankylosis : Hypomobility
Pernicious anemia : Primary anaemia, Addison’s anaemia
Thalassemia : Cooleys anemia, Erythroblastic anaemia
Polycythemia vera : Osler’s disease
Agranulocytosis : Granulocytopenia/Malignant leukopenia
Infectious mononucleosis : Glandular fever/Kissings disease
Hemophilia : Bleeders disease, disease of the hamburgs
Von wille brands disease : Pseudohemophilia/ vascular purpura
ANUG : Vincents infection/Trench mouth
Periodontitis : Periodontoclasia
Juvenile periodontitis : Periodontosis
White spongy nerves : Cannon’s disease
Systemic sclerosis : Scleroderma
Trigeminal neuralgia : Tic doulereux/ Fothergill’s disease.
Auriculotemporal syndrome : Frey’s syndrome.
Bell’s palsy : Facial paralysis
Plummer vinson’s syndrome : Syderophenic Dysphagia
Cushings syndrome : Hypercontiscalism
Mata aphthous ulcers : Suttons disease
Cheek bite/lip bite : Morsicato buccaru
Florid osseous dysplasia : Sclerotic cemental masses
Spindle cell carcinoma : Lane tumor
Acute adrenal insufficiency : Water hawe – Friderichsen syndrome
Rheumatoid arthritis in children : Still’s disease.
Common Sites
Fordyce’s granules : Bilaterally on mucosa of cheeks opposite the molar teeth.
Static bone cyst : Between mandibular canal & inferior border of mandible.
Talon cusp : Maxillary or Mandibular permanent incisor
Dens in dente : Permanent maxillary lateral incisors
Dens evaginatus : Between Buccal and lingual cups of premolar
Globulomaxillary cyst : Between maxillary lateral incisor and cuspid teeth
Nasoalveolar cyst : Near the attachment of all over the maxilla
Epsteins pearls : Linearly along the median raphe of hard palate
Bohn’s nodules : Scattered over hard palatMost numerous along the function of hard and soft palate
Branchial cleft cyst : Lateral aspect of neck
Thyroglossal cyst : Midline
Basal cell carcinoma : Middle third of face
Pleomorphic adenoma : Parotid gland
Primordial cyst : Retained, erupted deciduous tooth
Dentigerous cyst : Mandibular and maxillary third molars and maxillary cuspid areas
Enameloma : Near or in the bifurcation or trifurcation of roots of teeth on root surface near CEJ
Ameloblastoma Mandibular molar-ramus area
Pindborg’s tumor : Unerupted of impacted tooth
omposite complete odontoma : Posterior jaws
Composite compound odontoma : Anterior maxilla
Papilloma : Tongue
Keratoacanthoma : Lips
Intra oral carcinoma : Tongue
Intra oral carcinoma : Tongue
Most rapidly metastasing tumor : African Burkitt jaw lymphoma
Taurodontism : Permanent or deciduous molars
Missing permanent tooth : Third molars
Congenitally missing permanent tooth: Maxillary lateral and mandibular second premolar next to third molars in order
Commonly missing deciduous tooth : Upper lateral incisor
Most common natal and neonatal tooth: Deciduous mandibular central incisor
Commonly submerged tooth : Mandibular deciduous second molar
Common benign neoplasm : Mandibular deciduous second molar
Originating from oral epithelium : Fibroma
Adenomatoid odontogenic tumor : Maxillary canine region
Retrocuspid papilla : Mandibular canine
Turners hypoplasia : Maxillary incisor
Odontodysplasia : Maxillary Permanent Central Incisor
Oral papilloma : Tongue
Keratoacanthoma : Cheeks
Inter oral nevi : Hard palate
Labial melanotic macule : Lower lip near midline
Focal epithelial hyperplasia : Lower lip
Facial hemihypertrophy : Permanent canine
Carcinoma of gingiva : Mandibular edentulous gingiva
Spindle cell carcinoma : Lower lip
Giant cell fibroma : Gingiva
Oral melanoma : Palate and maxillary gingiva
Haemangioma : Lips
Vermiciform xanthoma : Alveolar ridge
Intra oral lymphangioma : Tongue
Congenital epulis of new born : Anterior maxillary gingiva pigmented ameloblast – maxilla
Chondroma : Anterior maxilla
Benign osteoblastoma : Vertebral column
Granular cell myloblastoma : Tongue
Oral soft tissue osteoma : Tongue
Rhabdomyoma : Tongue
Central giant cell granuloma : Anterior mandible
Peripheral giant cell granuloma : Mandible anterior to molars
Peripheral ossifying fibroma : Interdental papilla
Syndromes
Albright’s syndrome:
Severe form of polystotic fibrous dysplasia nearly involving all bones in the skeleton and accompanied by pigmented lesions of the skin and in addition, endocrine disturbances of varying types.
Aldrich syndrome:
Thrombocytopenic purpura, eczema usually beginning on the face, and a markedly increased susceptibility to infection.
Apert syndrome:
Craniosynostosis along with syndacyfly.
Ascher’s syndrome:
Acquired double lip in association with blepharochalasis and non-toxic thyroid enlargement.
Auriculo temporal syndrome/Frey’s syndrome:
Flushing and sweating of the involved side of the face, chiefly in the temporal area, during eating, profuse lacrimation while eating spicy/hot food (crocodile tears).
Baby bottle syndrome:
Nursing bottle caries
Behcet’s syndrome:
Recurrent oral ulcers, recurrent genital ulcers and ocular inflammation.
Bingneel syndrome:
Hyperglobinemia with CNS involvement or a toxic infectious basis.
Beckwith wiedmann syndrome:
Macroglossia, neonatal hypoglycemia and umbilical hernia.
Chediak higashi syndrome:
Oculocutaneos albinism, photophobia, nystagmus and recurrent infections. Oral ulcers, severe gingivitis and glossitis.
Carotid artery syndrome:
In which pressure exerted by either a deviant styloid process or an ossified ligament causes impingement on the internal or external carotid arteries between which the styloid process normally lies.
Costens syndrome:
Impairment of hearing, tinnitus, otalgia, dizziness, headache, a burning sensation in the throat, tongue side and nose due to temperomandibular joint dysfunction.
Cowdens syndrome:
(Multiple Hamartoma and Neoplasia Syndromfacial trichilemmomas associated with GI tract, thyroid, CNS and musculo skeletal abnormalities as well as oral lesions.
Cleft face syndrome:
Hypertelorism, mediancleft of premaxilla and palate cranium bifidumoccultum. Crest syndrome:
Calcinosis cutis, Raynaud’s phenomenon, oesophageal dysfunction, sclerodactyly and talangiectasia.
Down’s syndrome:
Trisomy of 21st chromosome
Clinical features:
- Flat face, large anterior fontanel, open sutures, epicanthal folds, open mouth, frequent pragnathion, sexual under development, hypermobility of faints oral manifestation: macroglossia, fissured tongue, high arched palate microdontia, enamel hyperplasia.
Eagle’s syndrome:
Elongation of styloid process or ossificate and the stylohyoid ligament causing dysphagia, sore throat, otalgia, glossodynia, headache, vago orofacial pain or pain along the distribution of the internal and external carotid arteries.
Ehler’s danlos syndrome:
Group of hereditary disorder of connective tissue – hyperelasticity of skin, hyperex tensibility of joints, fragilities of skin and blood vessels resulting in excessive bruising as well as defective healing of skin wounds.
Fanconi’s syndrome:
Congenital and sometimes familial aplastic anemia associated with a variety of other congenital objects including bone abnormalities, microcephaly, hypogenitalism and a generalized brown pigmentation of the skin.
Floppy infant syndrome:
Generalised weakness so that their bodies hang simply with inability to sit, stand or walk; hypotonia involves muscles of face, tongue as well.
Gardners syndrome:
Multiple polypsis of large intestine, osteomas of the bones, multiple epidermoid or sebaceous cysts of the skin and impacted supernumerary and permanent teeth.
Goltz gorlin syndrome:
Relative focal absence of the dermis associated with herniation of the subcutaneous fat into the defects. skin atrophy, streaky pigmentation and telangiectasia, multiple papillomas of the mucosa, anomalies of the extremities including syndactyly, polydactyly and adactyly.
Sjogren’s syndrome:
Keratoconjuctivitis sicca, xerostomia and rheumatoid arthritis.
Grinspan’s syndrome:
Lichen planus, diabetes mellitus, vascular hypertension
Heerfordt’s syndrome:
Form of sarcoidosis in which characteristically there is firm, painless, usually bilateral enlargement of the parotid glands, accompanied by inflammation of the uveal tracts, of the eye and cranial nerve involvement.
Horner’s syndrome:
- Miosis
- Ptosis
- Anhidrosis and vasodilation of face.
- Horner’s syndrome (sphenopalatine neuralgia, cluster headach- is characterised by unilateral paroxysms of intense pain in the origin of the eyes, the maxilla, the ear and mastoid, base of the nose, beneath the zygoma,
Hurlers syndrome:
Disturbances of mucopolysaccharide metabolism.
James ramsay hunt’s syndrome:
Zoster infection of the geniculate ganglion with involvement of the external ear and oral mucosa.
Clinical features:
- Facial paralysis as well pain of the external auditory meatus and pinna of the ear, vesicular eruptions in oral cavity and nasopharynx with hoarseness, tinnitis, vertigo.
Jaw cyst- basal cell naevous bifid rib syndrome:
- Cutaneous anomalies: Multiple basal cell carcinomas palmar pitting, plantar keratosis, dermal calcinosis.
- Dental osseous anomalies: Multiple odontogenic keratocysts mandibular prognathism, rib anomalies, vertebral anomalies and brachymetacarpalism.
- Ophthalmolgic abnormalities: Hypertelorism, dystopia canthorum, congenital blindness, and internal strabism.
- Neurologic anomalies: Mental retardation, ductal calcification agenesis of corpus callosum, congenital hydrocephalus.
- Sexual abnormalities: Hypogonadism.
Marfan syndrome:
Disease of connective tissue gelatin to a defective organization of collagen.
Clinical features:
- Excessive length of tubular bones resulting in blichostenomalia arachnodactly.
- Shape of skull and face- long narrow, hyperextensibility of joints action habitual dislocations, kyphosis or scoliosis and flat foot high arched palate, bifid uvula.
Melkerson rosenthal syndrome:
Recurrent attacks of facial paralysis, associated with multiple episodes of non pitting, non inflammatory pain less edema of the face, chielitis granulomatosa, with fissured tongue or lingua plication.
Myofacial pain – dysfunction syndrome:
Four cardinal signs and symptoms:
- Pain
- Muscle tenderness
- Limitations of jaw motion.
- Negative disease characteristics
- Absence of clinical roentgenographic or biochemical evidence of organic changes in the joint itself
- Lack of tenderness in the joint when it is palpitated through the external auditory meatus.
Papillon – lefevre syndrome:
Severe destruction of alveolar bone involving both the deciduous and permanent dentitions.
- Characteristic skin lesions – hyperparakeratosis palmo plantar, generalized hypersiderosis, very fine body hair, rectus dirty colored skin.
Pierre robin syndrome:
- Cleft palate, micrognathia and glossoptosis.
- Plummer vinsons syndrome:
- One of the manifestation of iron deficiency anaemia.
- Cracks or fissures at corner of the mouth.
- Lesson tinted pallor of skin.
- A smooth red painful tongue with atrophy of the filiform and later the fungi form papilla.
- Dysphagia.
- Koilonychia.
Para-trigeminal neuralgia/Raeder’s syndrome:
Severe headache or pain the area of the trigeminal distribution with signs of ocular sympathetic paralysis.
Reiters syndrome:
Tetrad of urethritis, arthritis, conjunctivitis and mucocutaneous lesions.
Rubinstein – Taybi syndrome:
Developmental retardation, broad thumbs and great toes, delayed on incomplete descent of the testes in males, talons cusp.
Steven Johnson’s syndrome:
Severe bullous form of erythema multiforme with wide spread involvement typically including skin, oral cavity, eyes and genitalia.
Treachers collins syndrome:
- Antimongaloid palpebral fissures
- Malformation of external ear
- Hypoplasia of facial bones
- Macrostomia, high palate and malocclusion
- Blind fistulas
Vander wounds syndrome:
Association of pits of lower lip and cleft lip/cleft palate.
Peutzjeugher’s syndrome:
Small intestinal polyposis associated with malanosis of the oral mucous membrane occurs.
Radiographic Appearances
Dentin dysplasia : Thistle tube appearance (Type II)
Odontodysplasia : Ghost appearance
Globulomaxillary cyst : Pear shaped radiolucent area between roots of lateral and cuspid.
Peripheral giant cell granuloma : Peripheral cuffing of bone
Aneurismal bone cyst : Honey comb/soap bubble appearance
Chondroma : Mottled appearance
Ewing’s sarcoma : Onion skin appearance
Osteosarcoma : Sunburst appearance
Multiple myeloma : Punched out areas
Sjogren’s syndrome : Cherry drop blossom or branchless fruit laden tree effect
Pindborg tumor : Driven snow appearance
Odeontogenic myxoma : Mottled or honey comb appearance
Chronic diffuse sclerosing osteomyelitis : Cotton wool appearance
Pagets disease : Cotton wool appearance
Monostotic fibrous dysplasia: Ground glass or ‘Peaud’ orange appearance
Hyperparathyrodism : Ground glass appearance
Thalassemia : Hair on end appearance/Salt pepper effect
Sickle cell anaemia : Hair on end appearance
Hemangioma : Sun burst appearance and honey comb appearance
Eosonophilic granuloma : Floating teeth.
Histological Appearances
Malignant melanoma : Pagetoid manner
Junctional nerves : Abtropfung or chopping off effect
Central giant cell granuloma : Whorled appearance
Multiple myeloma : Cart wheel or checker board pattern
Adenoid cystic carcinoma : Cribriform honey comb on swiss cheese pattern
Primordial cyst: Picket fence or tomb stone pattern.
Familial benign chronic pemphigus: Brick wall effect.
Ameloblastoma:
- Histologic forms
- Follicular
- Plexiform
- Acanthomatous
- Granulomatous cell type
- Basal cell type.
Garre’s osteomyelitis : Retiform pattern
Chronic diffuse sclerosing osteomyelitis : Mosaic pattern
Pagets disease : Mosaic bone and jig saw puzzle appearance
Radicular dentin dysplasia : Lava flowing around boulders
Monostotic fibrous dysplasia : ‘C’ shaped or Chinese character shaped.
Familial benign chronic pemphigus: Diploidated prick well appearance
Lichen planus : Saw tooth appearance
Herpes simplex : Balooning degeneration
Burkitt’s lymphoma : Starry sky appearance.
Cells And Bodies Associated With Some Conditions
Russels bodies : Periapical granuloma
Rushton bodies : Radicular cyst
Target cells and safety pin cells : Thalassemia
Tzank cells : Pemphigus, herpes
LE cells : Lupus erythematosis.
Anitschkow cells : Aphthous ulcer
Lipschutz bodies : Herpes
Lepra cells : Leprosy
Ghost cells : Odantoma
Amyloid bodies and Liesegang rings : Pindborg tumor
Epimyothelial islands : Sjogrens syndrome/ Mikulicz disease
Hyaline cells : Pleomorphic adenoma
Reed – steinberg cells : Hodgkins disease/mycosis
fungoides/infectious mononucleosis
Clear or gorgoyle cells and Hurlers cells : Hurlers syndrome
Reilly bodies (cells of origin – fibroblasts)
Racquet/ Ribbon/ Strap cell : Pleomorphic rhabdomyosarcoma
Angulate body cell : Granular cell myoblastoma
Arbikosor cells : Myeloblastoma
Asteroid bodies : Sporotrichosis
Cystoid and civette bodies : Lichen planus
Corps and rounds : Keratosis follicularis
Carpet tack extensions : Erythema multiforme and lupus erythematosis
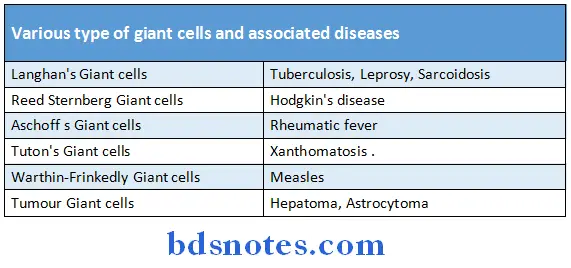
Classifications
1. Classification of Cysts of Jaws
- Odontogenic Cysts
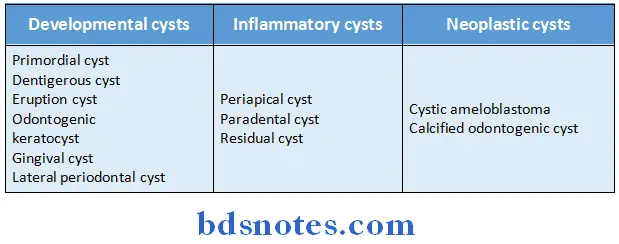
- Non Odontogenic Cyst
- Median mandibular cyst
- Median palatine cyst
- Nasopalatine cyst
- Nasolabial cyst
- Globulo maxillary cyst
- Pseudocysts
- Residual cyst
- These cysts do not contain epithelial linings.
- Aneurismal bone cyst
- Traumatic bone cyst
- Static bone cyst/Stafne’s cyst.
- Soft Tissue Cysts
- Branchial cysts
- Dermoid cyst
- Thyroglossal cyst
2. Classification of Salivary Gland Tumours
WHO classification:
- Epithelial Tumours
- Adenomas
- Pleomorphic adenoma
- Monomorphic adenomas
- Adenolymphoma (Warthin’s humour)
- Oxyphil adenoma
- Others:
- Basal cell adenoma
- Clear cell adenoma
- Tubular adenoma
- Alveolar adenoma
- Trabecular adenoma
- Canalicular adenoma
- Carcinomas
- Mucoepidermoid carcinoma
- Acinic cell carcinoma
- Adenoid cystic carcinoma
- Clear cell carcinoma
- Adenocarcinoma
- Epidermoid carcinoma
- Undifferentiated carcinoma
- Carcinoma of pleomorphic adenoma.
- Adenomas
Connective tissue tumours:
-
- Lymphomas
- Sarcomas
3. Classification of Pulpal Diseases:
1. Pulpitis
- Acute
- Chronic
2. Apical Periodontitis
- Acute
- Chronic
3. Periapical abscess
4. Periapical granuloma
5. Periodontal cyst
6. Osteomyelitis
- Acute
- Chronic
- Focal
- Diffuse
- Periostitis
7. Cellulites
8. Abscess
9. Septicemia, bacteremia
4. Fractures of Teeth:
Classification:
Class 1
- Simple fracture of crown, involving no or little dentin.
Class 2
- Fracture with involvement of dentin but no pulp.
Class 3
- Considerable dentin is involved with pulpal exposur
Class 4
- Traumatized tooth becomes non-vital with or without loss of crown structures.
Class 5
- Teeth lost due to fracture.
Class 6
- Fracture of root without loss of crown.
Class 7
- Displacement of tooth without fracture of crown or root.
Class 8
- Fracture of “crown en masse” and its replacement.
Class 9
- Traumatic injuries to deciduous teeth.
5. Stains:
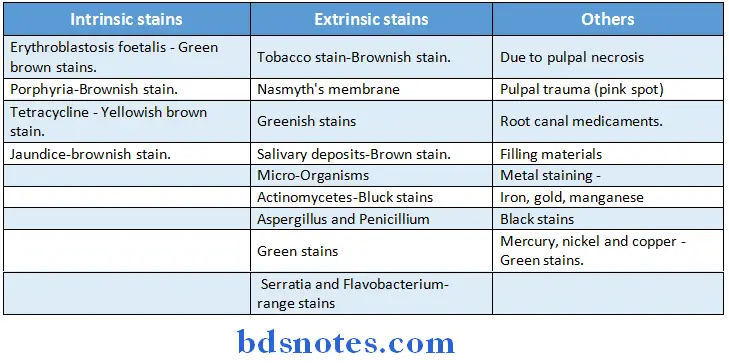
6. Diseases of Bones:
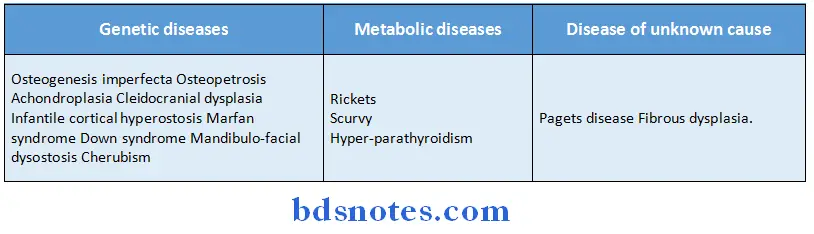
7. Caries activity tests:
- Snyder’s test (Media used is bactopeptone, sugar and sugar).
- Albans test (Same media is used for culture of bacteria).
- Diseases of unknown
- Salivary reductase test: Diazoresorcinol dye is used for measuring activity of salivary reductase enzyme.
- Buffer capacity test of saliva.
- Lactobacillus colony count test (tomato peptone agar culture media is used).
- Fosdick calcium dissolution test (it measures the activity of bacteria to dissolve enamel powder).
8. Diseases of temperomandibular joint:
- Developmental disturbances
- Mandibular condyle
- Aplasia and Hypoplasia and Hypoplasia
- Traumatic disturbances
- Luxation and subluxation
- Ankylosis
- Injuries of articular disc
- Fracture of the condyle
- Inflammatory disturbances
- Arthritis due to specific infection
- Rheumatoid arthritis
- Osteoarthritis
- Extra articular disturbances
- MPDS
- Neoplastic disturbances
9. Developmental disturbances classification Jaws:
- Micrognathia
- Macrognathia
- Agnathia
- Facial hymihypertrophy
- Facial hemiatrophy
Lips palate:
- Congenital lip and commisured pit and fistules
- Double lip
- Cleft lip and Cleft palate
- Cheilitis glandurias
- Cheilitis granulomatosa
- Heridatary intestinal polyposis
- Labial and oral melanotic macule
Oral mucosa:
- Fordyce granules
- Focal epithelial hyperplasic
Gingiva:
- Fibromatosis gingiva
- Retrocuspid papilla
Tongue:
- Macroglossia Ankyloglossia
- Cleft tongue
- Fissured tongue
- Median rhomboid glossitis
- Benign migratory glossitis
- Hairy tongue
- Lingual varices
Salivary glands:
- Aplasia
- Xerostomia
- Hyperplasia of palatal glands
- Atresia
- Abberancy
- Stafne cyst
Developmental Disturbances Of Teeth
- Size
- Microdontia
- Macrodontia
- Shape
- Fusion
- Gemination
- Concresence
- Dilacerations
- Talon cusp
- Dens in dente
- Dens evaginatus
- Supernumerary roots
- Number
- Anodontia
- Supernumerary tooth
- Prodecidous dentition
- Post permanent dentition
- Structure
- Amelognosis imperfecta
- Dentinogenesis imperfecta
- Dentin dysplasia
- Regional odanto dysplasia
- Dentin hypocalcificatin
- Growth/eruption
- Premature eruption
- Delayed eruption
- Multiple unerupted teeth
- Embedded and impacted teeth
- Ankyloglosed deciduous teeth and submerged teeth
10. Zones of caries:
Enamel caries:
- Zone 1: Translucent zone
- Zone 2: Dark zone
- Zone 3: The body of the lesion
- Zone 4: Surface zone
Dentinal caries:
- Zone 1: Zone of fatty degeneration of tomes fibres
- Zone 2: Zone of dentinal sclerosis
- Zone 3: Zone of decalcification of dentin
- Zone 4: Zone of bacterial invasion of decalcified but intact dentin
- Zone 5: zone of decomposed dentin.
11. Types of facial and cervical neuralgias:
- Atypical pain or neuralgia
- Geniculate neuralgia
- Migranous neuralgia
- Glossopharyngeal neuralgia
- Occipital neuralgia
- Para-trigeminal neuralgia of reader
- Post herpetic facial neuralgia
- Sphenopalatine ganglion neuralgia
- Superior laryngeal neuralgia
- Trigeminal neuralgia
- Tympanic plexus neuralgia
12. Pains of orofacial region:
Neuralgia:
- Trigeminal neuralgia (Tic douloueux)
- Hepes zoster
- Post herpetic neuralgia
- Geniculate neuralgia
- Glossopharyngeal neuralgia.
Pain of musculoskeletal origin:
- M. P. S
- T. M. J. arthritis
- Stylohyoid eagle’s syndrome.
Vascular diseases:
- Migraine
- Cluster headache
- Carotodynia
- Thrombophlebitis
Generalized pain syndrome:
- Sympathetically maintained pain (Causalgia)
- Phantom pain
- Post-traumatic pain.
Lesions of ear, nose and oral cavity:
- Maxillary sinusitis
- Otitis media
- Pulpitis
- Periapical abscess/pathology
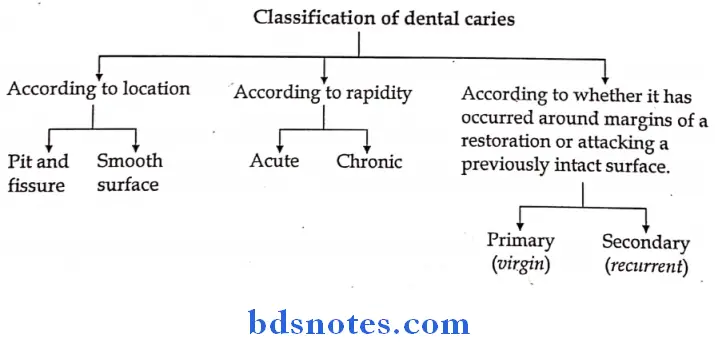
- Supernumerary teeth are associated with
- Cleidocranial dysostasis
- Gardners syndrome
- Cleft palate
- Hallermann – Streiff syndrome
- Median rhomboid glossitis is due to persistence of tuberculum impar.
- Hairy tongue is characterised hypertrophy of filiform papillae.
- Most common developmental disorder affecting the tongue is
abnormally fissured tongue. - Hutchinson’s triad – Intestitial keratitis
- Hypoplasia of incisors and molar teeth
- Eighth nerve deafness
- Talons cusp is associated with – Rubinstein – Taybi syndrome
- Taurodontism – Kleinfilters syndrome
- Teeth that erupts with in 1st month of birth – Neonatal teeth
- Teeth that are present at the line of birth – Natal teeth
- Café au lait spots on skin are seen in
- Albrights syndrome
- Hypothyroidism
- Neurofibromatosis.
- Pathognomic feature of osteogenesis imperfecta – blue sclera
- Green stains frequently seen on children teeth are caused by chromogenic bacteria.
- Taste buds are predominantly located on circumvallate papilla.
- Most common site of basal cell carcinoma – skin of lower lip
- Causative organism of syphilis – Treponema pallidum
- Pigment associated with haemochromatosis – haemosiderin
- Epulis fissuratum is caused by ill fitting dentures
- The structure that most often affected in a child with congenital absence of teeth is – Alveolar bone
- Phaechromocytoma is a tumor of adrenal medulla
- The enamel of the posterior tooth is thickest at occlusal surface
- Mouse eaten furrowed ulcer in oral cavity seen in tuberculosisis
- Adenomeloblastoma is commonly associated with a missing teeth.
- Immunoglobulins
- Highest serum concentration in humans – IgG
- Transmitted through placenta – IgG
- Infectious mononucleosis is caused in oral cavity by Ebstein barr virus.
- Classic example of vascular pain – Migraine
- Epimyoepithelial islands with deposition of eosinophilic hyaline material is characteristic histologic picture of mikulicz’s disease
Sulphur granules in actinomycosis contains colonies of organisms of actinomycosis - Bronze discoloration of oral mucosa – Addisons disease
- Most common malignancy in AIDS – kaposis sarcoma
- Deficiency of Vitamin A involving mucosa and epithelium – Darier’s disease
- Osteitis fibrosis cystica is caused by due to hyperparathyroidism.
- Primary cells which characterize eosinophilic granuloma are histiocytes.
- Most cariogenic carbohydrate – Sucrose
- Chronic diagnosis of candidiasis is confirmed by proliferation of inflamed pulp tissue.
- Clinical diagnosis at candidiasis is confirmed by demonstration of mycelia and in scrapings.
- Clinical significance of sclerotic dentin is that it is resistant to caries spores
- The feature that frequently distinguish herpes zoster from other vesiculobullous eruption is – unilateral occurrence.
- The specific feature of oral candidiasis sometimes seen in otherwise healthy patients is – median rhomboid glossitis.
- Most common extra oral cause of halitosis – chronic sinusitis
- Substances deposited in entire reticuloendothelial system in Gaucher’s disease- kerasin.
- The fungus which has an apparent predilection for blood vessels and is able to penetrate their walls and produce thromboses is – Rhinosporidium thromboses.
- A benign inflammatory reaction of salivary gland tissue which both clinically and histologically mimics salivary glands malignancy – necrotising sialometaplasia.
- Macrognathia of both jaws – Pituitary gigantism
- Baelz’s disease is associated with cheilitis glandularis
- The odontome which resembles anatomy of normal teeth is a compound odontoma.
- Most common salivary gland tumor – pleomorphic adenoma shows slow growth but a tendency to local recurrence after incomplete removal.
- Features of sturge weber disease – hematoma port vine nevi Telangiectasia.
- Sarcoma of soft tissues spread by blood vessels.
- Traumatic bone cyst is treated by opening of the cavity and inducing bleeding.
- Most common intra oral pigmented lesion – Amalgam tattoo
- Epithelium of the oral cavity differs from the epithelial lining of the cyst in stratum granulosum
- The odontogenic tumour frequently found in children and associated with unerupted tooth in the anterior portion of the maxilla is odontogenic adenamatoid tumour.
- Pagets test is done in the examination of a small swelling.
- Most common type of dentigerous cyst – central type
- Cyst that has a highest recurrence rate – odontogenic keratocyst
- Tissue removal for microscopic examination should be immersed immediately in 10% formalin.
- Dysplastic lesions of squamous epithelium occur most often on the floor of the mouth.
- Hyperplastic lingual tonsils may resemble – Squamous cell carcinoma
- Site of attachment of dentigerous cyst to the tooth is – cemento enamel function
- Epstein pearls – small keratin cyst of the new born infant.
- Congenital epulis of new born resembles – granular cell myoblastoma
- Epulis fissuratum resembles – irritational fibroma
- Most common malignancy of oral cavity – squamous cell carcinoma
- Most reliable single histologic criterion for a diagnosis of oral squamous cell carcinoma is invasion.
- Intra oral myloblastomas occur more frequently in the tongue.
- Most common complication of rheumatoid arthritis involving TMJ – Fibrous ankylosis.
- Biochemical abnormality seen in osteogenesis imperfecta is increase in phosphorylase enzyme,
- Most frequent cause of ankylosis of TMJ – Trauma
- Pagets disease – characteristically exhibits either hypercementosis or root resorption.
- Found among geriatric patients.
- Osteitis fibrosa cystica – Amber colored tooth transluscency, blue sclera, and bone fragility with history of previous bone fractures.
- Blue sclera seen in – Marfans syndrome, cherubism, Osteogenesis imperfecta.
- Wormian bones are common in cleidocranial dysplasia.
- Tumor osteoid is seen in – Osteosarcoma
- Dentinogenesis imperfecta is always associated with type I
osteogenesis imperfecta - Blood dyscrasias having racial predilection – Sickle cell anaemia.
- Bence jones proteins are seen in
- Multiple myeloma
- Polycythemia vera
- Leukaemia
- Monros abscess and auspitz sign are characteristic of psoriasis. Pseudorhagades are found in ectodermal dysplasia.
- Forms of erythema multiforme
- Steven Johnson syndrome
- Toxic epidermic necrolysis
- Lyell disease
- The immunological test which is most valuable in differential diagnosis of pemphigus and pemphigoid – Immunoflorescence.
- Psoriosis – Formation of multiple pin point bleeding spots on scratching the skin associated with geographic tongue.
- Function of facial nerve is best tested by whistling.
- Drug of choice in facial nerve palsy – corticosteroids
- Cervical sympathetic paralysis – causes an hydrosis of the
homolateral side of face. - Trigeminalneuralgia most often affects the right side nerve.
- Paralysis of tongue – Glossoplegia.
- Marcus gun phenomenon is a characteristic of jaw winking syndrome
- Charcots triad – intention tremors, Nystagmus and dysorthrosis
- Alarm clock headache is seen in Horton’s syndrome
- Mask like appearance – Systemic sclerosis, Parkinsonism, Bells palsy
- Nerve affected
- Bells palsy – 7th nerve
- Herpes zoster – 5th nerve
- Trigeminal neuralgia – 5th nerve
- Ramsay hunt syndrome – 7th nerve
- Pathologic fracture of maxilla and mandible is seen in
- Bone cyst
- Multiple myeloma
- Giant cell tumor of bone
Developmental Anomalies
- Most common malformation of head and neck region – Cleft lip and cleft palate
- Micrognathia of maxilla is most commonly due to deficiency of premaxillary area.
- Post natal type of mandibular micrognathia is most frequently due to distortion in – TMJ.n
- Most common associated abnormality seen in patients of hemihypertrophy – mental deficiency.
- Most common type of cleft in
- Females – Cleft palate
- Side mostly effected – left side
- Common type of cleft lip – Unilateral complete
- Mildest form of cleft palate – Bifid uvula
- Surgery to close cleft palate – 1/2 year
- Lip pits:
- Commisural lip pits – Elle vancravald syndrome
- Paramedian lip pits – Vander woude syndrome.
- Cheilitis glandularis
- Most sex effected – adult male
- Site – lower lip
- Common form – simple type.
- Most common intra oral site exhibiting melanin pigmentation in peutz-jeughers syndrome – Buccal mucosa
- Facial pigmentation tends to back later in life while oral pigmentation persists.
- Lingual rampant of thyroglossal tract – Foramen caecum.
- The condition in which a normal tooth germ is divided resulting into one normal and one supernumerary tooth is twining.
- Fusion of teeth is more common in deciduous dentition.
- Epstein pearls are most numerous along the mid palatal raphae
- Epithelial lining of Bohn’s module is derived from epithelium of palatal salivary glands
- Most common type of development cyst of maxilla – nasopalatine duct cyst.
- Embedded teeth – unerupted teeth which has last eruption force.
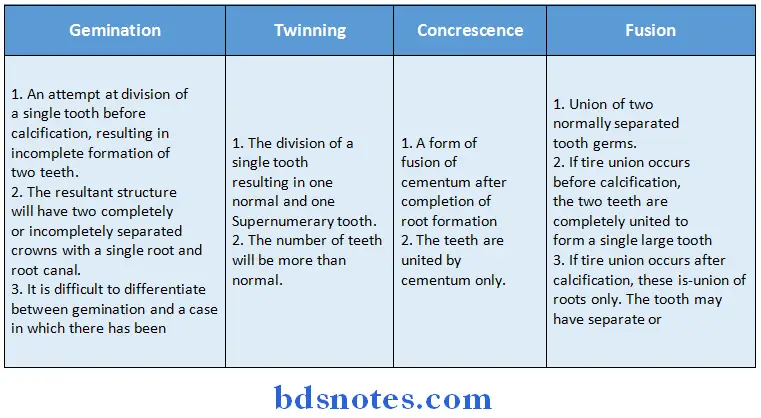
Dentinogenesis imperfecta:
Type 1 and 2:
- Type 1 always occurs in families with Osteogenesis imperfecta. Type 2 dentinogenesis imperfecta cases never occurs in association with Osteogenesis imperfecta.
- The most striking feature of Type and Type II is partial or total precocious obliteration of the pulp chambers and root canals by continued formation of dentin.
Type 3:
- Also known as bradywine type or shell teeth.
- The dentin is extremely thin and the pulp chambers are enormous due to insufficient and defective dentin formation.
- In roentgenograms, the teeth appear as shells of enamel and dentin surrounding extremely large pulp chambers and root canals.
- Dentin dysplasia (rootless teeth) is characterized by normal enamel but atypical dentin formation with abnormal pulpal morphology.
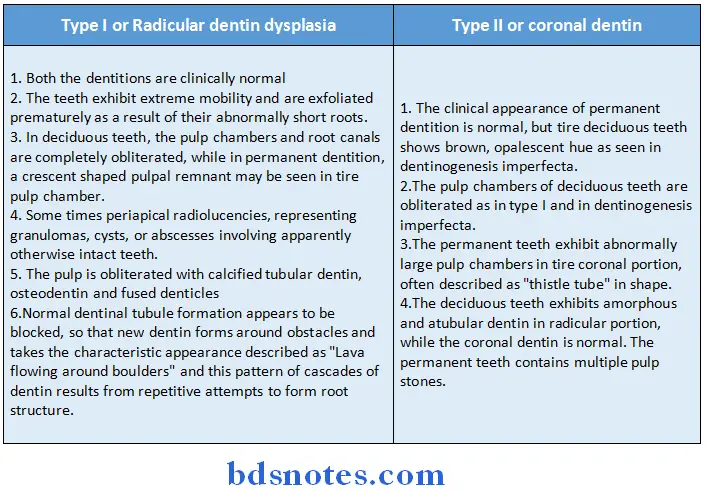
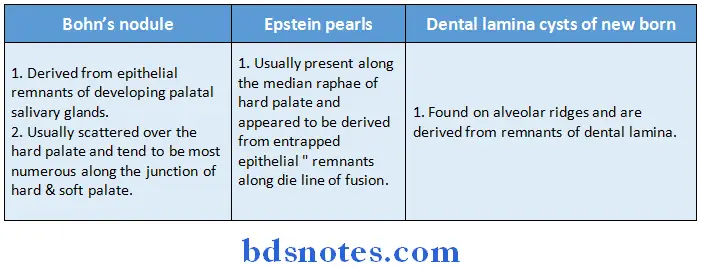
Benign And Malignant Tumours
Premalignant conditions:
- Erosive lichen planus
- Actinic or solar keratosis
- Sideropenic Dysphagia
- Bowens disease or carcinoma in situ.
- Syphilitic glossitis
- DLE
- Dyskeratosis congenital
- Hyperplatic candidiasis.
Premalignant lesions:
- Leukoplakia
- Erythroplakia.
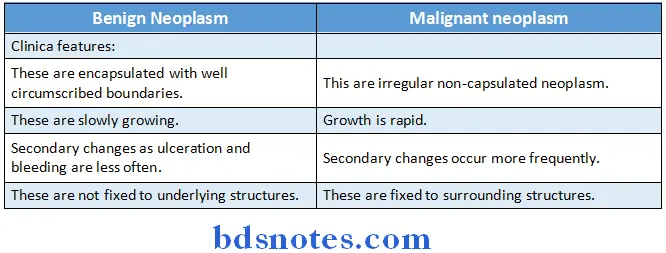
- Multiple oral papillomas are present in focal dermal hypoplasia syndrome
- Essential histopathological feature of oral papilloma is – Proliferation of spinous layer of epithelium in papillary pattern with connective tissue forming the supportive stroma only.
- Clinically and histologically keratocanthoma may closely resemble squamous cell carcinoma
- Sex and age group – Male 50-70 years
- Characteristic histopathological feature of squamous acanthoma is – elevated and or umbilicated epithelial proferation with thickened orthokeratin and spinous cell layer.
- Characteristic features of keratoacanthoma – Elevation of normal epithelium toward the central portion of the lesion with an abrupt change in normal epithelium as hyperplastic antholytic epithelium is reached.
- Most common type of acquired naevus – intradermal naevus
- Chiefly occurring in children – Spindle cell naevus
- Nerve cells are believed to be derived from – neural rest arrangement of nevi cells in alveolar pattern is – Theques.
- Naevus showing maximum risk of transformation into malignant
melanoma – congenital nerves treatment of choice of intra oral nevi – surgical excision - Most frequently suggested etiological agent causing leukoplakia – Tobacco.
- Site most frequently involved – Buccal mucosa
- Most common malignant neoplasm of skin – basal cell carcinoma
- H/F of submucous fibrosis – Epithelial atrophy and loss of rete pegs, Epithelial atypia, hyalinization of connective tissue.
- Most specific factor in sunlight responsible for skin carcinogenesis – UV radiation.
- Most common malignant neoplasia of oral cavity is squamous cell carcinoma
- Most common etiological factor in development of oral carcinoma – smoking.
- Etiology of Burkitts lymphoma – Epstein barr virus
- Kaposis sarcoma is due to cytomegalo virus
- Metastasis from oral carcinoma occurs most commonly to submaxillary lymph nodes.
Lip carcinoma:
-
- Usually begins on – vermillion border of lip
- Most are grade I
- Most significant factor affecting prognosis in patients of carcinoma of tongue is presence of absence of metastasis.
- Recommended treatment for carcinoma of floor of mouth – Radiation therapy.
- Characteristic H/F of various carcinoma – parakeratin lining the clefts with parakeratin plugging.
- Most common initial lesion of carcinoma is ulcer.
Malignant melanoma (MM):
-
- Common type – Nodular melanoma
- Treatment of choice for cutaneous MM – Surgical excision
- Most common benign soft tissue tumor of oral cavity – fibroma
- Pathogenesis for aneurismal bone cyst – change in hemodynamics leading to increased venous pressure causing resorption of surrounding bone.
Lymphangioma:
-
- Common site – Anterior portion of dorsal surface of tongue
- Common type – cavernous
- Treatment of choice – Surgical excision
- Chondroma is composed of hyaline cartilage
- R/F of osteoid osteoma – small ovoid and round radiolucent are surrounded by a rim of sclerotic bone.
- Sarcoma melastasize through blood vessels.
- Burkitts lymphoma is originated from T. lymphocytes
- Treatment of choice – Chemotherapy (Cyclophosphamid)
Multiple myeloma:
-
- Cells of origin closely resembles – plasma cells
- Cause of painuclear halo seen in cells of is due to prominent golgi complex.
- Treatment of choice – Chemotherapy (Malphanx)
- Criteria for diagnosis of epithelial dysplasia in carcinoma include.
- Increased abnormal mitoses
- Individual cell keratinisation.
- Epithelial pearls in the spinous layer
- Alterations in nuclear Cytoplasmic ratio
- Loss of polarity and disorientation of cells
- Hyper chromatism
- Large nucleoli
- Dyskaryosis or nuclear atypism including giant nuclei.
- Poikilokarynosis or division of nuclei without division of cytoplasm
Basilar hyperplasia:
Individual cell keratinisation and epithelial pearl formation is absent in carcinoma in situ or intra epithelial carcinoma.
Usually T1 and most T2 lesions without metastasis are treated by either surgery or radiotherapy. larger T2, T3 and T4 lesions are generally treated by combined approach.
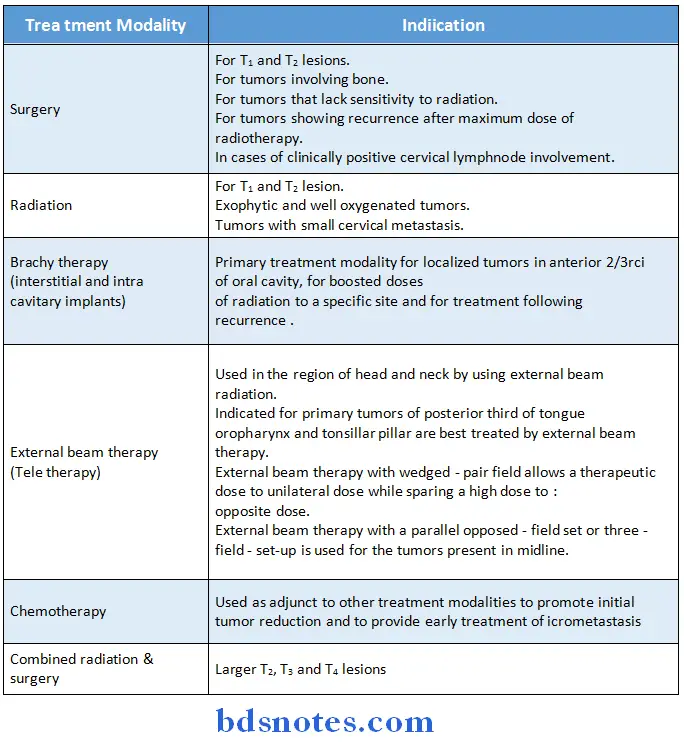
Definition of the TNM categories of malignancy T-primary tumor:
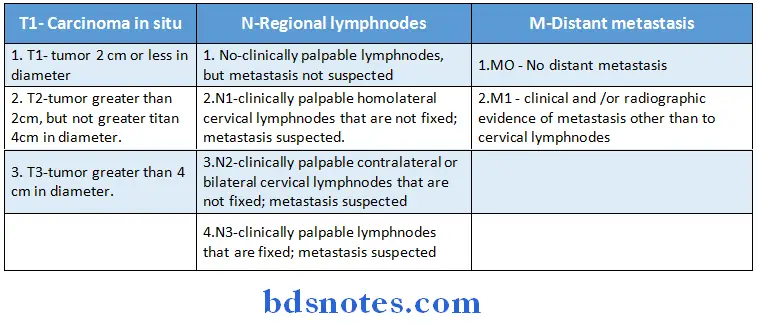
Clinically Leukoplakia is three types:
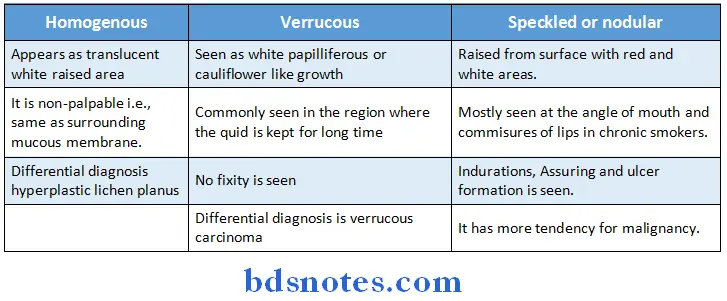
Diseases Of Bones And Joints
Common sites:
- Infantile cortical hyperostasis – mandible
- Pagets disease – sacrum
- Progressive osteolysis – clavicle
- The signs of cransfacial dysostosis is due to early synostosis of the sutures
Clinical features:
- Triangular frontal defect, parrots beak nose, hypertelorism and prognathic mandible.
- Basic defect in Pierre robin syndrome – Arrested development of hypoplasia of mandible.
- Complications – respiratory difficulty
- Bird facies appearances
- Basic defect in Marfan’s syndrome – abnormal solubility of collagen.
Diseases Of Nerves And Muscles
- Ricke’s bone and drill bone are feature of Traumatic myositis ossificans
- Drug of choice of myasthenia gravis – physostigmine
- Most common form of muscular dystrophy – muscular dystrophy of duchenne.
- Inverted – mucous Gunn’s phenomenon is seen in Marin Amats syndrome.
- Causalgia – severe pain which arises after sectioning of peripheral sensory nerve is referred is causalgia.
- Myotonia is failure of muscle relaxation after cessation of voluntary contraction
- Irreversible side effect of phenothiazine therapy
- Orofacial dyskinesia
- Drug found to be most effective in case of periodic migranous neuralgia during acute phasse
- Ergotamine
- Must that most commonly shows tenderness in MPDS is lateral pterygoid.
Diseases Of Skin
- Butterfly shaped cutaneous lesions of face are seen in lupus erythematosis.
- Carpet tack extensions are seen in discoid lupus erythomatosis
- Antinuclear antibodies are seen in systemic lupus
- Erythematous, false positive tests for syphilis – SLE
- Morphea – localized type of systemic sclerosis
- Aerodomatite enteropathic occurs due to deficiency of Zn.
- Fusion of middle portion of upper lip to the maxillary gingival
margin is a feature of – chondro ectodermal dysplasia. - Lichen planus
- Initial symptoms – Pouritis
- Common site – buccal mucosa
- H/F: Saw tooth retepegs and civatte bodies colloid bodies – spinous and basal
- cell layers of epithelium.
- Herald spot is seen in pityriasis rosea
- Cause of acatholysis in pemphigus – autoimmunly
- In leprosy there is pink discoloration of teeth.
Diseases of skin:
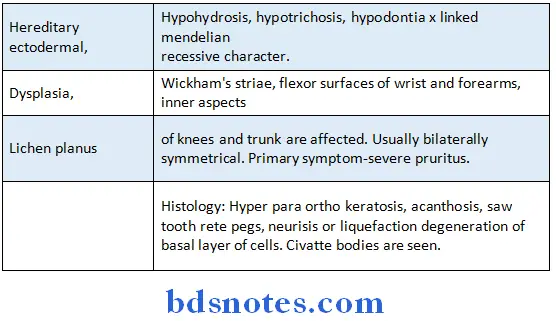
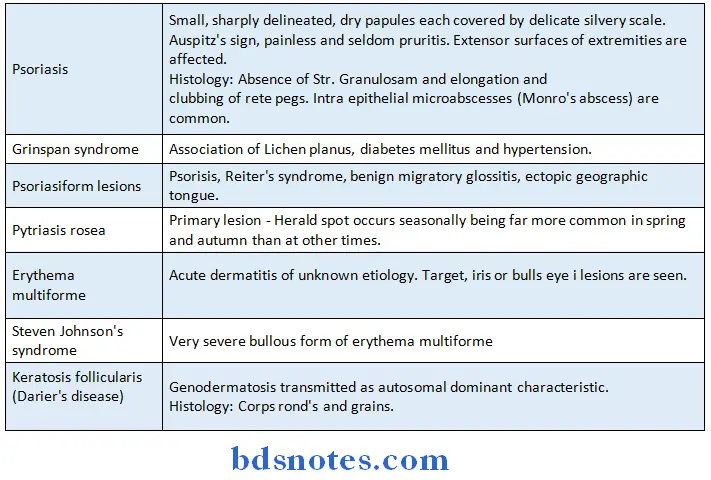
Diseases Of Blood And Blood Forming Organs
- Pernicious anemia:
- Hunters glositis occur due to def of intrinsic factor
- Nervous aberrations occur due to degeneration of posterior and lateral tracts of the apical card
- Constant feature – achlorhydria
- Howell – jolly bodies – RBC containing nuclear remnants
- Characteristic oral manifestation of thalassemia
- Prominence of premaxilla
- Type of anemia – Microcyst hypochromic
- Sickle cell anemia occur due to substitution of valine for glutamic acid of sixth position of ẞglobulin chain.
- Erythroblastosis fetalis
- Chances of infant mentality is high if mother is Rh negative and father is Rh positive.
- Common type of Rh antigen responsible in erythroblastalis fetals
- Positive direct Coomb’s test
- Enamel hypoplasia producing characteristic ‘Rh hump’
- Most common cause of agranulocytases – drugs and chemicals
- Infectious mononucleosis
- Lymph nodes 1st effected – cervical
- Early oral manifestation – palatal petechia
- High titre of serum heterophile antibodies
- Philadelphia chromosome (translocation of chromosome materials occurs between chromosome number 9 and 22) is seen in chronic myeloid leukemia.
- Gingival enlargement seen in leukaemic patient is due to infiltration by leukaemic cells.
- Most common form of leukaemic in children – acute lymphocytic leukemia
- Most common treatment for thrombocytosis is – Radioactive
phosphorus - Extraction method followed in hemophilia – Rubber band method.
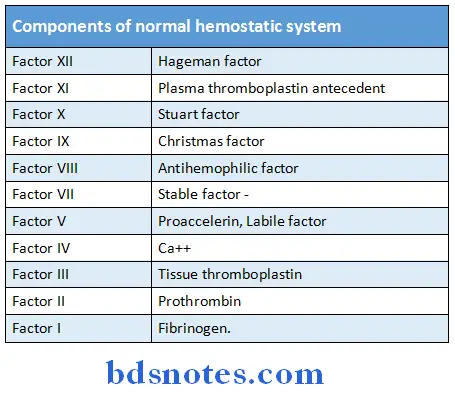
Blood:
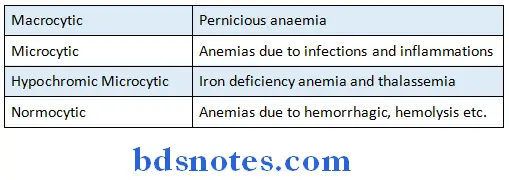
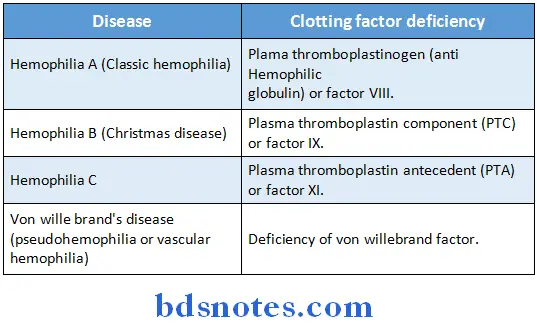
Oral Aspects Of Metabolic Diseases
- Tetany occurs if serum Ca level falls below 8 mg/dl.
- Most frequent type of pathological calcification is dystrophic calcification (Ca salts on deposited in dead or degenerating tissues)
- Hypercalcemia, hyperparathyroidism and hyper vitaminosis may cause – Metastatic calcification.
- Sodium
- Major extra celular cation
- Salivary amylase is activated by chlorine
- Wilsons disease – Deficiency of Copper
- One way substance – Cobalt
- Acrodermatitis eneteropthica – Def of Zn
- Helps in binding in insulin to cell membrane – Cr
- Selenium containing enzyme – glutathione peroxidase
- Optimum fluoride concentration for community water
- Fluoridation – 1.0 ppm
- Amino acid which is considered essential in infants but not in adults is Arginine.
- Gauchers disease
- Results due to disturbance in lipid metabolism there is abnormal deposition of keratin.
- Gauchers cells – Lipid filled histiocytes
- Abnormal storage of spingomyelins is characteristic of Neumann’s pick -disease
Vitamin A:
Essential for normal differentiation of epithelial cells, dental tissue mot frequently effected due to its deficiency – enamel.
Vitamin D:
- Bald tongue of sand with (Vit D def) Anti rachitic vitamin.
- Final step of formation occurs in kidney
- 1st change seen in rickets – cessation of calcification of epiphyseal discs
- osteomalacia – mostly seen in past menopausal females
(intake of fats must be avoided of osteomalacia secondary to malabsorption). - Basic defect seen in Vit D resistant rickets is failure of bone salts to be deposited in cartilage matrix.
- Pulp horns are seen in familial hypophostaemia
- Enzyme deficient in hypophosphatase – alkaline phosphatase
- Substance excreted in urine – Phosphoethanolamine
Vitamin ‘C’ deficiency:
- Most severe changes in teeth – dentin
- Primary bone change in scurvy – failure of osteoblast to form osteoid
- Amino acid that decreases the requirement of niacin- stryptoplasia.
- Biotin in constituent of CoA.
- In Vitamin B6deficiency – Xanthuronic acid is excreted in urine.
- Papillae of tongue most frequently effected in Vit def – Filiform papillae.
- Calciform is secreted by thyroid gland.
- Hyperparathyroidism
- Bone abnormality seen – osteitis fibrosa cystica common cause of secondary hyperparathyroidism – end stage renal
- Epinephrine is secreted by adrenal medulla.
Effects of specific vitamin deficiencies:
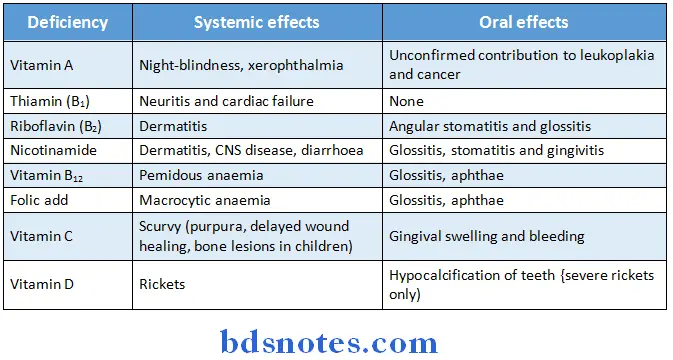
Healing Of Oral Wounds
- Human having most pronounced effect on healing of oral wound is Sterile field
- Fixative used in slide preparation in exfoliate cytology – 95% alcohol.
- Preservative generally used for biopsied specimen – 10% formalin.
- Bone formation in an extraction wound is derived from – undifferentiated cells of periodontal ligament.
- A complication of healing of extraction wound into the which antibiotic ointment with petroleum base has been placed is known as Myospherulosus
- During healing of extraction wound, the epithelium covering the socket is derived from epithelium at the margin of wound.
Cysts And Tumours Of Odontogenic Origin
- Primordial cyst
- It develops in the place of a tooth.
- It develops from stellate reticulum of enamel organ
- It is formed due to accumulation of fluid between reduced enamel epithelium and tooth crown.
- Histological features:
- Ruston bodies found in connective tissue lining
- Most common type odontogenic cyst – Radicular cyst.
- Its epithelial lining is derived from epithelial lining of mallasez.
- Gingival cysts of new born originates from remnants of dental lamina.
- Odontogenic keratocyst
- Cyst having highest recurrent rate
- Histological features (epithelium)
- Corrugated parakeratin or orthokeratin large uniform thickness
Polarized basal layer of cells having picket for or tomb stone appearance o Cholesterol crystals. - Soluble protein level is less than patients serum protein level
- Ameloblastoma
Types:- Follicular – cyst formation is common
- Plexiform
- Granular – shows marked tendency for recurrence shows evidence of metastasis
- Acanthomatous
- Basal cell type
- The loosely arranged polyhedral cells enclosed by cuboidal/columnar cells in follicular ameloblastoma resembles stellate reticulum of enamel organ.
- Treatment of choice for benign cementoblastoma – extraction
- The masses of irregular dentin found in dentinoma are termed or osteodenin.
- Most common odontogenic tumor – compound odontoma
Dentigerous cystic:
Key features:
- Arise in bone and contain the crown of an unerupted tooth which is usually displaced
- Are most frequently associated with unerupted third molars and canines
- Clinical and radiographic features usually provide an accurate preoperative diagnosis but confirmation is histological
- May be mistaken radiographically for an odontogenic keratocyst or ameloblastoma
- Respond to enucleation or marsupialisation and do not recur after treatment.
Odontogenic keratocyst:
Key features:
- Form intraosseously, most frequently in the posterior alveolar ridge or angle of mandible
- May grow round a tooth
- Sometimes multilocular radiographically
- Spread extensively along marrow spaces before expanding the jaw
- Frequently recur after enuclation
- Do not respond to marsupialisation
- Definitive diagnosis only by histopathology although clinical and radiographic features may allow fairly accurate preoperative diagnosis
- May be confused with ameloblastoma or with dentigerous cysts radiographically
- May be part of the jaw cyst/basal cell naevus syndrome.
- Can progress to malignan cell.
Possible reasons for recurrence of keratocysts:
- Thin, fragile linings, difficult to enucleate intact
- Fingerlike cyst extensions into cancellous bone.
- Daughter cysts sometimes present in the wall
- More rapid proliferation of keratocyst epithelium
- Other dental laminal remnants may produce another keratocyst (pseudo-recurrence)
- Inferior standard of surgical treatment.
Ameloblastoma:
Key features:
- Neoplasm of odontogenic epithelium
- The most common odontogenic neoplasm
- Usually presents between ages 30 and 50
- Locally invasive but does not metastasis
- Typically asymptomatic and appears as a multilocular cyst radio graphically
- Most common forms in posterior mandible
- Treated by excision with a margin of normal tissue
- Maxillary ameloblastomas can invade the cranial base and be lethal.
- Treated by hemimandibulectomy.
Adenomastoid odontogenic tumour:
Key feature:
- Rare
- Hamartoma of odontogenic epithelium
- Usually presents between ages 15 and 20
- Most common in the anterior maxilla
- Often appears radiographically as a unilocular dentigerous cyst
- Responds to enucleation.
Calcifying epithelial odontogenic tumour:
Key features:
- Rare neoplasm of odontogenic epithelium
- Usually presents between ages 30 and 50
- Many bizarre pleomorphic and hyperchromatic nuclei and formation of amyloid-like material
- Solid tumour, mixed radiolucency
- Most commonly forms in posterior mandible
- Locally invasive; but does not metastasise
- Treated by excision with a small margin.
Calcifying odontogenic cyst:
Key features:
- Rare
- Probably a neoplasm of odontogenic epithelium
- Wide age range
- Radiographically unilocular often undistinguishable from non-neostatic jaw cysts
- Calcifications in the cyst wall may suggest the diagnosis
- Forms at any site in alveolar ridge, usually posteriorly
- Occasionally forms in soft tissue of the gingiva
- Diagnosis by finding ghost and ameloblast-like cells histologically
- Usually responds to enucleation like a non neoplastic cyst
- Solid lesions may be more aggressive.
Cyst Common sites:
- Dentigerous cyst – mandible, third molar ramus area Lateral periodontal cyst – mandibular pre molar
- Odontogenic keratocyst – mandible 3rd molar ramus area
- Adamantinoma of long bones – tibia
- Adenamatoid odontogenic tumor – Anterior maxilla
- Squamous odontogenic tumor- maxillary incisor region and mandible molar region
- Periapical cemental dysplasia – mandibular incisors
- Benign cementoblastoma – mandibular permanent 1st molar
- Compound odontoma – anterior maxilla.
Odontogenic cysts and tumours:
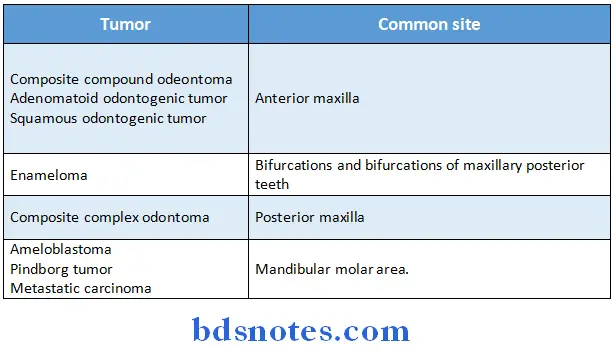
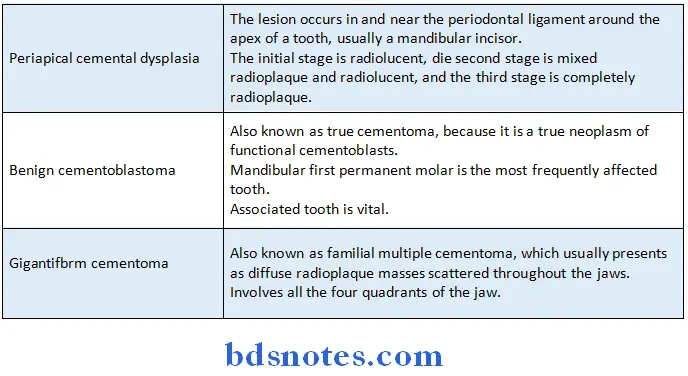
Regression alterations of teeth:
- Attrition
- Physiologic wearing of tooth as a result of tooth is tooth contact.
- 1st clinical manifestation is small polished facet on a cusp lip or ridge.
- Abrasion
- Occurs on exposed root surfaces of teeth.
- Common cause – use of an abrasive dentifrice
- Clinically manifested as
- ‘V’ shaped on wedge shaped polished ditch on root side of cementoenamel function in teeth with gingival recession.
- Notching of incisal edge of one maxillary incisor in people who use their teeth to open bobby pins.
- Notching of teeth in pipe smokes that conform to a shape of the pipe stem.
- Erosion may be defined as loss of tooth substance by a chemical process that does not involve tumor bacterial action.
- Tooth most commonly undergoing idiopathic root resorption
- Maxillary incisors
- Histologically the pulp of teeth undergoing internal resorption exhibits chronic inflammatory reaction.
- Foci of calcified tissue that lie freely in periodontal ligament space are known as cementicles
- Characters of ageing pulp
- Increased fibrosis
- Decreased vascularity
- Decreased cellularity.
- Treatment of choice for non perforating internal resorption – endodontic therapy
- Most common pathologic cause for secondary dentin formation is caries (other trauma)
- Clinical evidence that precede the formation of secondary dentin is – decreased tooth sensitivity.
Bacteria Viral And Mycotic Infections
Common etiologies:
- Scarlet fever -ẞ hemolytic streptococcus (toxin is erythrogenic toxin)
- Diphtheria corynebacterium sp
- Behcet’s syndrome – auto immune
- Herpangina – cox sackie group A virus
- Acute post operative parotitis – staphylococcus aureus
- Pyogenic granuloma – local irritant
Common site or entry:
- Tuberculous lesion – Tongue
- Route of entry of mycobacterium – Respiratory tract
- Oral lesion of wegeners granulomatosis – gingiva
- Pyogenic granuloma – gingiva
- Pyostomatitis vegetans – Buccal mucosa
- Oral lesions of hand, fool and mouth disease – hard palate
Scarlet fever:
- Characteristic appearance of tongue – Strawberry tongue
- The characteristic scarlet skin rash of scarlet fever forms on second on third day of illness.
Diphtheria:
Clinical features:
- Fever, headache, sore throat, formation of pseudo membrane in pharynx
Complications:
- Myocarditis, polyneuritis, acute intestinal nephritis
Tuberculosis:
- In military T.B, dissemination of microorganisms occur usually via blood stream. TB of lymph nodes – scrofula
- Sarcoidosis – features
- Depression of delayed type of hypersensitivity
- Raised on abnormal serum immunoglobulin
- Most of epithelial cells with multinucleated giant cell
- Cranial nerve paralysis most common in uveoparotid fever and cephalic tetanus – VII
- Cells of origin of leprae cells in lesion of leprosy is macrophages.
- Actinomycosis /Ray fungus
- Common form – Cervico facial
- Serious form – abdominal
- Endogenous infection
- Actinomycosis Israeli – Anaerobic, gram positive, non acid fast bacteria.
- Clostridium tetani cause blockage of spinal inhibition.
Syphilis:
-
- Characteristic lesion of primary stage of acquired syphilis is chancre
- The lesion of secondary stage of acquired syphilis is highly infective and mimics leukoplakia.
- Hexheimer reaction following antibiotic therapy is seen.
- Granuloma inguinale
- Characteristic oral manifestation – cicatrization
- Donavan bodies are seen.
- Hebra nose is seen in Rhinoscleroma.
- Herpes characteristic lesion – vesicle
- Tisues involved are derived from ectoderm nerve ganglia involved by HSV I- Trigeminal.
- HSV I can be isolated from oral lesions after approximately – 31⁄2 day after onset of lesion
- Recurrent herpetic lesions of fingers and hands are known as Herpetic whitlow.
- Lesions of recurrent herpatic gingivostomatitis is found on tightly attached area of oral mucosa like attached gingiva and hard palate.
Aphthous ulcers:
-
- Etiology – bacterial infection, vitamin B12 folic acid def
- Immunological abnormalities
- Most common from recurrent apththous minor
- Koplick’s spots are seen in measles on rubella
- Rubella
- No Koplik’s spots
- Complications – rare
- Rubeola
- Present
- Oral mucous membrane not usually inflamed inflamed common.
- Salivary gland enlargement in nutritional mumps and due to
- In acute phase-hypertrophy or acinar cells
- In chronic phase – due to replacement of normal gland parenchyma by fat
- Chemical mumps occur most commonly following the administration of Iodine.
- Most common viral cause of mental retardation is cytomegalic inclusion disease
- Fungal infections having special prediction for occurrence in reticulo endothelial system is histoplasmosis
- Fungal infection exhibiting pseudo epitheliomatous hypoplasia on histologic examination – Blastomycosis
Candidiasis:
- Most opportunistic infection, occurs mostly in old age group, painful – acute atrophic oral candidiasis (denture sore mouth)
- Resembling leukoplakia – chronic hyperplastic oral conditions.
- Fungi having predilection for blood vessels – phycomycetes
- Primary herpetic gingivostomatitis
- Age group – 16 years
- Treatment of choice – Gentle debridement of mouth increased liquid intake.
- Mucormycosis – severe mycotic infection of head and neck characterised by triad of uncontrolled diabetes orbital infection and meningoencephalitis.
Infections:
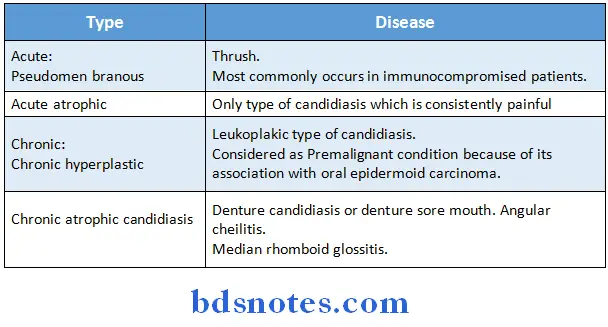
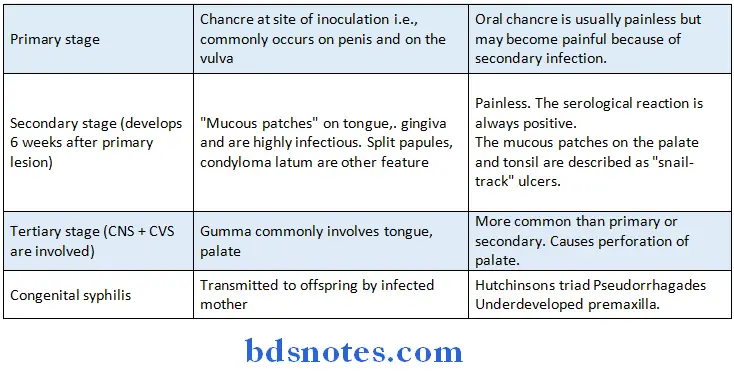
Dental Caries
- In the initial stage of carious lesion, there is the loss of interprismic substance.
- Plaque is primarily composed of micro organisms.
- The micro organisms primarily responsible for root surface caries are actinomyces viscosus.
- In the initial stage of carious lesion, there is the loss of interprismic substance. Plaque is primarily composed of microorganisms.
- Normal pH of saliva is 6.5 to 6.8.
- Dietary carbohydrate most likely involved in the etiology of caries is sucrose.
- pH threshold level at which enamel demineralization occurs is 5.5
- Radiation caries occurs commonly at cervical area of tooth.
- A soluble polysaccharide found in dental plaque and formed from fructose moiety of sugar is called Levan.
- The best method of detecting incipient caries in proximal surfaces of posterior teeth is by transillumination.
- Most effective way of prevention of dental decay of general population is systemic fluorides.
- Excessive fluoride intake causes staining of teeth.
- The severity of this staining (fluorosis) is measured by Dean’s Index and CFI (Clinical fluorosis index).
- Fluoride content is greatest in cementum among the dental tissues.
- In experimental animals the offspring of carious prone male and caries resistant female parents would be carious activity same as male.
Diseases Of Pulp And Periapical Tissues
Theories of dental caries:
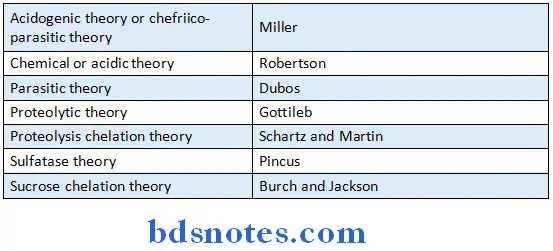
- Most common cause of pulpitis – Dental caries
- Periapical granuloma (Bacteria – streptococcus viridans)
- Histological features
- Proliferation of fibroblasts
- Endothelial proliferation
- Frequent cause of apical root resorption
- Pathogenesis of periapical cyst – proliferation of epithelial rests in the periapical area involved by the granuloma increased osmotic pressure in cyst lumen.
- Features of periapical cyst – Rushton bodies, cholesterol slits.
- R/F of acute apical abscess.
- Slight thickening of periodontal ligament in the periapical area
- Osteomyelitis of jaw
- Common cause of acute osteomylitis – dental infection
- Bacteria implicated acute osteomylitis – Staphylococcus aureus
- Chief inflammatory cells acute osteomyelitis – PMN’s
- Chronic focal sclerosing osteomyelitis
- Tooth commonly involved – mandible 1st molar
- Common cause a large carious lesion
- Treatment of choice – Endodontic therapy
- Common site of occurrence of Gare’s osteomylitis – Tibia left and characterized by periodontal bone formation.
Acute pulpitis:
- Symptom – Pain on application of cold, which persists even after the removal of irritant.
- Earliest common symptom secondary to carious lesion and thermal sensitivity.
- Most typical indication of acute periapical abscess – pain is relieved by drainage
- Chronic hyperplastic pulpitis is proliferation of chronically inflamed pulp tissue
- It is generally seen in young teeth with large apical foramina.
- The reversible disease of pulp is pulpal hyperemia.
- Root canals are commonly infected with gram positive micro-organisms.
- Efferent nerves in dental pulp are somatic post ganglionic type.
- Defense cells of pulp are fibroblasts.
- Acute apical periodontitis is best diagnosed by percussion.
- Tooth with crowns can be tested for thermal sensitivity by solid CO2, difluorodichloroethane or frigident.
- Pulpotomy is done to preserve of radicular pulp.
- Formaceresol used during pulpotomy causes fixation and coagulative necrosis.
- Pulpectomy and pulp capping are more successful in primary teeth because of increased blood supply through the wide apical foramen.
- Percussion is a dental diagnostic procedure used to determine
periapical/periodontal status of teeth. - Following amputation of coronal portion of the pulp of an immature permanent molar; the stump should be capped with calcium hydroxide.
- The most common consequences of bleaching non-vital teeth is cervical resorption, while the most common consequence of bleaching vital tooth is apical periodontitis.
- Acute exacerbation of chronic periapical abscess is termed as phoenix abscess.
- Referred pain of dental origin is always ipsilateral and does not cross midline.
Acute osteomyelitis of the jaws:
Key features:
- Mandible mainly affected, usually in adult males
- Infection of dental origin – anaerobes are important
- Pain and swelling of jaw
- Teeth in the urea re tender: gingivae red and swollen
- Sometimes paraesthesia of the lip
- Minimal systemic upset
- After about 10days, radiographs show moth-eaten pattern of bone destruction
- Good response to prompt antibiotic treatment and debridement.
Diffuse sclerosing osteomyelitis:
Key features:
- Adults
- No sex predeliction
- Sclerosis round site of periapical or periodontal chronic inflammation
- Sclerosis round site of periapical or periodontal chronic inflammation
- No pain or swelling
- Radiographically resembles but is distinct from florid cementosseous dysplasia
- Pathology
- Bone sclerosis and remodeling
- Scanty marrow spaces and little or no inflammatory infiltrate, though adjacent to area of inflammation
- Treatment
- Elimination of originating source of inflammation, but sclerotic areas remain radiographically.
Focal sclerosing osteomyelitis:
Key features:
- Rare bony reaction to low-grade periapical infection or unusually strong host defensive response
- Children and young adults affected
- Premolar or molar region of mandible affected
- Bone sclerosis associated with a non-vital or pulpitic tooth
- Localized but uniform radiodensity related to tooth with widened periodontal ligament space or periapical area
- No expansion of the jaw
- Pathology
- Dense sclerotic bone with scanty connective tissue or inflammatory cells
- Treatment
- Elimination of the source of inflammation of by extraction or endodontic treatment.
Proliferative periostitis (Garre’s osteomyelitis):
Key features:
- Adolescents mainly affected
- Usually associated with periapical but sometimes other inflammatory foci
- Periosteal reaction affecting lower border of mandible causing ‘onion skin’ thickening and swelling of bone
- Pathology
- Parallel layers of highly cellular woven bone interspersed with scantily inflamed connective tissue
- Small sequestra if present
- Treatment
- Eliminate focus of infection
- Bone gradually remodels after 6 to 12 months.
Alveolar osteitis:
Key features:
The most common painful complication of dental extractions
- Loss of clot normally filling extraction socket
- Loss of clot may be due to excessive local fibrinolytic action or bacterial enzymes or body
- Bare, whitish lamina dura exposed in socket
- Pain relieved by irrigation and repeated dressing of socket
- Dead bone usually shed as crumb-like fragments
- Eventual healing of socket from its base by granulation.
Spread Of Oral Infection
- Organism implicated as causative case of cellulites is streptococcus.
- Diffuse spreading inflammation reaction produced by sore microorganisms is due to elaboration for hylaronidinase.
- Ludwigs angina
- Spaces involved – submaxillary, submental, sublingual.
Clinical features:
-
- Dysphagia, dyspnoea, fever
- Origin in mandibular molars
- Complications – edema of glottis
- Most serious complication of infection involving maxillary tooth is cavernous sinus thrombosis.
- Infection of maxillary teeth traverse to cavernous sinus via pterygoid plexus.
- Etiology of maxillary sinusitis
- Upper respiratory tract infection
- Perforation of antral floor following extraction
- An allergic reaction.
- Examination of cases of chronic maxillary sinusitis shows clouding and fluid level.
- Mechanisms of focal infectionMetastasis of microorganisms from an infected focus by either hematogenous on lymphatic spread dissemination of toxins on toxic products produced by microorganisms via blood stream or lymphatics.Antibiotic prophylaxis before performing dental procedure is of absolute necessary in patients in history of rheumatic fever or valvular damage in order to prevent subacute bacterial endocarditis.
Physical And Chemical Injuries To The Oral Cavity
- A healthy pulp respond to minimal injury by dentin formation.
- Initial response of dental pulp to cavity preparation is migration of odontoblastic nuclei.
- Calciotraumatic line is seen in Dentine
- Copper cement has germicidal properly.
- Approximate time required for new odontoblasts to differentiate and produce
- reparative dentin after cavity preparation is 20 days.
- Most common suggested cause of bruxism – psychologic
- Pathogenesis of hemorrhagic bone cyst – failure of organization of
blood clot after on injury to an area of spongy bone.
Traumatic bone cyst:
- Occurs due to failure of organization of blood clot after an injury.
- Generally seen in young people
- Commonly involves mandibular molar area
- Treatment of choice – opening into the cavity and inducing bleeding.
- Self inflicted injuries are known as factitial injuries
- Constituent of denture base acrylic resin responsible for allergic reaction – monomer or methyl methacrylate
- Commonest of base metal alloy most commonly responsible for allergic reaction- Nickel
- Component of vulcanite denture bases which cause allergy reaction – sulfur
- Mucocele:
- Occurs as a result of rupture of salivary duct (Minor salivary glands)
- Common site – lower lip
- Treatment of choice – excision with removal of associated minor salivary gland.
Ranula:
- Most commonly occurs in association with ducts of submandibular glands
Clinical features:
- Painless, fluctuant, bluish colored swelling in the floor of mouth.
Sialolithiasis:
-
- Frequent site-upper lip
- Commonly seen during radiographic examination of submandibular gland
- Sialoliths are composed of calcium and phosphorus.
- Alpha particle are beam of doubly charged helium nucleus
- Majority of radiation emitted by radioactive isotopes of most element is ẞ radiation.
- Most frequently used unit to denote biologic measurement of dose is skin erythema dose (SED)
- Units of measurement of radiation
- Roentgen – most commonly used
- Rad
- Rem
- Curie
- Primary cause of radiation damage is ionization.
- Most radio resistant cell – muscle cell
- Oral tissue most sensitive to X ray radiations are developing tooth bed and salivary glands
- Most of the biologic damage produced by ionizing radiation is due to damage resulting from radiation produced free radicals.
- First observable clinical reaction to radiation is skin erethema.
- Typical pattern of causes occurring due to therapeutic irradiation of head and neck region is known as amputation caries/Radiation caries.
- It generally starts in the cervical area as tooth.
- Effect of LASER radiation on tooth enamel generally consists of glass like fusion of enamel.
- Poisoning of arsenic, lead and mercury causes excess salivation.
- Raindrop pigmentation of skin mucosa is seen in arsenic poisoning.
- Oral pigmentation following metal poisoning is due to formation of metal sulphite.
- Sloughing of necrotic epithelium is characteristic of aspirin burn.
- Test tube retepegs are seen in dilantin sodium hyperplasia.
- Pigment formed in metal poisoning is usually present in intercellular substance.
- lead poisoning:
- Plumbism
- Burtonian line is seen here
- Feature of Hg poisoning – acrydynia
- Oral ulceration, loosening and exfoliation of teeth and swelling of salivary glands.
- Raw beef appearance of skin is seen in pink disease.
Saliva poisoning-Argyria. - Most common intra oral pigmented lesion – Amalgam tattoos frequent site – gingiva
- Tetracyclic induced staining of deciduous incisors may occur if the drug is administered during four months in utera to three months post partum.
- Angioneurotic edema due to deficiency of 1 esterase inhibition.
- Treatment of choice – E-amino caproic acid.
- Allergic reaction occurring to systemic ingestion of a drug is known as dermatitis medicamentosa.
- Allergic reaction occurring due to repeated contact of allergen at a localized site is known as dermatitis venenata.
- Diseases of bones and Joints
- Pain in region of TMJ is most often caused by muscle spasm.
- Treatment of MPDS:
- Relief of emotional factors tranquilizers and muscle relaxants physiotherapy
- Muscle most affected – lateral pterygoid
- Most common complication of rheumatoid arthritis involving TMJ – Fibrous ankylosis
- Most common cause of ankylosis – trauma
- Pain and tenderness on palpation of TMJ is usually associated with – deviation of jaw to painful side upon mouth opening.
- Dental finding characteristic of pagets disease is hyperligamentary hematologic examination – elevated serum alkaline phosphatase
- Others – Caffeys’s disease, severe polyostatic fibrous dysplasia
An accentuation of osteoblastic and osteoclastic activity with a mosaic bone pattern is seen in – Osteopetrosis
- Others – Caffeys’s disease, severe polyostatic fibrous dysplasia
- Most common cause of referred pain to TMJ area are impacted third molars.
- Bony protruberances of condyle and glenoid fossa are common is osteoarthritis.
- Most common type of arthritis
- Microorganisms most frequently responsible for TMJ arthritis-Staphylococci
- Direction of pressure to reduce the condylar dislocation – downward and backward
- Pain in region of TMJ is most often caused by muscle spasm.
- Treatment of MPDS –
- Relief of emotional factors tranquilizers and muscle relaxants physiotherapy
- Muscle most affected – lateral pterygoid
- Most common complication of rheumatoid arthritis involving TMJ – Fibrous ankylosis
- Most common cause of ankylosis – trauma
- Pain and tenderness on palpation of TMJ is usually associated with -deviation of jaw to painful side upon mouth opening.
- Dental finding characteristic of pagets disease is
hyperligamentary hematologic examination – elevated serum alkaline phosphatase- Others – Caffeys’s disease, severe polyostatic fibrous dysplasia
- An accentuation of osteoblastic and osteoclastic activity with a mosaic bone pattern is seen in – Osteopetrosis
- Most common cause of referred pain to TMJ area are impacted third molars.
- Bony protruberances of condyle and glenoid fossa are common is osteoarthritis.
- Inability to retrude mandible in case of TMJ dislocation is believed to be due to spasm of temporalis.
- Calciform and diphephenates are used in treatment of pagets disease
- Bone most frequently involved in progressive oteolysis is clavicle
- Best most commonly involved in pagets disease is sacrum
- Achondroplasia
- Type of malocclusion – class III
- Basic defect – Retardation of zone of provisional calcification of endochondral growth.
- Ulcerative, Vesicular and Bullous lesions
- Acute multiple lesions – Herpes Virus infections Erythema
multiforme,ANUG,contact allergic stomatitis, oral ulcer secondary to cancer – chemotherapy.- Chronic multiple lesions – Pemphigus subepithelial bullous dermata herpes simplex infection in – immuno compromised patient.
- Recurrent oral ulcers – Recurrent apthous stomatitis
- Bechet’s syndrome
- Recurrent Herpes simplex infection
- Single ulcers – Histoplasmosis – Blastomycosis – Mucormycosis
Principles of dental management of diabetics
- Time treatment to avoid disturbance of routine insulin administration or meals
- Use local anaesthesia for routine dentistry – the amount of adrenaline (epinephrine) in local anaesthetic solutions has no significant effect on the blood sugar
- Sedation can be given if required
- Dental operations under general anaesthesia should only be carried out in hospital under expert supervision
- Deal with any diabetic complications
- Manage hypoglycaemic coma by giving sugar.
Management of myocardial infarction
- Put the patient in a comfortable position that allows easy
breathing. - Do not lay flat if there is left ventricular failure and pulmonary oedema
- Send an assistant to telephone for an intensive care ambulance
- Give 50/50 nitrous oxide and oxygen from a general anaesthetic or relative analgesia machine, to relive pain and anxiety
- Constantly reassure the patient
- Give oxygen if necessary
- Give aspirin 150 mg by mouth as soon as more urgent measures have been carried out
- Check for possible cardiac arrest
Management of prolonged dental haemorrhage
- Reassure the patient
- Coax excited relatives out of surgery
- Clean the mouth with swabs and locate the source of bleeding
- Give adrenaline (epinephrine) – containing local anaesthetic, remove ragged tissue, squeeze up the socket edges and suture it
- When bleeding has been controlled, ask about the history and especially any family history of prolonged bleeding
- If bleeding continues despite suturing or if the patient is obviously anaemic or debilitated, transfer to hospital for investigation and management of any haemorrhagic defect
- Mean while, limit bleeding as much as possible with a pressure pad over the socket and by supporting the patient’s jaw with a firm barrel bandage
- Ideally, tranexamic acid (500 mg in 5 ml., by slow intravenous injection) should be given and may be effective in a mild haemophilic while awaiting transfer to hospital.
Important side-effects of long-term use of corticosteroids
- epression of adrenocortical function and risk of circulatory collapse
Depression of inflammatory and immune responses - Opportunistic infections
- Depressed protein metabolism
- Impaired wound healing
- Moon face
- Raised blood sugar
- Sodium and water retention
- Mood changes
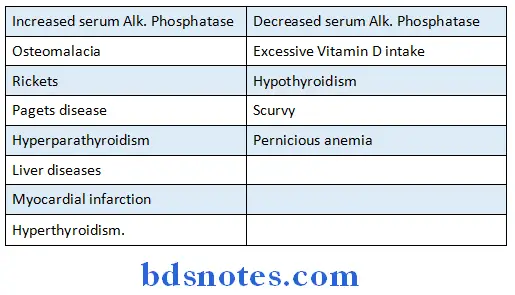
Characteristic appearance of teeth:
Shell teeth:
- Dentinogenesis imperfecta (Brandy wine type)
Ghost teeth:
- Odontogenesis imperfecta (Regional odontodysplasia)
Thistle tube teeth:
- Type II dentinal dysplasia
Snow capped teeth:
- Amelogenesis imperfecta of hypomaturation type
Floating teeth:
- Cherubism
- Hand schuller Christian disease.
- Various common causes of macroglossia are:
- Down syndrome
- Amyloidosis.
- Hurlers syndrome
- Calcinonis cutis.
- Lymphangioma
- Haemangioma
- Acromegaly
- Congenital hypothyroidism/cretinism.
- Multiple supernumerary teeth are common in:
- Cleidocranial dysplasia
- Gardner’s syndrome
- Cleft lip and cleft palate
Examples of haematoxylin and eosin staining of various tissues:
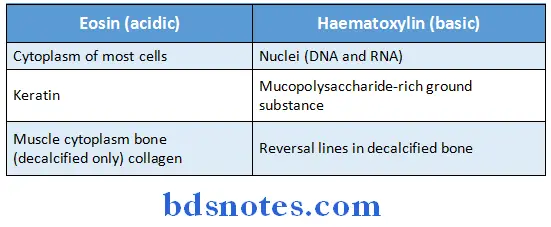
Important uses of immunostaining techniques:
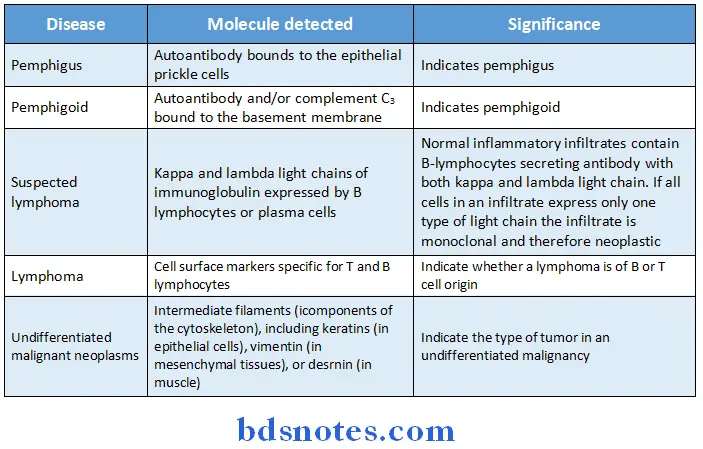
Types of blood test useful in oral diagnosis:
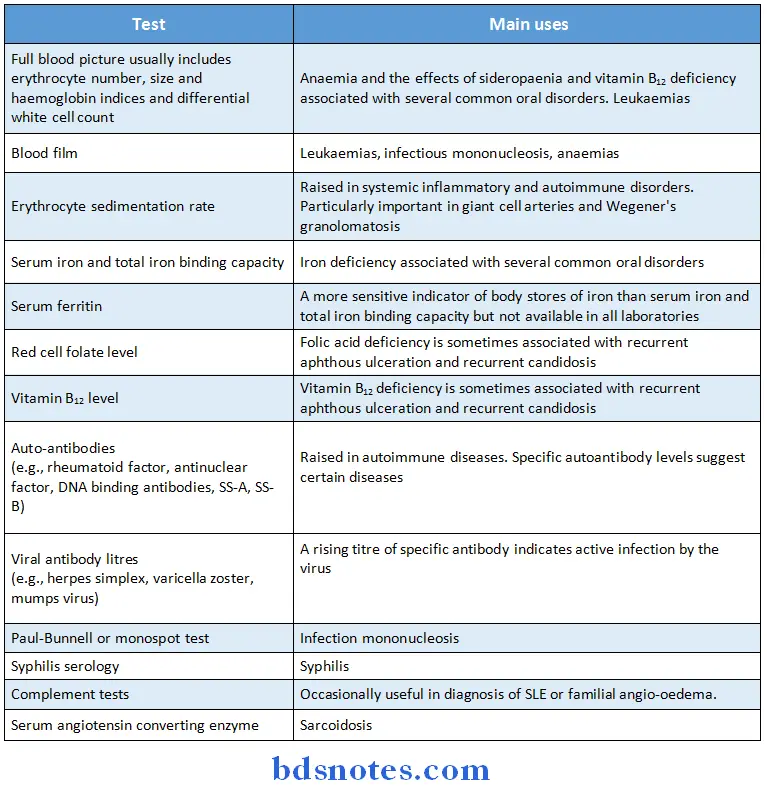
Microbiological tests useful in oral diagnosis:
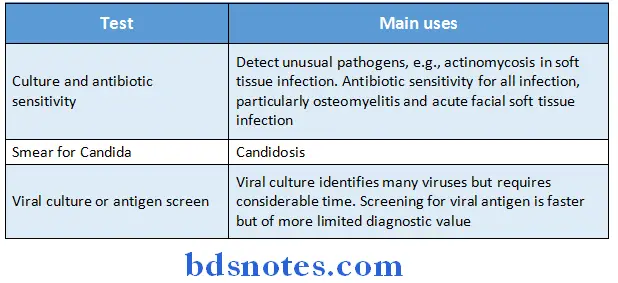
Causes of gingival enlargement:
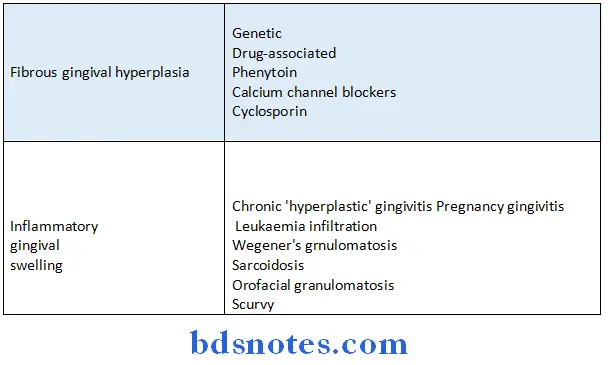
Causes of limitation of mandibular movement:
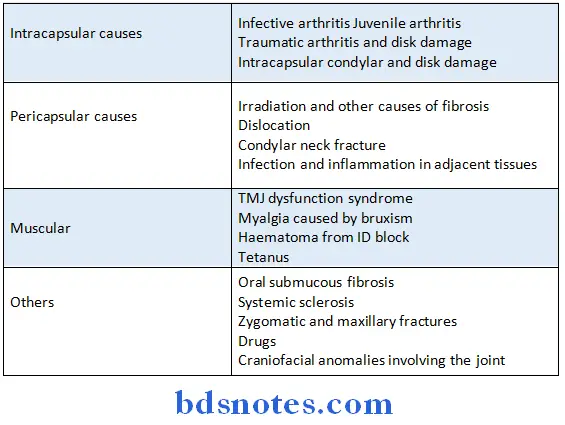
Important causes of oral mucosal ulcers:
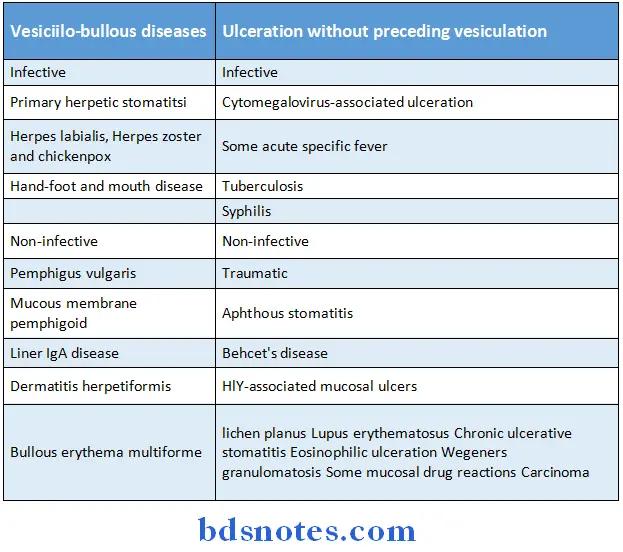
Causes of xerostomia:
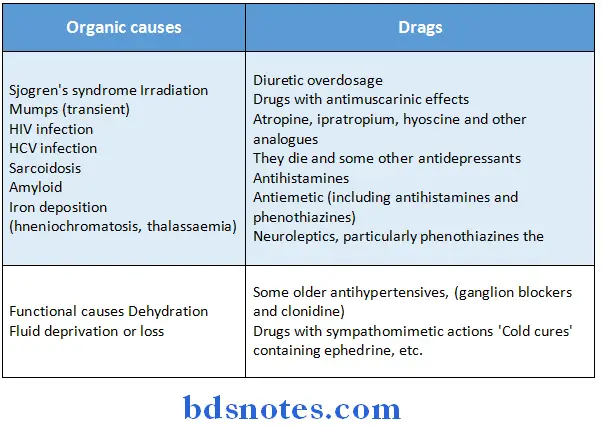
Enlarged Pulp Chamber:
- Hypophosphatasia
- Dentin dysplasia type 2
- Internal resorption
- Taurodontism
- Dentinogenesis imperfecta
- Regional odontodysplasia
- Vitamin D resistant rickets
Generalized Loss of Lamina Dura:
- Hyperparathyroidism
- Osteomalacia
- Paget’s disease of bone
- Fibrous dysplasia
Generalized widening of the periodontal ligament:
- Osterosarcoma
- Scleroderma
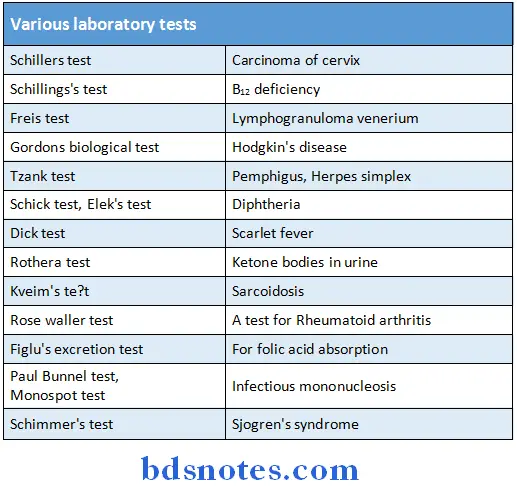
Commonly Asked Definitions
Dental caries:
- According to miller dental decay is a chemicoparasitic process consisting of two stages, the decalcification of enamel, which results in its total destruction and decalcification of dentin, as a preliminary stage, followed by dissolution of the softened residue.
- Pre malignant lesion is defined as a morphologically altered tissue in which cancer is more likely to occur than its apparently normal counter part.
- Pre malignant condition is defined as a generalized condition with significant risk of cancer.
- A tumor is a simple swelling of the tissue
- Neoplasm is considered as an independent, uncordinated new growth of the tissue which is potentially capable of unlimited proliferation and does not regress after the removal of the stimulus produced by the lesion.
- Cyst: A pathologic epithelium lined cavity, often filled with liquid or semi solid contents.
- Leukoplakia is a term that has been used for many years to indicate a white patch or plaque occurring on the surface of a mucous membrane, not only that of cord cavity,
- I but also that of the vulva, uterine cervix, urinary bladder, renal pelvis and upper respiratory tract.
- Erythroplakia is a clinical entity and represents a lesion of mucous membrane which histologically in large percentage of cases, exhibits epithelial changes ranging from mild dysplasia to carcinoma in situ and even invasive carcinoma.
- Oral sub mucous fibrosis:An insidious chronic disease affecting any part of the oral cavity and some times the pharynx.
- Although occasionally proceded by and or associated with vesicle formation, it is always associated with a juxtaepithelial inflammatory reaction followed by a fibroelastic change of the lamina propria, with epithelial atrophy leading to stiffness of the oral mucous and causing trismus and inability to eat.
- Acanthosis increase in thickness of stratum spinosum
Herpes:
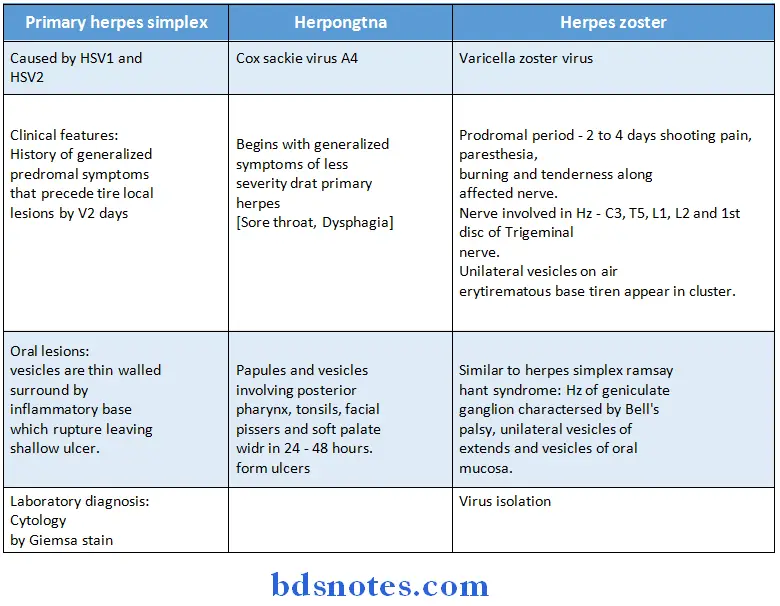
Signs:
Some important points:
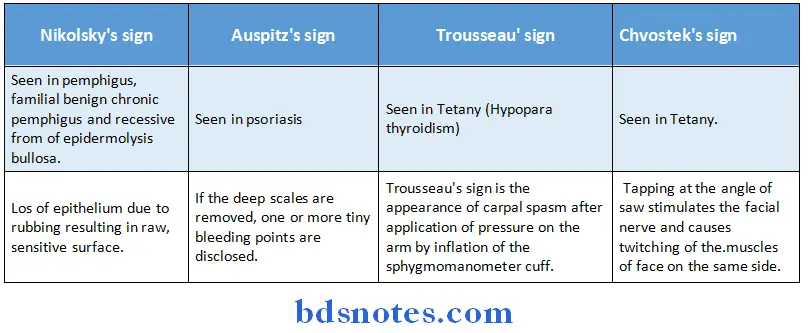
Sports:
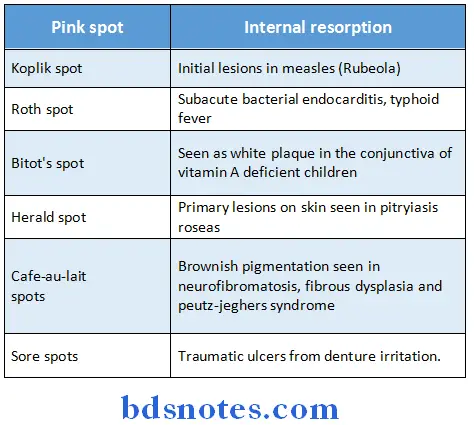
Retepegs:
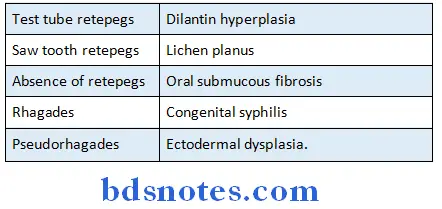
Appearance:
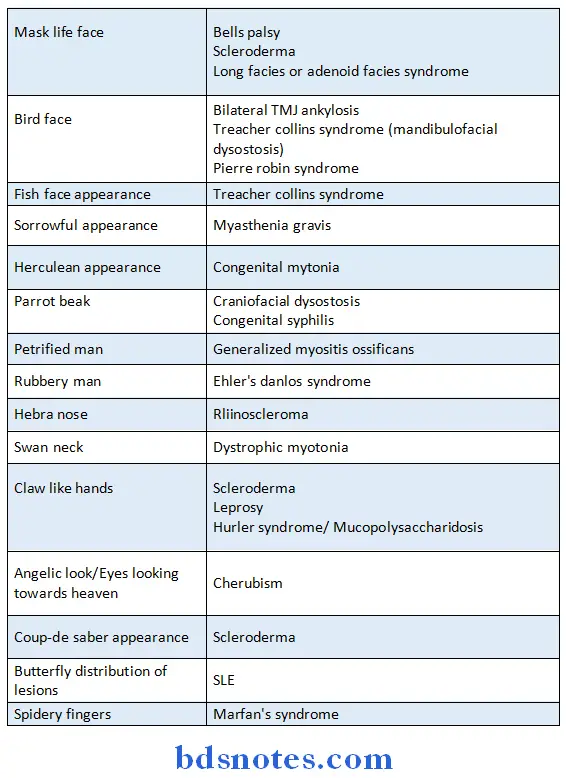
Exfoliation of teeth:
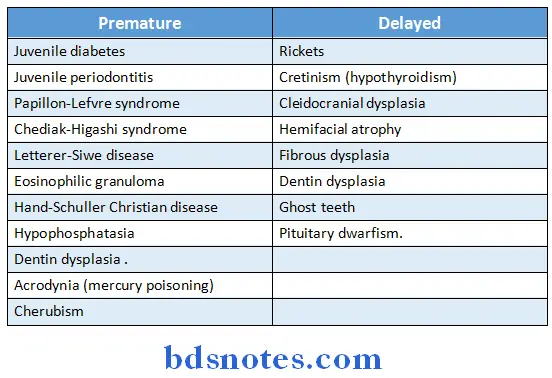
Similar features with different diseases:
Multinucleated giant cells are seen in:
- Cherubism
- Hyperparathyroidism
- Aneurismal bone cyst
- Giant cell granulomas
- Osteoclastoma
- Osteosarcoma
- Herpes
- Leprosy (langerthans giant cells)
- Eosinophilic granuloma.
Psoriasis form of lesions with Monro’s abscess are seen in:
- Benign migratory glossitis
- Psoriasis
- Reiter’s syndrome (Micro-abscess formation is also seen in Vitamin A deficiency)
Bence jones protein is diagnostic of:
- Multiple myeloma (important feature)
- Polycythemia vera
- Leukemia
- Solitary myeloma.
Blue sclera are seen in:
- Osteogenesis imperfecta.
- Marfan’s syndrome
- Cherubism
- Ehlers-danlos syndrome
- Osteopetrosis
- Fetal rickets.
Abnormal dentino-enamel junction is seen in:
- Dentinogenesis imperfecta
- Ehlers-Danlos syndrome
Widening of periodontal ligament is seen in:
- Osteosarcoma
- Scleroderma
- Trauma from occlusion.
Hypercementosis is seen in:
- Pagets disease
- Hyperpituitarism.
Obliteration of periodontal ligament space is seen in:
- Hypercementosis
- Ankylosis
- Hypofunction of teeth
- Paget’s disease.
Hyper mobility of joints is seen in:
- Ehlers danlos syndrome
- Marfan’s syndrome
- Osteogenesis imperfecta
- Down’s syndrome.
Absence of lamina dura:
- Hyperparathyroidism
- Paget’s disease.

Leave a Reply