Multiple Choice Questions
Question 1. Oral hairy leukoplakia involves:
1. Lateral border of tongue
2. Dorsal surface of tongue
3. Posterior 1/3rd of tongue
4. Ventral surface of tongue
Answer. 1. Lateral border of tongue
Question 2. Target lesions are seen in:
1. Pemphigus vulgaris
2. Erythema multiforme
3. Syphilis
4. Herpes zoster infection
Answer. 2. Erythema multiforme
Question 3. Macroglossia is seen in:
1. Meckel’s syndrome
2. Cleft lip and palate
3. Fetal face syndrome
4. Happy puppet syndrome
Answer. 4. Happy puppet syndrome
Question 4. Jone criteria of diagnosis is used for:
1. Infective endocarditis
2. Rheumatic fever
3. Subacute bacterial endocarditis
4. Hypertension
Answer. 3. Subacute bacterial endocarditis
Read And Learn More: Oral Medicine Question And Answers
Question 5. “Butterfly rash” is a characteristic feature of facial cutaneous lesion of:
1. Lichen planus
2. Systemic lupus erythematosus
3. Psoriasiform lesions
4. Erythema multiforme
Answer. 2. Systemic lupus erythematosus
Question 6. Sharp, shooting, lancinating and paroxysmal pain is a feature of:
1. Burning mouth syndrome
2. Atypical facial pain
3. Trigeminal neuralgia
4. Postherpetic neuralgia
Answer. 3. Trigeminal neuralgia
Question 7. Abnormal increase in number of red blood cells is known as:
1. Polycythemia
2. Anemia
3. Leukemia
4. Agranulocytosis
Answer. 1. Polycythemia
Question 8. Oral melanotic macule is:
1. Red colored
2. Brown-black colored
3. Purple colored
4. Yellow colored
Answer. 2. Brown-black colored
Question 9. Cracked mud appearance is seen in:
1. Speckled leukoplakia
2. Atrophic candidiasis
3. Bullous lichen planus
4. Homogeneous leukoplakia
Answer. 4. Homogeneous leukoplakia
Question 10. One of the oral manifestations of diabetes is:
1. Median rhomboid glossitis
2. Geographic tongue
3. Black hairy tongue
4. Benign migratory glossitis
Answer. 1. Median rhomboid glossitis
Question 11. Elevated blister like lesion less than 1 cm in diameter containing clear fluid is:
1. Nodule
2. Vesicle
3. Bulla
4. Pustule
Answer. 2. Vesicle
Question 12. Actinic keratosis is caused by:
1. Betel nut chewing
2. Tobacco chewing
3. Smoking
4. Exposure to sun
Answer. 4. Exposure to sun
Question 13. Contact allergy is most accurately diagnosed by:
1. Penny test
2. Pathergy test
3. Patch test
4. Tuberculin test
Answer. 3. Patch test
Question 14. Necrotizing ragged ulceration with no apparent inflammatory response is indicative of:
1. Leukocytosis
2. Polycythemia vera
3. Thrombocytosis
4. Agranulocytosis
Answer. 4. Agranulocytosis
Question 15. Oral pigmentation following metal poisoning is due to formation of:
1. Oxide
2. Sulfide
3. Chloride
4. Phosphate
Answer. 2. Sulfide
Question 16. Geographic tongue is also known as:
1. Wandering rash
2. Hairy tongue
3. Hairy leukoplakia
4. Fissured tongue
Answer. 1. Wandering rash
Question 17. Definitive diagnosis for oral squamous cell carcinoma is done by:
1. Aspiration cytology
2. Exfoliative cytology
3. Brush biopsy
4. Incisional biopsy
Answer. 4. Incisional biopsy
Question 18. Brown tumor is seen in:
1. Hyperpituitarism
2. Hyperthyroidism
3. Hyperparathyroidism
4. Hypoparathyroidism
Answer. 3. Hyperthyroidism
Question 19. Wickham’s striae are associated with:
1. Leukoplakia
2. Candidiasis
3. Oral lichen planus
4. Oral submucous fibrosis
Answer. 3. Oral lichen planus
Question 20. Most common complication of phenytoin or dilantin is:
1. Xerostomia
2. Ataxia
3. Gingival enlargement
4. Urticaria
Answer. 3. Gingival enlargement
Question 21. “Butterfly rash” is the characteristic feature of facial cutaneous lesion of:
1. Lichen planus
2. Systemic lupus erythematosus
3. Psoriasiform lesions
4. Erythema multiforme
Answer. 2. Systemic lupus erythematosus
Question 22. Aphthous ulcer more than l cm in diameter is seen in:
1. Mikuliz disease
2. Cook’s disease
3. Hand foot mouth disease
4. Sutton’s disease
Answer. 4. Sutton’s disease
Question 23. Definitive diagnosis for oral squamous cell carcinoma is done by:
1. Aspiration cytology
2. Exfoliative cytology
3. Brush biopsy
4. Incisional biopsy
Answer. 4. Incisional biopsy
Question 24. Sialolith is most common with:
1. Parotid gland
2. Sub-mandibular gland
3. Sub-lingual gland
4. Von Ebner’s gland
Answer. 2. Sub-mandibular gland
Question 25. Causative organism for herpangina is
1. Coxsackie virus
2. Herpes zoster virus
3. Human herpes virus
4. Cytomegalovirus
Answer. 1. Coxsackie Virus
Question 26. Cracked mud appearance is seen in:
1. Speckled leukoplakia
2. Atrophic candidiasis
3. Bullous lichen planus
4. Homogeneous leukoplakia
Answer. 4. Homogeneous leukoplakia
Question 27. Histologically pemphigus shows:
1. Acanthosis
2. Acantholysis
3. Keratin pearl
4. Civatte bodies
Answer. 2. Acantholysis
Question 28. Blue sclera, brittle bone, opalescent dentin is a sign of:
1. Osteogenesis imperfecta
2. Paget’s disease
3. Marfan’s syndrome
4. Osteopetrosis
Answer. 1. Osteogenesis imperfecta
Question 29. Mumps is caused by
1. Cytomegalovirus
2. Herpes simplex virus
3. Paramyxovirus
4. Epstein-Barr virus
Answer. 3. Paramyxovirus
Question 30. Plumbism is due to:
1. Mercury poisoning
2. Bismuth poisoning
3. Silver poisoning
4. Lead poisoning
Answer. 4. Lead poisoning
Question 31. Contact allergy is most accurately diagnosed by:
1. Rose Bengal test
2. Pathergy test
3. Patch test
4. Diascopy test
Answer. 3. Patch test
Question 32. Causative organism for hand, mouth and foot disease is:
1. Herpes zoster virus
2. Coxsackie virus
3. Human herpes virus
4. Cytomegalovirus
Answer. 2. Coxsackie virus
Question 33. Café-au-lait pigmentation is seen in patient with:
1. Hemangioma
2. Neurofibromatosis
3. Kaposi’s sarcoma
4. Cherubism
Answer. 2. Neurofibromatosis
Question 34. Nikolsky’s sign is seen in:
1. Erythema multiforme
2. BehÇet’s syndrome
3. Pemphigus vulgaris
4. Allergic stomatitis
Answer. 3. Pemphigus vulgaris
Question 35. Thrush is also known as:
1. Acute pseudomembranous candidiasis
2. Chronic hyperplastic candidiasis
3. Chronic mucocutaneous candidiasis
4. Acute atrophic candidiasis
Answer. 1. Acute pseudomembranous candidiasis
Question 36. Abnormal increase in number of red blood cells is known as:
1. Agranulocytosis
2. Leukemia
3. Anemia
4. Polycythemia
Answer. 4. Polycythemia
Question 37. The cyst with high recurrence rate is:
1. Odontogenic keratocyst
2. Adenomatoid odontogenic cyst
3. Radicular cyst
4. Dentigerous cyst
Answer. 1. Odontogenic keratocyst
Question 38. Laskin’s cardinal sign involves the following features except:
1. Unilateral pain in preauricular area
2. Muscle tenderness
3. Masticatory muscle spasm
4. Limited jaw movements
Answer. 3. Masticatory muscle spasm
Question 39. The absence of clavicle is seen in:
1. Cleidocranial dysplasia
2. Osteogenesis imperfecta
3. Sturge Weber syndrome
4. Ectodermal dysplasia
Answer. 1. Cleidocranial dysplasia
Question 40. Epstein-Barr virus has been implicated in etiology of:
1. Oral lichen planus
2. Oral hairy leukoplakia
3. Oral black hairy tongue
4. Oral melanoplakia
Answer. 2. Oral hairy leukoplakia
Question 41. The basic defect in hairy tongue is hypertrophy of:
1. Filiform papilla
2. Foliate papilla
3. Fungiform papilla
4. Circumvallate papilla
Answer. 1. Filiform papilla
Question 42. Primary infection with vericella zoster virus is:
1. Infectious mononucleosis
2. Chickenpox
3. Shingles
4. Herpes labialis
Answer. 2. Chickenpox
Question 43. Melanin pigmentation seen in pregnancy is called as:
1. Melasma
2. Melanoma
3. Ephelis
4. Macule
Answer. 1. Melasma
Question 44. Homogeneous leukoplakia gives:
1. Speckled appearance
2. Atrophic appearance
3. Bullous appearance
4. Cracked mud appearance
Answer. 4. Cracked mud appearance
Question 45. Lacrimal gland function test for diagnosing Sjögren’s syndrome include:
1. Pathergy test
2. Patch test
3. Schirmer’s test
4. Diascopy test
Answer. 3. Schirmer’s test
Question 46. Sharp, shooting, lancinating and paroxysmal pain is a feature of:
1. Burning mouth syndrome
2. Trigeminal neuralgia
3. Atypical facial pain
4. Myofacial pain dysfunction syndrome
Answer. 2. Trigeminal neuralgia
Question 47. Solid lesion raised above the skin surface, over 1 cm in diameter is called as:
1. Macule
2. Plaque
3. Papule
4. Nodule
Answer. 2. Plaque
Question 48. Abnormal increase in number of red blood cells is known as:
1. Agranulocytosis
2. Leukemia
3. Anemia
4. Polycythemia
Answer. 4. Polycythemia
Question 49. Which of the following is the most common cause of ankylosis of TMJ:
1. Osteoarthritis of TMJ
2. Congenital syphilis
3. Traumatic injury to TMJ
4. Traumatic occlusion
Answer. 3. Traumatic injury to TMJ
Question 50. Strawberry tongue is seen in:
1. Scarlet fever
2. Wegener’s granulomatosis
3. Midline lethal granuloma
4. Sarcoidosis
Answer. 1. Scarlet fever
Question 51. Hairy leukoplakia is caused by:
1. Epstein-Barr virus
2. Fungal infection
3. Bacterial infection
4. Herpes simplex infection
Answer. 1. Epstein-Barr virus
Question 52. Hunter’s glossitis is seen in:
1. Niacin deficiency
2. Vitamin C deficiency
3. Vitamin B12 deficiency
4. Riboflavin deficiency
Answer. 1. Niacin deficiency
Question 53. Intrinsic yellowish discoloration of teeth is due to:
1. High protein diet
2. Erythromycin
3. Penicillin
4. Tetracycline
Answer. 4. Tetracycline
Question 54. Decreased number of circulating platelets is called as:
1. Thrombocytopenia
2. Thrombocytosis
3. Thrombocythemia
4. Multiple myeloma
Answer. 1. Thrombocytopenia
Question 55. In geographic tongue there is desquamation of:
1. Fungiform papillae
2. Filiform papillae
3. Circumvallate papillae
4. Foliate papillae
Answer. 2. Filiform papillae
Question 56. Non-inflammatory, non-neoplastic enlargement of salivary gland is:
1. Sialolith
2. Sialosis
3. Ptyalism
4. Sialorrhea
Answer. 2. Sialosis
Question 57. Contact allergy is most accurately diagnosed by:
1. Penny test
2. Pathergy test
3. Patch test
4. Tuberculin test
Answer. 3. Patch test
Question 58. Which of the following is hereditary white lesion?
1. Leukoedema
2. Leukoplakia
3. Oral lichen planus
4. Oral submucous fibrosis
Answer. 1. Leukoedema
Question 59. Nystatin is a drug of choice for:
1. Lichen planus
2. Leukoplakia
3. Herpangina
4. Candidiasis
Answer. 4. Candidiasis
Question 60. Plicated tongue is a feature of:
1. Melkersson-Rosenthal syndrome
2. Vitamin deficiency
3. Hurler syndrome
4. Pierre-Robin syndrome
Answer. 1. Melkersson-Rosenthal syndrome
Question 61. Ely’s cyst is seen in:
1. Maxillary sinus
2. Maxilla
3. Condyle
4. Coronoid
Answer. 3. Condyle
Question 62. Tzanck smear test is used for:
1. Pemphigus
2. Lichen planus
3. Leukoplakia
4. Aphthous ulcer
Answer. 1. Pemphigus
Question 63. Triamcinolone acetonide is used in the management of:
1. Oral lichen planus
2. Aphthous ulcer
3. OSMF
4. All of the above
Answer. 4. All of the above
Question 64. Which among these have high recurrence rate:
1. Ameloblastoma
2. Radicular cyst
3. Dentigerous cyst
4. Odontogenic keratocyst
Answer. 4. Odontogenic keratocyst
Question 65. Multiple OKCs are seen in:
1. Gardner’s syndrome
2. Gorlin-Goltz syndrome
3. Greenspan syndrome
4. All of the above
Answer. 2. Gorlin-Goltz syndrome
Question 66. Petechiae are seen commonly in:
1. Diabetes mellitus
2. Hepatitis
3. Aplastic anemia
4. Hypothyroidism
Answer. 3. Aplastic anemia
Question 67. High recurrence rate is observed in:
1. Radicular cyst
2. Dentigerous cyst
3. Odontogenic keratocyst
4. Residual cyst
Answer. 3. Odontogenic keratocyst
Question 68. Oral and ocular lesions are seen in:
1. Behcet’s disease
2. OSMF
3. Leukoplakia
4. Scarlet fever
Answer. 1. Behcet’s disease
Question 69. Drug used in xerostomia:
1. Atropine
2. Beta blockers
3. Pilocarpine
4. Hyoscine
Answer. 3. Pilocarpine
Question 70. Tennis racquet appearance is seen in:
1. CGCG
2. Myxoma
3. Ameloblastoma
4. Fibrous dysplasia
Answer. 2. Myxoma
Question 71. Antioxidants do not include:
1. Beta carotene
2. Vitamin D
3. Vitamin C
4. Vitamin E
Answer. 2. Vitamin D
Question 72. Hepatitis B can be transmitted through:
1. Blood transfusion
2. Needle sharing
3. Homosexuals
4. All of the above
Answer. 4. All of the above
Question 73. Nikolsky’s sign can be elicited in the following lesions except:
1. Pemphigus vulgaris
2. Pemphigus vegetans
3. Mucous membrane pemphigoid
4. Epidermolysis bullosa
Answer. 2. Pemphigus Vegetans
Question 74. Complication of diabetes includes the following except:
1. Nephropathy
2. Neuropathy
3. Retinopath
4. Myopathy
Answer. 4. Myopathy
Question 75. Among the odontogenic cysts the most common is:
1. Radicular cyst
2. Dentigerous cyst
3. Odontogenic keratocyst
4. Residual cyst
Answer. 2. Dentigerous Cyst
Fill In The Blanks
Question 1. Most common site for hairy leukoplakia is ……………
Answer. Lateral border of tongue
Question 2. Lyell’s disease is complication of ……………
Answer. Toxic epidermal necrolysis
Question 3. HSV-l causes the lesions of ……………..
Answer. Upper body
Question 4. Hypoacusis, hypomobility of soft palate, VIII nerve neuralgia associated with nasopharyngeal mass is termed as ……………..
Answer. Wegner’s granulomatosis
Question 5. Deep, irregular, foul-smelling oral ulcer devoid of erythematous halo is seen in ……………..
Answer. Fungal infections
Question 6. Snow-driven appearance radiologically is seen in……………..
Answer. Calcifying epithelial odontogenic tumor
Question 7. Dens-in-Dente is most commonly associated with ……………..
Answer. Maxillary lateral incisor
Question 8. Multiple impacted teeth and odontoma are associated with osteoma is seen in ……………..
Answer. Gardner’s syndrome
Question 9. Generalized loss of lamina dura with generalized osteoporosis which is reversible after removal of endocrine tumor is seen in ……………..
Answer. Hyperparathyroidism
Question 10. Ground-glass appearance seen in ……………..
Answer. Paget’s disease
Question 11. Association of hypertension, diabetes mellitus and lichen planus is termed as ……………..
Answer. Gardner’s syndrome
Question 12. Hairy leukoplakia is caused by ……………..
Answer. Epstein-Barr virus
Question 13. Schirmer’s test is used for the diagnosis of ……………..
Answer. Sjögren’s syndrome
Question 14. Malignant tumors arising from mesenchymal tissues are known as ……………..
Answer. Sarcomas
Question 15. Nikolsky’s sign is a clinical feature of which disease……………..
Answer. Pemphigus vulgaris
Question 16. Pel-Ebstein type of fever is characteristic feature of……………..
Answer. Hodgkin’s Disease
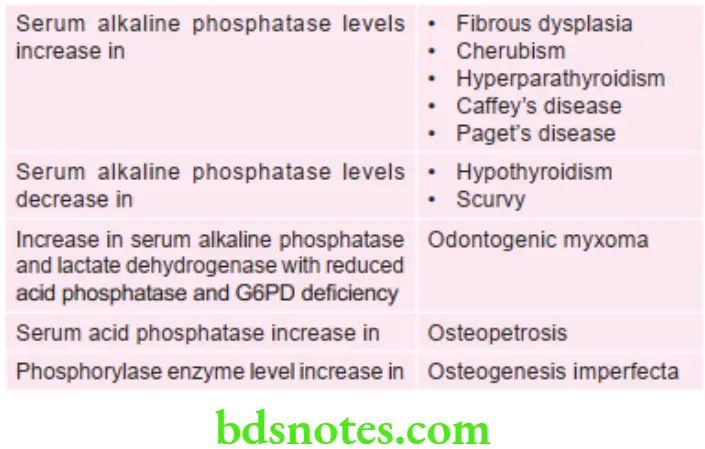
Question 17. The serum …………….. level is highly increased in Paget’s disease.
Answer. Alkaline phosphatase
Question 18. …………….. is the drug of choice for the treatment of xerostomia.
Answer. Pilocarpine
Question 19. The most common synonym of infectious mononucleosis……………..
Answer. Glandular fever
Question 20. The…………….. is common screening test in HIV infection/AIDS.
Answer. ELISA
Question 21. Drug of choice for the treatment of trigeminal neuralgia……………..
Answer. Carbamazepine
Question 22. Hairy leukoplakia is caused by…………….. virus.
Answer. Epstein-Barr virus
Question 23. Oral candidiasis is most commonly caused by…………….. Microorganism.
Answer. Fungal
Question 24. Deficiency of vitamin C causes……………..
Answer. Scorbutic gums
Question 25. The most common benign tumor of oral cavity is……………..
Answer. Fibroma
Question 26. The most commonest odontogenic tumor to occur is……………..
Answer. Odontoma
Question 27. Facial paralysis, herpes zoster of face, tinnitus and vertigo are typically seen in……………..
Answer. Post-herpetic syndrome
Question 28. Enlargement of jaws resulting in tightening of dentures is suggestive of……………..
Answer. Paget’s disease
Question 29. Aphthous ulceration, genital lesion, ocular involvement with arthritis is found in ……………..
Answer. Behçet’s Disease
Question 30. The term ghost teeth is synonymus with……………..
Answer. Regional odontodysplasia
Question 31. Hairy leukoplakia is caused by……………..
Answer. Epstein-Barr virus
Question 32. Typical unilateral vesiculobullous lesions which stop at the midline area are seen in……………..
Answer. Secondary varicella zoster or shingles
Question 33. Union of two or more teeth by cementum is known as……………..
Answer. Concrescence
Question 34. Chevostek’s sign is one of the diagnostic features of……………..
Answer. Tetany
Question 35. Reed-Sternberg cell is most commonly associated with……………..
Answer. Non-hodgkin’s lymphoma
Question 36. Oral lichen planus occurs most frequently on …………………..mucosa.
Answer. Buccal
Question 37. Dentigerous cyst is usually associated with ……………………..teeth.
Answer. Impacted
Question 38. ANUG is found in…………………..gingiva. The most common odontogenic cyst is…………………….
Answer. Radicular cyst
Question 39. Taurodontism is associated with………………syndrome. Drug of choice in herpes simplex virus infection is ……………………….
Answer. Acyclovir
Question 40. Mumps is caused by………………. virus
Answer. Paramyxovirus
Question 41. Fothergill’s disease is also called as……………………
Answer. Trigeminal neuralgia
Question 42. Most common benign salivary gland tumor of parotid gland is……………………
Answer. Pleomorphic adenoma
Question 43. Treponema palladium spirochete bacterium causes …………………..
Answer. Syphilis
Question 44. Candidiasis is caused by……………………………..
Answer. Candida albicans
Question 45. Koebner’s phenomenon is a diagnostic feature of…………………………..
Answer. Lupus erythematosus
Question 46. Cyst associated with a non-vital tooth is called as…………………………
Answer. Radicular cyst
Question 47. The most common odontogenic tumor of head and neck area is…………………
Answer. Ameloblastoma
Question 48. The teeth with the longest root is……………………..
Answer. Canine
Question 49. Herpes infection above the waist is caused by………………….
Answer. Herpes simplex Virus – 1 (HSV – 1)
Question 50. Gingival lesions associated with erosive lichen planus is…………………..
Answer. Desquamative
Question 51. Eagle’s syndrome associated with morphological bony changes in…………………
Answer. Styloid process
Question 52. Painful long duration multinodular pleomorphic adenoma with adhesions is suggestive of…………….
Answer. Metastasizing pleomorphic adenoma
Question 53. Secondary oral syphilis lesion is……………..
Answer. Mucous patches
Question 54. Drug of choice in dentoalveolar abscess is………………
Answer. Metronidazole
Question 55. Most common infection in HIV/AIDS is………………….
Answer. Oral candidiasis
Question 56. Gingival involvement is seen in……………………deficiency.
Answer. Vitamin C
Question 57. Café au lait spots are seen in………………..
Answer. Neurofibromatosis
Question 58. Stone in salivary gland is called…………….
Answer. Sialolith
Question 59. A keratotic white lesion found on the oral mucosa adjacent to a restoration is most likely to be……………………..
Answer. Lichenoid reaction
Question 60. ‘Mask-like’ facies, rigidity of tongue, reduction in mouth opening, fibrosis of buccal mucosa are all features of…………………….
Answer. Scleroderma
Question 61. Localized gingival enlargement, adjacent to a large carious tooth, with pulpal involvement and history of pus discharge from adjoining gingiva is known as…………………
Answer. Periodontal abscess
Question 62. Infectious mononucleosis is caused by…………………
Answer. Epstein Barr Virus
Question 63. Submandibular swelling associated with intake of food, which regress after a couple of hours is due to………………………
Answer. Stone formation
Additional Information
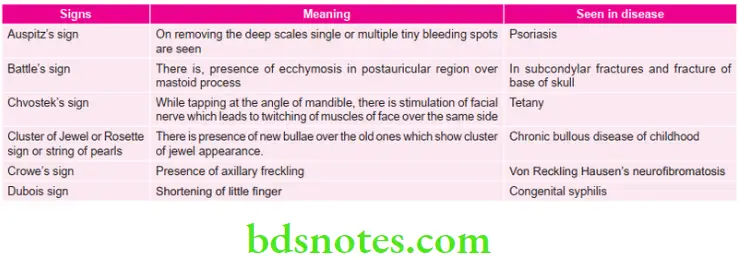
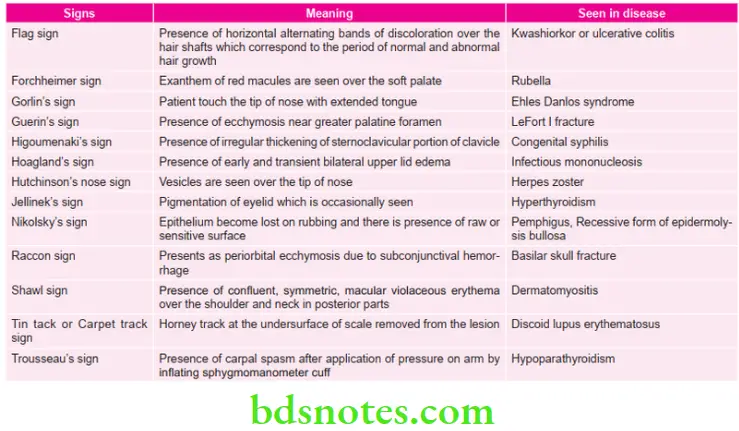
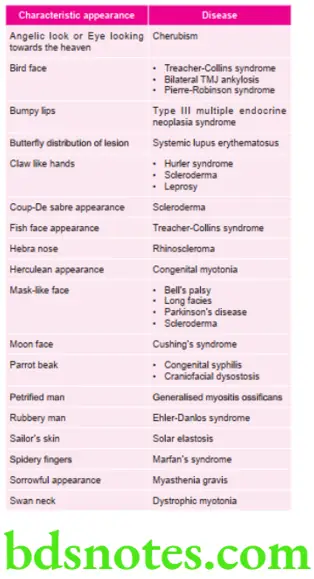
Various Signs in Oral Medicine
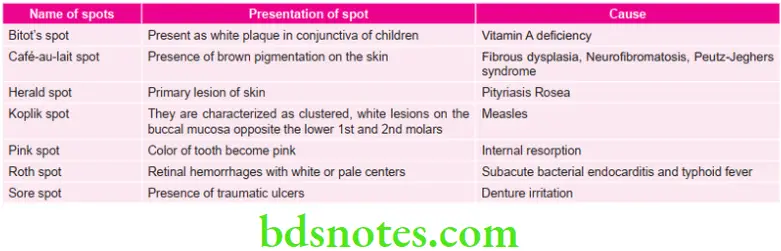
Various Spots in Oral Medicine Diagnosis
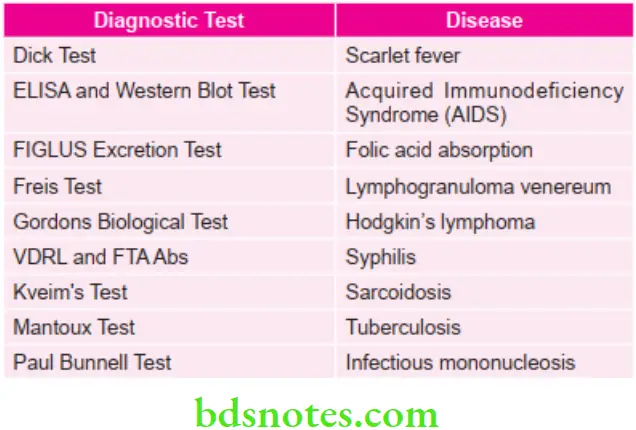
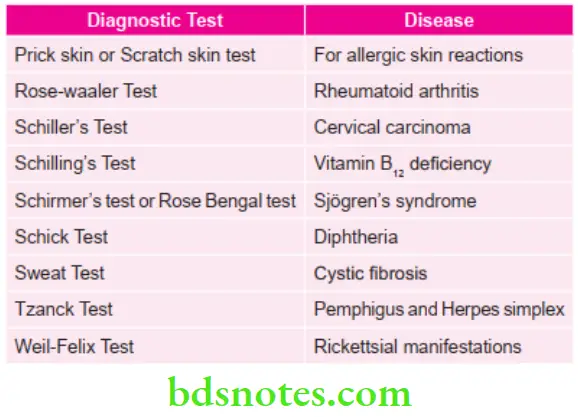
Various Important Diagnostic Tests for Various Diseases
FIGLU: folic acid deficiency, formiminoglutamic
Incubation Periods of Various Diseases

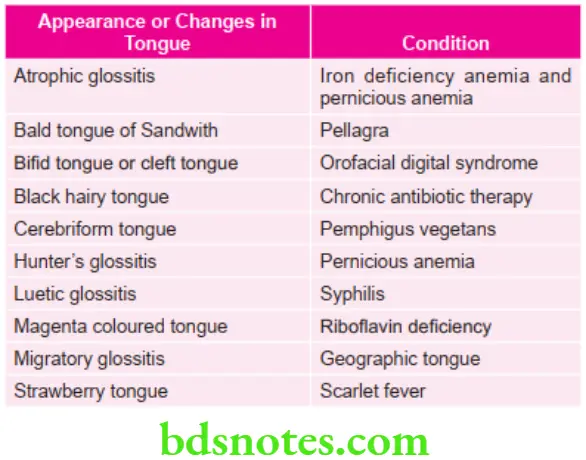
Characteristic Features of Tongue in Various Conditions
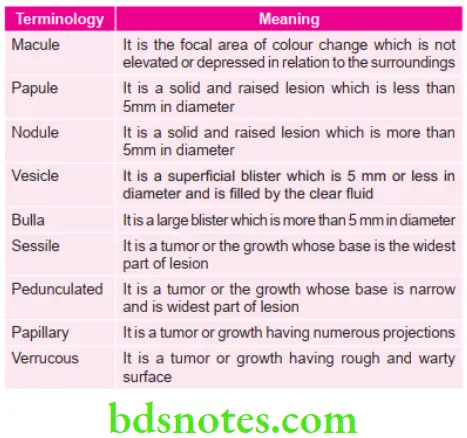
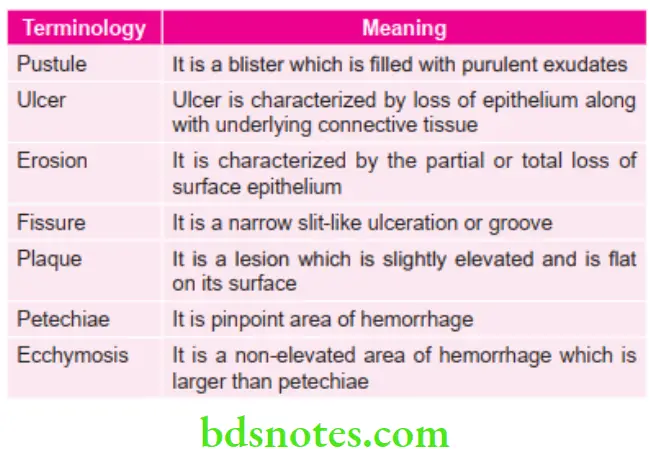
Important Terminologies with Their Meanings in Oral Pathology
Various appearances and Diseases Associated with them
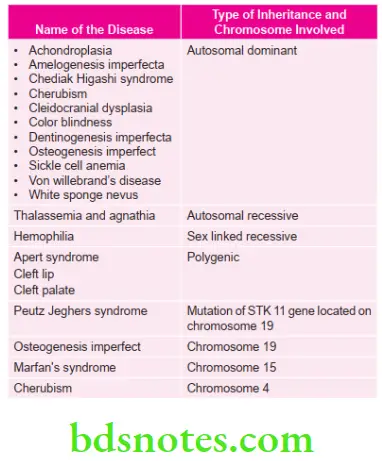
Various Genetically Transmitted Diseases
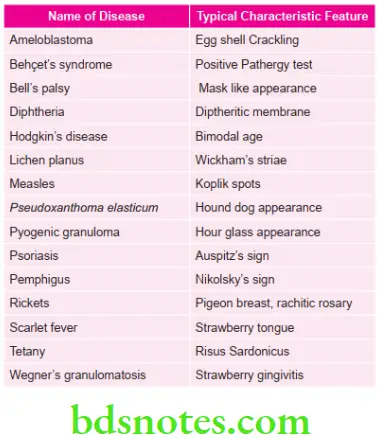
Various Typical Characteristic Features of Lesions
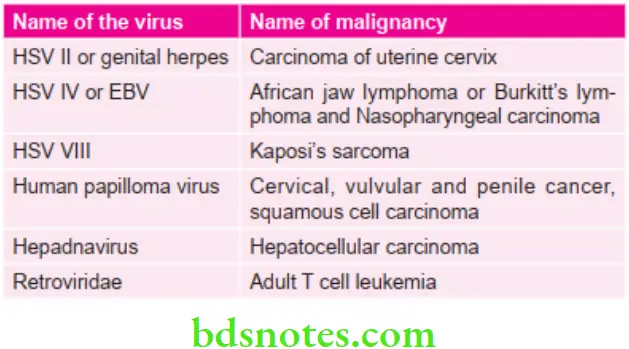
Various malignancies caused by viruses
Various surgeries and their indications
Important information about carcinomas
Levels of various enzymes in diseases
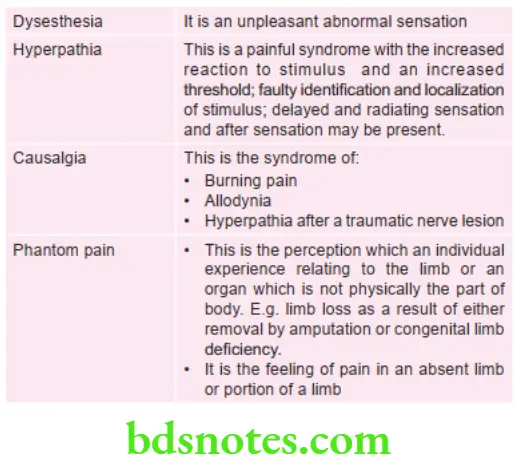
Taxonomy of pain
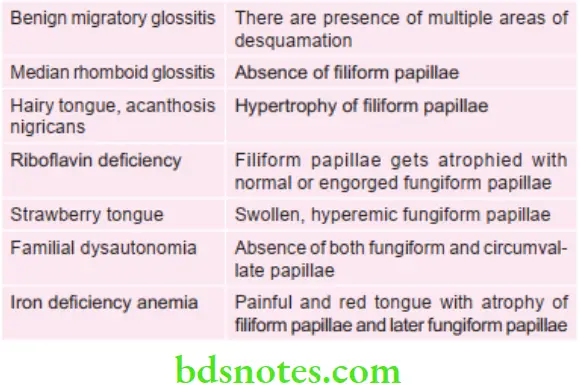
Various conditions of tongue and effect on papilla
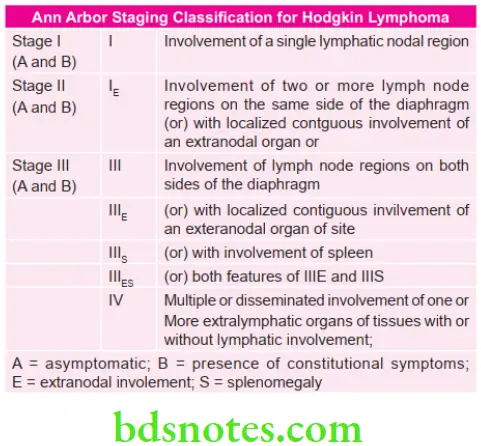
Various Important Classifications
Classification of Supernumerary Teeth
According to morphology
- Conical: This small peg shaped conical tooth is supernumerary tooth.
- Tuberculate: This type of supernumerary tooth possesses more than one cusp or tubercle. It is of barrel shaped and may be invaginated.
- Supplemental: It refers to the duplication of the teeth in normal series. The most common tooth is permanent maxillary lateral incisor.
- Odontome: This represents the hamartomatous malformation.
According to location
- Mesiodens: They are located between two upper central incisors.
- Distomolars: They are located on the distal aspect of regular molar teeth in dental arch.
- Paramolar: They are located either in buccal or lingual aspect of normal molars.
- Extra lateral incisors: They are more common in maxillary arch.
Classification of Amelogenesis Imperfecta
Witkop, 1988 Four major categories based primarily on phenotype (hypoplastic, hypomaturation, hypocalcified, hypomaturationhypoplastic with taurodontism) subdivided into 15 subtypes by phenotype and secondarily by mode of inheritance.
- Type 1. Hypoplastic
- Type 1A. Hypoplastic, pitted autosomal dominant
- Type 1B. Hypoplastic, local autosomal dominant
- Type I1C. Hypoplastic, local autosomal recessive
- Type 1D. Hypoplastic, smooth autosomal dominant
- Type 1E. Hypoplastic, smooth X-linked dominant
- Type 1F. Hypoplastic, rough autosomal dominant
- Type 1G. Enamel agenesis, autosomal recessive
- Type 2. Hypomaturation
- Type 2A. Hypomaturation, pigmented autosomal recessive
- Type 2B. Hypomaturation, X-linked recessive
- Type 2C. Hypomaturation, snow-capped teeth, X-linked
- Type 2D. Hypomaturation, snow-capped teeth, autosomal dominant?
- Type 3A. Autosomal dominant
- Type 3B. Autosomal recessive
- Type 4. Hypomaturation-hypoplastic with taurodontism
- Type 4A. Hypomaturation-hypoplastic with taurodontism, autosomal dominant
- Type 4B. Hypoplastic-hypomaturation with taurodontism, autosomal dominant
Classification of White Lesions of Oral Cavity
- Hereditary condition:
- Leukoedema
- White sponge nevus
- Hereditary benign intraepithelial dyskeratosis
- Keratosis follicularis
- Ptylosis syndrome.
- Leukoplakia and malignancies:
- Chronic cheek biting
- Friction or trauma associated leukoplakia
- Tobacco associated leukoplakia
- Carcinoma in situ
- Squamous cell carcinoma
- Verrucous carcinoma.
- Dermatosis:
- Lichen planus
- Lupus erythematous.
- Inflammation:
- Mucous patches of syphilis
- Candidiasis
- Koplik spots of measles.
- Miscellaneous conditions:
- Oral submucous fibrosis
- Papilloma
- Lipoma
- Hairy tongue
- Geographic tongue
- Fordyce’s granules.
Classification of Hemangiomas by Watson and McCarthy
- Capillary hemangioma
- Cavernous hemangioma
- Angioblastic hemangioma
- Racemose hemangioma
- Diffuse systemic hemangioma
- Metastasizing hemangioma
- Port-Wine Stain
- Hereditary hemorrhagic telangiectasia
Classification of Giant Cell Lesions of Oral Cavity
According to the Nature of Different Pathologic Conditions
- Infections
- Bacterial
- Viral
- Fungal
- Protozoal
- Parasitic
- Fibro-Osseous Lesions and Osteodystrophies
- Immunologic
- Idiopathic
- Orofacial granulomatosis
- Reaction to Materials
- Benign and Malignant Tumors
In This Classification Giant Cells are Categorized into Three Categories
Giant cells are the main cause for the pathology
Giant cells characterize these lesions
Lesions that may be associated with giant cells
- Main Cause for the Pathology
- Giant Cell Granuloma
- Peripheral
- Central
- Giant Cell Tumors
- Giant Cell Fibroma
- Hyperparathyroidism
- Giant Cell Granuloma
- Giant Cells that Characterize Lesions
- Infections:
- Tuberculosis
- Hansen’s disease
- Syphilis
- Measles
- Granulomatous lesions:
- Wegener’s granulomatosis
- Orofacial granulomatosis
- Pulse granuloma
- Sarcoidosis
- Lesions in bone:
- Aneurysmal bone cyst
- Cherubism
- Paget’s disease
- Foreign body lesions
- Silicosis
- Berylliosis
- Malignancies:
- Lymphoma—Hodgkin’s disease
- Bronchogenic carcinoma
- Carcinoma of thyroid
- Miscellaneous:
- Xanthoma
- Giant cell arteritis
- Infections:
- Lesions that may be associated with giant cell
- Malignancies:
- Multiple myeloma
- Ewing’s sarcoma
- Fibrosarcoma
- Chondrosarcoma
- Fibro-osseous lesions
- Osteoblastoma
- Fibrous dysplasia
- Cemento-ossifying fibroma
- Radicular cyst
- Malignancies:
Based on their origin
- Epithelially derived, i.e. Warthin-finkeldey giant cells, tumor giant cells
- Stromally derived, i.e. Reed-Sternberg giant cells.
Enumeration of Premalignant Lesion
- Leukoplakia
- Erythroplakia
- Mucosal changes associated with smoking habits
- Carcinoma in situ
- Bowen disease
- Actinic keratosis, actinic cheilitis and actinic elastosis.
Enumeration of Premalignant Condition
- Syphilis
- OSMF
- Oral lichen planus
- Sideropenic dysplasia
- Dyskeratosis congenita
- Lupus erythematosus
Unusual Variants of Squamous Cell Carcinoma
- Verrucous carcinoma
- Spindle cell carcinoma
- Basaloid squamous cell carcinoma
- Adenoid/acantholytic squamous cell carcinoma
- Papillary squamous cell carcinoma
- Carcinoma cuniculatum
Latest Who 2017 Classification Of Odontogenic Tumors And Cysts
WHO (2017) Classification of Odontogenic Tumors
Malignant Odontogenic Tumors
- Ameloblastic carcinoma
- Primary intraosseous carcinoma, NOS
- Sclerosing odontogenic carcinoma
- Clear cell odontogenic carcinoma
- Ghost cell odontogenic carcinoma
- Odontogenic carcinosarcoma
- Odontogenic sarcomas
Benign Odontogenic Tumors
- Epithelial Origin
- Ameloblastoma, conventional
- Ameloblastoma, unicystic type
- Ameloblastoma, extraosseous/peripheral type
- Metastasizing (malignant) ameloblastoma
- Squamous odontogenic tumor
- Calcifying epithelial odontogenic tumor
- Adenomatoid odontogenic tumor
- Mixed (Epithelial-Mesenchymal) Origin
- Ameloblastic fibroma
- Primordial odontogenic tumor
- Odontoma
- Compound type
- Complex type
- Dentinogenic ghost cell tumor
- Mesenchymal Origin
- Odontogenic fibroma
- Odontogenic myxoma/myxofibroma
- Cementoblastoma
- Cemento-ossifying fibroma
WHO (2017) Classification of Odontogenic Cysts
Developmental Origin
- Dentigerous cyst
- Odontogenic keratocyst
- Lateral periodontal and botryoid odontogenic cyst
- Gingival cyst
- Glandular odontogenic cyst
- Calcifying odontogenic cyst
- Orthokeratinized odontogenic cyst
Inflammatory Origin
- Radicular cyst
- Collateral inflammatory cyst
Classification of Non-Odontogenic Tumors of Oral Cavity
Epithelial Tissue
- Benign Tumors
- Papilloma
- Keratoacanthoma
- Squamous acanthoma
- Nevus
- Malignant Tumors
- Squamous cell carcinoma
- Mucoepidermoid carcinoma
- Adenocarcinoma
- Basal cell carcinoma
- Transitional cell carcinoma
- Melanoma
- Verrucous carcinoma
- Intraepidermoid carcinoma
Fibrous Connective Tissue
- Benign Tumors
- Fibroma
- Fibrous hyperplasia
- Fibrous epulis
- Giant cell fibroma
- Myxoma
- Myxofibroma.
- Malignant Tumors
- Fibrosarcoma
Cartilage Tissue
- Benign Tumors
- Chondroma
- Chondroblastoma
- Chondromyxoid fibroma.
- Malignant Tumors
- Chondrosarcoma
Adipose Tissue
- Benign Tumors
- Lipoma
- Angiolipoma.
- Malignant Tumors
- Liposarcoma
Bone
- Benign Tumors
- Osteoma
- Osteoid osteoma
- Osteoblastoma
- Malignant Tumors
- Osteosarcoma
- Osteochondrosarcoma
Vascular tissue
- Benign Tumors
- Hemangioma
- Hereditary hemorrhagic telangiectasia
- Lymphangioma
- Malignant Tumors
- Hemangioendothelioma
Neural tissue:
- Benign Tumors
- Neurofibroma
- Neurilemmoma
- Schwannoma
- Malignant Tumors
- Neurosarcoma
- Neurofibrosarcoma
Muscles
- Benign Tumors
- Leiomyoma
- Rhabdomyoma
- Malignant Tumors
- Leiomyosarcoma
- Rhabdomyosarcoma
Giant Cell Tumor
- Central and peripheral giant cell tumor
- Giant cell granuloma
- Giant cell tumor of hyperthyroidism.
Teratoma
Salivary Gland Tumor
- Benign Tumors
- Adenoma
- Warthin’s tumor
- Pleomorphic adenoma.
- Malignant Tumors
- Mucoepidermoid carcinoma
- Adenocystic carcinoma
- Adenocarcinoma
- Acinic cell carcinoma
- Malignant change in pleomorphic adenoma
Lymphoid Tissue
- Malignant Tumors
- Hodgkin’s and non-hodgkin’s lymphoma
- Lymphosarcoma
- Reticular cell sarcoma
- Ewing’s sarcoma
- Burkitt’s lymphoma
- Multiple myeloma
- Leukemia.
Classification of Oral Submucous Fibrosis
Khanna JN and Andrade N (1995) develop classification of OSMF based on clinical features and histopathological features
Group 1: Very Early Cases
- Common symptom is burning sensation in the mouth
- Acute ulceration and recurrent stomatitis
- Not associated with mouth opening limitation
Histology
- Fine fibrillar collagen network interspersed with marked edema
- Blood vessels are dilated and congested
- Largest aggregate of plump, young fibroblasts present in abundant cytoplasm
- Inflammatory cells mainly consists of PMN leukocytes with few eosinophils
- Epithelium is normal.
Group 2: Early cases
- Buccal mucosa appears mottled and marble like
- Widespread sheets of fibrosis palpable
- Patients with inter-incisal distance of 26 to 35 mm
Histology
- Juxtaepithelial hyalinization present
- Collagen presents as thickened but separate bundles
- Blood vessels are dilated and congested
- Young fibroblasts are seen in moderate number
- Inflammatory cells mainly consists of polymorphonuclear leukocytes with few eosinophils and occasional plasma cells
- Flattening or shortening of epithelial rete pegs evident with varying degree of keratinization.
Group 3: Moderately Advanced Cases
- Trismus evident with inter-incisal distance of 15 to 25 mm
- Buccal mucosa appears pale and firmly attached to underlying tissues
- Atrophy of vermilion border
- Vertical fibrous bands are palpable at soft palate, pterygomandibular raphae and anterior faucial pillars
Histology
- Juxtaepithelial hyalinization present
- Thickened collagen bundles faintly discernable separated by very light residual edema
- Blood vessels are mostly constricted
- Mature fibroblasts with scanty cytoplasm and spindleshapes nuclei
- Inflammatory exudates consists mainly of lymphocytes and plasma cells
- Epithelium is markedly atrophic with loss of rete pegs
- Muscle fibers seen interspersed with thickened and dense collagen fibers
Group IV A: Advanced Cases
- Trismus is severe with interincisal distance less than 15 mm
- The fauces are thickened, shortened and firm on palpation
- Uvula is shrunken and appears as small, fibrous bud
- Tongue movements get limited
- On palpation of lips, circular bands are felt at around entire mouth
Group 4B: Advanced Cases with Premalignant and Malignant Changes
Hyperkeratosis, leukoplakia or squamous cell carcinoma can be seen.
Histology
- Collagen hyalinized as small sheet
- Extensive fibrosis obliterates the mucosal blood vessel and eliminates melanocytes
- Fibroblasts were markedly absent within hyalinized zones
- Total loss of epithelial rete pegs
- Mild-to-moderate atypia present
- Extensive degeneration of muscle fibers evident.
Classification of Oral Hamartomas
- Those involving teeth
- Dens invaginatus
- Dens evaginatus
- Talon cusp
- Those not involving teeth
- Peripheral odontogenic fibroma
- Ameloblastic fibro-odontoma
- Odontoma
- Adenomatoid odontogenic tumor
- Squamous odontogenic tumor
- Dental lamina cyst of newborn
- Non-odontogenic origin
- Vascular origin
- Hemangioma
- Lymphangioma
- Glomus tumor
- Osseous origin
- Fibrous dysplasia
- Oral and labial melanotic macule
- Pigmented cellular nevus
- Vascular origin
- Neural origin
- Neurofibromatosis
- Syndrome
- Multiple hamartoma syndrome
- Salivary gland
- Adenomatoid hyperplasia of mucous glands
Enumeration of round cell tumors
- Lymphoma
- Rhabdomyosarcoma
- Melanoma
- Ewing’s sarcoma
- Glomus tumor
- Esthesioneuroblastoma
- Merkel cell tumor
- Adenocarcinoma
- Squamous cell carcinoma (poorly differentiated)
- Plasmacytoma
- Multiple myeloma
- Langerhan’s cell disease
- Peripheral neuroectodermal tumor
Enumeration of Lesions Associated with Impacted Tooth
- Cysts:
- Dentigerous cyst
- Keratocystic odontogenic tumor
- Calcifying odontogenic cyst
- Salivary gland:
- Mucoepidermoid carcinoma (central variety)
- Odontogenic tumors:
- Central odontogenic fibroma
- Ameloblastic fibroma
- Ameloblastic fibro odontome
- Odontoma
- Adenomatoid odontogenic tumor
- Squamous odontogenic tumor
- Unicystic ameloblastoma
Enumeration of Clear Cell Lesions
- Clear cell carcinoma
- Clear cell ameloblastic carcinoma
- Clear cell odontogenic tumor
- Mucoepidermoid carcinoma
- Oncocytoma
- Epimyoepithelial carcinoma
- Acinic cell adenocarcinoma
- Clear cell ameloblastoma
- Clear cell chondrosarcoma
Enumeration of granular cell diseases
- Granular cell in salivary gland diseases
- Oncocytoma
- Acinic cell carcinoma
- Warthin’s tumor
- Oncocytic carcinoma
- Oncocytosis
- Oncocytic variant of mucoepidermoid carcinoma
- Sclerosing polycytic adenosis
- Pleomorphic adenoma
- Granular cell in odontogenic tumors
- Granular cell ameloblastoma
- Granular cell ameloblastic fibroma
- Granular cell adontogenic tumor
- Granular cells in soft tissue tumors
- Granular cell tumor (Myoblastoma, Schwanoma)
- Congenital epulis
- Rhabdomyoma
- Rhabdomyosarcoma
- Alveolar soft part sarcoma
- Verruciform xanthoma
- Fibrous histiocytoma
- Langerhans cell histiocytosis
- Granular cells in viral, fungal and bacterial infections
- Molluscum contagiosum
- Botryomycosis
- Histoplasmosis
TNM Classification By American Joint Committee on Carcinoma (AJCC)
T is suggestive of primary tumor
N is suggestive of regional lymph nodes
M is suggestive of distant metastasis
T – primary Tumor
- TX – Primary tumor cannot be assessed.
- T0 – No evidence of primary tumor
- Tis – Carcinoma in Situ
- T1 – Tumor 2 cm of less in greatest dimension
- T2 – Tumor more than 2 cm but not more than 4 cm in greatest dimension
- T3 – Tumor more than 4 cm in greatest dimension
- T4a (Lip) – Tumor invades through cortical bone, inferior alveolar nerve, floor of mouth or skin (chin or nose)
- T4a (Oral Cavity) – Tumor invades through cortical bone, into deep/extrinsic muscle of tongue (genioglossus, hyoglossus, palatoglossus and styloglossus), maxillary sinus or skin of face.
- T4b (lip and oral cavity) – Tumor invades masticatory space, pterygoid plates or skull base or encases internal carotid artery
- N – Regional lymph nodes
- NX – Regional lymph nodes cannot be assessed
- N0 – No regional lymph node metastasis
- N1 – Metastasis in a single ipsilateral lymph node, 3 cm or less in greatest dimension
- N2a – Metastasis in a single ipsilateral lymph node, more than 3 cm but not more than 6 cm in greatest dimension
- N2b – Metastasis in multiple ipsilateral lymph nodes, not more than 6 cm in greatest dimension
- N2c – Metastasis in bilateral or contralateral lymph nodes, not more than 6 cm in greatest dimension
- N3 – Metastasis in a lymph node more than 6 cm in greatest dimension
- M – Distant Metastasis
- MX – Distant metastasis cannot be assessed
- M0 – No distant metastasis
- M1 – Distant metastasis
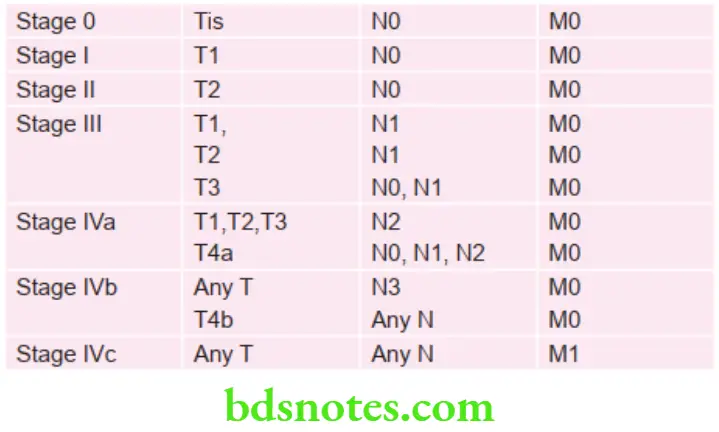
Stage Grouping of Oral Cancer
Grading of Squamous Cell Carcinoma
Grading is defined as macroscopic and microscopic degree of differentiation of a tumor.
Squamous cell carcinoma is divided in following categories by Broder also known as Broader’s classification
Grade 1: Well differentiated, i.e. less than 25% anaplastic cells
This is characterized by the presence of relatively mature cell with little nuclear aberration and with presence of keratin pearls and individual cell keratinization.
Grade 2: Moderately differentiated, i.e. 25–50% anaplastic cells
This is characterized by the presence of tumor cell exhibiting a wide range of differentiation, keratinization is occasionally present and nuclear aberrations are moderately abundant. Invasion is poor delineated from stroma.
Grade 3: Moderately differentiated, i.e. 50–75% anaplastic cells
This is characterized by the presence of disordered and poorly differentiated cells with no tendency towards keratinization, nuclear aberrations are abundant.
Grade 4: Poorly differentiated i.e. more than 75% anaplastic cells
This is characterized by the presence of cells which are so poorly differentiated that they cannot be identified as epithelial origin on basis of histology, nuclear aberrations are abundant and no keratinization is present.
STNMP Classification of Oral Squamous Cell Carcinoma
S Category
S (Site)
S1 Lip – Skin
S2 Lip – Mucous membrane
S3 Tongue
S4 Cheek
S5 Palate
S6 Floor of the mouth
S7 Alveolar process
S8 Antrum
S9 Central carcinoma of bone
T Category
T (Tumor)
T1 – Tumor less than 20 mm in diameter
T2 – Tumor between 20 mm and 40 mm in diameter
T3 – Tumor between 40 mm and 60 mm in diameter and/or extend beyond the primary region and/or through adjacent periosteum
T4 – Any tumor greater than 60 mm in diameter and/or extending to involve adjacent structure
N Category
N (Node)
N0 – No palpable nodes
N1 – Equivocal node enlargement
N2 – Clinically palpable homolateral regional node (s) – not fixed
N3 – As N2 but fixed
N4 – Clinically palpable contralateral or bilateral node (s) – not fixed
N5 – As N4 but fixed
M Category
M (Metastases)
M0 – No distant metastasis
M1 – Clinical evidence of distant metastasis without definite histological and/ or radiographic confirmation
M2- Proven evidence of metastasis beyond the regional nodes
P Category
P (Pathology)
P0 – Hyperkeratotic lesion showing atypia
P1 – Carcinoma in situ
P2 – Basal cell carcinoma
P3a – Verrucous carcinoma
P3b – Well-differentiated squamous cell carcinoma
P3c – Moderately differentiated squamous cell carcinoma
P3d – Poorly differentiated squamous cell carcinoma150 Mastering the BDS IVth Year-I (Last 25 Years Solved Questions)
STNMP Weighting and Stages
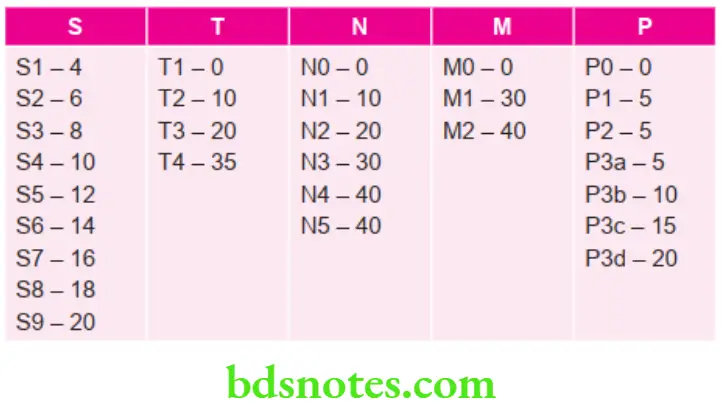
For convenience and to enable direct comparison with TNM staging, the scores are banded to form similar stages
Stage 1 – 0 to 30
Stage 2 – 31 to 50
Stage 3 – 51 to 70
Stage 4 – 70 to 155
Salivary Gland Tumor Classification by WHO (2005)
- Benign Epithelial Tumors
- Pleomorphic adenoma (8940/0)
- Myoepithelioma (8982/0)
- Basal cell adenoma (8147/0)
- Warthin tumor (adenolymphoma) (8561/0)
- Oncocytoma (oncocytic adenoma) (8290/0)
- Canalicular adenoma (8149/0)
- Sebaceous adenoma (8410/0)
- Lymphadenoma (8410/0)
- Sebaceous
- Nonsebaceous
- Ductal papilloma (8503/0)
- Inverted ductal papilloma
- Intraductal papilloma
- Sialadenoma papilliferum
- Cystadenoma (8440/0)
- Malignant epithelial tumors
- Acinic cell carcinoma (8550/3)
- Mucoepidermoid carcinoma (8430/3)
- Adenoid cystic carcinoma (8200/3)
- Polymorphous low-grade adenocarcinoma
- Epithelial-myoepithelial carcinoma (8562/3)
- Clear cell carcinoma, not otherwise specified (8310/3)
- Basal cell adenocarcinoma (8147/3)
- Sebaceous carcinoma (8410/3)
- Sebaceous lymphadenocarcinoma (8410/3)
- Cystadenocarcinoma (8440/3)
- Low-grade cribriform cystadenocarcinoma
- Mucinous adenocarcinoma (8480/3)
- Oncocytic carcinoma (8290/3)
- Salivary duct carcinoma
- Adenocarcinoma NOS (8140/3)
- Myoepithelial carcinoma (8982/3)
- Carcinoma in pleomorphic adenoma (8941/3)
- Carcinosarcoma (8980/3)
- Metastatizing pleomorphic adenoma (8940/1)
- Squamous cell carcinoma (8070/3)
- Small cell carcinoma (8041/3)
- Large cell carcinoma (8012/3)
- Lymphoepithelial carcinoma (8082/3)
- Sialoblastoma (8974/1)
- Soft tissue tumors
- Hemangioma (9120/0)
- Hematolymphoma tumors
- Hodgkin’s lymphoma
- Diffuse large B cell lymphoma
- Extranodal marginal zone B cell lymphoma
- Secondary tumors
Classification of Odontogenic Tumors by WHO (2005)
Benign Tumors
- Odontogenic Epithelium with Mature Fibrous Stroma without Odontogenic Mesenchyme:
- Ameloblastoma (Solid, Multicystic, Extraosseous, Peripheral, Desmoplastic, Unicystic)
- Squamous Odontogenic Tumor
- Calcifying Epithelial Odontogenic Tumor
- Adenomatoid Odontogenic Tumor
- Keratocystic Odontogenic Tumor
- Odontogenic Epithelium with Odontogenic Ectomesenchyme with or without hard tissue formation:
- Ameloblastic Fibroma
- Ameloblastic Fibro-Dentinoma
- Ameloblastic Fibro-Odontoma
- Odontoma
- Complex
- Compound
- Odonto-Ameloblastoma
- Calcifying Cystic Odontogenic Tumor
- Dentinogenic Ghost Cell Tumor
- Mesenchyme and/or Odontogenic Ectomesenchyme with or without Odontogenic Epithelium:
- Odontogenic Fibroma
- Odontogenic Myxoma
- Cementoblastoma
Malignant Tumors
- Odontogenic Carcinomas:
- Malignant Ameloblastoma
- Ameloblastic Carcinoma
- Primary Intraosseous Carcinoma
- Clear Cell Odontogenic Carcinoma
- Ghost Cell Odontogenic Carcinoma
- Odontogenic Sarcoma:
- Ameloblastic Fibro-Sarcoma
- Ameloblastic Fibro-Dentino Sarcoma
- Ameloblastic Fibro-Odonto-Sarcoma.
Bone related Lesions
- Ossifying Fibroma
- Fibrous Dysplasia
- Osseous Dysplasia
- Central Giant Cell Lesions
- Cherubism
- Aneurysmal Bone Cyst
- Simple Bone Cyst
Melanotic Neuroectodermal Tumor of Infancy.
Classification of Odontogenic Ghost Cell Lesions (By Praetorious 2006)
Group 1: Simple cysts – Calcifying odontogenic cyst
Group 2: Cyst associated with odontogenic hamartomas or benign neoplasms – Calcifying cystic odontogenic tumor (CCOT). Following are the combinations:
- CCOT associated with odontome
- CCOT associated with adenomatoid odontogenic tumor
- CCOT associated with Ameloblastoma
- CCOT associated with Ameloblastic fibroma
- CCOT associated with Ameloblastic fibro odontome
- CCOT associated with Odonto-ameloblastoma
- CCOT associated with odontogenic myxofibroma
Group 3: Solid benign odontogenic neoplasms with similar cell morphology to that in calcifying odontogenic cyst and with dentinoid formation – Dentinogenic ghost cell tumor
Group 4: Malignant odontogenic neoplasms with features similar to those of dentinogenic ghost cell tumor – Ghost cell odontogenic carcinoma
Classification of Cyst by Mervin Shear
Cysts of the Jaws
Epithelial:
- Developmental:
- Odontogenic:
- Gingival Cyst of Infants
- Odontogenic Keratocyst (Neoplasm)
- Dentigerous Cyst
- Eruption Cyst
- Lateral Periodontal Cyst
- Gingival Cyst of Adults
- Botryoid Odontogenic Cyst
- Glandular Odontogenic Cyst
- Calcifying Odontogenic Cyst (Neoplasm)
- Non-Odontogenic:
- Nasopalatine Duct Cyst
- Naso Labial Cyst
- Midpalatal Raphe Cyst of Infants
- Median Palatine, Median Alveolar
- Median Mandibular Cyst
- Globulo Maxillary Cyst
- Odontogenic:
- Inflammatory:
- Radicular Cyst, Apical and Lateral
- Residual Cyst
- Paradental Cyst and Mandibular Infected Buccal Cyst
- Inflammatory Collateral Cyst
Non-epithelial (Pseudo cysts)
- Solitary Bone Cyst
- Aneurysmal Bone Cyst
Cyst Associated With Maxillary Antrum
- Benign Mucosal Cyst of the Maxillary Antrum
- Postoperative Maxillary Cyst
Cyst of the Soft Tissues of Mouth, Face and Neck
- Dermoid and epidermoid cyst
- Lymphoepithelial cyst (branchial cyst)
- Thyroglossal duct cyst
- Anterior medial lingual cyst (intralingual cyst of foregut origin)
- Oral cyst with gastric or intestinal epithelium
- Cystic hygroma
- Nasopharyngeal cyst
- Thymic cyst
- Cyst of salivary glands—mucous extravasation cyst
- Mucous retention cyst, ranula, polycystic disease of the parotid.
- Parasitic cyst—hydatid cyst, cysticercus cellulosae, trichinosis.
Classifications of Viral Lesions in Oral Cavity
RNA Virus
- Orthomyxovirus, i.e. Influenza
- Paramyxovirus, i.e. Measles and mumps
- Rhabdovirus, i.e. Rabies
- Arenavirus, i.e. Lassa fever
- Calicivirus, i.e. upper respiratory tract infection
- Coronavirus
- Bunyavirus
- Picornavirus
- Reovirus
- Togavirus
- Retrovirus
DNA Virus
- Herpes virus
- Herpes simplex
- Herpes zoster
- Epstein-Barr virus
- Pox virus
- Smallpox
- Monkey pox
- Adenovirus, i.e. pharyngoconjunctival fever
- Parvovirus
- Iridovirus
- Papova virus, i.e. papillomas.
Classification of Ulcerative Lesions
Microbial Origin
- Bacterial:
- Streptococcal
- Tuberculosis
- Syphilis
- Scarlet fever
- Diphtheria
- Typhoid
- Noma
- Fungal:
- Histoplasmosis
- Blastomycosis
- Paracoccidioidomycosis
- Coccidioidomycosis
- Cryptococcus
- Zygomycosis
- Aspergillosis
- Viral:
- Herpes
- HIV
- Pox virus
- Protozoal:
- Entamoeba histolytica
- Leishmaniasis
- Toxoplasmosis
Physical Origin
- Cheek bite (Morsicatio buccarum)
- Traumatic
- Thermal
- Electrical
- Osteoradionecrosis
- Anesthetic
Chemical Origin
- Phenol
- Silver nitrate
- Hydrogen peroxide
- Aspirin
Immunological
- BehÇet’s syndrome
- Reiter’s syndrome
- Erythema multiforme
- Erosive Lichen Planus ( Secondary Ulcer)
- Lupus Erythematosus
- Sarcoidosis
- Cyclic Neutropenia
- Ulcerative Colitis
- HIV
- Pemphigus
- Epidermolysis Bullosa
Metabolic Ulcers
- Diabetes
- Uremia
- Neutropenia
- Sickle Cell Anemia
- Agranulocytosis
- Crohn’s Disease
NonSpecific Ulcers
- HIV Ulcers
- Graft versus Host Reaction
- Necrotizing Sialometaplasia
- Raynaud’s Phenomenon
- Bacterial Angiomatosis
Neoplastic
- Squamous cell carcinoma
Classification of Pigmented Lesions
Blue lesions
- Mucocele
- Ranula
- Salivary duct cyst
- Submucosal hemorrhage
- Eruption cyst
- Blue nevus
Brown lesions
- Macules
- Cellular nevus
- Malignant melanoma
- Drug induced melanoma
- Café-au-lait spots
- Smoker’s melanosis
- Endocrine pigmentation
- Pigmented lichen planus
- HIV-oral melanosis
- Peutz-Jeghers syndrome
Yellow lesions
- Lipoma
- Fordyce’s granules
- Verruciform xanthoma
- Jaundice
- Superficial abscess
Grey-black lesions
- Amalgam tattoo
- Graphite tattoo
- Hairy tongue
- Heavy metal ingestion
- Racial pigmentation
- Slough of ANUG
Red lesions
- Reactive lesions:
- Pyogenic granuloma
- Peripheral giant cell granuloma
- Premalignant: malignant tumors
- Erythroplakia
- Hemangioma
- Kaposi’s sarcoma
- Lesions-associated with dermatologic conditions:
- Erythema migrans
- Systemic lupus erythematosus
- Erythema multiforme
- CREST syndrome
- Metabolic:
- Vitamin B complex
- Anemia
- Burning mouth syndrome
- Blood disorders:
- Hemophilia
- Thrombocytopenic purpura
- Leukemia
- Infectious conditions:
- Gingivitis
- Stomatitis
- Pharyngitis
- Scarlet fever
- Koplik spots
- Infectious mononucleosis
- Syphilis
- Candidiasis
- Median rhomboid glossitis
- Immunological abnormalities:
- Plasma cell gingivitis
- Drug reactions and contact allergies
- Wegener’s granulomatosis
- Others:
- Traumatic ulcer
- Petechiae
- Ecchymosis
- Radiation mucositis
- Thermal and chemical burns
Classification of Oral Manifestations of HIV/AIDS by EC-Clearinghouse
Group 1: Strongly associated with HIV infection
- Candidiasis: Erythematous, pseudomembranous, angular cheilitis
- Hairy leukoplakia
- Kaposi’s sarcoma
- Non-Hodgkin’s lymphoma
- Periodontal diseases: Linear gingival erythema, necrotizing gingivitis, necrotizing periodontitis
Group 2: Less commonly associated with HIV infection
- Bacterial infections: Mycobacterium avium-intracellulare, Mycobacterium tuberculosis
- Melanotic hyperpigmentation
- Necrotizing ulcerative stomatitis
- Salivary gland disease: Dry mouth, unilateral or bilateral
- swelling of major salivary glands
- Thrombocytopenic purpura
- Oral ulcerations NOS (not otherwise specified)
- Viral infections: Herpes simplex, human papilloma virus, varicella—zoster
Group 3: Seen in HIV infection
- Bacterial infections: Actinomyces israelii, Escherichia coli, Klebsiella pneumonia.
- Cat-scratch disease (Bartonella henselae).
- Epithelioid (bacillary) angiomatosis (Bartonella henselae)
- Drug reactions: Ulcerative, erythema multiforme, lichenoid, toxic epidermolysis.
- Fungal infections other than candidiasis: Cryptococcus neoformans, Geotrichum candidum, Histoplasma capsulatum, Mucoraceae (mucormycosis/zygomycosis), Aspergillus flavus.
- Neurologic disturbances: Facial palsy, trigeminal neuralgia
- Recurrent aphthous stomatitis.
- Viral infections: Cytomegalovirus, Molluscum contagiosum.
Classification of Candidiasis by Axell et al. 1997
Primary oral candidiasis:
- Acute form:
- Pseudomembranous candidiasis
- Erythematous candidiasis
- Chronic form:
- Hyperplastic candidiasis
- Erythematous candidiasis
- Pseudomembranous candidiasis
- Candida-associated lesion:
- Denture stomatitis
- Angular stomatitis
- Median rhomboid glossitis
- Keratinized primary lesion super-infected with Candida:
- Leukoplakia
- Lichen planus
- Lupus erythematosus
Secondary candidiasis:
- Candidal endocrinopathy syndrome.
Classification of Gingival Hyperplasia
On Basis of Etiological Factors and Pathologic Changes
Inflammatory enlargement
- Chronic
- Acute
Drug induced enlargement
Enlargement associated with systemic disease
- Conditional enlargement:
- Pregnancy
- Puberty
- Vitamin C deficiency
- Plasma cell gingivitis
- Non-specific conditioned enlargement (Pyogenic granuloma)
- Systemic diseases causing gingival enlargement
- Leukemia
- Granulomatous disease (e.g. Wegener’s granulomatosis, sarcoidosis)
Neoplastic enlargement
- Benign tumors
- Malignant tumors
False enlargement
Using the criteria of location and distribution gingival enlargement is designated as follows:
- Localized: Gingival enlargement limited to one or more teeth.
- Generalized: Involving the gingiva throughout the mouth.
- Marginal: Confined to marginal gingiva.
- Papillary: Confined to interdental papilla.
- Diffuse: Involving the marginal and attached papillae.
- Discrete: Isolated sessile or pedunculated tumor like enlargement.
On basis of degree of gingival enlargement
Grade 0: No sign of gingival enlargement.
Grade 1: Enlargement confirmed to interdental papilla
Grade 2: Enlargement involves papilla and marginal gingiva.
Grade 3: Enlargement covers three quarters or more of the crown.
Classification of Pulpal Diseases
Grossman’s Clinical Classification
Pulpitis (Inflammation)
- Reversible pulpitis
- Symptomatic (acute).
- Asymptomatic (chronic).
- Irreversible pulpitis
- Acute
- Abnormally responsive to cold.
- Abnormally responsive to heat.
- Chronic
- Asymptomatic with pulp response.
- Hyperplastic pulpitis.
- Internal resorption.
- Acute
Pulp Degeneration
- Calcific (Radiographic diagnosis)
- Others (Histopathologic diagnosis).
Pulp Necrosis.
Seltzer and Bender’s Classification
This classification is based on clinical tests and histological diagnosis.
Treatable without pulp extirpation and endodontic treatment
- Intact uninflamed pulp
- Transition stage
- Atrophic pulp
- Acute pulpitis
- Chronic partial pulpitis without necrosis.
Untreatable without pulp extirpation and endodontic treatment
- Chronic partial pulpitis with necrosis
- Chronic total pulpitis
- Total pulp necrosis.
Ingle’s Classification
Inflammatory changes:
- Hyper-reactive pulpalgia:
- Hypersensitivity
- Hyperemia
- Acute pulpalgia:
- Incipient
- Moderate
- Advanced
- Chronic pulpalgia:
- Hyperplastic pulpitis:
- Pulp necrosis
Retrogressive changes
- Atrophic papulosis
- Calcific papulosis.
Classification of Dental Caries
Based on location of the lesion
- Pit and fissure caries
- Occlusal
- Buccal or lingual pit
- Smooth surface caries
- Proximal
- Buccal or lingual surface
- Root caries
Based on tissue involved
- Enamel caries
- Dentinal caries
- Cementum caries
Based on virginity of the lesion
- Primary caries
- Secondary caries
Based on progression of lesion
- Progressive caries
- Rapidly progressive-like nursing caries and radiation caries
- Slowly progressing
- Arrested caries
Classification of Granulomatous Lesions or Diseases
Specific or Infective Type:
- Bacterial:
- Tuberculosis
- Leprosy
- Syphilis
- Granuloma Inguinale
- Brucellosis
- Cat scratch disease
- Tularemia
- Glanders
- Actinomycosis
- Fungal:
- Blastomycosis
- Cryptococcosis
- Coccidioidomycosis
- Histoplasmosis
- Parasitic: Schistosomiasis
Non-specific:
- Sarcoidosis
- Crohn’s disease
- Silicosis
- Berylliosis
- Foreign body granuloma
- Orofacial granulomatosis
Classification of Osteomyelitis
- Acute Osteomyelitis:
- Acute suppurative osteomyelitis
- Acute subperiosteal osteomyelitis
- Acute periostitis
- Chronic Osteomyelitis:
- Non- Specific Type
- Chronic intramedullary osteomyelitis
- Chronic focal sclerosing osteomyelitis
- Chronic diffuse sclerosing osteomyelitis
- Chronic osteomyelitis with proliferative periostitis
- Chronic subperiosteal osteomyelitis
- Chronic periostitis
- Specific Type
- Tuberculous osteomyelitis
- Syphilitic osteomyelitis
- Actinomycotic osteomyelitis
- Non- Specific Type
- Radiation-induced osteomyelitis
- Idiopathic osteomyelitis
Classification of Fibro-osseous Lesions
- Developmental:
- Solitary bone cyst
- Gigantiform Cementoma
- Cherubism
- Reactive/Reparative:
- Aneurysmal bone cyst
- Central giant cell granuloma
- Garre’s Osteomyelitis
- Osseous Dysplasia
- Florid Osseous Dysplasia
- Cemental osseous dysplasia
- Focal osseous dysplasia or sclerosing osteomyelitis
- Osseous Keloid
- Traumatic periostitis
- Neoplasms:
- Benign cementoblastoma
- Ossifying Fibroma
- Conventional
- Juvenile Trabecular
- Juvenile Psammomatoid
- Osteoma
- Osteoid Osteoma
- Osteoblastoma
- Endocrinal/Metabolic:
- Brown tumor of hyperparathyroidism
- Idiopathic:
- Fibrous dysplasia
- Paget’s disease
Classification of Bone Disorders of Face and Jaw
- Developmental defects of bone formation of face and jaw:
- Agnathia
- Micrognathia
- Macrognathia
- Facial hemiatrophy
- Facial hemihypertrophy
- Cleft palate.
- Benign and malignant lesions of bone:
- Osteoma
- Osteosarcoma
- Ewing’s sarcoma.
- Fibrosseous lesions
- Fibrous dysplasia of bone
- Ossifying fibroma
- Cementifying fibroma
- Paget’s disease of bone
- Cherubism
- Osteogenesis imperfecta
- Cleidocraniodysplasia
- Hurler’s syndrome
- Garre’s osteomyelitis
- Jaw lesions in hyperparathyroidism
- Aneurysmal bone cyst.
Classification of Anemia
Etiological Classification of Anemia (By Lea & Febiger 1981)
Loss of blood
- Acute posthemorrhagic anemia
- Chronic posthemorrhagic anemia
Excessive destruction of red blood corpuscles
- Extracorpuscular causes
- Antibodies
- Infections-like malaria
- Splenic sequestration and destruction
- Associated diseases like lymphomas
- Drugs, chemical and physical agents
- Trauma to RBC
- Intracorpuscular hemolytic diseases:
- Hereditary:
- Disorders of glycolysis
- Faulty synthesis or maintenance of reduced glutathione.
- Qualitative or quantitative abnormalities in the synthesis of globulin
- Abnormalities in RBC membrane
- Erythropoietic porphyria
- Hereditary:
- Acquired:
- Paroxysmal nocturnal hemoglobinuria
- Lead poisoning
Impaired blood production resulting from deficiency of substances essential for erythropoiesis
- Iron deficiency
- Deficiency of various B vitamins: Vitamin B12 and folic acid (pernicious anemia and megaloblastic anemia); pyridoxine responsive anemia
- Protein deficiency
- Possibly ascorbic acid deficiency
Inadequate production of mature erythrocytes
- Deficiency of erythroblast
- Atrophy of bone marrow: Aplastic anemia
- Chemical or physical agents
- Hereditary
- Idiopathic
- Isolated erythroblastopenia
- Thymoma
- Chemical agents
- Antibodies
- Atrophy of bone marrow: Aplastic anemia
- Infiltration of bone marrow:
- Leukemia, lymphomas
- Multiple myeloma
- Carcinoma, sarcoma
- Myelofibrosis
- Endocrine abnormalities:
- Myxedema
- Addison’s disease
- Pituitary insufficiency
- Sometimes hyperthyroidism
- Chronic renal failure:
- Chronic inflammatory disease:
- Infectious
- Non-infectious including granulomatous and collagen disease
Cirrhosis of liver
Morphological Classifaction of Anemia
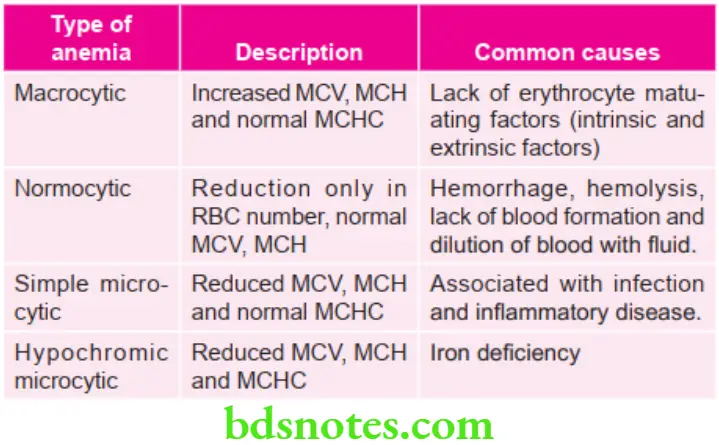
MCV = mean corpuscular valume; MCH = mean corpuscular hemoglobin;
MCHC = mean corpuscular hemoglobin concentration
Classification of Acute Leukemia (FAB Classification)
Acute Myeloblastic Leukemia
- Minimally differentiated: Myeloblasts lack definite cytologic and cytochemical features but have myeloid lineage antigens
- AML without maturation: Myeloblasts predominate with distant nucleoli, few granules or auer rods are present.
- AML with maturation: Myeloblasts wtih promyelocytes predominate and Auer rods may be present.
- Acute promyelocytic leukemia: Hypergranular promyelocytes often with multiple Auer rods are seen.
- Acute myelomonocytic leukemia: Mature cells of both myeloid and monocytic series in peripheral blood; myeloid cells resemble M2
- Acute monocytic leukemia: Promonocytes or undifferentiated blast.
- Acute erythroleukemia: Erythroblast predominate; myeloblasts and promyelocytes also increased
- Acute megakaryocytic leukemia: Pleomorphic undifferentiated blast cells predominate and react with anti-platelet antibodies.
Acute Lymphoblastic Leukemia
- Acute lymphoblastic (Seen in children): Homogeneous small lymphoblasts; scanty cytoplasm, regular round nuclei, inconspicuous nucleoli.
- Acute lymphoblastic (Seen in adults): Heterogeneous lymphoblasts; variable amount of cytoplasm, irregular or cleft nuclei, large nucleoli.
- Burkitt’s Type (Uncommon): Large homogenous lymphoblasts; Nuclei are round to oval, prominent nucleoli, cytoplasmic vacuolation.
Classification of Vesiculobullous Lesions
Vesiculo Bullous Lesions
Fitz Patrick Classification
- According to Anatomical Plane:
- Intraepidermal blister granular layer
- Pemphigus foliaceus
- Frictional blisters
- Staphylococcus scalded syndrome
- Spinous layer
- Eczematous dermatitis
- Secondary to heat and cold
- Herpes virus infection
- Familial Benign Pemphigus
- Suprabasal
- Pemphigus vulgaris
- Pemphigus vegetans
- Darier’s disease
- Basal layer
- Erythema multiforme
- Toxic epidermal necrolysis
- Lupus erythematosus
- Lichen planus
- Epidermolysis bullosa simplex
- Intraepidermal blister granular layer
- Dermal-Epidermal Junction Zone:
- Lamina lucida
- Bullous pemphigoid
- Cicatricial pemphigoid
- Epidermolysis bullosa junctional
- Below basal lamina
- Erythema multiforme
- Epidermolysis bullosa dystrophica
- Lamina lucida
Vesiculobullous Lesions
- Primary Blistering:
- Pemphigus
- Bullous pemphigoid
- Cicatrical pemphigoid
- Epidermolysis bullosa acquisita
- Secondary Blistering:
- Contact
- Erythema multiforme
- Toxic epidermal necrolysis
- Infection:
- Varicella Zoster
- Herpes Simplex
- Bullous Impetigo
- Systemic Disease:
- Infection-Cutaneous Emboli
- Metabolic
- Diabetic with Bullae
- Porphyria Cutanea tarda
Classification of Mucocutaneous Lesions of Oral Cavity
Genodermatosis:
- Darier’s Disease
- White sponge nevus
- Hereditary benign intraepithelial dyskeratosis
- Peutz-Jeghers syndrome
- Pachyonychia Congenita
- Dyskeratosis Congenita
- Pseudoxanthoma elasticum
Non-Infective Disease:
- Vesicular
- Bullous pemphigoid
- Benign mucous membrane pemphigoid
- Pemphigus
- Erythema multiforme
- Lichen planus
- Epidermolysis Bullosa
- Non-Vesicular
- Geographic tongue
- Lichen planus
- Collagen disorders:
- Wegener’s granulomatosis
- Midline lethal granuloma
- Polyarteritis nodosa
- Scleroderma
- Lupus erythematosus
- Vasculitis
- Degenerative disorders:
- OSMF
- Amyloidosis
- Solar elastosis
- Pigmentation:
- Anemia
- Albert syndrome
- Addison’s disease
- Racial pigmentation
- Endocrinopathy
Precancerous Lesions
- Leukoplakia
- Erythroplakia
- Palatal lesion associated with reverse smoking
- Verrucous hyperplasia
- Carcinoma in situ
Precancerous Condition
- Oral submucous fibrosis
- Sideropenic anemia
- Lichen planus (Erosive)
- Discoid lupus erythematosus
- Dyskeratosis congenita

Leave a Reply