Oral Cavity, Odontomes, Lip And Palate Oral Cancer
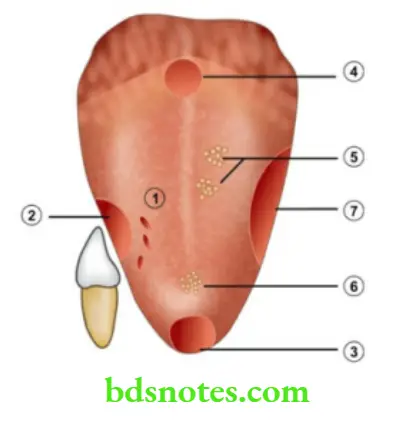
- The oral cavity is bounded by the lips anteriorly, cheek on both sides, tonsils posteriorly, above by the palate and below by the floor of the mouth. It is lined by squamous epithelium.
- The oral cavity suffers from various ulcers including malignancy because it is insulted by various agents such as alcohol, smoking, tobacco chewing, etc.
- Oral cancer is the most common malignant neoplasm in the head and neck. Hence, it is discussed first.
Read And Learn More: Clinical Medicine And Surgery Notes
Oral Cancer Definitions
- Hyperkeratosis refers to an increase in keratin layers. It occurs due to constant irritation. Once the cause is removed it is reversible. It is a microscopic diagnosis, e.g. smokers’ hyperkeratosis of the palate and lips. Once the aetiological agent is withdrawn, the lesion returns back to normal.
Incidence Of Oral Cancer
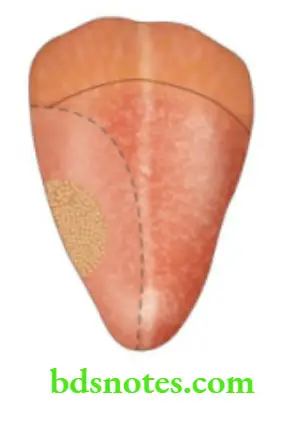
- Tounge: 50%
- Cheek: 20-50%
- Floor: 10-15%
- Gums: 10%
Leukoplakia appears clinically as a white patch in the mouth and cannot be scraped off. It is irreversible and not attributable to any known diseases. It is important to biopsy the leukoplakic portion to rule out malignancy.
Premalignant Conditions For Oral Cancer
1. Leukoplakia: The causes of leukoplakia are as follows:
- Smoking results in hyperkeratosis. Nicotine in the form of cigarettes chewed tobacco1, and powdered snuff produces premalignant changes in the oral cavity.
- Spices
- Spirits have synergistic action with smoking
- Sharp tooth, sepsis, poor oral hygiene
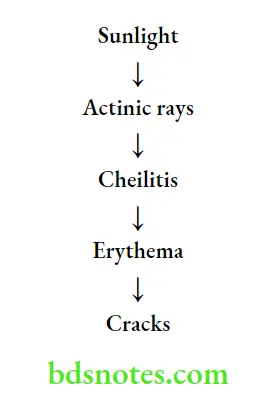
- Sunlight — actinic rays
- Syphilis causes endarteritis obliterans and results in chronic superficial glossitis of the tongue which is a precancerous condition (rare nowadays).
- Susceptibility²of a person
- Betel nut and slaked lime with betel leaf and tobacco (Pan) are eaten and usually kept inside the cheek for many hours. Over the years, it brings about chronic irritation of the mucosa of the cheek and causes leukoplakia. Tobacco contains multiple carcinogens including aromatic hydrocarbons.
Stages in the development of leukoplakia
- Keratosis appears as a milky blush on the surface.
- Acanthosis refers to the elongation of rete pegs. This appears as a smooth, white, dry patch.
- Dyskeratosis means the formation of keratin cell layers in the deeper aspect of the epidermis before they reach the surface.
- Speckled leukoplakia appears as multiple, small white patches.
- Carcinoma in situ

Treatment of leukoplakia
- About 10% of leukoplakia patients develop oral cancer. Hence, superficial excision of the lesion followed by skin grafting should be done. Even though leukoplakia is irreversible, Isoretinoin (13-cis-retinoic acid) can reverse some cases of leukoplakia and possibly reduce the development of squamous cell carcinoma.
- Erythroplakia is a red, velvety lesion with incidence of malignancy around 15% (more malignant than leukoplakia).
- Submucous fibrosis
- This is supposedly due to hypersensitivity reaction to chillies, camphor, tobacco or due to vitamin deficiencies.
- Initially, it produces ulceration of the mucosa of the cheek. These ulcers heal resulting in a dense submucous fibrosis, which appears clinically firm to hard. It can affect the tongue also.
- The chances of malignancy are around 10–15%
- It is treated by excision with reconstruction.
- Papilloma of the tongue or cheek
- Chronic hyperplastic candidiasis
- Syphilitic glossitis: Tertiary syphilis produces chronic superficial glossitis which can lead to carcinoma of the tongue. However, it is rare nowadays.
- Discoid lupus erythematosus.
- Dyskeratosis congenita.
American Joint Committee Staging System —TNM Staging
Primary Tumour (T)
- T0: No evidence of primary tumour
- Tis: Carcinoma in situ
Stage Grouping
- Stage 1: T1 N0, M0
- Stage 2: T2, N0, M0
- Stage 3: T3, N0, M0,T13, N0, M0
- Stage 4: T4, N0, M0 T1, N2-3, M0,T, N, M1
- T1: ≤ 2 cm
- T2: > 2 cm and ≤ 4 cm
- T3: > 4 cm
- T4: Any cancer invading adjacent structures such as cartilage, cortical bone, deep (extrinsic) muscles of the tongue, skin or soft tissue of the neck.
Cervical Lymph Nodes (N)
- Nx: Nodes cannot be assessed
- N0: No lymph node metastasis
- N1: Single positive ipsilateral node less than or equal to 3 cm in diameter
- N2A: Single positive ipsilateral node more than 3 cm but less than or equal to 6 cm.
- N2B: Multiple ipsilateral nodes, but all less than 6 cm.
- N2c: Bilateral or contralateral lymph nodes, but all less than 6 cm.
- N3: Lymph node more than 6 cm.
Distant Metastasis (M)
- M0: No distant metastasis
- M1: Distant metastasis present
General Principles In The Treatment Of Oral Cancer
Aim Of The Cancer Treatment
- Cure of the patient: Cure of the cancer if possible, with wide excision of the tumour which includes removal of the tumour with 2 cm of the surrounding normal tissues with or without bone.
- Palliation: If a cure is not possible, palliation should be attempted by surgery or radiotherapy.
- Preservation of function such as swallowing speech, vision, etc.
- Cosmetic function: Following wide excision reconstruction with myocutaneous/ osteomyocutaneous flap must be done to maintain cosmetic function.
- Lymph nodes are treated by radical neck dissection or curative radiotherapy (RT).
- To achieve minimal mortality and morbidity.
- Treatment of advanced tumours – T3 and T4 lesions:
- These are managed by a combination of surgery with postoperative RT. Surgery is the principal therapeutic modality of the treatment usually followed by postoperative radiotherapy.
- The treatment depends upon the general condition of the patient, risks of anaesthesia, adequate intensive care management, etc. Chemotherapy also has been tried before surgery or after surgery. However, the response rate is improved, but it has not affected the survival.
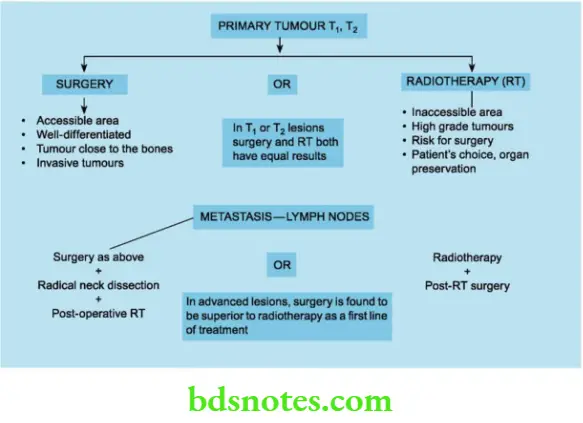
- The treatment of primary tumour and metastasis is given in
Role of chemotherapy in head and neck cancers
- The most benefit has been in the treatment of laryngeal and nasopharyngeal carcinomas.
- Cisplatin is clearly the most effective drug. Other drugs such as carboplatin, 5-fluorouracil (5-FU), bleomycin, gemcitabine etc. are also used.
- Induction chemotherapy: In advanced cases, chemotherapy is given before surgery or RT. In more than 80% of cases, tumour regression can occur.
- Concurrent chemoradiotherapy (CCRT): It improves both local and regional control, especially in those patients with high-risk cancers.
- Examples: Locally advanced cancers of the oral cavity, larynx, oropharynx, etc.
A drug used in CCRT can be high-dose cisplatin — 100 mg/m2 IV for 3 cycles every 21 days concomitantly with RT. (For another dosage, kindly refer oncology manual). Side effects include severe mucositis and xerostomia. A gastrostomy may be necessary.
Radiotherapy
- Irradiation of the oral cancers achieves a cure in about 80–90% of patients. It preserves the anatomical part and also preserves the function.
RT: Advantages
- Easy, safe with minimal mortality
- Preservation of an organ
- The function of the part is preserved
- The cure rate is around 80—90%
- First line in early cases
RT: Disadvantages
- Long stay in the hospital
- Tumour cure cannot be assessed by pathology
- Soft tissue fibrosis resulting in ankylostomia
- Adverse effects on the skin, loss of hair, mucositis of the oral cavity, xerostomia, etc.
The dose of RT: 6500–7500 cGy units is required to eradicate squamous cell carcinoma of the head and neck. It is usually given in the daily dose of 180–200 cGy units.
Radiotherapy is given in T1 and T2 lesions as the first line of treatment and postoperatively in T3 and T4 lesions after surgery.
Role Of Surgery
- Surgery is done in all stages of oral cancers. It may be in the form of wide excision or wide excision with removal of the bone (composite resection).
- In advanced stages, it may be a palliative surgery such as the excision of a fungating, ulcerating, or bleeding mass. Surgery is also done for the lymph nodes in the form of radical neck dissection (RND), or modified RND.
Oral Cancer Surgery Advantages
- It removes a fungating, ulcerating, bleeding lesion
- It relieves the pain
- The specimen is available for histopathological examination to assess cancer clearance
- 80–90% cure is possible
Oral Cancer Surgery Disadvantages
- Loss of an organ-total glossectomy
- Functional and cosmetic disability
- Significant morbidity
- Mortality—8–10%
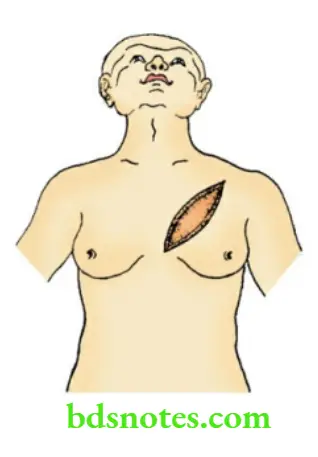
The pectoralis major myocutaneous flap (PMMC Flap): It is the most widely used flap for the reconstruction of oral cancers.
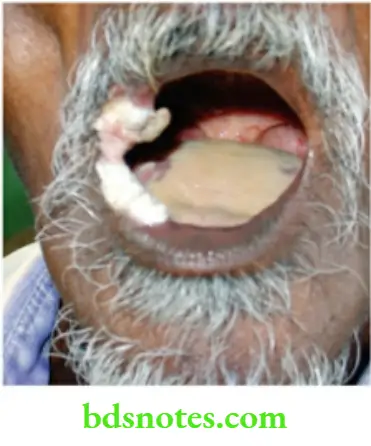
Carcinoma Of Buccal Muscles
Carcinoma of the cheek is very common in India due to the habit of keeping the tobacco quid in the cheek pouch.
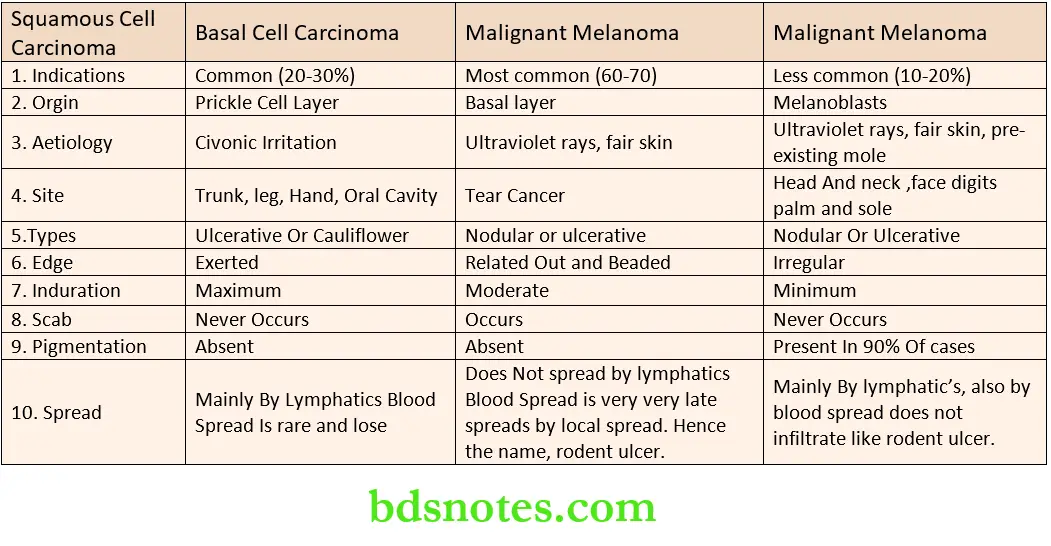
Pathological Types
- A non-healing ulcer, with a slough in the centre of the lesion
- An exophytic growth, or a proliferative growth — verrucous carcinoma
- An infiltrative lesion slowly involves the adjacent structures such as the tongue, mandible, floor of the mouth, skin, etc.
Carcinoma Clinical Features
- A non-healing ulcer or cauliflower-like growth. Verrucous carcinoma is an exophytic growth.
- Edges are everted with induration at the base as well as at the edge. Induration clinically presents as a hard feeling.
- Pathologically, it is due to fibrosis, caused by malignancy (carcinomatous fibrosis). It is a diagnostic feature of squamous cell carcinoma.
- Possibly, it is a host reaction indicating good immunity. Due to fibrosis, some lymphatics get obliterated. This delays the spread of the disease thereby improving the prognosis.
- Ulcer bleeds on touch. Due to secondary infection, most of the oral cancers are tender to touch.
- Fixity to the underlying structures such as the mandible may be present.
- The surrounding area may also show induration.
- Evidence of leukoplakia may be present in the oral cavity.
- Trismus is due to the involvement of pterygoid muscles and masseter. This occurs when the carcinoma cheek extends into the retromolar trigone. Trismus can also be due to soft tissue fibrosis caused by radiation.
- Halitosis is very characteristic.
- Assessment of fixity to the mandible: Severe pain over the jaw indicates periostitis.
- Bidigital palpation of the mandible: The index finger is inserted in the oral cavity in the gingivolabial sulcus nearer the 3rd molar tooth and slowly withdrawn towards the angle of the mouth.
- At the same time, the index finger of the other hand is inserted in the gingiobuccal sulcus and slowly withdrawn. Periosteal thickening is suggestive of the involvement of the mandible.

- Proliferative lesions are often verrucous carcinoma.
Peculiarities Of Verrucous Carcinoma
- Very slow growing
- Growth is exophytic (then infiltrative)
- Rarely spreads by lymphatics
- Well-differentiated carcinoma
- Surgery is the treatment of choice
Spread
- Local spread: Once it involves the entire thickness of the cheek it results in an orocutaneous fistula. Involvement of the mandible results in the sinus.
- Lymphatic spread: Submandibular nodes and upper deep cervical nodes get enlarged (Level I and II). In 50% of the cases, lymph node enlargement is due to infection and in the remaining 50% it is due to metastasis. Metastatic deposits are hard in consistency, indurated and with or without fixity.
- Blood spread is very rare and it occurs late.
Carcinoma cheek with oro cutaneous fistula Investigations


- Tumour cells are concentrated more in the growing edge.
- Comparison with the normal tissues is possible.
- The Centre has a slough.
The histopathological report is squamous cell carcinoma and in the majority of the cases, it is well differentiated.
- Wedge biopsy from the edge of the ulcer is taken because of the following reasons:
- Orthopantomography: X-ray of the mandible to rule out mandibular involvement
- Chest X-ray to detect inhalation pneumonia
- FNAC of the lymph node.
Treatment Of Carcinoma Cheek Early Disease
Surgery
- A small superficial ulcer (T1, T2) is treated by wide excision followed by split skin graft (SSG).
- A small infiltrative ulcer is treated by wide excision followed by a flap reconstruction. Following flaps can be used.
Both these flaps have been replaced by pectoralis major myocutaneous flap now (PMMC flap).
Early Carcinoma Cheek
- T1, T2 lesions—Surgery/RT
- T1, lesion and near commissure—RT
- T2 – Exophytic and superficial—RT
- T2 – Deep—Surgery is better
- Early disease—No nodes—Surgery is better – No other treatment is necessary.
- Early disease—Positive lymph nodes—Same modality to be used for primary and secondary.
Radiotherapy: As mentioned earlier, early lesions can be managed with radiotherapy.
Indications for radiotherapy
- The patient is not willing for surgery
- Patient not fit for surgery
- T1 and T2 lesions
- Lesion near the commissure.
Radiotherapy Types
- External radiotherapy large total dose of 6000–8000 cGy units are given; 200 cGy units/day.
- Interstitial radiotherapy is indicated in infiltrative small lesions. Caesium 137 or Iridium wires are placed within the tumour. The advantage of this method is minimal tissue reaction.
Advanced Carcinoma Cheek
Surgery: T3 and T4 lesions require surgery as the main modality of the treatment followed by postoperative radiotherapy.
Most of the lesions require full thickness resection leaving behind large defects. Such defects can be repaired by myocutaneous flap.
- PMMC flap: This is the most widely used flap now for head and neck reconstruction. The flap is raised along with muscle and an island of skin based on the pectoral branch of the thoracoacromial artery. It is tunnelled under the skin of the chest wall and neck and brought to the area of the defect. It has been described as a ‘workhorse’ for head and neck reconstruction.
Examples of various surgeries for advanced carcinoma cheek
- Carcinoma cheek fixed to the mandible: Wide excision of the growth along with segmental resection of the mandible or hemimandibulectomy is done depending upon the infiltration of the tumour. Very often the whole thickness of the cheek is lost which is reconstructed by using a PMMC flap.
- Orocutaneous fistula is treated by wide excision which refers to the removal of the entire thickness of the cheek along with the growth. Reconstruction is done by using a PMMC flap. Radiotherapy should not be given as it results in the persistence of fistula.
- Carcinoma of the cheek with lymph nodes: Along with the primary, submandibular nodes and upper deep cervical nodes (Level I, II, III) are removed, along with the submandibular salivary gland.
- This is called suprahyoid block dissection. If surgery has been used to treat the primary, the lymph nodes also should be treated by surgery in the form of neck dissection.
- Carcinoma of cheek with fixed lymph nodes: Both primary lesion and lymph nodes should be treated by radiotherapy and reassessment done after 3–4 weeks.
- If residual glands persist or if the glands become mobile, neck dissection can be done at a later date.
- Fixity to an internal jugular vein or sternocleidomastoid muscle is not a contraindication for radical block dissection.
- Those structures can be removed. However, when the lymph nodes are fixed to the carotid artery, radiotherapy is preferred
Prophylactic Neck Dissection
It is advocated in T3 and T4 lesions irrespective of lymph nodal status. This amounts to minimal suprahyoid neck dissection with the removal of Level 1, 2 and 3 lymph nodes. It has shown survival benefits.
Carcinoma Of Tongue
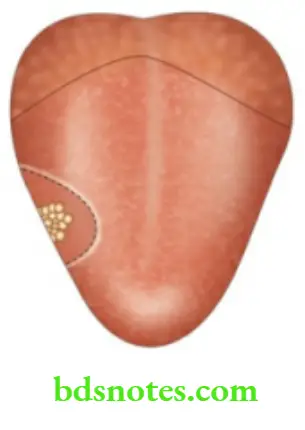
Carcinoma Of Tongue Pathological Types
- Non-healing ulcer, commonly on the lateral border of the tongue in 60% of cases, with slough
- A proliferative growth, with an everted edge.
- Frozen tongue or indurated variety.
- In this variety, there is maximum induration and sometimes it is more than the size of the tumour. The tongue is converted into a hard woody “mass”.
- Fissure variety: The tongue is indurated with deep fissure.
Carcinoma Of Tongue Clinical Presentation
- A bleeding ulcer
- Pain in the tongue is due to the involvement of the lingual nerve. In such cases, pain from the tongue can be referred to the ear and lower temporal region
- The auriculotemporal nerve and lingual nerve are posterior branches of the mandibular division of the trigeminal nerve.
- Ankyloglossia has restricted mobility of the tongue. It is due to infiltration of the floor of the mouth or mandible, or due to an advanced lesion.
- Dysarticulation—difficulty in talking is due to the inability of the tongue to move freely.
- Dysphagia is a common presentation from carcinoma of the posterior 1/3 (in 20% of cases). An elderly gentleman sitting in the outpatient department spitting blood-stained saliva is suggestive of carcinoma posterior 1/3 of the tongue.
- Foetor oris is due to infected necrotic growth.
- Bilateral massive enlargement of lower deep cervical nodes in an elderly patient is suggestive of carcinoma of posterior 1/3. The patient may not be aware of growth at all.


- Please note: Tongue cancers tend to be more rapid in their onset than other cancers in the oral cavity. Compared with other cancers within the oral cavity tongue cancers have greater potential for lymph node metastasis.
Carcinoma Of Tongue Clinical Examination
- Inspection and palpation of the growth or the ulcer should be described in the same manner as that of the carcinoma cheek. Typically, the ulcer bleeds in touch with the central slough.
- The edge, base and surrounding area are indurated. The carcinoma of the tongue and carcinoma of the penis are the two places in the body wherein induration can be much more extensive than the primary growth or an ulcer. In some cases, induration may be the only finding.
- Digital palpation of the posterior 1/3 of the tongue should be done with a glove.
- Test for mobility of the tongue.
- Forward protrusion-genioglossus. This is the muscle commonly involved.
- Backward movement-styloglossus
- Elevation-palatoglossus
- Depression-hyoglossus.
- All these muscles are supplied by the hypoglossal nerve except palatoglossus which is supplied by glossopharyngeal nerve.
- Bidigital palpation of the mandible should be done which may show thickening.
Lymphatic Spread
- Apical vessels drain the tip of the tongue into submental lymph nodes, bilaterally.
- Lateral vessels drain into submandibular lymph nodes, from here to the lower deep cervical lymph nodes, jugulo-omohyoid nodes – level 4.
- Central vessels drain into submandibular nodes.
- Basal vessels drain the posterior 1/3 of the tongue. There is a crisscrossing of the lymphatics on both sides.
- Hence, they drain into bilateral lower deep cervical lymph nodes. (Some lymphatics on their way to the nodes, pass through the mandible which explains the frequent involvement of the mandible in carcinoma tongue. This is a debatable issue now.)
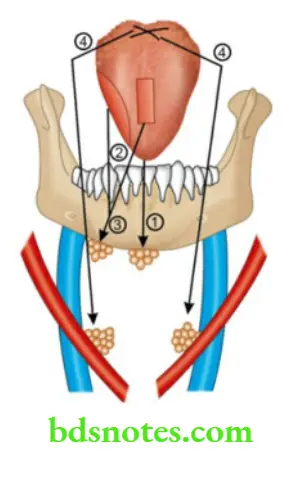

- In 50% of cases, the lymph node enlargement is due to secondary infection. Such nodes are tender and firm and respond to antibiotics. In the remaining cases, they are hard and fixed and hence, significant.
The posterior 1/3 tongue has very little cornification but has abundant lymphatics which explains the massive nodes.
Carcinoma Of Tongue Investigations
- Wedge biopsy from the edge of the ulcer can be taken under local anaesthesia. In cases of proliferative growth, punch biopsy is recommended. In cases of growth arising from the posterior 1/3 of the tongue, a biopsy can be taken under general anaesthesia. It also provides an opportunity to examine in detail the posterior spread of the disease into the tonsils, pharynx, etc.
- Orthopantomogram: X-ray of the mandible can demonstrate an irregular defect due to invasion, erosion or pathological fracture.
- Chest X-ray is taken to rule out aspiration or inhalation pneumonia.
- Routine investigations such as complete blood pictures, fasting and postprandial sugar estimation to rule out diabetes, and electrocardiography to assess cardiovascular function should be done.
Carcinoma Posterior 1/3 Of Tongue
- It presents as dysphagia or change of voice
- Easily missed in a clinical examination
- Palpation will give the diagnosis-Induration
- It is one of the occult primaries for lymph node secondaries in the neck.
- The crisscrossing of the lymphatics explains bilateral lymph nodes in the neck.
- Blood spread is more common.
- The prognosis is bad because well-differentiated carcinoma in this location is rare, and
- Lymphoepithelioma can occur.
- Transitional cell carcinoma (rare) with undifferentiated epithelial cells can also occur.
Carcinoma Posterior 1/3 Of Tongue Treatment
Carcinoma of the tongue is managed similarly to cancer in the oral cavity.
However, preserving the function of the tongue, widespread disease in the posterior one-third of tumours, and the general health of patients (elderly with bad bronchopneumonia) may decide the treatment in favour of radiotherapy. However, the results of surgery or radiotherapy for early carcinoma of the tongue are equivalent.
Various types of surgery
- Carcinoma in situ: This type is uncommon in our country. A wide excision with a 1 cm margin and a depth of 1 cm is sufficient. The reconstruction of the tongue is not necessary.
- Partial glossectomy is indicated when the lesion is less than 2 cm (T1) and confined to the lateral border of the tongue.
- About 1/3 of the anterior 2/3 of the tongue is removed. The wide excision should include at least 2 cm of tissue away from the palpable indurated edge of the tumour. Alternatively, radiotherapy can be given.
- Hemiglossectomy refers to the removal of around 50% of the tongue. This is indicated in a radio-residual tumour, radio-recurrent tumour or where radiotherapy facilities are not available. Reconstruction of the tongue can be done by using a PMMC flap.
- Total glossectomy: Indications are similar to those mentioned above. However, very extensive growths involving the entire tongue are given radiotherapy initially, to reduce the size of the tumour. Surgery can then be undertaken. Total glossectomy carries significant mortality and morbidity.
- Commando’s operation: This is indicated when carcinoma of the tongue is fixed to the mandible with infiltration of the floor of the mouth. Hemiglossectomy with hemimandibulectomy and removal of the floor of the mouth and radical neck dissection is described as Commando’s operation
- However, in a few selected cases, removal of the hemimandible is not necessary. Growths which are close to the margin of the mandible without infiltration (confirmed by X-ray) need to be treated by marginal excision.
- Carcinoma of the tongue with involvement of only a small portion of the mandible can be managed by segmental excision.
- The advantage of this method is that it is not only cosmetic but also preserves the function of the tongue by preserving genioglossus. Hence, the tongue may not fall backwards after surgery.
Structures Removed In Radical Block Dissection Of The Neck
- The fat, fascia, and lymphatics are from the midline to the anterior border of the trapezius, from the mandible to the clavicle below.
- The lymph nodes — submental, submandibular, upper and lower deep cervical nodes, posterior group of nodes (Level I – V).
- Submandibular salivary gland, sternomastoid
- Internal Jugular Vein (IJV)
- Spinal accessory nerve
Treatment of lymph nodes
Lymph node metastasis in the neck from squamous cell carcinoma can be managed both by surgery as well as radiotherapy. Radiotherapy can be given in all stages of secondaries in the neck. However, its main indication is a large primary tumour with neck nodes.
In such situations both the primary and secondary can be managed with radiotherapy alone which carries minimal morbidity and mortality.
- If the general condition of the patient is good and the lymph nodes are hard and mobile, hemiglossectomy with excision of the floor of the mouth with radical dissection of the neck is done (Commando’s operation).
- If radical neck dissection has to be done on both sides, the IJV should be preserved at least on one side to prevent cerebral oedema. In such cases, radiotherapy is a very good alternative.
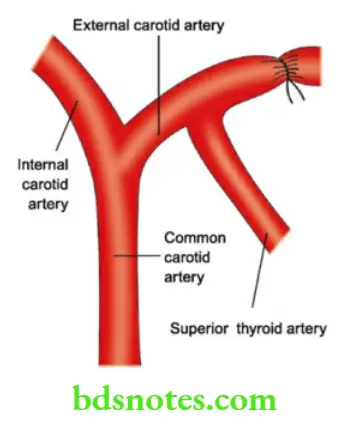
Causes of death in carcinoma tongue
- Recurrent aspirational pneumonia
- Gross local recurrence, fungation, ulceration, cachexia.
- Uncontrolled haemorrhage from growth: In such cases, ligation of the external carotid artery above the superior thyroid branch should be done. If the ligature is applied below the origin of the superior thyroid artery it results in eddying currents and thrombus at bifurcation of the common carotid artery.
Carcinoma Of The Lip
- The incidence of carcinoma of the lip is about 10 to 12%. It is common in the Western, elderly, white people, especially those exposed to sunlight. The actinic rays produce actinic cheilitis — inflammation of the lip, especially the lower lip, which over a period of years turns into malignancy.
- Since this is common in agriculturists, who are constantly exposed to sunlight, it is called a Countryman’s lip.
Countryman’s Lip
- Carcinoma lip includes growth arising from vermilion surfaces and mucosa.
- Leukoplakia is also responsible for squamous cell carcinoma. Smoking, spirits, and spices are the common precipitating factors.
- Genetic factors may also play a role. Blacks are less susceptible. On the other hand, an increased incidence of carcinoma lips has been found in Caucasians.
- Khaini chewers are more susceptible to carcinoma of the lip. (Khaini is a mixture of tobacco and lime.)
- It can also present as verrucous carcinoma of the lip.
Carcinoma Of The Lip Clinical features
- Elderly males are affected in 90% of cases.
- Nonhealing ulcers or growth is a common presentation.
- Edge is everted and indurated. Induration of the edge and the base is characteristic.
- The floor is covered with slough. Bleeding spots may be visible.
- Mobility: Ulcer or the growth moves with the lip, it is fixed to the subcutaneous structures of the lip.
- The entire upper lip, and lateral portions of the lower lip drain into upper deep cervical nodes. The central portion of the lower lip drains to submental nodes and submandibular nodes. Like elsewhere in the oral cavity, in 50% of the cases. nodes are enlarged due to secondary infections.

In the remaining 50% of the cases, they are enlarged due to metastasis. Such nodes are hard, with or without fixity. Blood spread is uncommon.
Carcinoma Of The Lip Differential Diagnosis
In a classical case of carcinoma of the lip with everted edges, with induration, there is no differential diagnosis. However, the following are the few conditions to be remembered.
1. Keratoacanthoma
It is a cutaneous tumour arising from hair follicles on the lips
Differential Diagnosis Of Carcinoma Lip
- Keratoacanthoma
- Ectopic salivary gland tumour
- Pyogenic granuloma
- Leukoplakia
- It is common in white, western, males between 50–70 years of age.
- Sunlight (actinic rays), chemical carcinogens, and viral factors may be responsible for this lesion.
- The central portion of the nodule may ulcerate. The lesion may progress for 6 weeks and may resolve spontaneously within 4–6 months.
2. Ectopic salivary gland tumour
- The lip is one of the common sites of malignant salivary gland tumours. This presents with submucous nodules which slowly grow and ulcerate and may mimic squamous cell carcinoma.
- They are also indurated lesions.
- However, the characteristic everted edge may not be seen.
- These are adenocarcinomas which are treated by surgery.
3. Pyogenic granuloma
- Recurrent infections or trauma produce a polypoidal mass with significant bleeding.

- It is rich in granulation tissue and resembles a polyp.
- It is devoid of epithelium
- Histologically, it is a capillary haemangioma
- Absence of induration gives the diagnosis.
4. Leukoplakia
- A slow-developing leukoplakia presents as a whitish nodule or an ulcer. However, a biopsy confirms the diagnosis.
Leukoplakia Treatment
Surgery and radiotherapy are the two modalities available for the treatment of carcinoma of the lip.
Leukoplakia Surgery
- T1 and T2 lesions can be excised followed by direct suturing without many functional problems. This is described as “V” excision which includes the removal of growth with a 1 cm healthy margin. Care should be taken to excise the full thickness of the lip.
- When removal of more than 1/3 of the lip is required flap reconstruction may be necessary. The primary goal in lip reconstruction surgery is oral competence.
Leukoplakia Examples:
- Abbe flap: Based on the upper labial artery – a pedicled flap is rotated down and sutured to the defect at the lower lip.
- Estlander’s flap: A wedge-shaped flap is used to reconstruct carcinoma of the lower lip when it involves the angle.
- Larger tumours: T3 and T4 lesions are irradiated first. If the tumour persists after radiotherapy, excision of the entire lip may be necessary followed by PMMC flap reconstruction.
- Significant lymph nodes can be removed along with the primary tumour — suprahyoid block dissection.
Radiotherapy
- It is indicated in all stages of carcinoma of the lip. Radiotherapy produces tumour necrosis resulting in a slow healing rate.
- Treatment lasts for several weeks and it delays the wound healing. Elderly patients who are not fit for surgery and carcinoma lips with fixed nodes are treated by irradiation.
- Commissure involvement is treated with RT rather than surgery.
- Dose: 4000–6000 centigram (cGy) units.
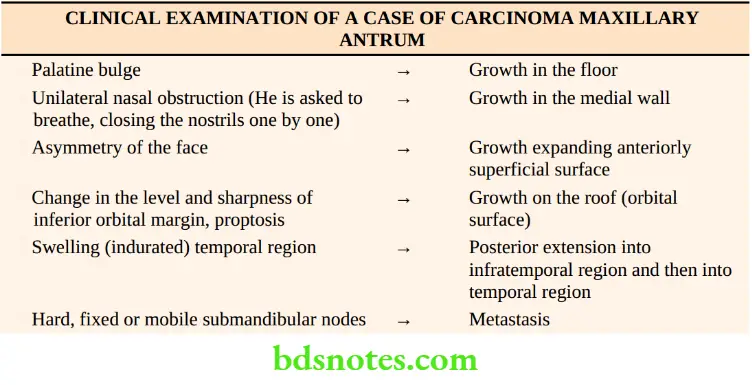
Carcinoma Maxillary Antrum
It is rare in Western countries but common in Asia. The workers in the furniture industries, chromic and nickel industries are more prone to the development of carcinoma maxillary antrum.
Carcinoma Maxillary Antrum Clinical Presentation
- Growth originating on the floor of the antrum may result in the bulge of the hard palate. This results in pain in the teeth and they may become loose.
- When the medial wall is involved, nasal obstruction and epiphora occur due to obstruction of the lacrimal duct. Bleeding from the nose can also occur if there is ulceration.
- If the anterolateral wall is involved, asymmetry of the face results in pain in the cheek.
- Anaesthesia over the skin of the cheek including the upper lip results due to the involvement of the infraorbital nerve, a branch of the maxillary division of the trigeminal nerve.
- If the roof is invaded proptosis and diplopia occur.
- Posterior extension of the growth is difficult to assess clinically. When it involves the pterygoid muscles, it results in trismus.
- Paraesthesia over the cheek, gums, lower lip, and postnasal discharge are the other features of these tumours. They carry poor prognosis because of late presentation.
Lymphatic Spread
About 50% of the tumours present with enlargement of submandibular lymph nodes and upper deep cervical lymph nodes — jugulodigastric nodes.
Lymphatic Spread Investigations
- Computed tomography (CT scan) can define a lesion, its extent, bony destruction, posterior extension, etc.— hence it is the first investigation of choice.
- Sinoscopy: Fenestration will provide tissue for biopsy followed by curettage to reduce the tumour bulk and to drain necrotic contents outside.
Lymphatic Spread Treatment
- Radiotherapy is the main modality of treatment in carcinoma maxillary antrum.
- The curative rate is around 70% in early cases. In advanced cases, radiotherapy is given first. This reduces the tumour bulk so that an unresectable lesion becomes resectable and maxillectomy can be done.
- Surgery can be done in the form of total maxillectomy when the growth involves the entire maxilla or it is of high grade followed by postoperative radiotherapy.
- Tumours of the lower half of the antrum are treated by partial maxillectomy.
- It includes the removal of the entire hard palate, the alveolus and the medial wall of the antrum up to and including the middle turbinate.
- Indications and contraindications for surgery and radiotherapy are on similar lines.
Benign Lesions In The Oral Cavity
Differential diagnosis of ulcer in the tongue
1. Aphthous ulcer
- Small, multiple, very painful ulcers can occur at any age group, more common in females at the time of menstruation. These are called as minor aphthous ulcers
- When they are larger, deeper, and painful, they are called major aphthous ulcers.
- They are due to viral infection. These ulcers are superficial ulcers with erythematous margins.
- They subside within a few days. Temporary relief can be obtained by applying salicylate gel.
- Vitamin B complex is usually given for the satisfaction of the patients.
Painful Ulcers In The Tongue
- Aphthous ulcers
- Dental ulcers
- Tubercular ulcers
Painless Ulcers In The Tongue
- Carcinomatous ulcers
- Gummatous ulcers
- Systemic diseases
2. Dental ulcer
- These ulcers occur due to broken teeth, sharp teeth, ill-fitting dentures, prostheses, etc. They are very painful ulcers.
- Such ulcers are common on the lateral margin and they heal when the tooth is removed. This is an example of a traumatic ulcer. It should not be confused with carcinomatous ulcer which commonly occurs on the lateral margin.
3. Tubercular ulcer of the tongue
- Tuberculosis affects the tip of the tongue. These ulcers are very painful with enlargement of regional nodes.
- It occurs in patients with fulminating pulmonary tuberculosis.
- Ulcers have undermined edges. These ulcers are sometimes multiple with serous
discharge.
4. Gummatous ulcer
- Gumma is a complication of tertiary syphilis resulting in a firm swelling in the midline in the anterior 2/3 of the tongue. Induration is absent.
- An ulcer is non-tender. Severe endarteritis obliterans results in the necrosis of gumma giving rise to gummatous ulcer. It has punched-out edges and washes leather slough on the floor. Other sites of gumma include testis, palate, clavicle and liver. These ulcers are rare nowadays.
5. Systemic diseases
- Pemphigus
- Systemic lupus erythematosus (SLE)
- Lichen planus
6. Post-pertussis ulcer
- It occurs in children due to repeated coughing. The typical location of the ulcer on the undersurface of the tongue and on the frenulum clinches the diagnosis
7. Carcinomatous ulcer
- Lateral margin
- Non-healing ulcer
- Everted edge
- Edge and base are indurated
- Bleeds on touch
- Fixity
- Significant lymph nodes in the neck.
Macroglossia
Diffuse painless enlargement of the tongue is described as macroglossia. It is a rare condition and can occur due to various causes.
1. Lymphangioma: In this condition, the tongue diffusely enlarges. Sometimes, it is a localised swelling. It may be associated with lymphangiomas elsewhere in the body like cheek mucosa, lips, etc.
The tongue becomes larger and indurated and gives rise to severe discomfort to the patients. Due to repeated trauma, the surface becomes ulcerated. It is treated by injecting sclerosants like ethanolamine oleate, hypertonic saline, etc. Partial excision may be necessary in cases of large lymphangioma.
Causes Of Macroglossia
- Haemangioma
- Lymphangioma
- Cretinism—Muscular macroglossia
- Neurofibroma
2. Haemangioma: Cavernous haemangiomas occur in the tongue, lips, etc. It is present since birth but manifests during childhood. It presents with soft, cystic, fluctuant swelling, at times pulsatile.
Trauma due to teeth or food results in bleeding. Haemangioma of the tongue is treated on the same lines as lymphangioma. It is much more difficult to excise it, especially a large haemangioma. Preoperative angiography and ligation of the lingual artery on both sides may be necessary.
Neurofibroma: It may be associated with Von Recklinghausen’s disease. It is treated by hemiglossectomy.
Muscular macroglossia: This condition, though rare, is seen in cretins. The tongue is thickened and cannot be held in place. Hence, it protrudes outside. It is treated by partial excision.
Syphilitic Lesions of the Tongue
The tongue is involved in all stages of syphilis.
1. Primary syphilis: Primary chancre that occurs in the tongue is highly contagious. It affects the tip of the tongue. It produces a painful ulcer with a large significant enlargement of regional lymph nodes.
2. Secondary syphilis: It produces a white patch on the tongue, lips and anterior pillars of fauces. In the tongue, these are multiple which coalesce to form snail track ulcers. The ulcers heal with fine tissue paper scar. In some cases, syphilitic organisms produce a flat, hypertrophied epithelium which is described as condyloma. This is called Hutchinson’s wart.
3. Tertiary syphilis: It produces gumma. Syphilis also produces chronic superficial glossitis, which is characterised by a bald tongue with loss of papilla and a fissured tongue, it is a precancerous condition.
Please Note: Dental students are commonly asked theory questions related to the head and neck. Head and neck clinical cases are the exam cases for you also. So I have given a possible list of cases and clinical methods or clinical examination here.
The Possible List Of Common Cases In The Oral Cavity Include
- Carcinoma: Cheek, alveolus, tongue, lip, etc.
- Benign lesions in the tongue: Ulcers, haemangioma, lingual thyroid
- Benign lesions in the cheek: Leucoplakia
- The floor of the mouth: Ranula, dermoid cyst and enlarged submandibular salivary gland
- Palate: Mixed tumour from ectopic salivary gland, gumma (rare nowadays)
- Gums and teeth: Epulis, carcinoma.
Clinical Examination Of The Oral Cavity
Oral Cavity Introduction: Malignancies of the oral cavity are the common short or long cases in the university examination.
They include carcinoma buccal mucosa, carcinoma alveolus, carcinoma floor of the mouth, carcinoma lip and carcinoma tongue.
All these lesions start as ulcers or growth. Any lesion which begins as a swelling in the oral cavity and later ulcerates, but having features of malignancy is most likely a malignant ectopic salivary gland tumour.
Other lesions such as epulis, mucous cysts, submucous fibrosis leukoplakia are also included under short cases. A few specific tongue lesions which manifest as swellings have been also included.
Patient Data
Age: Carcinoma buccal mucosa or tongue occur in the middle age group or elderly patients.
Mucus cysts are the retention cysts that occur in young patients.
Sex: Oral cancers are more common in men
Occupation: Carcinoma lip is more common in patients with outdoor occupations such as agriculturists. The lower lip is more commonly affected than the upper lip. Hence, it is called a countryman’s lip.
History Of Oral Cavity
1. Ulcer: The first complaint is usually a painless ulcer. When did you notice the ulcer? To start with any pain? How is it progressing? are the usual questions. It is painless to start with but secondary infection is very common in the oral cavity and results in pain later. A rapidly growing ulcer is most likely a malignant ulcer. Generally patient says it has been there for 2– 3 months and it is spreading and not healing. If the ulcer shows evidence of healing or becoming small, it means it is not a malignant ulcer. For example, the Patient had an ulcer on the lateral border of the tongue. It started becoming less once the sharp tooth was removed.
2. Pain: It is due to a secondary infection. Referred pain is due to the involvement of the nerve. Often carcinoma tongue patients complain of pain in the ear and temporal region which is the distribution of the auriculotemporal nerve. This is because the lingual nerve and auriculo-temporal nerve are the branches of the mandibular nerve. Severe pain over the jaw indicates periostitis.
3. Bleeding: Did you notice any bleeding? Malignant ulcers bleeds on touch. Minor trauma from the teeth or due to the food bolus drops of blood may be seen during mastication or chewing.
4. Any drooling of saliva: This should be enquired when you suspect malignancy of the posterior one-third tongue where in patient is not able to swallow (dysphagia). You may see a patient sitting with a sputum cup with or towel with him and frequently spitting there. It suggests carcinoma posterior one-third tongue.
5. Can you open the mouth? The inability to open the mouth is called a trismus. Trismus in oral cancers is due to the involvement of pterygoid muscles and masseter.
This occurs when carcinoma buccal mucosa extends into the retromolar trigone. Trismus can also be due to soft tissue fibrosis caused by radiation.
Once perineural lymphatics are involved, spread can occur in the infratemporal fossa resulting in trismus.
Please remember other important causes of trismus are tetanus, temporomandibular joint disorders and severe inflammatory painful conditions of the oral cavity such as acute tonsillitis, peritonsillar abscess, etc.
6. Any of your teeth have become loose Gingival cancers present as the loosening of a tooth.
7. Do you have difficulty swallowing It is a feature of carcinoma posterior one-third of the tongue.
8. Do you have difficulty in speech (disarticulation) Disarticulation is a feature of carcinoma tongue wherein effective tongue movements cannot take place.
9. Do you eat pan? Do you smoke, what are your food habits? – Betel nut and slaked lime with betel leaf and tobacco (Pan) is eaten and usually kept inside the cheek (Quid) for many hours.
Over the years, it brings about chronic irritation of the mucosa of the cheek and causes leukoplakia.
Tobacco contains multiple carcinogens including aromatic hydrocarbons. Among all the risk factors for oral cancer, tobacco consumption and the quid is the most important cause. Causes of leukoplakia can be remembered as 8 causes.
The causes of leukoplakia are as follows:
- Smoking results in hyperkeratosis. Nicotine in the form of cigarettes chewed tobacco, and powdered snuff produces premalignant changes in the oral cavity. In fact, smoking is one of the important factors responsible for malignancy of the upper aerodigestive tract.
- Spices
- Spirits have synergistic action with smoking
- Sharp teeth may cause chronic and constant irritation, (for carcinoma tongue)
- Sepsis, poor oral hygiene
- Sunlight—actinic rays: This is especially for carcinoma lip
- Syphilis causes endarteritis obliterans and results in chronic superficial glossitis of the tongue which is a precancerous condition (rare these days–only for academic interest).
- Susceptibility of a person
- Halitosis is very characteristic. The most common location for mouth-related halitosis is the tongue. No wonder halitosis is common in carcinoma tongue. Tongue bacteria produce malodorous compounds and fatty acids, and account for 80 to 90 per cent of all cases of mouth-related bad breath. Large quantities of naturally occurring bacteria are often found on the posterior dorsum of the tongue, where they are relatively undisturbed by normal activity
Patient Data Clinical Examination
Patient Data Inspection
1. Appearance, Attitude: Is the patient looking sick? Does he have a nasogastric tube in place? (because of dysphagia or he may be receiving radiation or he may not be able to swallow).
Has he received radiation? (radiation skin changes will be seen). Are there any lesions on the outer aspect of the cheek? – percutaneous fistulas or oedema of the cheek. Is there any drooling of saliva? (due to dysphagia).
2. Tongue: Ask the patient to open the mouth and note any trismus (inability to open the mouth). Note down the following points.
- Ulcer: Note down the location, size and shape, extension, edge, floor, and surrounding area.
- Carcinomatous lesions are described as an ulcer or ulcerative growth or ulceroproliferative growth. (Do not describe them as swelling).
- Surface: Is it normal with papilla or bald due to loss of papilla which reflects anaemia? The red tongue can be due to glossitis, white patch in the tongue can be due to leucoplakia. Black colour can be due to malignant melanoma of the tongue.
- Also, look at the posterior third more carefully for any growth or ulcer. Foramen caecum is the site of lingual thyroid, and gumma (rare nowadays).
- Swelling: Grossly swollen tongue can be due to haemangioma. The surface will have a blue colour.
- Movements: Restricted movements or inability to protrude the tongue is called ankyloglossia. This is one of the important features of malignancy of the tongue.
- It is due to carcinomatous infiltration of the floor of the mouth. If the tongue is deviated to one side, it could be due to paralysis of the tongue musculature.
- This can happen due to hypoglossal nerve paralysis. Forward movement, backward movement, elevation depression and rotating movements have to be checked.
3. Cheek: Examine the cheek with normal light or with a torch for any ulcers, white patches or swellings—describe them.
4. Palate
- Cleft: Mention if there is a congenital cleft. If present, describe the extent – has it involved the soft or the hard palate?
- Swelling: If swelling is present describe the swelling. Swelling in the palate can be due to an ectopic salivary gland tumour or due to carcinoma maxillary antrum which pushes the upper jaw.
- Perforation: Nowadays, it is not due to syphilis. The hole may persist after surgery of the cleft palate due to the breakdown of the suture line.
5. Floor: Ask the patient to touch the palate with the tongue
- Ulcer or growth: Is it from carcinoma tongue? or has it started there? Describe the growth or ulcer. Typically carcinoma will have an everted edge.
- Swelling: The most common swelling in the floor of the mouth is Ranula which will have a typical blue colour and is lateral to the midline. Another swelling is a sublingual dermoid cyst which is in the midline, opaque with no transillumination.
- Wharton’s duct opening: Mention the opening of the submandibular duct on the side of the frenulum. Is it inflamed or is there any discharge of pus or stone that may be visible?
- Frenulum: It may be short — cause of slurred speech in children. Rarely ulcers in the frenulum of the tongue can be due to whooping cough.
6. Gums And Teeth
- The normal colour of the gums is pink. In Vincent’s angina, it is altered — more red and edematous.
- Blue black line in the free margin of the gums can be due to chronic lead poisoning as seen in painters and it is also seen in bismuth treatment given for leishmaniasis.




- Red pedunculated mass is usually an epulis.
- Tenderness over the teeth with an apical abscess can be the cause of the median mental sinus.
- Recent history of loosening of the tooth can be due to carcinoma alveolus or due to dental cyst.
Palpation
Wash your hands, wear a glove and tell the patient what you are doing.
1. Tongue
- If you have found a lesion such as an ulcer or swelling, mention tenderness first. Carcinoma tongue or cheek can be very tender contradictory to the traditional teaching of “carcinoma is painless”. The lesion tends to be irregularly ovoid with a long axis parallel to the midline of the tongue. It has indistinct edges. Sometimes, the lesion can be papuliferous or warty which is pale when compared to the rest of the tongue. The base of Such lesion is broad with induration.
- Sometimes you may see a fissure. It is a nodule to start with which invades the tongue so fast that it appears as a fissure with gross induration.
- If there is a swelling — a local rise of temperature can be mentioned, e.g. haemangioma can have increased temperature.
- Induration: However, the most important clinical finding of carcinoma tongue is induration which means hardness.
- This should be tested with the tongue relaxed (kept within the oral cavity). If you examine the tongue when it is protruding outside, the contracted muscles of the tongue may give a firm feeling and students can get confused.
- In fact, carcinomatous lesions posterior third can present without ulcer but with gross induration.
- Bleeding on touch: It is a feature of friable lesions, typically of carcinoma oral cavity. Students should palpate very gently. For the sake of demonstration, no forceful attempt should be made to prove the bleeding from the ulcer. Because it results in too much pain and discomfort to the patient.
- Mobility: Feel the base of the ulcer and try moving it is fixed to the tongue musculature.
- Please palpate the posterior one-third. If you find any ulcer or growth describe them.
- Often you will feel only induration. If so, describe how much induration is present and how much it is extending.
2. Cheek: On palpation give the details about the growth or ulcer. However, the most important physical findings to be tested here are induration and mobility of the lesion – the carcinomatous lesion is indurated, it will have restricted mobility, and it bleeds on touch.
3. Palate
- If there is swelling examine it in the usual format of swelling like size, shape, surface, and borders. The most important findings here are the consistency, e.g. if it is hard it can be a tumour. If it is firm think of some benign lesion. If it is soft it may be a vascular lesion.
- Check for signs of emptying. If it is present it is haemangioma. Tender swelling on the side of the palate can be due to alveolar abscess.
- If there is an ulcer, examine it as mentioned above.
4. The floor of the mouth
- Find out the extension of the growth or ulcer from the tongue — mention any induration.
- Find out whether it has involved the inner aspect of the jaw.
- Soft fluctuant swellings have to be tested for transillumination. If it is positive, it is runula.
- A sublingual dermoid cyst is not transilluminated because it contains sebaceous material.
- As you feel the floor, complete a digital examination of the mandible to rule.
The involvement of the mandible is as follows:
- Is there thickening?
- Is there tenderness?
- Is there a pathological fracture?
5. The outer aspect of the mouth
- If any obvious ulcers or skin changes are present, describe them.
- If any fistula induration or oedema is present, describe it.
6. Bidigital palpation of mandible.
7. Examination of the cervical lymph nodes
- Submental
- Submandibular
- Upper deep cervical — jugulodigastric
- Lower deep cervical





Jaw Tumour- Odontomes
Odontomes Definition
Odontomes are cysts, and malformations arising from epithelial or mesothelial elements of a tooth resulting in swelling of the jaw. As a developmental anomaly, few epithelial cells proliferate, persisting as epithelial debris of mallasuez.
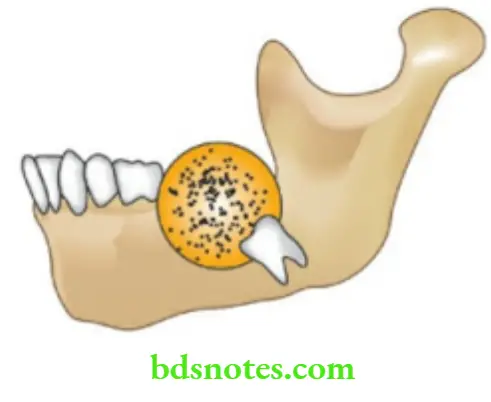
Dental Cyst Radicular Cyst/ Periapical Cyst Pathogenesis
This arises from a normally erupted, chronically infected, pulpless caries tooth. The caries tooth produces a low-grade, chronic inflammation which stimulates epithelial debris to proliferate. Later this brings about degeneration of epithelial and mesothelial cells resulting in a cyst within the maxilla.
Dental Cyst Clinical features
- Common in women around 3rd–4th decade
- Commonly affects the upper jaw (maxilla)
- It presents as a slow-growing swelling in the maxillary region resulting in deformity of the face.
Dental Cyst Diagnosis
- Presence of caries tooth with the expansion of the maxilla
- X-ray—large, unilocular cyst in maxilla or orthopantomogram showing cyst in the mandible
- Aspiration of the cyst demonstrates cholesterol crystals.
Dental Cyst Treatment
Excision of cyst with its epithelial lining through the intra-oral approach. After excision of the epithelium, the cyst wall should be corrected, followed by soft tissue ‘push-in’ to obliterate dead space.
Dentigerous Cyst—Follicular Odontome
- Common in lower jaw (mandible) in women 30–40 years.
- It occurs in relation to unerupted, permanent, molar tooth, most commonly an upper or lower third molar tooth.
- This unerupted tooth constantly irritates the cells, producing degeneration of the cells resulting in a dentigerous cyst.
- The cyst is lined by squamous epithelium surrounded by connective tissue. Within the cyst, the tooth lies obliquely or sometimes is embedded in the wall of the cyst.
- As it grows further, the cyst displaces the tooth to which it is attached. Thus, the tooth is displaced deeper and deeper and prevented from eruption.
Follicular Odontome Clinical features
- Absence of molar tooth
- Expansion of the mandible—Since the inner table of the mandible is strong, the expansion mainly occurs in the outer aspect of the mandible. The bone gets thinned out resulting in egg-shell crackling.
Follicular Odontome Diagnosis
X-ray mandible
- Tooth in the cyst
- Soap-bubble appearance due to multiple trabeculations of the bone
- Radiolucent well-defined swelling.
Follicular Odontome Treatment
- Small cyst—excision of the cyst by intraoral approach.
- Large cysts—managed by marsupialisation.
Adamantinoma
- It is also called multilocular cystic disease, ameloblastoma, or Eve’s disease.
- This tumour arises from ameloblasts (Enamel forming cells).
- It is a benign tumour, very slow growing, and behaves like a basal cell carcinoma. Inadequate treatment results in local recurrence and later metastasis. Hence, even though the tumour is benign, it has to be treated like a malignant tumour.

Adamantinoma Sites
- Mandible is the most common site
- Tibia-2nd common site. It can be explained by the inclusion of abnormal embryonic epithelium.
- The pituitary is another common site where adamantinoma can occur. Both pituitary stalk and enamel arise from oral epithelium.
Adamantinoma Clinical features
- Patients in the 4th or 5th decades are commonly affected.
- This is a slow-growing jaw tumour in the region of the angle of the mandible and horizontal ramus of the mandible.
- As the tumour grows, it undergoes cystic degeneration resulting in multiple cystic spaces. Hence, it is called multilocular cystic disease.
- As it grows it causes expansion of the outer table of the mandible and causes fracture mandible.
- The patient may present with complaints of falling teeth.
Adamantinoma Diagnosis
X-ray: A large cyst and small multiple cysts due to the trabeculations called honeycomb appearance.
Surgical treatment of adamantinoma
Even though it is benign, simple curettage or enucleation may result in recurrence and chances of recurrent adamantinoma turning into malignancy are high.
Hence, a wide excision with 1 cm of healthy normal tissue should be removed. It may amount to segmental excision of the mandible or hemimandibulectomy.
Differential diagnosis
1. Giant-celled reparative granuloma (Jaffe tumour)
- It is a benign tumour which occurs due to haemorrhage within the bone marrow.
Pathology
- It affects the antral part of the maxilla or mandible causing enlargement of the jaw.
- Stroma is vascular consisting of thin-walled blood vessels, scanty collagen, and connective tissue cells.
- Microscopic features mimic giant cell epulis or brown tumours of hyperparathyroidism.
Jaffe tumour Clinical features
- Unlike an adamantinoma, this tumour affects females in the age group of 10–25 years.
- Painless enlargement of the jaw is the presenting feature. X-ray demonstrates radiolucent artery.
Adamantinoma
- Locally invasive solid tumour
- Spreads within the medullary bone
- Invades soft tissues
- Should not fragment the tumour cells
- Subperiosteal excision should not be done as it may result in recurrence
Incomplete excision results in recurrence and metastasis to the lung - Hence, even though it is a benign tumour it is treated by wide excision or hemimandibulectomy
Jaffe tumour Treatment
- Calcitonin 0.5 mg (100 units) daily subcutaneous injection over a period of one year has been recommended as a first line of treatment. It has shown the resolution of the tumour.
- Curettage is the surgical line of treatment.
2. Osteoclastoma
- This is a rare tumour seen in the lower jaw.
- Males between the age of 25–40 years are commonly affected Unlike adamantinoma, it is a rapidly growing tumour.
- As the tumour enlarges, both tables of the lower jaw are thinned out.
- An X-ray may show a large, radiolucent cyst with pseudo trabeculation. Even though benign, it is radiosensitive.
- However, recurrence can occur and can turn into malignancy like that of adamantinoma.
Epulis Means “Upon The Gum.” It Refers To Solid Swelling Situated On The Gum
- Soft epulis – Granulomatous
- Firm epulis – Fibrous
- Giant cell
- Hard epulis – Carcinomatous
- Malignant epulis – Carcinomatous
- Dangerous epulis – Fibrosarcomatous
- It arises from the alveolar margin of the jaw.
- Very often patients present with swelling on the gum which is painless.


Granulomatous Epulis
- Precipitating factors are — caries teeth, dentures, and poor oral hygiene.
- It manifests as a mass of granulation tissue around the teeth on the gums. It is a soft to firm fleshy mass and bleeds on the touch.
- Pregnancy epulis refers to this variety (gingivitis gravidarum).
Fibrous Epulis
It is the most common form of simple fibroma arising from the periodontal membrane, present on the gum. It may undergo sarcomatous change. It is a firm polypoidal mass, slowly growing and nontender.
Giant Cell Epulis
- It is also called myeloid epulis.
- It is an osteoclastoma arising in the jaw. It presents as hyperaemic vascular, oedematous, soft to firm gums with indurated underlying mass due to expansion of the bone.
- It may ulcerate and result in haemorrhage. X-ray shows bone destruction with ridging of walls (pseudo-trabeculation).
- Small tumours are treated by curettage
- Large tumours are treated by radical excision.
Carcinomatous Epulis
- This is an epithelioma arising from the mucous membrane of the alveolar margin.
- Typically, it presents as a nonhealing, painless ulcer. It slowly infiltrates the bone.
- Hard regional lymph nodes are due to metastasis.
- Treated by wide excision which includes the removal of a segment of the bone.
Median Mental Sinus
This is a sinus in the midline just beneath the mentum.
Aetiopathogenesis
It is produced by an apical abscess of lower incisors which penetrate the buccal cortical plate below the origin of the mentalis muscle.
This muscle takes origin from the labial surface of the alveolar process ust above the labial sulcus. Hence, pus discharges through a sinus in the centre of the chin.
Aetiopathogenesis Clinical Presentation
- Patients present with recurrent swelling in the submental region which bursts open spontaneously discharging at times mucus and sero-purulent fluid.
- Repeated history of swelling, discharge and healing are common presentations.
- Diagnosis is established by examination of the oral cavity which reveals evidence of caries tooth.
Aetiopathogenesis Treatment
- Once the caries tooth is extracted, the sinus will heal spontaneously.
Aetiopathogenesis Clinical Notes
We had a patient with a discharging sinus in the mental region for 1½ years who had seen many practitioners including a surgeon who curetted the lesion twice. However, the lesion reappeared soon. This case is a classical example of what the mind does not know, eyes cannot see.

Vincent’s Angina
It is an acute ulceromembranous stomatitis or acute ulcerative gingivitis and stomatitis. The disease is caused by Vincent’s organisms – Borrelia vincenti, an anaerobic spirochaete and fusiformis. These are gram-negative rods which are the normal pathogens of the oral cavity.
Precipitating Factors
- Malnutrition, diabetes mellitus, caries tooth, war seasons, winter, etc.
- The disease starts in the intergingival defects as a deep penetrating ulcer which results in a spontaneous gingival haemorrhage. There is a thick membrane covering the ulcer.
- Once the infection spreads to the tonsillar region, it is called Vincent’s angina – a very severe painful condition.
Precipitating Factors Clinical features
- Common in children and young adults between 20–40 years of age.
- It presents with very painful gums with fever, malaise and toxaemia.
- Gums are swollen, red, and inflamed with or without slough.
- Difficulty in swallowing, painful swallowing (odynophagia), foetor oris, features of toxaemia and high-grade fever are characteristic of this condition.
Precipitating Factors Treatment
- Improve nutrition; mouthwashes with hydrogen peroxide help in washing away the membrane.
- Injection penicillin — 10 lakh units, IM 6th hourly for 6–7 days
- Since they are anaerobic organisms, metronidazole 400 mg thrice/day for 7–10 days, should be given.
Cleft Lip And Cleft Palate
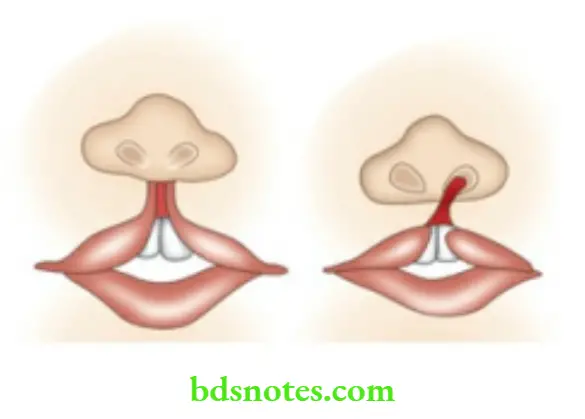
- Cleft lip results from abnormal development of the median nasal and maxillary process.
- Cleft palate results from a failure of fusion of the two palatine processes.
Types of Cleft Lip
- Central: It is very rare and occurs due to the failure of the fusion of two median nasal processes.
- Lateral: It is the commonest variety wherein there is a cleft between the frenulum and the lateral part of the upper lip.
- This is due to the imperfect fusion of the maxillary process with the median nasal process. Lateral variety can be unilateral or bilateral.
- Complete or incomplete: In cases of complete variety, cleft lip extends to the floor of the nose. In cases of incomplete variety, the cleft does not extend upto the nostril.
- Simple or compound: Compound refers to a cleft lip associated with a cleft in the alveolus.
Types of Cleft Lip Clinical Features
- In 80% of the cases, cleft lip is unilateral and in about 60% of the cases, it is associated with cleft palate.
- In many cases, the nostril is widened.
- Maldevelopment or malalignment of the teeth in relation to the cleft is common.
Functional effect
- The presence of cleft lip does not interfere much with sucking. However, there may be some difficulty in bottle feeding.
- Some degree of difficulty in speech (disarticulation) is present.
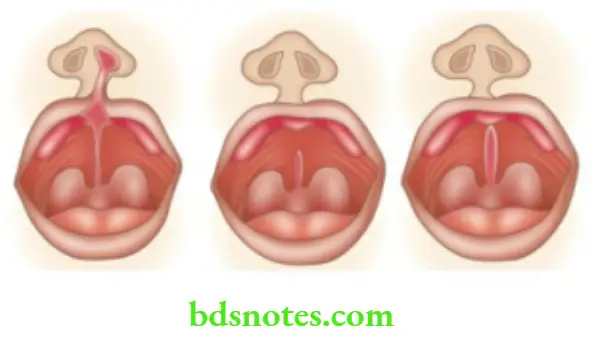
Cleft Palate
Development of palate
The palate is developed around 6–8 weeks of life from 3 components.
- The premaxilla is developed from the median nasal process.
- and 3. Maxillary process which contributes one palatine process on each side. The line of fusion of these processes is in the form of a letter Y.
- Imperfect fusion or developmental anomalies result in cleft palate.
Cleft Palate Types
- Complete: Failure of fusion of palatine processes and premaxilla results in complete cleft palate. In such situations, the nasal cavity and mouth are interconnected.
- When the premaxilla is not fused with both palatine processes, it hangs down from the septum of the nose. Thus, a complete cleft can be of two types as shown below in the diagram.
- Incomplete: When the fusion of three components of the palate takes place, it starts from the uvula and then backwards. Thus, various types of incomplete fusion results.
- Bifid uvula.
- The whole length of the soft palate is bifid.
- The whole length of the soft palate and the posterior part of the hard palate are involved. On the other hand, the anterior part of the palate is normally developed. In about 25% of cases, cleft palate alone and in 50% of cases, both cleft palate and cleft lip are encountered.
Effects of Cleft Palate
- The presence of cleft palate interferes with swallowing to some extent
- They are unable to make the consonant sounds like B, D, K, P, T.
- Teeth: Upper lateral incisors may be small or even absent. The maxilla tends to be smaller. Teeth are crowded.
- Nose: Oral organisms contaminate the upper respiratory mucous membrane through the cleft palate.
- Hearing: Even with repair, acute and chronic otitis media and hearing problems can occur.
Management of cleft lip and palate
- A multidisciplinary approach involving plastic surgery, orthodontics, speech pathology, ENT department, prosthodontics and paediatrics department is needed to rehabilitate the cleft cases. This approach to the problem results in aesthetically acceptable end results without many functional deficiencies.
- Feeding advice: Cleft palate babies are unable to suck mothers’ milk because intraoral negative pressure cannot be created due to communication between oral and nasal cavities. Thus, expressed mother milk is given by spoon with the head end of the baby elevated by 45 degrees. Swallowed air during feeding is released frequently by burping.
Cleft Lip Repair
Timing: The majority of surgeons follow “RULE OF 10” as a guide for timing of lip and anterior palate repair. At the time of repair, haemoglobin should be more than 10 gm%, age approximately 10 weeks, weight more than 10 lbs (4.54 kg) and total leukocyte count less than 10,000 cells/cumm (i.e. no infection).
Types of Cleft Lip Repair
- For unilateral cleft lip repair most commonly used methods are the Millard rotation advancement flap and the Tennison — Randall triangular flap method.
- Bilateral cleft lip can be repaired in a single stage or in two stages at the interval of 3–6 months. For two-stage repair, any one of the methods described for unilateral cleft lip can be used. For bilateral repair in one stage, the Veau 3 method is simple and gives satisfactory results. Other single methods which give good results are Millard’s single-stage procedure and black procedure.
Rule Of 10
- Hb > 10 gm %
- Age approx: 10 weeks
- Weight > 10 lbs
- TC < 10,000 cells/mm
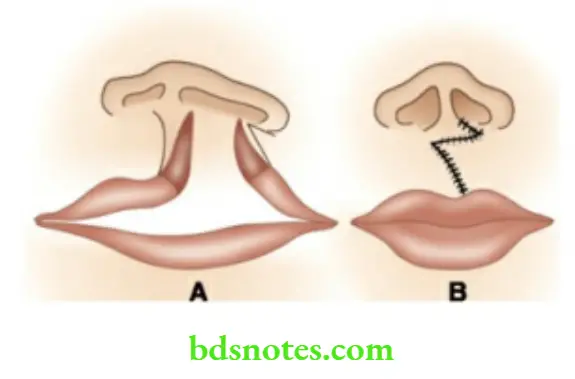
Basic Steps of Lip Repair
- Markings are made according to the method selected (e.g. Millard’s repair – Fig. 18.35A; Tennison Randall repair
- Adrenaline-saline solution 1: 2,00,000 is injected into the lip and labial sulcus for haemostasis.
- The full thickness of the lip is incised along the marking.
- Lip repair is done in 3 layers — mucosa, muscle and skin. For better aesthetic results, Cupid’s bow should become horizontal, white line continuity should be repaired and there should be no vermilion notching.
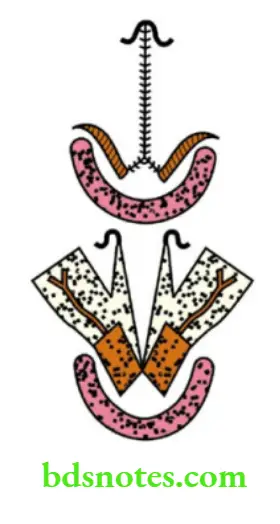
Cleft Palate Repair
Cleft Palate Timing: Early repair results in retarded maxillary growth due to surgical trauma to the growth centre and periosteum.
Delay in repair results in speech defect. The best-balanced result is achieved by repairing between one and a half years.
Cleft Palate Types
- Palate repair: Palate is repaired by palatal shelves. Mucoperiosteal flaps raised from various methods are available for palate repair.
- The most commonly used method is V-Y, pushback palatoplasty.
Steps of ‘V-Y’ Pushback Palatoplasty
- The palate is infiltrated with 1:2 lakhs adrenaline saline solution.
- Two mucoperiosteal flaps are elevated, one from either side of palatal shelves. Then, nasal layers are mobilised.
- The palate is closed in 3 layers-nasal layers, the muscle layer, and the oral layer.
- In V-Y push-back palatoplasty, palatal lengthening is achieved by V-Y plasty.
- The hook of the hamulus can be fractured to relieve tension on the suture line by relaxing the tensor palate muscle.

Leave a Reply