Oral Cavity, Lip, And Palate
Question.1. Write note on leukoplakia.
Or
Write briefly leukoplakia.
Or
Answer briefly on leukoplakia.
Or
Write in brief about leukoplakia.
Answer. Leukoplakia is defined as a white patch or plaque that cannot be characterized clinically or pathologically as any other disease and is not associated with any physical or chemical causative agent except use of tobacco.
First International Conference on Oral Leukoplakia Malmo, Sweden (1984) or modified WHO definition (1984).
Leukoplakia Etiology
1. Tobacco: Tobacco is widely used in two forms
- Smokeless tobacco: Chewable tobacco and snuff When tobacco is chewed, various chemical constituents leach out such as nitrosonornicotine, nicotine, pyridine and N picoline.
Alkaline ph: 8.2–9.3 acts as local irritants and leads to alterations of mucosa. - Smoked tobacco: Cigar, cigarette, beedi and pipe.
Smoking tobacco is harmful as this smoke contains polycyclic hydrocarbons, beta naphthylamine,nitrosoamines, carbon monoxide, nicotine, all of which acts as source of irritation.
Heat also plays a major role.
Heat induces alterations in tissues increasing reddening and stippling of mucosal surface.
Read And Learn More: General Surgery Question And Answers
2. Alcohol: Whether the use of alcohol itself is an independent etiological factor in the development of leukoplakia is still questionable.
Its effect, at best may be synergistic to other well-known etiological factors (physical irritants).
Alcohol leads to irritation and burning sensation of oral mucosa.
Alcohol facilitates entry of carcinogen in exposed cells of oral mucosa and alters the oral epithelium as well as its metabolism.
3. Chronic irritation: Continuous trauma or local irritation in the oral cavity leads to leukoplakia. Irritation or trauma can be caused by malocclusion, ill-fitting dentures, sharp tooth or broken tooth, hot spicy food and root piece.
4. Candida albicans: As a possible etiological factor in leukoplakia and its possible role in malignant transformation is still unclear.
About 10% of oral leukoplakias satisfy the clinical and histological criteria for chronic hyperplastic candidiasis.
5. Viruses: The possible contributory role of viral agents such as human papillomavirus 16 and 18 in the pathogenesis of oral leukoplakia particularly with regard to exophytic verrucous leukoplakia.
6. Vitamin deficiency: Serum levels of vitamin A, B12, C, beta-carotene and folic acid were significantly decreased in patients with oral leukoplakia than compared to normal patients.
7. Genetic factor: Relatively little is known yet with regard to possible genetic factors in the development of leukoplakia.
Leukoplakia Clinical Features
- Usually, the lesion occurs in 4th, 5th, 6th and 7th decades of life.
- Buccal mucosa and commissural areas are most frequent affcted sites followed by alveolar ridge, tongue, lip, hard and soft palate, etc.
- Oral leukoplakia often present solitary or multiple white patches.
- The size of lesion may vary from small well localized patch measuring few millimeters in diameter.
- The surface of lesion may be smooth or fiely wrinkled or even rough on palpation and lesion cannot be removed by scrapping.
- The lesion is whitish or grayish or in some cases, it is brownish yellow in color due to heavy use of tobacco.
- Inmostofthe cases, these lesionare asymptomatic, however in some cases, they may cause pain, feeling of thickness and burning sensation, etc.
Leukoplakia Differential Diagnosis
- Lichen planus: Shows Wickham’s straie
- Syphilis: Split papule or condyloma latum is seen
- Leukoedema: Shows faint milky appearance with folded and wrinkled pattrn. Most commonly seen on buccal mucosa.
Leukoplakia Treatment
Removal of etiological factors may lead to the reversal or elimination of disease.
Leukoplakia Conservative treatment
- Vitamin therapy is given to patient. Vitamin A should be given to apply topically.
- Along with vitaminA, vitamin E should be given this leads to inhibit metabolic degeneration.
- Nystatin therapy is given to eliminate candidal infection.
- Vitamin B complex can be given as supplemental therapy.
Leukoplakia Surgical treatment
Leukoplakia Conventional Surgery
- Incision is made around the lesion including the safe margins.
- Incision is deep and wide.
- Affected area is undermined and is dissected from underlying tissue.
- Sliding mucosal flp should be prepared for covering the wound.
- Fine iris scissors and skin hook is used for decreasing trauma.
- Extensive undermining of mucosal flp should be carried out so that when flp is advanced into its position, amount of tension will be minimum.
- As mobilization of mucosal flap is completed, it is advanced and free edges are approximated by multiple interrupted silk sutures.
Leukoplakia Fulguration
It is a technique in which there is destruction of tissues by high voltage electric current and the action is controlled by movable electrode.
This is done by electrocautery and electrosurgery.
Leukoplakia Laser
Laser peel: It is used to remove the lesion which involves relatively large surface area.
Leukoplakia Procedure
- Beam of laser is highly defocussed and should be kept at distant from the tissue.
- Initially, not any effct is seen on the tissue plane.
- Beam of laser should be gradually brought closer in focus,but remains in defocussed mode until tissue have white appearance and it begins to blister.
- Blistering usually occur at the basement membrane.
- The technique is extended over the rest of the lesion to be peeled.
- White area is then grafted with tissue forcep or hemostat.
Question.2. Describe clinical feature and treatment of submucous firosis.
Answer. OSMF is defined as “An insidious chronic disease affcting any part of oral cavity and sometime pharynx.
Although occasionally preceded by and/or associated with vesicle formation, it is always associated with juxta-epithelial inflammatory reaction followed by firoelastic changes in lamina propria, with epithelial atrophy leading to stiffess of oral mucosa and causing trismus and inability to eat.” —Pindborg (1966)
Submucous fibrosis Clinical Features
- It occurs during 20 to 40 years of age.
- Most commonly involved sites are buccal mucosa,retromolar area, uvula, soft palate, palatal fauces, tongue,lips, pharynx and esophagus.
- Onset of disease is insidious or develop over the period of 2 to 4 years.
- Initially the patient complains of burning sensation in the mouth, particularly during taking hot and spicy foods.
- It is often accompanied or followed by the formation of multiple vesicles over the palate or ulcers or inflammatory reactions in other parts of oral mucosa.
- There can be either excessive salivation or deceased salivation (xerostomia) along with recurrent stomatitis.
- Patients also develop a defective gustatory sensation.
- In the initial phases of the disease, palpation of the mucosa elicits a “wet-leathery” feeling.
- Petechial spots may also be seen in the early stages of the disease over the mucosal surfaces of tongue, lips and cheek, etc.
- Oral mucous membrane is very painful upon palpation at this stage.
- One of the most important characteristic features of oral submucous firosis is the gradual stiffning of the oral mucosa with progressive reduction in the mouth opening.
- Stiffness of the oral mucosa and the subsequent trismus develops gradually within a few years after the development of the initial symptoms.
- In the advanced stage of OSF, the oral mucosa losses its resiliency to a great extent and it becomes blanched and stiff Severe trismus develops at this stage.
- Because of stiffess of the lips and the tongue patients are unable to blow whistles or even blow out a candle.
- Oral mucosa is symmetrically affcted on both sides of the mouth and it shows extreme pallor.
- Oral submucous firosis often causes a blanched opaque (white marble-like) appearance of the mucosa, on which,there may be occasional presence of leukoplakic or erythroplakic patches.
- Palpation of the mucosa often reveals many vertical white firous bands on the inner aspect of the cheek.
- Patients of OSMF often develops diffilty in deglutition,referred pain in the ear or deafness and nasal intonation of voice.
- Depapillation of the tongue with recurrent or sometimes persistent glossitis occurs. Later on the tongue becomes stif and shows restricted movements.
- Uvula become ’ bud—like” or hockey stick shaped or become shrunken.
Submucous fibrosis Treatment
Submucous fibrosis Supportive treatment
- Diet rich with the vitamins along with iron preparation should be given to the patient.
- IM injection of Iodine B complex is given to the patient.
- During early phase low doses are given and later on high doses are effctive.
- Local injection of hydrocortisone in the lesional area is of value.
- Intralesional injection of hyaluronidase can be given.
- Systemically 100 mg/day of hydrocortisone is effctive in reducing the burning sensation.
- 2 mL injection of placentrex intralesional is effctive.
- Lycopene as an antioxidant should be given to the patient.
- Vitamin E along with hyalurodinase and dexamethasone is effctive.
- Intralesional injection of interferon-gamma helps in increment in mouth opening.
Submucous fibrosis Surgical treatment
Conventional Surgery:
- Tongue mucosa as a graft: The fibrous bands are excisioned and tongue mucosa as a flp is used.
- Implantation of fresh human placenta can be done following the surgical excision of firous bands.
- Fibrotic bands are excisioned and nasolabial flp is taken for reconstruction.
- Bilateral palatal flp is taken for generally covering of exposed area.
Submucous fibrosis Laser:
- Patient should be incorporated with general anesthesia. CO 2 LASER incise the buccal mucosa and vaporizes mucosal connective tissue.
Cryosurgery: It helps in providing the relief from the local lesions.
Question.3. Describe about etiology, clinical features and treatment of epulis.
Answer. Epulis means upon gum.
It refers to solid swelling situated on the gum.
Localized enlargement of gingiva is mainly known asepulis.
It arises from alveolar margin of jaw.
Epulis can originate from the bone, periosteum or the mucous membrane.
Types Of Epulis
Granulomatous epulis/Pyogenic Granuloma
- It is also called false epulis or pyogenic epulis.
- Precipitating factors are: Carious tooth, dentures, poor oral hygiene.
Epulis Clinical features
- The important point is that it does not contain pus while its name is pyogenic epulis.
- Pregnancy epulis refer to this variety.
- It is a mass of granulation tissue around the carious tooth on the gum.
- It is a soft to fim flshy mass and bleed on touch.
Epulis Treatment
- Extraction of associated carious tooth.
- Removal of local irritation as ill-fitng denture.
- Excision of granulation tissue.
- Pregnancy epulis regress spontaneously after delivery.
Epulis Fibrous epulis
It is the most common type of epulis.
Epulis Clinical Features
- Arises from periosteum at the neck of teeth.
- It is localized inflmmatory hyperplasia of gum.
- It occurs in response to local irritation.
- It is composed of firous tissue and blood vessels.
- It is a fim polypoidal mass, slowly growingand non-tender.
Epulis Treatment
Excision of growth and removal of local irritants.
Giant Cell epulis/Myeloid epulis
Giant Cell epulis Clinical Features
- It is less common, purple and pedunculated tumor.
- It is an “osteoclastoma” arising in the jaw.
- It present as hyperemic vascular edematous, soft to fim gums with indurated underlying mass due to expansion of the bone.
- It may ulcerate and result in hemorrhage.
- Multinucleated giant cells are found in histology.
- It is more rapidly growing tumor than any other epulis.
Giant Cell epulis Treatment
- Small tumors are treated by curettge.
- Large tumors are treated by radical excision.
Carcinomatous epulis
Carcinomatous Clinical Features
- This is an “epithelioma” arising from mucous membrane of alveolar margin.
- It presents as a non-healing, painless ulcer.
- It slowly infitrates the bone.
- Hard regional lymph nodes are due to metastasis.
Carcinomatous Treatment
Treated by wide excision, which include removal of segment of the bone.
Congenital epulis
- This is a benign condition seen in a newborn arising from the gum pads.
- This is the variant of granular cell myeloblastoma originating from the gums.
- This is common in girls and more common in upper jaw mainly in canine or premolar area.
- Congetinal epulis is a well localized swelling from the gum which bleeds on touch.
- Excision of congenital epulis should be done.
Myelomatous epulis
- This occurs mainly in leukemic patients.
- Treatment of leukemia resolves this condition.
Giant Cell epulis
This is the osteoclastoma causing ulceration and hemorrhage of gingiva.
Fibrosarcomatous epulis
It is the firosarcoma arising from the firous tissue of gums.
Carcinomatous epulis
Squamous cell carcinoma of alveolus and gingiva, present localized, hard, indurated, swelling with ulceration.
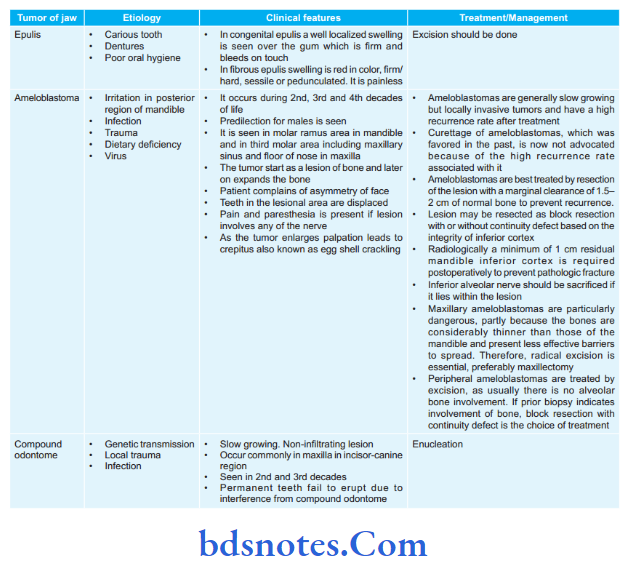
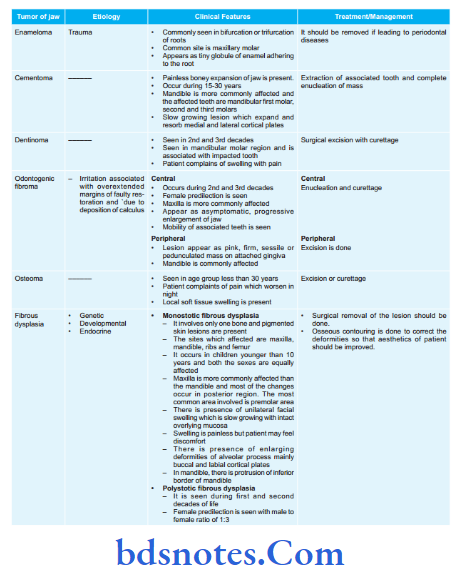
Question.4. Classify tumors of jaw. How will you treat a case of epulis?
Answer.
Classification of Tumors of Jaw
Swelling arising from the gums (Epulis)
- Congenital epulis
- Fibrous epulis
- Pregnancy epulis
- Giant cell epulis
- Myelomatous epulis
- Sarcomatous epulis
- Carcinomatous epulis
Swelling arising from the dental epithelium (Odontomes):
- Ameloblastoma
- Compound odontome
- Enameloma
- Cementoma
- Dentinoma
- Odontogenic firoma and myxoma
- Radicular odontome
- Composite odontome
Cysts arising in relation to dental epithelium:
- Dental cyst
- Dentigerous cyst
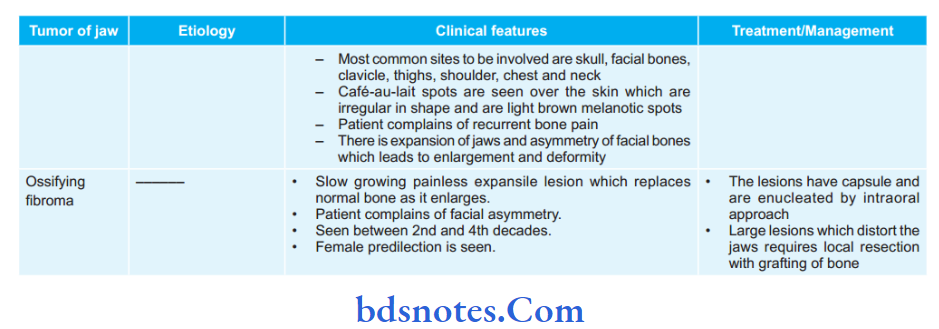
Swelling arising from the mandible or maxilla:
- Osteoma and osteoblastoma
- Torus palatinus and mandibularis
- Fibrous dysplasia
- Osteoclastoma
- Osteosarcoma
- Secondaries
- Giant cell reparative granuloma
Surface tumors:
Tumors from the surface which extend into the jaw.
- Ossifying firoma
- Osteofirosis of maxilla
- Ivory osteoma of jaw
- Leontiasis ossea (diffse osteitis)
- Carcinoma extending into the jaw
Question.5. Write in short adamantinoma.
Or
Write short answer on adamantinoma.
Answer. In 1885, Malassez coined the term adamantinoma. In 1934, Churchill replaced the term adamantinoma with ameloblastoma.
Ameloblastoma is defied as “usually unicentric, nonfunctional, intermittnt growth, anatomically benign and clinically persistent”— By Robinson
Ameloblastoma Pathogenesis
Ameloblastoma originates from:
- Epithelial rest of Malassez.
- Epithelium of odontogenic cysts
- Disturbances in developing enamel organ
- Basal cells of surface epithelium
- Heterotrophic epithelium.
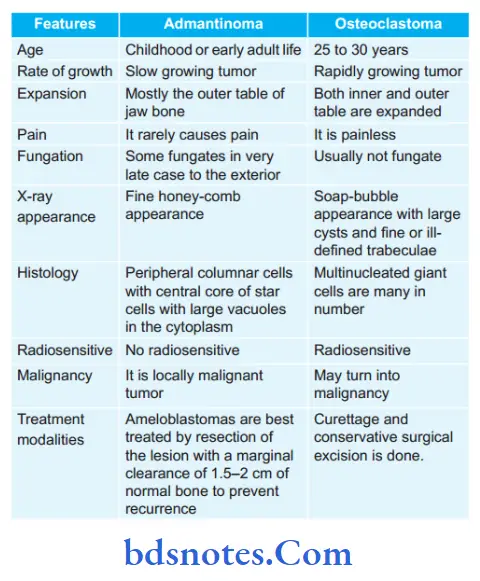
Ameloblastoma Clinical Features
- It occurs during 2nd, 3rd and 4th decades of life.
- Predilection for males is seen.
- Itis seeninmolar ramus area inmandible and inthird molar area including maxillary sinus and flor of nose in maxilla.
- Tumor start as a lesion of bone and later on expands the bone.
- Patient complains of asymmetry of face.
- Teeth in the lesional area are displaced.
- Pain and paresthesia is present if lesion involves any of the nerve.
- As the tumor enlarges palpation leads to crepitus also known as egg shell crackling.
Ameloblastoma Investigations
- Clinically: Presence of swelling in posterior mandible with expansion as well as egg shell crackling.
- Radiographically: Honey comb or soap bubble appearance in posterior region of mandible. Labial and lingual plate expansion is also seen.
- Biopsy: Biopsy of the lesion is needed for the confimation of diagnosis so that histological type of ameloblastoma is diagnosed.
Ameloblastoma Treatment
- Ameloblastomas are generally slow growing but locally invasive tumors and have a high recurrence rate after treatment.
- Curettage of ameloblastomas, which was favored in the past, is now not advocated because of the high recurrence rate associated with it.
- Ameloblastomas are best treated by resection of the lesion with a marginal clearance of 1.5–2 cm of normal bone to prevent recurrence.
- The lesion may be resected as block resection with or without continuity defect based on the integrity of inferior cortex.
- Radiologically a minimum of 1 cm residual mandible inferior cortex is required postoperatively to prevent pathologic fracture.
- Inferior alveolar nerve should be sacrified if it lies within the lesion.
- Maxillary ameloblastomas are particularly dangerous, partly because the bones are considerably thinner than those of the mandible and present less effctive barriers to spread.
Therefore, radical excision is essential, preferably maxillectomy. - Peripheral ameloblastomas are treated by excision, as usually there is no alveolar bone involvement.
If prior biopsy indicates involvement of bone, block resection with continuity defect is the choice of treatment.
Question.6. Discuss the differential diagnosis of jaw swellings.
Describe the investigation, clinical features, and treatment of adamantinoma.
Answer.
Differential Diagnosis of Jaw Swellings
Swelling arising from the mucoperiosteum, i.e. epulis. It has 5 varieties:
- Fibrous
- Granulomatous
- Myeloid
- Sarcomatous
- Carcinomatous.
Swellings arising from tooth germs, i.e. odontomes. The diffrent varieties are:
Epithelial odontomes
- Dental cyst
- Dentigerous cyst
- Adamantioma.
The following are the rare varieties:
Connective tissue odontomes
- Fibrous
- Cementous
- Sarcomatous.
Composite odontomes (i.e. arising from both epithelial and connective tissue elements):
- Radicular
- Compound follicular
- Composite complex.
Osseous tumors: Any bone tumor can affect jaw
Benign:
- Fibro-osseous group
- Paget’s disease
- Osteoclastoma.
Malignant tumors:
- Osteosarcoma
- Squamous cell carcinoma
- Burkitts tumor
- Columnar cell carcinoma of maxillary antrum.
Inflammatory group:
- Alveolar abscess
- Osteomyelitis
- Actinomycosis.
Question.7. Write short note on Vincent’s angina.
Answer. It is an acute ulceromembranous stomatitis or acute ulcerative gingivitis.
This disease is caused by Vincent’s organism-Borrelia vincentii an anaerobic spirochete and fusiform.
Vincent’s angina Precipitating Factors
- Malnutrition, diabetes mellitus, carious tooth, war seasons,winter, etc.
- The disease starts in the intergingival defects as a deep penetrating ulcer, which results in a spontaneous gingival hemorrhage.
- Once infections spread to tonsillar region, it is called as Vincent’s angina. Very severe painful condition.
Vincent’s angina Clinical Features
- Common in children and young adults between 20 and 40 years of age.
- It is a gangrenous devastating stomatitis which begins in mucus membrane of corner of mouth or cheek which progress rapidly to involve entire thickness of lips or cheek or both with necrosis and sloughing of entire tissue which is observed in poorly nourished children and debilitated adults.
- It start from lips extend to gums, spread to cheeks, bone,soft tissues and skin leading to extensive tissue loss with severe toxemia.
- There is presence of excessive salivation, fetid odor with destruction, discharge and toxic features.
Vincent’s angina Investigations
- Culture of Borrelia vincentii
- X-ray of involved part shows bony destruction.
Vincent’s angina Treatment
- Systemic antibiotics, i.e. higher doses of penicillin and metronidazole should be given.
- High protein and vitamin rich diet should be given through nasogastric intubation.
- Wound irrigation is done and liberal excision ofdead tissue should be carried out.
- Blood transfusion is given.
- Later on patient require flaps to cover the defect.
Question.8. Write short note on tumors of jaw.
Or
Write short note on swelling of jaw.
Or
Discuss etiology, clinical features and treatment of tumor of jaw.
Or
Describe swelling of the jaw and its management.
Answer.
Question.9. Name the treatment modalities and differentiating features of adamantinoma and osteoblastoma.
Answer.
Question.10. Classify oral mucosal lesions. Describe the clinical features and histopathological features of submucosal fibrosis.
Answer. Classifiation of oral mucosal lesions
Genodermatous
White sponge nevus
Hereditary benign intraepithelial dyskeratosis
Pachyonychia congenita
Porokeratosis
Darier’s disease
Pseudoxanthoma elasticum.
Non-infective Disease
1. Vesicular:
- Erythema multiforme
- Pemphigus
- Bullous lichen planus.
2. Non-vesicular:
Lichen planus.
3. Collagen disorders:
- Lupus erythematous
- Scleroderma.
4. Degenerative
- Oral submucous firosis.
5. Pigmentation:
- Anemia
- Addison’s disease
- Racial pigmentation
OSMF is defined as “An insidious chronic disease affecting any part of oral cavity and sometime pharynx.
Although occasionally preceded by and/or associated with vesicle formation, it is always associated with juxta-epithelial inflammatory reaction followed by firoelastic changes in lamina propria, with epithelial atrophy leading to stiffness of oral mucosa and causing trismus and inability to eat.” —Pindborg (1966)
submucosal fibrosis Clinical Features
- It is caused during 20 to 40 years of age.
- Females are affcted more than males.
- In OSMF firotic changes are frequently seen in buccal mucosa, retromolar area, vulva, tongue, etc.
- Initially patient complains of burning sensation in the mouth, particularly during taking hot and spicy foods.
- There can be excessive salivation, decreased salivation and defective gustatory sensation.
- In initial phase of disease palpation of mucosa elicits a“wet leathery” feeling.
- In advanced stage, the oral mucosa losses its resilience and become blanched and stif and thereby causing trismus.
- Palpation of mucosa often reveals vertical firous bands.
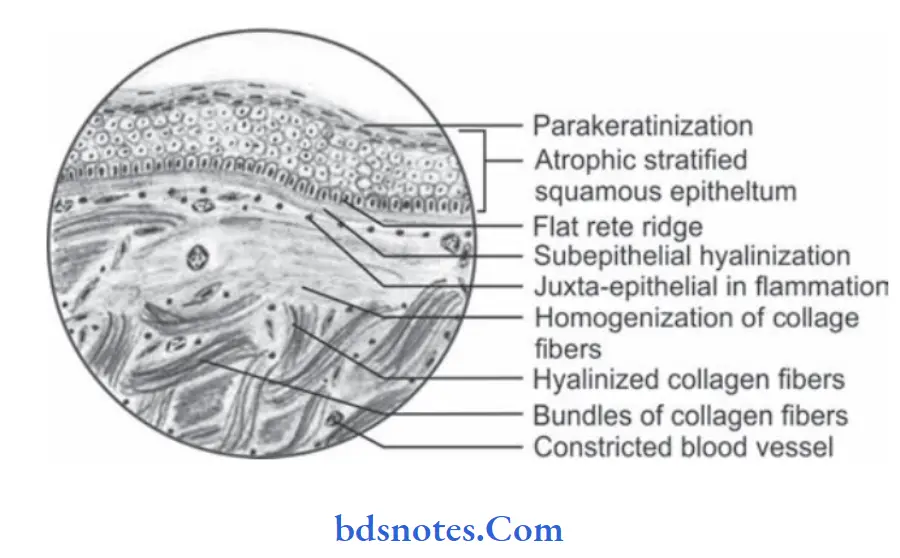
submucosal fibrosis Histopathology
Microscopically OSMF reveals following features:
- Overlying hyperkeratinized, atrophic epithelium often shows flttning and shortening of rete pegs.
- There can be variable degree of cellular atypia or epithelial dysplasia.
- In OSMF dysplastic changes are found in epithelium which include nuclear pleomorphism, severe intercellular edema, etc.
- Stromal blood vessels are dilated and congested and there can be areas of hemorrhage.
- Underlying connective tissue stroma in advanced stage of disease shows homogenization and hyalinization of collagen fiers.
- Decreased number of firoblastic cells and narrowing of blood vessels due to perivascular firosis are present.
- There can be presence of signet cells in some cases.
Question.11. Write the oral manifestations of systemic disease.
Answer.
Oral Manifestations Of Systemic Disease
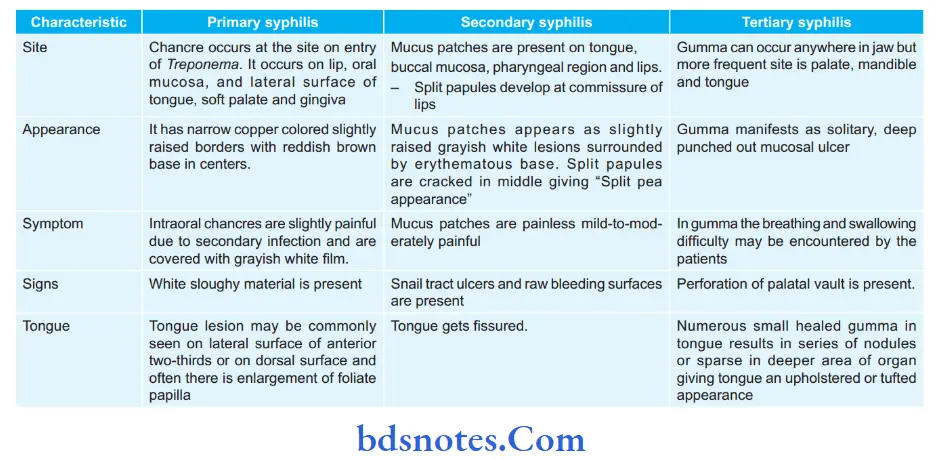
Systemic disease Syphilis
The oral manifestations of syphilis are given in the folowing table.
Systemic disease Tuberculosis
Oral Manifestations Of Tuberculosis
- Tuberculous infection in oral cavity may produce nodules,vesicles, fisures, plaque, granulomas or verrucal papillary lesions.
- The tuberculous lesions oforal cavity are tuberculous ulcers,tuberculous gingivitis and tuberculosis of salivary gland.
- Tongue is most common location for the occurrence,besides this palate, gingiva, lips, buccal mucosa, alveolar ridge and vestibules may also be affcted.
- Tongue lesions: Tuberculous lesion of tongue develops on the lateral borders and appears as single ormultiple ulcers which are well defied, painful, fim and yellowish gray in color.
- Lip lesions: The lesions produce small, non-tender, granulating ulcer at the mucocutaneous junction.
- Gingival lesions: These lesions produce small granulating ulcers with concomitant gingival hyperplasia.
- Tuberculous lesion of jaw bone: Chronic osteomyelitis of maxilla and mandible may occur and infection reaches to bone via blood or root canal or extraction socket.
Tuberculous osteomyelitis of jaw bone produces pain, swelling, sinus or fitula formation.
Systemic disease Leprosy
- Oral manifestations of leprosy
- In oral cavity, the disease produces tumor like lesions called as “lepromas” which are found on lips, gingiva,tongue and hard palate.
- Oral lesion appears as yellowish soft or hard sessile growth which have tendency to breakdown and ulcerate.
- Ulceration, necrosis and perforation of palate.
- Fixation of palate with loss of uvula.
- Diffilty in swallowing and regurgitation.
- Cobblestone appearance of tongue with loss of taste sensation.
- Chronic gingivitis, periodontitis and candidiasis are present.
- The enamel hypoplasia of teeth, pinkish discoloration of teeth and tapering of teeth is present.
Systemic disease Herpes Zoster
Oral Manifestations of Herpes Zoster
- Herpes zoster may involve the face by infection of trigeminal nerve, mainly fist branch.
- There is usually involvement of skin and oral mucosa supplied by trigeminal nerve.
- Lesions of the oral mucosa are extremely painful vesicles which may be found on the buccal mucosa, tongue,
- pharynx and larynx and uvula.
- This vesicle generally ruptures and leaves the area of erosion.
- The erosive ulcers heal up in a few days without scar formation.
- In herpes zoster, neuralgic pain in oral cavity stimulates tooth ache.
- The pain may persist long after the lesion heals up and the condition is known as post-herpetic neuralgia.
Question.12. Write short note on lipoma.
Answer. Lipoma is a benign neoplasm arising from yellow fat.
Often it can be hyperplasia or combination of neoplasm and hyperplasia.
- It is the most common benign tumor
- It is also called as universal tumor (ubiquitous tumor) as it can occur anywhere in the body except brain.
Types Of Lipoma
- Localized (encapsulated): Localized lipoma is encapsulated with yellowish orange.
- Color.
- Diffse (nonencapsulated): Diffse lipomas are not encapsulated and not localized. It is common in palm, sole, head,neck. lt is seen in subcutaneous and intermuscular tissues.
- Superficial lipomas: They are more common; common in subcutaneous plane. It is common in back, neck, proximal extremities and abdomen. It is commonly less than 5 cm,but can attin large size.
- Deep lipomas: They are commonly intramuscular, but often may be intermuscular; often both intraand intermuscular (infitrating lipoma). They are common in lower limbs (45%), trunk (l7%), shoulder and upper limb. They attin large size compared to superfiial lipomas.
- Single lipoma: It is common. It is usually superfiial in subcutaneous plane but can be deep also.
- Multiple lipomas: They are l5% common; common in males (6:1). Common in back, shoulder and upper arm; can be symmetrical. It can be associated with many syndromes like multiple endocrine neoplasia (MEN), Cowden’s,Frohlich syndromes, etc.
- Hibernoma: Benign tumor arising from brown fat is called as hibernoma (reddish brown), which has got serpentine vascular elements.
- Fibrolipoma: Lipoma with firous component is called as firolipoma.
- Naevolipoma: Lipoma with telangiectasis is called as naevolipoma.
- Neurolipoma: (with nerve tissue and is painful), angiolipoma (with vascular element), myolipoma, chondroid lipoma, spindle cell lipoma, pleomorphic lipoma-are different types
- Depending on the type of nonadipose component associated.
Lipoma Clinical Features
- Localized swelling, which is lobular (surface), nontender.
- Oftenflctuantlike feel butactually not(because fatinbody temperature remains soft). It is usually nontransilluminant.
- Mobile, with edges slipping between the palpating figer (slip sign).
- Skin is free.
- Lipomas may be pedunculated at times.
- It is rare in children.
- Pain in lipoma may be due to neural element or compression to nerves or adjacent structures. Angiolipoma was being highly vascular is commonly tender.
- Trunk is the most common site; nape of neck and limbs are next common.
- Clinically lipoma can be single, multiple or diffse.
Lipoma Differential Diagnosis
- Neurofiroma: It moves horizontally but not longitudinally along the line of nerve. Neurofiroma is fimer.
- Cystic swellings like dermoid, sebaceous cyst.
- Liposarcoma: All lipomas are benign. Large lipoma should be diffrentiated from liposarcoma.
Lipoma Investigations
- Ultrasound or CT or MR imaging is done in deep or large or intracavitary lipomas.
- FNAC or incision biopsy is needed in large or deep or intracavitary lipomas to confim it as benign.
Lipoma Complications
- Myxomatous changes—occurs in retroperitoneal lipoma.
- Saponifiation
- Calcifiation—11% mineralization.
- Submucosal lipoma can cause intussusception and so intestinal obstruction.
Lipoma Treatment
- Excision should be done if lipomas are painful. Small lipoma is excised under local anesthesia and larger one under general anesthesia.
- Percutaneous liposuction is relatively new treatment option
Question.13. Discuss the differential diagnosis of submandibular swelling.
Answer. Differential diagnosis of submandibular swellings.
Submandibular swellings are of three types, i.e.
- Stenosis: Most commonly occurs as complication of Ludwig’s angina
- Sialectasia: It is an aseptic dilatation of salivary ductules causing grape like dilatation.
It present as a smooth, soft, fluctuant, nontransilluminating swelling which increases in size during mastication. It is tender initially. It last for many days being asymptomatic. - Acute Lymphadenitis: Very often, poor oral hygiene or a caries tooth produces painful,tender, soft enlargement of these lymph nodes.
Extraction of tooth or with improvement of oral hygiene, lymph nodes regress.
Submandibular swellings Recurrent acute
- Stones
- Stenosis
- Sialectasis.
Submandibular swellings Chronic
- Sialosis
- Autoimmune diseases
- Neoplasms.
Chronic Tuberculous Lymphadenitis: Can affect these nodes along with upper deep cervical lymph nodes.
These nodes are fim and matted.
Secondaries in the sub-mandibular lymph node arises from carcinoma of cheek, tongue, palate. The nodes are hard with or without fiity.
Non-Hodgkin’s Lymphoma: It can involve sub-mandibular lymph nodes along with horizontal group of lymph nodes in neck. The nodes are firm and rubbery in consistency.
Question.14. Describe different types of odontomes and their management.
Answer. Odontome is defied as “tumorformed byanovergrowth of complete dental tissue”. — Broca
In WHO classification of odontogenic tumors (2017) odontomes are classifid as benign mixed epithelial and mesenchymal odontogenic tumor.
Under this heading two types of odontomas are there:
- Complex odontoma
- Compound odontoma.
Compound odontome
It is defied as “A tumor like malformation (hamartoma) with varying numbers of tooth like elements (odontoids)”. —WHO
Odontome Pathogenesis
It is produced by repeated divisions oftooth germ or by multiple budding of from dental lamina with formation of many tooth germs.
Odontome Clinical Features
- It is a painless slow growing lesion.
- It occurs commonly in maxilla in incisor-canine region.
- Male and females are equally affcted.
- It is seen during 2nd and 3rd decades of life.
- At times permanent teeth fails to erupt.
Odontome Radiographic Features
Compound odontoma appears as collection of tooth like structures surrounded by radiolucent zone.
Odontome Management
- Surgical removal by enucleation is the treatment of choice.
- Odontomascanbeapproachedbyintraoralmucosalincision and removal of adequate overlying bone to expose lesion.
- Removal of entire soft tissue portion is recommended to prevent recurrence.
Odontome Complex odontome
It is defied as “a tumor-like malformation (hamartoma) in which enamel and dentin and sometimes cementum is present”.
— WHO
Odontome Pathogenesis
- It develops from dental lamina or enamel organ in place of normal tooth.
Odontome Clinical Features
- Painless slowly growing lesions.
- They form hard masses.
- Mandible is more frequently affcted.
- When the lesion becomes large it leads to expansion of bone and facial symmetry.
- Adjacent teeth may be displaced.
Odontome Radiographic Features
It appear as irregular dense radiopaque mass surrounded by thin radiolucent area overlying displaced unerupted tooth.
Odontome Management
- Enucleation or curettge is done if odontoma is source of obstruction to erupting teeth.
- Large complex odontomas should be cut in segments for removal in order to conserve normal bone and prevent jaw fracture.
Question.15. Write in brief tumors of tongue.
Answer. Following are the tumors of tongue:
Tumors of Tongue Benign
- Fibroma
- Granular cell myoblastoma
- Glomus tumor
- Leiomyoma
- Rhabdomyoma
- Neurofiroma
- Keratoacanthoma
- Traumatic neuroma
- Papilloma
- Pyogenic granuloma
- Adenoma
- Hemangioma
- Lymphangioma.
Tumors of Tongue Malignant
- Squamous cell carcinoma
- Adenocarcinoma
- Transitional cell carcinoma
- Verrucous carcinoma
- Mucoepidermoid carcinoma
- Reticular cell carcinoma
- Lymphosarcoma
- Angiosarcoma
- Kaposi’s sarcoma
- Melanoma
- Rhabdomyosarcoma.
Tumors of Tongue Benign tumors
- Fibroma: It is a painless, sessile, dome shaped or pedunculated lesion with smooth contour.
On tongue it is present as circumscribed nodule.
Color of tumor is pink and its surface is smooth consistency ranges from soft to firm and elastic. - Granular cell myoblastoma: It occur over the dorsum of tongue. It is single, fim, submucosal nodule which is present within the substance of tongue.
- Glomus tumor: It is present over dorsum oftongue. Lesion is small usually less than 1 cm. Color of lesion ranges from red to purple. It is tender.
- Leiomyoma: It is present in circumvallate papillae of tongue. It is a slow growing painless lesion which is mostly pedunculated.
- Rhabdomyoma: It is a well circumscribed tumor mass, painless and growth is slow.
- Neurofiroma: It has diffse involvement over tongue.
Sessile or pedunculated elevated small nodules of various sizes are present.
Due to its diffse involvement it leads to macroglossia.
- Keratoacanthoma: Lesion is tender, present as an elevated umblicated or crateriform with depressed central core which represent plug of keratin.
- Neuroma: It presents as small swelling or nodule over the tongue.
- Papilloma: It is an exophytic lesion with cauliflwer like surface. Projections are pointed or blunt. Appearance is due to presence of deep clefts.
- Hemangioma: Part of tongue or entire tongue is involved. Loss of mobility of tongue. Color of tumor is bluish.
- Lymphangioma: It involves dorsal and ventral surfaces of tongue.
Presence of irregular nodularity over surface of tongue with grape like projections which are gray and pink in color.
Tumors of Tongue Malignant Tumors
- Squamous cell carcinoma: Non-healing ulcer present over the tongue. Edges of ulcer are everted and base is indurated. Ulcer bleeds on touch.
- Transitional cell carcinoma: Lesion arises from the base of tongue. Lesion is ulcerated with granular eroded appearance.
- Malignant melanoma: A deep pigmented area is seen over the tongue which is ulcerated and hemorrhagic.
- Verrucous carcinoma: Pebbly surface is present which is keratinized. Have rugae like folds with a cleft in between.
Question.16. Write short note on cavernous lymphangioma.
Answer. It is a congenital localized cluster of dilated lymph sacs in the skin and subcutaneous tissue that has failed to join the normal lymph system during development period.
Cavernous Lymphangioma Clinical Features
- It is present at birth.
- It is common on face, mouth, lips and tongue.
- Disfigurement is present over the child which is noticed by his/her parents.
- Lesion is soft, lobulated and is flctuant.
- It is a brilliant transilluminant larger lymphatic swelling with multiple communicating lymphatic cysts.
- It often extends in deeper plane like muscle. It is common on face, mouth, lips and tongue
Cavernous Lymphangioma Differential Diagnosis
- Hemangioma: It occurs at posterior triangle ofneck. Hemangioma is soft, cystic and flctuant. Its transillumination is negative and sign of compressibility is positive.
- Lipoma: It is a soft lobular swelling with fluctuation.
While palpating edge of lipoma slips between palpating figers.
Both transillumination and compressibility tests are negative. - Cold abscess: It is a soft, cystic, fluctuant swelling with negative transillumination. It is located at the carotid triangle.
Cavernous Lymphangioma Management
- Surgical excision of lesion is done for removing complete bulk of lesion. All the loculi or cysts should be removed.
- As lymphangioma extends to the muscle plane, to avoid recurrence careful examination should be done.
Cavernous Lymphangioma Complications
- As the size of lymphangioma is large, it can lead to diffiulty in breathing in both neonates and infants.
- Secondary infection can occur in lymphangioma
- In mediastinum, it can lead to dyspnea, dysphagia because of compression of trachea.
Question.17. Write short note on acute laryngitis.
Answer. Acute laryngitis may occur as an isolated infection or as a part of a generalized bacterial or viral upper respiratory Tract Infection.
Acute laryngitis Etiology
- Infection, i.e. viral
- Excessive use of voice, i.e. in teaching, public speaking,singing
- Leisure activities such as cheering at sport event
- Inhalation of smoke or fumes
- Aspiration of caustic chemicals.
Acute laryngitis Clinical Features
- It begins with hoarseness of voice.
- Pain is present while speaking or swallowing.
- Presence of dry cough
- Fever, malaise, restlessness and dyspnea
- Shortness of breadth
- Throat clearing
- Laryngeal edema.
Acute laryngitis Treatment
- Primary treatment involves resting of voice.
- For viral infection symptomatic care includes an analgesic and throat lozenges for pain relief.
- Bacterial infections require antibiotic therapy, i.e. 250 mg of cefuroxime twice daily.
- Severe acute laryngitis requires hospitalization.
- When laryngeal edema results in airway obstruction tracheostomy should be done.
Question.18. Discuss briefly stridor.
Or
Write briefly on stridor.
Answer. Stridor is an abnormal, high-pitched sound produced by turbulent airflow through a partially obstructed airway at the level of the supraglotts, glotts, subglotts, and/or trachea.
- Stridor is a symptom, not a diagnosis or disease, and the underlying cause must be determined.
- Stridor may be inspiratory, expiratory, or biphasic depending on its timing in the respiratory cycle.
- Inspiratory stridor suggests a laryngeal obstruction,while expiratory stridor implies tracheobronchial obstruction.
- Biphasic stridor suggests a subglottic or glottic anomaly.
- In addition to a complete history and physical,as well as other possible additional studies, most cases require flxible and/or rigid endoscopy to adequately evaluate the etiology of stridor.
Stridor Pathophysiology
Gases produce pressure equally in all directions; however,when a gas moves in a linear direction, it produces pressure in the forward vector and decreases the lateral pressure.
When air passes through a narrowed flxible airway in a child, the lateral pressure that holds the airway open can drop precipitously (the Bernoulli principle) and cause the tube to close.
This process obstructs airflw and produces stridor.
Stridors may result from lesions involving the CNS, the cardiovascular system, the GI system, and the respiratory tract.
Stridor Etiology
Stridor may occur as a result of:
- Foreign bodies (e.g., aspirated foreign body, aspirated food bolus);
- Tumor (e.g., laryngeal papillomatosis, squamous cell carcinoma of larynx, trachea or esophagus)
- Acute lymphatic leukemia (ALL) (T-cell ALL can present with mediastinal mass that compresses the trachea and causes inspiratory stridor)
- Infections (e.g., epiglottitis, retropharyngeal abscess, croup)
- Subglottc stenosis (e.g., following prolonged intubation or congenital)
- Airway edema (e.g., following instrumentation of the airway, tracheal intubation, drug side effct, allergic reaction)
- Subglottc hemangioma (rare)
- Vascular rings compressing the trachea
- Many thyroiditis such as Riedel’s thyroiditis
- Vocal cord palsy
- Tracheomalacia or tracheobronchomalacia (e.g., collapsed trachea)
- Congenital anomalies of the airway are present in 87% of all cases of stridor in infants and children.
- Vasculitis.
Stridor Treatment
Stridor Medical Care
- Immediate tracheal intubation should be done.
- Expectant management with full monitoring, oxygen by facemask, and positioning the head on the bed for optimum conditions (e.g., 45–90°).
- Use of nebulized racemic adrenaline epinephrine (0.5 to 0.75 mL of 2.25% racemic epinephrine added to 2.5 to 3 mL of normal saline) in cases where airway edema may be the cause of the stridor.
- Use of dexamethasone (Decadron) 4–8 mg IV, 8 12 hourly in cases where airway edema may be the cause of the stridor; note that some time (in the range of hours) may be needed for dexamethasone to work fully.
- Use of inhaled Heliox (70% helium, 30% oxygen); the effct is almost instantaneous.
Helium, being a less dense gas than nitrogen, reduces turbulent flw through the airways.
Always ensure an open airway. - In obese patients elevation of the panniculus has shown to relieve symptoms by 80%.
Stridor Surgical Care
- Certain conditions, such as severe laryngomalacia,laryngeal stenosis, critical tracheal stenosis, laryngeal and tracheal tumors and lesions (e.g., laryngeal papillomas, hemangiomas, others), and foreign body aspiration,require surgical correction.
- Occasionally, tracheotomy is done to protect the airway to bypass laryngeal abnormalities and stent or bypass tracheal abnormalities.
- Other conditions, such as retropharyngeal and peritonsillar abscess, may have to be dealt with on an emergent basis.
Question.19. Write briefly on lesions of lips.
Answer. Following are the lesions of lips:
Developmental Lesions
- Congenital lip pits
- Commissural lip pits
- Double lip
- Cleft lip.
Inflammatory Lesions
- Glandular cheilitis
- Angular cheilitis
- Granulomatous cheilitis
- Contact cheilitis
- Actinic cheilitis
- Eczematous cheilitis
- Exfoliative cheilitis
- Plasma cell cheilitis
- Cheilitis due to drugs.
lip Carcinoma
Miscellaneous
- Actinic elastosis
- Lip ulcers.
Developmental Lesions Of Lip
Congenital lip Pits
- It is also known as congenital fitula.
- Pathogenesis: It occur due to failure of union of embryonic sulcus of lip which leads to persistent lateral sulci on embryonic mandibular arch.
- Features: It more commonly occurs in females; vermilion border of lip is commonly involved.
Lower lip is involved; lesion is present in form of depression; on palpation, mucous secretion is seen from the base of lip pit. - Treatment: Surgical excision is done.
Commissural lip Pits
- They are mucosal invagination which arises at vermilion border of lip.
- Pathogenesis: Its occurrence is due to failure of normal fusion of embryonic maxillary and mandibular processes.
- Features: Males are commonly affcted; it present as unilateral or bilateral pit at corners of mouth on vermilion border.
Its size ranges from a shallow depression to an open tract measuring 4 mm; On palpation less amount of saliva ooze out. - Treatment: Surgical excision is done.
Double Lip
- It is a fold of excessive tissue over inner mucosa of lip.
- Pathogenesis: It arises during second week of gestation because of persistence of sulcus between pars glabrosa and pars villosa of lip.
- Features: Inner aspect of lip is involved; at times when the upper lip become tensed, double lip give appearance of cupid bow.
- Treatment: Surgical excision is done
Cleft lip
- Cleft lip results from abnormal development ofthe median nasal and maxillary process.
- Pathogenesis: This is due to imperfect fusion of maxillary process with median nasal process which produce lateral cleft lip and due to failure of fusion of two median nasal processes which produce central cleft lip.
- Features: Patient has diffilty in sucking; defective speech is present, i.e. patient is unable to speak word such as B,F, M, P and V.
- Treatment: Millard’s criteria is use to undertake surgery for cleft lip, i.e. Rule of ten, i.e. 10 pound in weight; 10 weeks old; 10 g% hemoglobin; Millard cleft repair by rotating local nasolabial flps; proper postoperative management like control of infection, training for sucking, swallowing and speech.
Inflammatory Lesions of Lip
- Glandular cheilitis: Lower lip is mostly affected and the lip become enlarged, become fim and get everted. It mainly occurs due to sun exposure.
- Angular cheilitis: In it cracking of lips is seen from the corners. Main cause is nutritional deficiency.
- Actinic cheilitis: It is a pre-malignant lesion. Occurs due to sun exposure.
Lower lip is mostly affcted. Lip become dry and scaly. If scales are removed bleeding points are seen.
Lip Carcinoma
Vermilion border oflip and mucosa is the main site ofcarcinoma of lip.
It is common in the western elderly, white people,especially those people exposed to sunlight.
Lip Carcinoma Clinical Features
- Elderly males are affcted in 90% of cases.
- Non-healing ulcer or growth is a common presentation.
- Lesion appears in the form of white plaque of non-healing ulcers.
- Edges are everted and indurated, this is characteristic of carcinoma.
- Ulcer contain slough in flor.
- Bleeding may occur from ulcer.
- Pain and paresthesia may occur.
- Lesion may get fied to the subcutaneous structure of lip.
- Ulcer spreads and destroys the tissue of lip and chin.
- Submental and submandibular lymph nodes are involved,lymph node becomes hard and maybe fied.
Lip Carcinoma Treatment
- If lesion is less than 2 cm, then curative radiotherapy, either brachytherapy or external beam radiotherapy. It gives a good cure.
- If tumor is more than 2 cm, wide excision is done. Excision of lower lip up to one-third can be sutured primarily,in layers keeping vermilion border in proper apposition without causing any microstomia.
- Excision of more than one-third of the lip requires reconstruction using different flaps.
Question.20. Write short note on tongue tie.
Answer. It is also known as ankyloglossia.
Ankyloglossia is the condition which arises when the inferior frenulum attaches to the bottom of tongue and subsequently restricts free movements of the tongue.
Tongue Tie Clinical Features
- Males are affected more commonly than females
- It can cause feeding problems in infants
- Tongue movements become restricted.
- It causes speech defects specially articulation of the sounds l,r,t,d,n,th,sh and z
- It leads to persistent gap between the mandibular incisors.
- When attmpt is made for sticking the tongue out a V shaped notch is seen at the tip of tongue.
- As high frenal attachment is present and patient has periodontal problems.
- During protrusion, lateral margin and tip of tongue is everted with dorsal mid part heaping.
Tongue Tie Management
Tongue tie should be treated surgically under the local anesthesia.
Tongue Tie Procedure
- Local anesthesia should be given to the patient.
- Retract the tongue and held the tongue by traction suture.
- This makes frenum taut and easily visible for surgical release.
Take a sharp scissor and made a cut of 1 to 2 cm midway between the tip of tongue and lingual surface of mandible.
Cut should be given in such a way that blade of scissor should be parallel to flor of mouth. - Place a hemostat across frenal attchment at base of tongue and keep it clamped for 3 min. This provide bloodless fild for surgery.
- As hemostat is removed, place an incision through area of previously closed hemostat.
- Care should be taken not to injure submandibular duct,papilla and blood vessels under flor of mouth.
- Wound margins are carefully undermined should be approximated and closed without tension, i.e. in linear fashion.
Question.21. Describe diagnostic features and treatment of aphtous ulcers of tongue.
Answer.Diagnostic Features
Diagnosis of aphtous ulcers is made on basis of clinical examination:
- Minor aphthous ulcers: Painful round ulcer with yellow base and red margins. Size of the lesion is 0.4 to 1 cm.
- Major aphthous ulcers: Large and deep ulcers. Size may reach to 5 cm. They restrict the mobility of tongue and uvula.
- Herpetiform aphthous ulcers: These ulcer are numerous and very painful. They are small 1-2 mm in diameter. They occur in crops.
Aphtous Ulcers of TongueTreatment
- Minor aphthous ulcers: Topical corticosteroid ointment is applied over ulcer 4 to 5 times a day. Nutritional supplements should be given. Oral hygiene should be maintained.
- Major aphthous ulcer: Chlorhexidine gluconate should be given. Triamcinolone acetate is locally applied, choline salicylate gel is given.
- Herpetiform aphthous ulcer: Nutritional supplements should be given. Oral hygiene should be maintained.
Chlorhexidine or tetracycline mouthwash will lead to rapid heading.
Question.22. Write short note on myeloid epulis.
Answer. It is also known as giant cell epulis.
Myeloid Epulis Origin
Two views are given over the origin of myeloid epulis:
1. It is an osteoclastoma arising from the peripheral part of jaw and so present under the gums.
2. It is an inflammatory hyperplasia. Granuloma extends in the body of bone where it produces cyst like structure and is surrounded by shell of bone giving the pseudo appearance of osteoclastoma.
Myeloid Epulis Clinical Features
- Myeloid epulis is found on gingival margin between teeth anterior to permanent molars.
- Swelling is round, soft and is maroon or purplish in color.
- Tumor is painless.
- Its consistency is firm and surface is smooth.
Myeloid Epulis Investigations
- After doing biopsy on microscopical examination there is presence of firous tissue with rich vascularity and giant cells of foreign body type.
- X-ray examination shows typical soap bubble appearance of osteoclastoma.
Myeloid Epulis Complications
- Ulceration
- Serious hemorrhage.
Myeloid Epulis Treatment
- If swelling is small the treatment is curettge along with filing the cavity with cancellous bone chips.
- If tumor is large radical excision of bone is done along with the grafting.
Question.23. Define, and describe clinical features and principles of treatment of leukoplakia.
Answer. Leukoplakia is defined as a white patch or plaque that cannot be characterized clinically or pathologically as any other disease and is not associated with any physical or chemical causative agent except use of tobacco.
First International Conference on oral leukoplakia Malmo, Sweden (1984) or Modified WHO
Leukoplakia Definition (1984)
Leukoplakia Clinical Features
- Usually the lesion occurs in 4th, 5th, 6th and 7th decades of life.
- Buccal mucosa and commissural areas are most frequent affcted sites followed by alveolar ridge, tongue, lip, hard and soft palate, etc.
- Oral leukoplakia often present solitary or multiple white patches.
- The size of lesion may vary from small well-localized patch measuring few millimeters in diameter.
- The surface of lesion may be smooth or fiely wrinkled or even rough on palpation and lesion cannot be removed by scrapping.
- The lesion is whitish or grayish or in some cases it is brownish yellow in color due to heavy use of tobacco.
- In most of the cases these lesion are asymptomatic, how-ever in some cases they may cause pain, feeling ofthickness and burning sensation, etc.
Leukoplakia Principles Of Treatment
- Take thorough history and do proper clinical examination.
- Remove the causative factor
- Excisional or incisional biopsy should be done.
- Manage the lesion by oral medication or by eliminating the lesion
- Long-term follow-up should be done at every 3 months interval.
- At each review, submandibular and cervical lymph nodes should be checked for signs of metastasis.
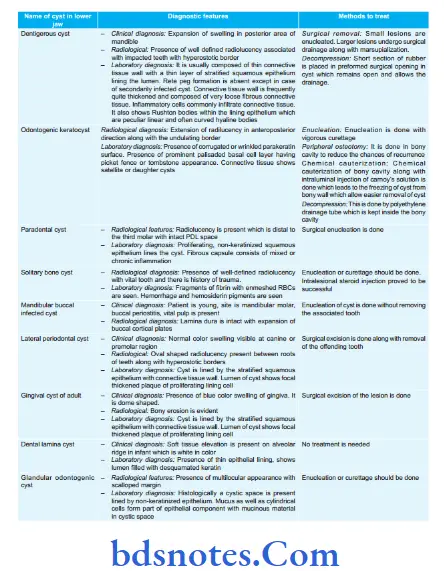
Question.24. Name cysts and tumors of “lower jaw” with diagnostic features and method to treat them.
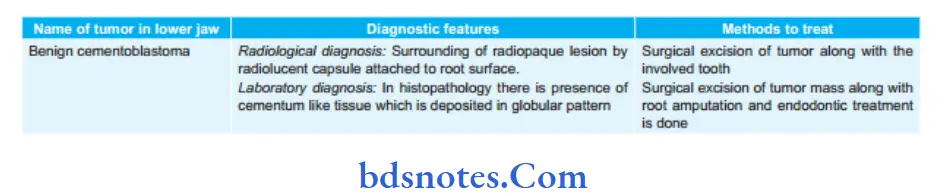
Answer. Cysts of lower jaw in see below Table.
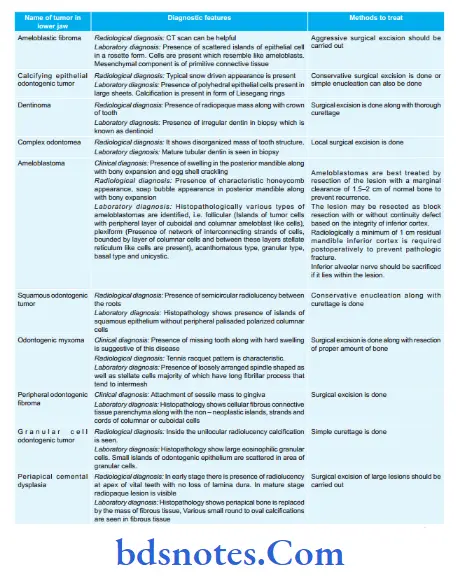
Tumors Of Lower Jaw
Question.25. Write long answer on types and causes of oral ulcer and their treatment.
Answer. Aphthous ulcer is the most common type of nontraumatic, ulcerative condition of the oral mucosa.
Types Of Oral Ulcers
Clinically, aphthous ulcers present three recognizable forms,namely:
1. Minor aphthous ulcers
2. Major aphthous ulcers
3. Herpetiform ulcers.
Oral Ulcers Minor aphthous ulcer
- It is the most common type of aphthous ulcer of the oral cavity and it appears episodically either as single lesion or in clusters of l to 5 lesions.
- The ulcers are very painful, shallow, round or elliptical in shape and they measure about 0.5 cm in diameter with a crateriform margin.
- The lesion is usually surrounded by an erythematous “halo” and is covered by a yellowish, firinous membrane.
- Minor aphthous ulcers mostly develop over the nonkeratinized mucosa, e.g. lips, soft palate, anterior fauces,flor of
- the mouth and ventral surface of the tongue (gland bearing mucosa), etc.
- The ulcer lasts for about 7–10 days and then heals up without scarring but recurrence is common.
- New lesions may continue to appear during an attck for about 3–4 weeks period.
- Few lesions may be present in the mouth almost continuously.
Oral Ulcers Major Aphthous ulcers
- Major aphthous ulcers are less common than the minor form of the disease.
- These are larger, 0.5 cm in diameter and can be as big as several centimeters in diameter.
- Major aphthous ulcers are more painful lesions than the minor variety; and they persist in the mouth for longer durations as they take more time to heal.
- These lesions are considered to be the most severe among all types of aphthae and they often make the patients ill.
- Only one or two lesions develop at a time and are mostly seen over the lips, soft palate and fauces, etc.
Besides involving the non-keratinized mucosa, major aphthous ulcers can involve the masticatory mucosa as well, such as the dorsum of the tongue and gingiva, etc. - The ulcer appears crateriform (owing to its increased depth), and it heals with scar formation in about 6 weeks time.
- Few lesions may look like malignant ulcers, moreover sometimes these lesions occur in association with HIV infections.
- Major aphthous ulcers often become secondarily infected and in such cases, the healing process is further delayed.
Oral Ulcers Herpetiform ulcers
- Herpetiform type of aphthous ulcers produce recurrent crops of extremely painful, small ulcers in the oral mucosa, which resemble herpetic ulcers. However, these ulcers do not develop following vesiculations and exhibit no virus-infected cells.
- Their numbers vary from few dozens to several hundred and each ulcer is surrounded by a wide zone of erythema.
- The size of these ulcers ranges between l to 2 mm in diameter only. However, on few occasions, small ulcers coalesce
- together to form large irregular ulcers.
- The ulcers last for several weeks or months.
- Children in their late teens often suffer from this disease and the lesions occur in both gland bearing mucosa as well as over-keratinized mucosa.
- The lesions usually heal up within l to 2 week time.
Causes of oral ulcer
The exact etiology is not known and only the probable factors have been identified which are as follows:
- Genetic predisposition: The disease often affects several members of the same family and moreover identical twins are most frequently affected.
- Exaggerated response to trauma: The ulcer develops in those mucosal sites which are subjected to trauma in the past. e.g. tooth prick injury.
- Immunological factors: The disease may occur due to some autoimmune reactions, or in patients with immunosuppression, e. g. AIDS.
Some investigators believe, then it is an immune complex-mediated Type III or cell-mediated type IV reaction. - Microbiologic factors: The disease may be caused by herpes simplex virus Type I or S. sanguinis.
- Nutritional factors: Deficiency of vitamin B12, folate and iron, etc. often reported in patients with aphthous ulcer; moreover supplementation of these elements may cause rapid recovery.
- Systemic conditions: Behcet’s syndrome, Crohn’s disease and celiac disease are associated with increased incidences of aphthous ulcer.
- Hormonal imbalance: Hormonal change during menstrual cycle may be associated with higher incidence of aphthous ulcer.
- Non-smoking: The disease almost exclusively occurs in nonsmokers or the people those who have given up smoke recently.
- Allergy and chronic asthma: Allergic manifestations to any medicines or foods (e.g. Nuts and chocolates, etc.) may lead to the development of aphthous ulcer.
- Miscellaneous factors: Stress and anxiety.
Oral Ulcers Treatment
Oral Ulcers Medicinal treatment
- Topical corticosteroid i.e. 0.1% triamcinolone acetonide QDS is effctive on daily use.
- Topical anesthetics i.e. 2% viscous lidocaine, benzocaine and benzydamine hydrochloride can reduce pain.
Topical protective emollient base can be given. - Topical application of sucralfate 4 times a day has soothing effect on an ulcer.
- Topical tetracycline mouthwash QDS for 5 to 7 days provides good response.
- Beclomethasone spray is given in severe cases.
- In resistant cases systemic steroids can be given.
Most commonly beclomethasone or prednisolone syrup in swish and swallow method is advised.
In some cases prednisolone tabelet 20 to 30mg/day and beclomethasone 2 to 3 mg per day for 4 to 8 days can be given.
Oral Ulcers Surgical treatment
Oral Ulcers Laser surgery
Surgical removal of apthous ulcer should also be used.
Laser ablation shortens the duration and decreases the associated symptoms.
CO2 or Nd: YAG lasers are used. Laser treatment requires frequent visits.
Oral Ulcers Local Cauterization
Application of 0.5% hydrogen peroxide, 1 to 2% of silver nitrate or silver nitrate caustic stick represents several older therapeutic methods which reduce duration of solitary oral ulcer.
Question.26. Write short answer on premalignant conditions of oral cavity.
Answer. The premalignant condition is defined as “A generalized state of body, which is associated with significantly increased risk of cancer development”.
Following are the premalignant conditions of oral cavity:
- Leukoplakia: Its incidence in those who smoke or chew pan is 20% while its incidence in nonsmokers is 1%.
Its incidence in turning malignancy is 4 to 10% which increases with age, duration of pan chewing and smoking. - Erythroplakia: It is a red velvety lesion which has incidence of malignancy till around 15%. It is 17 to 20 times more potentially malignant than leukoplakia
- Oral submucus firosis: 4.5 to 7.6% of oral submucus fi brosis cases turn into malignancy.
- Syphilitic glossitis: Tertiary syphilis leads to chronic superfiial glossitis which leads to carcinoma of tongue. This is rare nowadays.
- Dyskeratosis congenita: Reticular atrophy, nail dystrophy and leukoplakia in oral cavity.
- Sideropenic dysphagia: It is common in Scandinavian females. It leads to atrophy of epithelium and become potentially malignant. Proper iron therapy controls the disease and reduces the risk.
- Chronic hyperplastic candidiasis: It is common in commissures of moth and tongue.
Dense plaque of leukoplakia is common with curdy white patches due to candida albicans infection.
It is treated by systemic antifungals or surgical excision or laser therapy. - Papilloma of tongue or cheek
- Discoid Lupus erythematosus
- Oral lichen planus

Leave a Reply