Odontogenic Tumors Question And Answers
Question 1. Classify odontogenic tumors and describe clinical features, radiological appearance and differential diagnosis of ameloblastoma.
Or
Write short note on ameloblastoma.
Answer.
Classification of Odontogenic Tumors by WHO (2017)
- Malignant Odontogenic Tumors
- Ameloblastic carcinoma
- Primary intraosseous carcinoma, NOS
- Sclerosing odontogenic carcinoma
- Clear cell odontogenic carcinoma
- Ghost cell odontogenic carcinoma
- Odontogenic carcinosarcoma
- Odontogenic sarcomas
Benign Odontogenic Tumors
- Epithelial Origin
- Ameloblastoma, conventional
- Ameloblastoma, unicystic type
- Ameloblastoma, extraosseous/peripheral type
- Metastasizing (malignant) ameloblastoma
- Squamous odontogenic tumor
- Calcifying epithelial odontogenic tumor
- Adenomatoid odontogenic tumor
- Mixed (Epithelial-Mesenchymal) Origin
- Ameloblastic fibroma
- Primordial odontogenic tumor
- Odontoma
- Compound type
- Complex type
- Dentinogenic ghost cell tumor
- Mesenchymal Origin
- Odontogenic fibroma
- Odontogenic myxoma/myxofibroma
- Cementoblastoma
- Cemento-ossifying fibroma
Read And Learn More: Oral Medicine Question And Answers
Ameloblastoma
Ameloblastoma is defined as “usually unicentric, non – functional, intermittent in growth, anatomically benign and clinically persistent”. –Robinson.
Etiology
- Irritation which occurs in the posterior region of mandible may lead to ameloblastoma.
- As per Robinson, one third cases of ameloblastoma had historyof oral infection, extraction of teeth and injuries to the teeth.
- Dietary deficiency may lead to ameloblastoma as this causes defect in development of tooth germ which cause an irregularity in the ameloblastic layer.
Pathogenesis
Since epithelium of the tumor resemble normal enamel organ, this suggests that ameloblastoma arises from dental epithelium. Various possibilities of development of ameloblastoma are:
- Ameloblastoma originates either in maxilla or in mandible from the epithelium which forms the tooth. Various potential epithelial sources are enamel organ, epithelial cell rest of Malassez, reduced enamel epithelium and epithelial lining of odontogenic cysts mainly the dentigerous cysts.
- Trigger or the stimulus for neoplastic transformation of epithelial residues is an unknown mechanisms by which ameloblastomas acquire growth and invasion, an advantage include overexpression of anti-apoptotic proteins such as Bcl-2 and Bcl-XL and the interface proteins.
- Heterotrophic epithelium in other parts of body mainly in pituitary gland acts as source of origin.
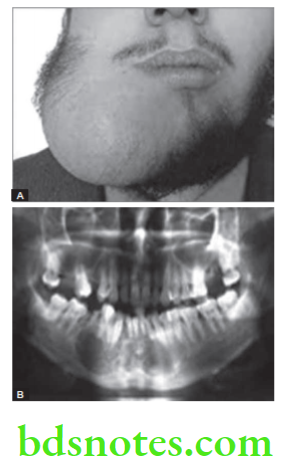
Odontogenic Tumors Clinical Features
- It has high predilection for males and is seen in blacks. Most of the patients between 20 to 50 years of age. Mean age of is about 40 year.
- It develops in molar area of ramus of mandible and occurs in maxilla in third molar area followed by maxillary sinus and floor of the nose.
- Neoplasm is preceded by the extraction of teeth, cystectomy and some other traumatic episodes.
- It begins as a central lesion of bone which is slowly destructive but tends to expand bone rather than perforating bone.
Odontogenic Tumors Symptoms
- Patient notices a increasing facial asymmetry.
- Teeth in involved area are displaced and become mobile.
- Pain and paresthesia may occur, if lesion is pressing any nerve or is secondarily infected.
Odontogenic Tumors Signs
- In later stage, lesion show ovoid and fungiform enlargement, which is hard and nontender.
- As tumor enlarges palpation may elicit hard sensation and crepitus.
- Surrounding bone become thin so fluctuation and eggshell crackling is elicited.
- It left untreated for many years the expansion is extremely disfiguring, fungating and ulcerative type of growth characteristic of that of carcinoma is seen.
Odontogenic Tumors Radiographic Appearance
- Radiodensity: In early stages, area of bone destruction which is well-defined and is indicative of slow growth with hyperostotic borders.
- Margins: Outline is smooth, scalloped, well-defined and well-corticated. Walls of the cavity are coarse.
- Appearance: Honeycomb appearance or a soap-bubble appearance. In advance stage, perforated cortical plate may contribute to multilocular appearance.
- Progress: In early stage, ameloblastoma present as bubblelike appearance with fairly large, round and distinct compartments. As tumor grows and expands compartments may coalesce and fuse. As lesion again increases in size the cortex is expanded and destroyed.
- Effect on Surrounding Structure: Jaws are enlarged, depending on overall size of the tumor. Excessive root resorption may occur.
- Egg-shell of bone: Expansion and thinning of cortical plate occurs leaving thin eggshell of bone. Perforation of bone is seen.
Ameloblastoma Differential Diagnosis
- Small and unilocular ameloblastoma:
- Residual cyst: There is history of extraction of teeth.
- Lateral periodontal cyst: Found in incisor, canine and premolar area in maxillary and in molar area in mandible.
- Giant cell granuloma: Anterior to molar and ameloblastoma occur in molar area.
- Traumatic bone cyst: Occur in mid-twenties and ameloblastoma occur in molar area.
- Primordial cyst: Occur in second and third decades.
- Multilocular ameloblastoma:
- Odontogenic keratocyst: It contains curved septae but tends to grow along the bone without marked expansion.
- Odontogenic myxoma: There is history of missing tooth and has a presence of septa that divide the image into much finer coarse than those in ameloblastoma. Myxoma has one or two thin sharp, straight septa which are characteristic of it. Myxomas are not expansile and tend to grow along the bone.
- Ossifying fibroma: The septa are usually wide, granular and ill-defined. Small irregular trabeculae are seen.
Ameloblastoma Diagnosis
- Clinical diagnosis: Presence of swelling in posterior region of mandible along with expansion and eggshell crackling can clinch the diagnosis.
- Radiological diagnosis: Presence of honeycomb appearance, soap bubble appearance along with expansion of bone in posterior region of mandible clinch the diagnosis.
- Laboratory diagnosis: Biopsy is to be done. Under microscope various types of ameloblastomas are present which should provide conformational diagnosis. In follicular ameloblastoma there is presence of small islands of tumor cells with peripheral layer of cuboidal and columnar ameloblast like cells. In plexiform ameloblastoma peripheral layer of cells are tall columnar in nature and often resemble ameloblast like cells. Cells situated at center portion of strands resemble stellate reticulum. In acanthomatous type cells occupying the position of the stellate reticulum undergo squamous metaplasia, sometimes with keratin formation in the anterior portion of tumor islands. In granular ameloblastoma, there is marked transformation of the cytoplasm, usually of the stellate reticulum like cells that it takes a very coarse granular eosinophilic appearance.
Ameloblastoma Treatment
- Patients having ameloblastoma should not be undergone with single standard type of therapy. Each of the patient is judged on its own merits which are of prime considerations that either the lesion is solid, cystic, extraosseous or malignant.
- Solid lesions need less surgical excision since there is recurrence after doing curettage which is in 50 to 90% of cases.
- In patients with larger lesions en bloc excision or resection is carried out.
- Cystic ameloblastomas should be treated less aggressively.
- Peripheral ameloblastomas should be treated in conservative methodology while the malignant lesions should be treated as carcinomas.
- Follow up of patients with central carcinoma is must because recurrences can be seen even after 10 to 20 years of primary treatment.
- Intra-osseous maxillary ameloblastomas can be excised with wider normal margin as compared to mandibular ameloblastomas.
Question 2. Define neoplasm. Classify benign tumors affecting jaw bone. Describe in detail clinical features, radiographic features and differential diagnosis of adamantinoma.
Or
Classify benign tumors. Write in detail about ameloblastoma.
Answer. Neoplasm is defined as an abnormal mass of tissues, the growth of which exceeds and is uncoordinated with that of normal tissue and persists in same excessive manner after cessation of stimuli which evoke the changes.
Classification of Benign Tumors
- Epithelial tissue:
- Papilloma
- Keratoacanthoma
- Squamous acanthoma
- Nevus
- Fibrous connective tissue:
- Fibroma
- Fibrous hyperplasia
- Fibrous epulis
- Giant cell fibroma
- Myxoma
- Myxofibroma.
- Cartilage tissue:
- Chondroma
- Chondroblastoma
- Chondromyxoid fibroma.
- Adipose tissue:
- Lipoma
- Angiolipoma.
- Bone:
- Osteoma
- Osteoid osteoma
- Osteoblastoma.
- Vascular tissue:
- Hemangioma
- Hereditary hemorrhagic telangiectasia
- Lymphangioma.
- Neural tissue:
- Neurofibroma
- Neurolemmoma
- Schwannoma.
- Muscles:
- Leiomyoma
- Rhabdomyoma.
- Giant cell tumor:
- Central and peripheral giant cell tumor
- Giant cell granuloma
- Giant cell tumor of hyperthyroidism.
- Teratoma
- Salivary gland tumor:
- Adenoma
- Warthin’ s tumor
- Pleomorphic adenoma.
For clinical features, radiographic features and differential diagnosis of adamantinoma refer to Ans 1 of the same chapter.
Question 3. Write short note on periapical cemental dysplasia.
Answer. Periapical cemental dysplasia is a reactive fibro-osseous lesion which is derived from the odontogenic cells in PDL.
- Usually, it is located at the apex of the teeth.
- It is an incidental finding during routine radiography.
- It is also known as fibrocementoma, sclerosing cementum, periapical osteofibrosis, periapical fibrosarcoma.
Cemental dysplasia Etiology
- Due to trauma, chronic irritation.
- Female sex hormone estrogen or progesterone may act as an etiologic factor since the disease is commonly seen in women.
- Various other factors such as metabolic disturbance, nutritional deficiency, syphilis and endocrinal imbalance leads to the condition.
Cemental dysplasia Clinical Features
- Occurs during the middle age with a mean age of 37 years.
- Male to female ratio is l:9. It is three times more common in blacks as compared to whites.
- Mandibular anterior region is commonly affected.
- Involved teeth are vital and have no history of sensitivity or pain. Occasionally, the lesions get localized very near to the mental foramen and get impinged on the mental nerve and produce pain, paresthesia or even anesthesia.
- Hypercementosis is seen with the involved teeth.
Cemental dysplasia. Radiographic Features
Radiographic features are divided into three stages:
- Radiolucent Stage:
- During the condition as the bony structure get replaced by connective tissue, the lesion appear to be radiolucent.
- There is formation of circumscribed area of periapical fibrosis which is associated with localized bone destruction.
- Margins of the radiolucent area appears to be different in lesions; some are well defined, while some are poorly defined; Some are corticated while others are non corticated.
- A thin rim of dense bone surrounds the periphery of lesion.
- Lamina dura surrounding the tooth is lost.
- Mixed Stage:
- Shape of the lesion is round, oval or irregular.
- Margins of the radiopacity are sharp but at times they are ill-defined and irregular.
- Small radiopacities are seen in the radiolucent apical area due to cementum or bone formation. This is known as cementoblastic stage.
- Radiopacity may vary from a millimeter to a centimeter or much more.
- Radiopaque Stage:
- During this stage, lesion appears to be completely opacified.
- Margins vary from well-defined to poorly defined.
- Lesion appears as well-defined radiopaque bordered by a radiolucent covering separating it from the adjacent bone.
- Hypercementosis is produced in variable cases which can be seen at the periapical region.
Radiological diagnosis Diagnosis
- Radiological diagnosis: Presence of radiolucency at apex of vital teeth with no loss of lamina dura at the early stage. In mature lesions radiopacity is present.
- Laboratory diagnosis: Biopsy demonstrates replacement of periapical bone by fibrous tissue mass. There is deposition of small, round to ovoid calcifications.
Management Radiological diagnosis
- Patient should be on follow-up as the diagnosis is made and is verified through periodic radiographic examination.
- Surgical removal or surgical enucleation is done in larger lesions.
Question 4. Write short note on radiographic features of odontomas.
Answer. Generally, the odontomes lie in between the roots of two teeth.
On radiographic examination, they usually appear like mass of calcified material which is irregular and is bounded by radiolucent bands with small periphery. (on the outer part of periphery).
Odontoma Compound Composite
- Multiple teeth like structures are seen in canine region.
- Internally multiple irregular masses are seen with varying density. The masses are separated from each other by a dark line. In some of cases, fusion of crown portion with radicular portion is seen.
- Borders of lesion are well defined in it was observed that in some cases they are smooth while in some they are irregular.
Odontoma Complex Composite
- On radiographic examination, it appear as radiopaque oval or round mass whose density is more than a bone and equal to tooth.
- Internally, a radiolucency is seen which consists of irregular masses of the calcified hard tissue.
- It is associated with an unerupted tooth.
Odontoma Cystic
- Cystic complex odontoma: It shows solid mass of the odontome but without any unerupted tooth. Dark shadow is present which represent the cystic cavity. It consists of well defined and corticated margins.
- Cystic compound odontoma: It consists of area of bone destruction which appear as dark shadow and has well defined margins which are lined by thin white layer of the cortical border. In cystic cavity, there are numerous white radiopacities which vary in both size and shape. In some of the patient, small amorphous granular densities are scattered in various parts of cavity and in some cases small denticles are present with enamel caps or without any of the distinction mass.
Odontoma Dilated
This is a single calcified structure with the more radiolucent central portion which has overall form of doughnut.
Question 5. Classify benign odontogenic tumors. Discuss clinical features and radiographic features of odontomas.
Answer.
Classification of Odontogenic Tumors by WHO
- Epithelial Origin
- Ameloblastoma, conventional
- Ameloblastoma, unicystic type
- Ameloblastoma, extraosseous/ peripheral type
- Metastasizing (malignant) ameloblastoma
- Squamous odontogenic tumor
- Calcifying epithelial odontogenic tumor
- Adenomatoid odontogenic tumor
- Mixed (Epithelial-Mesenchymal) Origin
- Ameloblastic fibroma
- Primordial odontogenic tumor
- Odontoma
- Compound type
- Complex type
- Dentinogenic ghost cell tumor
- Mesenchymal Origin
- Odontogenic fibroma
- Odontogenic myxoma/myxofibroma
- Cementoblastoma
- Cemento-ossifying fibroma
Odontomas
- Odontomas are hamartomas
- Odontomas are of two types, i.e. complex odontome and compound odontome.
Odontoma Clinical Features
- Odontomas occur during first or second decades of life.
- Compound odontome occur twice as common as compared to complex odontome.
- Mainly compound odontome occur in maxilla in canine, incisor region while the complex odontome occur in mandibular first and second molar region.
- Compound odontoma is 1 to 3cm in size but at times it can increase more than the size of a tooth.
- Patient complaints of swelling in the jaw which leads to facial asymmetry.
- Main sign of odontoma is absence of tooth from the arch, while palpating jaw expansion can be seen.
- In patients with odontoma there is presence of impaction or malpositioning or diastema or aplasia or malformation.
- For radiographic features of odonotmas in detail refer to Ans 4 of same chapter.
Question 6. Define tumor. Enumerate and classify various benign odontogenic tumors. Write in detail about ameloblastoma.
Answer. Tumor is defined as a mass of tissue formed as a result of abnormal, excessive, uncoordinated, autonomous, purposeless proliferation of cells.
For enumeration and classification of benign odontogenic tumors refer to Ans 5 of same chapter.
For ameloblastoma in detail refer to Ans 1 of same chapter.
Question 7. Describe in detail about differential diagnosis of ameloblastoma.
Answer. Ameloblastoma is defined as “usually unicentric, non-functional, intermittent in growth, anatomically benign and clincally persistent”. –Robinson
Radiological Differential Diagnosis
Ameloblastoma Small and Unilocular
- Residual cyst: There is history of extraction of the tooth.
- Lateral periodontal cyst: It is found in incisor, canine and premolar area in the maxilla, ameloblastoma occurs more in the mandibular molar area.
- Giant cell granuloma: It is found more often in areas anterior to the molars, younger age group and have more granular and ill-defined septae.
- Traumatic bone cyst: It occurs in the mid-twenties, whereas ameloblastoma is more common in the 3rd and 4th decades.
- Primordial cyst: It occurs in the mid-twenties, whereas ameloblastoma is more common in the 3rd and 4th decades.
Ameloblastoma Multilocular
- Odontogenic keratocyst: It consists of curved septae but tends to grow along the bone without marked expansion.
- Odontogenic myxoma: History of missing tooth and has a presence of septa that divide the image into much finer coarse than those in ameloblastoma. Myxoma has one or two thin, sharp, straight septa which are characteristic of it. Myxomas are not expansile and tend to grow along the bone.
- Ossifying fibroma: Septa are usually wide, granular and ill-defined. Small irregular trabeculae are seen.
Question 8. Enumerate different multilocular radiolucent lesions of jaw. Write in detail about clinical and radiographic features with differential diagnosis of ameloblastoma.
Answer. Enumeration of multilocular radiolucent lesions of jaw
- Odontogenic keratocyst
- Ameloblastoma
- Ameloblastic fibroma
- Ameloblastic fibro-odontoma
- Odontogenic myxoma
- Central giant cell granuloma
- Brown tumor
- Cherubism
- Aneurysmal bone cyst
- Metastatic tumor of jaw
- Calcifying epithelial odontogenic tumor
- Fibrous dysplasia
- Burkitt’s lymphoma
- Squamous odontogenic tumor
For details of clinical, radiographic features with differential diagnosis of ameloblastoma refer to Ans 1 of same chapter.

Leave a Reply