Nutrition And MetaBolIc DeFects
Question.1.Write short note on vitamin A defiiency.
Or
Describe the clinical features of vitamin A defiiency.
Answer. Defiiency of vitaminA causes interference with growth,reduced resistance to infections and interference with nutrition of cornea, conjunctiva, trachea, hair follicle and renal pelvis.
- VitaminA defiiency interferes with ability ofeyes to adapt to darkness and impairs visual affity.
- Children with vitamin A deficiency will experience impaired growth and development.
Causes
- Poor intake
- Malabsorption
- Disease of liver and intestine.
Clinical Features
- Earliest sign of defiiency of vitamin is diffilty in reading or sewing at night or fiding anything in darkness.
- Conjunctiva becomes dry and small grayish white raised spots appear. Bitot’s spots form grayish white triangular plaques on conjunctival surface lateral to cornea.
- Microcytic anemia.
- Cornea subsequently becomes dry and lusterless, and if there is lack of treatment changes are irreversible.
- *Keratomalacia involving the cornea leading to the ulceration and blindness may result.
- Children with vitaminA defiiency not only have retarded growth but also increased tendency to chest infection.
- Skin become dry and rough
- Imperfect enamel formation of teeth.
- Hemeralopia: Patient is unable to see bright light.
- Asteatosis, i.e. persistent dry scaling of the skin is the earliest manifestation.
- Phrynoderma, i.e. toad skin. Brown to dark brown,dry, rough, hyperkeratotic follicular papules with central keratotic horny spurs. Bilateral and symmetrical distribution in anterolateral aspects of thighs, posterolateral aspects of arms.
Read And Learn More: General Medicine Question And Answers
Treatment
- Prevention of vitamin A deficiency by giving good nutrition, intake of fresh leafy green vegetables and addition of vitamin A to food stuff.
- Single dose of oral retinol palmitate 60 mg or 200,000 IU should be given. In cases of diarrhea 50 mg IV may be given. Second dose is repeated next day and the third and last dose is given at the time of followup visit.
- Various other associated conditions such as diarrhea, dehydration, electrolytic imbalance, protein energy malnutrition should be treated by appropriate measures.
- For local treatment of eyes patient should be sent to ophthalmologist.
- If primary or secondary infections are present, antibiotics should be given to the patient.
Question.2. Write short notes on beriberi.
Answer. Beriberi is caused due to the defiiency of vitamin B1,i.e. thiamine.
Defiiency of vitamin B1 affcts growth, nutrition and carbohydrate metabolism.
Etiology
Defiiency of vitamin B1 occurs due to:
- Chronic alcohol intake
- Severe malnutrition
- Chronic debilitating diseases
Pathogenesis
Thiamine forms an essential part of two coenzymes which are important in oxidative decarboxylation of alphaketoacidosis.
Deficiency of vitamin leads to accumulation of alphaketoacidosis whose toxic effcts results in production ofberiberi.
Types Of Beriberi
- Wet Beriberi or cardiovascular beriberi: Beriberi is wet when there is cardiac involvement.
- Dry beriberi or neuritic type: Beriberi is dry when there is CNS involvement.
Clinical Features
- Beri-beri
- Wet beriberi: Palpitation, dyspnea, Cardiomegaly,warm extremities, anasarca (severe generalized edema), signs of congestive heart failure in late stage.
- Dry beriberi: Cramps, tingling and numbness in the limbs, nystagmus (cyclic movements of eyes), wrist and foot drop, ataxia, loss of equilibrium, parasthesia and confusion.
- Wernick’s encephalopathy: There is involvement of brain which is characterized by ataxia, ophthalmoplegia,confusion and disorientation.
- Korsakoff psychosis: It occurs due to involvement of mammillary bodies and confabulates with amnesia.
- Presence of angular stomatitis.
Diagnosis
- Blood thiamine is low
- Raised pyruvate and lactate levels.
- Low urinary excretion of thiamine and its metabolites
- Measuring of whole blood or erythrocyte transketolase activity before and after addition of thiamine.
In this there is low transketolase activity which increases by 15% after addition of thiamine confim the diagnosis. - There is clinical improvement after single dose of thiamine,i.e. 50 mg IM with increase in diastolic blood pressure and decrease in heart rate is another diagnostic criteria.
Treatment
- Vitamin B1 (50–100 mg daily) IM or IV is given.
- As acute crisis is over, patient has given small dose of 5 mg daily along with nourishing diet.
- Diet consists of high B complex and protein content like eggs, milk, nuts and green vegetables.
- Wet beriberi with cardiac involvement require digoxin and diuretics, if congestive heart failure is present.
Question.3.Describe briefly vitamin D defiiency.
Answer.
- Vitamin D defiiency leads to rickets in growing child and osteomalacia in adults.
- Vitamin D is essential in calcium and phosphorus metabolism. It is required for normal development of bones and teeth.
- Deficiency of vitamin D causes imperfect skeletal formation, bone disease, rickets and caries.
Vitamin D Deficiency Rickets
It occurs generally in growing children.
Clinical Features
- Infistsixmonths oflife tetanyand convulsions are common.
These above manifestations are due to hypocalcaemia. - Wrist and ankles are swollen
- Changes in bone are found in epiphyseal plates, metaphysis and shaft.
- Localized area of thinning are sometime present in skull so that a figer can produce indentation. This condition is called craniotabes.
- Pigeon breast is present.
- Developmental abnormalities of dentin and delayed eruption.
- Higher caries index.
- Hypoplasia of enamel is present.
- Pulp chamber is large.
- Malocclusion of teeth is present.
Investigations
- Radiological: Radiograph of wrist show widening of distal ends of shaft of both radius and ulna.
Zone of epiphyseal cartilage get thickened.
As these changes get completely developed, they cause saucer shaped deformity. - Biochemical changes:
- Low plasma calcium and phosphate levels
- High serum alkaline phosphatase levels
- Plasma 25 dehydroxy cholecalciferol is low or absent.
Vitamin D Defiiency Osteomalacia
It is also known as adult rickets. Only flt bones and diaphysis of long bones are affcted.
Clinical Features
- Pelvic deformities are seen in females.
- Remodeling of bone occur in absence of adequate calcium resulting in softening and distortion of skeleton.
- Bone pain and muscle weakness is present.
- Severe periodontitis is present.
Management of rickets and osteomalacia
- Dietary enrichment of vitamin D in form of milk.
- If tetany is present give IV calcium gluconate. Daily dose is 1000–2000 IU of vitamin D combined with 500–1000 mg of calcium.
- Curative treatment includes 2000–4000 IU of calcium daily for 6–12 weeks followed by daily maintenance dose of 2000–4000 IU for long period.
- Patients with osteomalacia require large dose of vitamin D and calcium, i.e. 40,000–1,00,000 IU of vitamin D and 15–20 gm of calcium lactate per day.
Question.4. Write short note on protein calorie malnutrition.
Answer. Protein calorie malnutrition leads to two diseases known as marasmus and kwashiorkor.
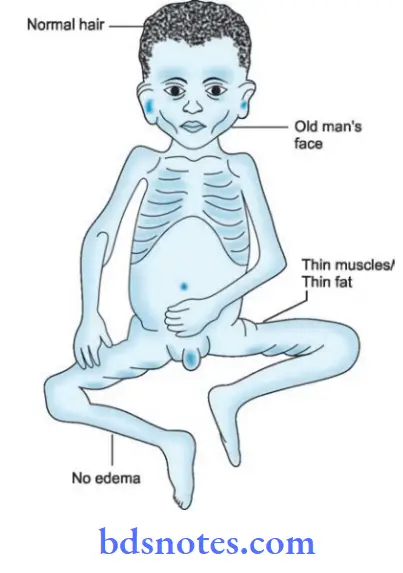
Marasmus
It is seen in infants and young children.
In marasmus, there is total defiiency of calories including protein defiiency.
Causes
- Poor intake of breastfeeds and or inadequate supply of milk and other nutrients.
- Lack of digestion
- Impaired absorption of protein.
- Protein is absorbed but cannot be metabolized satisfactorily.
- Protein is metabolized but not properly utilized.
Clinical Features
- It occurs below the age of 1 year
- There is progressive loss of subcutaneous fat.
- Child is irritable and cries excessively.
- Typical appearance of monkey face.
- Sunken and lusterless eyes.
- Delay in sittng, standing and walking.
- Abdomen may be *distended or sunken and it does not has fat in wall Lack of playful movements and persistent crying.
- Gross degree of muscle wasting is present
- Limbs are thin, look like sticks and buttcks do not contain fat.
- Head is large for body and ribs are visible.
Management
- Correction of flid, electrolytes, acidosis, hypoglycemia,hypothermia.
- Look for the infections and treat them from proper antibiotic therapy.
- Diet is given to the child which is rich in proteins, energy and essential nutrients.
Diet therapy should be continued till the child attins normal weight as well as nutritional status.
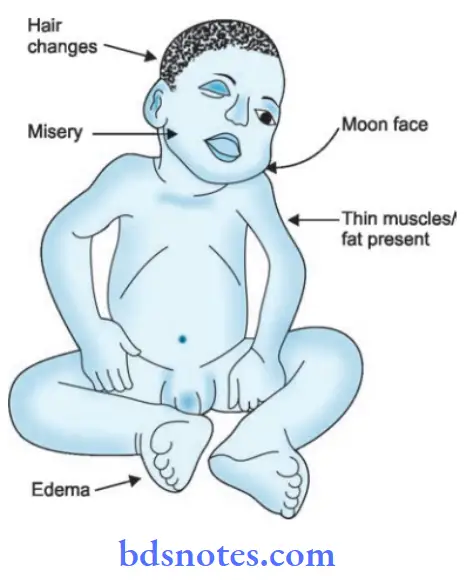
Kwashiorkor
It occurs in children between 1 to 4 years.
In Kwashiorkor there is defiiency of proteins and amino acids
cause
- Prolong febrile illness, massive burns and large chronic ulcers.
- Stress, starvation, persisting vomiting and diarrhea.
- Chronic infections, i.e. urinary tract infections, TB and parasitic infections.
Clinical Features (Signs And Symptoms)
- Growth: Failure of growth is present, child appears lean and thin. Presence of generalized edema.
- Hair: Change in the color of hair from black to blond,reddish or grey. Hairs are fie, straight and show sparse pigmentation.
- Skin: Skin become thick, pigmented, desquamated and ulcerated. A severe case with desquamation looks like the child is burnt. Dermatosis with fisuring is also seen in moderate cases.
- Gastrointestinal tract: Anorexia and diarrhea are common.
Liver is enlarged and palpable due to fatt changes. - Blood: There is presence of moderate degree of anemia.
- Mucosa changes: There is presence of stomatitis, chelosis,smooth tongue and ulceration is present around anus.
- Mental changes: Child becomes miserable, apathetic and has mewing cry.
- Muscles and fats: Presence of wasting of muscles of chest,upper arm, legs and hips. Fat is seen plentiful at these sites.
- Vitamin defiiencies: Vitamin A defiiency is present,folate defiiency is common, defiiency of vitamin K can cause purpura and bleeding.
Management
Diet
- Diet for mild-to-moderate cases: Diet should be easily digestable.
It should be rich in proteins, minerals and vitamins with extra calories.
Milk should be given.
Egg is a good flp with milk and water as a source of fist class protein Plant protein mixtures such as corn,soya, diet milk can be given.
Additional fats should be included. If there is lactose intolerance dal, rice and buttr can be given. - Diet for acute cases: Protein intake should be 3 to 4 g/Kg/day and energy intake of 150 kcal/kg/day. If child is unable to take diet from mouth go for nasogastric intubation.
Care mustbe takento take suffientamount of plant, animal proteins and fats to maintain the weight.
Vitamins and mineral supplementations
- Vitamin A, D, B complex and C are given at therapeutic dosages.
- In vitamin A defiiency 30 mg of Vitamin A should be given for 3 days.
- 0.5–1 g of potassium chloride dissolve in feeds or water should be given daily in divided dosages.
Maintenance of body temperature
- For maintainence of body temperature at night blankets or room heaters are useful.
Skincare
- In cases of dermatoses skin should be kept clean and protected.
In Hospital treatment
- Correction of dehydration, electrolyte disturbances,hypoglycemia, acidosis and hypothermia.
- Parenteral therapy with half of saline and 2.5% glucose before diet therapy.
- In anemia, packed erythrocyte infusion is given.
Question.5. Write causes and management of malnutrition in India.
Answer.
Causes of Malnutrition
1. Due to defective intake offood:
- Loss of appetite due to depression, anxiety, anorexia nervosa, etc.
- Due to persistent vomiting
- Alcohol intake
- Unbalanced therapeutic diet
- Administration of prolong IV flids, parenteral flids in hospitalized patients
2. Maldigestion and disordered absorption:
- In hypochlorhydria or achlorhydria
- In steatorrhea
- Intestinal hurry due to surgical resection
- Due to prolong use of antibiotics
3. Defective utilization:
- In cirrhosis of liver
- In malignancy
- In infections
- In renal failure
- Due to inborn error of metabolism, i.e. hartnup’s disease
- Due to drugs such as antiepileptics
4. Loss ofnutrients from body:
- Proteinuria in nephrotic syndrome leads to hypoproteinemia.
- In diabetes mellitus, glycosuria causes loss of energy and undernutrition
- Due to excessive menstrual blood loss
- Hypokalemia due to severe persistant diarrhea.
5. Due to increased demands:
- In pregnancy, lactation, adolescence, illness and heavy manual work.
- In fever and thyrotoxicosis
- In burn, surgery and trauma, there is increase in catabolism of proteins and vitamin C.
- Malignant cachexia causes loss of weight due to increased demand.
Treatment of Malnutrition
In adults
- For mild starvation, adequate supplementation of nutrients is necessary
- In moderately starved people, extrafeeding is needed
- In severely starved persons, food is given in small amount at frequent intervals. Food should be staple meal, i.e. cereal with some sugar, milk and oils, salt is restricted. Potassium, magnesium and vitamins are adequately given. This is continued till patient feel active.
In children
Diet
- Diet for mild-to-moderate cases: Diet should be easily digestable. It should be rich in proteins, minerals and vitamins with extra calories.
Milk should be given.
Egg is a good flp with milk and water as a source of fist class protein.
Plant protein mixtures such as corn,soya, diet milk can be given.
Additional fats should be included.
If there is lactose intolerance dal, rice and buttr can be given. - Diet for acute cases: Protein intake should be 3 to 4 g/Kg/day and energy intake of 150 Kcal/kg/day.
If child is unable to take diet from mouth go for nasogastric intubation.
Care must be taken to take suffieicnt amount of plant, animal proteins and fats to maintain the weight.
Vitamins and mineral supplementations
- Vitamin A, D, B complex and C are given at therapeutic dosages.
- In vitamin A defiiency 30 mg of vitamin A should be given for 3 days.
- 0.5–1 gm of potassium chloride dissolve in feeds or water should be given daily in divided dosages.
Maintenance of body temperature
For maintenance of body temperature at night blankets or room heaters are useful.
Skincare
- In cases of dermatoses skin should be kept clean and protected.
In hospital treatment
- Correction of dehydration, electrolyte disturbances,hypoglycemia, acidosis and hypothermia.
- Parenteral therapy with half of saline and 2.5% glucose before diet therapy.
- In anemia, packed erythrocyte infusion is given.
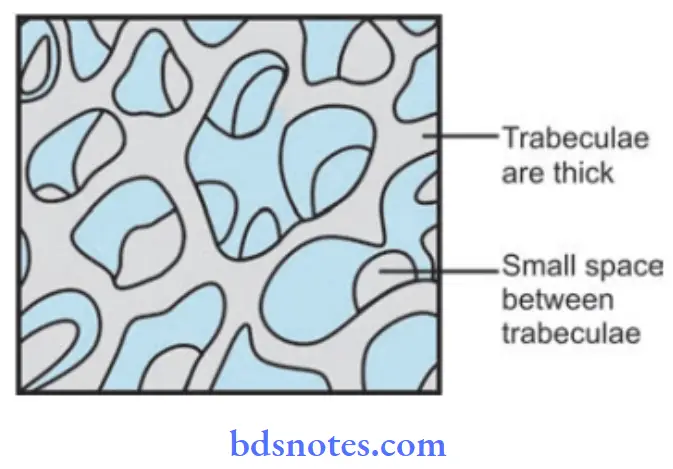
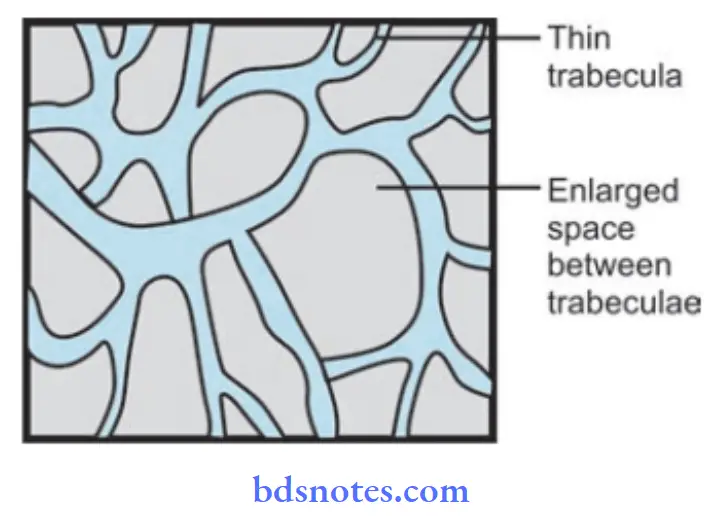
Question.6. Write short note on osteoporosis.
Answer. Osteoporosis is a group of skeletal disorders characterized by reduction in bone mass per unit bone volume, which results in increased risk of fracture, even in absence of noticeable injury.
Causes
- Dietary calcium deficiency: Especially in case of women both premenopausal and postmenopausal .
Apart from increased requirements, degree of calcium absorption from intestine decreases with age. - Excessive alcohol or caffine.
- Genetic inflences.
Other disorders affcting mineral homeostasis:
- Endocrine: Cushing syndrome, hyperthyroidism, type I diabetes mellitus, hypogonadism and acromegaly
- Drugs: Glucocorticoids, thyroxin and diuretics.
Clinical Features
- Bone loss progresses for many years without causing symptoms.
- Shortened heights, bone pain, low back pain, diffilty in gettng up from chair are complaints in women at menopause with osteoporosis.
- Signs of osteoporosis include deformities of skeleton,such as kyphosis (Dowager’s hump) and loss of height especially in vertebral compression fracture.
Diagnosis
- History offracture: Fractures associated with osteoporosis are vertebral fractures, hip fractures and Colle’s fracture of distal radius.
- Radiograph: It shows prominence of vertical trabeculae,generalized loss of contrast between bone and soft tissue.
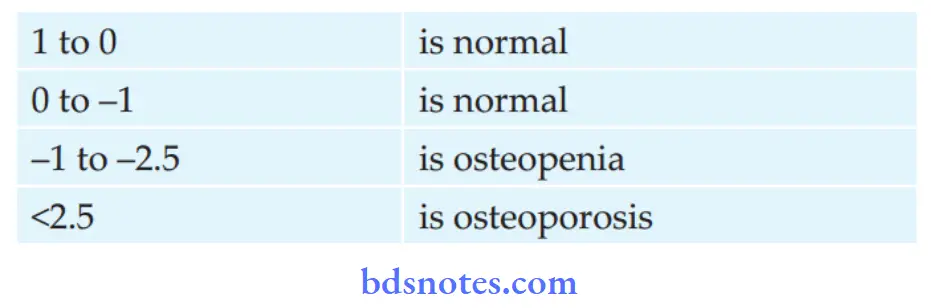
- Bonedensity measurement: Dual-energy Xray absorptiometry is the gold standard. It is performed in spine, both hips and both wrists.
Bone densities are then plottd against normal database to provide standard deviation from normal, i.e.
T score. For postmenopausal women, T score values are:
Management
- Active physical activity helps to maintain strength,flxibility and co-ordination of body improves.
- Calcium 1.5–2 g/day, if calcium malabsorption is there,cholecalciferol 0.25 mg, alfacalcidol 0.5 µg/day.
- Estrogen therapy: 0.635 mg daily estrogen is given in small thin women, early women, etc.
- Biphosphates, i.e. etidronate 400 mg/day for 2 weeks inhibit bone resorption.
- Calcitonin 100 IU SC inhibits bone resorption.
- Sodium floride 40–60 mg/day stimulates osteoblasts and causes bone formation.
Question.7. Mention the complications of diabetes mellitus.
Or
Write short note on complications of diabetes mellitus.
Or
Enumerate the complications of diabetes mellitus.
Or
Write notes on ten complications of diabetes mellitus.
Answer. Diabetes mellitus is collection of disorders that have hyperglycemia as hallmark.
Complications
Acute Or Immediate Complications
- Diabetic ketoacidosis or coma
- Hypoglycemia or hypoglycemic coma
- Nonketotic hyperosmolar diabetic coma
- Lactic acidosis
First two complications occur in Type I diabetes mellitus and other two occur in Type II diabetes mellitus.
Diabetic Ketoacidosis
- It is an exclusive complication of type I diabetes. It can develop in patients with severe insulin defiiency combined with glucagon excess.
Failure to take insulin and exposure to stress are precipitating causes. - As the ketogenesis continues the excess ketone bodies produced cannot be degraded by the muscles and other tissues resulting in ketosis, which manifests as anorexia, nausea, vomiting, deep and fast breathing, mental confusion and coma. However, most of the patients recover.
Hypoglycemia
- It is defied as fall in blood glucose concentration below 3.1 mmol/L.
- It is seen in type I diabetes patients due to excessive administration of insulin, missing a meal or due to stress.
- As the hypoglycemia continues, it can lead to comma,cardiac arrhythmias and is fatal.
- This can lead to worsening of control of diabetes and rebound hyperglycemia.
Nonketotic Hyperosmolar Diabetic Coma
- It is common in type II diabetes mellitus.
- The clinical hallmark is hyperglycemia, hyperosmolality and dehydration without ketoacidosis.
- Precipitating features are infection, myocardial infarction,drugs such as thiazides, steroids, diphenylhydantoin.
- Loss of glucose in urine is so intense that the patient is unable to drink suffient water to maintain urinary flid loss.
- Because of high viscosity of blood, thrombotic and bleeding complications are frequent. Mortality rate is high in this complication.
Lactic Acidosis
- It is seen in type II diabetes mellitus.
- It is caused due to excess lactate production and/or inadequate utilization.
- This can be precipitated by metformin or other systemic disorders such as liver or renal failure, pancreatitis or leukemia.
- Cardiovascular collapse leads to mortality.
Chronic or late-onset complications
These complications are due to changes in small blood vessels i.e.microangiopathy or in large blood vessels, i.e. macroangiopathy.
Microvascular are retinopathy, neuropathy, nephropathy and miscellaneous
Macrovascular are atherosclerosis, hypertension, peripheral vascular disease and diabetic foot ulcer
The chronic complications occur more frequently in Type II diabetes mellitus rather than Type I diabetes mellitus.
Diabetic Retinopathy
- This is the very important cause of blindness in diabetic patients.
- Dilatation of retinal capillaries is earliest sign. Besides these there is also presence of microaneurysms, retinal hemorrhage, neovascularization, hard and soft exudates,vitreous hemorrhage and firosis.
- Frequency, onset and severity of retinopathy vary in diabetic patients.
- Background retinopathy is most common and proliferative retinopathy is less common.
Diabetic Neuropathy
- It can involve any part of nervous system except the brain.
- Neuropathy is an early and common complication which leads to morbidity and disability.
- Poor glycemic control and long duration of diabetes is associated with high incidence of neuropathy.
- Sign and symptoms are of peripheral nervous system.
- Main pathological changes in peripheral nerves are axonal degeneration of myelinated and non-myelinated fiers,
Segmental demyelination, Schwann cell injury.
Diabetic Nephropathy
- This is the most common cause of mortality and morbidity in diabetic patients.
- 40 to 50% of type II diabetes patient develop it and 25% patients with type I diabetes develop end stage renal disease and die of it.
- It is divided into three stages, in fist stage patient is asymptomatic but has high GFR, in next stage there is renal hypertrophy which leads to microalbuminuria.
- In advance stage, patient develop macroproteinuria and passes onto nephrotic syndrome.
- 25% of patients with diabetic nephropathy can go directly at end stage renal disease with hypertension and undergo chronic renal failure.
Miscellaneous
It consists of various infections, gastroparesis, arthropathy.
Atherosclerosis
- In diabetic patient development of athroma is faster as compared to normal individual.
- Hyperlipidemia, decreased HDL levels, increased platelet adhesiveness, obesity and associated hypertension are contributory factors for athrosclerosis.
- Atherosclerosis leads to coronary artery disease, silent myocardial infarction, cerebral stroke and gangrene of toes and feet.
Diabetic Foot Ulcer
- This is the frequent site of complication in diabetes.
- Pathogenic components of diabetic foot are neuropathy,peripheral vascular disease causing ischemia and secondary infection causing ulceration.
Question.8. Outline the management of diabetes mellitus.
Or
Write short note on treatment of diabetes mellitus
Answer. Management
Diet Management
- Restoration of normal blood glucose and optimum levels.
- Maintenance of blood glucose levels as near to physiologic levels to prevent onset or progression of complications.
- Maintenance of normal growth rate in children and adolescents as well as attinment and maintenance of reasonable body weight in adolescents and children.
- Provision of adequate nutrition for pregnant women and fetus during lactation.
- Consistency in timing of meals and snacks to prevent inordinate swings in blood glucose level.
- Motivation to have small frequent meals.
- Determination of meal plan appropriate for individual and based on dietary history to have good compliance.
- Management of weight reduction for obese individuals with NIDDM.
- Improvement in the overall health of patients with diabetes through optimal nutrition.
Total Calories
Requirements are determined by the patients activity:
- Overweight NIDDM should be encouraged to establish their weight within a desirable range. A reduction of approximately 500 kcal/ day can result in loss of 1–2 kg/month.
- Carbohydrates: Carbohydrates should be taken in form of starch and complex sugars. 100–300 g of carbohydrates should be spreaded over 3 meals, i.e. 60g each and 3 snacks,i.e. 30 geachwithhalflitre ofmilk. Unrefied carbohydrates should be substituted by refied carbohydrates to the extent possible.
- Proteins: Recommended dietary allowance of 0.85 g/kg body weight for adult is an appropriate guide.
- Fat: Fat intake should be 50–150 g daily divided between the meals. Replacement of saturated with polyunsaturated fat is desirable to reduce cardiovascular risk. Cholesterol intake should be < 300 mg/day.
- Fiber: Increased consumption of dietary fier especially soluble fier are associated with lower levels of blood glucose and serum lipids. The water insoluble fiers such as cellulose, lignin and most hemicelluloses found in whole grain breads, cereals and wheat bran affct gastrointestinal transit time and fecal bulk with litte impact on plasma glucose. However highly viscous water soluble fiers such
as pectins, gums and storage polysaccharide found in fruits, legumes, lentils roots, tubers, oat and oat bran, when eaten in purifid form, reduce serum levels of glucose and insulin. Ideal recommended amount of fier in patient’s diet is 35–40 g/day. - Alternative sweeteners: Both nutritive and nonnutritive sweeteners are acceptable in diabetes management.
- Sodium: It should be restricted to 1000 mg/1000 kcal, not to exceed 3000 mg/day to minimize symptoms of hypertension.
- Alcohol: It should be taken in moderation and may need to be restricted entirely by person with diabetes and insulin—induced hypoglycemia, neuropathy, poor control of glucose and lipids, or obesity.
- Vitamins, minerals and antioxidants: intake should be encouraged.
Forbidden foods: Sugar, jam, jellies, honey, jaggery, tinned fruits and juices, sweets, chocolate, ice creams, pastries, glucose drinks, foods made with sugar, pudding, sauces.
Foods allowed in moderation: Bread of all kinds and chapatts made from wheat or millets, plain biscuits, all fresh fruits, baked beans, breakfast cereals.
Free foods: All meat, fih, eggs (not fried), clear soup or meat extracts; tea or coffe; vegetables such as cabbage, cauliflwer, spinach, pumpkin, brinjal, lady’s figer, turnip, French beans,cucumber, lettce, tomato, spring onions, radish, asparagus.
Spices, salt, pepper and mustard; buttr and margarine. Sugar substitutes for sweetening.
Oral Hypoglycemics
These drugs are used in patients of Type II diabetes mellitus(NIDDM) who do not respond to dietary management and who would otherwise require treatment with insulin in later situation, so they are also used as adjuvant drugs to insulin in overweight diabetes patients.
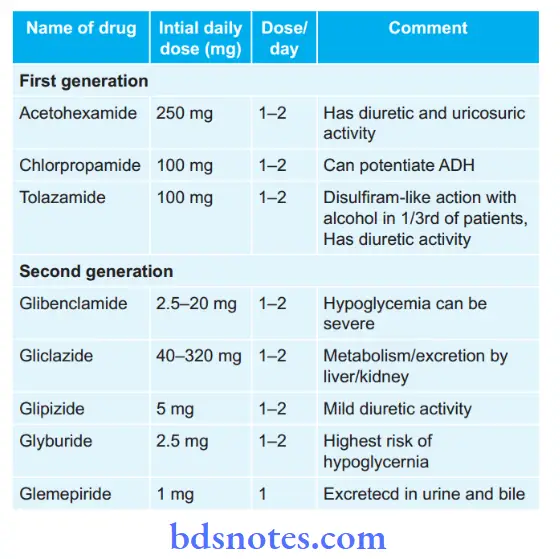
Insulin secretagogues i.e. drugs increasing secretion of insulin
- Sulfonyl ureas
Meglitinides:
- Repaglinide, i.e. 0.5–4 mg three times a day
- Netaglinide, i.e. 60–120 mg three times a day 15 to 30 min before each meal
- Voglibose, i.e. 0.2–0.3 mg, 15–30 min before each meal.
Insulin sensitizers, i.e.drugs sensitizing action of insulin and overcome insulin resistance
- Biguanides, i.e. metformin should be given 1.5–2.5 g/day in three divided doses after meals.
- Thiozolidinediones, i.e.rosiglitazone should be given 2–8 mg or pioglitazone 15–45 mg in a single or two divided doses.
They can be combined with sulfonyl ureas or metformin
- Alpha glucosidase inhibitors, i.e. Acarbose 25 to 100 mg TDS or Voglibose 0.2–5 mg TDS taken orally in three main meals.
- It can be given in combination with metformin 500 mg for increased effiency.
- DPP-4 inhibitor: Vildagliptin 50–100 mg daily in two dived doses with meals ot saxagliptin 2.5 to 5mg OD.
- Pramlinide: Initial dose is 15 μg before each meals in Type I diabetes mellitus and 60 μg in Type II diabetes mellitus.
Insulin
Following are the indications for insulin therapy:
- In type I diabetes mellitus
- In gestational diabetes
- Hyperglycaemia despite maximum doses of oral agents
- Decompensation due to intercurrent events such as infection, acute injury or stress
- Development of severe hyperglycemia with ketosis
- Perioperative in patients undergoing surgery
- Kidney or hepatic disease
Various Insulin Preparations
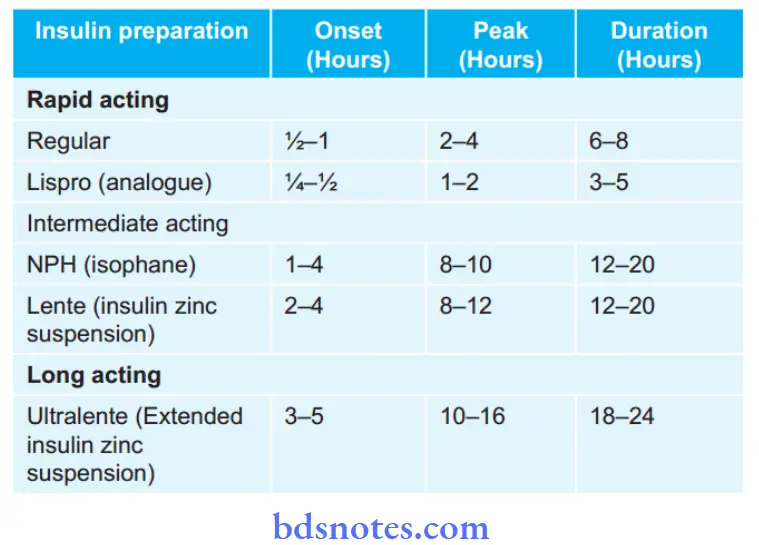
Treatment Strategies with Insulin
- Single dose regimen: Daily injection of intermediate act ing insulin given before breakfast.
The starting dose 0.3–0.4 U/Kg/ day; increased gradually to obtain glucose values in acceptable range.
Regular insulin can be added to decrease the glucose level that follows breakfast. - Twice daily regimen: Combination of regular and intermediate acting insulin BD, i.e. before breakfast and before dinner (“Split mix” regimen).
- Multiple daily injections: For achievement of more tight control of blood glucose which requires administration of at least 3 injections per day.
These can be given with use of mixture of intermediate and shortacting insulins (premixed insulin) in the morning before breakfast, with regular insulin before supper and intermediateacting at bedtime; or again a combination of regular and intermediateacting before dinner.
Divide the total daily into 2 equal doses following 1:1 transfer from basal insulin.
Give half before breakfast and other half before dinner.
The largest meal will require larger proportion of insulin.
Reduce total dose by 20%, if patient experiences recurrent hypoglycemia. - Insulin concentrations: The insulins are available in many concentrations. In India the commonly used is 40 U/mL
- Insulin purity: The impurities which may be contained are proinsulin, insulin intermediates and contaminating proteins from islet tissue or exocrine pancreas such as glucagon, somatostatin and pancreatic polypeptides.
Standard insulins currently have only 10–20 PPM of proinsulin and purifid monocomponent insulins less than 1 PPM.
Best sites for the insulin injection are subcutaneous fat on abdomen, buttck, anterior thigh and dorsal area of arm.
Exercise
- Exercise must be adjusted to patient’s preference and existing medical condition.
- Aerobic exercise is preferred, i.e. swimming, cycling,walking, running. etc
- Addition of moderate resistance should be considered.
- Duration should be 20–45 minutes per session.
- Frequency is 3–4 sessions per week is required to observe benefiial metabolic effcts. 4–5 sessions per week for weight reduction.
- ADA recommends 150 min/week of moderate aerobic physical activity with no gaps longer than 2 days.
- Program of exercise should be:
- Stretching for 5–10 min
- Warm up for 5–10 min
- Exercise for 20–45 min
- Warm down for 10 min at 30% offull exercise intensity.
Question.9. Write short note on insulin.
Answer. Insulin is required for proper control of diabetes and to keep blood sugar within limits.
Following are the indications for insulin therapy:
- In type I diabetes mellitus
- In gestational diabetes
- Hyperglycemia despite maximum doses of oral agents
- Decompensation due to intercurrent events such as infection, acute injury or stress
- Development of severe hyperglycemia with ketosis
- Perioperative in patients undergoing surgery
- Kidney or hepatic disease
Various insulin preparations
Treatment Strategies with Insulin
- Single dose regimen: Daily injection of intermediate acting
insulin given before breakfast.
The starting dose 0.3–0.4 U/Kg/ day; increased gradually to obtain glucose values in acceptable range.
Regular insulin can be added to decrease the glucose level that follows breakfast. - Twice daily regimen: Combination of regular and intermediate acting insulin BD, i.e. before breakfast and before dinner (“Split mix” regimen).
- Multiple daily injections: For achievement of more tight control of blood glucose which requires administration of at least 3 injections per day.
These can be given with use of mixture of intermediate and short acting insulins (premixed insulin) in the morning before breakfast, with regular insulin before supper and intermediateacting at bedtime; or again a combination of regular and intermediate acting before dinner.
Divide the total daily into 2 equal doses following 1:1 transfer from basal insulin.
Give half before breakfast and other half before dinner.
The largest meal will require larger proportion of insulin.
Reduce total dose by 20%, if patient experiences recurrent hypoglycemia. - Insulin concentrations: The insulins are available in many concentrations. In India, the commonly used is 40 U/mL
- Insulin purity: The impurities which may be contained are proinsulin, insulin intermediates and contaminating proteins from islet tissue or exocrine pancreas such as glucagon, somatostatin and pancreatic polypeptides.
- Standard insulins currently have only 10–20 PPM of proinsulin and purifid monocomponent insulins less than 1 PPM.
Site of Insulin Injection
Best sites for the insulin injection are subcutaneous fat on abdomen, buttck, anterior thigh and dorsal area of arm.
Insulin Delivery System
- Insulin pens are used in both Type I and Type II diabetes mellitus.
- Continuous insulin infusion systems are used in Type II diabetes mellitus.
Complications
Following are the complications of insulin therapy:
- Hypoglycemia: It is the most frequent and most serious reaction. Hypoglycemia can occur in any diabetic following inadvertent injection of large doses, by missing a meal or by performing various exercises
- Local reaction: Swelling, erythema and stinging sometimes occurs especially in beginning. *Lipodystrophy occurs at injection site after long usage.
- Insulin allergy: This is infrequent and is due to contaminating proteins. Urticaria, angiedema and anaphylaxis are manifestations.
- Edema: Some patients develop shortlived dependent edema when insulin therapy is started.
- Weight gain: Patients on longterm insulin therapy gain weight.
Question.10. Outline management of diabetic comma.
Answer. Diabetic ketoacidosis or diabetic comma is the exaggeration or deranged energy metabolism due to defiiency of insulin which results in accumulation of acid metabolites and ketone bodies.
Management
Following is the management of diabetic comma
Admission of patient
- Diagnosis is confirmed by examination of blood glucose and ketone measurements.
- Initial assessment of dehydration, hyperosmolality, serum potassium, acidosis and kidney function is done.
- Fluid loss is measured by subtracting admission weight by last known stable weight.
- Patient should be evaluated for sepsis.
Management during hour 1
- If patient is hypovolemic and hypotensive fluid administration is done, i.e. normal saline is administered and if necessary colloids should be given.
Rate of administration is necessary to restore circulatory function.
As blood pressure become normal and urine output becomes adequate rate of administration of normal saline is 1000 mL/hour. - Continuous I.V. infusion of regular insulin 5–10 units/hour is given.
- I.V, infusion of potassium is done at 10–40 mmol/ hour during initiation of insulin therapy.
- Sodium bicarbonate IV is given in cases with acidosis.
Dose is 50–100 mmol/L sodium bicarbonate in 0.45% saline for 30–60 minutes. Additional potassium should also be given with bicarbonate therapy.
Management during hour 2
- Normal saline should be continued at 500 mL/ hour.
Plasma osmolality should be greater than 285 mmol/ L during fist 12 hours. If serum sodium is greater than 150 mmol/L switch to 0.45% saline. - Blood glucose should be checked and insulin is adjusted to 5 mmol/litre/hour. Blood glucose should not fall below 11.1–14.0 mmol/L. Anion gap is decreasing and blood pH is increasing.
- Serum potassium should be maintained at 4–5 mmol/litre by addition of potassium to IV flids.
Management during hours 3 to 4
- Management should be continued as given in second hour.
- Cognitive and neurological symptoms should be observed for 12 hours.
Management during hours 5 to 8
- Normal saline should be continued at 250 mL/ hour.
- As blood glucose reaches 11.1–14 mmol/ L, change IV flid to 500 mL/hour normal saline with 5% glucose.
Insulin should be continued at maintenance dose until ketoacidosis is cleared. - Potassium should be continued at 10–40 mmol/ hour,since ketoacidosis is cleared.
- Phosphate replacement is done at 6 hours, if serum phosphate is < 2 mg/dL
Management during hours 8 to 24
- IV repletion is continued with 0.45% saline with or without 2.5% or 5% glucose as needed.
- As diabetic comma is subsided, patient should be switched to subcutaneous insulin and stop IV and IM insulin.
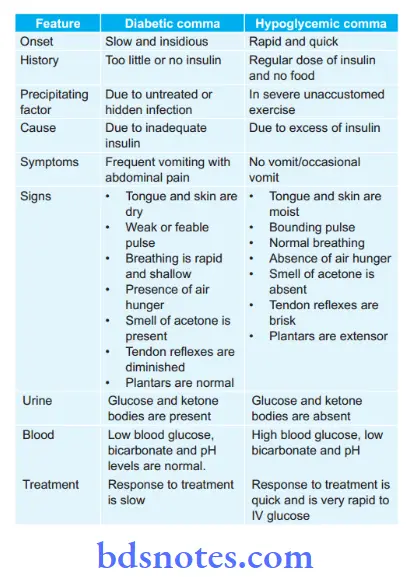
Question.11. Differentiate between diabetic comma and hypoglycemic comma.
Answer
Question.12. Write short note on hypoglycemia.
Answer.
Hypoglycemia is defined as fall in blood glucose concentration below 2.5 mmol/L.
It can be present as asymptomatic, mild, severe or may be present as coma.
Etiology
- Postprandial
- Alcohol ingestion
- Starvation, prolonged exercise, infection
- Nonislet cell tumors, e.g. hepatoma, adrenal carcinoma,mesothelioma, etc
- Iatrogenic, i.e. drug induced due to oral hypoglycemic,salicylism, due to propranolol.
Clinical Features
- Cardiovascular system: Palpitation, tachycardia, anxiety,cardiac arrhythmias
- Central nervous system: Tremors, confusion, headache,tiredness, difficulty in concentration, in cordination,slurred speech, drowsiness, convulsion and coma.
- Gastrointestinal tract: Nausea and vomiting
- Skin: Sweating and hypothermia
Diagnosis
1. In hypoglycemia state:
- Suggestive history
- Dramatic response to IV glucose during attck
- Low plasma level glucose during attck
- C-peptide concentration > 200pmL/L
2. Ofcause:
- Clinical: Exclude hypopituitarism, Addison’s disease,liver cirrhosis or failure, sarcoma, alcohol ingestion after fasting, self administration of insulin or sulphonylurea.
- Investigations for insulinomas:
- Overnight fasting plasma glucose and insulin measurements will demonstrate spontaneous hvpoglycemia and raised plasma insulin
- Low plasma Cpeptide with high plasma insulin.
- High fasting plasma proinsulin.
Management
1. In acute attck:
- Administration of rapidly absorbable carbohydrate
- In mild reaction, orange juice (100 mL) or corn syrup or candy taken orally suffient.
- In unconscious or uncooperative patients 50 mL of 50% glucose IV if vein not available glucagon 1 mg SC or IM will cause suffient increase in blood sugar to allow the patient to become rational and cooperative.
- When recovery is slow, e.g. after overdose of insulin or sulphonylurea therapy, constant infusion of 10–20% dextrose is given to maintain the blood sugar.
2. Conservative treatment and prevention ofacute attcks
- Diet: Carbohydrate not more than 150 gms in slowly absorbable form like cereals, bread, fruits and vegetables.
Liberal protein because glucose derived from it is liberated slowly; fat to make up calories.
In hepatogenic type bedtime meal to prevent early morning hypoglycemia. - Restriction of physical exercise.
3. Surgical measures:
- Removal of islet cell tumors, or partial resection of pancreas
- In fulminating cases where convulsions are not controlled by glucose.
- In severe, chronic cases not controlled by diet.
- Patients with marked, neuropsychiatric syrnptoms.
4. Drugs
- Glucagon: The efficy depends on size of hepatic glycogen stores. The drug has litte effct on blood glucose in patients who have been fasting or are hypoglycemic for long periods. IM injection of 1mL of glucagon is given, if hypoglycemia is insulin induced.
- Diazoxide and Octreotide may be used to control symptoms while the patient is awaiting surgery or when the patient is not a candidate for surgery.
Question.13.Write short note on vitamin B12 defiiency.
Answer. It is also known as Wonder vitamin and cyanocobalamin.
Causes of Vitamin B12 Defiiency
- Due to inadequate dietary intake
- Due to malabsorption
- Intrinsic factor deficiency in pernicious anemia,gastrectomy, congenital lack of intrinsic factor
- Intestinal causes, i.e. tropical sprue, Ileal resection,
Crohn’s disease - Removal of vitamin B12 from intestines i.e. In tapeworm infestation and due to bacterial proliferation in intestinal blind loop syndrome
- Drugs such as neomycin, PAS and colchicine.
Clinical Features
- Blood: Megaloblastic anemia
- General features: Pallor, anorexia, diarrhea
- Oral manifestations: Glossitis, Glossodynia, Angular stomatitis, xerostomia
- Nervous system manifestations:
- Subjective sensory disturbances: Paraesthesia, Tingling and numbness in toes, tips of fingers, rarely simultaneously in both upper and lower extremities.
Sometimes burning or stabbing pains or even lightning pains like tabes. - Objective sensory loss: Sense ofvibration, posture and passive movement affcted fist in lower, later in upper limbs. Glove and stocking type of superfiial sensory loss. Tenderness of calf muscles.
- Motor symptoms: Pyramidal weakness and ataxia develop at variable interval after onset of sensory disturbances.
- Reflxes: Ankle jerks lost, knee jerks may be absent. Both exaggerated, if lateral column lesion predominates.
Plantars extensor. - Sphincter disturbances: First diffilt or precipitate micturition, later retention of urine or incontinence.
Impotence is early. - Mental changes: Mild dementia, impaired memory.
Confusional psychosis or irritability or depression. - Bilateral primary optic atrophy in 5%.
Diagnosis
- Presence of low hemoglobin
- Macrocytosis,
- High MCHC
- Megaloblastic bone marrow
- Gastric achlorhyclria
- Serum vitamin B12 less than 100 pg/mL
- Elevated homocysteine
Treatment
- Vitamin B12 defiiency especially in those with megaloblastic anemia is treated by giving hydroxycobalamin 1000 microgram IM twice a week for fist week.
This is followed by 1000 µg weekly for 6 weeks. - Replacement therapy is given throughout the life in dosage of hydroxycobalamin 1000 µg IM for every three months.
- For patients sensitive to injections, Oral B12 in large daily doses is given, i.e. 100 µg or more.
Question.14. Write short note on scurvy.
Answer. Deficiency of vitamin C leads to scurvy.
Due to vitamin C defiiency, there is defective collagen formation.
Etiology
- In artifiially fed infants
- It is precipitated by febrile disease, infections and diarrhea
Clinical Features
- Onset of the disease is usually gradual, there is fretfulness and increasing pallor, or tenderness of legs which causes child to cry whenever touched, anorexia and loss of weight. First symptom is inability of the child to use his legs.
- Symptoms due to hemorrhages:
- Under periosteum of long bones: “Pithed frog posture”with thighs flxed and abducted and knees flxed,sometimes diffse swelling above or below the knee;in severe cases, infitration of muscles with blood causing edematous limbs, i.e woody leg; hemorrhage between diaphysis and epiphysis causes separation of epiphysis from shaft.
- Perifollicular hemorrhage.
- In orbit, there is proptosis with swelling of eyelids
- Hematuria: May be an early symptom and is only microscopic.
- Scorbutic beading of the ribs
- Presence of anemia
- Keratosis of hair follicles with ‘corkscrew’ hair
- Failure of wound healing
Oral Manifestations
- It chiefl affcts the gingival and periodontal region.
- The interdental and marginal gingiva becomes bright red,swollen, smooth, shiny producing appearance known as scurvy bud. In fully developed scurvy, gingiva becomes boggy, ulcerated and bleeds easily
- There is a typical fetid breath of a patient with fusospirochetal stomatitis.
- Color of the gingiva changes to violaceous red.
- In severe cases, hemorrhage and swelling of periodontal
ligament membrane occur followed by loss of bone and loosening of teeth which are exfoliated.
Diagnosis
- Low ascorbic acid level in platelets and plasma
- Anemia is mildtomoderate but may be severe.
- Xray shows characteristic features such as
- Pencilled cortex
- White lines of Frankel
- Zone of Trummerfeld
- Halo sign of Wimberger
- Subperiosteal hematoma
- Joint effsion
- Scorbutic rosary
Management
- About 3 to 4 ounces of fresh orange juice or tomato juice daily.
- Ascorbic acid 100 mg or more orally or parenterally twice or thrice daily for 10 to 15 days.
Question.15. Write short note on balanced diet.
Or
Write notes on balanced diet.
Or
Write about balanced diet.
Answer. A diet adequate in energy providing substances, i.e.carbohydrates and fats, tissue building compounds,i.e. proteins, inorganic chemical, i.e. water and mineral salts, agents that regulate or catalyze metabolic process,i.e. vitamins and substances for certain physiological processes such as bulk for promoting peristaltic movement of digestive tract known as balanced diet.
- For proper growth, maintenance and development of our body an ideal combination of essential nutrient, vitamins and minerals should be aimed.
- An average Indian diet is poor in quality as well as quantity in meeting the daily needs.
- A balanced diet should contain 30 cal/kg optimum body weight.
- Balanced diet should contain 60–70% carbohydrates of total calories, 12–18% protein of total calories,20–25% fats of total calories.
- Diet should contain as much as of fresh fruits,vegetables which provide nutrients.
- Fiber is an important part of the food.
- Milk is an ideal food and contains or proximate the principles of balanced diet.
- A balanced diet not only looks after the well-being of person but may have role to play in prevention of certain diseases.
- So while planning a balanced diet, care should be taken that all essential ingredient in diet are adequately incorporated with fresh fruits, vegetables and fier diet.
- Food should be palatable, properly cooked and well balanced providing a balance between food intake and energy output.
Question16. Write note on pellagra.
Answer. It is the clinical condition produced due to the defiiency of nicotinic acid or niacin.
Etiology
- Inadequate intake or absorption of niacin.
- Restricted or limited diet in which single serial grain, i.e.corn is consumed without consumption of wheat, eggs, beef and another niacin rich food.
In chronic alcoholism.
Clinical Features
- Pellagra is triad of dermatitis, diarrhea and dementia.
- Dermatitis is bilaterally symmetrical and occur in parts exposed to sunlight. In acute cases skin lesions may produce vesiculation, cracking, exudation, crusting with ulceration and desquamation. In chronic cases, dermatitis occurs.
- Gastrointestinal manifestations: Presence of anorexia,nausea, dysphagia. Glossitis precede the skin lesions.
Diarrhoea is also present. - Mental features consists of apathy, insomnia, fatigue followed by encephalopathy characterized by confusion,disorientation, loss of memory and hallucination.
- Other features: Loss of appetite, irritability and burning sensation in diffrent areas of body.
Oral Manifestations
- Oral mucosa is firy red and is painful.
- Glossitis is present. Tongue is red, swollen and beefy. In early stage, only the tip and margins of tongue are swollen and red but in advance cases, tongue looses the papillae and reddening is intense.
- Presence of angular stomatitis
- Superimposed acute necrotizing ulcerative gingivitis is present involving gingiva, tongue and mucosa.
Diagnosis
- NAD and NADP levels are low in RBCs in patients with pellagra.
- Plasma tryptophan is low.
Treatment
- Initially by injection nicotinamide 50–100 mg IM daily for a week. Maintenance dose of 50 mg orally per day.
Question.17. Write in brief clinical features and management of diabetic ketoacidosis.
Answer. Diabetic ketoacidosis or diabetic comma is the exaggeration or deranged energy metabolism due to defiiency of insulin which results in accumulation of acid metabolites and ketone bodies.
Clinical Features
Symptoms
- Polyuria
- Thirst
- Weight loss
- Weakness
- Nausea
- Vomiting
- Leg cramps
- Blurred vision
- Abdominal pain.
signs
- Dehydration
- Hypotension
- Tachycardia
- Confusion
- Drowsiness
- Comma.
Management
Following is the management of diabetic comma
Admission of patient
- Diagnosis is confirmed by examination of blood glucose and ketone measurements.
- Initial assessment of dehydration, hyperosmolality, serum potassium, acidosis and kidney function is done.
- Fluid loss is measured by subtracting admission weight by last known stable weight.
- Patient should be evaluated for sepsis.
Management during hour 1
- If patient is hypovolemic and hypotensive fluid administration is done, i.e. normal saline is administered and if necessary colloids should be given.
Rate of administration is necessary to restore circulatory function.
As blood pressure become normal and urine output becomes adequate rate of administration of normal saline is 1000 mL/hour. - Continuous I.V. infusion of regular insulin 5–10 units/hour is given.
- I.V, infusion of potassium is done at 10–40 mmol/ hour during initiation of insulin therapy.
- Sodium bicarbonate IV is given in cases with acidosis.
Dose is 50–100 mmol/L sodium bicarbonate in 0.45% saline for 30–60 minutes. Additional potassium should also be given with bicarbonate therapy.
Management during hour 2
- Normal saline should be continued at 500 mL/ hour.
Plasma osmolality should be greater than 285 mmol/ L during fist 12 hours. If serum sodium is greater than 150 mmol/L switch to 0.45% saline. - Blood glucose should be checked and insulin is adjusted to 5 mmol/litre/hour. Blood glucose should not fall below 11.1–14.0 mmol/L. Anion gap is decreasing and blood pH is increasing.
- Serum potassium should be maintained at 4–5 mmol/litre by addition of potassium to IV flids.
Management during hours 3 to 4
- Management should be continued as given in second hour.
- Cognitive and neurological symptoms should be observed for 12 hours.
Management during hours 5 to 8
- Normal saline should be continued at 250 mL/ hour.
- As blood glucose reaches 11.1–14 mmol/ L, change IV flid to 500 mL/hour normal saline with 5% glucose.
Insulin should be continued at maintenance dose until ketoacidosis is cleared. - Potassium should be continued at 10–40 mmol/ hour,since ketoacidosis is cleared.
- Phosphate replacement is done at 6 hours, if serum phosphate is < 2 mg/dL
Management during hours 8 to 24
- IV repletion is continued with 0.45% saline with or without 2.5% or 5% glucose as needed.
- As diabetic comma is subsided, patient should be switched to subcutaneous insulin and stop IV and IM insulin.
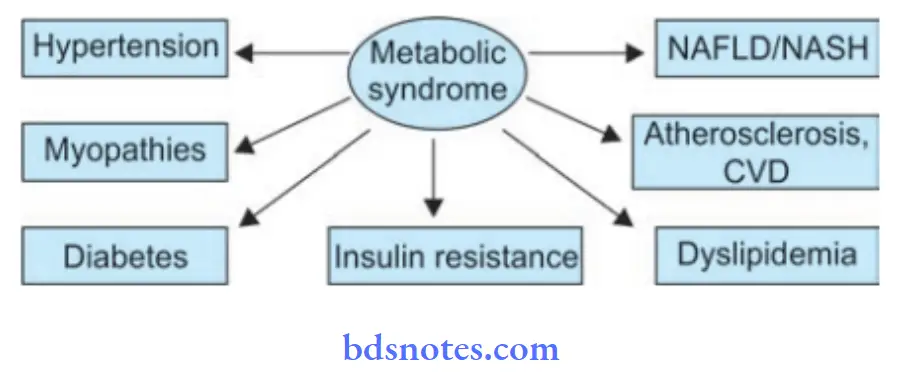
Question.18. Write short note on metabolic syndrome X /dysmetabolic syndrome.
Answer. Metabolic syndrome is a combination of medical disorders that increase one’s risk for cardiovascular disease and diabetes.
It affcts a large number of people in a clustered fashion.
It is known under various other names, such as (metabolic) syndrome X, insulin resistance syndrome,Reaven’s syndrome or CHAOS.
Clinical Features
Symptoms
- Fasting hyperglycemia
- High blood pressure
- Central obesity (also known as visceral, male pattrn or appleshaped adiposity), overweight with fat deposits mainly around the waist.
- Weakness, fatigue and restlessness.
Signs
- Fatt liver (especially in concurrent obesity),
- Non-alcoholic fatt liver disease
- Polycystic ovarian syndrome
- Hemochromatosis (iron overload);
- Acanthosis nigricans (a skin condition featuring dark patches).
Treatment
The main treatment is lifestyle, i.e. caloric restriction and physical activity.
However, drug treatment may occasionally be necessary.
Generally, the individual diseases that comprise the metabolic syndrome are treated separately, e.g. diuretics and ACE inhibitors for hypertension.
Cholesterol drugs may be used to lower LDL cholesterol and triglyceride levels, if they are elevated.
Question.19. Write short note on diabetic ketoacidosis.
Answer. Diabetic ketoacidosis a state of acidemia induced by excess production of ketoacids.
Dehydration and hyperglycemia are the rule and lactic acidosis may also be present.
Pathophysiology
Diabetic ketoacidosis is caused by severe insulin defiiency and is accentuated by excessive glucagon secretion.
This leads to major clinical and laboratory abnormalities seen in diabetic ketoacidosis, which includes excess mobilization of free acids from adipose tissue, increased glucose production from the liver, impaired glucose uptake and utilization by muscle.
The two major effcts of uncontrolled diabetes are:
- Increased glucose production which causes hyperglycemia,osmotic diuresis, electrolyte depletion and dehydration
- Increased ketogenesis, resulting in metabolic acidosis
Precipitating causes
- Acute infection viral or bacterial single most common cause.
- Omission of insulin or inadequate dosage.
- Vomiting.
- Diarrhea.
- Prolonged neglect of diabetes.
- Indiscretions in diet.
- Surgical operations.
- Trauma.
- Myocardial infarction.
- Pregnancy.
- Thyrotoxicosis.
- Resistance to insulin.
- Unnoticed interruption of insulin delivery in diabetics treated with continuous subcutaneous insulin infusion.
Clinical Features
Symptoms
- Polyuria
- Thirst
- Weight loss
- Weakness
- Nausea
- Vomiting
- Leg cramps
- Blurred vision
- Abdominal pain.
signs
- Dehydration
- Hypotension
- Tachycardia
- Confusion
- Drowsiness
- Comma.
Diagnosis
The cardinal features are:
- Acidosis, i.e. arterial pH ≤ 7.3
- Plasma anion gap ≥ 16 mmol/L
- Serum ketone is positive
- Serum bicarbonate ≥ 15 mmol/L
- Hyperglycemia, i.e. Plasma glucose ≥ 11.1 mmol/L
Management
Following is the management of diabetic ketoacidosis
1. Admission of patient
- Diagnosis is confimed by examination of blood glucose and ketone measurements.
- Initial assessment of dehydration, hyperosmolality, serum potassium, acidosis and kidney function is done.
- Fluid loss is measured by subtracting admission weight by last known stable weight.
- Patient should be evaluated for sepsis.
2. Management during hour 1
- If patient is hypovolemic and hypotensive flid administration is done, i.e. normal saline is administered and if necessary colloids should be given.
Rate of administration is necessary to restore circulatory function.
As blood pressure become normal and urine output becomes
adequate rate of administration of normal saline is 1000 mL/hour. - Continuous IV infusion of regular insulin 5–10 units/hour is given.
- IV infusion of potassium is done at 10–40 mmol/hour during initiation of insulin therapy.
- Sodium bicarbonate IV is given in cases with acidosis. Dose is 50–100 mmol/L sodium bicarbonate in 0.45% saline for 30–60 minutes.
Additional potassium should also be given with bicarbonate therapy.
3. Management during hour 2
- Normal saline should be continued at 500 mL/hour.
Plasma osmolality should be greater than 285 mosmol / L during fist 12 hours.
If serum sodium is greater than 150 mmol/L switch to 0.45% saline. - Blood glucose should be checked and insulin is adjusted to 5 mmol/L/hour.
Blood glucose should not fall below 11.1–14.0 mmol/L. Anion
gap is decreasing and blood pH is increasing. - Serum potassium should be maintained at 4–5 mmol/L by addition of potassium to IV flids.
4. Management during hours 3 to 4
- Management should be continued as given in second hour.
- Cognitive and neurological symptoms should be observed for 12 hours.
5. Management during hours 5 to 8
- Normal saline should be continued at 250 mL/hour. As blood glucose reaches 11.1–14 mmol/
lt, change IV flid to 500 mL/hour normal saline with 5% glucose. - Insulin should be continued at maintenance dose until ketoacidosis is cleared.
- Potassium should be continued at 10–40 mmol/hour since ketoacidosis is cleared.
- Phosphate replacement is done at 6 hours if serum phosphate is < 2 mg/dL
6. Management during hours 8 to 24
- IV repletion is continued with 0.45% saline with or without 2.5% or 5% glucose as needed.
- As ketoacidosis is subsided patient should be switched to subcutaneous insulin and stop IV and IM insulin.
Question.20. Write short note on vitamin D.
Answer. Vitamin D are a group of sterol and commonly found in animals mainly there are two types of active form:
D2 – Ergosterol/Ergocalciferol
D3 – 7- dehydrocholesterol.
Source
Fish liver oil, egg yolk, buttr milk, the cheapest source is sun light which forms vitamin D3 from its precursor present in the skin.
Physiological Functions
- Vitamin D increases the absorption of Ca and P.
- It increases the calcifiation of bones in children and adult.
- So, it is essential for the development of bones and normal growth of body.
- It increases the excretion of phosphate by kidney and helps in lowering of serum phosphate concentration.
- It increase the citrate levels of blood, bone, kidney and heart tissues.
- It decreases the pH in the lower intestinal tract which helps in increasing the absorption of calcium and phosphate.
Daily Requirements
- Infants and children:400 IU
- Adult: 200 IU
- Pregnant and lactating women:400 IU
Defiiency of Vitamin D
- Rickets: Due to defect in bone growth and calcifiation of long bones in children.
- Osteomalacia: Due to defective calcifiation of steroid tissue in adult.
Causes of Defiiency of Vitamin D
- Dietary insuffiency or insuffient exposure to sunlight.
- Gastrointestinal disorder.
- Chronic obstructive jaundice.
- Prolonged treatment with anticonvulsant drugs.
Toxicity or excess of vitamin D
There is presence of anorexia, lassitude, vomiting, diarrhea,profuse sweating, polydipsia, polyuria and headache.
Hypercalcemia causes calcium deposition in tissues and kidneys which leads to renal failure.
Question.21. Write short note on vitamin C.
Answer. Vitamin C was named ascorbic acid owing to its antiascorbic properties.
Ascorbic acid is a white crystalline watersoluble substance with sour taste.
It is easily destroyed by cooking.
Absorption And Storage
- Ascorbic acid is easily absorbed from the small intestine,peritoneum and subcutaneous tissues.
- It is not stored in any particular organ and is spread throughout the body.
Sources
Amla, citrus fruits, tomatoes, guava, green peppers.
Physiological Functions
- It is involved in oxidation reaction of cell.
- It is required for the metabolism of amino acid, e.g. tyrosine and tryptophan.
- It is also involved in conversion of folic acid into its active coenzyme.
- It is required for iron absorption and also for the formation of collagen fiers and mucopolysaccharides of connective tissue.
Daily Requirements
- Infants: 35 mg
- Children: 40 mg
- Adults: 45 mg
- Pregnant and lactating women 80 mg.
Defiiency Manifestations
- Severe ascorbic acid defiiency produces—Scurvy.
Deficiency of vitamin C leads to scurvy.
Due to vitamin C defiiency, there is defective collagen formation.
Etiology
- In artifiially fed infants
- It is precipitated by febrile disease, infections and diarrhea
Clinical Features
- Onset of the disease is usually gradual, there is fretfulness and increasing pallor, or tenderness of legs which causes child to cry whenever touched, anorexia and loss of weight. First symptom is inability of the child to use his legs.
- Symptoms due to hemorrhages:
- Under periosteum of long bones: “Pithed frog posture”with thighs flxed and abducted and knees flxed,sometimes diffse swelling above or below the knee;in severe cases, infitration of muscles with blood causing edematous limbs, i.e woody leg; hemorrhage between diaphysis and epiphysis causes separation of epiphysis from shaft.
- Perifollicular hemorrhage.
- In orbit, there is proptosis with swelling of eyelids
- Hematuria: May be an early symptom and is only microscopic.
- Scorbutic beading of the ribs
- Presence of anemia
- Keratosis of hair follicles with ‘corkscrew’ hair
- Failure of wound healing
Oral Manifestations
- It chiefl affcts the gingival and periodontal region.
- The interdental and marginal gingiva becomes bright red,swollen, smooth, shiny producing appearance known as scurvy bud. In fully developed scurvy, gingiva becomes boggy, ulcerated and bleeds easily
- There is a typical fetid breath of a patient with fusospirochetal stomatitis.
- Color of the gingiva changes to violaceous red.
- In severe cases, hemorrhage and swelling of periodontal
ligament membrane occur followed by loss of bone and loosening of teeth which are exfoliated.
Diagnosis
- Low ascorbic acid level in platelets and plasma
- Anemia is mildtomoderate but may be severe.
- Xray shows characteristic features such as
- Pencilled cortex
- White lines of Frankel
- Zone of Trummerfeld
- Halo sign of Wimberger
- Subperiosteal hematoma
- Joint effsion
- Scorbutic rosary
Management
- About 3 to 4 ounces of fresh orange juice or tomato juice daily.
- Ascorbic acid 100 mg or more orally or parenterally twice or thrice daily for 10 to 15 days.
Question.22. Write short note on Thiamin (Vitamin B1).
Answer.
Thiamine (vitamin B1)
Synonyms: Antiberiberi factor, antineuritic vitamin, aneurin.
Properties
- Thiamine is readily soluble in water
- It is stable in acid medium.
- It is destroyed when autoclave at 120°C for 30 minutes.
Source
- Rich sources: Polishing rice, wheat jaw and yeast
- Good source: Cereals, pulses, nuts, oil seeds
- Fair sources: Meat, fih, egg, milk, vegetable and fruit.
Daily requirement
- Infants: 0.3 to 0.5 mg
- Children: 0.7 to 1.2 mg
- Adults: 1 to 1.5 mg
- Pregnant woman: 1.3 to 1.5 mg.
Physiological role
- Thiamine is essential for growth.
- It is essential for maintaining the nerves in normal condition.
Defiiency Manifestations
- Beri-beri: It is a nutritional disorder.
- Wet-beriberi
- Edema is the most prominent feature
Anorexia and dyspepsia are present. - Dry beriberi
- Essential feature is polyneuropathy
- Muscles become wasted and weak and diffilty in walking.
- Infantile Beriberi.
- Wernick’s encephalopathy: There is involvement of brain which is characterized by ataxia, ophthalmoplegia,confusion and disorientation.
- Korsakoff psychosis: It occurs due to involvement of mammilary bodies and confabulates with amnesia.
Presence of angular stomatitis.
Question.23. Write short note on diabetic diet.
Answer. The golden rule for a diabetic on diet therapy should be to eat litte and more often.
- A heavy meal is not desirable since it gives rise to rise in blood lipids.
- One must time the meals, food must have variety and monotony in diet be avoided.
- Foods should be adjusted in such a way that they form part of the family ratios.
Requirements are determined by the patient’s activity
- Overweight NIDDM should be encouraged to establish their weight within a desirable range.
A reduction of approximately 500 kcal/ day can result in loss of 1–2 kg/month. - Carbohydrates: Carbohydrates should be taken in form of starch and complex sugars.
100–300 gm of carbohydrates should be spreaded over 3 meals, i.e. 60 gm each and 3 snacks, i.e. 30 gm each with half liter of milk.
Unrefied carbohydrates should be substituted by refied carbohydrates to the extent possible. - Proteins: Recommended dietary allowance of 0.85 g/kg body weight for adult is an appropriate guide.
- Fat: Fat intake should be 50 to 150 gm daily divided between the meals.
Replacement of saturated with polyunsaturated fat is desirable to reduce cardiovascular risk.
Cholesterol intake should be < 300 mg/day. - Fiber: Increased consumption of dietary fier especially soluble fier are associated with lower levels of blood glucose and serum lipids.
The water insoluble fiers such as cellulose, lignin and most hemicelluloses found in whole grain breads, cereals and wheat bran affct gastrointestinal transit time and faecal bulk with litte impact on plasma glucose.
However, highly viscous water soluble fiers such as pectins, gums and storage polysaccharide found in fruits, legumes, lentils roots, tubers, oat and oat bran, when eaten in purifid form, reduce serum levels of glucose and insulin.
Ideal recommended amount of fier in patient’s diet is 35–40 g/day. - Alternative sweeteners: Both nutritive and nonnutritive sweeteners are acceptable in diabetes management.
- Sodium: It should be restricted to 1000 mg/1000 kcal, not to exceed 3000 mg/day to minimize symptoms of hypertension.
- Alcohol: It should be taken in moderation and may need to be restricted entirely by person with diabetes and insulin—induced hypoglycemia, neuropathy, poor control of glucose and lipids, or obesity.
- Vitamins, minerals and antioxidants — intake should be encouraged.
Forbidden foods: Sugar, jam, jellies, honey, jaggery, tinned fruits and juices, sweets, chocolate, ice creams, pastries, glucose drinks, foods made with sugar, pudding, sauces.
Foods allowed in moderation: Bread of all kinds and chapatts made from wheat or millets, plain biscuits, all fresh fruits, baked beans, breakfast cereals.
Free foods: All meat, fih, eggs (not fried), clear soup or meat extracts; tea or coffe; vegetables such as cabbage, cauliflwer, spinach, pumpkin, brinjal, lady’s figer, turnip, French beans, cucumber, lettce, tomato, spring onions, radish, asparagus.
Spices, salt, pepper and mustard; buttr and margarine. Sugar substitutes for sweetening.
Question.24.Give defiition, etiology, sign, symptoms, complication and management of diabetes mellitus.
Answer. Diabetes mellitus is a group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action or both.
Etiology
- Heredity: It is inherited as mendelian type of recessive trait and is predominant in children born to parents who are diabetic.
Every person who has a history of diabetes in his or her family is a carrier of disease.
The risk percentage in fist degree relatives is generally up to 20% while in second degree relatives it is about 5 % and the overall percentage of diabetes among the children of diabetics goes up to 10 %. Identical twins of a diabetic have almost 40 % chances of developing the disease. - Obesity: Obese people are more prone to suffer from diabetes probably because obesity imposes strain on the islets of Langerhans and there is a relative defiiency of insulin.
Obese also show a relative resistance to insulin due to reduction in the number of insulin receptors on target cells. Obesity results due to uninhibited indulgence in food and lack of physical activity and imposes a constant stress on the pancreas.
Thus these people are more prone to get diabetes. - Race: All races are involved and suffer from diabetes though a number of factors operate in one ethnic group or the other. Jewish race has been known to be more commonly affcted than others.
Some communities are known to have less incidence of diabetes as compared to others, but here the role of diet, physical exercise and environmental factors come into play.
A certain community in Japan (Ainus) was known to have practically no or litte diabetes probably due to undernourishment and poverty, but with the rapid industrialization and boom in the economy of the community, the incidence of diabetes among them has gone up. - Social and environmental factors: Diabetes has been considered a disease of civilization and its prevalence is closely related to the economic afflnce.
Diabetes occurs more in richer and afflnt classes of society though the poorer class of people are equally liable to suffr from early onset diabetes.
Diabetes in richer class of people is closely related to their eating habits, lack of physical effrt and obesity. - Exercise: Lack of physical effrt and exercise promotes obesity and indirectly predisposes to diabetes.
Physical effrt and leading an active life goes a long way in keeping one self trim and helps in the proper utilization of body glucose and maintains a homeostatic balance. - Diet: Excessive intake of carbohydrates and refied sugars produces strain on the pancreas and this combined with sedentary occupation goes a long way in predisposing to diabetes.
- Parity: Women with repeated pregnancies are more liable to develop diabetes since too many pregnancies are a strain on the carbohydrate metabolism and often there is hormonal imbalance.
Sign and symptoms/ clinical Features
In type I diabetes Mellitus
Symptoms
- Polydypsia, polyuria and polyphagia
- Weight loss
- Weakness and lassitude.
Sign
- Severe emaciation with wastening of muscles
- Ribs are prominent.
- In such patients if diabetic ketoacidosis is severe patient develop mental apathy, confusion and undergo coma.
In type II diabetes Mellitus
Symptoms
Patient remains asymptomatic in the beginning. Disease is detected during routine check up.
Sign
In this multiple systems are affcted, so considering this various signs are:
- Eyes: Errors of refraction leads to frequent change in spectacles, premature formation of cataract, retinopathy,recurrent sty.
- Skin: Abscess, carbuncle, boils, nonhealing wounds.
- Gastrointestinal tract: Chronic diarrhea, malabsorption and dilatation of stomach.
- Cardiovascular system: Hypertension, ischemic heart disease, diabetic foot, cold extremities.
- Respiratory system: Pneumonia, tuberculosis and lung abscess.
- Nervous system: Autonomic neuropathy and peripheral neuritis.
- Urinary tract: Nephrotic syndrome, urinary tract infection.
- Genital tract: Pruritis vulvae, menstrual irregularity and infertility.
Complications
Acute Or Immediate Complications
- Diabetic ketoacidosis or coma
- Hypoglycemia or hypoglycemic coma
- Nonketotic hyperosmolar diabetic coma
- Lactic acidosis
First two complications occur in Type I diabetes mellitus and other two occur in Type II diabetes mellitus.
Diabetic Ketoacidosis
- It is an exclusive complication of type I diabetes. It can develop in patients with severe insulin defiiency combined with glucagon excess.
Failure to take insulin and exposure to stress are precipitating causes. - As the ketogenesis continues the excess ketone bodies produced cannot be degraded by the muscles and other tissues resulting in ketosis, which manifests as anorexia, nausea, vomiting, deep and fast breathing, mental confusion and coma. However, most of the patients recover.
Hypoglycemia
- It is defied as fall in blood glucose concentration below 3.1 mmol/L.
- It is seen in type I diabetes patients due to excessive administration of insulin, missing a meal or due to stress.
- As the hypoglycemia continues, it can lead to comma,cardiac arrhythmias and is fatal.
- This can lead to worsening of control of diabetes and rebound hyperglycemia.
Nonketotic Hyperosmolar Diabetic Coma
- It is common in type II diabetes mellitus.
- The clinical hallmark is hyperglycemia, hyperosmolality and dehydration without ketoacidosis.
- Precipitating features are infection, myocardial infarction,drugs such as thiazides, steroids, diphenylhydantoin.
- Loss of glucose in urine is so intense that the patient is unable to drink suffient water to maintain urinary flid loss.
- Because of high viscosity of blood, thrombotic and bleeding complications are frequent. Mortality rate is high in this complication.
Lactic Acidosis
- It is seen in type II diabetes mellitus.
- It is caused due to excess lactate production and/or inadequate utilization.
- This can be precipitated by metformin or other systemic disorders such as liver or renal failure, pancreatitis or leukemia.
- Cardiovascular collapse leads to mortality.
Chronic or late-onset complications
These complications are due to changes in small blood vessels i.e.microangiopathy or in large blood vessels, i.e. macroangiopathy.
Microvascular are retinopathy, neuropathy, nephropathy and miscellaneous
Macrovascular are atherosclerosis, hypertension, peripheral vascular disease and diabetic foot ulcer
The chronic complications occur more frequently in Type II diabetes mellitus rather than Type I diabetes mellitus.
Diabetic Retinopathy
- This is the very important cause of blindness in diabetic patients.
- Dilatation of retinal capillaries is earliest sign. Besides these there is also presence of microaneurysms, retinal hemorrhage, neovascularization, hard and soft exudates,vitreous hemorrhage and firosis.
- Frequency, onset and severity of retinopathy vary in diabetic patients.
- Background retinopathy is most common and proliferative retinopathy is less common.
Diabetic Neuropathy
- It can involve any part of nervous system except the brain.
- Neuropathy is an early and common complication which leads to morbidity and disability.
- Poor glycemic control and long duration of diabetes is associated with high incidence of neuropathy.
- Sign and symptoms are of peripheral nervous system.
- Main pathological changes in peripheral nerves are axonal degeneration of myelinated and non-myelinated fiers,
Segmental demyelination, Schwann cell injury.
Diabetic Nephropathy
- This is the most common cause of mortality and morbidity in diabetic patients.
- 40 to 50% of type II diabetes patient develop it and 25% patients with type I diabetes develop end stage renal disease and die of it.
- It is divided into three stages, in fist stage patient is asymptomatic but has high GFR, in next stage there is renal hypertrophy which leads to microalbuminuria.
- In advance stage, patient develop macroproteinuria and passes onto nephrotic syndrome.
- 25% of patients with diabetic nephropathy can go directly at end stage renal disease with hypertension and undergo chronic renal failure.
Miscellaneous
It consists of various infections, gastroparesis, arthropathy.
Atherosclerosis
- In diabetic patient development of athroma is faster as compared to normal individual.
- Hyperlipidemia, decreased HDL levels, increased platelet adhesiveness, obesity and associated hypertension are contributory factors for athrosclerosis.
- Atherosclerosis leads to coronary artery disease, silent myocardial infarction, cerebral stroke and gangrene of toes and feet.
Diabetic Foot Ulcer
- This is the frequent site of complication in diabetes.
- Pathogenic components of diabetic foot are neuropathy,peripheral vascular disease causing ischemia and secondary infection causing ulceration.
Management
Diet Management
- Restoration of normal blood glucose and optimum levels.
- Maintenance of blood glucose levels as near to physiologic levels to prevent onset or progression of complications.
- Maintenance of normal growth rate in children and adolescents as well as attinment and maintenance of reasonable body weight in adolescents and children.
- Provision of adequate nutrition for pregnant women and fetus during lactation.
- Consistency in timing of meals and snacks to prevent inordinate swings in blood glucose level.
- Motivation to have small frequent meals.
- Determination of meal plan appropriate for individual and based on dietary history to have good compliance.
- Management of weight reduction for obese individuals with NIDDM.
- Improvement in the overall health of patients with diabetes through optimal nutrition.
Total Calories
Requirements are determined by the patients activity:
- Overweight NIDDM should be encouraged to establish their weight within a desirable range. A reduction of approximately 500 kcal/ day can result in loss of 1–2 kg/month.
- Carbohydrates: Carbohydrates should be taken in form of starch and complex sugars. 100–300 g of carbohydrates should be spreaded over 3 meals, i.e. 60g each and 3 snacks,i.e. 30 geachwithhalflitre ofmilk. Unrefied carbohydrates should be substituted by refied carbohydrates to the extent possible.
- Proteins: Recommended dietary allowance of 0.85 g/kg body weight for adult is an appropriate guide.
- Fat: Fat intake should be 50–150 g daily divided between the meals. Replacement of saturated with polyunsaturated fat is desirable to reduce cardiovascular risk. Cholesterol intake should be < 300 mg/day.
- Fiber: Increased consumption of dietary fier especially soluble fier are associated with lower levels of blood glucose and serum lipids. The water insoluble fiers such as cellulose, lignin and most hemicelluloses found in whole grain breads, cereals and wheat bran affct gastrointestinal transit time and fecal bulk with litte impact on plasma glucose. However highly viscous water soluble fiers such
as pectins, gums and storage polysaccharide found in fruits, legumes, lentils roots, tubers, oat and oat bran, when eaten in purifid form, reduce serum levels of glucose and insulin. Ideal recommended amount of fier in patient’s diet is 35–40 g/day. - Alternative sweeteners: Both nutritive and nonnutritive sweeteners are acceptable in diabetes management.
- Sodium: It should be restricted to 1000 mg/1000 kcal, not to exceed 3000 mg/day to minimize symptoms of hypertension.
- Alcohol: It should be taken in moderation and may need to be restricted entirely by person with diabetes and insulin—induced hypoglycemia, neuropathy, poor control of glucose and lipids, or obesity.
- Vitamins, minerals and antioxidants: intake should be encouraged.
Forbidden foods: Sugar, jam, jellies, honey, jaggery, tinned fruits and juices, sweets, chocolate, ice creams, pastries, glucose drinks, foods made with sugar, pudding, sauces.
Foods allowed in moderation: Bread of all kinds and chapatts made from wheat or millets, plain biscuits, all fresh fruits, baked beans, breakfast cereals.
Free foods: All meat, fih, eggs (not fried), clear soup or meat extracts; tea or coffe; vegetables such as cabbage, cauliflwer, spinach, pumpkin, brinjal, lady’s figer, turnip, French beans,cucumber, lettce, tomato, spring onions, radish, asparagus.
Spices, salt, pepper and mustard; buttr and margarine. Sugar substitutes for sweetening.
Oral Hypoglycemics
These drugs are used in patients of Type II diabetes mellitus(NIDDM) who do not respond to dietary management and who would otherwise require treatment with insulin in later situation, so they are also used as adjuvant drugs to insulin in overweight diabetes patients.
Insulin secretagogues i.e. drugs increasing secretion of insulin
- Sulfonyl ureas
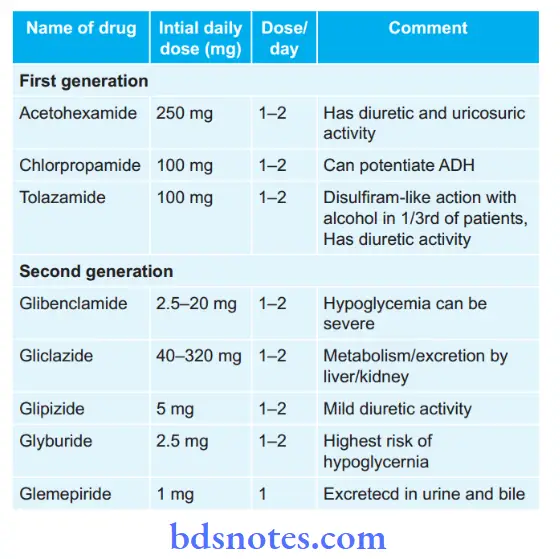
Meglitinides:
- Repaglinide, i.e. 0.5–4 mg three times a day
- Netaglinide, i.e. 60–120 mg three times a day 15 to 30 min before each meal
- Voglibose, i.e. 0.2–0.3 mg, 15–30 min before each meal.
Insulin sensitizers, i.e.drugs sensitizing action of insulin and overcome insulin resistance
- Biguanides, i.e. metformin should be given 1.5–2.5 g/day in three divided doses after meals.
- Thiozolidinediones, i.e.rosiglitazone should be given 2–8 mg or pioglitazone 15–45 mg in a single or two divided doses.
They can be combined with sulfonyl ureas or metformin
- Alpha glucosidase inhibitors, i.e. Acarbose 25 to 100 mg TDS or Voglibose 0.2–5 mg TDS taken orally in three main meals.
- It can be given in combination with metformin 500 mg for increased effiency.
- DPP-4 inhibitor: Vildagliptin 50–100 mg daily in two dived doses with meals ot saxagliptin 2.5 to 5mg OD.
- Pramlinide: Initial dose is 15 μg before each meals in Type I diabetes mellitus and 60 μg in Type II diabetes mellitus.
Insulin
Following are the indications for insulin therapy:
- In type I diabetes mellitus
- In gestational diabetes
- Hyperglycaemia despite maximum doses of oral agents
- Decompensation due to intercurrent events such as infection, acute injury or stress
- Development of severe hyperglycemia with ketosis
- Perioperative in patients undergoing surgery
- Kidney or hepatic disease
Various Insulin Preparations
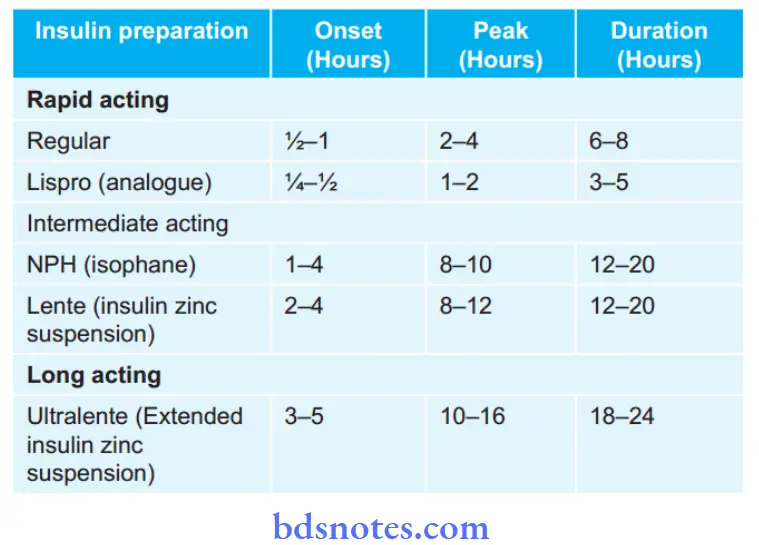
Treatment Strategies with Insulin
- Single dose regimen: Daily injection of intermediate act ing insulin given before breakfast.
The starting dose 0.3–0.4 U/Kg/ day; increased gradually to obtain glucose values in acceptable range.
Regular insulin can be added to decrease the glucose level that follows breakfast. - Twice daily regimen: Combination of regular and intermediate acting insulin BD, i.e. before breakfast and before dinner (“Split mix” regimen).
- Multiple daily injections: For achievement of more tight control of blood glucose which requires administration of at least 3 injections per day.
These can be given with use of mixture of intermediate and shortacting insulins (premixed insulin) in the morning before breakfast, with regular insulin before supper and intermediateacting at bedtime; or again a combination of regular and intermediateacting before dinner.
Divide the total daily into 2 equal doses following 1:1 transfer from basal insulin.
Give half before breakfast and other half before dinner.
The largest meal will require larger proportion of insulin.
Reduce total dose by 20%, if patient experiences recurrent hypoglycemia. - Insulin concentrations: The insulins are available in many concentrations. In India the commonly used is 40 U/mL
- Insulin purity: The impurities which may be contained are proinsulin, insulin intermediates and contaminating proteins from islet tissue or exocrine pancreas such as glucagon, somatostatin and pancreatic polypeptides.
Standard insulins currently have only 10–20 PPM of proinsulin and purifid monocomponent insulins less than 1 PPM.
Best sites for the insulin injection are subcutaneous fat on abdomen, buttck, anterior thigh and dorsal area of arm.
Exercise
- Exercise must be adjusted to patient’s preference and existing medical condition.
- Aerobic exercise is preferred, i.e. swimming, cycling,walking, running. etc
- Addition of moderate resistance should be considered.
- Duration should be 20–45 minutes per session.
- Frequency is 3–4 sessions per week is required to observe benefiial metabolic effcts. 4–5 sessions per week for weight reduction.
- ADA recommends 150 min/week of moderate aerobic physical activity with no gaps longer than 2 days.
- Program of exercise should be:
- Stretching for 5–10 min
- Warm up for 5–10 min
- Exercise for 20–45 min
- Warm down for 10 min at 30% offull exercise intensity.
Question.25.Write briefl on sign, symptoms and treatment of protein malnutrition.
Answer. Protein malnutrition is caused due to deficiency of proteins in body.
Symptoms
- Patient has high urge for food and water.
- Patient becomes weak, exhausted and fatigued.
- Presence of loss of libido
- Patient feels cold
- Amenorrhea is present.
- Patient looks old and mature and face is expressionless.
- Diarrhea may occur.
- Patient in inactive and is depressed.
- There is loss of libido
Signs
- Muscle wastening is present.
- Extremities of patient are cold.
- Skin is dry, lustureless and become fisured.
- Subcutaneous fat is absent and bony prominences are prominent.
- Circumference of arm is subnormal.
- In females edema is present which is not due to hypoalbuminemia.
- Body temperature is subnormal
- Tendon jerks become diminished.
- Pulse of patient is slow and blood pressure becomes low.
- Abdominal distention is commonly present.
Treatment
In adults
- For mild starvation adequate supplementation of nutrients is necessary
- In moderately starved people extrafeeding is needed
- In severely starved persons food is given in small amount at frequent intervals.
Food should be staple meal, i.e. cereal with some sugar, milk and oils, salt is restricted.
Potassium,magnesium and vitamins are adequately given. This is continued till patient feel active.
In children
1. Diet
- Diet for mild to moderate cases: Diet should be easily digestable. It should be rich in proteins, minerals and vitamins with extra calories. Milk should be given.
Egg is a good flp with milk and water as a source of fist class protein.
Plant protein mixtures such as corn,soya, diet milk can be given. Additional fats should be included.
If there is lactose intolerance dal, rice and buttr can be given. - Diet for acute cases: Protein intake should be 3 to 4g/kg/day and energy intake of 150kcal/Kg/day.
If child is unable to take diet from mouth go for nasogastric intubation.
Care must be taken to take sufficient amount of plant, animal proteins and fats to maintain the weight.
2. Vitamins and mineral supplementations:
- Vitamin A, D, B complex and C are given at therapeutic dosages.
- In vitamin A defiiency 30 mg of vitamin A should be given for 3 days.
- 0.5 to 1gm of potassium chloride dissolve in feeds or water should be given daily in divided dosages.
3. Maintainence of body temperature
For maintainence of body temperature at night blankets or room heaters are useful.
4. Skincare
In cases of dermatoses skin should be kept clean and protected.
In-hospital treatment:
- Correction of dehydration, electrolyte disturbances, hypoglycemia, acidosis and hypothermia.
- Parenteral therapy with half of saline and 2.5% glucose before diet therapy.
- In anemia packed erythrocyte infusion is given.
Question.26. Discuss the clinical features, diagnosis and management of diabetes mellitus.
Answer.
Sign and symptoms/ clinical Features
In type I diabetes Mellitus
Symptoms
- Polydypsia, polyuria and polyphagia
- Weight loss
- Weakness and lassitude.
Sign
- Severe emaciation with wastening of muscles
- Ribs are prominent.
- In such patients if diabetic ketoacidosis is severe patient develop mental apathy, confusion and undergo coma.
In type II diabetes Mellitus
Symptoms
Patient remains asymptomatic in the beginning. Disease is detected during routine check up.
Sign
In this multiple systems are affcted, so considering this various signs are:
- Eyes: Errors of refraction leads to frequent change in spectacles, premature formation of cataract, retinopathy,recurrent sty.
- Skin: Abscess, carbuncle, boils, nonhealing wounds.
- Gastrointestinal tract: Chronic diarrhea, malabsorption and dilatation of stomach.
- Cardiovascular system: Hypertension, ischemic heart disease, diabetic foot, cold extremities.
- Respiratory system: Pneumonia, tuberculosis and lung abscess.
- Nervous system: Autonomic neuropathy and peripheral neuritis.
- Urinary tract: Nephrotic syndrome, urinary tract infection.
- Genital tract: Pruritis vulvae, menstrual irregularity and infertility.
Management
Diet Management
- Restoration of normal blood glucose and optimum levels.
- Maintenance of blood glucose levels as near to physiologic levels to prevent onset or progression of complications.
- Maintenance of normal growth rate in children and adolescents as well as attinment and maintenance of reasonable body weight in adolescents and children.
- Provision of adequate nutrition for pregnant women and fetus during lactation.
- Consistency in timing of meals and snacks to prevent inordinate swings in blood glucose level.
- Motivation to have small frequent meals.
- Determination of meal plan appropriate for individual and based on dietary history to have good compliance.
- Management of weight reduction for obese individuals with NIDDM.
- Improvement in the overall health of patients with diabetes through optimal nutrition.
Total Calories
Requirements are determined by the patients activity:
- Overweight NIDDM should be encouraged to establish their weight within a desirable range. A reduction of approximately 500 kcal/ day can result in loss of 1–2 kg/month.
- Carbohydrates: Carbohydrates should be taken in form of starch and complex sugars. 100–300 g of carbohydrates should be spreaded over 3 meals, i.e. 60g each and 3 snacks,i.e. 30 geachwithhalflitre ofmilk. Unrefied carbohydrates should be substituted by refied carbohydrates to the extent possible.
- Proteins: Recommended dietary allowance of 0.85 g/kg body weight for adult is an appropriate guide.
- Fat: Fat intake should be 50–150 g daily divided between the meals. Replacement of saturated with polyunsaturated fat is desirable to reduce cardiovascular risk. Cholesterol intake should be < 300 mg/day.
- Fiber: Increased consumption of dietary fier especially soluble fier are associated with lower levels of blood glucose and serum lipids. The water insoluble fiers such as cellulose, lignin and most hemicelluloses found in whole grain breads, cereals and wheat bran affct gastrointestinal transit time and fecal bulk with litte impact on plasma glucose. However highly viscous water soluble fiers such
as pectins, gums and storage polysaccharide found in fruits, legumes, lentils roots, tubers, oat and oat bran, when eaten in purifid form, reduce serum levels of glucose and insulin. Ideal recommended amount of fier in patient’s diet is 35–40 g/day. - Alternative sweeteners: Both nutritive and nonnutritive sweeteners are acceptable in diabetes management.
- Sodium: It should be restricted to 1000 mg/1000 kcal, not to exceed 3000 mg/day to minimize symptoms of hypertension.
- Alcohol: It should be taken in moderation and may need to be restricted entirely by person with diabetes and insulin—induced hypoglycemia, neuropathy, poor control of glucose and lipids, or obesity.
- Vitamins, minerals and antioxidants: intake should be encouraged.
Forbidden foods: Sugar, jam, jellies, honey, jaggery, tinned fruits and juices, sweets, chocolate, ice creams, pastries, glucose drinks, foods made with sugar, pudding, sauces.
Foods allowed in moderation: Bread of all kinds and chapatts made from wheat or millets, plain biscuits, all fresh fruits, baked beans, breakfast cereals.
Free foods: All meat, fih, eggs (not fried), clear soup or meat extracts; tea or coffe; vegetables such as cabbage, cauliflwer, spinach, pumpkin, brinjal, lady’s figer, turnip, French beans,cucumber, lettce, tomato, spring onions, radish, asparagus.
Spices, salt, pepper and mustard; buttr and margarine. Sugar substitutes for sweetening.
Oral Hypoglycemics
These drugs are used in patients of Type II diabetes mellitus(NIDDM) who do not respond to dietary management and who would otherwise require treatment with insulin in later situation, so they are also used as adjuvant drugs to insulin in overweight diabetes patients.
Insulin secretagogues i.e. drugs increasing secretion of insulin
- Sulfonyl ureas
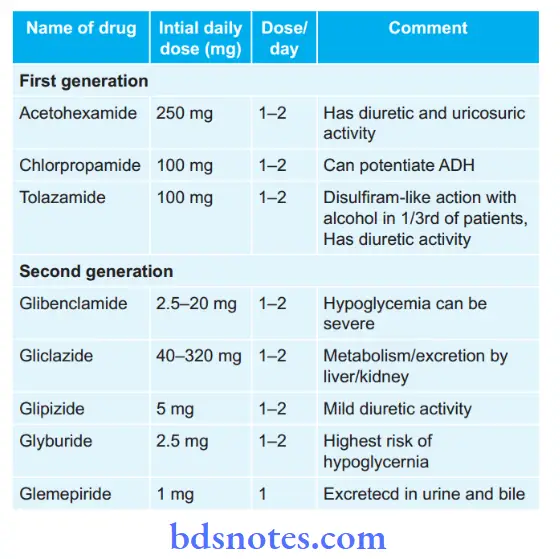
Meglitinides:
- Repaglinide, i.e. 0.5–4 mg three times a day
- Netaglinide, i.e. 60–120 mg three times a day 15 to 30 min before each meal
- Voglibose, i.e. 0.2–0.3 mg, 15–30 min before each meal.
Insulin sensitizers, i.e.drugs sensitizing action of insulin and overcome insulin resistance
- Biguanides, i.e. metformin should be given 1.5–2.5 g/day in three divided doses after meals.
- Thiozolidinediones, i.e.rosiglitazone should be given 2–8 mg or pioglitazone 15–45 mg in a single or two divided doses.
They can be combined with sulfonyl ureas or metformin
- Alpha glucosidase inhibitors, i.e. Acarbose 25 to 100 mg TDS or Voglibose 0.2–5 mg TDS taken orally in three main meals.
- It can be given in combination with metformin 500 mg for increased effiency.
- DPP-4 inhibitor: Vildagliptin 50–100 mg daily in two dived doses with meals ot saxagliptin 2.5 to 5mg OD.
- Pramlinide: Initial dose is 15 μg before each meals in Type I diabetes mellitus and 60 μg in Type II diabetes mellitus.
Insulin
Following are the indications for insulin therapy:
- In type I diabetes mellitus
- In gestational diabetes
- Hyperglycaemia despite maximum doses of oral agents
- Decompensation due to intercurrent events such as infection, acute injury or stress
- Development of severe hyperglycemia with ketosis
- Perioperative in patients undergoing surgery
- Kidney or hepatic disease
Various Insulin Preparations
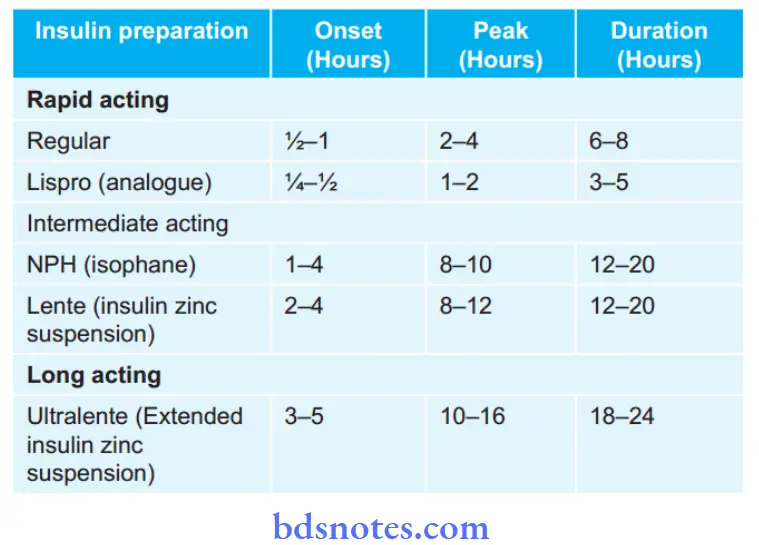
Treatment Strategies with Insulin
- Single dose regimen: Daily injection of intermediate act ing insulin given before breakfast.
The starting dose 0.3–0.4 U/Kg/ day; increased gradually to obtain glucose values in acceptable range.
Regular insulin can be added to decrease the glucose level that follows breakfast. - Twice daily regimen: Combination of regular and intermediate acting insulin BD, i.e. before breakfast and before dinner (“Split mix” regimen).
- Multiple daily injections: For achievement of more tight control of blood glucose which requires administration of at least 3 injections per day.
These can be given with use of mixture of intermediate and shortacting insulins (premixed insulin) in the morning before breakfast, with regular insulin before supper and intermediateacting at bedtime; or again a combination of regular and intermediateacting before dinner.
Divide the total daily into 2 equal doses following 1:1 transfer from basal insulin.
Give half before breakfast and other half before dinner.
The largest meal will require larger proportion of insulin.
Reduce total dose by 20%, if patient experiences recurrent hypoglycemia. - Insulin concentrations: The insulins are available in many concentrations. In India the commonly used is 40 U/mL
- Insulin purity: The impurities which may be contained are proinsulin, insulin intermediates and contaminating proteins from islet tissue or exocrine pancreas such as glucagon, somatostatin and pancreatic polypeptides.
Standard insulins currently have only 10–20 PPM of proinsulin and purifid monocomponent insulins less than 1 PPM.
Best sites for the insulin injection are subcutaneous fat on abdomen, buttck, anterior thigh and dorsal area of arm.
Exercise
- Exercise must be adjusted to patient’s preference and existing medical condition.
- Aerobic exercise is preferred, i.e. swimming, cycling,walking, running. etc
- Addition of moderate resistance should be considered.
- Duration should be 20–45 minutes per session.
- Frequency is 3–4 sessions per week is required to observe benefiial metabolic effcts. 4–5 sessions per week for weight reduction.
- ADA recommends 150 min/week of moderate aerobic physical activity with no gaps longer than 2 days.
- Program of exercise should be:
- Stretching for 5–10 min
- Warm up for 5–10 min
- Exercise for 20–45 min
- Warm down for 10 min at 30% offull exercise intensity.
Diagnosis
Diagnosis is based on symptoms, signs and laboratory tests.
In presence ofsigns and symptoms confimation is done by fiding random blood glucose higher than 200 mg/dL.
Investigations
- Blood sugar estimation: Both fasting and postprandial (2 hours after a meal) levels of blood sugar be estimated.
Mean value of blood sugar in healthy adults is 70 to 80 mg%. When fasting blood sugar level exceeds 110 mg% diagnosis is clear.
Postprandial blood sugar level is further screening test, if value exceeds 120 mg% it is strongly suggestive of diabetes mellitus.
Random blood sugar estimation is not of much help as screening test.
Value exceeding 160 mg% in presence of glycosuria is suggestive but values about 200 mg% is diagnostic. - Oral glucose tolerance test: In this fist sample is taken after an overnight fast of 8 hours following which patient is given glucose 1g/kg body weight.
Blood is then collected at 30, 60, 120 and 180 minutes.
In diminished glucose tolerance, level of blood glucose is raised at 180 minutes. - Glycosylated hemoglobin: It measures the longterm glycemic control.
Slow nonenzymatic attachment of glucose to hemoglobin result in formation of glycosylated hemoglobin. - Microalbumin: Patients with microalbumineria are on greater risk in developing kidney failure as well as cardiovascular damage.
- Urine protein/creatinine ratio: It provides information of proteinuria in patients with diabetic nephropathy.
More is the ratio greater is the damage. - Insulin levels: Elevated blood glucose levels with low insulin levels indicate insufficient insulin levels for adequate control of blood glucose.
High insulin levels with low blood glucose indicate change in dosage of drug. - Insulin antibody test: In this there is quantitative determination of antibodies against insulin in serum.
- GAD 65 antibody: These antibodies are common in newly diagnosed diabetic patient and often appear years before clinical onset in the disease. Presence of this antibody is the strong predictive marker for onset of type I diabetes mellitus.
Criterias Given By WHo In 1999
- Presence of classic symptoms of diabetes and causal plasma glucose greater than or equal to 200 mg/dL.
Causal is any time of day without regard to time since last meal.
Classic symptoms of diabetes include polyuria, polydypsia and unexplained weight loss.
Or - Fasting plasma glucose greater than or equal to 126 mg/dL.
Fasting is defied as no caloric intake for 8 hours.
Or - Twohoursplasmaglucosegreaterthanorequalto200 mg/dL during an oral glucose tolerance test.
Test is performed as described by World Health Organization by using glucose load containing equivalent of 75 gm anhydrous glucose dissolved in water.
In absence of unequivocal hyperglycemia with acute metabolic decompensation above criterias are confimed by repeated testing on other days.
Question.27. Write sign and symptoms of diabetes mellitus.
Or
Describle clinical features of diabetes mellitus.
Answer.
Diabetes mellitus is a group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action or both.
Etiology
- Heredity: It is inherited as mendelian type of recessive trait and is predominant in children born to parents who are diabetic.
Every person who has a history of diabetes in his or her family is a carrier of disease.
The risk percentage in fist degree relatives is generally up to 20% while in second degree relatives it is about 5 % and the overall percentage of diabetes among the children of diabetics goes up to 10 %. Identical twins of a diabetic have almost 40 % chances of developing the disease. - Obesity: Obese people are more prone to suffer from diabetes probably because obesity imposes strain on the islets of Langerhans and there is a relative defiiency of insulin.
Obese also show a relative resistance to insulin due to reduction in the number of insulin receptors on target cells. Obesity results due to uninhibited indulgence in food and lack of physical activity and imposes a constant stress on the pancreas.
Thus these people are more prone to get diabetes. - Race: All races are involved and suffer from diabetes though a number of factors operate in one ethnic group or the other. Jewish race has been known to be more commonly affcted than others.
Some communities are known to have less incidence of diabetes as compared to others, but here the role of diet, physical exercise and environmental factors come into play.
A certain community in Japan (Ainus) was known to have practically no or litte diabetes probably due to undernourishment and poverty, but with the rapid industrialization and boom in the economy of the community, the incidence of diabetes among them has gone up. - Social and environmental factors: Diabetes has been considered a disease of civilization and its prevalence is closely related to the economic afflnce.
Diabetes occurs more in richer and afflnt classes of society though the poorer class of people are equally liable to suffr from early onset diabetes.
Diabetes in richer class of people is closely related to their eating habits, lack of physical effrt and obesity. - Exercise: Lack of physical effrt and exercise promotes obesity and indirectly predisposes to diabetes.
Physical effrt and leading an active life goes a long way in keeping one self trim and helps in the proper utilization of body glucose and maintains a homeostatic balance. - Diet: Excessive intake of carbohydrates and refied sugars produces strain on the pancreas and this combined with sedentary occupation goes a long way in predisposing to diabetes.
- Parity: Women with repeated pregnancies are more liable to develop diabetes since too many pregnancies are a strain on the carbohydrate metabolism and often there is hormonal imbalance.
Sign and symptoms/ clinical Features
In type I diabetes Mellitus
Symptoms
- Polydypsia, polyuria and polyphagia
- Weight loss
- Weakness and lassitude.
Sign
- Severe emaciation with wastening of muscles
- Ribs are prominent.
- In such patients if diabetic ketoacidosis is severe patient develop mental apathy, confusion and undergo coma.
In type II diabetes Mellitus
Symptoms
Patient remains asymptomatic in the beginning. Disease is detected during routine check up.
Sign
In this multiple systems are affcted, so considering this various signs are:
- Eyes: Errors of refraction leads to frequent change in spectacles, premature formation of cataract, retinopathy,recurrent sty.
- Skin: Abscess, carbuncle, boils, nonhealing wounds.
- Gastrointestinal tract: Chronic diarrhea, malabsorption and dilatation of stomach.
- Cardiovascular system: Hypertension, ischemic heart disease, diabetic foot, cold extremities.
- Respiratory system: Pneumonia, tuberculosis and lung abscess.
- Nervous system: Autonomic neuropathy and peripheral neuritis.
- Urinary tract: Nephrotic syndrome, urinary tract infection.
- Genital tract: Pruritis vulvae, menstrual irregularity and infertility.
Complications
Acute Or Immediate Complications
- Diabetic ketoacidosis or coma
- Hypoglycemia or hypoglycemic coma
- Nonketotic hyperosmolar diabetic coma
- Lactic acidosis
First two complications occur in Type I diabetes mellitus and other two occur in Type II diabetes mellitus.
Diabetic Ketoacidosis
- It is an exclusive complication of type I diabetes. It can develop in patients with severe insulin defiiency combined with glucagon excess.
Failure to take insulin and exposure to stress are precipitating causes. - As the ketogenesis continues the excess ketone bodies produced cannot be degraded by the muscles and other tissues resulting in ketosis, which manifests as anorexia, nausea, vomiting, deep and fast breathing, mental confusion and coma. However, most of the patients recover.
Hypoglycemia
- It is defied as fall in blood glucose concentration below 3.1 mmol/L.
- It is seen in type I diabetes patients due to excessive administration of insulin, missing a meal or due to stress.
- As the hypoglycemia continues, it can lead to comma,cardiac arrhythmias and is fatal.
- This can lead to worsening of control of diabetes and rebound hyperglycemia.
Nonketotic Hyperosmolar Diabetic Coma
- It is common in type II diabetes mellitus.
- The clinical hallmark is hyperglycemia, hyperosmolality and dehydration without ketoacidosis.
- Precipitating features are infection, myocardial infarction,drugs such as thiazides, steroids, diphenylhydantoin.
- Loss of glucose in urine is so intense that the patient is unable to drink suffient water to maintain urinary flid loss.
- Because of high viscosity of blood, thrombotic and bleeding complications are frequent. Mortality rate is high in this complication.
Lactic Acidosis
- It is seen in type II diabetes mellitus.
- It is caused due to excess lactate production and/or inadequate utilization.
- This can be precipitated by metformin or other systemic disorders such as liver or renal failure, pancreatitis or leukemia.
- Cardiovascular collapse leads to mortality.
Chronic or late-onset complications
These complications are due to changes in small blood vessels i.e.microangiopathy or in large blood vessels, i.e. macroangiopathy.
Microvascular are retinopathy, neuropathy, nephropathy and miscellaneous
Macrovascular are atherosclerosis, hypertension, peripheral vascular disease and diabetic foot ulcer
The chronic complications occur more frequently in Type II diabetes mellitus rather than Type I diabetes mellitus.
Diabetic Retinopathy
- This is the very important cause of blindness in diabetic patients.
- Dilatation of retinal capillaries is earliest sign. Besides these there is also presence of microaneurysms, retinal hemorrhage, neovascularization, hard and soft exudates,vitreous hemorrhage and firosis.
- Frequency, onset and severity of retinopathy vary in diabetic patients.
- Background retinopathy is most common and proliferative retinopathy is less common.
Diabetic Neuropathy
- It can involve any part of nervous system except the brain.
- Neuropathy is an early and common complication which leads to morbidity and disability.
- Poor glycemic control and long duration of diabetes is associated with high incidence of neuropathy.
- Sign and symptoms are of peripheral nervous system.
- Main pathological changes in peripheral nerves are axonal degeneration of myelinated and non-myelinated fiers,
Segmental demyelination, Schwann cell injury.
Diabetic Nephropathy
- This is the most common cause of mortality and morbidity in diabetic patients.
- 40 to 50% of type II diabetes patient develop it and 25% patients with type I diabetes develop end stage renal disease and die of it.
- It is divided into three stages, in fist stage patient is asymptomatic but has high GFR, in next stage there is renal hypertrophy which leads to microalbuminuria.
- In advance stage, patient develop macroproteinuria and passes onto nephrotic syndrome.
- 25% of patients with diabetic nephropathy can go directly at end stage renal disease with hypertension and undergo chronic renal failure.
Miscellaneous
It consists of various infections, gastroparesis, arthropathy.
Atherosclerosis
- In diabetic patient development of athroma is faster as compared to normal individual.
- Hyperlipidemia, decreased HDL levels, increased platelet adhesiveness, obesity and associated hypertension are contributory factors for athrosclerosis.
- Atherosclerosis leads to coronary artery disease, silent myocardial infarction, cerebral stroke and gangrene of toes and feet.
Diabetic Foot Ulcer
- This is the frequent site of complication in diabetes.
- Pathogenic components of diabetic foot are neuropathy,peripheral vascular disease causing ischemia and secondary infection causing ulceration.
Management
Diet Management
- Restoration of normal blood glucose and optimum levels.
- Maintenance of blood glucose levels as near to physiologic levels to prevent onset or progression of complications.
- Maintenance of normal growth rate in children and adolescents as well as attinment and maintenance of reasonable body weight in adolescents and children.
- Provision of adequate nutrition for pregnant women and fetus during lactation.
- Consistency in timing of meals and snacks to prevent inordinate swings in blood glucose level.
- Motivation to have small frequent meals.
- Determination of meal plan appropriate for individual and based on dietary history to have good compliance.
- Management of weight reduction for obese individuals with NIDDM.
- Improvement in the overall health of patients with diabetes through optimal nutrition.
Total Calories
Requirements are determined by the patients activity:
- Overweight NIDDM should be encouraged to establish their weight within a desirable range. A reduction of approximately 500 kcal/ day can result in loss of 1–2 kg/month.
- Carbohydrates: Carbohydrates should be taken in form of starch and complex sugars. 100–300 g of carbohydrates should be spreaded over 3 meals, i.e. 60g each and 3 snacks,i.e. 30 geachwithhalflitre ofmilk. Unrefied carbohydrates should be substituted by refied carbohydrates to the extent possible.
- Proteins: Recommended dietary allowance of 0.85 g/kg body weight for adult is an appropriate guide.
- Fat: Fat intake should be 50–150 g daily divided between the meals. Replacement of saturated with polyunsaturated fat is desirable to reduce cardiovascular risk. Cholesterol intake should be < 300 mg/day.
- Fiber: Increased consumption of dietary fier especially soluble fier are associated with lower levels of blood glucose and serum lipids. The water insoluble fiers such as cellulose, lignin and most hemicelluloses found in whole grain breads, cereals and wheat bran affct gastrointestinal transit time and fecal bulk with litte impact on plasma glucose. However highly viscous water soluble fiers such
as pectins, gums and storage polysaccharide found in fruits, legumes, lentils roots, tubers, oat and oat bran, when eaten in purifid form, reduce serum levels of glucose and insulin. Ideal recommended amount of fier in patient’s diet is 35–40 g/day. - Alternative sweeteners: Both nutritive and nonnutritive sweeteners are acceptable in diabetes management.
- Sodium: It should be restricted to 1000 mg/1000 kcal, not to exceed 3000 mg/day to minimize symptoms of hypertension.
- Alcohol: It should be taken in moderation and may need to be restricted entirely by person with diabetes and insulin—induced hypoglycemia, neuropathy, poor control of glucose and lipids, or obesity.
- Vitamins, minerals and antioxidants: intake should be encouraged.
Forbidden foods: Sugar, jam, jellies, honey, jaggery, tinned fruits and juices, sweets, chocolate, ice creams, pastries, glucose drinks, foods made with sugar, pudding, sauces.
Foods allowed in moderation: Bread of all kinds and chapatts made from wheat or millets, plain biscuits, all fresh fruits, baked beans, breakfast cereals.
Free foods: All meat, fih, eggs (not fried), clear soup or meat extracts; tea or coffe; vegetables such as cabbage, cauliflwer, spinach, pumpkin, brinjal, lady’s figer, turnip, French beans,cucumber, lettce, tomato, spring onions, radish, asparagus.
Spices, salt, pepper and mustard; buttr and margarine. Sugar substitutes for sweetening.
Oral Hypoglycemics
These drugs are used in patients of Type II diabetes mellitus(NIDDM) who do not respond to dietary management and who would otherwise require treatment with insulin in later situation, so they are also used as adjuvant drugs to insulin in overweight diabetes patients.
Insulin secretagogues i.e. drugs increasing secretion of insulin
- Sulfonyl ureas
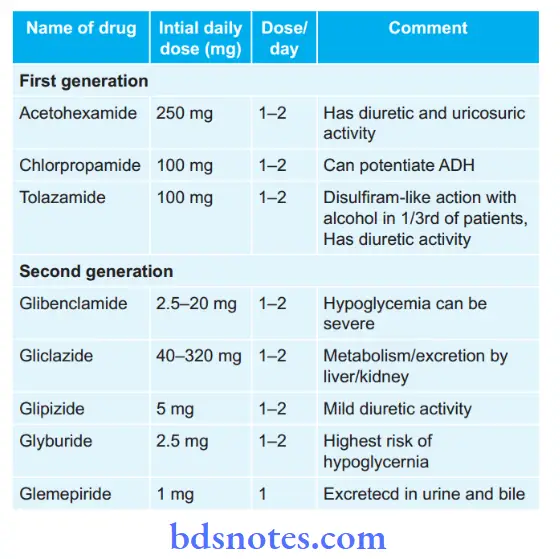
Meglitinides:
- Repaglinide, i.e. 0.5–4 mg three times a day
- Netaglinide, i.e. 60–120 mg three times a day 15 to 30 min before each meal
- Voglibose, i.e. 0.2–0.3 mg, 15–30 min before each meal.
Insulin sensitizers, i.e.drugs sensitizing action of insulin and overcome insulin resistance
- Biguanides, i.e. metformin should be given 1.5–2.5 g/day in three divided doses after meals.
- Thiozolidinediones, i.e.rosiglitazone should be given 2–8 mg or pioglitazone 15–45 mg in a single or two divided doses.
They can be combined with sulfonyl ureas or metformin
- Alpha glucosidase inhibitors, i.e. Acarbose 25 to 100 mg TDS or Voglibose 0.2–5 mg TDS taken orally in three main meals.
- It can be given in combination with metformin 500 mg for increased effiency.
- DPP-4 inhibitor: Vildagliptin 50–100 mg daily in two dived doses with meals ot saxagliptin 2.5 to 5mg OD.
- Pramlinide: Initial dose is 15 μg before each meals in Type I diabetes mellitus and 60 μg in Type II diabetes mellitus.
Insulin
Following are the indications for insulin therapy:
- In type I diabetes mellitus
- In gestational diabetes
- Hyperglycaemia despite maximum doses of oral agents
- Decompensation due to intercurrent events such as infection, acute injury or stress
- Development of severe hyperglycemia with ketosis
- Perioperative in patients undergoing surgery
- Kidney or hepatic disease
Various Insulin Preparations
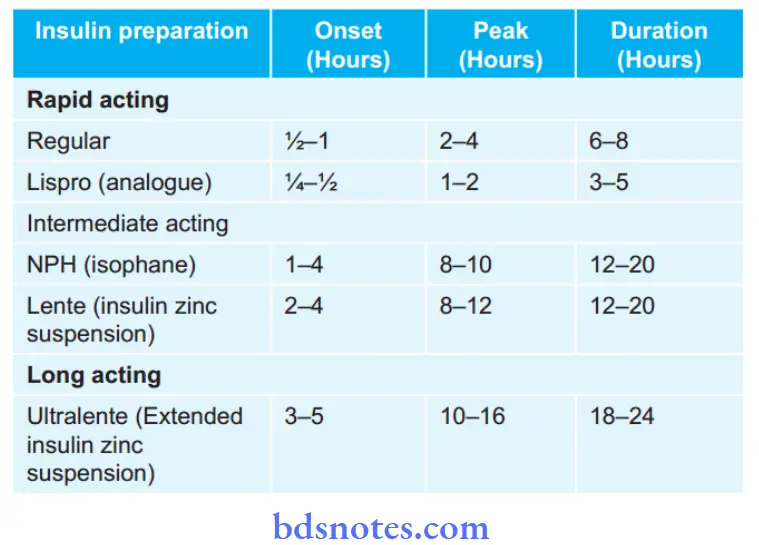
Treatment Strategies with Insulin
- Single dose regimen: Daily injection of intermediate act ing insulin given before breakfast.
The starting dose 0.3–0.4 U/Kg/ day; increased gradually to obtain glucose values in acceptable range.
Regular insulin can be added to decrease the glucose level that follows breakfast. - Twice daily regimen: Combination of regular and intermediate acting insulin BD, i.e. before breakfast and before dinner (“Split mix” regimen).
- Multiple daily injections: For achievement of more tight control of blood glucose which requires administration of at least 3 injections per day.
These can be given with use of mixture of intermediate and shortacting insulins (premixed insulin) in the morning before breakfast, with regular insulin before supper and intermediateacting at bedtime; or again a combination of regular and intermediateacting before dinner.
Divide the total daily into 2 equal doses following 1:1 transfer from basal insulin.
Give half before breakfast and other half before dinner.
The largest meal will require larger proportion of insulin.
Reduce total dose by 20%, if patient experiences recurrent hypoglycemia. - Insulin concentrations: The insulins are available in many concentrations. In India the commonly used is 40 U/mL
- Insulin purity: The impurities which may be contained are proinsulin, insulin intermediates and contaminating proteins from islet tissue or exocrine pancreas such as glucagon, somatostatin and pancreatic polypeptides.
Standard insulins currently have only 10–20 PPM of proinsulin and purifid monocomponent insulins less than 1 PPM.
Best sites for the insulin injection are subcutaneous fat on abdomen, buttck, anterior thigh and dorsal area of arm.
Question.28. Write management of diabetic ketoacidosis.
Answer. Following is the management of diabetic ketoacidosis
1. Admission of patient
- Diagnosis is confimed by examination of blood glucose and ketone measurements.
- Initial assessment of dehydration, hyperosmolality, serum potassium, acidosis and kidney function is done.
- Fluid loss is measured by subtracting admission weight by last known stable weight.
- Patient should be evaluated for sepsis.
2. Management during hour 1
- If patient is hypovolemic and hypotensive flid administration is done, i.e. normal saline is administered and if necessary colloids should be given.
Rate of administration is necessary to restore circulatory function.
As blood pressure become normal and urine output becomes
adequate rate of administration of normal saline is 1000 mL/hour. - Continuous IV infusion of regular insulin 5–10 units/hour is given.
- IV infusion of potassium is done at 10–40 mmol/hour during initiation of insulin therapy.
- Sodium bicarbonate IV is given in cases with acidosis. Dose is 50–100 mmol/L sodium bicarbonate in 0.45% saline for 30–60 minutes.
Additional potassium should also be given with bicarbonate therapy.
3. Management during hour 2
- Normal saline should be continued at 500 mL/hour.
Plasma osmolality should be greater than 285 mosmol / L during fist 12 hours.
If serum sodium is greater than 150 mmol/L switch to 0.45% saline. - Blood glucose should be checked and insulin is adjusted to 5 mmol/L/hour.
Blood glucose should not fall below 11.1–14.0 mmol/L. Anion
gap is decreasing and blood pH is increasing. - Serum potassium should be maintained at 4–5 mmol/L by addition of potassium to IV flids.
4. Management during hours 3 to 4
- Management should be continued as given in second hour.
- Cognitive and neurological symptoms should be observed for 12 hours.
5. Management during hours 5 to 8
- Normal saline should be continued at 250 mL/hour. As blood glucose reaches 11.1–14 mmol/
lt, change IV flid to 500 mL/hour normal saline with 5% glucose. - Insulin should be continued at maintenance dose until ketoacidosis is cleared.
- Potassium should be continued at 10–40 mmol/hour since ketoacidosis is cleared.
- Phosphate replacement is done at 6 hours if serum phosphate is < 2 mg/dL
6. Management during hours 8 to 24
- IV repletion is continued with 0.45% saline with or without 2.5% or 5% glucose as needed.
- As ketoacidosis is subsided patient should be switched to subcutaneous insulin and stop IV and IM insulin.
Question.29.Write classifiation, clinical features, investigations and treatment of diabetes mellitus.
Answer. Diabetes mellitus is a clinical syndrome of hyperglycemia with glycosuria due to lack of insulin or insulin resistance is termed as diabetes mellitus.
Classification
Primary diabetes
1. Type I insulin dependent diabetes mellitus (IDDM). It is subdivided:
- Immuned mediated (islet cell antibodies).
- Nonimmune (no antibody).
2. Type II noninsulin dependent diabetes mellitus (NIDDM)
It is subdivided:
- Obese (insulin resistance with relative insulin defiiency).
- Nonobese (insulin secretory detect with insulin resistance).
Secondary Diabetes
- Pancreatic diabetes due to pancreatitis.
- Hormonal or endocrinal abnormalities, i.e., acromegaly,shing’s syndrome, pheochromocytoma, etc.
- Drugs induced (Iatrogenic) due to steroids and thiazides.
- Insulin receptors antibodies.
- Genetic syndromes, i.e., Lipodystrophies, muscular dystrophies, Klinefelter’s syndrome, Turner’s syndrome,
- Down’s syndrome, DIDMOAD (Diabetes insipidus,diabetes mellitus, optic atrophy and deafness) syndrome.
Clinical Features
In type I diabetes Mellitus
Symptoms
- Polydypsia, polyuria and polyphagia
- Weight loss
- Weakness and lassitude.
Sign
- Severe emaciation with wastening of muscles
- Ribs are prominent.
- In such patients if diabetic ketoacidosis is severe patient develop mental apathy, confusion and undergo coma.
In type II diabetes Mellitus
Symptoms
Patient remains asymptomatic in the beginning. Disease is detected during routine check up.
Sign
In this multiple systems are affcted, so considering this various signs are:
- Eyes: Errors of refraction leads to frequent change in spectacles, premature formation of cataract, retinopathy,recurrent sty.
- Skin: Abscess, carbuncle, boils, nonhealing wounds.
- Gastrointestinal tract: Chronic diarrhea, malabsorption and dilatation of stomach.
- Cardiovascular system: Hypertension, ischemic heart disease, diabetic foot, cold extremities.
- Respiratory system: Pneumonia, tuberculosis and lung abscess.
- Nervous system: Autonomic neuropathy and peripheral neuritis.
- Urinary tract: Nephrotic syndrome, urinary tract infection.
- Genital tract: Pruritis vulvae, menstrual irregularity and infertility.
Investigations
- Blood sugar estimation: Both fasting and postprandial (2 hours after a meal) levels of blood sugar be estimated.
Mean value of blood sugar in healthy adults is 70 to 80 mg%. When fasting blood sugar level exceeds 110 mg% diagnosis is clear.
Postprandial blood sugar level is further screening test, if value exceeds 120 mg% it is strongly suggestive of diabetes mellitus.
Random blood sugar estimation is not of much help as screening test.
Value exceeding 160 mg% in presence of glycosuria is suggestive but values about 200 mg% is diagnostic. - Oral glucose tolerance test: In this fist sample is taken after an overnight fast of 8 hours following which patient is given glucose 1 g/kg body weight.
Blood is then collected at 30, 60, 120 and 180 minutes. In diminished glucose tolerance, level of blood glucose is raised at 180 minutes. - Glycosylated hemoglobin: It measures the longterm glycemic control. Slow nonenzymatic attachment of glucose to hemoglobin result in formation of glycosylated hemoglobin.
- Microalbumin: Patients with microalbuminria are on greater risk in developing kidney failure as well as cardiovascular damage.
- Urine protein/Creatinine ratio: It provides information of proteinuria in patients with diabetic nephropathy. More is the ratio greater is the damage.
- Insulin levels: Elevated blood glucose levels with low insulin levels indicate insufficient insulin levels for adequate control of blood glucose.
High insulin levels with low blood glucose indicate change in dosage of drug. - Insulin antibody test: In this there is quantitative determination of antibodies against insulin in serum.
- GAD 65 antibody: These antibodies are common in newly diagnosed diabetic patient and often appear years before clinical onset in the disease. Presence of this antibody is the strong predictive marker for onset of type I diabetes mellitus.
Treatment
Treatment Strategies with Insulin
- Single dose regimen: Daily injection of intermediate act ing insulin given before breakfast.
The starting dose 0.3–0.4 U/Kg/ day; increased gradually to obtain glucose values in acceptable range.
Regular insulin can be added to decrease the glucose level that follows breakfast. - Twice daily regimen: Combination of regular and intermediate acting insulin BD, i.e. before breakfast and before dinner (“Split mix” regimen).
- Multiple daily injections: For achievement of more tight control of blood glucose which requires administration of at least 3 injections per day.
These can be given with use of mixture of intermediate and shortacting insulins (premixed insulin) in the morning before breakfast, with regular insulin before supper and intermediateacting at bedtime; or again a combination of regular and intermediateacting before dinner.
Divide the total daily into 2 equal doses following 1:1 transfer from basal insulin.
Give half before breakfast and other half before dinner.
The largest meal will require larger proportion of insulin.
Reduce total dose by 20%, if patient experiences recurrent hypoglycemia. - Insulin concentrations: The insulins are available in many concentrations. In India the commonly used is 40 U/mL
- Insulin purity: The impurities which may be contained are proinsulin, insulin intermediates and contaminating proteins from islet tissue or exocrine pancreas such as glucagon, somatostatin and pancreatic polypeptides.
Standard insulins currently have only 10–20 PPM of proinsulin and purifid monocomponent insulins less than 1 PPM.
Best sites for the insulin injection are subcutaneous fat on abdomen, buttck, anterior thigh and dorsal area of ar
Question.30. Write short note on obesity.
Answer.
Obesity is the condition in which there is excessive accumulation of body fat.
Obesity is the common disorder of the nutrition of afflnt societies.
Etiology
- GeneticandEnvironmentalfactors: Genetic and environmental factors play important role in causing the obesity.
Familial predisposition is also seen.
Overeating and other factors also cause obesity.
If both the parents of a child are overweight then chances of child being obese are 80%. - Socioeconomic status: Obesity is the disorder of afflnt societies.
Some occupations also predisposes to obesity, such as cooks.
In some of the societies obesity is considered as the sign of heritage. - Energy intake: Minute excess of calories causes accumulation of fat. If there is lag of physical activity, this also causes obesity.
- Drugs: Various drugs such as steroids, oral contraceptives,etc causes increase in apetite, this leads to weight gain.
- Endocrine: During pregnancy there is increase in the body fat which is under hormonal inflence.
Obesity can also occur in hypothyroidism due to decrease calorie demands.
Clinical Features
- Type II diabetes mellitus, gallbladder stones, gout and various other metabolic disorders are associated with obesity.
- Varicose vein, hernia and osteoarthritis are the mechanical disorders associated with obesity.
- Various respiratory infections are also associated with the obesity along with the sleep disorders.
- Hypertension, atherosclerosis and ischemic heart diseases are the cardiovascular diseases which are associated with the obesity.
Management
- Diet: Calories uptake should depend on the age, sex,occupation and urgency of the weight reduction.
An obese person should spare from fats, buttr, ghee, cream dryfruits (nuts) vegetables (potatoes and peas).
Person should follow strict diet regime and maintain discipline in choice of foods to which he/she takes and the amount ofcalories consumed per day.
Food should be taken in intervals, chewed slowly. - Exercise: Habit of regular physical exercise should be cultivated by an obese person.
An obese person should do morning and evening walks, jogging, stretch exercise and taking part in outdoor games. - Drug therapy: In this recent era serotonergic drugs are used.
DL-fenflramine which was the fist generation drug was used to reduce weight.
These days it is replaced by second generation drugs dL-fenflramine, floxetine which is a slow releasing serotonin antagonist, sibutramine which is a slow serotonin and noradrenaline reuptake inhibitor.
These drugs increase the satiety and potentiate serotonin in hypothalamus. - Surgical treatment: This method is employed in the persons having severe obesity. The surgical methods employed are:
- Wiring ofjaws: This is carried out to prevent eating and only taking liquids.
This method is good but as wires are removed patient regains the weight. - Gastric plcation: In this stomach is reduced by creating a small pouch due to stapling of stomach to abdominal wall. Good results can be attined.
- Bariatric surgery: It is done in persons with extreme obesity.
Question.31. Write short note on gestational diabetes.
Answer. Gestational diabetes is defined as development of hyperglycemia, fist time in pregnancy.
- It occurs in women who are genetically predisposed to type 1 and type 2 diabetes.
- The condition is asymptomatic.
- Repeated hyperglycemia in every pregnancy lead the women to undergo suffring from permanent diabetes.
- Gestational diabetes can occur in any women, so at the time of pregnancy during each trimester random blood sugar screening is done by oral glucose tolerance test.
In this test blood glucose is more than 126 mg%.
Obstetric Complications Associated With Gestational
Diabetes Mellitus
1. Maternal risk
- Maternal hypertension
- Eclampsia
- Nephropathy, retinopathy and vascular complications can worsen.
2. Fetal risk
- Stillbirth
- Neonatal hypoglycemia
- Neonatal hypocalcemia
- Macrosome
- Hyaline membrane disease
- Growth retardation
- Congenital anomalies diagnostic criteria
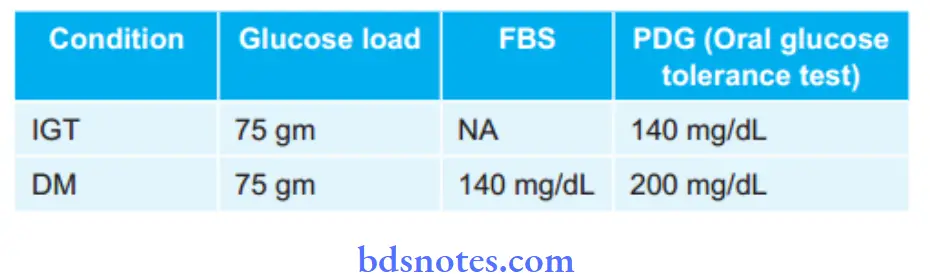
A two-step strategy has been proposed for establishment of diagnosis of gestational diabetes.
First step is to give 50 mg oral glucose and measure serum glucose at 60 min; if glucose is found less than 140 mg then test is normal and if found greater than140 mg, then it warrants second step of administration of 100 g glucose and measure the serum glucose in fasting state and at 1, 2 and 3 hrs. Normal plasma glucose concentration is given below:
- Fasting <105 mg/L.
- At 1 hr < 190 mg/L.
- At 2 hr <165 mg/L
- At 3 hr <145 mg/L.
Deviations from the normal indicate gestational diabetes mellitus.
Management
- High dietary protein intake. Salt restriction if edema is present.
- Exercise should be done regularly
- Insulin therapy is essential.
- Oral hypoglycemic should be avoided except metformin which is effctive in women with PCOD to aid conception.
Question.32.Describe briefl on Type II diabetes.
Answer. Type II diabetes is also known as non insulin dependent diabetes mellitus.
Etiology
- Genetic: It is inherited as mendelian type of recessive trait and is predominant in children born to parents who are diabetic.
Every person who has a history of diabetes in his or her family is a carrier of disease.
The risk percentage in fist degree relatives is generally up to 20 %t while in second degree relatives it is about 5 %.
Type II diabetes is caused due to abnormal insulin secretion and insulin resistance. - Due to pancreatic beta cell failure: In Type II diabetes there is reduction of pancreatic beta cell mass with reduction in insulin levels.
As beta cells decreases alpha cells secrete glucagon and this causes hyperglycemia. - Environmental factors: Physical inactivity and obesity are the factor leading to type II diabetes in genetically susceptible individuals.
- Age: Type II diabetes occur after age of 30 years.
Clinical Features
Symptoms
Patient remains asymptomatic in the beginning. Disease is detected during routine check up.
Sign
In this multiple systems are affcted, so considering this various signs are:
- Eyes: Errors of refraction leads to frequent change in spectacles, premature formation of cataract, retinopathy,recurrent sty.
- Skin: Abscess, carbuncle, boils, nonhealing wounds.
- Gastrointestinal tract: Chronic diarrhea, malabsorption and dilatation of stomach.
- Cardiovascular system: Hypertension, ischemic heart disease, diabetic foot, cold extremities.
- Respiratory system: Pneumonia, tuberculosis and lung abscess
- Nervous system: Autonomic neuropathy and peripheral neuritis
- Urinary tract: Nephrotic syndrome, urinary tract infection.
- Genital tract: Pruritus vulvae, menstrual irregularity and infertility.
Management
- Low energy and weight reducing diet is given to the patient of obese type II diabetes mellitus.
- Nonobese type II diabetes should have to maintain their weight, so they have to take weight maintenance diet.
These drugs are used in patients of Type II diabetes mellitus (NIDDM) who do not respond to dietary management and who would otherwise require treatment with insulin in later situation, so they are also used as adjuvant drugs to insulin in overweight diabetes patients.
Insulin secretagogues, i.e. drugs increasing secretion of insulin
- Sulfonyl ureas
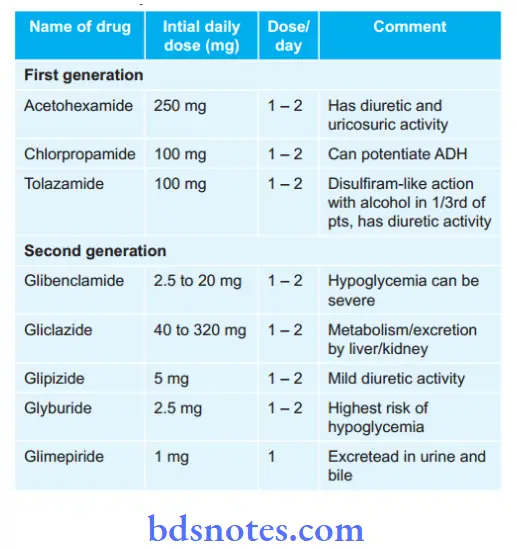
Meglitinides
- Repaglinide, i.e. 0.5 to 4 mg three times a day
- Netaglinide, i.e. 60 to 120 mg three times a day 15 to 30 min before each meal
- Voglibose, i.e. 0.2 to 0.3 mg, 15 to 30 min before each meal.
- Insulin sensitizers, i.e.drugs sensitizing action of insulin and overcome insulin resistance
- Biguanides, i.e. metformin should be given 1.5 to 2.5gm/day in three divided doses after meals.
- Thiozolidinediones, i.e.Rosiglitazone should be given 2 to 8mg or pioglitazone 15 to 45 mg in a single or two divided doses.
They can be combined with sulfonyl ureas or metformin. - Alpha-glucosidase inhibitors, i.e. Acarbose 25 to 100 mg
TDS or Voglibose 0.2 to 5 mg TDS taken orally in three main meals.
It can be given in combination with metformin 500 mg for increased effiency. - DPP 4 inhibitor: Vildagliptin 50 to 100 mg daily in two dived doses with meals ot saxagliptin 2.5 to 5 mg OD.
- Pramlinide: Initial dose is 15μg before each meals in Type I diabetes mellitus and 60 μg in Type II diabetes mellitus.
Question.33. Write short note on tetany.
Answer: Tetany is a clinical condition with low levels of ionized calcium causing increased neuromuscular excitability.
Etiology
Low levels of calcium, potassium, magnesium causes tetany.
- Hypocalcemia: This is due to following factors, i.e. malabsorption of calcium, osteomalacia, hypoparathyroidism,acute pancreatitis, anticonvulsant drugs.
- Hypokalemia: This is caused due to repeated vomiting,excessive intake of alkali, due to acute anion load, primary hyperaldosteronism, due to acute anion load.
- Acute hypocalcemia is caused by sepsis, burns, alkalosis,parathyroid surgery, malignancy, hypomagnesemia, etc.
Clinical Features
- In children there is presence of triad of symptoms, i.e.
carpopedal spasm, stridor and convulsion. - In carpopedal spasm the hands adopt a posture in which flxion occurs at metacarpophalangeal joint and extension at interphalangeal joint and opposition of thumb occur.
- Stridor occurs due to closure of glotts.
- In case of adults tingling sensation occur in peripheral part of limbs and around the mouth.
- Trousseau’s sign: Increasing the blood pressure by the infltion of sphygmomanometer cuf at above the systolic level leads to carpopedal spasm in 2 to 5 minutes.
Chvostek’s sign: Tapping at the facial nerve especially at angle of mandible leads to twitching of facial muscles.
Management
In management etiological factor leading to tetany is eliminated and hypocalcemia and alkalosis should be treated.
Treatment Of Hypocalcemia
10% calcium gluconate 20 mL IM is given. For long lasting effct 10 mL of drug is given additionally.
Treatment Of Alkalosis
- If vomiting is present IV isotonic saline should be given.
- If alkali is the etiological factor, alkalis should be withdrawn, after withdrawal if effect is not proper ammonium chloride 2 gm orally is given after every 4 hours.
- If hyperventilation is the etiological factor, patient is asked to inhale 5% carbon dioxide in oxygen.
Question.34. What are the non-communicable diseases. Write down the diagnostic criteria of diabetes mellitus,complication and management of type-2 diabetes mellitus.
Answer.
Noncommunicable disease is a medical condition or
disease that is noninfectious or nontransmissible.
Noncommunicable disease can refer to chronic diseases which last for long periods of time and progress slowly.
The most noncommunicable diseases are obesity,diabetes, cancer, cardiovascular, chronic respiratory and neurological diseases.
Diagnosis
Diagnosis is based on symptoms, signs and laboratory tests.
In presence ofsigns and symptoms confimation is done by fiding random blood glucose higher than 200 mg/dL.
Investigations
- Blood sugar estimation: Both fasting and postprandial (2 hours after a meal) levels of blood sugar be estimated.
Mean value of blood sugar in healthy adults is 70 to 80 mg%. When fasting blood sugar level exceeds 110 mg% diagnosis is clear.
Postprandial blood sugar level is further screening test, if value exceeds 120 mg% it is strongly suggestive of diabetes mellitus.
Random blood sugar estimation is not of much help as screening test.
Value exceeding 160 mg% in presence of glycosuria is suggestive but values about 200 mg% is diagnostic. - Oral glucose tolerance test: In this fist sample is taken after an overnight fast of 8 hours following which patient is given glucose 1g/kg body weight.
Blood is then collected at 30, 60, 120 and 180 minutes.
In diminished glucose tolerance, level of blood glucose is raised at 180 minutes. - Glycosylated hemoglobin: It measures the longterm glycemic control.
Slow nonenzymatic attachment of glucose to hemoglobin result in formation of glycosylated hemoglobin. - Microalbumin: Patients with microalbumineria are on greater risk in developing kidney failure as well as cardiovascular damage.
- Urine protein/creatinine ratio: It provides information of proteinuria in patients with diabetic nephropathy.
More is the ratio greater is the damage. - Insulin levels: Elevated blood glucose levels with low insulin levels indicate insufficient insulin levels for adequate control of blood glucose.
High insulin levels with low blood glucose indicate change in dosage of drug. - Insulin antibody test: In this there is quantitative determination of antibodies against insulin in serum.
- GAD 65 antibody: These antibodies are common in newly diagnosed diabetic patient and often appear years before clinical onset in the disease. Presence of this antibody is the strong predictive marker for onset of type I diabetes mellitus.
Criterias Given By WHo In 1999
- Presence of classic symptoms of diabetes and causal plasma glucose greater than or equal to 200 mg/dL.
Causal is any time of day without regard to time since last meal.
Classic symptoms of diabetes include polyuria, polydypsia and unexplained weight loss.
Or - Fasting plasma glucose greater than or equal to 126 mg/dL.
Fasting is defied as no caloric intake for 8 hours.
Or - Twohoursplasmaglucosegreaterthanorequalto200 mg/dL during an oral glucose tolerance test.
Test is performed as described by World Health Organization by using glucose load containing equivalent of 75 gm anhydrous glucose dissolved in water.
In absence of unequivocal hyperglycemia with acute metabolic decompensation above criterias are confimed by repeated testing on other days.
Complications
Acute Or Immediate Complications
- Diabetic ketoacidosis or coma
- Hypoglycemia or hypoglycemic coma
- Nonketotic hyperosmolar diabetic coma
- Lactic acidosis
First two complications occur in Type I diabetes mellitus and other two occur in Type II diabetes mellitus.
Diabetic Ketoacidosis
- It is an exclusive complication of type I diabetes. It can develop in patients with severe insulin defiiency combined with glucagon excess.
Failure to take insulin and exposure to stress are precipitating causes. - As the ketogenesis continues the excess ketone bodies produced cannot be degraded by the muscles and other tissues resulting in ketosis, which manifests as anorexia, nausea, vomiting, deep and fast breathing, mental confusion and coma. However, most of the patients recover.
Hypoglycemia
- It is defied as fall in blood glucose concentration below 3.1 mmol/L.
- It is seen in type I diabetes patients due to excessive administration of insulin, missing a meal or due to stress.
- As the hypoglycemia continues, it can lead to comma,cardiac arrhythmias and is fatal.
- This can lead to worsening of control of diabetes and rebound hyperglycemia.
Nonketotic Hyperosmolar Diabetic Coma
- It is common in type II diabetes mellitus.
- The clinical hallmark is hyperglycemia, hyperosmolality and dehydration without ketoacidosis.
- Precipitating features are infection, myocardial infarction,drugs such as thiazides, steroids, diphenylhydantoin.
- Loss of glucose in urine is so intense that the patient is unable to drink suffient water to maintain urinary flid loss.
- Because of high viscosity of blood, thrombotic and bleeding complications are frequent. Mortality rate is high in this complication.
Lactic Acidosis
- It is seen in type II diabetes mellitus.
- It is caused due to excess lactate production and/or inadequate utilization.
- This can be precipitated by metformin or other systemic disorders such as liver or renal failure, pancreatitis or leukemia.
- Cardiovascular collapse leads to mortality.
Chronic or late-onset complications
These complications are due to changes in small blood vessels i.e.microangiopathy or in large blood vessels, i.e. macroangiopathy.
Microvascular are retinopathy, neuropathy, nephropathy and miscellaneous
Macrovascular are atherosclerosis, hypertension, peripheral vascular disease and diabetic foot ulcer
The chronic complications occur more frequently in Type II diabetes mellitus rather than Type I diabetes mellitus.
Diabetic Retinopathy
- This is the very important cause of blindness in diabetic patients.
- Dilatation of retinal capillaries is earliest sign. Besides these there is also presence of microaneurysms, retinal hemorrhage, neovascularization, hard and soft exudates,vitreous hemorrhage and firosis.
- Frequency, onset and severity of retinopathy vary in diabetic patients.
- Background retinopathy is most common and proliferative retinopathy is less common.
Diabetic Neuropathy
- It can involve any part of nervous system except the brain.
- Neuropathy is an early and common complication which leads to morbidity and disability.
- Poor glycemic control and long duration of diabetes is associated with high incidence of neuropathy.
- Sign and symptoms are of peripheral nervous system.
- Main pathological changes in peripheral nerves are axonal degeneration of myelinated and non-myelinated fiers,
Segmental demyelination, Schwann cell injury.
Diabetic Nephropathy
- This is the most common cause of mortality and morbidity in diabetic patients.
- 40 to 50% of type II diabetes patient develop it and 25% patients with type I diabetes develop end stage renal disease and die of it.
- It is divided into three stages, in fist stage patient is asymptomatic but has high GFR, in next stage there is renal hypertrophy which leads to microalbuminuria.
- In advance stage, patient develop macroproteinuria and passes onto nephrotic syndrome.
- 25% of patients with diabetic nephropathy can go directly at end stage renal disease with hypertension and undergo chronic renal failure.
Miscellaneous
It consists of various infections, gastroparesis, arthropathy.
Atherosclerosis
- In diabetic patient development of athroma is faster as compared to normal individual.
- Hyperlipidemia, decreased HDL levels, increased platelet adhesiveness, obesity and associated hypertension are contributory factors for athrosclerosis.
- Atherosclerosis leads to coronary artery disease, silent myocardial infarction, cerebral stroke and gangrene of toes and feet.
Diabetic Foot Ulcer
- This is the frequent site of complication in diabetes.
- Pathogenic components of diabetic foot are neuropathy,peripheral vascular disease causing ischemia and secondary infection causing ulceration.
Management
- Low energy and weight reducing diet is given to the patient of obese type II diabetes mellitus.
- Nonobese type II diabetes should have to maintain their weight, so they have to take weight maintenance diet.
These drugs are used in patients of Type II diabetes mellitus (NIDDM) who do not respond to dietary management and who would otherwise require treatment with insulin in later situation, so they are also used as adjuvant drugs to insulin in overweight diabetes patients.
Insulin secretagogues, i.e. drugs increasing secretion of insulin
- Sulfonyl ureas
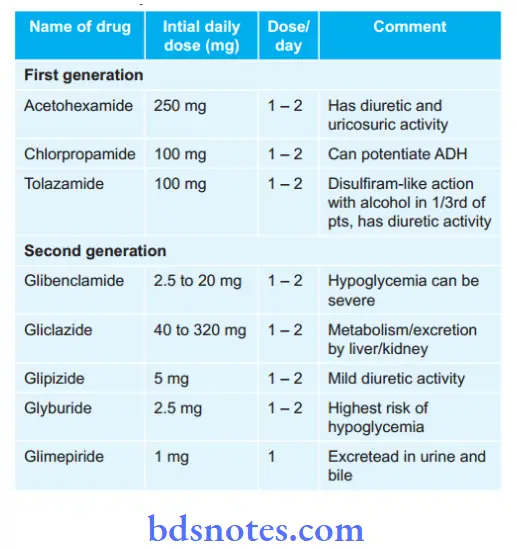
Question.35. Write diagnosis, clinical features and complications of diabetes mellitus.
Answer. Diagnosis is based on investigations,
Investigations
- Blood sugar estimation: Both fasting and postprandial (2 hours after a meal) levels of blood sugar be estimated.
Mean value of blood sugar in healthy adults is 70 to 80 mg%. When fasting blood sugar level exceeds 110 mg% diagnosis is clear.
Postprandial blood sugar level is further screening test, if value exceeds 120 mg% it is strongly suggestive of diabetes mellitus.
Random blood sugar estimation is not of much help as screening test.
Value exceeding 160 mg% in presence of glycosuria is suggestive but values about 200 mg% is diagnostic. - Oral glucose tolerance test: In this fist sample is taken after an overnight fast of 8 hours following which patient is given glucose 1 g/kg body weight.
Blood is then collected at 30, 60, 120 and 180 minutes. In diminished glucose tolerance, level of blood glucose is raised at 180 minutes. - Glycosylated hemoglobin: It measures the longterm glycemic control. Slow nonenzymatic attachment of glucose to hemoglobin result in formation of glycosylated hemoglobin.
- Microalbumin: Patients with microalbuminria are on greater risk in developing kidney failure as well as cardiovascular damage.
- Urine protein/Creatinine ratio: It provides information of proteinuria in patients with diabetic nephropathy. More is the ratio greater is the damage.
- Insulin levels: Elevated blood glucose levels with low insulin levels indicate insufficient insulin levels for adequate control of blood glucose.
High insulin levels with low blood glucose indicate change in dosage of drug. - Insulin antibody test: In this there is quantitative determination of antibodies against insulin in serum.
- GAD 65 antibody: These antibodies are common in newly diagnosed diabetic patient and often appear years before clinical onset in the disease. Presence of this antibody is the strong predictive marker for onset of type I diabetes mellitus.
Diagnosis
Diagnosis is based on symptoms, signs and laboratory tests.
In presence ofsigns and symptoms confimation is done by fiding random blood glucose higher than 200 mg/dL.
Investigations
- Blood sugar estimation: Both fasting and postprandial (2 hours after a meal) levels of blood sugar be estimated.
Mean value of blood sugar in healthy adults is 70 to 80 mg%. When fasting blood sugar level exceeds 110 mg% diagnosis is clear.
Postprandial blood sugar level is further screening test, if value exceeds 120 mg% it is strongly suggestive of diabetes mellitus.
Random blood sugar estimation is not of much help as screening test.
Value exceeding 160 mg% in presence of glycosuria is suggestive but values about 200 mg% is diagnostic. - Oral glucose tolerance test: In this fist sample is taken after an overnight fast of 8 hours following which patient is given glucose 1g/kg body weight.
Blood is then collected at 30, 60, 120 and 180 minutes.
In diminished glucose tolerance, level of blood glucose is raised at 180 minutes. - Glycosylated hemoglobin: It measures the longterm glycemic control.
Slow nonenzymatic attachment of glucose to hemoglobin result in formation of glycosylated hemoglobin. - Microalbumin: Patients with microalbumineria are on greater risk in developing kidney failure as well as cardiovascular damage.
- Urine protein/creatinine ratio: It provides information of proteinuria in patients with diabetic nephropathy.
More is the ratio greater is the damage. - Insulin levels: Elevated blood glucose levels with low insulin levels indicate insufficient insulin levels for adequate control of blood glucose.
High insulin levels with low blood glucose indicate change in dosage of drug. - Insulin antibody test: In this there is quantitative determination of antibodies against insulin in serum.
- GAD 65 antibody: These antibodies are common in newly diagnosed diabetic patient and often appear years before clinical onset in the disease. Presence of this antibody is the strong predictive marker for onset of type I diabetes mellitus.
Criterias Given By WHo In 1999
- Presence of classic symptoms of diabetes and causal plasma glucose greater than or equal to 200 mg/dL.
Causal is any time of day without regard to time since last meal.
Classic symptoms of diabetes include polyuria, polydypsia and unexplained weight loss.
Or - Fasting plasma glucose greater than or equal to 126 mg/dL.
Fasting is defied as no caloric intake for 8 hours.
Or - Twohoursplasmaglucosegreaterthanorequalto200 mg/dL during an oral glucose tolerance test.
Test is performed as described by World Health Organization by using glucose load containing equivalent of 75 gm anhydrous glucose dissolved in water.
In absence of unequivocal hyperglycemia with acute metabolic decompensation above criterias are confimed by repeated testing on other days.
clinical Features
In type I diabetes Mellitus
Symptoms
- Polydypsia, polyuria and polyphagia
- Weight loss
- Weakness and lassitude.
Sign
- Severe emaciation with wastening of muscles
- Ribs are prominent.
- In such patients if diabetic ketoacidosis is severe patient develop mental apathy, confusion and undergo coma.
In type II diabetes Mellitus
Symptoms
Patient remains asymptomatic in the beginning. Disease is detected during routine check up.
Sign
In this multiple systems are affcted, so considering this various signs are:
- Eyes: Errors of refraction leads to frequent change in spectacles, premature formation of cataract, retinopathy,recurrent sty.
- Skin: Abscess, carbuncle, boils, nonhealing wounds.
- Gastrointestinal tract: Chronic diarrhea, malabsorption and dilatation of stomach.
- Cardiovascular system: Hypertension, ischemic heart disease, diabetic foot, cold extremities.
- Respiratory system: Pneumonia, tuberculosis and lung abscess.
- Nervous system: Autonomic neuropathy and peripheral neuritis.
- Urinary tract: Nephrotic syndrome, urinary tract infection.
- Genital tract: Pruritis vulvae, menstrual irregularity and infertility.
Complications
Acute Or Immediate Complications
- Diabetic ketoacidosis or coma
- Hypoglycemia or hypoglycemic coma
- Nonketotic hyperosmolar diabetic coma
- Lactic acidosis
First two complications occur in Type I diabetes mellitus and other two occur in Type II diabetes mellitus.
Diabetic Ketoacidosis
- It is an exclusive complication of type I diabetes. It can develop in patients with severe insulin defiiency combined with glucagon excess.
Failure to take insulin and exposure to stress are precipitating causes. - As the ketogenesis continues the excess ketone bodies produced cannot be degraded by the muscles and other tissues resulting in ketosis, which manifests as anorexia, nausea, vomiting, deep and fast breathing, mental confusion and coma. However, most of the patients recover.
Hypoglycemia
- It is defied as fall in blood glucose concentration below 3.1 mmol/L.
- It is seen in type I diabetes patients due to excessive administration of insulin, missing a meal or due to stress.
- As the hypoglycemia continues, it can lead to comma,cardiac arrhythmias and is fatal.
- This can lead to worsening of control of diabetes and rebound hyperglycemia.
Nonketotic Hyperosmolar Diabetic Coma
- It is common in type II diabetes mellitus.
- The clinical hallmark is hyperglycemia, hyperosmolality and dehydration without ketoacidosis.
- Precipitating features are infection, myocardial infarction,drugs such as thiazides, steroids, diphenylhydantoin.
- Loss of glucose in urine is so intense that the patient is unable to drink suffient water to maintain urinary flid loss.
- Because of high viscosity of blood, thrombotic and bleeding complications are frequent. Mortality rate is high in this complication.
Lactic Acidosis
- It is seen in type II diabetes mellitus.
- It is caused due to excess lactate production and/or inadequate utilization.
- This can be precipitated by metformin or other systemic disorders such as liver or renal failure, pancreatitis or leukemia.
- Cardiovascular collapse leads to mortality.
Chronic or late-onset complications
These complications are due to changes in small blood vessels i.e.microangiopathy or in large blood vessels, i.e. macroangiopathy.
Microvascular are retinopathy, neuropathy, nephropathy and miscellaneous
Macrovascular are atherosclerosis, hypertension, peripheral vascular disease and diabetic foot ulcer
The chronic complications occur more frequently in Type II diabetes mellitus rather than Type I diabetes mellitus.
Diabetic Retinopathy
- This is the very important cause of blindness in diabetic patients.
- Dilatation of retinal capillaries is earliest sign. Besides these there is also presence of microaneurysms, retinal hemorrhage, neovascularization, hard and soft exudates,vitreous hemorrhage and firosis.
- Frequency, onset and severity of retinopathy vary in diabetic patients.
- Background retinopathy is most common and proliferative retinopathy is less common.
Diabetic Neuropathy
- It can involve any part of nervous system except the brain.
- Neuropathy is an early and common complication which leads to morbidity and disability.
- Poor glycemic control and long duration of diabetes is associated with high incidence of neuropathy.
- Sign and symptoms are of peripheral nervous system.
- Main pathological changes in peripheral nerves are axonal degeneration of myelinated and non-myelinated fiers,
Segmental demyelination, Schwann cell injury.
Diabetic Nephropathy
- This is the most common cause of mortality and morbidity in diabetic patients.
- 40 to 50% of type II diabetes patient develop it and 25% patients with type I diabetes develop end stage renal disease and die of it.
- It is divided into three stages, in fist stage patient is asymptomatic but has high GFR, in next stage there is renal hypertrophy which leads to microalbuminuria.
- In advance stage, patient develop macroproteinuria and passes onto nephrotic syndrome.
- 25% of patients with diabetic nephropathy can go directly at end stage renal disease with hypertension and undergo chronic renal failure.
Miscellaneous
It consists of various infections, gastroparesis, arthropathy.
Atherosclerosis
- In diabetic patient development of athroma is faster as compared to normal individual.
- Hyperlipidemia, decreased HDL levels, increased platelet adhesiveness, obesity and associated hypertension are contributory factors for athrosclerosis.
- Atherosclerosis leads to coronary artery disease, silent myocardial infarction, cerebral stroke and gangrene of toes and feet.
Diabetic Foot Ulcer
- This is the frequent site of complication in diabetes.
- Pathogenic components of diabetic foot are neuropathy,peripheral vascular disease causing ischemia and secondary infection causing ulceration.

Leave a Reply