Neurological Injuries
Question.1. Write short note on trigeminal neuralgia.
Or
Answer briefly on trigeminal neuralgia.
Or
Write in short about trigeminal neuralgia.
Or
Discuss the treatment of trigeminal neuralgia.
Or
Write short answer on trigeminal neuralgia.
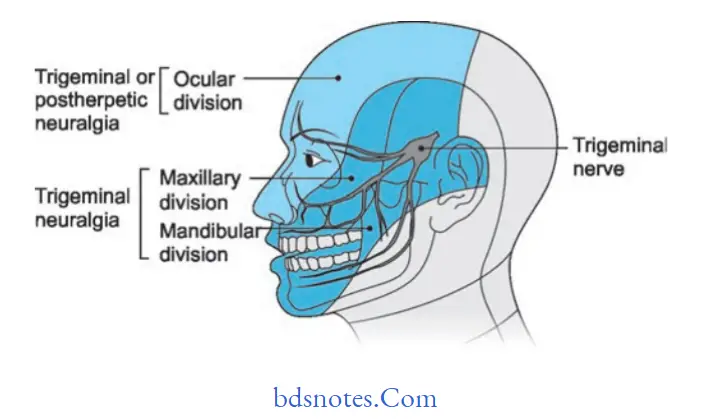
Answer. It is also called as Tic Douloureux, trifacial neuralgia or Fothergill’s disease.
Trigeminal neuralgia is an extremely painful condition along the distribution of any branches of the trigeminal nerve.
Trigeminal neuralgia Etiology
- Dental pathosis at times leads to trigeminal neuralgia.
- Due to excessive traction divisions of trigeminal nerve are affcted which leads to trigeminal neuralgia.
- Allergic and hypersensitivity reaction may lead to trigeminal neuralgia.
- Mechanical factors such as pressure caused by aneurysms of internal carotid artery.
- Secondary lesions such as carcinomas ofmaxillary antrum,carcinoma of the nasopharynx leads to trigeminal neuralgia.
Read And Learn More: General Surgery Question And Answers
Trigeminal neuralgia Clinical Features
- It occurs in middle age and older people.
- Female predilection is seen.
- Pain is paroxysmal in nature, last for few minutes and is of extreme intensity.
- Pain is usually limited to the distribution of trigeminal nerve and is unilateral. At times pain is bilateral too.
- Pain is provoked by obvious stimuli to the face. A touch, a draft of air, any movement of face as in talking, chewing,yawning or swallowing.
- Pain attacks are precipitated by touching some “trigger zone” on the face, i.e. vermilion border of lip, the ala of nose, the cheek, and around the eyes.
Patient usually avoid touching of skin over these areas.
Patient has unshaven face, avoid brushing, and undergo dental extraction. - Objective signs or sensory loss are demonstrated on examination.
- Onset of pain is sudden and tends to persist for weeks or months before remitting spontaneously.
Trigeminal neuralgia Treatment
Trigeminal neuralgia Medical treatment
- Carbamazepine (tegretol) has a special effct on the paroxysmal pain. This is considered to be the best conservative treatment for trigeminal neuralgia.
As an initial dose, 100 mg twice daily till relief is established. - Dilantin: Diphenylhydantoin, an anticonvulsant drug has been recommended, effective when given orally, 300 to 400 mg/day.
- Recently, baclofen an antispastic drug is also being used.
- A combination of dilantin and carbamazepine may also be given.
- Clonazepam an antiepileptic found to be useful.
- Anti-inflammatory agents like indomethacin and short course of steroids have been found to be useful.
Trigeminal neuralgia Surgical treatment
- Infection of the nerve with an anesthetic solution: Local anesthetics of various types are injected near the peripheral branches of the trigeminal nerve to serve to provide temporary relief from pain.
- Injection ofthe nerve with alcohol:
- The most popular material, alcohol, can be placed directly into the area where a nerve exits from the skull or more peripherally.
- When alcohol contracts the nerve, neurolysis occurs distal to the injection site.
- Generally, 95% alcohol is used or procaine or monocaine 2%, chloroform 5%, absolute alcohol 70%, and Ringer’s solution 23% can also be used.
- Nerve sectioning and nerve evolution (peripheral neurectomy):
This procedure is more lasting and effective than an injection with alcohol.
Peripheral neurectomy results in high degree of success in the elimination of pain. - Electrocoagulation of gasserian ganglion: Diathermy apparatus is placed in the gasserian ganglion to coagulate and destroy it.
- Percutaneous radiofrequency trigeminal neurolysis: It is performed by insertion of temperature monitoring electrode through foramen ovale into trigeminal ganglion.
Advantages include decreased mortality and morbidity and permanent cure. - Rhizotomy: Actual cutting of trigeminal sensory root results in permanent anesthesia in most patients.
- Bulbar trigeminal tractotomy: The descending tract of the trigeminal nerve may be cut in the area of medulla oblongata to induce loss of pain and temperature sensation.
Question.2. Describe in brief Bell’s palsy.
Or
Write short note on bell’s palsy.
Answer. It is also called as 7th nerve paraplegia or facial palsy.
Bell’s palsy Etiology
- Cold: It occurs after exposure to cold.
- Trauma: Extraction of teeth or injection of local anesthetic may damage the nerve and causes subsequent paralysis.
- Surgical procedure: Such as removal of parotid gland tumor in which the facial nerve is sectioned can also cause facial
paralysis. - Tumors: Tumors of the cranial base, parapharyngeal space and infratemporal fossa cause facial nerve palsy.
- Familial: Familial and hereditary occurrence is also reported in case of Bell’s palsy.
- Facial canal and middle ear neoplasms may lead to Bell’s palsy.
Bell’s palsy Clinical Features
- It is in older age group.
- Female predilection is most common.
- There is presence of paralysis over one side of the face.
- Drooping of angle of mouth is present over the affected side and saliva is drooling from the affected side.
- Patient is unable to raise the eyebrow of the affected side.
- Patient is unable to close the eye over affected side and tears continuously roll down.
- Eyeball roll upward when attmpted to close the eye, this is known as
- Bell’s phenomenon.
- Over the affected side, patient has lost the taste sensation.
- Patient complaints of pain in or behind the ear.
- Presence of numbness over the affected side of face.
- Patient has mask-like appearance when he/she tries to smile.
- There is difficulty in blowing or clenching.
- Obliteration of nasolabial fold
- Presence of wide palpebral fisure
- Presence of epiphora.
Bell’s palsy Treatment
Bell’s palsy Medicinal treatment
- Patients with Bell’s palsy have excellent prognosis.
- Treatment of Bell’s palsy is controversial as spontaneous recovery is present.
- Treatment is given to the patients who have onset of paralysis under 1–4 days of an initial visit.
- Corticosteroids, i.e. prednisolone 1 mg/kg or 60 mg per day for 6 days followed by the taper of 10 days.
- Anti-viral drugs can be given in the patients in which bell’s palsy is associated with herpes infection.
- In Bell’s palsy eye of the patient is at risk for drying which cause corneal abrasion and corneal ulcer.
Eye care consists of inducing the artifiial tears in daytime along with eyeglasses.
At night eye lubricant can be used.
Bell’s palsy Surgical treatment
- Surgical treatment for Bell’s palsy is surgical decompression and anastomosis of the nerve.
In this facial and hypoglossal nerves get anastomosed which helps in restoring partial function. - Nerve grafting using greater auricular nerve, sural nerve, lateral cutaneous nerve of thigh or hypoglossal nerve.
- Suspension of angle of mouth to zygomatic bone using temporal fascia sling.
- Lateral tarsorrhaphy: This prevent corneal ulceration
- Medial canthus reconstruction: To decrease epiphora
- Cross facial nerve transplantation from opposite side using its insignifiant branches.
- Dynamic neurovascular muscle graft
- Upper lid gold weights to protect cornea.
Question.3. Discuss etiology and management of injury of facial nerve.
Answer. Injuries of facial nerve causes facial palsy or Bell’s palsy.
Etiology Of Facial Paralysis
- Congenital: Mobius syndrome (Uncommon and poorly understood)
- Traumatic:
- Birth injury
- Iatrogenic injury at the time of surgeries, e.g. surgery for parotid gland surgery etc.
- Blunt or penetrating trauma to nerve.
- Fracture of the temporal bone can lead to facial nerve injury.
- Infections
- Virally mediated diseases, i.e. herpes zoster, mumps,coxsackie virus, and mononucleosis.
- Bacterial infections, i.e. sequelae to otitis media, Lyme disease, mastoiditis.
- Inflammatory conditions: Sarcoidosis
- Neoplastic: Tumors of the parotid gland (typically malignant tumors)
- Facial nerve schwannomas
- Acoustic neuromas
- Neoplasms of the brain such as brainstem tumors.
- Idiopathic:
- Bell`s palsy is most common type of facial paralysis.
- It occurs due to virally induced inflammation of the nerve resulting in compromise of the function of nerve, swelling and vascular supply to the nerve.
- Melkersson—Rosenthal syndrome
- Myasthenia gravis.
Management Of Facial Paralysis
Facial nerve repair can be done by following surgical methods,i.e.
- Direct repair
- Cable nerve grafting
- Nerve substitution techniques.
Direct repair Of Facial Paralysis
Preoperative Details
- Direct repair of the facial nerve is the best method to rehabilitate the paralyzed face.
By this method,there are chances of restoring spontaneous, emotional expression to the face. - Direct repair is indicated in cases where the length of nerve is adequate and reapproximation of the nerve is possible without tension along the nerve.
- It involves restoring the continuity of both ends of the nerve directly by using sutures.
- For the successful repair of nerve, it is mandatory that functional motor unit be available to receive the innervations, i.e. facial musculature should not have undergone excessive atrophy and there should be no firosis at the motor end plate which prevent reinnervation.
Technique of Direct Repair
- Parotidectomy incision is given and the nerve is exposed.
Identify the nerve and its branches.
If the intratemporal portion of the nerve is injured, this area is exposed with the help of a mastoidectomy. - As identification is over, the nerve is followed distally as required.
- Handle the nerve as traumatically as possible.
Surgery should be performed by using a surgical microscope.
This allows precise alignment of the nerve ends. - 2 to 3 sutures should be placed by using 8-0 to l0-0 fie monofiament sutures.
Sutures are usually placed through the epineurium. - Perineurial, endoneurial and interfascicular suturing should also be done.
- Most important relationship is the size match of endoneurial surfaces. This must be inspected with magnification, and if a mismatch is seen, then one end may be trimmed in a beveled fashion to obtain a bettr surface area.
Cable nerve Grafting
If sufficient length is not present to approximate the nerve primarily, cable grafting is done.
Patient must be informed about the operation of the donor site.
Commonly used nerves are greater auricular nerve, sural nerve, lateral femoral cutaneous nerve, etc.
Cable nerve Grafting Technique
- Great auricular nerve is located by drawing a line between angle of jaw and mastoid tip.
Bisect this line at a right angle by great auricular nerve as it passes around the posterior border of the sternocleidomastoid muscle just behind the external jugular vein. - Sural nerve may be located between lateral malleolus and Achilles tendon.
It lies deep or posterior to the saphenous vein.
Sural nerve then runs superiorly up to back of lower leg in a subcutaneous plane until it descends between the two heads of the gastrocnemius toward the popliteal fossa and its origin of the tibial nerve.
Sural nerve can be harvested either by giving a single long incision from the ankle to popliteal fossa (depending on the length of nerve required) or a series of shorter transverse incisions.
The nerve may be dissected under direct vision with the single incision, or by employing a fascia stripper and making the stepwise incisions. Nerve grafting should be done same as for primary repair.
In cable grafting, it may be helpful to obtain enough nerve graft length to allow the graft to have some redundancy between the ends of facial nerve.
This provides a C or S shape and ensures tension-free coaptation. - Graft should lie in healthy and vascularized recipient site which is free of scar tissue.
- Epineurium should be intact and 10-0 sutures may be used to repair the nerve without tension.
A soft silicone tube can be used which surround the anastomotic site to prevent in growth of scar tissue inside the surgical site and also to keep cut axons approximated.
Nerve Substitution Techniques
There are two types of nerve substitution techniques:
1. Hypoglossal facial anastomosis
2. Cross-face grafting
Hypoglossal Facial nerve anastomosis
It is the most standard procedure to reanimate the face when proximal end of the facial nerve is not present or has undergone degeneration and the peripheral aspect of nerve is still viable.
This procedure can be done as a primary procedure, i.e it can be done along with the surgical procedure that lead to the sacrifice of the facial nerve or as a secondary procedure, i.e. when facial nerve paralysis is noticed postoperatively
Hypoglossal Facial nerve anastomosis Technique
- A parotidectomy incision is given and facial nerve is exposed.
Identify the nerve as it exits the stylomastoid foramen.
It is sharply transected here in this region. - Identify the hypoglossal nerve in the neck by following the posterior belly of the digastric muscle to the hyoid bone.
Nerve is followed distally to gain length for the anastomosis. - Transect descendants hypoglossal to gain length and mobilization for the anastomosis.
- Transect the hypoglossal nerve distally and approximate it to the facial nerve passing medial or lateral to the digastric muscle. The nerve ends are then grafted together.
Cross Face Grafting
- This procedure attmpts to connect the branches of paralyzed facial nerve to the corresponding branches on the normal side.
- It is done in cases where the proximal end of the nerve is not available for repair but the motor end plates on the
paralyzed side should be functional for the success of this procedure. - This procedure is not possible in cases in which the nerve has been paralyzed for over a year.
Cross Face Grafting Technique
- Very commonly sural nerve is used to carry nerve to opposite side as it consists of adequate length to thread across from one end of the face to another.
It is indicated in cases where multiple branches are to be anastomosed.
Great auricular nerve may be used in cases when a single nerve is grafted. - Dissect affected side first and identify all the branches. If multiple branches should be grafted they are identified and exposed a litte beyond the parotid gland.
- Expose the normal facial nerve and the donors should be taken from distal border of the parotid gland.
- Now identify sural nerve and the branches should be tunneled across the face. First suture the nerve graft to the normal side and then to the chosen branch on the paralyzed side.
- For good healing meticulous hemostasis and the use of drains to prevent the formation of hematoma is essential.
- Some iatrogenic weakness is expected on the donor side after this procedure and the patient must be warned of this before going for procedure.
Postoperative Care of the Patient
- As return of function takes few months with each of these procedures, attntion to patient care should be given such as eye protection.
- Various adjunctive procedures, i.e. gold weight eyelid implants or brow lift may be considered.
- Reexploration and revision should be done ifimprovement is not seen in one year following grafting.
Question.4. Discuss the management of head injury.
Answer. Initial assessment of head injuries must follow advanced trauma and life support (ATLS) guidelines with an initial primary survey, then *resuscitation followed by secondary survey then defiite management like: airway, breathing, circulation, disability and exposure.
Important Histories of Head injury
- Period of loss of unconsciousness
- Period of post-traumatic amnesia
- Cause and circumstances of injury
- Presence of headache and vomiting.
Head injury Physical examination includes
- Thorough general examination.
- Local examination for evidence of injury, skull fractures.
- Determination of conscious level by Glasgow coma scale.
Head injury Investigations
- X-ray skull: To look for fracture, relative position ofcalcifid pineal gland, presence of intracranial air.
- Serum electrolyte measurement is done
- Blood grouping and cross matching of blood is done.
- CT scan: Plain (not contrast) to look for cerebral edema,hematoma, midline shift, fractures, ventricles, brainstem injury.
- Carotid arteriography
- Investigations for other injuries such as ultrasound of abdomen.
- Monitoring of intracranial pressure.
Head injury Glasgow Coma Scale
Eye-opening
- Spontaneous 4
- To speech 3
- To pain 2
- Nil 1
Best Motor response
- Obeys command 6
- Localizes pain 5
- Withdrawal to pain 4
- Flexion to pain 3
- Extension to pain 2
- Nil 1
Verbal response
- Oriented 5
- Confused 4
- Inappropriate words 3
- Incomprehensible 2
- Nil 1
Total score is 15
Mild head injury score 13 to 15
Moderate head injury score 9 to 12
Severe head injury score less than 8 (3 to 8)
Any patient who has a coma score of 7 or less than 7 is said to be in coma.
Pupillary response should be elicitated to determine whether there is incipient transtentorial habitat, with Oculomotorpalsy and responses recorded.
Head injury General Management
- Management ofhead injuries includes ventilation, surgery,
ICU management of intracranial pressure, cerebral perfusion pressure and oxygenation. - Management of patients having head injury is based on
Glasgow coma scale following the resuscitation. - Patients with mild injury, i.e. having Glasgow comma scale of 14 to 15 should be admittd to the ward where thorough neurological examinations are performed.
- If patient with mild head injury subsequently deteriorate neurologically, CT scan of patient’s head should be done and local neurosurgical unit should be contacted.
- Mild head injury patients should remain under observation until complete neurological recovery occur. Such patients are discharged to the responsible adult which can take good care of such patient at home for few days.
- Patients with Glasgow comma scale of 13 or less should undergo for CT scan of their head. If there is presence of acute lesion on CT scan or there is presence of diffse cerebral edema should referred to local neurosurgical unit.
CT scan should also be sent to the unit. A provisional radiography report should also be sent to referring hospital. - If there is presence of compound depressed skull fracture,severely depressed fracture, CSF otorrhea and rhinorrhea patient should be referred to neurosurgical unit.
- Airways are protected by using mouth gag, endotracheal intubation or tracheostomy whenever required.
- Throat suction, bladder and bowel care as well as good nursing is essential.
- After evacuation of hematoma patient should be admittd to ICU and ventilated to a PCO 2 of 4 to 4.5 Kpa.
- A central line, arterial line and urinary catheter should be inserted.
- Head of bed should be positioned 40 degrees up and patient is given analgesia (Fentanyl)
- IV fluids are administered should be isotonic. It is administered till nasogastric tube is inserted for feeding.
- ICP monitor should be inserted intraparenchymally to measure ICP and CPP (ideally should be < 25 mm Hg and CPP should be about 70 mm Hg) If CPP is low, ionotropic agent should be used.
- Mannitol or frusemide could lower the ICP if it is not controlled by these agents then EEG burst suppression therapy with a barbiturates, ventriculator or lumber CSF drainage to be considered.
- Antibiotics like penicillin, ampicillin are given to prevent risk of meningitis.
Surgical Management
- Burr hole is made and hematoma is evacuated.
- Surgery is done in case when:
- Consciousness is decreasing continuously.
- Pupil becomes fied or dilated.
- Pulse rate becomes less than 60/minute.
Surgical Management
- Craniotomy is done and cranial flp is raised. Clot is evacuated applying hitch stitches between dural layer and scalp.
Question.5. Write short note on danger area of face.
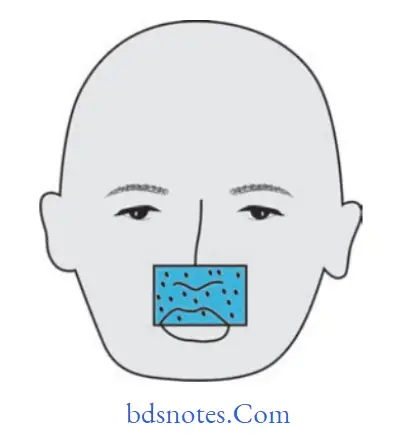
Answer. Dangerous area of face extends from corner of mouth to bridge of nose. It is basically the area of upper lip and lower part of nose.
- Infection from this area spreads through deep facial vein to pterygoid plexus and from pterygoid plexus to communicating vein and from communicating vein to cavernous sinus which can lead to life-threatening cavernous sinus thrombosis.
- Mainly due to the special nature of blood supply to human nose and the surrounding area there is possibility for retrograde infections from nose to spread to brain.
- One of the misconception is present that veins of head does not have one way valves as it is present in other veins of circulatory system. Reality is venous valves are not absent but there is communication between facial vein and cavernous sinus and the direction of blood flow which leads to spread of infection from face.
- Boils and pimples present in the area of upper lip and lower part of nose should never be squeezed and pricked by a needle, by doing so the infection spreads to cavernous sinus causing cavernous sinus thrombosis.
Question.6. Write short note on facial palsy.
Or
Write brief note on facial palsy.
Answer. Facial palsy refers to the paralysis of facial muscles.
It is of two types:
- Upper motor neuron palsy
- Lower motor neuron palsy or Bell’s palsy
Upper Motor neuron Palsy
- It affcets mainly muscles of lower part of face and is never complete.
- It is seldom isolated palsy.
- The emotional movements are preserved.
- There is no muscle contracture.
- There is no reaction of degeneration.
- Electromyography and nerve conduction is normal.
lower Motor neuron Palsy or Bell’s Palsy
It is also called as 7th nerve paraplegia or facial palsy.
Bell’s Palsy Etiology
- Cold: It occurs after exposure to cold.
- Trauma: Extraction of teeth or injection of local anesthetic may damage the nerve and causes subsequent paralysis.
- Surgical procedure: Such as removal of parotid gland tumor in which the facial nerve is sectioned can also cause facial paralysis.
- Tumors: Tumors of the cranial base, Parapharyngeal space and infratemporal fossa cause facial nerve palsy.
- Familial: Familial and hereditary occurrence is also reported in case of Bell’s palsy.
Facial canal and middle ear neoplasms may lead to Bell’s palsy.
Bell’s Palsy Clinical Features
- It is in older age group.
- Female predilection is most common.
- There is presence of paralysis over one side of the face.
- Drooping of angle of mouth is present over the affcted side and saliva is drooling from the affcted side.
- Patient is unable to raise the eyebrow of the affcted side.
- Patient is unable to close the eye over affcted side and tears continuously roll down.
- Eyeball rolls upward when attmpted to close the eye, this is known as Bell’s phenomenon.
- Over the affcted side, patient has lost the taste sensation.
- Patient complaints of pain in or behind the ear.
- Presence of numbness over the affcted side of face.
- Patient has mask-like appearance when he/she tries to smile.
- There is diffilty in blowing or clenching
- Obliteration of nasolabial fold
- Presence of wide palpebral fisure
- Presence of Epiphora.
Bell’s Palsy Treatment
Medicinal Treatment
- Patients with Bell’s palsy have excellent prognosis.
Treatment of Bell’s palsy is controversial as spontaneous recovery is present. - Treatment is given to the patients who have onset of paralysis under 1 to 4 days of an initial visit.
- Corticosteroids, i.e. prednisolone 1 mg/kg or 60 mg per day for 6 days followed by the taper of 10 days.
- Antiviral drugs can be given in the patients in which bell’s palsy is associated with herpes infection.
- In Bell’s palsy eye of the patient is at risk for drying which cause corneal abrasion and corneal ulcer.
Eye care consists of inducing the artifiial tears in day-time along with eyeglasses. At night, eye lubricant can be used.
Bell’s Palsy Surgical Treatment
- Surgical treatment for Bell’s palsy is surgical decompression and anastomosis of the nerve.
In this facial and hypoglossal nerve get anastomosed which helps in restoring the partial function. - Nerve grafting using greater auricular nerve, sural nerve,lateral cutaneous nerve of thigh or hypoglossal nerve.
- Suspension of angle of mouth to zygomatic bone using temporal fascia sling.
- Lateral tarsorrhaphy: This prevents corneal ulceration
- Medial canthus reconstruction: To decrease epiphora
- Cross facial nerve transplantation from opposite side using its insignifiant branches
- Dynamic neurovascular muscle graft
- Upper lid gold weights to protect cornea
Question.7. Classifiation of peripheral nerve injuries with methods of treatment of cut injured nerve.
Answer.
Classifiation of Peripheral Nerve Injuries
- Seddon’s Classifiation
- Neurapraxia: It is a temporary physiological paralysis of nerve conduction. Here recovery is complete.
- Axonotmesis: Division of nerve fiers or axons with intact nerve sheath. Reaction of degeneration is distally with near complete recovery.
- Neurotmesis: Here complete division of nerve fiers with sheath occurs. Degeneration occurs proximally up to the fist node of Ranvier as well as distal to the injury. Recovery is incomplete even after nerve suturing. There is complete loss of motor and sensory functions with loss of reflxes. lf the nerve is mixed type other than pure motor or sensory recovery is still poorer.
- Neuromas:
- True neuroma or false neuroma
- End neuroma or side neuroma.
- Sunderland’s classifiation
- Conduction block: Temporary neuronal block
- Axonotmesis but endoneurium is preserved.
- Axonotmesis with disruption of endoneurium, but perineurium is preserved
- Here disruption of endo and perineurium has occurred but endoneurium is intact.
- Neurotmesis with disruption of endoneurium,perineurium and epineurium has occurred.
Treatment of Cut injured nerve
Usually, microscope or loup is used for nerve suturing.
- Epineurorrhaphy: Only epineurium is sutured using interrupted sutures.
- Epi-perineurorrhaphy: Initially, perineural sheath and then epineurium is sutured.
- If nerve is lacerated marker stitches are placed at cut end site to identify the nerve for suturing at later period.
- If nerve suturing fails or it cannot be done, tendon transfer is done at later period after 4 to 6 months.
Nerve suturing can be:
- Primary repair:
- It is done immediately after injury.
- Nerve ends are minimally trimmed very close using a blade.
- Fascicles of the nerve are oriented correctly.
- Two stay sutures are placed to keep the orientation properly.
- Usually, epineural suturing is done using 8 zero polypropylene interrupted sutures.
- 6-8 sutures are placed for large peripheral nerve like median or ulnar nerve.
- For or small nerve like digital nerve, only 2-3 sutures are placed.
- Secondary repair:
- It is done at a later period.
- It is in a pre-existing scar tissue.
- Here fist nerve ends, but proximal and distal are identifid, carefully dissects; adequately.
- Proximal neuroma and distal glioma trimmed for l cm to expose the normal fascicles of nerve ends.
- Often guide sutures of silk may be present which were placed earlier during exploration of trauma.
- Once nerve ends are clean, it is sutured alike primary suturing with stay sutures, with proper alignment of fascicles, followed by epineural suturing.
- Here as epineurium is thicker, suturing is easier.
Question.8. Describe briefly Glasgow coma scale.
Answer. Glasgow coma scale is used in assessment of conscious level.
- It provides a grading of coma by using a numerical scale which allows serial comparison and prognostic information.
- It relates clinical observation under three headings,i.e. motor response, verbal response and eye opening.
- Following is the Glasgow coma scale
Glasgow Coma Scale
- Eye Opening (E):
- Spontaneous 4
- To speech 3
- To pain 2
- Nil 1.
- Motor Response (M):
- Obeys command 6
- Localizes pain 5
- Withdrawal to pain 4
- Flexion to pain 3
- Extension to pain 2
- Nil 1.
- Verbal Response (V):
- Oriented 5
- Confused 4
- Inappropriate words 3
- Incomprehensible 2
- Nil 1.
Coma Score = e + M + V
- Total score is 15
- Mild head injury score 13 to 15
- Moderate head injury score 9 to 12
- Severe head injury less than 8 (3 to 8).
Question.9. Write short note on peripheral nerve injuries.
Answer.
Peripheral Nerve Etiology
- Traumatic: Either closed or open injury
- Inflammatory: Leprosy, diphtheria, herpes zoster
- Lead and arsenical poisoning
- Alcoholism
- Diabetes mellitus
- Vitamin B1 deficiency
- Porphyria
- Neurofibroma and other neural tumors
- Idiopathic.
Peripheral Nerve Clinical Features
- Loss of sensory, motor, autonomous and reflx functions.
- Secondary changes in the skin and joint.
Peripheral Nerve Management
Peripheral Nerve Medicinal
- Steroids: They reduce the edema around nerve and is useful in neurapraxia. Prednisolone 5 to 10 mg is effctive.
- Nerve tonics: Vitamin B
1, B6, B12, they are supposed to facilitate nerve fier regeneration and are useful in cases of neuropraxia and axonotmesis. - In cases with acute neuralgic pain, drugs like carbamazepine or gabapentin can be prescribed. It is purely symptomatic treatment.
- Physiotherapy: Inthe form of electrical nerve stimulation (TENS) and in cases of motor nerve exercises and massage therapy can be given.
Peripheral Nerve Surgical
- Decompression: It is used if nerve compression occurs resulting into neuropraxia.
It is usually done when nerve due to bone deposition in the nerve canal; there is pressure on the nerve leading to neuropraxia. Here,enlargement of the canal boundaries is done to relieve the pressure on the nerve. - Anastomosis: It is microsurgical repair of the severed ends of the nerve. It is useful, when there is no loss of nerve tissue as in accidental clean surgical by transection of the nerve.
- Cross innervation: It is useful when there is motor nerve defiit due to a lesion in the course of the nerve.
In this repair, a nerve is grafted to connect the affcted nerve to the normal functional nerve on the other side of the body using microsurgical repair. - Nerve grafts: It is use of a nerve segment from one part of the body to reconstruct and repair an affcted nerve in some other part using microsurgical technique.
- Glasgow coma scale gives clear idea about neuronal injury.
- Autonomic disturbances with bradycardia, systolic hypertension, deep and slow respiration, Cheyne stokes ventilation.
- Cushing’s triad of raised intracranial pressure is obvious i.e. bradycardia, hypertension and respiratory irregularity.
- Features such as restlessness, irritability, headache,vomiting and progressive deterioration are common.
Question.10. Write briefly on clinical features of head injury.
Answer. The following are the clinical features of head injury:
- Unequal pupil size is potentially a sign of a serious brain injury.
- Symptoms are dependent on the type of traumatic brain injury (diffse or focal) and the part of the brain that is affcted.
- Unconsciousness tends to last longer for people with injuries on the left side of the rain than for those with injuries on the right.
- With mild traumatic brain injury, the patient may remain conscious or may lose consciousness for a few seconds or minutes.
- Other symptoms of mild traumatic brain injury include headache, vomiting, nausea, lack of motor coordination, dizziness, difficulty in balancing, lightheadedness, blurred vision or tired eyes,ringing in the ears, bad taste in the mouth, fatigue or lethargy, and changes in sleep pattrns.
- Cognitive and emotional symptoms include behavioral or mood changes, confusion, and trouble with memory, concentration, attntion, or thinking.
- A person with a moderate or severe traumatic brain injury may have a headache that does not go away, repeated vomiting or nausea, convulsions, an inability to awaken, dilation of one or both pupils, slurred speech, aphasia (word-finding difficulties), dysarthria (muscle weakness that causes disordered speech), weakness or numbness in the limbs, loss of coordination, confusion, restlessness, or agitation.
- Common long-term symptoms of moderate to severe traumatic brain injury are changes in appropriate social behavior, deficits in social judgment, and cognitive changes, especially problems with sustained attention, processing speed, and executive functioning.
- Alexithymia, a deficiency in identifying,understanding, processing, and describing emotions occurs in 60.9% of individuals with traumatic brain injury.
- Cognitive and social deficits have long-term consequences for the daily lives of people with moderate-to-severe traumatic brain injury, but can be improved with appropriate rehabilitation.
- When the pressure within the skull (intracranial pressure) rises too high, it can be deadly.
Signs of increased intracranial pressure include decreasing level of consciousness, paralysis or weakness on one side of the body, and a blown pupil, one that fails to constrict in response to light or is slow to do so. - Cushing’s triad, a slow heart rate with high blood pressure and respiratory depression is a classic manifestation of significantly raised intracranial pressure.
- Anisocoria, unequal pupil size, is another sign of serious traumatic bone injury.
- Abnormal posturing, a characteristic positioning of the limbs caused by severe diffuse injury or high intracranial pressure, is an ominous sign
Question.11. Describe features to extradural hematoma.
Answer. Following are the features to extradural hematoma
- Patient soon regain consciousness and again after 6 to 12-hour start deteriorating (Lucid interval).
- Later the patient presents with confusion, irritability, drowsiness, hemiparesis on same side of the injury.
Initially, pupillary constriction and later pupillary dilatation occurs on the same side, finally becomes totally unconscious—Hutchinson Pupils - Death can occur if immediate surgical intervention is not done.
- Features of raised intracranial pressure such as high blood pressure, bradycardia, vomiting is also seen.
- Occasionally, convulsions may be present.
Wound and hematoma in the temporal region of scalp may be seen. - Glasgow coma scale gives clear idea about neuronal injury.
- Autonomic disturbances with bradycardia, systolic hypertension, deep and slow respiration, CheyneStokes ventilation.
- Cushing’s triad of raised intracranial pressure is obvious, i.e. bradycardia, hypertension, and respiratory irregularity.
- Features such as restlessness, irritability, headache, vomiting, and progressive deterioration are common.
Question.12. Describe the types, pathology, clinical features, and management of peripheral nerve injuries.
Answer.
Peripheral Nerve Pathology
Guillain-Barré Syndrome
- Guillain-Barré syndrome is one of the most common lifethreatening diseases of the peripheral nervous system.
- It is a rapidly progressive acute demyelinating disorder affcting motor axons that results in ascending weakness that may lead to death from failure of respiratory muscles over a period of only several days.
- It appears to be triggered by an infection or a vaccine that breaks down self-tolerance, thereby leading to an autoimmune response.
- Associated infectious agents include Campylobacter jejuni, Epstein-Barr virus, cytomegalovirus, and human immunodeficiency virus.
- The injury is most extensive in the nerve roots and proximal nerve segments and is associated with mononuclear cell infiltrates rich in macrophages.
- Both humoral and cellular immune responses are believed to play a role in the disease process.
Chronic Inflammatory Demyelinating Polyneuropathy
- Chronic inflammatory demyelinating polyneuropathy
(CIDP) typically manifests as a symmetric demyelinating disease. - Both motor and sensory abnormalities are common, such as diffilty in walking, weakness, numbness, and pain or tingling sensations.
- CIDP is immune-mediated and occurs at increased frequency in patients with other immune disorders, such as systemic lupus erythematosus and HIV infection.
- CIDP follows a chronic, relapsing-remitting or progressive course.
- The peripheral nerves show segments of demyelination and remyelination.
- In long-standing cases, chronically regenerating Schwann cells may concentrically wrap around axons in multiple layers in an onion-skin pattrn.
Toxic and Vasculitic Forms of Peripheral neuropathy
- Drugs and environmental toxins that interfere with axonal transport or cytoskeletal function often produce peripheral neuropathies.
The longest axons are most susceptible, so the resulting clinical presentation is often most pronounced in the distal extremities. - Peripheral nerves are often damaged in many different forms of systemic vasculitis including polyarteritis nodosa, Churg-Strauss syndrome, and Wegener granulomatosis.
Overall, peripheral nerve damage is seen in about a third of all patients with vasculitis at the time of presentation.
The most common clinical picture is that of mononeuritis multiplex with a painful asymmetric mixed sensory and motor peripheral neuropathy. Patchy involvement also is apparent at the microscopic level, as single nerves may show considerable interfascicular variation in the degree of axonal damage.
Peripheral Nerve Leprosy
- There is peripheral nerve involvement in both lepromatous and tuberculoid leprosy.
- In lepromatous leprosy, Schwann cells are often invaded by Mycobacterium leprae, which proliferate and eventually infect other cells.
There is evidence of segmental demyelination and remyelination and loss of both myelinated and unmyelinated axons.
As the infection advances, endoneurial fibrosis and multilayered thickening of the perineurial sheaths occur.
Clinically, these patients develop a symmetric polyneuropathy that prominently involves pain fiers; the loss of sensation that results contributes to the tissue injury of the disease. - Tuberculoid leprosy shows evidence of active cell-mediated immune response to M. leprae, with nodular granulomatous inflammation situated in the dermis.
- The inflammation injures cutaneous nerves in the vicinity;axons, Schwann cells, and myelinare lost, and there is fibrosis of the perineurium and endoneurium.
With this form of leprosy, patients have much more localized nerve involvement but do develop areas of abnormal sensation from the injury.
Peripheral Nerve Diphtheria
- Peripheral nerve involvement results from the effcts of the diphtheria exotoxin and begins with paresthesias and weakness; early loss of proprioception and vibratory sensation is common.
- The earliest changes are seen in the sensory ganglia,where the incomplete blood-nerve barrier allows entry of the toxin.
- There is selective demyelination of axons that extends into adjacent anterior and posterior roots as well as into the mixed sensorimotor nerve.
Peripheral Nerve Varicella-Zoster Virus
- This virus is one of the few that produce lesions in the peripheral nervous system.
- Latent infection of neurons in the sensory ganglia of the spinal cord and brain stem follows chickenpox, and reactivation leads to a painful, vesicular skin eruption in the distribution of sensory dermatomes (shingles), most frequently thoracic or trigeminal.
- The virus may be transported along the sensory nerves to the skin, where it establishes an active infection of epidermal cells.
In a small proportion of patients, weakness is also apparent in the same distribution.
Although the factors giving rise to reactivation are not fully understood, decreased cell-mediated immunity is of major importance in many cases. - Affected ganglia show neuronal destruction and loss,usually accompanied by abundant mononuclear inflammatory infiltrates. Regional necrosis with hemorrhage may also be found.
- Peripheral nerve shows axonal degeneration after the death of the sensory neurons.
Focal destruction of the large motor neurons of the anterior horns or cranial nerve motor nuclei may be seen at the corresponding levels. Intranuclear inclusions generally are not found in the peripheral nervous system.
Question.13 Enumerate the cranial nerves.
Answer. Following are the cranial nerves:
- I Olfactory (Smell)
- II Optic (Sight)
- III Oculomotor (Moves eyelid and eyeball and adjusts the pupil and lens of the eye)
- IV Trochlear (Moves eyeballs)
- V Trigeminal (Facial muscles including chewing; Facial sensations)
- VI Abducens (Moves eyeballs)
- VII Facial (Taste, tears, saliva, facial expressions)
- VIII Vestibulocochlear (Auditory)
- IX Glossopharyngeal (Swallowing, saliva, taste)
- X Vagus (Control of PNS, e.g. smooth muscles of GI tract)
- XI Accessory (Moving head and shoulders, swallowing)
- XII Hypoglossal (Tongue muscles—speechand swallowing)
Question.14. Describe differentiating features of Bell’s palsy and trigeminal neuralgia.
Answer.

Question.15. Enumerate branches of facial nerve.
Answer. Following are the branches of facial nerve:
- Within the facial canal
- Greater petrosal nerve
- Nerve to stapedius
- Chorda tympani nerve
- At exit from stylomastoid foramen
- Posterior auricular
- Digastric
- Stylohyoid
- Terminal branches within the parotid gland
- Temporal
- Zygomatic
- Buccal
- Marginal mandibular
- Cervical
- Communicating branches with adjacent cranial and spinal nerves

Leave a Reply