Nerves Of The Upper Limb
Question 1. Enumerate five main nerves that supply the upper limb.
Answer.
These are
- Axillary nerve
- Musculocutaneous nerve
- Radial nerve
- Median nerve
- Ulnar nerve
Question 2. Describe the axillary nerve in brief and discuss its applied anatomy.
Answer.
Root value
Ventral rami of C5 and C6.
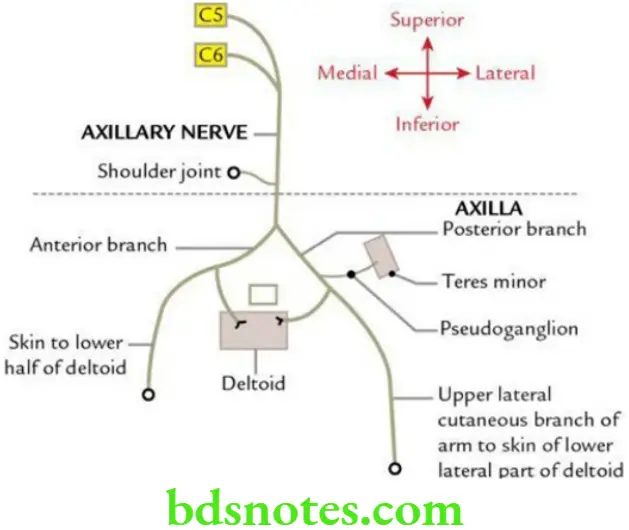
Course and relations
The axillary (or circumflex) nerve arises from the posterior cord of brachial plexus posterior to third part of axillary artery. It passes posteriorly through the quadrangular space. Here it lies below the capsule of the shoulder joint. As it is about to pass behind the surgical neck of humerus, it terminates by dividing into anterior and posterior branches.
The anterior branch (along with posterior circumflex artery) runs deep to deltoid muscle and supplies deltoid muscle and skin over it. The posterior branch supplies posterior part of deltoid and teres minor muscles. It pierces deep fascia to become upper lateral cutaneous nerve of arm.
Branches
Muscular:
To deltoid and teres minor. Nerves to teres minor possesses pseudoganglion.
Cutaneous
Upper lateral cutaneous nerve of arm
Sensory innervation of skin over the lower half of deltoid
Applied anatomy
The damage of axillary nerve in inferior dislocation of the shoulder joint and fracture of surgical neck of humerus will result in:
- Paralysis of deltoid leading to loss of power of abduction from 15° to 90°
- Loss of rounded contour of shoulder
- Prominence of greater tubercle of humerus
- Loss of cutaneous sensations over lower half of deltoid ‘regimental badge area of sensory loss’
Question 3. Describe the radial nerve under the following headings: (a) root value; (b) origin, course and relations, (c) branches and distribution and (d) applied anatomy.
Answer.
The radial nerve is the thickest and largest nerve of the upper limb.
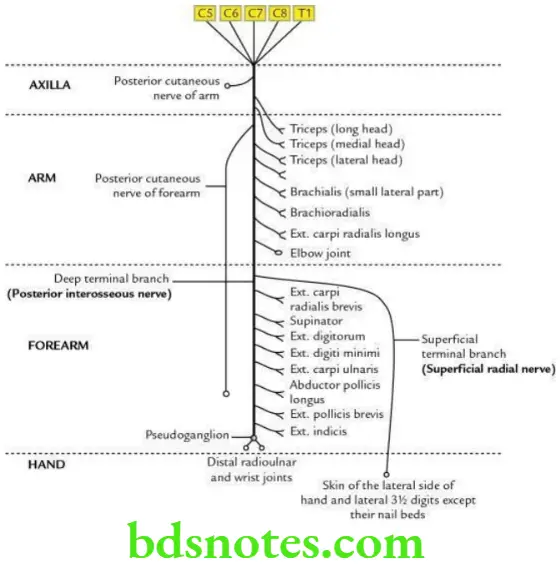
Root value
Ventral rami of C5, C6, C7, C8 and T1.
Read And Learn More: Selective Anatomy Notes And Question And Answers
Origin, course and relations
- It arises from the posterior cord of brachial plexus in axilla behind the third part of the axillary artery. It is the thickest and largest branch of the brachial plexus.
- It courses successively through three regions: axilla, radial groove on the back of arm and front of forearm. On the front of forearm, it ends by dividing into superficial and deep terminal branches. The course and relations of radial nerve in three regions traversed by it are as follows.
Axilla:
In the axilla, the radial nerve lies against the muscles forming the posterior wall of axilla, i.e. subscapularis, teres major and latissimus dorsi. Then it passes through the lower triangular space between teres major, long head of triceps brachii and shaft of humerus. In axilla, it gives two muscular branches to supply long and medial heads of triceps and one cutaneous branch (posterior cutaneous nerve of arm).
Radial groove
The radial nerve from axilla enters the radial groove through the lower triangular space, where it lies between the long and medial heads of triceps brachii along with profunda brachii artery. It leaves the radial groove by piercing the lateral intermuscular septum. In the radial groove, it gives three muscular branches to supply long and medial heads of triceps and anconeus and two cutaneous branches, i.e. lower lateral cutaneous nerve of arm and posterior cutaneous nerve of forearm.
Front of arm:
The radial nerve enters the lower anterolateral part of the front of arm and lies between brachialis on the medial side and brachioradialis and extensor carpi radialis longus on the lateral side. It supplies all these muscles.
Forearm:
The radial nerve enters the cubital fossa where in front of lateral epicondyle it ends by dividing into two terminal branches: (a) superficial terminal branch (superficial radial nerve) and (b) deep terminal branch (posterior interosseous nerve).
Deep terminal branch (posterior interosseous nerve):
It lies in the lateral part of cubital fossa, where it supplies extensor carpi radialis brevis and supinator muscles. Then it enters the back of forearm by passing through supinator muscle. Here, it supplies abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, extensor digitorum, extensor indicis, extensor digiti minimi and extensor carpi ulnaris. At the back of wrist, it ends in a pseudoganglion, branches of which supply the wrist and distal radioulnar joints.
Superficial branch (superficial radial nerve):
It is regarded as the downward continuation of the trunk of radial nerve. It runs on the lateral side of the front of forearm accompanied by the radial artery in the upper two third of forearm with radial artery being on its medial side. About 7 cm above the wrist, it curves posteriorly deep to tendon of brachioradialis to reach the anatomical snuff box. Here, it divides into four or five digital branches, which supply the skin of lateral half of dorsum of hand and lateral 2½ digits till their distal interphalangeal joints.
Branches and distribution
In axilla
- Muscular branches: Long and medial heads of triceps brachii
- Cutaneous branches: Posterior cutaneous nerve of arm
In radial groove
- Muscular
- Lateral head of triceps brachii
- Medial head of triceps brachii
- Anconeus
- Cutaneous
- Lower lateral cutaneous nerve of arm
- Posterior cutaneous nerve of forearm
- Vascular
- To profunda brachii artery
In the arm
- Muscular
- Brachioradialis
- Extensor carpi radialis longus
- Lateral part of brachialis (proprioceptive)
In the forearm
- Superficial terminal branch: Digital branches to supply the skin of lateral half of dorsum and lateral 3½ digits up to distal interphalangeal (DIP) joints.
- Deep terminal branch (posterior interosseous nerve): Muscular branches to all the muscles of back of forearm except anconeus, brachioradialis and extensor carpi radialis longus.
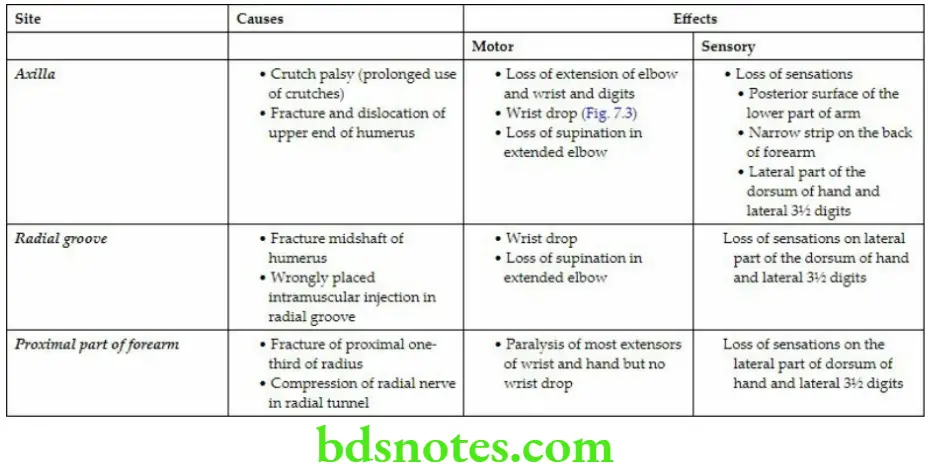
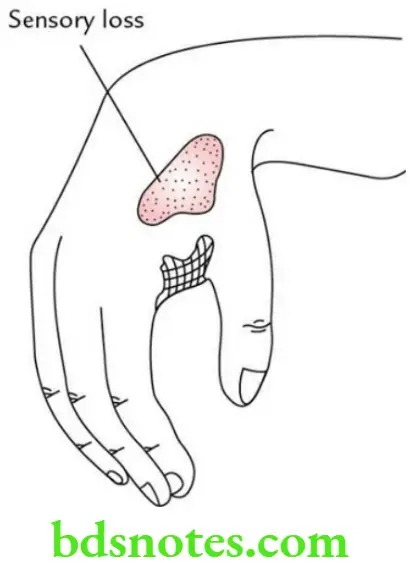
Applied anatomy
The effects of injury to the radial nerve at different levels.
Sites of Radial Nerve Injury and Their Effects
Question 4. Give the effects of injury to the posterior interosseous nerve.
Answer.
The posterior interosseous nerve supplies all the muscles on the back of forearm except anconeus, brachioradialis and extensor carpi radialis longus.
The posterior interosseous nerve is commonly injured in fracture or dislocation of the head of radius.
Effects
- Paralysis of all the muscles on the back of forearm except extensor carpi radialis longus, brachioradialis and anconeus (which are supplied by radial nervedirectly).
- There is no wrist drop because extensor carpi radialis longus being a powerful muscle keeps the wrist joint extended.
Question 5. Describe the median nerve under the following headings: (a) root value, (b) course and relations, (c) branches and distribution and (d) applied anatomy.
Answer.
The median nerve is so called because it runs in the median plane of the forearm.
Root value
Ventral rami of C5 to C8 and T1.
Course and relations
The median nerve is formed in the axilla by two roots – lateral root from lateral cord of brachial plexus and medial root from medial cord of brachial plexus. Then it courses successively through four regions: axilla, arm, forearm and palm of the hand. The medial root crosses the axillary artery to join the lateral root.
Axilla:
In the axilla, the median nerve lies first anterior and then lateral to the axillary artery.
Arm:
In the arm, the median nerve continues to run on the lateral side of brachial artery till the midarm (i.e. insertion of coracobrachialis), where it crosses in front of the brachial artery to lie on its medial side, and then passes anterior to elbow joint to enter the forearm.
Forearm:
In the forearm, the median nerve passes through cubital fossa lying medial to the brachial artery. It leaves the fossa between the two heads of pronator teres before crossing superficial to the ulnar artery from medial to lateral side and giving its anterior interosseous branch below this.
Then it passes deep to fibrous arch of flexor digitorum superficialis. It adheres to deep surface of flexor digitorum superficialis, and leaves the muscle, along its lateral border. About 5 cm above the wrist, it lies between the tendons of palmaris longus and flexor carpi radialis. It enters the palm through carpal tunnel under the flexor retinaculum, but in front of common synovial sheath enclosing tendons of flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP).
Palm:
In the palm at the distal border of flexor retinaculum, it ends by dividing into lateral and medial terminal branches. Before dividing into terminal branches, the median nerve gives off a recurrent muscular branch from its lateral side.
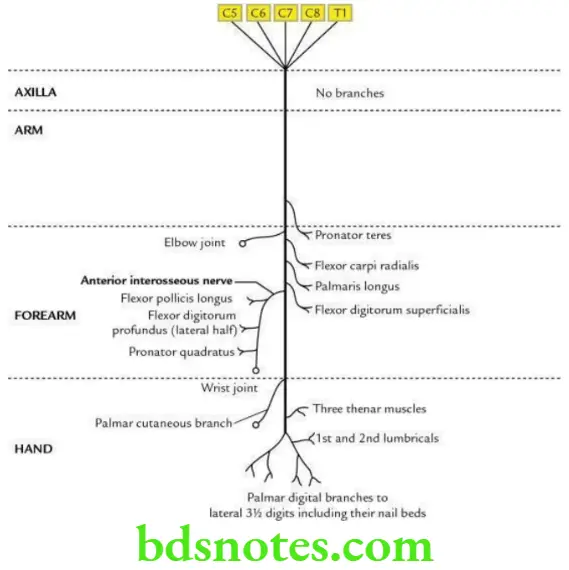
Branches and distribution
In axilla:
No branch
In arm:
Muscular branch to pronator teres
In the cubital fossa
- Muscular branches to:
- Flexor carpi radialis
- Palmaris longus
- Flexor digitorum superficialis
In the forearm
- Anterior interosseous nerve, which supplies:
- Lateral half of FDP
- Flexor pollicis longus
- Pronator quadratus
- Palmar cutaneous branch to supply lateral two-third of palm
In the palm
- Recurrent muscular branch, which supplies muscles of thenar eminence, i.e., abductor pollicis brevis, flexor pollicis brevis and opponens pollicis
- Lateral terminal branch, which gives off digital nerves to supply both the sides of thumb and radial side of index finger
Note: The digital branch to lateral side of index finger also supplies 1st lumbrical muscle. - Medial terminal branch, which gives off digital nerves to supply the adjacent sides of index and middle fingers and adjacent sides of index and little fingers 2nd lumbrical muscle.
Applied anatomy
The effects of lesion to the median nerve depend on the site of lesion.
Effects of Lesions of the Median Nerve
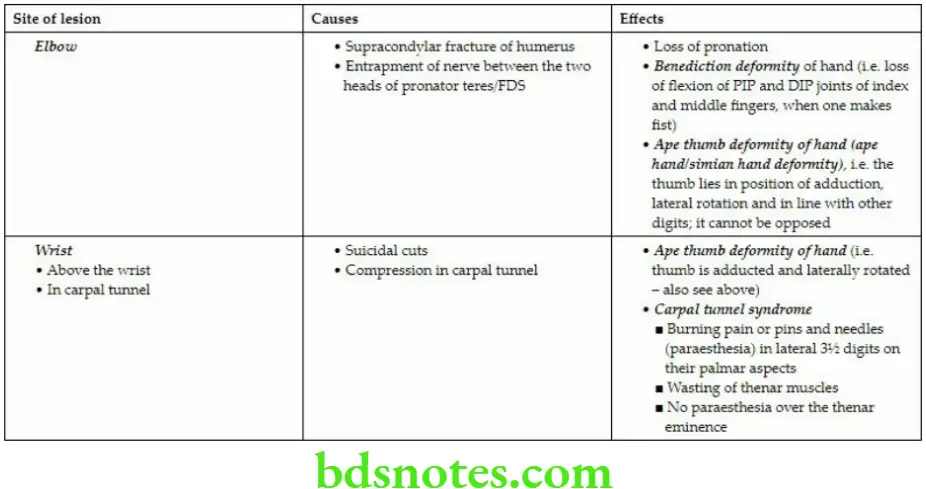
Question 6. Write a short note on carpal tunnel syndrome.
Answer.
It occurs due to compression of median nerve in the carpal tunnel. The carpal tunnel is an osseofibrous tunnel formed by the anterior concavity of the corpus bridged by the flexor retinaculum. This tunnel is tightly packed with long flexor tendons of the fingers with their surrounding synovial sheaths and the median nerve.
Clinical features
- Painful paraesthesia (i.e. burning pain or pins and needles) along the distribution of the median nerve to the palm and lateral 3½ fingers.
- Weakness and wasting of thenar muscles.
- No paraesthesia over the skin of thenar eminence because this area of skin is supplied by the palmar cutaneous branch of median nerve, which arises in the forearm proximal to flexor retinaculum.
- It is more frequent in women than in men.
- Intermittent attacks of pain are more common at night.
Question 7. Describe the ulnar nerve under the following headings: (a) root value, (b) course and relations, (c) branches and distribution and (d) applied anatomy.
Answer.
The ulnar nerve is so named because it runs along the ulnar side of the upper limb.
Root value
Ventral rami of C8 and T1. It also gets contribution from ventral ramus of C7.
Course and relations
It is the continuation of the medial cord of brachial plexus in the axilla. It courses successively through four regions: axilla, arm, forearm and hand, where it terminates by dividing into superficial and deep branches. The course and relations of ulnar nerve in these regions are as follows.
Axilla:
In axilla, the ulnar nerve lies between the axillary vein and the axillary artery on a deeper plane, medial to 3rd part of axillary artery.
Arm
It enters the arm by running downwards on the medial side of the brachial artery in its proximal part. At the midarm (i.e. at the level of insertion of coracobrachialis), it pierces the medial intermuscular septum to enter the back of arm. Here it descends to run in a groove on the back of medial epicondyle of humerus, where it can be palpated.
Forearm:
The ulnar nerve enters the front of forearm by passing between two heads of flexor carpi ulnaris. Here it lies on medial part of flexor digitorum profundus. It is accompanied by the ulnar artery on its lateral side in the lower two-third of forearm.
Hand:
The nerve enters the palm by passing superficial to the flexor retinaculum and medial to ulnar artery. At the distal border of flexor retinaculum, it ends by dividing into superficial and deep terminal branches.
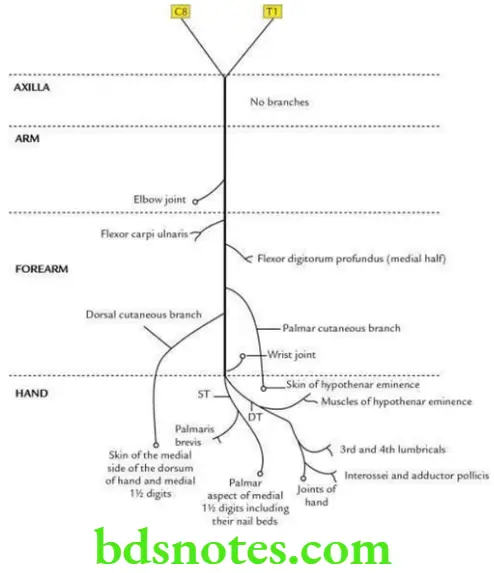
Branches and distribution
In axilla and arm:
No branches
In forearm
- Muscular branches to supply:
- Flexor carpi ulnaris
- Flexor digitorum profundus (medial half)
- Palmar cutaneous branch: It arises at about midforearm and provides cutaneous innervation to skin of the hypothenar eminence.
- Dorsal cutaneous branch: It arises about 5 cm above the wrist and gives off dorsal digital nerves to supply sensory innervation to dorsal aspects of the medial 1½ digits excluding their distal phalanges.
In hand
- Superficial terminal branch, which supplies:
- Palmaris brevis muscle
- Cutaneous innervation to medial one-third of palm and medial 1½ fingers, including their nail beds
- Deep terminal branch, which supplies:
- Medial two lumbricals
- Muscles of hypothenar eminence (abductor digiti minimi, flexor digiti minimi and opponens digiti minimi)
- All the interossei (three palmar and four dorsal)
- Adductor pollicis
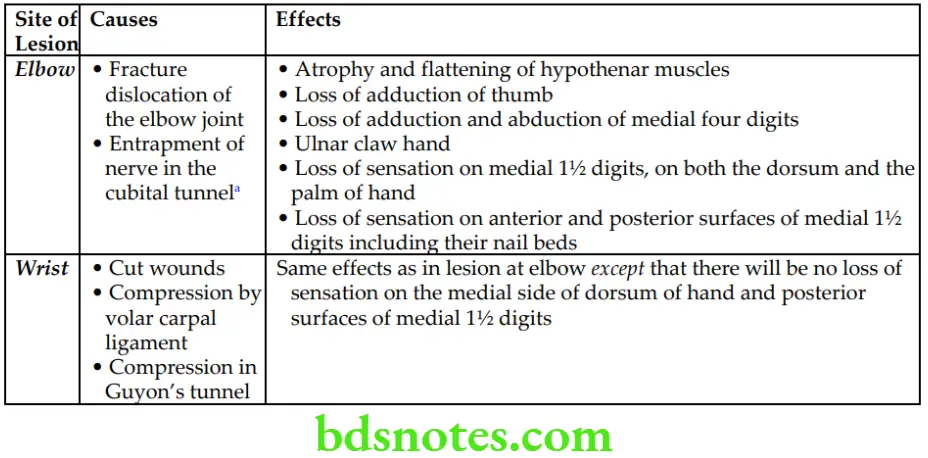
Applied anatomy
The effects of lesion to the ulnar nerve depend on the site of lesion.
Effects of the Ulnar Nerve Lesions

Leave a Reply