Mycology
Question 1. Write a short note on morphology, lab diagnosis, and lesions produced by Candida albicans.
Answer:
Morphology
- Candida albicans is an ovoid or spherical budding yeast cell, 3-5 µm in diameter.
- It produces pseudohyphae both in culture and in tissues.
Morphology Lab Diagnosis
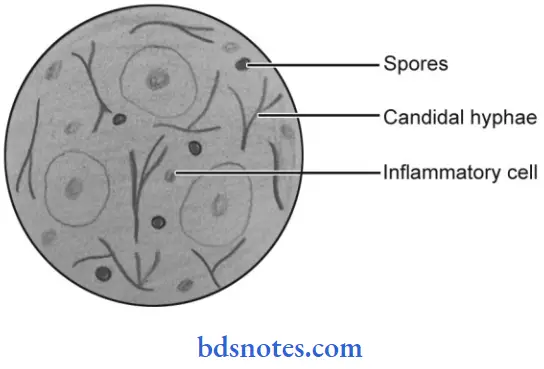
- Direct microscopic examination:
- KOH preparation shows yeast all with budding and pseudohyphae.
- Gram stain smear shows gram-positive yeast cells with budding and pseudohyphae.
- Culture and identifications: On sabouround’s dextrose with chloramphenicol, after 1 to 7 days of incubations at 37°C shows creamy white smooth colonies.
- Serology: A precipitation test with a carbohydrate extract of candida can be used.
- Antigen detection: ELISA is used for the detection of candidal antigens such as cell wall mannan or cytoplasmic constituents.
- Skin test: It shows universal positivity and is useful as an indicator of the intensity of cell-mediated immunity.
Lesions Produced by Candida Albicans
- Mucocutaneous lesions:
- Oral thrush: White patch on oral/buccal mucosa and tongue occurring commonly in bottle-fed infants and aged, a diabetic adults with ill fitting dentures, prolonged use of antibiotics.
- Vaginitis: Characterized by an acidic discharge, found frequently in pregnant and diabetics.
- Balanitis
- Conjunctivitis
- Keratitis.
- Skin and Nail Infections:
- Skin: Infection of the axilla , going, perineum, and sub mammary folds
- Nails: Infection of finger webs, nail folds and nails may occur.
- Chronic Mucocutaneous Candidiasis:
- Seen in immunodeficiencies.
- Systemic Diseases:
- Urinary tract infection
- Intestinal candidiasis
- Pulmonary candidiasis
- Endocarditis
- Meningitis
- Septicemia.
Question 2. Write down a short note on opportunistic fungal infection.
Or
Write a short note on opportunistic fungi.
Answer:
Some saprophytic fungi do not produce disease but may cause infection under special conditions such as in immunocompromised individuals and in terminal stages of chronic disease. The incidence of these fungal infections has increased with the wide use of antibiotics, corticosteroids, and immunosuppressive drugs.
These are called as opportunistic fungi:
- Some of them are common laboratory contaminants in culture media and can grow on anything.
- These fungi can produce fatal infections in debilitated patients.
- Examples of opportunistic fungi are Candida albicans, Aspergillus fumigatus, Penicillium sp., Rhizopus, and Mucor
- Candida is a spherical budding yeast cell that leads to oral thrush, vulvovaginitis, napkin dermatitis in infants, meningitis, septicemia, and much more.
- Aspergillus fumigatus may lead to asthma, aspergilloma and invasive aspergillosis.
- Aspergillus niger causes otomycosis
- Mucor and Rhizopus lead to zygomycosis.
- Penicillium marneffi is an important opportunist pathogen in HIV infected individuals.
Question 3. Write a short note on superficial mycosis.
Answer:
Superficial mycosis is of the following types, i.e. surface infections and cutaneous infections.
- In superficial mycosis, the fungi lie exclusively on the dead layers of skin and its appendages. They have no contact with living tissues and have elicited no inflammatory response.
- Tinea versicolor, tinea nigra and piedra are some surface infections.
- The most important cutaneous infection is dermatophytosis caused by dermatophytes. Dermatophytes only infect superficial keratinized tissue, i.e. skin, hair, and nails.
- Another type of cutaneous infection is caused by Candida albicans.
- Candida albicans cause cutaneous candidiasis which is an infection of skin and mucosa.
- Common mucosal lesions are vaginitis characterized by an acidic discharge and found frequently in pregnancy and oral thrush, found commonly in bottle-fed infants characterized by creamy white patches on the tongue and buccal mucosa.
Question 4. Classify dermatophytes and lesions caused by them.
Answer:
Dermatophytes are a group of fungi that infect only superficial keratinized tissue, i.e. skin, hair, and nails without involving the living tissue.
Classification of Dermatophytes
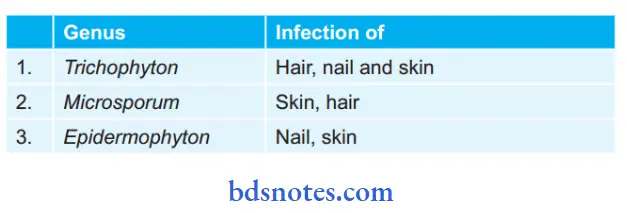
Lesions Caused by Dermatophytes
- Mycetoma: It is a chronic granulomatous infection of the subcutaneous tissue, it affects the foot and rarely the other parts of the body.
- Chromomycosis: It is a chronic localized infection of the skin and subcutaneous tissue. Fungus enters the body through wounds.
- Sporotrichosis: It is a nodular ulcerating disease of the skin and subcutaneous tissue. Fungus spreads through lymphatics up to regional lymph nodes and beyond that.
- Rhinosporidiosis: It is a chronic granulomatous disease characterized by the formation of friable polyps usually confined to the nose, mouth, and eye.
- Histoplasmosis: It is a disease of the reticuloendothelial system.
- Blastomycosis: It is a chronic infection of the lungs that may spread to other tissues, particularly skin, bone, and genitourinary tract.
- Paracoccidioidomycosis: It is a chronic granulomatous disease involving the lung, mucosa, skin and lymphatic system.
Question 5. Write short note on fungal infections of the oral cavity.
Or
Answer:
Following are the fungal infections of the oral cavity:
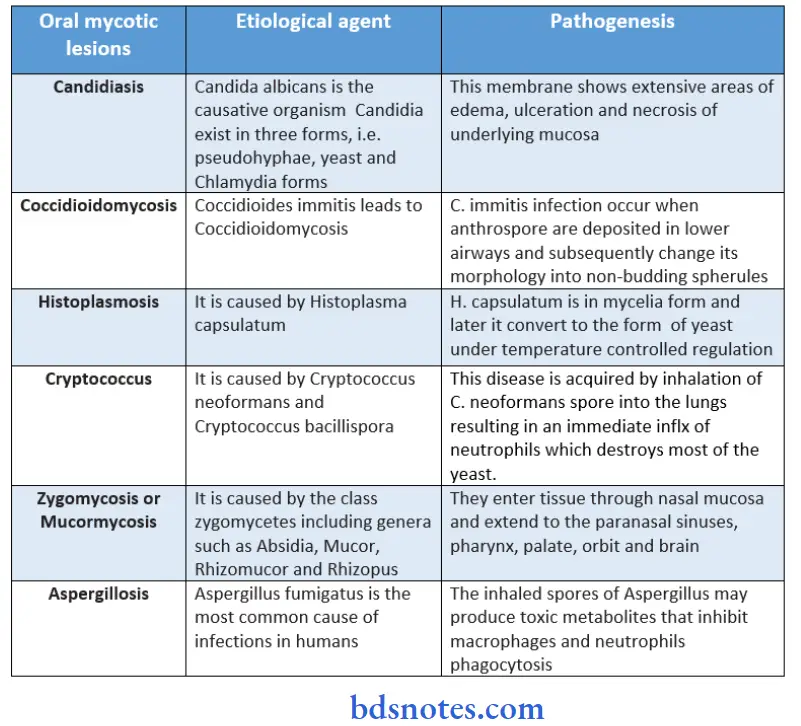
- Candidiasis
- Coccidioidomycosis
- Histoplasmosis
- Blastomycosis
- Paracoccidioidomycosis
- Sporotrichosis
- Chromomycosis and phaeomycotic abscess
- Aspergillosis
- Cryptococcosis
- Zygomycosis
- Mycetoma.
Question 6. Write a short note on candidiasis.
Or
Write a short note on oral candidiasis.
Answer:
Candidiasis is caused by Candida albicans.
Classifiation of Oral Candidiasis:
1. Primary Oral Candidiasis
- Acute form:
- Pseudomembranous candidiasis
- Erythematous candidiasis.
- Chronic form:
- Hyperplastic candidiasis
- Erythematous candidiasis
- Pseudomembranous candidiasis.
- Candida-associated lesion:
- Denture stomatitis
- Angular stomatitis
- Median rhomboid glossitis.
- Keratinized primary lesion super-infected with candida:
- Leukoplakia
- Lichen planus
- Lupus erythematosus.
2. Secondary Candidiasis:
- Candidal endocrinopathy syndrome.
Clinical Features Of Candidiasis
- Pseudomembranous Candidiasis:
- The common sites are the roof of the mouth, retromolar area, and mucobuccal fold.
- It is more common in women.
- The prodromal symptom is the rapid onset of bad taste. Spicy food causes discomfort.
- There is a presence of inflammation, erythema, and painful eroded areas that may be associated with this disease.
- White patches of candidiasis are easily wiped out with a wet gauge which leaves an erythematous area or atrophic area.
- Deeper invasion by the organism leaves an ulcerative lesion upon removal of the patch.
- Acute Atrophic Candidiasis:
- It can be seen anywhere in the oral cavity but the most common site involved are the tongue as well as the tissue underlying the prosthesis.
- It appears as an erythematous area.
- The patient complains of a burning sensation in the lesional area along with vague pain.
- Chronic Hyperplastic Candidiasis:
- Male predilection is seen.
- Most common in heavy smokers.
- The oral sites involved are the tongue, cheek, and lips.
- There is the presence of fim and white leathery plaques.
- The lesion cannot be rubbed with lateral pressure.
- The lesion is whitish or creamy whitish in color. Borders of the lesion are vague.
Histopathology
- Epithelium show increased thickness of parakeratin at the lesional area in conjunction with elongation of rete ridges.
- A small collection of neutrophils, i.e. microabscess is seen in the parakeratin layer and superficial spinous layer.
- Hyphae or mycelia and yeast cells are seen in the parakeratin layer of epithelium.
- There is a presence of chronic inflammatory infiltrate cells such as lymphocytes and plasma cells immediately subjacent to infected epithelium.
Question 7. Write briefly on oral mycotic lesions.
Or
Write a short note on oral fungal lesions.
Answer:
Following are the oral mycotic lesions:
- Candidiasis
- Coccidioidomycosis
- Histoplasmosis
- Blastomycosis
- Paracoccidioidomycosis
- Sporotrichosis
- Chromomycosis and phaeomycotic abscess
- Aspergillosis
- Cryptococcosis
- Zygomycosis
- Mycetoma.
Question 8. Write a short answer on oral thrush.
Answer:
Oral thrush is a mucocutaneous lesion caused by Candida albicans. Oral thrush is also known as pseudomembranous candidiasis.
Predisposing Factors Of Oral Thrush
- Changes in oral flora: Marked changes in oral flora occur due to the administration of antibiotics, excessive use of antibacterial mouth rinses, xerostomia secondary to an anticholinergic agent, or salivary gland disease. These charges result in the inhibition of competitive bacteria leading to candidiasis.
- Local irritant: Chronic local irritants, i.e. dentures, orthodontic appliances, etc.
- Drug therapy: Various drugs, i.e. corticosteroids, cytotoxic drugs, immunosuppressive agents, and radiation to the head and neck.
- Acute and chronic diseases such as leukemia, diabetes, tuberculosis, etc.
- Malnutrition states such as low serum vitamin A, pyridoxine, and vitamin A.
- Endocrinopathy: Such as hypothyroidism, hyper parathyroid and Addison’s disease
- Immunodeficiency states such as AIDS, and hypogammaglobulinemia.
Clinical Features Of Oral Thrush
- It occurs in both infants and adults. In infants, oral lesion occurs between the 6th and 10th day after birth.
- Common sites for infection to occur are the roof of the mouth, retromolar area, and mucobuccal fold.
- It is more common in women as compared to men.
- Patients can complain of a burning sensation.
- The lesion appears as white plaque which is pearls white or blue-white in color and is present on the oral mucosa.
- Lesions resemble as cottage cheese or curdled milk.
- Mucosa adjacent to the lesion appears red in color and is moderately swollen.
- White patches are easily wiped out with wet gauze which leaves the normal or erythematous areas. This area can be painful.
- Deep invasion of an organism leaves an ulcerative lesion on the removal of the patch.
- In severe infection, the involvement of the pharynx and esophagus causes dysphagia.
- The fungus may travel to the lower respiratory passages and may involve the lungs in fulminant infection.
Investigations of Oral thrush
- On staining with the periodic acid-Schiff (PAS) method, candidal hyphae are readily identified.
- Organisms are identified by bright magenta color.
- The candidal hyphae are 2 µm in diameter, vary in length, and may show branching.
- About 10–20% KOH is also used to identify organisms readily.
- Its shows budding gram-positive yeast cells Cultures can be obtained readily on Sabouraud’s medium and on ordinary bacteriological culture media.
- Colonies are creamy white, smooth with a yeasty color. Gram-stained smears from colonies show gram-positive budding yeast cells.
- On corn-meal agar medium C. albicans form chlamydospores.

Leave a Reply