Musculoskeletal System
Question 1. Write a short note on a giant cell tumor of bone.
Or
Write a short note on a giant cell tumor of bone.
Or
Write a short note on giant cell tumors.
Answer:
A giant cell tumor of bone is also known as osteoclastoma.
Giant cell tumor Origin
Tumor arises in the epiphysis of long bones which is close to the articular cartilage.
Giant cell tumor Clinical Features
- The tumor arises between 20 to 40 years of age.
- The most commonly involved sites are the lower end of the femur and the upper end of the tibia; the lower end of the radius and the upper end of the file.
- Patient complaints of pain especially over the weight-bearing areas and during movement.
- There is also the presence of swelling and pathological fracture.
Read And Learn More: Pathology Question And Answers
Giant cell Tumor Radiographic Feature
It appears as a large lobulated and osteolytic lesion at the end of the expanded long bone with a soap bubble appearance.
Giant cell tumor Gross Features
- Grossly, a giant cell tumor is eccentrically located in the epiphyseal end of a long bone that is expanded.
- The tumor is well-circumscribed, dark tan, and is covered by a thin shell of subperiosteal bone.
- The cut surface of the tumor is characteristically hemorrhagic, necrotic, and honeycombed due to focal areas of cystic degeneration.
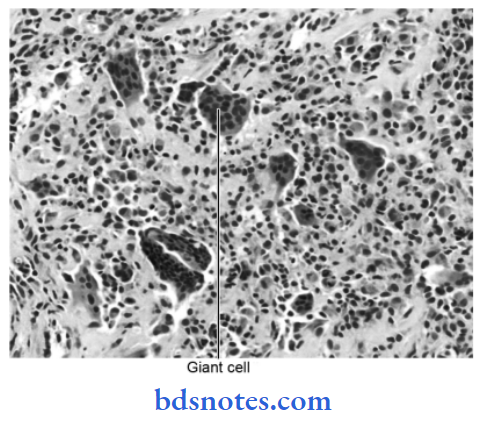
Giant cell tumor Histological Features
- Histologically there is the presence of a large number of multinucleated osteoclast-like giant cells which are scattered throughout the stromal mononuclear cells.
- Giant cells consist of 100 nuclei and are similar to normal osteoclasts.
- Stromal cells are mononuclear cells and are real tumor cells. They are uniform, plump, spindle-shaped or round to oval cells with numerous mitotic figures.
- Stroma is scanty collagenous, have rich vascularity, and areas of hemorrhage and macrophages are commonly seen.
Question 2. Discuss in brief osteomyelitis.
Or
Discuss etiopathogenesis and morphological changes in pyogenic osteomyelitis.
Answer:
Osteomyelitis is defined as an inflammation of the soft tissue components of the bone which includes bone marrow, haversian canals, and periosteum with secondary changes of the mineralized components of the bone.
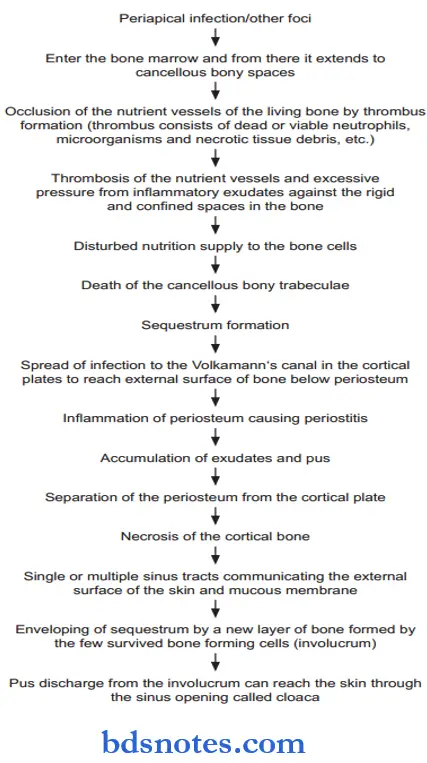
Osteomyelitis Etiopathogenesis
Morphological Changes in Pyogenic Osteomyelitis
- The morphologic changes in osteomyelitis depend on the stage (acute, subacute, or chronic) and the location of the infection.
- Infection begins at the metaphyseal end of the marrow cavity which is occupied by pus.
- Tension in the marrow cavity is increased because of the presence of pus and leads to the spread of infection along the marrow cavity, into the endosteum, and into the Haversian and Volkmann’s canal, causing periosteitis.
- The infection may reach the subperiosteal space forming subperiosteal abscesses. It may penetrate through the cortex forming draining skin sinus tracts.
- A combination of suppuration and impaired blood supply to the cortical bone leads to erosion, thinning, and infarction necrosis of the cortex called a sequestrum.
- Along with time, there is the formation of new bone beneath the periosteum present over the infected bone. This forms an encasing sheath around the necrosed bone and is known as an involucrum. Involucrum has an irregular surface and has perforations through which discharging sinus tracts pass.
- Long-continued neo-osteogenesis gives rise to a dense sclerotic pattern of osteomyelitis called chronic sclerosing nonsuppurative osteomyelitis of Garré.
- Occasionally, acute osteomyelitis may be confined to a localized area and walled off by fibrous tissue and granulation tissue. This is termed Brodie’s abscess.
- In vertebral pyogenic osteomyelitis, the infection begins from the disc (discitis) and spreads to involve the vertebral bodies.
Question 3. Discuss common neoplastic lesions of bone.
Answer:
Bone tumors are comparatively infrequent but they are clinically quite significant since some of them are highly malignant.
- Bone tumors may be primary or metastatic.
- Various types of bone tumors arise from different tissue components: Osseous and non-osseous, indigenous to the bone.
- Bone-forming (Osteoblastic) tumors:
- Osteoma: An osteoma is a rare benign, slow-growing lesion, regarded by some as a hamartoma rather than a true neoplasm.
- Osteoid osteoma and osteoblastoma: Osteoid osteoma and osteoblastoma are closely related to benign tumors occurring in children and young adults. Osteoid osteoma is more common than osteoblastoma. Osteoid osteoma is generally a small and painful tumor, located in the cortex of long bone. Osteoblastoma is larger in size, painless, and located in the medulla of a long bone.
- Osteosarcoma: It is the most common malignant tumor of the bone.
- The tumor is characterized by the formation of osteoid or bone or both, directly by sarcoma cells. Dependingontheirlocationwithinthebone, Osteosarcoma is classified into medullary and periosteal.
- Cartilage-forming tumors:
- Osteocartilagenous exostoses or osteochondromas are the commonest of benign cartilage-forming lesions. Exostoses or osteochondroma is not a true tumor but is regarded as a disorder of growth and development. Exostoses arise from the metaphysis of long bones as exophytic lesions.
- Enchondroma: It is the term used for a benign cartilage-forming tumor that develops centrally within the interior of the affected bone. The most common locations are short tubular bones of hand and feet. The tumor has a characteristic lobulated appearance.
- Chondroblastoma: It is a relatively rare benign tumor arising from the epiphysis of long bones adjacent to the epiphyseal cartilage plate.
- Ewing’s sarcoma: The skeletal Ewing sarcoma arises in the medullary canal of diaphysis or metaphysis.
The common sites are the shaft and metaphysis of long bones. Clinical features include pain, tenderness and swelling of the affected area.
Question 4. Write a short note on tuberculous osteomyelitis.
Answer:
An infection of the bone is termed osteomyelitis.
- When it occurs by tuberculous infection, it is called tuberculous osteomyelitis.
- The tubercle bacilli M. tuberculosis reaches the bone marrow and synovium most commonly by hematogenous dissemination from an infection elsewhere.
- 1 to 3% of cases of pulmonary and extrapulmonary tuberculosis present with osseous involvement.
- Skeletal tuberculosis is present as a solitary lesion but may be multifocal in an immunodeficient state.
Tuberculous Osteomyelitis Modes of Spread
- Hematogenous, i.e. from active visceral disease
- Direct extension, i.e. from pulmonary focus into ribs or tracheobronchial nodes into vertebrae.
Tuberculous Osteomyelitis Clinical Features
- Commonly affected sites are the spine, knee, and hip.
- All patients present with fever, pain, and weight loss.
Tuberculous osteomyelitis Morphologic Features
- Extension of caseous material along with pus from lumbar vertebrae to sheaths of psoas muscle produces psoas abscess or lumbar cold abscess.
- A cold abscess may burst through the skin and form a sinus.
- Longstanding cases may develop systemic amyloidosis.
- Histopathologically lesion consists of central caseation necrosis surrounded by tubercular granulation tissue.
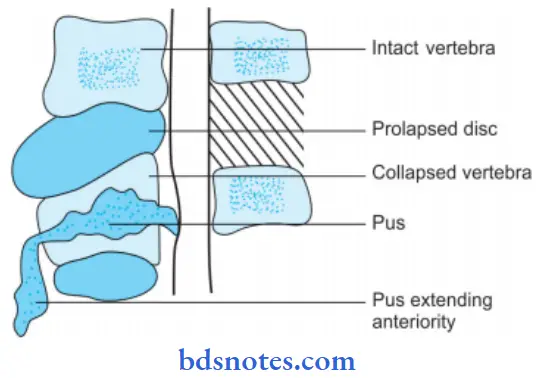
- The tubercular lesion appears as a focus of bone destruction and the replacement of the affected tissue by caseous material and the formation of multiple discharging sinuses through the soft tissue and skin.
- Tuberculosis of the spine, Potts disease may be associated with a compression fracture and destruction of intervertebral discs, producing permanent damage and paralysis.
Tuberculous osteomyelitis Complications
- Psoas abscess
- Fracture
- Neurological deficit and paraplegia due to extension of the disease process in the dural state with resultant pressure on the cord
- Tuberculous arthritis
- Sinus tract formation
- Ankylosis.
Question 5. Write a short note on chronic osteomyelitis.
Or
Write briefly on chronic osteomyelitis.
Answer:
Chronic osteomyelitis may be the sequelae of acute osteomyelitis, in which proper treatment is either not done or inadequately done.
- The disease may also arise primarily as a chronic, low-grade inflammatory reaction in the bone, without any pre-existing acute phase.
- It is generally believed that lower levels of virulence of the causative microorganisms, For Example. Staphylococci, Bacteroids, and Actinomyces, etc. are mostly responsible for the development of chronic suppurative osteomyelitis. Nonspecific microorganisms like staphylococci, streptococci, Bacteroids, and Actinomyces, etc. mostly cause the disease.
Chronic Osteomyelitis Clinical Features
- The molar area of the mandible is more frequently affected.
- In the case of chronic osteomyelitis, the pain is usually mild and dull vague in nature even if the disease is very extensive.
- Patients often give a history of dull vague pain in the jaw for several weeks, which had started following an acute tooth abscess, tooth fracture or extraction, etc.
- Pain is usually mild and insidious in nature.
- Jaw swelling is a common feature but mobility of teeth and sinus tract formations, etc. are rare.
- On rare occasions, sinus tracts may develop both intraorally and extraoral with the intermittent discharge of purulent materials.
- Sequestrum is often found, which protrudes from the ulcerated skin or mucosal surfaces.
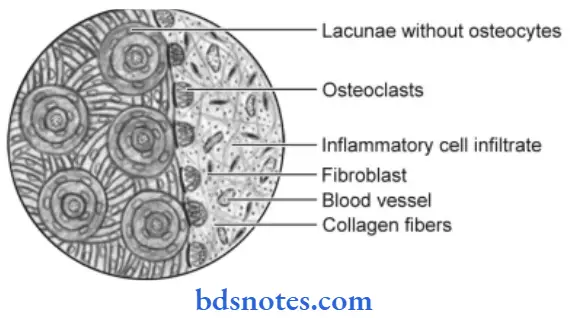
Chronic osteomyelitis Histopathology
Chronic suppurative osteomyelitis often presents the following features:
- Chronic inflammatory reaction in the bone with an accumulation of exudates and pus within the medullary spaces.
- The lymphocytes, plasma cells, macrophages, etc. predominate among the inflammatory cells.
- Osteoblastic and osteoclastic activity occur parallel with the formation of irregular bony trabeculae having reversal lines.
- Sequestrum may develop in the later stages of the disease.
Question 6. Write briefly on morphological changes in pyogenic osteomyelitis.
Answer:
Infection begins at the metaphyseal end of the marrow cavity which is occupied by pus.
- Tension in the marrow cavity is increased because of the presence of pus and leads to the spread of infection along the marrow cavity, into the endosteum, and into the Haversian and Volkmann’s canal, causing periosteitis.
- The infection may reach the subperiosteal space forming subperiosteal abscesses. It may penetrate through the cortex forming draining skin sinus tracts.
- A combination of suppuration and impaired blood supply to the cortical bone leads to erosion, thinning, and infarction necrosis of the cortex called sequestrum.
- Along with time, there is the formation of new bone beneath the periosteum present over the infected bone. This forms an encasing sheath around the necrosed bone and is known as an involucrum. Involucrum has an irregular surface and has perforations through which discharging sinus tracts pass.
- Long-continued neo-osteogenesis gives rise to a dense sclerotic pattern of osteomyelitis called chronic sclerosing nonsuppurative osteomyelitis of Garré.
- Occasionally, acute osteomyelitis may be confined to a localized area and walled off by fibrous tissue and granulation tissue. This is termed Brodie’s abscess.
- In vertebral pyogenic osteomyelitis, the infection begins from the disc (discitis) and spreads to involve the vertebral bodies.
Question 7. Write a short note on osteomyelitis.
Answer:
Classification of Osteomyelitis
Acute Osteomyelitis:
- Acute suppurative osteomyelitis
- Acute subperiosteal osteomyelitis
- Acute periostitis.
Chronic Osteomyelitis:
- Non-Specific Type:
- Chronic intramedullary osteomyelitis
- Chronic focal sclerosing osteomyelitis
- Chronic diffuse sclerosing osteomyelitis
- Chronic osteomyelitis with proliferative periostitis
- Chronic subperiosteal osteomyelitis
- Chronic periostitis.
- Specific Type:
- Tuberculous osteomyelitis
- Syphilitic osteomyelitis
- Actinomycotic osteomyelitis.
Radiation-induced osteomyelitis
Idiopathic osteomyelitis.
Acute suppurative osteomyelitis is serious sequelae of periapical infection, there is the diffuse spread of infection throughout medullary spaces with subsequent necrosis of a variable amount of bone.
Osteomyelitis Etiology
- Direct spread of infection from dental pulp into the mandible.
- Spread of infection in the mandible from presenting suppurative odontogenic infections.
- Spread of infection following removable of the tooth without proper asepsis and antibiotic coverage.
- Compound fracture of the mandible with exposure of bone outside the mucosa.
- Post-radiation secondary infection.
- Infection to the preexisting bony lesions, For Example. Paget’s disease of bone and fibrous dysplasia.
Osteomyelitis Clinical Features
- It occurs after 50 years of age and males are more commonly affected.
- The mandibular lesions are diffused in nature.
- Acute suppurative osteomyelitis of the mandible in young adults causes severe pain, and diffuse and enlarged swelling of the mandible.
- There is loosening and soreness of the regional teeth with difficulty in food intake.
- Multiple intraoral and extraoral pus-discharging sinuses often develop and moreover, discharge of pus is seen from the gingival service of the affected teeth.
- Paresthesia of the lip is common.
- The patient is slightly febrile and general symptoms include fever, malaise, anorexia and vomiting.
Osteomyelitis Histopathology
- In acute suppurative osteomyelitis, the bone marrow undergoes liquefaction and purulent exudates occupy the marrow space.
- A large number of acute inflammatory cell infiltrations are present which shows PMNs with the occasional presence of lymphocytes and plasma cells.
- Some areas of affected bone undergo necrosis with the generation of osteoblast and osteocytes cells and therefore results in the development of sequestrum (a piece of dead bone)
- When the acute phase of infection subsides the new shell of bone called “involucrum” is formed over inflammatory focus.
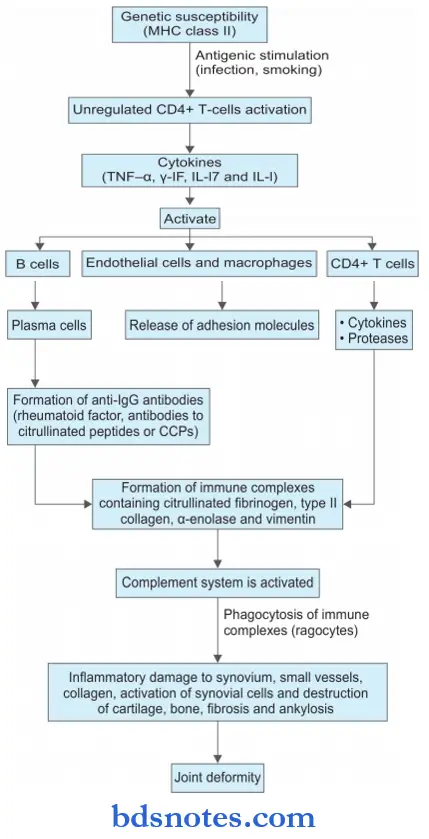
Question 8. Write a note on the pathophysiology of rheumatoid arthritis.
Answer:
Following is the pathophysiology of rheumatoid arthritis.

Leave a Reply