Miscellaneous
Question.1. Write short note on anaphylactic shock.
Or
Write notes on anaphylaxis.
Or
Discuss anaphylaxis and its management in detail
Answer. Anaphylaxis is an acute and dramatic lifethreatening immunological reaction to a drug or other stimulus.
Etiology
- Antibiotics: Penicillin and streptomycin.
- Radio contrast media
- Anesthetic agent, i.e. lignocaine
- Blood and blood products including sera.
- Hormones: Insulin and growth hormone.
- Venoms: Bees, spiders and wasps
- Others: NSAIDs, narcotic agents, heparin and thrombolytic agents.
Clinical Features
- Onset may be instantaneous or within a few minutes after the IV injection and 30 minutes after exposure.
- Cardiovascular: Tachycardia, arrhythmia, hypotension and circulatory collapse.
- Respiratory: Laryngeal obstruction, angiedema,bronchospasm or pulmonary edema may occur singly or in combination.
- Nervous: Syncope and seizures.
- GIT: Diaphoresis, abdominal pain and diarrhea may occur.
- Skin: Wheel and erythematous lesions are seen which are circumscribed, round, discrete, erythematous areas with irregular borders and blanched centres.
- Lesions are very pruritic.
- If not treated death may occur.
Read And Learn More: General Medicine Question And Answers
Management
- Airways: Endotracheal intubation or perform tracheostomy,if intubation is not possible.
- Oxygen is given in high concentration.
- Injection adrenaline 0.5 to 1 mL of 1:1000 solution IM
- Fluids: 0.5 or 1 liter of flid restores blood pressure but 6-9 liters is required for adequate restoration of blood volume.
- Hydrocortisone 300 mg IV.
- Aminophylline 250 mg IV in 20 mL dextrose to revert bronchospasm.
- Diphenhydramine 50 mg IV slowly.
- Dopamine, if hypotension persists.
- IV atropine and glucagon.
- Ventilatory support is necessary, if patient is critical.
Question.2. Write short note on drug interactions.
Answer.
Drug interaction has been defined as action of an administered drug upon the effctiveness or toxicity of another drug administered earlier, simultaneously or later.
When two or more drugs are prescribed either simultaneously or in quick succession, they may exhibit either a synergistic or antagonistic action.
Types Of Interaction
There are three types of interactions:
Pharmacokinetic Interactions
These results in alterations in delivery of drugs to their sites of action, i.e. impaired GI absorption, induction of hepatic enzymes and inhibition of cellular uptake.
Pharmacodynamic Interactions
In this, the responsiveness of the target system or organ is modifid by other agents.
Pharmacodynamic and other Interactions between drugs
They are usually therapeutically useful interactions in which combined effct of two drugs is greater than that of the either drug. For example: Amlodipine + Atenolol and Sulfonamides +Trimethoprim
The fist two interactions are detrimental while last one is useful interaction employed in therapeutic medicine.
Question.3. Write short note on urticaria.
Answer.
Urticaria is a vascular reaction characterized by transient,evanescent, pruritic wheals occurring on any site of the body.
It is type I hypersensitivity reaction of skin to variety of exogenous or endogenous agents.
When the subcutaneous tissue involves, it is known as angiedema.
Etiology
Exogenous causes:
- Ingestants, i.e. drugs and foods
- Inhalants, i.e. pollen, plant, dust, etc.
- Injectants, i.e. penicillin, insulin, anti sera, vaccines.
- Contactants, i.e. bee sting and bug bites.
Endogenous causes:
- Infections, i.e. urinary tract infection, respiratory tract infection and candida infections.
- Infestants, i.e. helminths, amoebiasis and giardiasis
- Systemic disease, i.e. systemic lupus erythmatosus and lymphomas.
- Psychogenic, i.e. emotional stress.
Management
Histamine-mediated Urticaria
1. First-line treatment:
- Loratadine 10 mg/day
- Tricyclic antidepressant doxepine 10 mg TDS or
ranitidine 150 mg BD
2. Second-line treatment
- Prednisolone 0.5 mg/kg 1 to 2 weeks.
3. Third-line treatment:
- Cyclosporine A
- IV immunoglobin
- Plasmapheresis.
Immune Complex-mediated Urticaria
- Dapsone 75–100 mg/day
- Indomethacin 25–50 mg TDS
- Hydroxy chloroquine 200–400 mg/day.
Question.4.Describe briefl pyrazinamide.
Answer. It is an antitubercular drug.
It inhibits mycolic acid synthesis.
- Pyrazinamide is absorbed orally and has good penetration in CSF.
- Hepatotoxicity is more important dose-dependent adverse effct.
- It is contraindicated in patient with the liver disease.
- Other adverse effcts are arthralgia, flshing, rashes,fever, etc.
Question.5.Describe briefl side effcts of corticosteroids.
Answer.
Side Effects
- In hyperglycemia, they cause precipitation of diabetes and glucosuria.
- They cause muscular weakness.
- They cause thinning of skin, fragile skin and purple striae hirsutism.
- They cause Cushing’s habitus in which there is moon face, narrow mouth and obesity of trunk with thinning of lungs.
- They increase susceptibility to infection, i.e. TB and opportunistic infection may flre up.
- They cause delayed healing of wound and surgical incisions.
- They causes peptic ulcer.
- They causes osteoporosis, glaucoma and growth retardation in children.
- At high doses, they causes psychiatric disturbance.
- They cause suppression of hypothalamopituitary axis.
Question.6.Write short note on fied drug eruption.
Answer. Fixed drug eruption occurs at the same site each time the offnding drug is taken.
- Causative agents are tetracyclines, sulphonamides,phenolphthalein, oxyphenbutazone.
- Lesions, which are often painful and may cause a burning sensation, appear as clearly demarcated oval or round erythematous plaques which are sometimes bullous and usually 20 mm in diameter, though lesions up to 10 cm in diameter may occur. After 1–2 days, the lesions become violaceous.
Typically, there are one to three lesions. Lesions fade over 7–10 days and leave a hyperpigmented patch. - Sites affcted are hands, feet, glans penis or lips.
- Lesions always occur at the same site.
Question.7.Write short note on diffrential diagnosis.
Answer.
Identifiation of disease by comparison of illness that share features of present illness but diffr in some critical ways is known as diffrential diagnosis.
It is given on the basis of determination of cause and pathogenic condition.
This is done by evaluating the history of disease process,sign and symptoms, laboratory test and special test such as radiography and ECG.
Question.8. Discuss in short lactose intolerance.
Answer.
An assessment of person’s blood sugar and exhaled hydrogen level within two hours after drinking a loading dose of lactose, i.e. is usually about 100 g of lactose for average size adult.
People who readily digest the lactose will have an increase in their blood sugar and litte increase in exhaled hydrogen gas during the test.
People who are unable to digest will have no increase in blood sugar and the level of hydrogen, they exhaled will exceed 50 ppm.
Question.9. Write short note on total parenteral nutrition.
Answer.
The intravenous provision of dextrose, amino acids, fats,trace elements, vitamin and minerals to patients who are unable to assimilate adequate nutrition to mouth.
Patients with many illness become malnutritioned, if they are unable to eat a balanced diet for more than few weeks, however only a small percentage of these patients clearly benefi from parenteral nutrition support.
Patient who benefi most from total parenteral nutrition are those at extremes of nutritional defiiency.
Question.10. Write short note on leukorrhea.
Answer.
Leukorrhea is strictly defied as an excessive normal vaginal discharge.
- The excess secretion is evident from persistent vulval moistness or staining of undergarments or need to wear a vulval pad.
- It is non-purulent and non-offensive.
- It is non irritant and never causes pruritus.
- The physiological basis involve in normal vaginal secretion in the development of an endogenous estrogen level.
- Excessive secretion is due to:
- Physiological excess: Normal secretion is expected to increase in condition when the estrogen level becomes high.
The condition is during puberty, during menstural cycle, pregnancy and during sexual excitement. - Cervical cause or cervical leukorrhea: Non infective cervical lesion may produce excess secretion which produces out at vulva.
- Vaginal cause or vaginal leukorrhea: Increase vaginal transudation during the uterine prolapse.
Treatment
- Improvement of general health
- Cervical factor requires surgical treatment such as electrocautery, cryosurgery
- Pelvic lesion producing vaginal leukorrhea requires appropriate therapy for pathology.
- Pills users stop the pill temporarily
- Local hygiene is to be maintained meticulously.
Question.11. Write short note on acne vulgaris.
Answer. Acne vulgaris is a disease in which the pilosebaceous follicle becomes oversensitive to normal levels of testosterone.
Etiology
- Androgens
- Follicular keratinization
- Hereditary
- Propionibacterium acnes
- Immunological factors
- Environmental factors
Exacerbating Factors
Acne worsens with stress and in premenstrual period.
In patients with aggressive or recalcitrant acne, underlying cause may be a virilizing syndrome in women, acromegaly,occupational exposure to acnegenic agents.
Drugs that worsen acne are steroids, hormones (androgen and progesterone), antiepileptic drugs, iodides; can follow facial massage.
Genetic and hormonal factors also play a role.
Grading
- Mild disease: Open (black heads) and closed (white heads) comedones with sparse inflmmatory lesions.
Some comedones are deepseated (submarine comedones). - Moderate: Numerous papules and pustules
- Severe: Polymorphic eruption with comedones, papules,pustules, nodules and cysts.
Management
- Topical therapies are the mainstay of treatment for mild acne:
- Benzoyl peroxide 5% has antibacterial and keratolytic properties. It treats both inflmed and non-inflmed lesions.
- Topical antibiotics, i.e. 1% clindamycin and 2% erythrmomycin are used.
- Topical retinoids, i.e. tretinoin cream or gel (0.25 to 1%), Adelphane (0.1%) cream or gel or solution applied in night to entire face and leave it for 20–30 minutes and then wash of with mild soap
- Sulphate calamine lotion can be used.
- Salicylic acid can be used as adjunctive therapy.
- Azelaic acid (20%) cream possess anti–microbial, anti inflmmatory and comedolytic properties.
Systemic therapy
- Antibiotics: Therapy is given for 3–6 months.
Tetracycline 500 mg BD or doxycycline 100 mg BD for 2 weeks to 10 months.
If tetracycline is not tolerated by the patient erythromycin 500 mg BD can be given - Corticosteroids: Prednisolone or dexamethasone once at night is useful in patients with severe acne unresponsive to conventional therapy.
- Other drugs: Oral contraceptives, spironolactone,fltamide help in young women
- Adjunctive therapy: Intralesional steroids for neurocystic lesions. Comedone extraction, chemical peels,dermabrasion, LASER and light therapy.
Question.12. Write short note on SLE.
Answer.
The full form of SLE is systemic lupus erythematosus.
It is an autoimmune disorder characterized by the destruction of tissue due to deposition of antibodies and immune complexes within it.
SLE produces lesion in the skin and oral mucous membrane and beside this it also involves certain body systems.
Clinical Features
- Skin lesions of SLE are characterized by the development of fied erythematous rashes thathave abuttrflconfiuration over the malar region and across the bridge of the nose.
- Skin rashes produce itching or burning sensation.
- Disease often causes hyperpigmentation of skin.
- Patchy or extensive loss of hair from the scalp is very common clinical fidings.
- There is severe burning sensation in the oral mucosa and the affcted area is extremely tendered to palpation.
- Formation of hemorrhagic macules in the oral mucosa that becomes frequently ulcerated.
- Fever, fatigue, malaise, vomiting, diarrhea and anorexia are present.
- Dysphagia and depression
- Splenomegaly and lymphadenopathy.
Treatment
Systemic steroid therapy is the treatment of choice.
Question.13. Write note on emergency drug tray.
Answer.
Medical emergencies in dental practice are of common occurrence and a dental surgeon must well prepare to meet them since correct and early management cannot only prevent morbidity but also mortality in such patients.
For management of any medical emergency dental clinic must consist of emergency drug tray.
Emergency tray contains IV fluids, administration set, disposable syringe and needles, stethoscope, BP apparatus, sterilized pad must be available.
A fare amount of emergency drugs such as the following must be readily available in the emergency drug tray.
- Inj. adrenaline
- Inj. atropine
- Inj. avil
- Inj. aminophylline
- Inj. methenamine
- Inj. dopamine
- Inj. lidocaine
- Inj. digoxin
- Inj. propranolol
- Inj. diazepam
- Inj. dilantin
- Inj. stemetil
- Inj. isoproterenol
- Inj. pethidine
- Inj. pentazocine
- Inj. morphine
- Inj. analgin
- Inj. diclofenac sodium
- Inj. dexamethasone
- Oxygen
- Capsule nifedipine
- Inj. serpasil
- Inj. glucose Or 5% dextrose saline.
- Inj. calcium carbonate
- Dextrose 50%
- Aromatic salts.
Question.14. Write short note on sepsis syndrome.
Answer.
It is defied as the inflmmatory response infection in which there is fever, tachycardia, tachypenia and evidence of inadequate blood flw to internal organs.
The syndrome is the common cause of death in severely ill patients.
Etiology
- It is caused due to combined effct of virulent infection and the powerful host response to the infection.
- Infection of lungs, abdomen and urinary tract.
- Infections at other body sites.
Complications
- Shock
- Organ failure
- Disseminated intravascular coagulation
- Altered mental status
- Jaundice
- Metastatic abscess formation.
Treatment
Eradication of underlying cause of infection and support of failing organ systems.
- Maintaining an open airway.
- IV flid is given.
- Adrenaline should be given to the patient.
- Draining or debriding abscess, if present.
- Heparin is given to lessen the risk of venous thrombosis.
- Antibiotics such as cephalosporins or penicillin are given.
Question.15. Mention complications of drug reaction.
Answer. The term adverse drug reaction has been defied as any noxious which is suspected to be due to a drug occur at doses normally used require treatment or decrease in dose or indicates caution in future use of same drug.
Adverse effct of drug have been classifid as:
Predictable reaction: These are related to the pharmacological effct of a drug. They include:
1. Side effects: These are unwanted but often unavoidable pharmacodynamic effect that occurs at therapeutic doses.
- A side effect may be based on the same action of the drug, for example, dryness of the mouth with atropine.
- A side effct may be based on a diffrent facet of action, for example estrogen causes nausea.
- An effct may be therapeutic in one contact but side effect in another contact, for example, codeine used for cough, produces constipation as a side effct.
2. Secondary effect: These are indirect consequences of a primary action of a drug, for example,suppressing of bacterial flra by tetracyclines can result in super infection.
- Toxic effects: These effcts are result due to over dosage or prolong use of drugs, for example,comma by barbiturates, complete AV block by digoxin.
- Drug habituation and dependence: Drugs capable of altering the moods and feeling, are liable to repetitive use to derive a feeling of euphoria to escape from the reality, social adjustment, etc.
- Drug withdrawal reaction: Sudden withdrawal or stoppage of certain drugs can result in a type of adverse reaction, e.g. withdrawal of beta
blockers can precipitate an effct of myocardial infarction. - Withdrawal of phenytoin can precipitate status epilepticus.
- Teratogenic effect: This refers to the ability of drug to cause congenital abnormality in the fetus,when given during pregnancy, e.g. cleft palate following the use of corticosteroids.
- Drug-induced disease or iatrogenic diseases: When certain drugs are used chronologically, they can produce disease, e.g. chronic use of aspirin can lead to production of peptic ulcer.
3. Unpredictable reactions: These are based on the peculiarities of the patient and not on the drug action.
- Drug allergy: It is an immunologically mediated reaction producing stereotype symptoms which are unrelated to the effct of drug or its doses, e.g. anaphylactic reactions resulting in urticaria,etching, angiedema, asthma.
- Photosensitivity: It is a cutaneous reaction,resulting from druginduced sensitization of the skin to UV radiation. Drugs that causes such reactions are demeclocycline, chloroquine.
- Idiosyncrasy: It is generally determined as abnormal reactivity to a chemical.
Certain adverse effects of some drugs are restricted to individuals with a particular genotype, e.g. barbiturates causes excitement and mental confusion in some person.
Question.16. Write short note on eczema.
Answer. Eczema is defied as an itchy red rash that initially weep or oozes serum and may become crusted, thickened or scaly.
Classification of Eczema
- Atopic
- Seborrhoeic
- Discoid
- Irritant
- Allergic
- Asteatotic
- Gravitational
- Lichen simplex
- Pompholyx.
Symptoms of eczema
Acute symptoms:
- Redness and swelling with ill defied margins.
- Papules, vesicles and more rending large blister.
- Exudation and cracking
- Scaling.
Chronic symptoms:
- Less vascular and exudative lichenification, i.e. a dry lathery thickening with increased skin margins,secondary to rubbing and scratching
- Fissures and stretch marks
- Pigmentation change.
Diagnostic Criteria
Itchy skin and at least three of the following:
- History of itch in skin creases
- History of asthma/hay fever.
- Dry skin
- Visible flxural eczema.
Management
General:
- Explanation, reassurance and encouragement
- Avoidance of contact with irritants
- Regular use of greasy emollients
Medical:
- Topical steroids, i.e. prednisolone and hydrocortisone are used.
- Topical immunosuppressants are used.
- Blend emollients are used regularly both directly on skin and in bath.
- Sedative antihistaminics, i.e. alimemazine tartrate or trimeprazine tartrate, if sleep is interrupted.
Question.17. Write short note on basic life support.
Answer. The aim of basic life support is to maintain the circulation,until more definitive treatment with advanced life support can be administered.
The management of the collapsed patient requires prompt assessment and restoration of the airway,breathing and circulation (ABC) using basic life support, with the aim of maintaining the circulation until more defiitive treatment with advanced life support can be administered.
Basic life support
Check responsiveness (Shake and shout)
↓
Open airway (Head tilt and chin tilt)
↓
Check breathing If breathing
(look, listen and feel) (Put in recovery position)
↓
Breathe (To effctive breaths)
↓
Assess Circulation present
(Signs of circulation) (Continue rescue breathing,10 seconds only)
↓
No circulation (Compress chest 100/min)
Question.18. Write short note on needle stick injury.
Answer. Needle stick injuries are wounds caused by needles that accidentally puncture the skin.
- Needle stick injuries are a hazard for people who work with hypodermic syringes and other needle equipment.
- These injuries can occur at any time: during use, disassembling or disposal.
- Needle stick injuries transmit infectious diseases,especially bloodborne viruses.
- In recent years, concern aboutAIDS, hepatitis B and hepatitis C has prompted research to fid out the causes of these injuries and develop measures to prevent them.
- Despite published guidelines and trainingprogramm,needle stick injuries remain an ongoing problem.
- Accidental punctures by contaminated needles can inject hazardous flids into the body through the skin.
There is potential for injection of hazardous drugs, but injection of infectious flids, especially blood, is by far the greatest concern. - Even small amounts of infectious flid can spread certain diseases effctively.
Accidental injection of bloodborne viruses is the major hazard of needle stick injuries, especially the viruses that cause AIDS (HIV), hepatitis B and hepatitis C.
Causes
- Equipment design: Safer innovative devices using protected needle devices or needlefree systems with selfsealing ports would alleviate many of these injuries.
Syringes with safety features reduce needle stick injuries. - Recapping: Recapping can account for 25 to 30% ofall needle stick injuries. Often, it is the single most common cause.
- Improper disposal: Virtually all needle stick injuries are from needles that have either been lost in the workplace or thrown into regular garbage.
Janitors and garbage handlers can also experience needle stick injuries or cuts from ’sharps’ when handling trash that contains needles or scalpels.
Management
- Stop all operative procedures.
- Identify and examine the wound
- Immediately wash but do not scrub the injury
- Encourage bleeding
- Blood specimen for both patient and health care worker is taken for specimen.
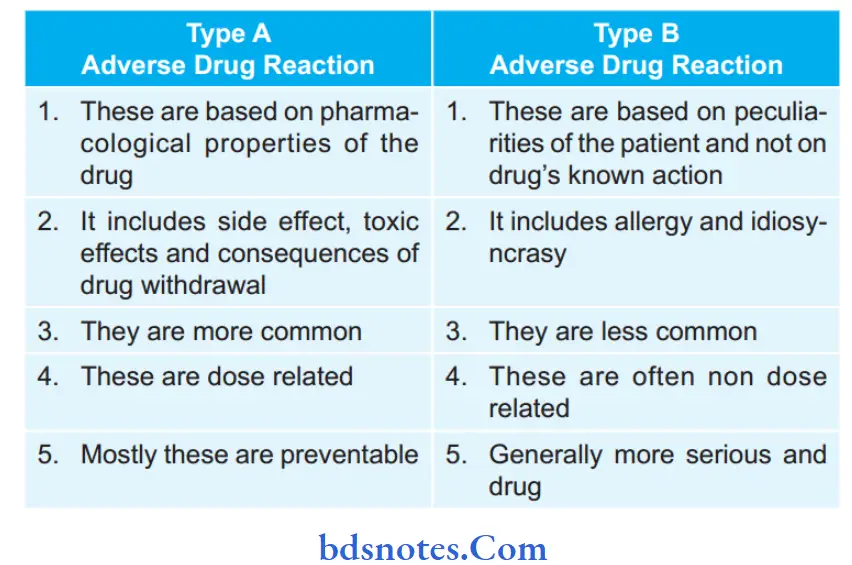
Question.19.Diffrentiate Type A and Type B adverse drug reaction.
Answer
Question.20. Describe treatment of septic shock.
Answer.
Septic Shock
This type of shock is mostly due to release of endotoxins in blood, which causes wide spread vasodilation of blood vessels resulting in fall in the cardiac output.
Fall in the cardiac output is not initial feature and vasoconstriction is not observed.
Bacteria responsible for release of endotoxins are E. coli,Pseudomonas proteus, etc.
Clinical Features
- Restlessness, anxiety
- Cyanosis
- Cold and clammy skin
- Tachycardia
- Oligouria or anuria
- Acidotic breathing.
Management
- Sedation with diazepam
- IV flids
- Blood culture and sensitivity
- Antimicrobial agents: Combination of penicillin or cephalosporins and aminoglycosides and metronidazole
- Injection hydrocortisone.
Question.21. Write short note on management of shock, while doing dental surgery.
Answer. In such case there following shock occurs:
Neurogenic Or Vasovagal Shock
- This is response to sudden fear or severe pain and the effcts from slight fainting fi to death.
- This type of shock is also known as neurogenic or psychogenic shock.
- There is sudden pooling of blood in the capacitance vessels of legs and splanchnic arterial bed. This causes hypoxia of vital center.
Clinical Features
- History of emotional stress or pain of a sudden nature.
- Bradycardia or pallor.
- Tachypenia
- Fainting
- Reflxes are usually intact.
Management
- Place the patient flt or in head low position.
- Ensure potency of airway
- IV atropine may be needed for persistent or increasing bradycardia.
Hypovolemic shock, i.e. Hemorrhagic shock
Management
- Control hemorrhage.
- IV flid is to restore circulating blood volume.
- Blood transfusion.
- Rising of foot end of bed.
- Oxygen inhalation.
- If acidosis develops. Sodium bicarbonate is infused till pH is normalized.
- Recovery is indicated by improvement in consciousness, dry and warm skin, CVP is more then 5 cm of H2O,distended veins and increased in urinary output.
Question.22. Write short note on ACE inhibitors.
Answer. The ACE inhibitors are Captopril, Enalapril and Ramipril.
Mechanism of action
- These drugs prevent conversion of angiotensin I into angiotensin II by inhibiting angiotensinconverting enzyme thus preventing action of angiotensin II, i.e. vasoconstriction and aldosterone synthesis and causes fall in BP
- ACE metabolizes bradykinin which is a potent vasodilator.
- ACE inhibitors increase bradykinin levels causing vasodilatation.
Pharmacological actions
- ACE inhibitors decrease total peripheral resistance, and hence there is decrease in systolic and diastolic blood pressure.
- ACE inhibitors increase blood supply to renal, cerebral and coronary arteries.
- ACE inhibitors causes decrease in aldosterone synthesis,and hence there is decrease in sodium and water retention.
Adverse Effects
ACE inhibitors produce hypotension, hyperkalemia, dry persistent cough, loss of taste sensation, urticaria, angiedema,etc.
Uses
- Hypertension: ACE inhibitors are fist line drugs to be used in the treatment of hypertension. They are used alone or in combination with other drugs. These drugs are more effctive in renovascular hypertension.
- Congestive heart failure: ACE inhibitors decreases preload and afterload in CHF.
- Diabetics: In diabetics, renal functions are improved.
- Myocardial infarction: In myocardial infarction motility is reduced.
Question.23. Write short note on ABCD rule.
Answer. This rule is given for diagnosis for malignant melanoma and skin cancers
- A is for ASYMMETRY: Half of a mole or birthmark does not match the other.
- B is for BORDER: The edges are irregular, ragged,notched, or blurred.
- C is for COLOR: The color is not the same all over,but may have diffring shades of brown or black,sometimes with patches of red, white, or blue.
- D is for DIAMETER: The area is larger than 6 millimeters (about ¼ inch) across, or the area has been growing.
Question.24. Write short note on statins.
Answer. They are also known as HMGCoA reductase inhibitors.
The statins are Lovastatin, Simvastatin, Pravastatin,Atorvastatin, Rosuvastatin.
The statins are the hypolipidaemic drugs.
Mechanism of action
- They decrease cholesterol synthesis by inhibition of 3-hydroxy-3-methyl glutaryl coenzyme A (HMG-CoA).
- Statins also decrease low density lipids (LDL) and triglycerides. They increases high density lipids (HDL).
Uses
- Used in hyperlipidemia with raised LDL and total cholesterol levels.
- Used in secondary hypercholestrolemia caused due to diabetes and nephritic syndrome.
Adverse Effects
- Headache, nausea, bowel upset and rashes
- Sleep disturbances
- Rise in serum transaminase
- Muscle tenderness can occur
- Myopathy can occur.
Question.25.Write short note on clinical uses and side effcts of prednisolone.
Answer. Prednisone is a synthetic corticosteroid drug that is particularly effctive as an immunosuppressant drug.
It is used to treat certain inflmmatory diseases (such as moderate allergic reactions) and (at higher doses) some types of cancer, but has signifiant adverse effcts.
Clinical Uses
- In asthma, chronic obstructive pulmonary disease (COPD), chronic inflammatory demyelinating polyradiculoneuropathy (CIDP), rheumatic disorders,allergic disorders, ulcerative colitis and Crohn’s disease, adrenocortical insuffiency, hypercalcemia due to cancer, thyroiditis, laryngitis, severe tuberculosis, urticaria(hives), lipid pneumonitis, pericarditis, multiple sclerosis,nephrotic syndrome, myasthenia gravis, and as part of a drug regimen to prevent rejection post organ transplant.
- Prednisone has also been used in the treatment of migraine headaches and cluster headaches and for severe aphthous ulcer.
- Prednisone is used as an antitumor drug.
- Prednisone is important in the treatment of acute lymphoblastic leukemia, nonHodgkin lymphomas, Hodgkin’s lymphoma, multiple myeloma and other hormonesensitive tumors, in combination with other anticancer drugs.
- Prednisone is also used for the treatment of the Herxheimer reaction, which is common during the treatment of syphilis, and to delay the onset of symptoms of Duchenne muscular dystrophy and also for uveitis.
- Prednisone also could be used in the treatment of decompensated heart failure
Side-effects
Major
- Increased blood sugar for diabetics
- Diffilty controlling emotion
- Diffilty in maintaining train of thought
- Immunosuppression
- Weight gain
- Facial swelling
- Depression, mania, psychosis, or other psychiatric symptoms
- Unusual fatigue or weakness
- Mental confusion / indecisiveness
- Blurred vision
- Abdominal pain
- Peptic ulcer
- Infections
- Painful hips or shoulders
- Steroidinduced osteoporosis
- Stretch marks
- Osteonecrosis
- Insomnia
- Severe joint pain
- Cataracts or glaucoma
- Anxiety
- Black stool
- Stomach pain or bloating
- Severe swelling
- Mouth sores or dry mouth
- Avascular necrosis
- Hepatic steatosis.
Minor
- Nervousness
- Acne
- Skin rash
- Appetite gain
- Hyperactivity
- Increased thirst
- Frequent urination
- Diarrhea
- Reduced intestinal flra
- Leg pain / cramps
- Sensitive teeth
Question.26. Write short note on drug reactions.
Answer.While achieving therapeutic levels drug produce unwanted side effects or toxicity. This is known as adverse drug reaction.
- Drug reactions are divided in two types i.e. predictable reactions in the form of side effcts, overdosage, toxicity and unpredictable reactions in form of idiosyncrasy and hypersensitivity reactions.
- Following are the adverse drug reactions:
- Side effect: Undesirable effcts which accompany therapeutic effcts ofdrug so does not necessitate stoppage of drug, e.g. Anticholinergics in treatment of peptic ulcer cause xerostomia.
- Toxic effct: They develop when drug is used for the longer period in therapeutic doses, e.g.
Patient taking isoniazid for tuberculosis develop peripheral neuropathy. - Poisoning: It occurs when large doses of drug are consumed for prolonged periods.
- Drug Intolerance: Some people are intolerant to the drug in small therapeutic doses, It is due to low threshold of the person to the drug, e.g.
Chloroquine in usual doses cause nausea and vomiting while in an intolerant person it causes vomiting with single tablet. - Idiosyncrasy: It is an abnormal reaction to any drug which occur in individuals who are genetically predisposed to it.
- Drug allergy: Allergy to any drug is independent of its dose. These reactions are based on humoral factor or cell mediated.
- Photosensitivity: Exposure of skin to ultraviolet rays of sun results in cutaneous reactions from drug induced sensitization.
- Teratogenicity: A drug is teratogenic when it harms the fetus. Such types of drugs should not be given to pregnant ladies.
Question.27. Evaluation for the case of general anesthesia.
Or
Write a short note on evaluation for the case of general anesthesia.
Answer.
History of Patient
- Detailed history of patient is taken about any major ailment in the past and recently.
Confirm the type of treatment given and if any residual effcts of disease are still persisting. - History of alcohol intake and addiction to other narcotic agents is taken.
- Some patients are allergic to certain drugs and general anesthesia.
It must be thoroughly ascertained, if the person is allergic to any of these drugs. - If a patient is chronic smoker, he / she is likely to have chronic cough and this has to be considered when giving general anesthesia.
- If there is presence of hypertension, the drugs being taken must be ascertained and recorded.
Anesthetist should assess degree of hypertension and its effct on the heart as well as any interaction of the antihypertensive drugs with the anesthetic agents. - If the patient is suffring from cardiac insuffiency the heart must be evaluated and certain emergency drugs must be kept at hand during operative procedure.
A detailed history about all drugs the patient is on anticoagulants,digoxin, nitrates, diuretics or any other drug must be enquired and recorded.
Physical examination
- A detailed general physical examination must be done preoperatively.
- Look for anaemia and state of nutrition. Patient who is severely anemic is not fi for general anesthesia. Anemia must be corrected before. If emergency operation is to be done, blood transfusion is given.
- Pulse rate should be in between 60–80 beats per minute. If the pulse rate is either high or slow, cause must be found out, and if possible it should be corrected.
- Blood pressure must be evaluated carefully.
Neither high or low blood pressure is desirable.
An hypertensive must be treated before going for general anesthesia and blood pressure levels brought to normal or near normal levels.
But if complications are present such as cardiomegaly,renal or lung complications or features of left heart or congestive failure, then great caution has to be employed. - Lungs are examined for evidence of chronic bronchitis with or without emphysema and other lung diseases.
Look for clubbing, cyanosis and emphysema. Patient’s respiratory functions must be evaluated.
A chronic smoker is likely to be at disadvantage.
For this breadth holding test is done.
In such patients, it is desirable to institute breathing exercises for at least a week before operation and the patient is encouraged to continue with these exercises as soon as he regains consciousness. In this way, many pulmonary complications are avoided.
Breathing exercises program must be carried out under the guidance of a physiotherapist with advice from the physician. - Abdomen should be examined for hepatomegaly,splenomegaly, ascites and any organomegaly.
Lymph glands in the body should be palpated for evidence of any disease of reticuloendothelial system. - Bleeding tendencies must be looked into. History of bleed from any source after any simple injury or bruising should be considered.
- Oral cavity must be carefully examined, and if any loose teeth are present or if there is any great degree of sepsis these should be taken care of before operation.
In patients using dentures these must be removed before administering premedication since failure to do this may choke the patient. - Patient color should be carefully examined and if any signs of anemia or polycythemia are present they must be attnded to.
- Urine should be carefully tested, and if any evidence of diabetes is present, blood sugar estimations be done.
Urine be examined not only for sugar but also for albumin and ketone bodies.
Diabetes must be controlled before hand with insulin. In the presence of ketone bodies, it is usual to institute 10 % glucose drip neutralizing with 25 units of soluble insulin in each botte.
This infusion is given till urine is ketone free.
It is preferable in any diabetic patient who is on oral antidiabetic drugs, to switch on to soluble insulin 48 hours before operation.
On the day of operation, patient is put on 5% or 10% glucose drip neutralized with soluble insulin.
After operation, patient has to be continued on insulin injections till the wound has healed.
This may have to be carried out for 10–14 days. Once recovery is complete and patient is ambulatory he can be switched on to oral antidiabetic drugs. - If urine contains considerable amount of albumin, this indicates renal pathology and anesthetist in consultation with the physician must evaluate the risks and the type of anesthesia.
- Heart size must be evaluated. Position of apex beat,presence of abnormal pulsations over the precordium and cardiac murmurs must be assessed.
- Look for patient veins especially over the ankles and antecubital fossa. Suitable veins must be identifid for intravenous purposes.
Investigations
In every patient due for general anesthesia following investigations be carried out:
- Hemoglobin to assess anemia.
- Total and diffrential leucocyte count.
- Bleeding time (BT) and clottng time (CT) for bleeding disorders.
- Platelet count: Low platelet count indicates thrombocytopenia.
- Complete urine examination for albumin, sugar, ketone bodies and presence of any casts and cells.
- Blood sugar (fasting and postprandial) to exclude diabetes.
- Prothrombin time for bleeding disorders.
- X-ray heart (PA view) for heart size: It shall also assess any pathology in the lungs.
- Electrocardiogram for any myocardial damage or insuffiency or presence of any arrhythmia.
- Pulmonary function tests to evaluate the lung functions.
Patient preparation before giving general anesthesia
- On the day of surgery, patient should be empty stomach.
- Litte bowel enema is given to patient so that his / her bowels are empty.
- Breathing exercises are performed a week before.
- Smokers should stop smoking 2 to 3 weeks before general anesthesia for preventing pulmonary complications during and after anesthesia.
- Sleeping pill is given to a patient in night so that proper sleep is taken
- Preanesthetic medication is given which helps in induction of general anesthesia.
Question.28. Write about medical emergencies in dental practice.
Or
Write short note on medical emergencies in dental practice.
Answer. Medical Emergencies in Dental Practice
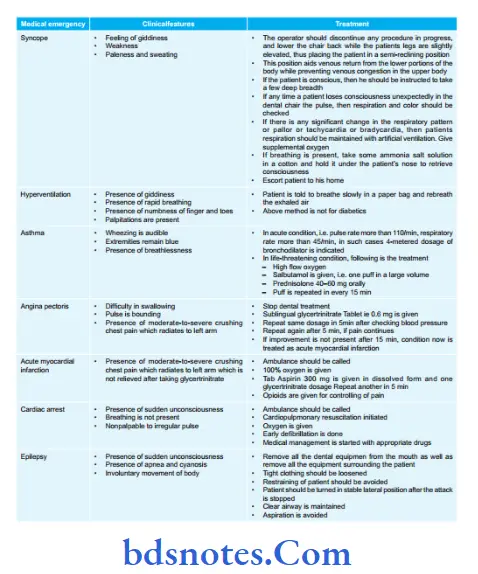
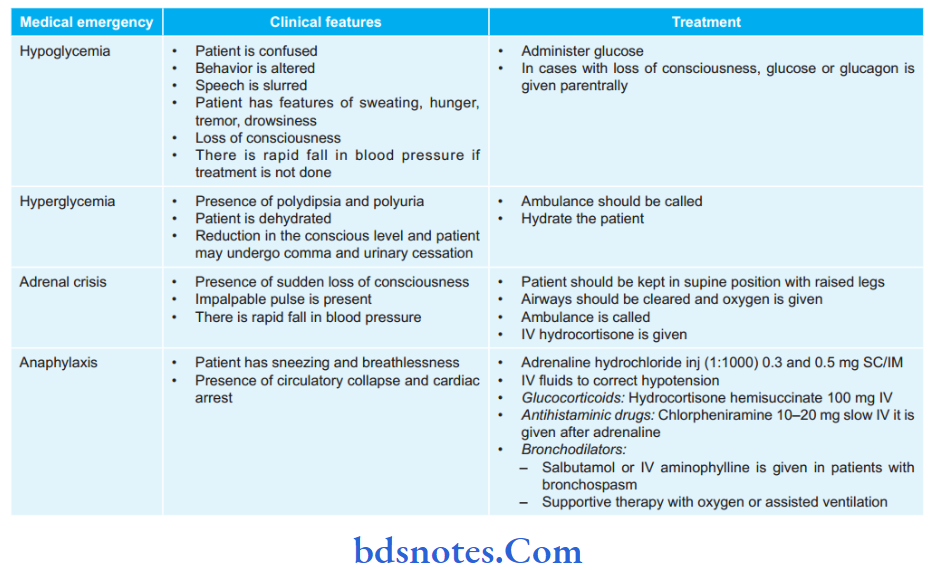
Question.29. Write short note on anaphylactic shock with diagnosis and management.
Answer. Anaphylaxis is defied as a state of rapid developing immune response to an antigen mediated by IgE antibodies.
Diagnosis
Diagnosis is based on physical examination and investigations.
Physical examination
- Presence of immediate respiration diffilty, laryngeal edema with stridor and wheeze is audible.
- Wheal and erythematous lesions are seen which are circumscribed, round, discrete, erythematous areas with irregular borders and blanched centres.
- Lesions are very pruritic.
Investigations
- Skin-Prick test: When an allergen is injected into the skin and is observed for the development of wheal and induration within 15 minutes.
There is a good correlation between diameter of wheal and levels of specifi IgE antibodies in serum. - In vitro radioallergosorbent test (RAST) is done to detect allergen specifi IgE for a variety of food, insect bites / stings, venom, latex and some drugs.
- Serum tryptase levels are done for detection of recent anaphylaxis.
Question.30. Discuss the clinical presentation and management of anaphylactic shock.
Answer.
Clinical Presentation
- Onset may be instantaneous or within a few minutes after the IV injection and 30 minutes after exposure.
- Cardiovascular: Tachycardia, arrhythmia, hypotension and circulatory collapse.
- Respiratory: Laryngeal obstruction, angiedema,bronchospasm or pulmonary edema may occur singly or in combination.
- Nervous: Syncope and seizures.
- GIT: Diaphoresis, abdominal pain and diarrhea may occur.
- Skin: Wheel and erythematous lesions are seen which are circumscribed, round, discrete, erythematous areas with irregular borders and blanched centres.
- Lesions are very pruritic.
- If not treated death may occur.
Question.31. Write short note on aspirin.
Answer. Chemical name of aspirin is acetyl salicylic acid.
Pharmacological action
- It decreases the temperature by bringing temperature regulating centre to normal when it becomes deranged.
- Aspirin block pain centre in thalamus. It also inhibits synthesis of prostaglandins and prevent sensation of pain receptors to histamine, bradykinin and 5 hydroxytryptamine, mediators ofpain and inflmmation.
- Aspirin inhibits platelet aggregation by inhibiting ADP release from platelets and inhibiting the synthesis of prostaglandin, endoperoxidase and thromboxane A2.
Indications
- It acts as keratolytic, fungistatic and mild antiseptic.
- As analgesic, antipyretic and antirheumatic.
- It prevents platelet aggregation.
Side Effects
- Nausea and vomiting
- Increases prothrombin time.
- Fatt infitration of liver and kidney.
- Salicylism: Headache, dizziness, vertigo, tinnitus,
diminished hearing and vision. - It causes respiratory depression.
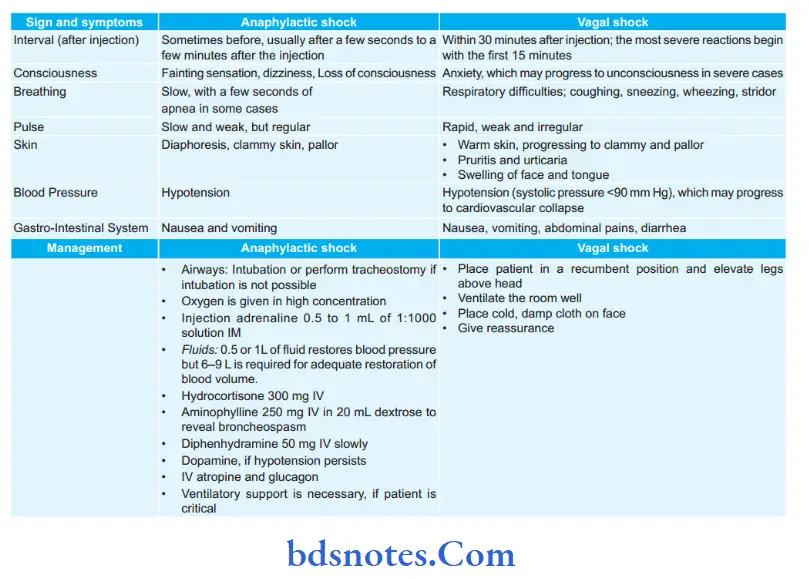
Question.32. Tabulate the differences, clinical features and management of anaphylactic shock and vagal shock.
Answer. Tabulation of diffrences between anaphylactic shock and vagal shock.
Question.33. Write down and discuss six common comorbid diseases where you should take medical consultation before dental extraction.
Answer. Comorbidity is the presence of one or more additional disorders or diseases cooccurring with a primary disease or disorder; or the effct of such additional disorders or diseases.
The additional disorder may also be a behavioral or mental disorder.
Following are the six comorbid diseases for which one should take medical consultation before dental extraction:
1. Diabetes mellitus
2. Seizure
3. AIDS
4. Cardiovascular risks
5. Respiratory disorders
6. Blood dyscrasias.
Diabetes Mellitus
There are three types of diabetes: Type I is considered insulin dependent, 5–10% of cases; Type II is when the body does not produce enough insulin and, therefore diet and medication may be regulated; Gestational diabetes occurs during pregnancy and is reversed after delivery.
If the patient indicates that they have diabetes, the type must be noted in the history.
Patients with uncontrolled diabetes have low resistance to infection and are prone to periodontal disease.
They have poor healing response, including excessive bleeding, and may experience hypoglycemia or hyperglycemia during dental treatment.
Patients who are undiagnosed diabetics may report the following symptoms: excessive thirst and hunger, increased urination, and higher birth weights in babies.
When reviewing a health history, the following questions should be asked of diabetic patients:
- Is your diabetes well controlled?
- When is the last time your blood glucose was checked?
- Are you currently taking oral antidiabetic medicationsor insulin injections?
- When was the last time you ate?
- Did you take your medication on time today?
It is advisable to keep sources of sugar on hand for hyper or hypoglycemic episodes.
Glucose gel from a pharmacy,granulated sugar packets, honey packets, or tubes of cake icingcan be easily stored and used in the case of an emergency.
When questioning diabetic patients before treatment and you fid out they have not eaten or taken their insulin, their appointment should be rescheduled.
Make sure they understand the importance of these steps to maintain a normal blood sugar level during dental treatment.
After approximately 8 hours of fasting, an average range is between 70–99 mg / dL. If they have eaten an average level should be less that 140 mg / DL.
A strategy for making a dental appointment for a diabetic patient is to keep it short and in the early to midmorning hours when sugar levels are more stable.
Seizure
Seizure disorder is caused by an electrical disturbance in the brain. Any person can experience a seizure in a stressful situation and approximately half of all seizures are considered idiopathic.
Epilepsy is a condition commonly associated with a syndrome of associated seizure types.
When a known epileptic patient is scheduled for treatment, the dental team should determine, if the patient has taken his / her antiseizure medication.
These patients should be scheduled for short appointments, when they are well rested.
Patients often report an aura before experiencing a seizure.
This aura can be a sound, feeling, or smell.
Shining a bright light in the patient’s eyes should be avoided, since this has been known to trigger a seizure.
Patients who are taking oral anticonvulsant medications, such as Dilantin, Zarontin, or Depacon, may experience gingival hyperplasia.
Emphasis must be placed on meticulous home care to prevent serious periodontal problems and the increased need for regular dental visits.
Cardiovascular Risks
Patients who state that they have experienced chest pain, shortness of breath, pain that radiates down their neck or arm, have swollen ankles, and / or have high blood pressure are at risk for cardiovascular disease.
They may or may not have been diagnosed by a physician.
If this patient also indicates that they are a smoker and / or are overweight, the risk is increased.
It is recommended that a medical consultation or evaluation be obtained for all patients who indicate some type of cardiovascular disease on their health histories.
Additionally,medical consultations should also be obtained for patients who are reporting or exhibiting symptoms of cardiovascular disease,but have not had a defiitive diagnosis. Preventing medical crises during dental treatment is the best method of protecting patients who are medically compromised.
Rheumatic heart disease is a result of rheumatic fever and can cause deformities in the heart valves.
Some patients will report taking antibiotics on a regular basis, although this is not a required practice.
If the patient reports a history of rheumatic fever, the dental practice must consult with the patient’s physician to determine the extent of the heart involvement.
This assessment will determine the need for antibiotic prophylaxis.
Congenital heart defects place the patient at high risk for bacterial endocarditis.
Again, a statement from a physician is advisable to determine the type of defect and to verify the need for prophylactic antibiotics.
Coronary artery disease results from atherosclerosis. Patients may report having been diagnosed with angina pectoris, or having chest pain after some type of physical activity or stress.
These patients may be taking several medications, particularly vasodilators such as nitroglycerin; or beta-blockers, such as propanolol.
The stress of a dental visit may cause an angina attck, therefore it is important to minimize patient stress, maximize patient comfort and make certain that the patient has his / her medications available, particularly nitroglycerin.
In addition, it is recommended that local anesthetic without epinephrine or other vasoconstrictors be used for these patients,to avoid further constriction of the blood vessels.
Patients with unstable or uncontrolled angina should wait for at least 30 days after their angina is stabilized to receive dental treatment.
Myocardial infarction is more commonly known as a heart attck.
Patients who have experienced a recent myocardial infarction should not receive any dental treatment for a minimum of 6 months after the heart attck.
Most fatalities from myocardial infarction occur within 3–4 months after the attck.
Stressful situations, like dental treatment can cause a rupture in the area of infarct, leading to further health problems and possible death.
Hypertension is a common condition characterized by high blood pressure.
Patients with uncontrolled hypertension are at risk for a stroke, kidney failure, or heart attck.
Since stress will increase blood pressure, dental treatment is contraindicated in patients with severe hypertension.
Patients presenting with a systolic pressure between 120–139 mm Hg should be advised to monitor their readings for improvement and see their physician for assessment.
As a rule, patients with a systolic pressure greater than 160 mm Hg and / or a diastolic pressure greater than 95 mm Hg should be referred for medical consultation and treatment, dental treatment should be delayed.
It is relatively common for patients to have undiagnosed hypertension, making it very important for the dental team to monitor patient’s vital signs during their dental visits.
A patient who reports having frequent dizziness, nosebleeds, or headaches may have high blood pressure and may be in need of medical intervention with antihypertensive drugs and / or diuretics.
Heart failure was more commonly known as “congestive heart failure” but the American Heart Association has recently renamed and shortened the title to characterize a broader spectrum of the disease.
Depending on the type of heart failure,patients will typically have swollen ankles and shortness of breath, due to poor circulation and flids backing up in the lungs.
These patients may indicate that they must sleep upright or with several pillows. In these cases, placing them in a supine position for dental treatment may cause them acute distress.
Heart failure patients are usually taking one or more diuretic medications to remove flid.
Supplemental oxygen may be needed for these patients and use of nitrous oxide analgesia is contraindicated.
Respiratory Disorders
Asthma is a chronic respiratory disorder that results in a narrowing of airways.
An asthma attck can be triggered in several ways including environmental allergens, medications,or exercise.
Patients with asthma may be prone to an attck or episode brought on by the stress of dental treatment, or exposure to an allergenlike latex.
The patient must always be instructed to bring his / her medication / inhaler to each appointment.
When the health history is reviewed at the beginning of treatment, the patient should be able to produce the medication or inhaler just in case it is needed.
Chronic Obstructive Pulmonary Disease (CoPd)
The two most common forms of COPD are emphysema and chronic bronchitis.
Emphysema is the irreversible enlargement of the air sacs in the lungs making it hard to expel all oxygen during breathing.
Chronic bronchitis is characterized as the irreversible condition of narrowed airways.
Like patients with heart failure, those with either of these types of COPD may not be able to breathe easily in a supine position or after walking certain distances.
Due to prolonged steroid use to treat their COPD, these patients may have Candida infections.
Before dental extraction medical consultation of such patients is necessary.
Tuberculosis (TB) is a bacterial infection that occurs primarily in the lungs, but can occur in other organ systems in the body.
It is spread through airborne particles, when an infectious patient coughs, sneezes, talks, or sings.
TB is most easily spread in small confied spaces where infectious people share the same airspace with others.
Because TB is highly infectious and its airborne transmission is diffilt to control, CDC has issued specifi guidelines to help protect healthcare workers when treating patients.
In the case of TB, these guidelines state that elective, (nonemergency) dental treatment should be postponed for patients who have or are suspected of having an active, infectious TB case.
If these patients can be referred for treatment in a facility that is specifially designed to treat TB patients (e.g. a hospital settng), it is acceptable for the dental practice to make this referral and not be liable for discriminatory practices.
In addition to asking patients on their health history if they have had TB, the patients should also be asked if they have experienced any of the following symptoms: night sweats,unexplained fever, weight loss, or a prolonged or bloody cough.
If a patient has experienced any of these symptoms, refer them to a physician for evaluation before proceeding with anything but emergency palliative treatment.
If emergency treatment must be performed on a patient suspected of having infectious TB, the following precautions should be taken:
- Schedule the patient at the end of the day, as the last patient treated.
- All team members present in the treatment room must wear a HEPA or NIOSH N95 mask.
- High volume evacuation and dental dam isolation must be used to reduce aerosols.
AIDS
AIDS is a viral infection that impairs a patient’s immune system, making the patient highly susceptible to other infectious diseases.
It is transmittd through blood and other body flids, which puts dental healthcare workers at some risk of infection from treating patients.
Again, the practice of standard precautions must be followed, since many patients will not disclose their HIV positive status for fear of humiliation or rejection.
Remember that information about a patient’s HIV positive status is highly sensitive and must be protected.
The dental team must take every precaution to protect the confientiality of that patient’s health history.
Although some dental health care workers are fearful of treating AIDS patients, it is illegal not to accept them into a dental practice or to refer them to another practice, unless the type of treatment is not performed in that practice.
For example, if a general dental practice does not perform periodontal surgeries,it is legal to refer HIV positive or AIDS patients to a periodontist,since nonHIV or nonAIDS patients are referred as well.
However, if only the HIV positive or AIDS patients are referred for periodontal surgery, this would be considered discriminatory.
When treating patients with full blown AIDS, who are typically immunosuppressed, the dental team should take extra precautions to protect the patient from opportunistic infections.
These may include wearing sterile surgical gloves rather than nonsterile exam gloves, having the patient use a pretreatment rinse of chlorhexidine gluconate or other mouthwash to prevent bacteremia, and using only sterile water for irrigation rather than from the air / water syringe, which may contain some bacterial contamination.
Blood Dyscrasias
Anemia is a defiiency of red blood cells, caused by vitamin or iron defiiency or bone marrow problems.
An anemic patient may have problems with slow wound healing and excessive bleeding.
They may report feeling weak and fatigued, and may appear very pale.
If a patient exhibits these symptoms a medical evaluation should be recommended before dental extraction.
Leukemia is a type of blood cancer, where there is an overgrowth of white blood cells.
These white blood cells may displace red blood cells, used to transport oxygen in the blood.
These patients may exhibit oral signs, often before other symptoms of their disease.
These signs typically include excessive gingival irritation in the absence of other causative agents, such as heavy plaque or calculus.
Patients with leukemia are very prone to infections, including periodontal infections. In addition, the chemotherapeutic agents used to treat the disease have many side effcts, most notably xerostomia (dry mouth).
Consult the treating physician before proceeding with dental treatment.
Hemorrhagic disorders are ailments in which patients experience excessive bleeding, due to a defiiency of clottng factors in their blood.
Common bleeding disorders are hemophilia A and B, factor II, V, VII, X, XII, and von Willebrand’s disease.
A patient with one of these disorders will bruise very easily,may experience spontaneous, excessive bleeding, including unprovoked epistaxis (bleeding from the nose).
Dental treatment, such as extractions, that may cause bleeding can be risky for these patients.
Close monitoring by the physician is necessary before dental extraction.
Extraction should be confied to specifi areas (e.g. one tooth or quadrant at a time) and transfusion with clottng factors may be necessary prior to treatment.
Aspirin must never be prescribed for pain control for these patients, since it is a natural blood thinner and increases bleeding.
Question.34. Write short answer on shock.
Answer. Shock is defined as an acute clinical syndrome characterized by a significant, systemic reduction in tissue perfusion, resulting in decreased tissue oxygen delivery and insuffient removal of cellular metabolic products, resulting in tissue injury and severe dysfunction of vital organs.
It can occur either because the function of the heart itself is impaired, or because heart is inadequately filed.
Classification of Shock
Following is the classifiation of shock:
- Hypovolemic shock
- Cardiogenic shock
- Distributive shock:
- Septic shock
- Anaphylactic shock
- Neurogenic shock
- Obstructive shock.
Clinical Features
- Cold clammy skin, profuse sweating
- Hypotension (systolic BP <100 mmHg)
- Tachycardia with thready pulse
- Rapid, shallow respiration
- Restlessness, drowsiness, confusion
- Oliguria, may progress to anuria
- Jugular venous pressure elevated in cardiogenic shock,reduced in hypovolaemic and anaphylactic shock, variable in septic shock
- Multiorgan failure
Stages Of Shock
Stage l: Stage of compensatory shock—by neuroendocrine response to maintain the perfusion of the vital organs like brain,heart, kidney, liver.
Stage 2: Stage of decompensatory shock—where there is progressive shock causing persistent shock with severe hypotension (with mean arterial pressure <65 mm Hg); oliguria,tachycardia.
Stage 3: Stage of irreversible shock with severe hypoxia and Multi organ dysfunction syndrome (MODS).
Causes Of Shock
Hypovolemic shock
Due to reduction in total blood volume. It may be due to:
Hemorrhage:
- External from wounds, open fractures
- Internal from injury to spleen, liver, mesentery or pelvis.
- Severe burns, which results in loss of plasma
- Peritonitis, intestinal obstruction
- Vomiting and diarrhea of any cause
Cardiac causes:
- Acute myocardial infarction, acute carditis
- Acute pulmonary embolism wherein embolus blocks the pulmonary artery at bifurcation or one of the major branches
- Drug induced
- Toxemia of any causes
- Cardiac surgical conditions like valvular diseases,congenital heart diseases
- Cardiac compression causes:
- Cardiac tamponade due to collection of blood,pus, flid in the pericardial space which prevents the heart to expand leading to shock.
- Trauma to heart.
- Septic shock—is due to bacterial infections which release toxins leading to shock.
- Neurogenic shock—due to sudden anxious or painful stimuli causing severe splanchnic vessel vasodilatation.
Here patient either goes for cardiac arrest and dies or recovers fully spontaneously—spinal cord injury/anaesthesia can cause neurogenic shock. - Anaphylactic shock—is due to type I hypersensitivity reaction
- Respiratory causes:
- Atelectasis (collapse) of lung
- Thoracic injuries
- Tension pneumothorax
- Anesthetic complications.
- Other causes:
- Acute adrenal insuffiency (Addison’s disease)
- Myxedema
Investigations and Monitoring of shock
- Regular monitoring with blood pressure, pulse, heart rate, respiratory rate, urine output measurement (hourly) should be done.
Urine output should be more than 0.5 ml/kg/hour. Pulse oximetry should be used. - Central venous pressure (CVP), pulmonary capillary wedge pressure (PCWP—an accurate assessment of left ventricular/function) monitoring should be done.
ICU care is needed during monitor period.
But both CVP and PCWP are not accurate method of assessing tissue perfusion.
Complete blood count, ESR, pH assessment, serum electrolyte estimation, chest Xray (to rule out acute respiratory distress syndrome/pulmonary problems). - Pus/urine/blood/bile/sputum cultures depending on the focus and need in sepsis.
- Serum lactate estimation is an important prognostic factor.
Level >2 mEq/L suggest tissue ischemia. - USG of a part, CT/MRI of the location of pathology of standard focus should be done; often may require repeti¬tion of these imaging to assess progress.
- Blood urea, serum creatinine, liver function tests,prothrombin time (PT), activated partial thromboplastin time (APTT), ECG monitoring are also should be done.
- All these tests including platelet count and arterial blood gas (ABG) should be repeated at regular intervals.
Treatment Of Shock
- Treat the cause, e.g. arrest hemorrhage, drain pus.
- Fluid replacement: Plasma, normal saline, dextrose,Ringer’s lactate, plasma expander (haemaccel).
Dosage is maximum l liter can be given in 24 hours. Initially crystalloids then colloids are given.
Blood transfusion is done whenever required. - Ionotropic agents: Dopamine, dobutamine, adrenaline infusions—mainly in distributive shock like septic shock.
- Correction of acidbase balance: Acidosis is corrected by using 8.4% sodium bicarbonate intravenously.
- Steroid is often lifesaving. 500–l000 mg of hydrocortisone can be given.
It improves the perfusion, reduces the capil¬lary leakage and systemic inflmmatory effcts. - Antibiotics in patients with sepsis; proper control of blood sugar and ketosis in diabetic patients.
- Catheterization to measure urine output (30–50 mL/hour or > 0.5 mL/kg/hour should be maintained).
- Nasal oxygen to improve oxygenation or ventilator support with intensive care unit monitoring has to be done.
- Central venous pressure line to perfuse adequately and to monitor flid balance. Total parentral nutrition is given when required.
- Pulmonary capillary wedge pressure to monitor very critical patient.
- Hemodialysis may be necessary when kidneys are not functioning.
- Control pain—using morphine (4 mg IV).
- Ventilator and ICU/critical care management.
- Injection ranitidine IV or omeprazole IV or pantoprazole IV.
- Activated protein even though costly is benefiial as it prevents the release and action of inflmmatory response.
- MAST(Military Anti shock Trouser ) provides circumferen¬tial external pressure of 40 mm Hg.
lt is wrapped around lower limbs and abdomen, and inflted with required pres¬sure.
It redistributes the existing blood and flid towards center. It should be deflted carefully and gradually.

Leave a Reply