Malarial Parasite
Question 1. Describe morphology, life cycle, pathogenicity and laboratory diagnosis of Plasmodium vivax.
Answer:
Morphology of Plasmodium Vivax
The morphology of Plasmodium vivax is based on its various morphological forms which is as follows:
- Sporozoites:
- They are narrow and slightly curved.
- Sporozoites are of two types, i.e. tachy—fast and brady— slow
- Pre-erythrocytic Schizogony:
- Its size is 42 µ in diameter
- The number of merozoites present per schizont are 10,000 to 12,000
- Merozoites invade reticulocytes and younger RBCs.
- Erythrocytic Schizogony:
- Each RBC is invaded by one parasite
- The percentage of infected RBC is 1 to 2%.
- Trophozoite:
- Ring stage: It is 2.5 to 3 µ and is large. They are motile. Its cytoplasm is blue, the nucleus is red and the vacuole remains unstained.
- Amoeboid form: It is large, irregular, accumulates pigment, RBC becomes irregular, it loses red color, and becomes colorless.
- Schizont:
- Early schizont: It is of 9 to 10µ. It is round, the vacuole disappears, and the nucleus is large and lies at the periphery.
- Late and mature schizont: The nucleus divides to form daughter nuclei and develops into merozoites with a central nucleus and the surrounding cytoplasm. The size of merozoite is 1.5 to 1.75 × 0.75 µ. Their number is 12 to 24 and is arranged in rosette form.
- Gametocyte:
- The size of male gametocytes is 9 to 10 µ and of female gametocytes is 10 to 12 µ.
- The shape of both male and female gametocytes is spherical.
- The cytoplasm of male gametocytes is light blue while female gametocytes is deep blue.
- The nucleus of the male gametocyte is large diffs and the female gametocyte is small and compact.
Read And Learn More: Microbiology Question And Answers
Life Cycle of Plasmodium Vivax (Given in below diagram)
The malarial parasite passes its life cycle in two hosts, i.e. man which is the intermediate host, and the female anopheles mosquito which is the definitive host. The asexual development of parasites occurs in men and sexual development in mosquitoes.
Human Cycle: Man get an infection when it gets bitten by infected mosquito and sporozoites are introduced directly into blood circulation.
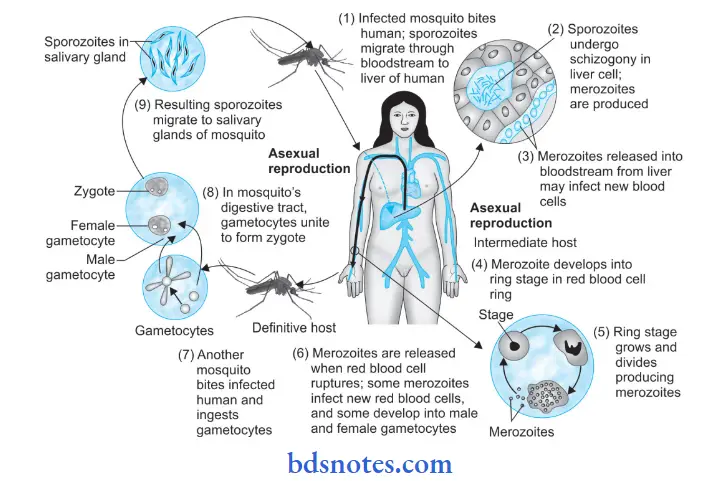
The human cycle start and it has the following phases:
- Pre-erythrocytic schizogony.
- Erythrocytic schizogony.
- Gametogony.
- Exo-erythrocytic schizogony.
- Pre-erythrocytic Schizogony:
- Sporozoites undergo a developmental phase inside the liver cells. This phase of development is known as pre erythrocytic schizogony.
- Within 1 hour, all the sporozoites which are entered directly in the blood leave the bloodstream and enter into liver parenchymal cells to start pre-erythrocytic schizogony.
- The sporozoites become rounded inside the liver parenchymal cells. They undergo multiple nuclear divisions and develop into schizonts.
- The size of the schizont is 9 to 10 µm in diameter and almost completely fills an enlarged erythrocyte. The pre-erythrocytic cycle lasts for 8 days in P. vivax.
- After completion of this cycle, the liver cells rupture and release merozoites into the bloodstream
- Erythrocytic Schizogony: The merozoites released from pre-erythrocytic schizogony penetrate red blood cells. They pass through the stages of trophozoite, schizont, and merozoite.
- In P. vivax trophozoite is irregular, amoeboid and vacuole is present.
- In P. vivax there are 12 to 24 merozoites in red blood cell.
- The red blood cells rupture to release the merozoites which attack new red blood cells and continue their erythrocytic schizogony repeating the cycle.
- The parasitic multiplication during the erythrocytic stage is responsible for the clinical attack of malaria.
- The duration of erythrocytic schizogony is 48 hours.
- Gametogony:
- Some merozoites of erythrocytic schizogony develop into male and female gametocytes known as microgametocytes and macrogametocytes respectively.
- They develop in the red blood cells of the capillaries of internal organs such as the spleen and bone marrow. These are sexual forms and only mature gametocytes are found in the peripheral blood.
- The microgametocytes (male gametocytes) are smaller in size, spherical, cytoplasm stains light blue and the nucleus is large and diffuse.
- Macrogametocytes (female gametocytes) are larger, spherical and the cytoplasm stains deep blue and the nucleus is small and compact.
- Exo-erythrocytic Schizogony:
- The exo-erythrocytic cycle resembles the pre-erythrocytic cycle.
- In case of P. vivax infections, some sporozoites on entering into liver cells, do not undergo asexual multiplication but enter into a resting (dormant) phase. The resting stage of the parasite is known as hypnozoite.
- It is rounded, uninucleate, and 4 to 6 µm in diameter.
- After some period hypnozoites reactivate to become schizonts and release merozoites.
- Merozoites attack red blood cells and lead to the relapse of malaria.
- Mosquito Cycle:
- The sexual cycle of the malarial parasite starts in the human host by the formation of gametocytes which are then transferred to the mosquito for growth.
- A female anopheles during its blood meal from the infected human, takes both the asexual and sexual forms of parasite.
- Only the mature sexual forms are capable of further development in mosquitoes and rest of the forms die immediately.
- In the midgut of the mosquito, one microgametocyte develops into 4 to 8 thread-like filamentous structures named microgametes by the process of flagellation.
- From one macrogametocyte only one macrogamete is formed.
- Fertilization occurs when a microgamete penetrates into a macrogamete.
- The fertilized macrogamete is known as a zygote. Within the next 24 hours, the zygote lengthens and matures into an ookinete. This is a motile vermiculate stage.
- Ookinete convert into an oocyst.
- As the oocyst matures, it increases in size and a large number of sporozoites develop inside it.
- The number of oocysts in the stomach wall varies from a few to more than a hundred.
- Oocyst ruptures and releases sporozoites in the body cavity of the mosquito.
- Sporozoites are distributed into various organs and tissues of the mosquito. However, they have a special predilection for salivary glands.
- The mosquito is now capable of transmitting the infection to man.
Pathogenicity And Laboratory Diagnosis
Pathogenicity:
Infection with P. vivax causes intermittent fever known as Vivax malaria or benign tertian malaria. Fever recurs after an interval of 48 hours or every third day so it is called Tertian malaria.
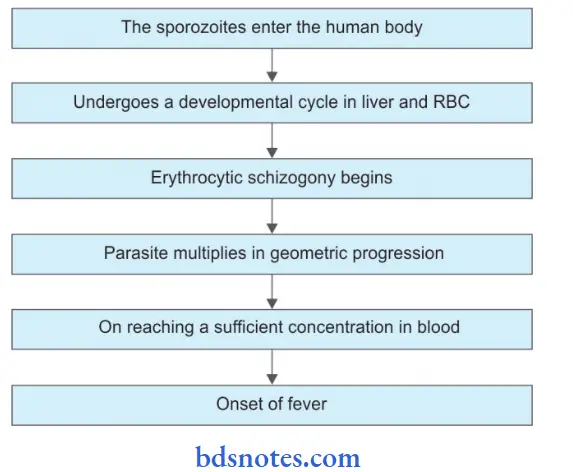
This period of development is known as the incubation period (10–14 days).
Laboratory Diagnosis:
- Microscopic examination of peripheral blood smear: Two slides are prepared, one is of thick smear and another is of thin smear. Both sides are stained with Giemsa or Leishman stain. After staining slides are examined under a microscope in oil immersion lens. In P. vivax all asexual erythrocytic stages, i.e. ring forms, trophozoites, and schizonts as well as gametocytes are seen. Schuffer’s dots in RBCs are seen. RBCs are enlarged.
- Fluorescent microscopy: Malarial parasites are demonstrated by fluorescent staining. A blood smear is prepared and is stained with acridine orange. The stained slide is examined under a fluorescent microscope. The nuclear DNA of the malarial parasite is green and cytoplasmic RNA is red.
- Rapid diagnostic tests: They are based on the detection of antigens using immunochromatographic methods. In these tests, a dipstick or test strip containing monoclonal antibodies directed against parasitic antigens is used. The test takes 15 minutes and so produces rapid results.
- Serological test: Indirect immunofluorescence test, indirect hemagglutination assay, and ELISA are serological tests for the diagnosis of malaria.
- DNA probes: These are specific diagnostic aid for the diagnosis of malaria. It can detect very low parasitemia.
Question 2. Describe the life cycle of P. falciparum and the pathology produced by it.
Or
Describe the life cycle of P. falciparum malarial parasite and enumerate the pathology produced by them.
Answer:
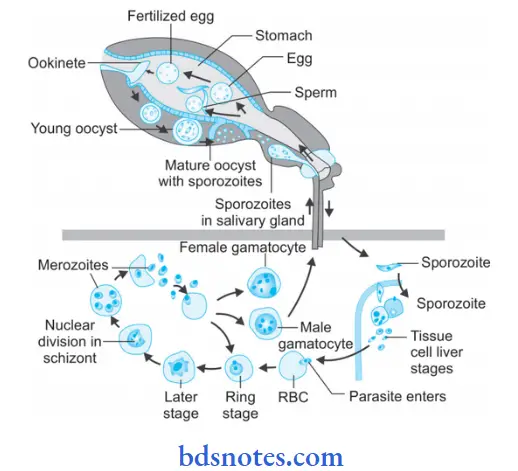
Life cycle of Plasmodium falciparum
Human Cycle: Man gets an infection when it get bitten by infected mosquito and sporozoites are introduced directly in blood circulation.
The human cycle starts and it has the following phases:
- Pre-erythrocytic schizogony
- Erythrocytic schizogony
- Gametogony
- Exo-erythrocytic schizogony.
- Pre-Erythrocytic Schizogony:
- Sporozoites undergo a developmental phase inside the liver cells. This phase of development is known as pre-erythrocytic schizogony.
- Within 1 hour, all the sporozoites which are entered directly in the blood leave the bloodstream and enter into liver parenchymal cells to start pre-erythrocytic schizogony.
- The sporozoites become rounded inside the liver parenchymal cells. They undergo multiple nuclear divisions and develop into schizonts.
- The size of the schizont is 4.5 to 5 µm in diameter and fil two third of a normal size erythrocyte. The pre-erythrocytic cycle lasts for 6 days in P. falciparum.
- After the completion of this cycle, the liver cells rupture and release merozoites into the bloodstream.
- Erythrocytic Schizogony:
- The merozoites released from pre-erythrocytic schizogony penetrate red blood cells. They pass through the stages of trophozoite, schizont, and merozoite.
- In P. falciparum trophozoite is compact, rarely amoeboid and pigment collects in a single mass.
- In P. falciparum there are 18 to 24 merozoites in red blood cells. The red blood cells rupture to release the merozoites which attack new red blood cells and continue their erythrocytic schizogony repeating the cycle.
- In P. falciparum infection, erythrocytic schizonts aggregate in the capillaries of the brain and other internal organs, so that only ring forms are found in the peripheral blood.
- The duration of erythrocytic schizogony is less than or equal to 48 hours.
- Gametogony:
- Some merozoites of erythrocytic schizogony develop into male and female gametocytes known as microgametocytes and macrogametocytes, respectively.
- They develop in the red blood cells of the capillaries of internal organs such as the spleen and bone marrow.
- These are sexual forms and only mature gametocytes are found in the peripheral blood.
- The microgametocytes (male gametocytes) of P. falciparum are sickle-shaped, broader, and shorter, the cytoplasm stains light blue and the nucleus is diffuse.
- Macrogametocytes (female gametocytes) are longer, sickle shaped, more slender, cytoplasm stains deep blue and the nucleus is compact.
- Exo-erythrocytic Schizogony: This stage is absent in P. falciparum so relapses do not occur in P. falciparum malaria.
- Mosquito Cycle:
- The sexual cycle of malarial parasites starts in the human host with the formation of gametocytes which are then transferred to the mosquito for growth.
- A female anopheles during its blood meal from the infected human, takes both the asexual and sexual forms of parasite.
- Only the mature sexual forms are capable of further development in mosquitoes and the rest of the forms die immediately.
- In the midgut of the mosquito, one microgametocyte develops into 4 to 8 thread-like filamentous structures named microgametes by the process of flagellation.
- From one macrogametocyte only one macrogamete is formed.
- Fertilization occurs when a microgamete penetrates into a macrogamete.
- The fertilized macrogamete is known as a zygote. Within the next 24 hours, the zygote lengthens and matures into an ookinete. This is a motile vermiculate stage.
- Ookinete converts into an oocyst.
- As the oocyst matures, it increases in size and a large number of sporozoites develop inside it.
- The number of oocysts in the stomach wall varies from a few to more than a hundred.
- Oocyst ruptures and releases sporozoites in the body cavity of the mosquito.
- Sporozoites are distributed into various organs and tissues of the mosquito. However, they have a special predilection for salivary glands.
- The mosquito is now capable of transmitting the infection to man.
Pathology Produced by P. falciparum
P. falciparum produces:
- Malignant tertian malaria: It is associated with fever, confusion, convulsion, coma, and death.
- Pernicious malaria: It results from anoxia due to obstruction of capillaries in various organs followed by necrosis of tissue.
- It may involve:
- Nervous system
- The gastrointestinal system has gastric, choleric, and dysentery.
- May involve cardiovascular, respiratory, and genitourinary systems.
Blackwater fever: It is characterized by sudden massive hemolysis followed by fever and hemoglobinuria
- Kidneys and the liver are particularly involved.
- Sequelae of blackwater fever include uremia, renal failure, circulatory failure, liver failure, anemia, and pigment calculi. Renal failure is the cause of death.
Question 3. Draw a labeled diagram of the life cycle of Plasmodium falciparum.
Answer:
Labeled diagram of the life cycle of Plasmodium Falciparum (P. falciparum)
Question 4. Draw a labeled diagram of P. vivax.
Answer:
Labeled diagram of Plasmodium vivax (P.vivax)

- Ring stage—early trophozoite
- Late trophozoite
- Amoeboid form
- Early schizont
- Late schizont
- Mature schizont with merozoites
- Male gametocytes
- Female gametocytes
Question 5. Draw the labeled diagram of P. falciparum (all stages) and discuss about the laboratory diagnosis of malaria.
Or
Write a short note on lab diagnosis of malaria.
Or
Write briefly on laboratory diagnosis of malaria.
Answer:
Diagram of all Stages of P. falciparum:

- Ring stage—early trophozoite
- Late trophozoite
- Amoeboid form
- Early schizont
- Late schizont
- Mature schizont with merozoites
- Male gametocytes
- Female gametocytes
Laboratory Diagnosis of Malaria
Microscopic examination of peripheral blood smear: Two slides are prepared, one is of thick smear and another is of thin smear. Both slides are stained with Giemsa or Leishman stain or Wright stain or Fild stain. In India, Jaswant SB stain (Singh and Bhattcharji) is commonly used. After staining slides are examined under a microscope in oil immersion lens at least 200 fields should be observed before it is declared negative.
- In P. vivax, P. malariae, and P. ovale all asexual erythrocytic stages, i.e. ring forms, trophozoites, and schizonts as well as gametocytes are seen. Schuffer’s dots in RBCs are seen in P. vivax and P. ovale. RBCs are enlarged in P. vivax and not in P. falciparum.
- In P. falciparum infection ring forms and gametocytes are seen. Multiple rings in individual RBC with accole forms is the diagnostic hallmark. Maurer’s dots are seen in P. falciparum infection.
- Ziemann’s dots are seen in P. malariae infection.
- Quantitation of parasites: In this phosphate-buffred solution (PBS) is graded as:
-
- +, i.e. 1 to 10 parasites per 100 thick fim fields.
- + +, i.e. 11 to 100 parasites per 100 thick fim fields.
- + + +, i.e. 1 to 10 parasites per single thick fim fields.
- + + + +, i.e. more than 10 parasites per single thick film file
This is done to fid the percentage of parasitized RBCs, to rule out species of malarial parasite, and to detect malarial pigment which provides a clue regarding infection in absence of malarial parasite.
- Quantitative buff coat method: Acridine orange is used to identify malarial parasites by quantitative buff coat method.
Fluorescent microscopy: Malarial parasites are demonstrated by fluorescent staining. A blood smear is prepared and is stained with acridine orange. Stained slide is examined under florescent microscope. The nuclear DNA of the malarial parasite is green and cytoplasmic RNA is red.
Rapid diagnostic tests: They are based on the detection of antigens using immunochromatographic methods. In these tests, a dipstick or test strip containing monoclonal antibodies directed against parasitic antigens is used. The test takes 15 minutes and so produces rapid results.
Serological test: Indirect immunofluorescence test, Indirect hemagglutination assay, and ELISA are a serological test for the diagnosis of malaria.
DNA probes: These are specific diagnostic aid for the diagnosis of malaria. It can detect very low parasitemia.
Question 6. Write a short note on malaria.
Answer:
Malaria is a blood protozoan disease. The disease has been eradicated due to destruction of its vector in the Anopheles mosquitoes.
Causative Organism Of Malaria :
- Plasmodium falciparum
- Plasmodium malariae
- Plasmodium vivax
- Plasmodium ovale.
Clinical Features of Malaria:
- The incubation period is about 10 days
- The symptoms are divided into three stages:
-
- Cold stage: In this stage there is a fever for 1-2 hours followed by cold hands and feel body ache and shivering.
- Hot stage: It lasts for 4 hours during which there in high fever (up to 105°F) vomiting and headache.
- Sweating stage: It lasts for 1-2 hours during which there is a lot of sweating and the fever comes to normal.
- Anemia: Microcytic or normocytic hypochromic is more pronounced in P. falciparum
- Splenomegaly: Spleen is palpable by the second week. It is the most important physical sign.
- In the benign form of the disease, fever develops on every third day (tertian fever) or fourth day (quatran fever).
- In malignant form, fever develops more often (less than 3 days) and there may be vomiting and jaundice.
Treatment Of Malaria:
- Chloroquine is the drug of choice in malaria.
- In choloroquine-resistant P. falciparum combination of sulphadoxine and pyrimethamine should be given.
- Primaquine should be given in relapse of P. vivax.
Question 7. Write a short note on pathogenicity of Plasmodium falciparum and laboratory diagnosis of falciparum malaria.
Answer:
Pathogenicity of Plasmodium falciparum
- Plasmodia invade the red blood cell growth and segment at the expense of these host cells which rupture when schizogony is complete.
- The debris of ruptured cells released the merozoites, and their metabolic products, stimulating chemoreceptors of the temperature-regulating mechanism of the host to conserve heat.
- As the number of the invaded red cells increases and the asexual cycle of the parasite becomes more synchronized the quantity of pyrogen released at one time becomes sufficient to produce the characteristic chills and fever of a malaria attack.
- The species of plasmodia differ greatly if their ability to multiply in the blood.
- Plasmodium vivax prefers to invade the youngest erythrocyte, whereas Plasmodium malaria prefers the older red cells. Hence these species parasitize around 2 % of host red blood cells.
- Plasmodium falciparum, on the other hand, invades erythrocytes of all ages and thus is capable of parasitizing a very high percentage of erythrocytes.
- Due to the varying number of merozoites produced in schizogony by the species of Plasmodium.
- Plasmodium falciparum multiplies more rapidly than Plasmodium vivax which in turn multiplies more rapidly than Plasmodium malariae and Plasmodium ovale. The parasitemia of Plasmodium falciparum also tends to be higher because more than one parasite frequently develops in a single erythrocyte.
- With each schizogony, the parasitized cells are destroyed, but there is also considerable destruction of unparasitized cells due to lysis and phagocytosis, phagocytosis especially occurs in the spleen and liver. In falciparum malaria with a very high parasitemia, hemolytic jaundice may be evident and anemia may be severe.
- The malignant character of falciparum malaria is not so much related to its rapid multiplication and invasiveness as to the manner in which it causes lesions in the human host.
- Characteristic lesions are due to the blockade of small vessels by sticky parasitized erythrocytes.
- The blockade cause stasis, then local anoxia, then increased vascular permeability, which allows plasma and unparasitized cells to leak into the perivascular space.
- This incidentally results in additional loss of erythrocytes.
- These factors combine to cause a decrease in circulating erythrocytes in the circulating blood volume, local tissue anoxia and edema.
Laboratory Diagnosis of Malaria Falciparum
- Microscopic examination of peripheral blood smear: Two slides are prepared, one is of thick smear and another is of thin smear. Both sides are stained with Giemsa or Leishman stain. After staining slides are examined undermicroscope in oil immersion lens. In P. falciparum infection ring forms and gametocytes are seen. Multiple rings in individual RBC with accolé forms is the diagnostic hallmark. Maurer’s dots are seen in P. falciparum infection. RBCs do not get enlarged in P. falciparum infection.
- Fluorescent microscopy: Malarial parasites are demonstrated by fluorescent staining. A blood smear is prepared and is stained with acridine orange. Stained slide is examined under florescent microscope. The nuclear DNA of the malarial parasite is green and cytoplasmic RNA is red.
- Rapid diagnostic tests: They are based on the detection of antigens using immunochromatographic methods. In these tests, a dipstick or test strip containing monoclonal antibodies directed against parasitic antigens is used. The test takes 15 minutes and so produces rapid results.
- Serological test: Indirect immunofluorescence test, indirect hemagglutination assay, and ELISA are a serological test for the diagnosis of malaria.
- DNA probes: These are specific diagnostic aid for the diagnosis of malaria. It can detect very low parasitemia.
Question 8. Write notes on pernicious malaria
Answer:
It results from anoxia due to obstruction of capillaries in various organs followed by necrosis (death) of tissues. The symptoms appearing depend on the site where the injury occurs. Pernicious malaria generally occurs in recently infected individuals without immunity to the parasite and in endemic conditions it is always due to P. falciparum infection. Under epidemic conditions, pernicious malaria becomes more common and may be due to P. vivax especially in children.
According to the organs affected pernicious malaria may be broadly divided into three groups:
- Pernicious malaria affects the nervous system.
- Pernicious malaria affects the gastrointestinal system.
- Pernicious malaria affects other systems.
1. Nervous system involvement: It may be cerebral type, cerebrospinal type, cord and peripheral type or special sense type. But cerebral malaria accounts for 55% of the pernicious forms.
- Cerebrospinal: It simulates disseminated sclerosis by scanning speech, intention tremors, nystagmus, spastic gait, etc.
2. Gastrointestinal forms: Localization of malaria infection may lead to algid malaria (cold malaria), gastrointestinal form may be of:
- Gastric form: With severe gastric distress, tender abdomen, vomiting, and even hematemesis. It may simulate cholecystitis, appendicitis or infective hepatitis.
- Choleric form: Simulating cholera with profuse stool, vomiting, dehydration, and collapse. But stool is not “rice-watery” and may contain blood.
3. Pernicious types: Affecting the cardiovascular, respiratory, and genitourinary systems:
- Septicemic form leads to cardiac failure and death.
- Acute hemolytic form leads to rapidly progressing anemia.
- The hemorrhagic form stimulates “purpura”
- Pneumonic fever: Pulmonary edema is a very serious complication.
- Nephrotic form: Nephritis, nephrosis, and even orchitis of malarial origin are known.
- Nephrosis is more common with P. malaria infection.
Question 9. Write short note on Plasmodium falciparum.
Or
Write a short answer on Plasmodium falciparum.
Answer:
Morphology of P. falciparum
The morphology of Plasmodium falciparum is based on its various morphological forms which is as follows:
- Sporozoites:
- They are sickle-shaped.
- Hypnozoites are not seen
- Pre-erythrocytic schizont:
- Its size is 60 × 30 µ in diameter
- The number of merozoites present per schizont are 30,000 to 50,000
- Merozoites invade reticulocytes, younger and older RBCs.
- Erythrocytic schizogony:
- Each RBC is invaded by more than one parasite.
- High parasitemia is seen, i.e. 50%.
- Trophozoite:
- Ring stage: It is 1.25 to 1.5 µ and is small. The ring is attached to the margin of RBC. It form appliqué or accole form. The presence of binucleate rings is common.
- Amoeboid form: It is large, irregular, 6 to 12 brick red, and Maurer’s dots are seen. There is no increase in the size of RBC, its color is reddish violet.
- Schizont:
- Early schizont: It is of 4.5 to 5 µ. It is not visible in peripheral blood, develops in a capillary of the heart, spleen, bone marrow, brain, and intestine
- Late and mature schizont: The nucleus divides to form daughter nuclei and develop into merozoites with a central nucleus and the surrounding cytoplasm. The size of merozoite is 0.5 to 0.7 µ in diameter. Their number is 18 to 24 and is arranged in grape cluster.
- Gametocyte:
- The size of male gametocyte is 8 to 10 µ × 2 to 3 µ and of female gametocyte is 10 to 12 µ × 2 to 3 µ.
- The shape of the male gametocyte is a kidney shape and the shape of the female gametocyte is a crescent shape.
- The cytoplasm of male gametocytes is light blue while of female gametocytes is deep blue.
- The nucleus of the male gametocyte is scattered and has fine granules and of the female gametocyte is small and compact.
Complications of P. falciparum
- Pernicious Malaria: It is a life-threatening complication if the infection is not effect- tively treated. It can present as
-
- Cerebral malaria: Presence of hyperpyrexia, convulsion, coma, and paralysis.
- Algid malaria: It is characterized by cold and clammy skin, peripheral circulatory failure, hypotension, and gastrointestinal symptoms.
- Septicemic malaria: Presence of hyperpyrexia, pneumonia, and cardiac syncope.
- Blackwater Fever
- It is characterized by sudden massive hemolysis followed by fever and hemoglobinuria.
- Kidneys and the liver are particularly involved.
- Sequelae of blackwater fever include uremia, renal failure, circulatory failure, liver failure, anemia, and pigment calculi. Renal failure is the cause of death.
Question 11. Write a short note on blackwater fever.
Answer:
Blackwater fever is so-called because of the production of dark-colored black urine due to intravascular hemolysis
- Blackwater fever occurs in those persons who had been previously infected to P. falciparum and had an inadequate dosage of quinine.
- It can be precipitated in small amounts of quinine in quinine-sensitive cases.
- Blackwater fever is characterized by intravascular hemolysis, fever, hemoglobinuria, vomiting, circulatory collapse, and acute renal failure.
- Parasitized erythrocytes during the previous infection act as an antigen against which antibodies are formed.
- When there is subsequent infection and treatment with quinine occurs there is massive destruction of erythrocytes due to antigen-antibody reaction.
- These days blackwater fever is rare because of the introduction of newer antimalarial drugs.
Question 12. Write a short note on the complications of malaria.
Or
Write short note on malarial complications.
Answer:
The following are the Complications of Malaria:
- Development of respiratory distress occurs in up to 25% of adults and 40% of children with severe P. falciparum malaria.
- Possible causes include respiratory compensation of metabolic acidosis, noncardiogenic pulmonary edema, concomitant pneumonia, and severe anemia.
- Although rare in young children with severe malaria, acute respiratory distress syndrome occurs in 5–25% of adults and up to 29% of pregnant women.
- Renal failure is a feature of blackwater fever, where hemoglobin from lysed red blood cells leaks into the urine.
- Infection with P. falciparum may result in cerebral malaria, which is characterized by the presence of hyperpyrexia, convulsion, coma, and paralysis.
- Algid malaria is characterized by cold and clammy skin, peripheral circulatory failure, hypotension, gastrointestinal symptoms, and septicemic malaria which is characterized by the presence of hyperpyrexia, pneumonia, and cardiac syncope.
- Splenomegaly, severe headache, hepatomegaly (enlarged liver), hypoglycemia, and hemoglobinuria with renal failure may occur.

Leave a Reply