Diseases Of Liver
Question 1. Write a short note on tender hepatomegaly.
Answer. The term tender hepatomegaly itself means there is an enlargement of the liver with tenderness present in it.
Causes of Tender Hepatomegaly
- Infections of Tender Hepatomegaly
- Viral hepatitis
- Amoebic abscess
- Acute alcoholic hepatitis
- Autoimmune hepatitis
- Actinomycosis of liver
- Weil’s disease
- Malaria
- Disturbances of Tender Hepatomegaly
- Congestive heart failure
- Hepatic vein occlusion
- Tumors of Tender Hepatomegaly
- Hepatocellular carcinoma
- Angiosarcoma
- BuddChiari syndrome of Tender Hepatomegaly
Read And Learn More: General Medicine Question And Answers
Hepatitis Of Tender Hepatomegaly
- Viral hepatitis: Inflammation of the liver due to viral hepatitis is a common cause of tender hepatomegaly.
- There is a moderate enlargement of the liver which is smooth with consistency varying from soft to firm.
- Amoebic liver abscess: This liver is enlarged and is tender and tenderness present on the lower costal cartilage on the right side.
- Bacterial liver abscess: Multiple small pyogenic abscesses or a single large abscess involves the liver mainly the right lobe producing an enlarged tender liver.
- Acute alcoholic hepatitis: This follows the period of heavy drinking. There is the presence of right upper abdominal pain, anorexia, nausea and vomiting, profound weakness.
- The liver becomes enlarged and tender.
- Autoimmune hepatitis: Prevalence is in young females.
- Presence of enlarged and tender liver, spider naevi, and enlarged spleen.
- Actinomycosis of the liver: Here liver becomes enlarged and tender.
- Weil’s disease: Spirochetes causes Weil’s disease. There is the presence of an enlarged and tender liver.
- Malaria: In the malignant form of malaria there is hepatomegaly and tenderness over the liver.
- The liver is palpable in half of the cases. The spleen is always palpable.
General Medicine BDS 3rd Year Question and Answers
Circulatory disturbances Of Tender Hepatomegaly
- Congestive heart failure: Congestive heart failure is an important cause of hepatomegaly moderate to massive.
- The liver is firm and tender.
- Hepatic vein occlusion: It is an uncommon condition and there is the presence of an enlarged and tender liver.
Tumors Of Tender Hepatomegaly
- Hepatocellular carcinoma: Liver becomes enlarged but sometimes it is tender.
- Angiosarcoma: In patients with exposure to gaseous chemicals, the liver becomes enlarged and tender.
Budd-Chiari syndrome Here liver is enlarged and tender. There is the failure of the jugular vein to fill when the liver is pressed.
Question 2. Enumerate causes of tender hepatomegaly.
Answer. Enumeration of causes of tender hepatomegaly
1. Infections Tender Hepatomegaly
- Viral hepatitis
- Amoebic abscess
- Acute alcoholic hepatitis
- Autoimmune hepatitis
- Actinomycosis of liver
- Weil’s disease
- Malaria
Fatty Liver
2. Circulatory disturbances Tender Hepatomegaly
- Congestive heart failure
- Hepatic vein occlusion
3. Tumors Tender Hepatomegaly
- Hepatocellular carcinoma
- Angiosarcoma
- BuddChiari syndrome
General Medicine BDS 3rd Year Question and Answers
Question.3. Describe causes, clinical features, diagnosis, and management of jaundice
Answer. Jaundice is a condition where there is yellow pigmentation of the skin or sclera due to excess bilirubin in the blood.
Causes of jaundice: The causes are based on the type of jaundice.
Hemolytic jaundice: In hemolytic jaundice, there is excessive breakdown of RBC due to which bilirubin is produced in excess from hemoglobin. The causes of hemolytic jaundice are:
- Jaundice of prematurity, physiological jaundice
- Defects in the shape of erythrocytes, i.e. spherocytes and sickle cell anemia
- There is parasitic destruction of erythrocyte
- Toxic agents, i.e. metal like lead, poison like snake venom
- Incompatible blood transfusion
- ABO and Rhincompatibility
- Excessive burns on the body
- Bacterial toxins, septicemia.
Obstructive jaundice: In obstructive jaundice, bilirubin conjugation takes place normally in the liver, but it does not reach into the intestine and goes into the bloodstream, the result is a rise in bilirubin level. The causes of obstructive jaundice are:
- Extrahepatic:
- Obstruction within the bile ducts: The common cause is gallstone.
- Obstruction due to change in wall of ducts:
- Congenital obliteration of ducts during operation procedure, sclerosing cholangitis, etc.
- Due to pressure on the bile ducts: Pressure on the bile duct occurs in a number of diseases, e.g. carcinoma of the liver, hydatid cyst or fever, etc.
- Intrahepatic: In it, there is no mechanical obstruction in bile ducts and it is due to the intake of drugs like oral contraceptives, antitubercular drugs, and chlorpromazine.
- Hepatocellular jaundice: In this liver cells fall to conjugate and excrete all the bile pigments. The causes of hepatocellular jaundice are:
- Infections like viral hepatitis, yellow fever, malaria, typhoid, etc.
- Chemical poisons like chloroform, halothane, CCl4, etc.
- Alcoholic hepatitis, postnecrotic cirrhosis, etc.
Symptoms jaundice
- Symptoms of a case of jaundice shall vary with the type of jaundice the patient is suffering from and the underlying condition.
- The commonest form of jaundice is due to hepatitis where the patient may start with malaise, low-grade fever, vomiting, and loss of appetite.
- A person may take his / her morning breakfast normally and as the day passes, appetite for food almost disappears.
- In smokers, the urge to smoke is the earliest to go. Yellowness appears fist in the conjunctiva and then the mucous membrane of the lips and palate became pale.
- Urine is highly colored while in the early stage, the stools may remain of normal color.
- When a person has got features of obstructive jaundice,color of conjunctiva is yellowish green. Stools become clay colored and there is severe degree of itching.
- Pulse becomes slow.
- Patient may suffr from bruises and bleeding from mucous surfaces due to lack of fat soluble vitamin K.
- If jaundice remains for prolonged periods as in case of malignancy patient suffrs from marked asthenia and wasting.
Signs jaundice
- Patient may show signs of anemia, malnutrition suggestive of malignancy or cirrhosis.
- In cirrhotics look for spider naevi, white nails, enlargement of parotid glands, testicular atrophy, palmar erythema,gynecomastia, edema over legs and feet, and ascites.
- There may be scratch marks on skin suggestive of cholestasis due to obstructive jaundice, bruising and petechial spots indicating rothrombin deficiency in alcoholic or Laennec’s cirrhosis may be observed.
- Liver may be palpable, smooth and tender in infective hepatitis, hard and nodular in malignancy.
- Gallbladder becomes palpable when obstruction at the level of common bile duct is incomplete. A hard, small nodular gallbladder may be palpated in carcinoma.
- In chronic cholecystitis, gallbladder may be palapable and tender (Murphy’s sign). In addition to looking for signs of disease in general examination, look specifially in abdomen for ascites, liver, spleen and any lymphadenopathy.
- Rectal examination may be carried out for any primary growth in rectum.
Diagnosis jaundice
Biochemical test: jaundice
- White cell count: Leukopenia is present in the hepatocellular jaundice. Eosinophilia is present in drug hepatitis.
- Urine: Urobilinogen is absent in the obstructive jaundice and is in excess in hemolytic jaundice.
- Bilirubin is in excess in urine in obstructive jaundice.
- Liver function test: Serum bilirubin estimation is done to asses level of jaundice. The flcculation test is positive for hepatocellular and is negative for hemolytic and obstructive jaundice. Serum albumin levels are low and globulin levels are high in chronic hepatocellular jaundice.
- Hematology: In hemolytic jaundice blood fim shows immature cells and spherocytosis, erythrocyte fragility is increased and Coombs test is positive.
Radiology: jaundice
- Imaging of liver by ultrasound technique should be initial technique for all the jaundiced patients.
- Imaging of liver through CT scan is done. The dilated bile ducts are seen during obstructive jaundice while imaging through CT scan.
Aspiration needle biopsy of liver:
- It is done cautiously in jaundice. Menghini needle is used. The histological appearance of hemolytic,hepatocellular and obstructive jaundice is distinctive.
Management jaundice
- Treatment is directed towards the underlying cause Patient should be given small feeds of fat free, low protein and high carbohydrate diet which can be easily assimilated.
- Additionally vitamin B and C are given orally in high dosages.
- In obstructive jaundice, vitamin K should be given 10 mg parentrally.
Question.8. Write short note on viral hepatitis.
Or
Discuss clinical features diagnosis, management and complications of viral hepatitis.
Answer.
Viral hepatitis is a clinical entity where systemic infection causes inflmmation and hepatic cell necrosis.
Viruses causing viral hepatitis are:
- Hepatitis A virus
- Hepatitis B virus
- Hepatitis C virus
- Hepatitis D virus
- Hepatitis E virus
Other viruses are:
- Cytomegalovirus
- EpsteinBarr virus
- Herpes simplex virus, etc.
Clinical ManifestationsViral Hepatitis Are
Prodromal symptoms proceed the development of jaundice in sclera and behind the tongue from few days to two weeks and common symptoms are:
- Mild fever with or without chills
- Headache
- Malaise
- Arthralgia and skin rashes particularly in HBV infection
- Prominent gastroenteritis symptoms like anorexia, nausea and vomiting
- Steady upper mild abdominal pain in right hypochondrium
- Liver is not palpable.
Physical signs Viral Hepatitis Are
- The liver is usually tender but is not palpable initially.
- Enlarged cervical nodes may be found.
- Splenomegaly is present, particularly in children.
- Dark urine and a yellow tint of sclera held the onset of jaundice.
Features of Jaundice
- It is fist observed in sclera in bulbar conjunctivitis
- Jaundice deepens following obstruction of bile canaliculi.
- Stool become pallor
- Urine is dark
- Liver is tender and is easily palpable
- At this time appetite often improves
- Gastrointestinal symptoms diminished intensity.
Thereafter jaundice recedes and all features comes to normal in 3 to 6 weeks of time which can be revealed by:
- Normal skin, sclera and urine color
- Normal stool color
- Appetite improves
- Liver enlargement regresses.
Diagnosis Viral Hepatitis Are
Diagnosis of viral hepatitis is done in a patient with history of severe anorexia, nausea, vomiting and fever for a few days,elevated serum bilirubin and value of SGPT over 500 indicates viral hepatitis. The etiological agent is detected by serological markers.
1. Hepatitis A:
- Non specifi lab tests
- Raised serum bilirubin within few days and remain high up to 12 weeks.
- Serum AST and ALT levels remain high for 1 to 3 weeks.
- Alkaline phosphatase level is mildly elevated,though it remains persistently high, it suggest hepatitis associated cholestasis.
- Specifi test
- Hepatitis A specifi IgM antibody can be detected at the onset of symptoms and at fist rise in serum ALT.
- It peaks within first month and remain positive for 3 to 6 months.
- IgG and hepatitis A virus become positive at onset of illness and is detectable for many years
- Nucleic acid based test like PCR.
2. Hepatitis B: In a patient with history of severe anorexia, nausea,vomiting, fever for few days, elevated serum bilirubin and value of SGPT over 500 indicates HBV. The etiological agent is identifid by serological markers.
Following is the serological diagnosis ofhepatitis B:
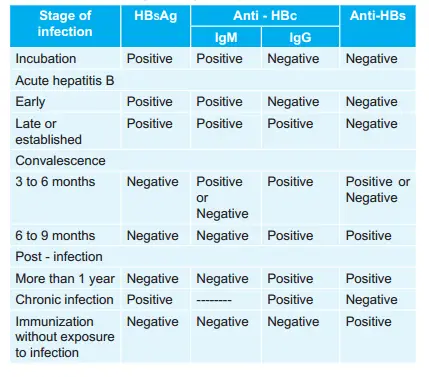
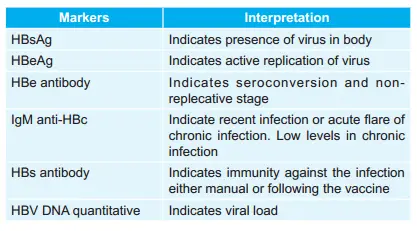
Viral Blood Hepatitis B:
- HBV DNA is measured by polymerase chain reaction in blood.
- Viral loads are in excess of 105 copies/mL in presence of active viral replication.
Other Investigations Hepatitis B:
- During early phase of hepatitis there is an increase in more than 400 units/L increase in plasma alaline aminotransferase and aspartate aminotransferase.
- High levels of alkaline phosphatase is suggestive of cholestasis.
- Prothrombin time is increased which indicates severe liver damage.
3. Hepatitis C
- Antibodies to HCV (antiHCV)
- Detection of antibodies to recombinant HCV polypeptides. Enzyme immunoassay measures antibodies against two antigens NS4 and NS3.
- These assays can detect antibodies within 6 to 8 weeks of exposure.
- Average time for seroconversion is 2 to 3 weeks
- Recombinant immunoassay
- Hepatitis C virus RNA testing qualitative test
- Hepatitis C virus RNA testing quantitative test
- HCV genotyping is helpful in predicting response to therapy.
4. Hepatitis D
- During Hepatitis D viral infection both IgM and IgG antibodies can be detected in serum in acute phase.
- HDV infection can also be detected using reverse transcriptase polymerase chain reaction (RTPCR)
5. Hepatitis E
- Identifiation of IgM antibodies to HEV from acute plasma serum samples. Antibodies detected are against ORF-2 and ORF-3
Management Hepatitis E
- Only the more severely affcted patients require care in hospital.
- Posthepatic syndrome is treated by reassurance.
Diet Hepatitis E
- Nutritious diet containing 2000–3000 Kcal daily is given.
- Light diet supplemented with glucose and food debris is acceptable.
- A good protein diet should be encouraged.
- In case of severe vomiting, IV flids and glucose may be required.
- Highly fatt diet should be avoided however complete restriction of fatt diet is not required.
Drugs Hepatitis E
- Drugs should be avoided, especially in severe hepatitis.
- Sedative and hypotonic drugs, alcohol, oral contraceptives should be especially avoided.
Surgery Hepatitis E
- During acute viral hepatitis surgery carries a signifiant role of post operative liver failure. Only life saving operation should be carried.
Liver transplantation
This may be required in acute or chronic liver failure due to hepatitis virus.
Prevention of viral Hepatitis
Prophylaxis of only hepatitis A virus and hepatitis B virus is present, i.e. active immunization.
In active immunization recombinant hepatitis B vaccine which consists of HBsAg is available and produce active immunization in 95% of individuals.
The complications ofviral hepatitis are:
- Acute hepatic failure: Fatalities are rare and usually occur in this case.
- Relapsing hepatitis: There is return of signs and symptom during recovery. It can be detected by
- clinical signs and biochemical tests. It resolves jaundice.
- Cholestasis: It can develop at any stage of illness and gives features of obstructive jaundice.
- Gillbert’s syndrome: It may come into picture during viral hepatitis.
- Connective tissue disease such as polyarthritits nodosa is observed in HBV and HCV infection.
- Renal failure, i.e. glomerulonephritis can occur also in relation to HBV and HCV infection.
- HenochSchönlein purpura and papular *acrodermatitis is repeated in children.
- Chronic hepatitis is observed with HBV infection with or without HDV and HCV viruses.
- Cirrhosis is also the complication of HBV and HCV and follows chronic hepatitis.
- Hepatocellular carcinoma: It is also the complication of HBV and HCV following cirrhosis of liver.
Question.10. Describe the causes, clinical features, complications and management in cases of cirrhosis of liver.
Or
Describe clinical features, etiology and management of cirrhosis of liver.
Or
Write short note on clinical features and complications of cirrhosis of liver.
Or
Write short note on cirrhosis of liver.
Or
Write etiology, clinical features, investigations and management of cirrhosis.
Answer. The term cirrhosis is applied to chronic diffuse liver disease of varied etiology and is characterized by hepatic cell necrosis, proliferation of connective tissue and nodular regeneration.
Causes of Cirrhosis of Liver
1. Common causes Cirrhosis of Liver
- Alcohol
- Viruses: Hepatitis B virus, hepatitis C virus.
2. Other causes Cirrhosis of Liver
- Hepatic venous congestion
- Venoocclusive disease
- BuddChairi syndrome
- Wilson’s disease
- Galactosemia
- Glycogen storage diseases
- *Hemochromatosis
- Drugs such as isoniazid, oral contraceptives, etc.
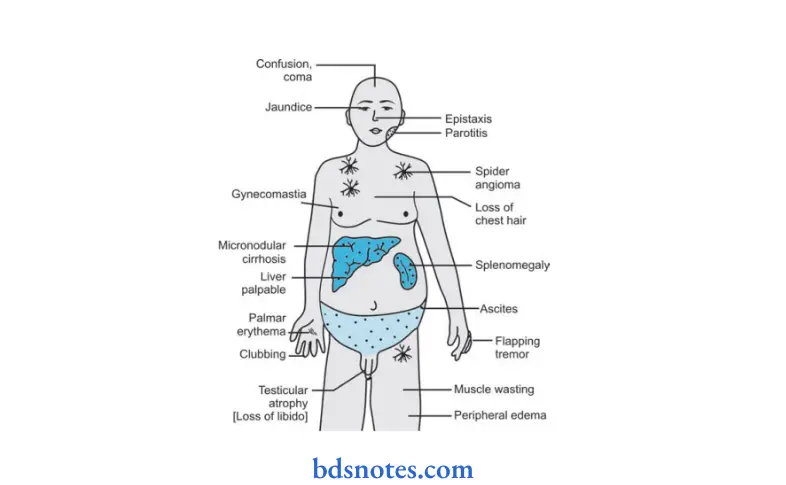
3. Clinical Features Cirrhosis of Liver
- Hepatomegaly
- Jaundice
- Ascites
- Circulatory changes
- Spider angioma
- Palmar erythema
- Cyanosis
- Endocrine changes.
Loss of libido
Hair loss of chest.
Men: Gynecomastia, testicular atrophy, impotence
Women: Breast atrophy, irregular menstrual cycle, amenorrhea - Hemorrhage tendency: Bruises, purpura, epistaxis, menorrhagia
- Portal hypertension: Splenomegaly, collateral vessels, variceal bleeding
- Hepatic encephalopathy
- Miscellaneous: Pigmentation, clubbing, low grade fever.
Complications Cirrhosis of Liver
- Posthepatic vein obstruction “BuddChiari syndrome” or extrahepatic and postsinusoidal.
- Intra-hepatic postsinusoidal / cirrhosis
- Esophageal varices causes severe hemorrhage
- Development of hepatocellular failure due to hepatocellular carcinoma.
- Renal failure
- Hypersplenism
- Due to infection, spontaneous bacterial peritonitis and secondary bacterial peritonitis occur.
Investigations Cirrhosis of Liver
1. Blood examination:
- Anemia can be present secondary to bleeding, folate defiiency, marrow suppression or hypersplenism.
Leukopenia and thrombocytopenia. - Aminotransferases (ALT, AST) get frequently elevated whereas a rise in the serum bilirubin and ALP may occur later. Serum albumin is low and Prothrombin time is frequently prolonged.
2. Imaging: Ultrasonography is done to assess the liver size and texture, ascites, portal hypertension and splenomegaly.
3. Endoscopy: Upper gastrointestinal endoscopy is being carried out to detect esophageal varices and to exclude other causes of upper gastrointestinal bleeding in the stomach and duodenum.
4. Liver biopsy: It is done for the assessment of severity of the cirrhotic changes and also confims the specifi cause of the cirrhosis.
Management Cirrhosis of Liver Cirrhosis of Liver
No treatment can reverse cirrhosis or even ensure that no further progression occurs, but medical therapy can improve general health and treat the symptom of disease effctively.
The main objectives are:
- Detect treatable causes
- Prevent and correct malnutrition
- Manage chronic cholestasis
- Treat the complication.
- Treatable causes: The treatable causes are alcohol abuse, drug ingestion, *hemochromatosis and Wilson’s disease, relief of biliary obstruction will prevent secondary biliary cirrhosis.
- Nutrition: In absence of ascites, a high energy 3000 kcal / day, protein rich (80–100 gm / day) diet should be advised.
Salt restriction is required if ascites are present.
Fat intake is not restricted unless cholestasis is a feature.
Complete absence of alcohol.
Vitamin and other supplements are not required when good diet is taken. - Drug treatment: Any drug should be avoided because as most of the drugs are metabolized in the liver which are liable to develop toxic reaction because they will unable to get metabolize.
- Liver transplantation: It is considered in all patients with chronic liver disease who develop liver failure.
Cirrhosis
Question.11.Write briefl complications of liver cirrhosis.
Answer. Following are the complications ofliver cirrhosis:
- Posthepatic vein obstruction “BuddChiari syndrome” or extrahepatic and postsinusoidal.
- Intra-hepatic postsinusoidal / cirrhosis
- Esophageal varices causes severe hemorrhage
- Development of hepatocellular failure due to hepatocellular carcinoma.
- Renal failure
- Hypersplenism
- Due to infection, spontaneous bacterial peritonitis and secondary bacterial peritonitis occur.
Question.12. Discuss management and etiopathogenesis of cirrhosis.
Answer. For management refers toAns 10 of same chapter.
Etiopathogenesis
Hepatic cirrhosis can occur at any age and often causes prolong morbidity.
- Any condition leading to persistent or recurrent hepatocyte death may lead to hepatic cirrhosis, e.g. viral hepatitis and alcohol, prolonged biliary damage and obstruction as occur in primary biliary cirrhosis, sclerosing cholangitis and postsurgical biliary structures will also result in cirrhosis.
- Persistent blockages of venous return from liver, e.g. venoocclusive disease and Budd Chiari syndrome, will eventually result in liver cirrhosis.
- Common to all cause of liver cirrhosis is activation of hepatic stellate cells.
- These cells are widely distributed throughout the liver in the space of disse.
- Following activation the fat storing stellate cells become transformed into multifunctional cells, and cytokine synthesis.
Question.13. Diffrentiate between hepatocellular jaundice and hemolytic jaundice.
Answer

Question 14. How will you diffrentiate between obstructive jaundice and infective jaundice?
Ans.

Question.15. Enumerate the causes of hepatomegaly.
Answer. Enumeration of causes of hepatomegaly
1. Infections Hepatomegaly
1. Viral
- Viral hepatitis
- Yellow fever
- Infectious mononucleosis
- Lassa fever
2. Bacterial
- Typhoid
- Pneumonia
- Brucellosis
- Tuberculosis
3. Protozoal
- Amoebiasis
- Malaria
- kalaazar
4. Spirochetal
- Weil’s disease
- Syphilis
- Relapsing fever
5. Parasitic
- Schistosomiasis
- Echinococcus
- Clonorchiasis
6.. Fungal
- Actinomycosis
- Histoplasmosis
2. Metabolic Hepatomegaly
- Fatt liver
- Amyloid
- Glycogen storage disease
3. Congestive Hepatomegaly
1. General
- Congestive heart failure
- Tricuspid regurgitation
- Constrictive pericarditis
2. Local
- Portal hypertension (cirrhosis)
- Hepatic vein thrombosis
3. Tumors
1. Primary
- Benign and malignant hepatoma
- Benign and malignant cholangioma
- Fibroma
- Sarcoma
- Hemangioma
2. Secondary: Direct due to spread by contiguity, or embolic metastatic
4. Cysts Hepatomegaly
- Hydatid
- Polycystic
5. Biliary obstruction Hepatomegaly
- Gallstones
- Strictures of bile ducts
6. Hematological Hepatomegaly
- Leukemias
- Lymphoma
- Myeloproliferative disorders
7. Storage disorders Hepatomegaly
- Gaucher’s disease
- Niemann Pick’s disease
- Amyloidosis
- Glycogen storage disease
- Gargoylism,
- Hemochromatosis
8. Myeloid metaplasia Hepatomegaly
- Secondary carcinoma of bone
- Myelofirosis
- Myelosclerosis
- Multiple myeloma
- Marblebone disease
9. Genetic abnormalities: Sickle cell disease
10. Congenital: Riedel’s lobe
Question.16. Write short note on soft tender liver.
Answer. Soft tender liver is the clinical condition of the liver in which on palpitation the liver assumes to be soft and palpable.
Soft Tender Liver Etiology
- Hydatid cyst
- Calcinosis cutis
- Nephritis and cerebellar ataxia
- Hypersensitivity reaction
- Oral contraceptives
- HIV
- Acute renal failure
- Obstructive jaundice
- Hepatocellular carcinoma
- Pleural and pericardial effsion
- Gallbladder injury.
Clinical Features soft tender liver.
- Fever is present
- Hepatomegaly is present
- Muscle cramp / fatigue due to lactic acid accumulation
- Jaundice is seen
- Non pittng edema is present
- Anorexia, ascites and anemia is present
- Amyloidosis is present.
Diagnosis soft tender liver.
- MRI should be done
- USG is done
- Xray of lower abdomen shows moderate enlargement of liver
- Lipid profie shows increase in lipid value.
- Blood picture reveals microcytic hypochromic anemia.
Treatment soft tender liver.
- Treatment of cause is done
- No drug is given, only conservative treatment is done.
- Fluid diet is given, restriction of salt and fatt acids and spicy foods is done.
- Electrolyte balance is maintained with digestive enzymes.
Question.17. How history taking and investigation will help in fiding the cause of the jaundice?
Answer. History taking of person mainly concerned with its illness, present past and family history which he describe to the doctor.
Its basic aim is to arrive a diagnosis of disease and outline the treatment.
- History taking is an important clinical presentation which helps in the diagnosis and finding the etiology / cause of jaundice.
- In history taking we are mainly concerned with the abdominal pain which patient undergoes like in hepatocellular jaundice patient will not feel abdominal colic while in obstructive and hemolytic jaundice patient feels sharp pain.
- The second point concerned in history taking with patient is pruritis, i.e. discoloration of skin.
Pruritis is transient in hepatocellular jaundice.
It is well, marked and is present in obstructive jaundice while it is fully absent in hemolytic jaundice. - Last and most important point in history taking is past history of patient, like patient can develop hepatocellular jaundice if he / she is in contact with jaundice patient before as well as certain drug can cause hepatocellular jaundice.
- A patient of obstructive jaundice will explain about pain, weight loss or any abdominal surgery before, which can give rise to the obstructive jaundice.
- A patient of hemolytic jaundice has a blood transfusion or certain drugs which can cause hemolytic jaundice which patient had taken in past.
Investigations jaundice
Investigation means laboratory diagnosis.

Question.19. Write short note on liver function test.
Answer.
Liver Function test
Serum Bilirubin
- The normal level is 1 mg / 100 mL.
- It increases in:
- Hepatocellular injury
- Posthepatic biliary obstruction.
Thymol turbidity test
- Demonstrating hepatic cellular dysfunction
- Gamma globulins are mainly responsible for positivity in this test.
Enzyme in liver disease
1. Alkaline phosphate:
- Elevation occurs in obstructive jaundice.
- Mild elevation in xanthomatous cirrhosis, hepatocellular injury, liver abscess.
2. SGOT (serum glutamine oxalate transferase):
- Normal level is 5 to 40 unit
- It increases in all conditions leading to hepatic necrosis and in alcoholic liver damage.
3. SGPT (serum glutamine pyruvic transferase)
- It is more specifi for liver disease.
- It is raised in sever parenchymal damage to liver.
- For example, chronic acute hepatitis, alcoholic liver disease, biliary obstruction.
4. GGT (gamma glutamyl transpeptidase): Sensitivity test for alcoholic liver disease and for hepatobiliary disease.
5. Leucine amylo peptidase: It increases in primary liver diseases.
6. Serum pseudocholinesterase:
- It has limited value.
- Value decreases in subacute and chronic parenchymal diseases of liver (Cirrhosis).
Question.20. Write short note on hepatitis B importance in dental practice.
Answer. Hepatitis may be defied as an infection of the liver caused by the hepatitis virus B.
The prevention for hepatitis will be
1. Prevention of mode of transmission
- Avoid infected blood transfusion, body organs, sperms and other tissues.
Blood should be screened before transfusion. - Strict sterilization process should be ensured in clinics.
- Presterilized needles and syringe should be used.
- Avoid injections unless they are absolutely necessary.
- Carrier should be told not to share razors or tooth brushes, use barrier methods of contraceptions, avoid blood donation.
2. Hepatitis B vaccination should be given.
Question.21. Diffrentiate between hepatitis A and hepatitis B viral infection.
Answer

Question.22. Write short note on jaundice.
Or
Write briefl on signs and symptoms and treatment of jaundice.
Or
Write short answer on jaundice.
Answer. Jaundice is a condition where there is yellow pigmentation of the skin or sclera by excess of bilirubin in the blood.
When levels of bilirubin exceed 2 mg or above clinical jaundice become apparent.
Classifiation jaundice
Hemolytic:
- Physiological: Jaundice of prematurity
- Congential: Spherocytosis, sickle cell anemia
- Parasitic destruction of erythocytes—malaria
- Toxins—heavy metals
- Poisons—snake venom
- Drugs—sulfonamides, nitrofurantoin
- Bacterial toxins: Septicemia
- Incompatible blood transfusions—ABO and Rh blood
- group incompatibility
- Extensive burns.
Obstructive: jaundice
1. Extrahepatic:
- Obstruction within the bile ducts—gallstones, neoplasm, round worm.
- Obstruction due to changes in the wall of the ducts congenital obstruction (biliary atresia), traumatic (following surgery), sclerosing cholangitis.
- Pressure from without: Carcinoma of liver (primary / secondary) gumma, hydatidcyst, enlargedglands in porta hepatis (Hodgkin’s, leukemia, tuberculosis) carcinoma head of pancreas, cancer stomach.
2. Intrahepatic (obstruction without mechanical cause):
- Drugs like chlorpromazine, antitubercular drugs,methyl testosterone, oral contraceptives.
- Viral hepatitis with prolonged cholestasis.
- Jaundice of pregnancy
- Primary biliary cirrhosis
- Hepatocellular:
- Viral hepatitis
- Infectious mononucleosis
- Yellow fever
- Bacterial diseases with fever, typhoid
- Malaria
- Weil’s disease
- Chemicals like chloroform, halothane, trinitrotoluene, carbon tetrachloride.
- Postnecrotic cirrhosis
- Alcoholic hepatitis
- Hemochromatosis.
3. Congenital hyperbilirubinemia
- Without liver pigment:
- Gilbert’s disease
- Crigler-Najjar syndrome.
- With liver pigment:
- Dubin-Johnson syndrome
- Rotor syndrome.
Symptoms jaundice
- Symptoms of a case of jaundice shall vary with the type of jaundice the patient is suffring from and the underlying condition.
- Most common form of jaundice is due to hepatitis where the patient may start with malaise, low grade fever, vomiting and loss of appetite.
- Person may take his / her morning breakfast normally and as the day passes, appetite for food almost disappears.
- In smokers, urge to smoke is the earliest to go. Yellowness appears fist in the conjunctiva and then the mucous membrane of the lips and palate became pale.
- Urine is high colored while in early stage, the stools may remain of normal color.
- When a person has got features of obstructive jaundice, color of conjunctiva is yellowish green. Stools become clay colored and there is severe degree of itching.
- Pulse becomes slow.
- Patient may suffr from bruises and bleeding from mucous surfaces due to lack of fat soluble vitaminK.
- If jaundice remains for prolonged periods as in case of malignancy patient suffrs from marked asthenia and wasting.
Signs jaundice
- Patient may show signs of anemia, malnutrition suggestive of malignancy or cirrhosis.
- In cirrhotics look for spider naevi, white nails, enlargement of parotid glands, testicular atrophy, palmar erythema, gynecomastia, edema over legs and feet, and ascites.
- There may be scratch marks on skin suggestive of cholestasis due to obstructive jaundice, bruising and petechial spots indicating prothrombin deficiency in alcoholic or Laennec’s cirrhosis may be observed.
- Liver may be palpable, smooth and tender in infective hepatitis, hard and nodular in malignancy.
- Gallbladder becomes palpable when obstruction at the level of common bile duct is incomplete. A hard, small nodular gall bladder may be palpated in carcinoma.
- In chronic cholecystitis, gallbladder may be palapable and tender (Murphy’s sign). In addition to looking for signs of disease ingeneral examination, lookspecifiallyinabdomen for ascites, liver, spleen and any lymphadenopathy.
- Rectal examination may be carried out for any primary growth in rectum.
Treatment jaundice
- Treatment is directed towards the underlying cause:
- Patient should given small feeds of fat free, low protein and high carbohydrate diet which can be easily assimilated.
- Additionally Vitamin B and C are given orally in high dosages.
- In obstructive jaundice, vitamin K should be given 10 mg parentrally.
Question.23. Describe causes, clinical features and management of portal cirrhosis.
Answer. It is characterized by the diffse involvement of the liver in form of necrosis of liver cells, collapse of hepatic lobules, reticulin framework followed by diffse firosis and formation of structurally abnormal nodules.
- This interferes not only with liver blood flw, but also its function.
- This results in portal cirrhosis which is due to inadequacy of liver cells and portal hypertension.
Causes Portal Cirrhosis.
- Hepatitis B and D
- Consumption of excessive alcohol
- Hemochromatosis
- Alpha-1 antitrypsin defiiency
- Autoimmune chronic active hepatitis
- Wilson’s disease
- Malaria
- Schistosomiasis
- Venoocclusive disease
- Hepatic venous congestion to drugs like methyldopa etc.
Clinical Features Portal Cirrhosis. Case of cirrhosis may present either in compensated or decompensated forms.
Compensated Form Portal Cirrhosis
- A compensated case of cirrhosis has features of dyspepsia in the form of morning anorexia, nausea, vomiting and vague illhealth.
This is more so when it is early stage of alcoholic cirrhosis. - There is palmar erythema, spider naevi, splenomegaly and hepatomegaly with a non tender liver.
- There is loss of weight, illhealth and edema of the ankles.
- There may be no fim signs of cirrhosis and diagnosis is made on clinical suspicion to be confimed by biochemical investigations and liver biopsy.
- This stage of compensated form of cirrhosis may continue for a variable period of time ranging from months to years and bleed from esophageal varices may draw attntion to the disease or some precipitating cause like severe bacteremia may produce hepatocellular decompensation.
Decompensated Form Portal Cirrhosis
- A decompensated cirrhosis is characterized by a downhill course, abdominal distension, ascites, weight loss, edema over the dependent parts, cirrhotic facies (sunken eyes, hollow cheeks, pinched nose), skin dry and sallow.
- Jaundice may appear indicating progressive liver cell destruction.
- Liver may be palpable with irregular surface or it may not be palpable when it is shrunken.
- Splenomegaly is present in 80% of patients. Nails are white and clubbed.
- Endocrinal changes in the form of spider naevi, palmar erythema, gynecomastia, loss of axillary and pubic hair, and testicular atrophy are seen.
There may be bleeding spots or bruising due to prothrombin defiiency. - Ascites may be massive and is disproportionate to the edema of feet.
- Hepatocellular failure may supervene as liver cell necrosis proceeds.
- Breath becomes foul smelling often giving a mousy smell (Fetor hepaticus).
- Flapping tremors and encephalopathy appear.
- Appearance of jaundice, rapid accumulation of ascites and development of hepatic encephalopathy are poor signs in cirrhosis.
Management Portal Cirrhosis. It is palliative:
- Rest in bed: To maximize treatment of any reversible element of underlying liver disease and to improve renal perfusion.
- Correction ofany etiological factor: i.e. stoppage of alcohol, stoppage of drugs causing portal cirrhosis.
- Diet: Low salt. Total daily intake of 2000 calories with protein intake of 120 gm. If patient can tolerate it.
Fats and carbohydrates in normal amount. Vitamin B complex. - Symptomatic treatment:
- For anemia vitamin B12 and folic acid is given
- For restlessness sedatives such as lorazepam should be given
- For ascites low sodium diet and diuretics should be given.
Question.24. Write management of Amoebic liver abscess.
Answer.
Management of amoebic liver abscess
- Injection dehydroemetine 60 mg IM daily for 6 days.
- Tab. Tinidazole 600 mg TDS for 7 days.
- Tab. Chloroquine 500 mg TDS for 11 days.
If Amoebic liver abscess is large:
- The abscess should be aspirated and all flid pus, etc. Will be removed.
- Open drainage of pus may be undertaken if there is large amount of pus secondarily infected or if there are signs of pus, but aspiration is negative.
- Depending on the patient’s response aspiration of abscess may be carried out.
Question.25. Describe the etiology, diagnostic criterias and management of viral hepatitis.
Answer. Viral hepatitis is a clinical entity where systemic infection causes inflmmation and hepatic cell necrosis.
Etiology
- Hepatitis A,B,C,D,E, cytomegalovirus, herpes simplex virus,
- Epsteinbarr virus and yellow fever virus.
Diagnostic Criterias Diagnosis is based on investigations. Following are the investigation which confim the diagnosis of viral hepatitis
Investigations Viral Hepatitis.
1. Hepatitis A:
- Non-specifi lab tests
- Raised serum bilirubin within few days and remain high up to 12 weeks.
- Serum AST and ALT levels remain high for 1 to 3 weeks.
- Alkaline phosphatase level is mildly elevated, though it remains persistently high, it suggest hepatitis associated cholestasis.
- Specifi test
- Hepatitis A specifi IgM antibody can be detected at the onset of symptoms and at fist rise in serum
- ALT. It peaks within first month and remain positive for 3 to 6 months.
- IgG and hepatitis A virus become positive at onset of illness and is detectable for many years
- Nucleic acid based test like PCR.
2. Hepatitis B:
In a patient with history of severe anorexia, nausea, vomiting, fever for few days, elevated serum bilirubin and value of SGPT over 500 indicates HBV. The etiological agent is identifid by serological markers.
Following is the serological diagnosis of hepatitis B:


3. Hepatitis C
1. Antibodies to HCV (antiHCV)
- Detection of antibodies to recombinant HCV polypeptides. Enzyme immunoassay measures antibodies against two antigens NS4 and NS3.
- These assays can detect antibodies within 6 to 8 weeks of exposure.
- Average time for seroconversion is 2 to 3 weeks
2. Recombinant immunoassay
3. Hepatitis C virus RNA testing qualitative test Hepatitis C virus RNA testing quantitative test
4. HCV genotyping is helpful in predicting response to therapy.
4. Hepatitis D
- During Hepatitis D viral infection both IgM and IgG antibodies can be detected in serum in acute phase.
- HDV infection can also be detected using reverse transcriptase Polymerase chain reaction (RTPCR)
5. Hepatitis E:
- Identifiation of IgM antibodies to HEV from acute plasma serum samples. Antibodies detected are against ORF-2 and ORF-3
- Peak titers for IgM are observed during fist 4 weeks while onset of infection. A rising titer of IgG antibody is also diagnostic of infection.
Question.26. Write in brief the signs, symptoms and treatment of ascites.
Answer. Ascites is the accumulation of free flid in the peritoneal cavity.
Symptoms Ascites.
- Patient has sudden abdominal pain and fever may also be present.
- Edema over ankles and feet.
- Skin over abdomen is stretched.
Sign Ascites.
- Bulging of abdomen and in flnks is present.
- Umbilicus is transversely stretched or everted.
- Presence of flid thrill and shifting dullness.
- Increase in inferior vena cava pressure.
- Diaphragm may be pushed upwards and there can be respiratory distress.
- Pleural effsion on right side can be present.
- Urinary output is reduced.
Treatment Ascites.
- In every case of ascites oral diuretics, i.e. furosemide 40 to 80 mg + spironolactone 25 to 100 mg is administered.
- Sodium intake is restricted and diet which is low in sodium is given.
- In case of massive ascites which produce cardiorespiratory enlargement, abdominal paracentesis is done and flid is drained slowly.
Fluid should not be drained quickly because it causes vasovagal attck.
Question.27. Write short note on fulminant hepatic failure.
Answer. Fulminant hepatic failure is seen in a healthy person which develop acute hepatitis and goes into hepatic encephalopathy within the 8 weeks of illness.
Etiology
- Acute viral hepatitis
- Drugs all hepatotoxic drugs
- Pregnancy with hepatitis
- Wilson’s disease
- Due to Reye’s syndrome.
Clinical Features Fulminant Hepatic Failure
- Cerebral features: Poor alertness, slurred speech, drowsiness, confusion, disorientation, convulsion and coma.
- Jaundice is present.
- Fetor hepaticus
- Flapping tremors are present.
- Signs of portal hypertension are present, i.e. ascites, edema.
- Cerebral edema is present.
Investigations Fulminant Hepatic Failure
- Bilirubin levels are high
- Serum transaminase levels are high
- Prothrombin time is prolonged
- Urine may contain urobilinogen and bilirubin
- Serum ammonia levels are high
- USG of liver shows reduced liver size.
Treatment Fulminant Hepatic Failure
- Phenobarbitone or 5 mg IV diazepam is given to patient.
- Care of pulse, blood pressure, bowel and bladder is taken.
- 5 to 10% of glucose drip IV is given.
- IV vitamin K is given 10 mg for 3 days.
- IV vitamin C is given 500 mg daily for prevention of bleeding.
- IV ranitidine is given 50 mg twice daily.
- Encephalopathy is treated by with drawl of protein intake; Sterilization of gut by neomycin 1 gm orally for 6 hours; increased fecal output of nitrogen by changing bacterial flra with lactulose 30 to 60 mL orally after 2–3 hours till loose stool is produced.
- Infections should be treated with amoxicillin or ceftzxime.
Question.28. Enumerate the causes of cirrhosis liver.
Answer. Following are the causes of cirrhosis of liver:
1. Viral hepatitis B and C
2. Alcohol
3. Cryptogenic
4. Metabolic:
- Hemochromatosis
- Wilson’s disease
- α1—antitrypsin defiiency
- Cystic firosis
- Glycogen storage disease
- Galactosemia
5. Biliary obstruction:
- Primary biliary cirrhosis
- Sclerosing cholangitis
- Secondary biliary cirrhosis
6. Venous outflw obstruction:
- BuddChiari syndrome
- Venoocclusive disease
- Congestive heart failure
7. Drugs:
- Methotrexate
- Methyldopa
- Oxyphenisatin
- Amiodarone
8. Indian childhood cirrhosis.
Question 29. Write short note on high-risk groups and prophylaxis of hepatitis B.
Answer.
High-risk Groups of Hepatitis B The hepatitis B virus can infect infants, children, teens and adults.
Although everyone can be at some risk for a hepatitis B infection, there are people who are at greater risk because of their ethnic background, occupation, or lifestyle choices.
The following list is a guide for screening highrisk groups, but it certainly does not represent all potential risk factors.
- Health care providers and emergency responders
- Sexually active heterosexuals (more than 1 partner in the past six months)
- Men who have sex with men (Homosexuals)
- Individuals diagnosed with a sexually transmittd disease (STD)
- Illicit drug users (injecting, inhaling, snorting, pill popping)
- Sex contacts or close household members of an infected person
- Children adopted from countries where hepatitis B is common (Asia, Africa, South America, Pacifi Islands,
- Eastern Europe, and the Middle East)
- All pregnant women
- Recipients of a blood transfusion before 1992 Kidney dialysis patients and those in early renal failure
- Inmates of a correctional facility Staf and clients of institutions for the developmentally disabled
- Any individual who may have other risk factors not included on this list.
Prophylaxis of Hepatitis B Following is the prophylaxis of hepatitis B:
- Recombinant hepatitis B vaccine having HBsAg capable of producing active immunization.
- Usually three injections of vaccine should be given IM during current, fist and sixth month.
These vaccinations provide 90% of prophylaxis from hepatitis B virus. - If patient is immunocompromised larger doses of vaccination should be given.
- Passive immunization is provided by IM injection of hyperimmune serum globulins which is given within 24 hours or almost within a week of exposure to infected blood.
- Active along with passive immunization is provided to the paramedicos who has undergone needle stick injury, to newborn babies of hepatitis B positive mothers and to regular sexual partner of hepatitis B positive patient.
Dosage is 500 IU for adults and 200 IU for babies.
Following precautions are to be taken for prevention from hepatitis B:
- Avoid infected blood transfusion, body organs, sperms and other tissues. Blood should be screened before transfusion.
- Strict sterilization process should be ensured in clinics.
- Presterilized needles and syringe should be used.
- Avoid injections unless they are absolutely necessary.
- Carrier should be told not to share razors or tooth brushes, use barrier methods of contraceptions, avoid blood donation.
Question 30. Write short note on causes and investigations of ascites.
Answer.
Causes of Ascites
1. Disease of peritoneum
1. Infections:
- Tuberculous peritonitis.
- Spontaneous bacterial peritonitis.
- Fungal: Candida, histoplasma.
- Parasitic: Schistosoma, enterobius.
- Viral: Acute severe hepatitis.
2. Neoplasms:
- Primary mesothelioma.
- Secondary carcinomatosis, e.g. adenocarcinoma,
- sarcoma, teratoma, leukemia, Hodgkin’s disease,
- lymphocytic lymphoma, myeloid metaplasia.
- Pseudomyxoma peritonei
3. Familial paroxysmal peritonitis
4. Miscellaneous:
- Vasculitis — SLE and other collagen vascular
- diseases, allergic vasculitis (HenochSchönlein purpura).
- Eosinophilic gastroenteritis.
- Whipple’s disease.
- Granulomatous peritonitis — Sarcoidosis,
- Crohn’s disease, starch peritonitis.
- Peritoneal loose bodies.
- Peritoneal encapsulation.
2. Portal hypertension
3. Congestive heart failure
4. Hypoalbuminemia:
- Nephrosis
- Malnutrition
- Proteinlosing enteropathy
5. Beriberi
6. Myxedema
7. Ovarian disease:
- Meigs’syndrorne
- Struma ovari
- Ovarian overstimulation syndrome
8. Pancreatic ascites due to retroperitoneal leakage of pancreatic enzymes from a ruptured cyst or pancreatic duct.
9. Bile ascites
10. Chylous ascites
11. Epidemic dropsy
Investigations Ascites
- Blood examination: Anemia can be present. Presence of neutrophilic leukocytosis indicates infection.
- Urine examination: Massive albuminuria greater than 3.5 gm per day is present in nephritic syndrome.
- Stool for occult blood: It may indicate gastrointestinal malignancy as cause for ascites.
- Ultrasonography: It detect ascites
- Diagnostic paracentesis: 50–100 mL of ascetic fluid is aspirated and biochemical analysis is done. Bacteriological examination should also be done. It should detect whether the ascetic flid is exudate or transudate.
- Serum-ascites albumin gradient: Albumin present in serum and ascetic flid is determined for calculating the gradient.
Gradient > 1.1 g / dL indicates transudative ascites and < 1.1 g / dL indicate exudative ascites.
Fluid protein < 50% of serum protein indicates transudate while > 50% is indicative of exudates.
Question.31. Describe clinical features of portal hypertension. How will you investigate and manage a case of cirrhosis of liver.
Answer. Following are the clinical features ofportal hypertension:
- Splenomegaly: Spleen gets enlarged to the size of 5–6 cm.
- Hypersplenism: It is common leading to anemia,thrombocytopenia and leukemia. Pancytopenia can also occur.
- Collateral vessels form at gastroesophageal junction which may rupture leading to hematemesis or malena.
- Ascites is present.
- Caput-medusae is seen around umbilicus and at times large umbilical collateral give rise to venous hum.
- Fetor hepaticus results from shunting of portal blood. In fetor hepaticus foul smell from breadth is present due to mercaptans.
Investigation of case of cirrhosis of liver
1. Assessment of severity of cirrhosis of liver :
- Liver biochemistry:
- It may be normal in compensated cirrhosis.
- SGOT / SGPT reflct the activity of the disease, which is low when cirrhosis is established,but increased in evolution of cirrhosis due to autoimmune hepatitis.
- Alkaline phosphatase and transaminases may be slightly raised in decompensated cirrhosis.
- Serum albumin reflcts liver cell function, its low level indicates cirrhosis.
- Plasma bilirubin is normal in most of the cases but it gets increased in decompensated cirrhosis.
- Low albumin, i.e. <2.5 g / L and rising bilirubin are signs of progressive liver damage and these constitute bad prognostic signs.
- Hematology:
- Anemia, leukopenia and thrombocytopenia or pancytopenia may be seen in cirrhosis.
- Increased prothrombin time is a bad prognostic sign.
- Ascitic flid examination: Ascites is transudate in nature.
2. Assessment of type or cause of cirrhosis of liver:
- Blood biochemistry
- Viral markers, i.e. HbSAg are of value in identifiation.
- Serum autoantibodies, antinuclear, antismooth muscle and antimitochondrial antibodies level increase in cryptogenic cirrhosis and biliary cirrhosis.
- Rise in alkaline phosphatase indicates biliary cirrhosis.
- Serum immunoglobins: The IgG is increased in autoimmune hepatitis, IgA increases in alcoholic cirrhosis and IgM in primary biliary cirrhosis.
- Imaging
- Ultrasound examination: USG reveals changes in size, shape and echotexture of the liver.
- Fatt change and firosis produce diffse increases echogenicity.
- Presence of ascites, varices portal vein diameter and enlarge in size of spleen can be determined on ultrasound.
- Barium meal swallow is done for esophageal varices.
- Endoscopy can be done for detection and for treatment of varices
- Liver biopsy: It is also necessary to confirm the diagnosis of cirrhosis.
Management of case of cirrhosis of liver No treatment can reverse cirrhosis or even ensure that no further progression occurs, but medical therapy can improve general health and treat the symptom of disease effctively.
The main objectives are:
- Detect treatable causes
- Prevent and correct malnutrition
- Manage chronic cholestasis
- Treat the complication.
- Treatable causes: The treatable causes are alcohol abuse, drug ingestion, *hemochromatosis and Wilson’s disease, relief of biliary obstruction will prevent secondary biliary cirrhosis.
- Nutrition: In absence of ascites, a high energy 3000 kcal / day, protein rich (80–100 gm/day) diet should be advised.
Salt restriction is strictly required if ascites are present.
Fat intake is not restricted unless cholestasis is a feature.
Complete absence of alcohol.
Vitamin and other supplements are not required when good diet is taken. - Drug treatment: Any drug should be avoided because as most of the drugs are metabolized in the liver which are liable to develop toxic reaction because they will unable to get metabolize.
- Liver transplantation: It is considered in all patients with chronic liver disease who develop liver failure.
Question.32. Describe hepatitis-B under following headings.
- Etiology
- Clinical features
- Diagnosis
- Prophylaxis
Answer.
Diagnosis
Serology Hepatitis-B
- HBV consists of number of antigens. The three important antigens are hepatitis B surface antigen (HBsAg), core antigen (HBeAg) and hepatitis e antigen (HBeAg).
- Appearance of hepatitis B surface antigen (HBsAg) in serum is the fist evidence of infection.
It normally persists for 3–4 weeks, but can persist up to 6 months. - After disappearance of HBsAg, antibody against HBsAg (antiHBs) appears and persists for years and confers immunity.
Presence of antiHBs antibody means either previous infection or vaccination. - HBeAg is not seen in the blood.
However, antibody to it (antiHBc) appears early during the illness.
Presence of IgM antiHBc indicates acute infection and IgG antiHBc suggests chronic infection (when HBsAg positive) or recovery (when antiHBs positive). - Presence of HBeAg indicates active viral replication and high degree of infectivity.
AntiHBe appears as HBeAg disappears and its presence suggests low level of viral replication and decreased infectivity.
Above mentioned serological tests are done to identify the cause of hepatitis.
Viral Blood Hepatitis-B
- HBV DNA is measured by polymerase chain reaction in blood.
- Viral loads are in excess of 105 copies/mL in presence of active viral replication.
Other Investigations Hepatitis-B
- During early phase of hepatitis there is an increase in more than 400 units/L increase in plasma Alaline aminotransferase and aspartate aminotransferase.
- High levels of alkaline phosphatase are suggestive of cholestasis.
- Prothrombin time is increased which indicates severe liver damage

Leave a Reply