Insulin And Oral Hypoglycemic Drugs
Question 1. Write Basis Of Use Of Insulin In Type 1 Diabetes.
Or
Write The Basis Of Use Of Insulin In Juvenile Diabetes.
Answer:
In Type I diabetes mellitus 90% of beta cells of the pancreas are destroyed by an autoimmune process. In this type of diabetes mellitus, there is complete insulin deficiency.
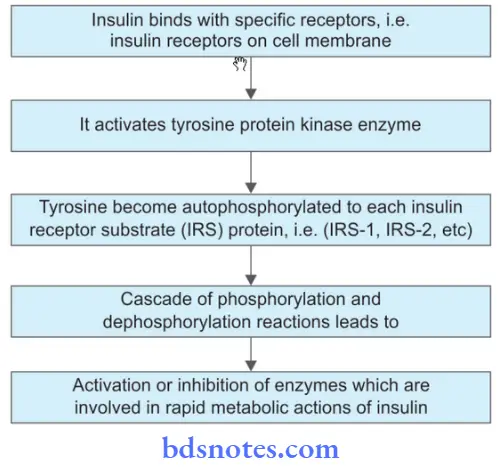
So here insulin binds to tyrosine kinase receptors which lie over the cell membrane The receptor consists of two α and β subunits.
Here α subunits are extracellular while β subunits are transmembrane proteins along with tyrosine kinase activity.
As insulin binds to α subunits this activates tyrosine kinase activity of β subunits which leads to phosphorylation of the tyrosine residue of the receptor.
Oral Hypoglycemic Drugs Mechanism Of Action
In turn, there is the occurrence of phosphorylation and dephosphorylation reactions which causes the entry of glucose inside the cell and mediate various actions of insulin.
Average Insulin Dose Type 1 Diabetes – The main aim of insulin is to maintain fasting blood glucose between 90 and 120 mg/dl and postprandial glucose levels below 150 mg/dl.
Read And Learn More: Pharmacology Question And Answers
Oral Hypoglycemic Drugs Mechanism Of Action Of Insulin
- Carbohydrate metabolism: Insulin decreases blood glucose levels, inhibits glycogenolysis, inhibits gluconeogenesis, promotes glycogenesis in muscle and liver, and increases the rate of utilization of glucose.
- Protein metabolism: It promotes protein synthesis and inhibits protein breakdown.
- Fat metabolism: Insulin promote the synthesis of free fatty acids and triglyceride and inhibit lipolysis.
- It increases potassium entry into the cells.
- It decreases urea output from the liver.
Question 2. Write Classification And Uses Of Insulin.
Answer:
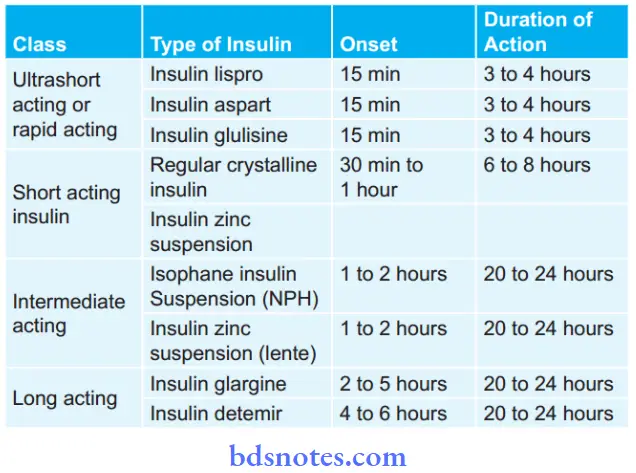
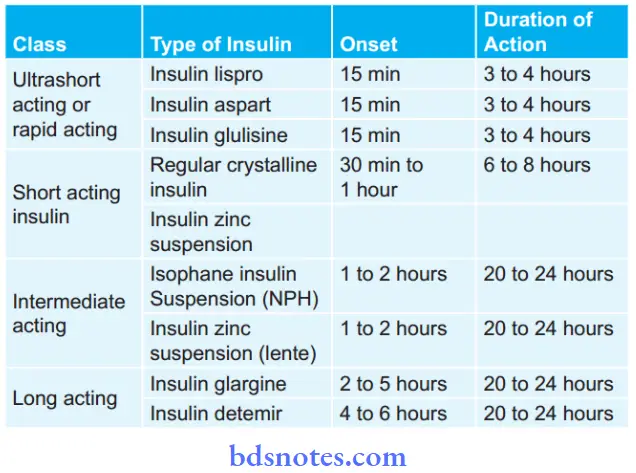
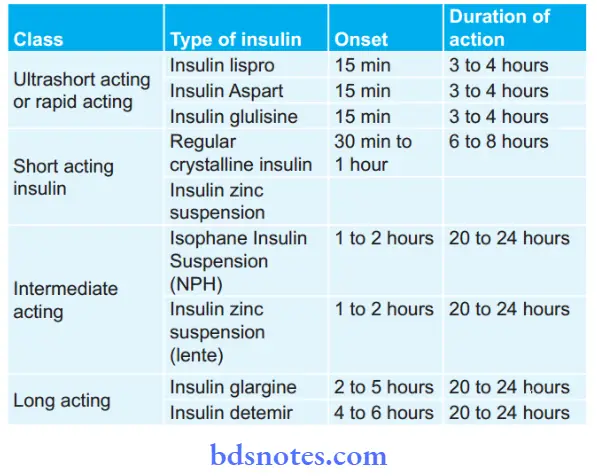
Classification of insulin preparation based on onset and duration of action
Classification Of Insulin Based On Its Source
- Bovine insulin or Beef insulin: It differs from human insulin by three amino acid residues and is more antigenic to men.
- Porcine insulin or pig insulin: It differs from human insulin by one amino acid residue and is less immunogenic.
- Human insulin: It is prepared by enzymatic modification of porcine insulin or DNA recombinant technology. This insulin is the least immunogenic.
Uses Of Type 1 Diabetes Insulin
- In Type I diabetes mellitus or Juvenile diabetes.
- In diabetic ketoacidosis
- In non-ketotic hyperglycemic coma.
- In diabetes at the time of pregnancy
- In diabetics during surgery, infection, and trauma.
- In gangrene of extremities in diabetics.
- In patients with Type II diabetes mellitus when oral hypoglycemics fail.
Question 3. Describe the Indication Of Type I diabetes Insulin or Type 1 Diabetes Risk Factors
Answer:
The following are the indications of insulin:
- In Type I diabetes mellitus or Juvenile diabetes.
- In diabetic ketoacidosis
- In a non-ketotic hyperglycemic coma
- In diabetes at the time of pregnancy
- In diabetics during surgery, infection, and trauma
- In gangrene of extremities in diabetics
- In patients with Type II diabetes mellitus when oral hypoglycemics fail.
Question 4. Describe Various Preparation Of Diabetes Insulin.
Or
Give A Description Of The Preparation Of Diabetes Insulin.
Or
Describe Insulin Preparations.
Or
Write Short Note On Diabetes Insulin Preparations.
Answer:
Various insulin preparations are based on the onset and duration of action.
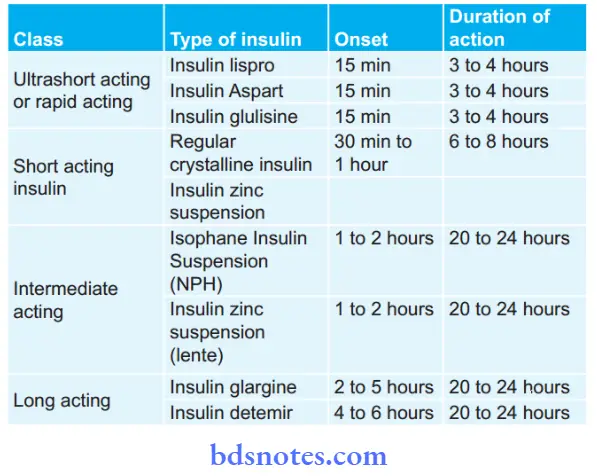
Rapidly Acting Diabetes Insulin Preparations
- It consists of insulin lispro, insulin aspart, insulin glulisine
- These insulins are in the form of clear solutions
- This insulin forms fewer hexamers.
- On giving subcutaneously they immediately dissociate in monomers and rapidly get absorbed.
- They get mixed with all types of insulin solutions.
- These insulin preparations are taken just before meals.
- They lower the risk of late postprandial hypoglycemia.
Diabetes Short Acting Insulin
- These insulin preparations are short-acting and soluble.
- This insulin forms hexamers.
- On giving subcutaneously they are slowly absorbed.
- Their onset of actions occurs within 30 min and is administered 30 to 45 min before meals.
- They can be given IM and IV also.
- Regular insulin is a clear solution and can be mixed with all types of insulin preparations.
Diabetes Intermediate Acting Insulin
- These insulins are complexed with protamine and zinc.
- On giving subcutaneously they dissociate slowly
- Their onset of action is delayed and the duration of action is 10 to 20 hours.
- Their solution is cloudy.
- They should be given once or twice daily subcutaneously.
Long-Acting Diabetes Insulin
- These insulins should be given subcutaneously.
- They have a prolonged duration of action.
- They cannot be mixed with any other human insulin due to their acidic Ph.
- They should be avoided in pregnant patients.
- Glargine has a lower risk of nocturnal hypoglycemia and provides better-fasting blood glucose levels as compared to NPH insulin.
Diabetes Insulin Detemir
- On giving subcutaneously it binds to albumin in the blood, and they have prolonged duration of action.
- They have minimal peak levels.
- It is given twice a day.
Diabetes Insulin Preparations Based On Its Source
- Bovine insulin or Beef insulin: It differs from human insulin by three amino acid residues and is more antigenic to men.
- Porcine insulin or pig insulin: It differs from human insulin by one amino acid residue and is less immunogenic.
Both bovine and porcine insulin are antigenic so they are not used. - Human insulin: It is prepared by enzymatic modification of porcine insulin or DNA recombinant technology. This insulin is the least immunogenic. In this resistance to insulin and lipodystrophy at the site of injection is very rare.
Question 5. Discuss Management Of Diabetic Coma.
Answer:
Diabetic coma is seen in insulin-dependent diabetes mellitus and less in non-insulin diabetes mellitus.
During the diabetic coma, the symptoms are hyperglycemia, acidosis, hyperventilation, dehydration, hypotension, shock, and impaired consciousness.
Management Of Diabetic Coma
- Replacement of insulin: Administer IV bolus of regular insulin of dose 0.2 to 0.3 U/Kg followed by 0.1 U/Kg/hr IV infusion. The level of blood glucose should decrease by 10% an hour.
For optimal insulin replacement monitoring of blood glucose level is done. As the patient becomes conscious, insulin is given subcutaneously. - Fluid replacement: Initially IV infusion of normal saline is done at 1L/hr, then the rate of infusion should be decreased gradually which depends on the requirement of the patient.
As blood glucose levels fall below 250 mg/dL, 5% glucose in 0.5 N saline is given to prevent hypoglycemia and cerebral edema. - Potassium chloride: KCl 10 to 20 mEq/hr is infused after 4 hours of initiation of insulin therapy. For determining the potassium replacement serum potassium and ECG should be monitored.
- IV sodium bicarbonate should be given.
- If the patient has hypophosphatemia, phosphate replacement is given.
- Antibiotics are to be given to treat the infection.
Question 6. Describe Oral Antidiabetic Drugs.
Or
Enumerate And Write The Mode Of Actions Of Oral Antidiabetic Drugs.
Or
Write Short Note On Oral Hypoglycemic Drugs.
Answer:
Oral antidiabetic drugs lower blood glucose levels on oral administration.
Classification Of Antidiabetic Or Hypoglycemic Drugs
1. Enhance insulin secretion
- Sulfonylureas (KATP channel blockers)
- Ist Generation: Tolbutamide and chlorpropamide
- IInd Generation: Glibenclamide, glipizide, gliclazide and glimepiride
- Meglitinide/phenylalanine analogs: Repaglinide, Nateglinide
- Glucagon-like peptide-1 (GLP-1) receptor agonists: Exenatide, Liraglutide
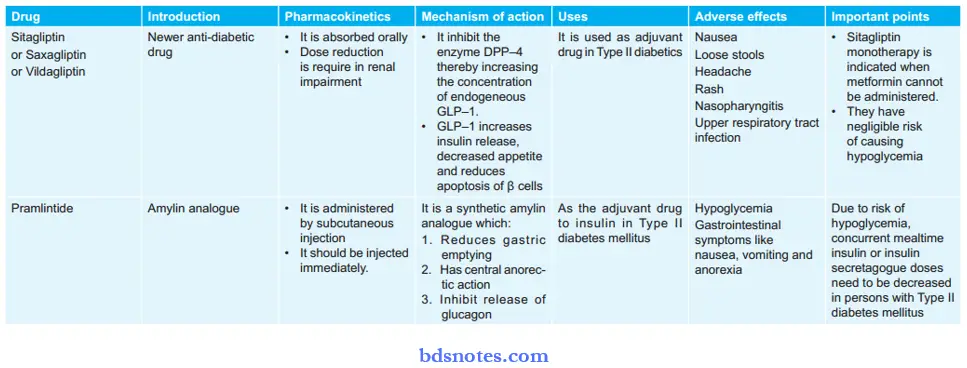
- Dipeptidyl peptidase-4 (DPP- 4): Sitagliptin, Saxagliptin, Vildagliptin, Alogliptin, Linagliptin
2. Drugs overcoming insulin resistance
- Biguanides (AMPk activator): Phenformin, Metformin
- Thiazolidinediones (PPARγ activator): Rosiglitazone, Pioglitazone.
3. Miscellaneous antidiabetic drugs
- α-Glucosidase Inhibitor: Acarbose, Miglitol, Voglibose
- Amylin analog: Pramlintide
- Dopamine – D2 receptor agonist: Bromocriptine
- Sodium-glucose cotransport-2 (SGLT-2) inhibitor: Dapagliflzine.
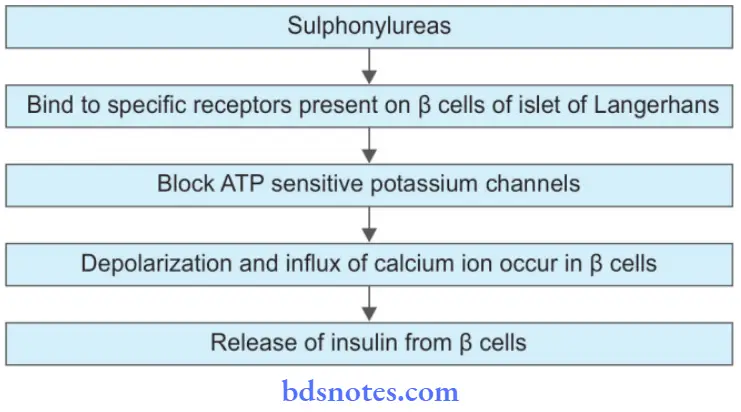
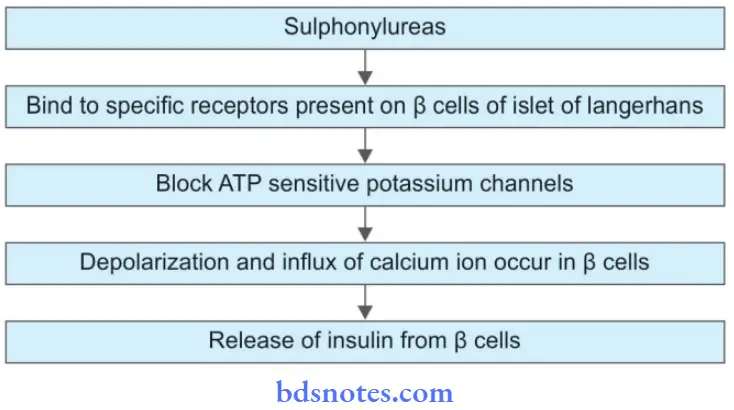
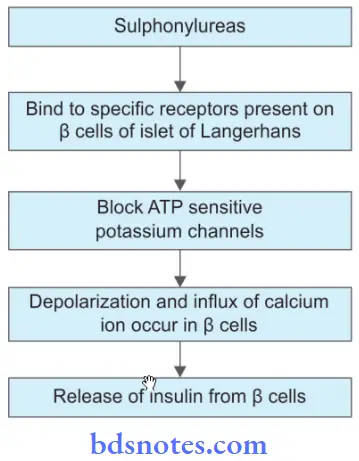
Mechanism Of Action Sulphonylureas
Mechanism Of Action Biguanides
- They suppress gluconeogenesis in the liver.
- They promote peripheral utilization of glucose.
- They inhibit intestinal absorption of glucose, amino acid, and vitamin B12.
Mechanism Of Action Meglitinides
These drugs stimulate insulin release by closing ATP-sensitive potassium channels in β cells of islet of L Langerhans leading to depolarization and causing the release of insulin.
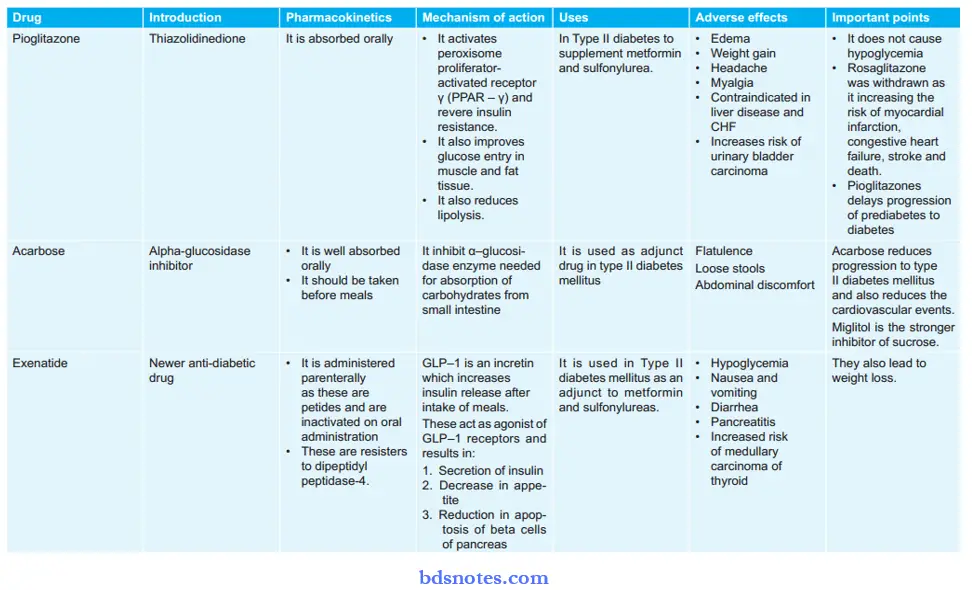
Mechanism Of Action Thiazolidinediones
These drugs bind to nuclear peroxisome proliferator-activated receptor – γ which causes activation of insulin-responsive genes and sensitizes peripheral tissues to insulin which decreases blood glucose by:
- Increasing transport of glucose in muscle and adipose tissue
- By inhibiting liver gluconeogenesis
- By promoting lipogenesis.
α Glucosidase Inhibitors
These drugs lead to the reduction of intestinal absorption of carbohydrates by inhibiting enzyme α glucosidase and decreasing postprandial hyperglycemia.
Newer Drugs
- GLP-1 receptor agonist: It suppresses the release of glucagon and stimulates insulin secretion.
- DPP-4 inhibitor: It inhibits enzyme DPP-4 decreases the release of glucagon and increases insulin secretion.
Uses Of Oral Antidiabetic Drugs
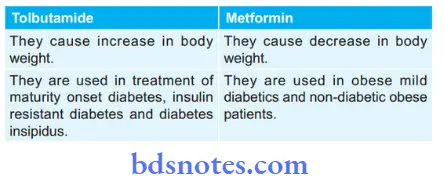
- Sulfonylureas are used in the treatment of maturity-onset diabetes, insulin-resistant diabetes, and diabetes insipidus.
- Biguanides are used in obese mild diabetics, non-diabetic obese patients, and patients allergic to sulfonylureas.
- Meglitinides are used in type II diabetes mellitus for controlling postprandial hyperglycemia.
- Thiazolidinediones are used in combination with sulphonylureas or metformin in Type II diabetes mellitus.
- Alpha-glucosidase inhibitors are used in Obese type II diabetes mellitus patients
- Both the newer drugs, i.e. GLP-1 receptor agonist and DPP-4 inhibitors are used in Type II diabetes mellitus patients.
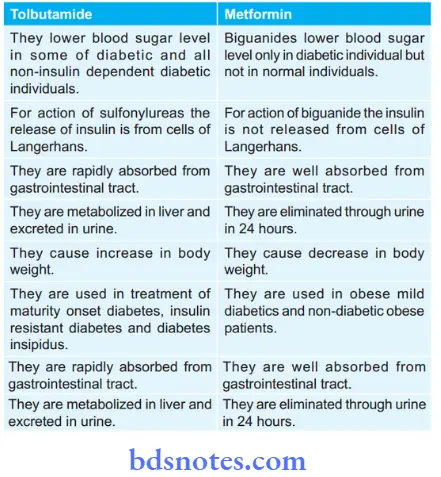
Question 7. Compare And Contrast Tolbutamide And Metformin.
Answer:
Question 8. Classify oral hypoglycemic drugs. Discuss sulphonylureas in detail
Answer:
Classification Of Antidiabetic Or Hypoglycemic Drugs
1. Enhance insulin secretion
- Sulfonylureas (KATP channel blockers)
- Ist Generation: Tolbutamide and chlorpropamide
- IInd Generation: Glibenclamide, glipizide, gliclazide and glimepiride
- Meglitinide/phenylalanine analogs: Repaglinide, Nateglinide
- Glucagon-like peptide-1 (GLP-1) receptor agonists: Exenatide, Liraglutide
- Dipeptidyl peptidase-4 (DPP- 4): Sitagliptin, Saxagliptin, Vildagliptin, Alogliptin, Linagliptin
2. Drugs overcoming insulin resistance
- Biguanides (AMPk activator): Phenformin, Metformin
- Thiazolidinediones (PPARγ activator): Rosiglitazone, Pioglitazone.
3. Miscellaneous antidiabetic drugs
- α-Glucosidase Inhibitor: Acarbose, Miglitol, Voglibose
- Amylin analog: Pramlintide
- Dopamine – D2 receptor agonist: Bromocriptine
- Sodium-glucose cotransport-2 (SGLT-2) inhibitor: Dapagliflzine.
The sulfonyl urea is an antidiabetic drug.
The sulfonylurea consists of two generations, i.e.
lst generation: Tolbutamide and Chlorpropamide.
IInd generation: Glibenclamide, glipimide, glicazide and glimepiride.
Pharmacological Actions
- These drugs lower blood sugar levels on oral and parenteral administration.
- They lower blood sugar levels in some of the diabetics and all nondiabetic patients.
- They are effective only in the presence of a functional pancreas.
- They produce an increase in body weight.
Mechanism Of Action
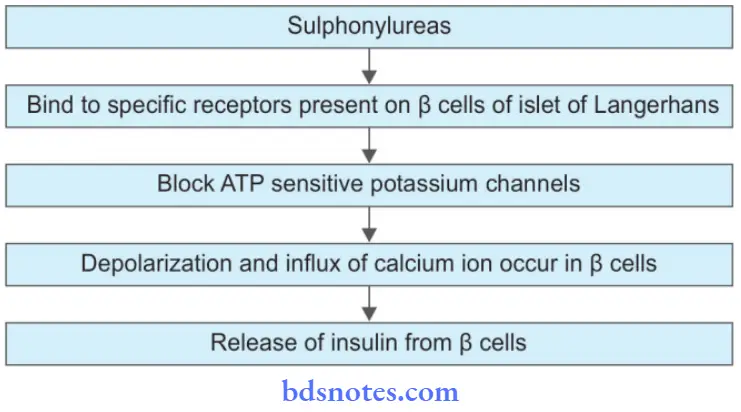
- Sulfonylureas also increase the sensitivity of peripheral tissues to insulin by increasing the number of insulin receptors.
- Sulfonylureas decreases the release of glucagon.
Absorption, Fate, And Excretion Or Pharmacokinetics
Sulphonylureas are rapidly absorbed from the gastrointestinal tract. They are partly bound to plasma proteins. They are metabolized in the liver and are excreted in the urine.
Pharmacokinetics Adverse Reaction
- Hypoglycemia and its effect are potentiated by phenylbutazone and salicylates.
- Allergic reactions lead to skin rashes.
- Bone marrow changes like leucopenia and thrombocytopenia are caused.
- It also leads to hyperthyroidism and goiter.
Pharmacokinetics Therapeutic Uses
Sulfonylureas are used in the treatment of maturity-onset diabetes, insulin-resistant diabetes, and diabetes insipidus.
Pharmacokinetics Drug Interactions
- Sulphonylureas along with salicylates or sulphonamides: Salicylates or sulphonamides bound to plasma protein and displace sulfonylureas from the plasma protein binding site which causes an increase in free plasma concentration of sulfonylureas which leads to hypoglycemia.
- Propranolol with sulfonylureas: Propranolol blocks β2 receptors and inhibits glycogenolysis and delay in recovery from hypoglycemia.
- Rifampicin, phenobarbitone along with sulphonylureas: Both Rifampicin and phenobarbitone are enzyme inducers and they increase the metabolism of sulfonylureas and decrease their effects.
- Warfarin, sulphonamides along with sulphonylureas: These drugs inhibit the metabolism of sulphonylureas and increase its plasma level which causes severe hypoglycemia.
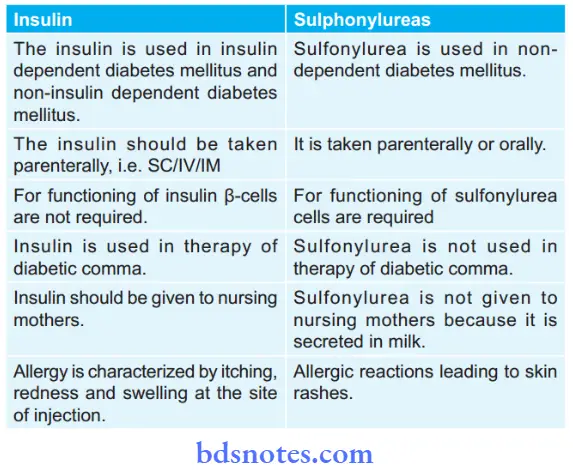
Question 9. Compare And Contrast Insulin And Sulfonylureas.
Answer:
Question 10. Write The Drug Treatment Of Juvenile Diabetes.
Answer:
Juvenile diabetes is an insulin-dependent diabetes mellitus. It is immune-mediated and there is the destruction of β-cells due to which deficiency of insulin occurs.
Treatment Of Juvenile Diabetes
Along with diet, insulin therapy is given. Insulin therapy is generally started with regular insulin given parenterally as subcutaneously before each major meal. The requirement is assessed by testing urine or blood glucose level.
Dosage: 0.4–0.5 U/kg/day.
Question 11. Write A Note On Glipizide.
Answer:
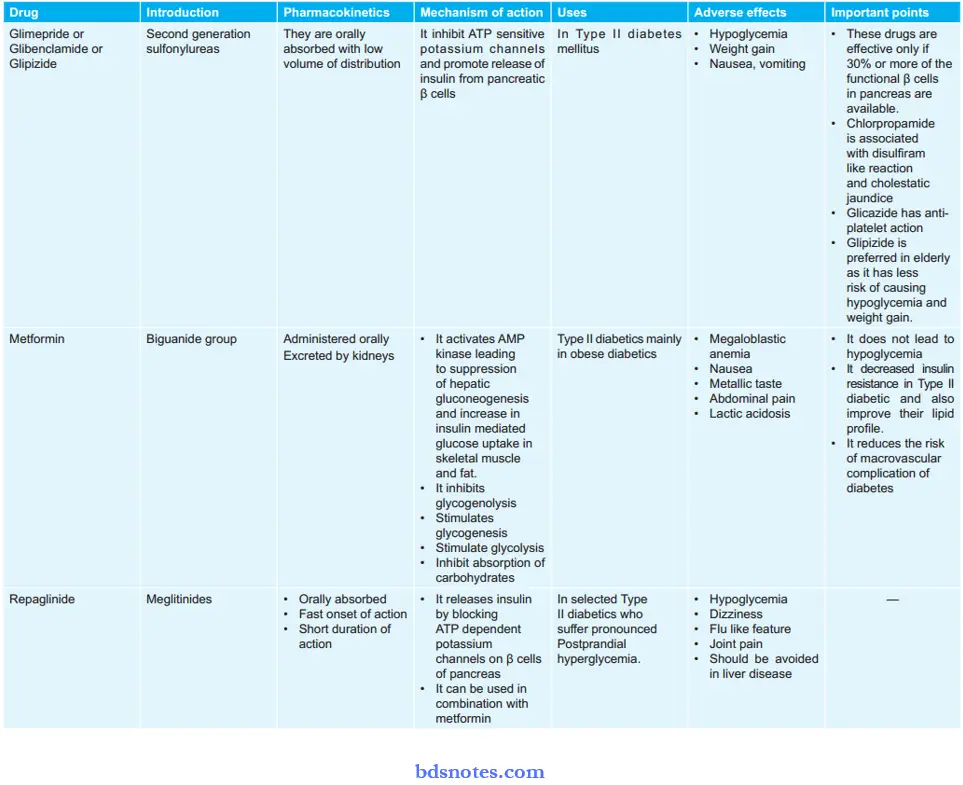
Glipizide is a second-generation sulphonylurea drug.
Glipizide has lower potency and a shorter duration of action.
Glipizide Mechanism Of Action
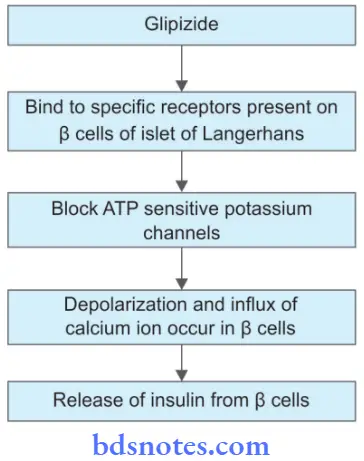
Glipizide Pharmacokinetics
It is absorbed orally with a low volume of distribution.
Glipizide Indication
It is indicated in Type II diabetes mellitus. It is preferred in the elderly as it has less risk of causing hypoglycemia and weight gain.
Glipizide Adverse Effects
- Hypoglycemia
- Weight gain
- Nausea and vomiting.
Glipizide Dosage
It can be given 5 to 40 mg in one to two doses for 12 to 18 hours.
Question 12. Compare And Contrast Conventional Insulin With Newer Insulin.
Answer:
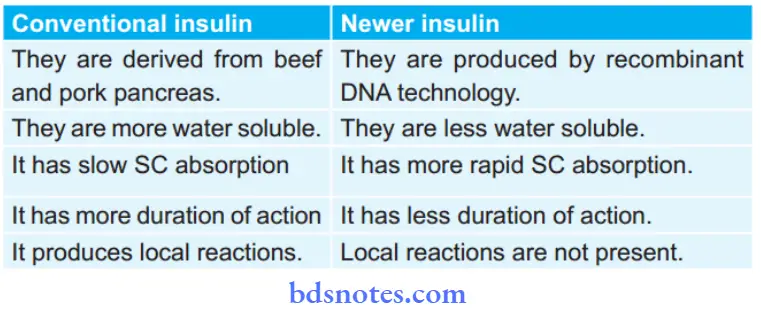
Question 13. Write A Short Note On Human Insulin.
Answer:
It is prepared either by enzymatic modification of porcine insulin (semisynthetic human insulin) or by DNA recombinant technology. Human insulin is the least immunogenic.
- Human insulin is more water soluble as well as hydrophobic than porcine or bovine insulin.
- It has more rapid subcutaneous absorption, an earlier and more defined peak, and a slightly shorter duration of action.
- Human insulin was alleged to produce hypoglycemic unawareness, exposing the patients to the risk of severe hypoglycemia.
- After prolonged treatment, irrespective of the type of insulin, many diabetics develop relative hypoglycemic unawareness or change in symptoms, because of autonomic neuropathy, change in perception/attitude, and other factors.
Human Insulin Mechanism Of Action
Human Insulin Actions
- Carbohydrate metabolism: Insulin decreases blood glucose levels, inhibits glycogenolysis, inhibits gluconeogenesis, promotes glycogenesis in muscle and liver, and increases the rate of utilization of glucose.
- Protein metabolism: It promotes protein synthesis and inhibits protein breakdown.
- Fat metabolism: Insulin promote the synthesis of free fatty acids and triglyceride and inhibit lipolysis.
- It increases potassium entry into the cells.
- It decreases urea output from the liver.
Human Insulin Uses
- In juvenile diabetic patients.
- In non-insulin-dependent diabetes mellitus, it is required when diabetes is not controlled by diet or exercise.
- When there is failure of diabetes control by oral hypoglycemia.
- In patients having stressed the surgical procedure, infection, trauma, pregnancy, and labor.
- In diabetic patients having gangrene of extremities.
- In patients suffering from diabetic ketoacidosis.
Human Insulin Side Effects
The following are the adverse effects of insulin:
- Hypoglycemia is the most frequent and the most serious reaction to insulin.
- Hypoglycemia can occur in any diabetic following inadvertent injection of large doses, by missing a meal, or by performing vigorous exercise. The symptoms can be divided into those due to counter-regulatory sympathetic
stimulation—sweating, anxiety, palpitation, tremor; and those due to deprivation of the brain of its essential nutrient glucose (neuroglycopenia symptoms)—dizziness, headache, behavioral changes, visual disturbances,
hunger, fatigue, weakness, muscular incoordination and sometimes fall in BP. Generally, the reflex sympathetic symptoms occur before neuroglycopenia.
Finally, when blood glucose falls further (to < 40 mg/dl) mental confusion, seizures, and coma occur. - Local reactions: Swelling, erythema, and stinging sometimes occur at the injection site, especially in the beginning. Localized lipodystrophy occurs in the subcutaneous fat after long usage.
- Allergy: This is infrequent and is due to contaminating proteins. It is very rare with human/highly purified insulins. Urticaria, angioedema, and anaphylaxis are the manifestations.
- Nonspecific adverse effects: These are headache, paresthesia, weight gain, nausea, diarrhea, vomiting, and constipation.
- Insulin resistance: The development of acute insulin resistance is due to trauma, surgery, psychological stress, etc. Chronic insulin resistance occurs in patients with the usage of prolonged conventional beef or pork insulin.
Question 14. Write Important Uses, Side Effects, And Contraindications Of Any Human Insulin.
Answer:
Human Insulin Uses
- In juvenile diabetic patients.
- In non-insulin-dependent diabetes mellitus, it is required
- when diabetes is not controlled by diet or exercise.
- When there is failure of diabetes control by oral hypoglycemia.
- In patients having stress from the surgical procedure, infections, trauma, pregnancy, and labor.
- In diabetic patients having gangrene of extremities.
- In patients suffering from diabetic ketoacidosis.
Human Insulin Side Effects
The following are the adverse effects of insulin:
- Hypoglycemia is the most frequent and the most serious reaction to insulin.
- Hypoglycemia can occur in any diabetic following inadvertent injection of large doses, by missing a meal, or by performing vigorous exercise. The symptoms can be divided into those due to counter-regulatory sympathetic
stimulation—sweating, anxiety, palpitation, tremor; and those due to deprivation of the brain of its essential nutrient glucose (neuroglycopenia symptoms)—dizziness, headache, behavioral changes, visual disturbances,
hunger, fatigue, weakness, muscular incoordination and sometimes fall in BP. Generally, the reflex sympathetic symptoms occur before neuroglycopenia.
Finally, when blood glucose falls further (to < 40 mg/dl) mental confusion, seizures, and coma occur. - Local reactions: Swelling, erythema, and stinging sometimes occur at the injection site, especially in the beginning. Localized lipodystrophy occurs in the subcutaneous fat after long usage.
- Allergy: This is infrequent and is due to contaminating proteins. It is very rare with human/highly purified insulins. Urticaria, angioedema, and anaphylaxis are the manifestations.
- Nonspecific adverse effects: These are headache, paresthesia, weight gain, nausea, diarrhea, vomiting, and constipation.
- Insulin resistance: The development of acute insulin resistance is due to trauma, surgery, psychological stress, etc. Chronic insulin resistance occurs in patients with the usage of prolonged conventional beef or pork insulin.
Human Insulin Contraindications
- Beta-adrenergic blockers prolong hypoglycemia by inhibiting compensatory mechanisms operating through β2 receptors.
- Thiazides, furosemide, corticosteroids, oral contraceptives, salbutamol, and nephidipine tend to raise blood sugar and reduce the effectiveness of human insulin.
- Acute ingestion of alcohol can precipitate hypoglycemia by depleting hepatic glycogen.
- Lithium, high-dose aspirin, and theophylline may also accentuate hypoglycemia by enhancing insulin secretion and peripheral glucose utilization.
Question 15. Enumerate The Adverse Effects Of Insulin.
Or
Write A Short Note On The Adverse Effects Of Conventional Insulin Preparation.
Answer:
Following are the adverse effects of insulin.
- Hypoglycemia is the most frequent and the most serious reaction to insulin.
Hypoglycemia can occur in any diabetic following inadvertent injection of large doses, by missing a meal, or by performing vigorous exercise. The symptoms can be divided into those due to counterregulatory sympathetic stimulation—sweating, anxiety, palpitation, tremor; and those due to deprivation of the brain of its essential nutrient glucose (neuroglycopenia symptoms)—dizziness, headache, behavioral changes, visual disturbances, hunger, fatigue, weakness, muscular incoordination and sometimes falling. Generally, the reflex sympathetic symptoms occur before neuroglycopenia.
Finally, when blood glucose falls further (to < 40 mg/ dl) mental confusion, seizures, and coma occur. - Local reactions: Swelling, erythema, and stinging sometimes occur at the injection site, especially in the beginning. Localized lipodystrophy occurs in the subcutaneous fat after long usage.
- Allergy: This is infrequent and is due to contaminating proteins. It is very rare with human/highly purified insulins. Urticaria, angioedema, and anaphylaxis are the manifestations.
- Nonspecific adverse effects: These are headache, paresthesia, weight gain, nausea, diarrhea, vomiting, and constipation.
- Insulin resistance: The development of acute insulin resistance is due to trauma, surgery, psychological stress, etc. Chronic insulin resistance occurs in patients with the usage of prolonged conventional beef or pork insulin.
Question 16. Explain Oral Hypoglycemic Drugs Are Not Indicated In The Treatment Of Juvenile Diabetes.
Answer:
It is important to note that because type 1 diabetes results from an absolute deficiency of pancreatic β-cells, most oral agents are not indicated in the treatment of patients with type 1 diabetes. Type 1 diabetes involves a lack of insulin and requires insulin for treatment.
Question 17. Classify and enumerate insulin preparations and oral hypoglycemic. Discuss the treatment of diabetic ketoacidosis.
Answer:
Classification Of Insulin Preparation
Classification of insulin preparation based on onset and duration of action
Classification Of Insulin Based On Its Source
- Bovine insulin or Beef insulin: It differs from human insulin by three amino acid residues and is more antigenic to men.
- Porcine insulin or pig insulin: It differs from human insulin by one amino acid residue and is less immunogenic.
- Human insulin: It is prepared by enzymatic modification of porcine insulin or DNA recombinant technology. This insulin is the least immunogenic.
Enumeration Of Insulin Preparation
- Ultra short-acting insulins
- Insulin lispro
- Insulin aspart.
- Short-acting insulins
- Regular crystalline insulin
- Insulin zinc suspension.
- Intermediate-acting insulins
- Isophane Insulin Suspension (NPH)
- Insulin zinc suspension (lente).
- Long-acting insulins.
- Protamine zinc insulin (PZI)
- Extended insulin zinc suspension (Ultra lente)
- Glargine.
Treatment Of Diabetic Ketoacidosis
- Treatment is with regular insulin as IV bolus in a dose of 0.2 to 0.3 U/Kg followed by 0.1 U/Kg/Hour IV infusion.
- After the patient has fully recovered, SC insulin should be administered 30 minutes before stopping the infusion.
- Fluid and electrolyte replacement should be done. Normal saline is infused IV, initially at the rate of 1L/hr and then the rate of infusion is decreased depending on the requirement of the patient.
- KCl 10–20 mEq/hr is added to IV fluid after 4 hours of initiation of insulin therapy.
- Sodium bicarbonate IV is administered if needed.
- When serum phosphate is in the low normal range 5-10 m mol/hr of sodium or potassium phosphate is infused.
- Antibiotics and supportive measures should be used.
Classification And Enumeration Of Oral Hypoglycemic Drugs
1. Enhance insulin secretion
- Sulfonylureas (KATP channel blockers)
- Ist Generation: Tolbutamide and chlorpropamide
- IInd Generation: Glibenclamide, glipizide, gliclazide and glimepiride
- Meglitinide/phenylalanine analogs: Repaglinide, Nateglinide
- Glucagon-like peptide-1 (GLP-1) receptor agonists: Exenatide, Liraglutide
- Dipeptidyl peptidase-4 (DPP- 4): Sitagliptin, Saxagliptin, Vildagliptin, Alogliptin, Linagliptin
2. Drugs overcoming insulin resistance
- Biguanides (AMPk activator): Phenformin, Metformin
- Thiazolidinediones (PPARγ activator): Rosiglitazone, Pioglitazone.
3. Miscellaneous antidiabetic drugs
- α-Glucosidase Inhibitor: Acarbose, Miglitol, Voglibose
- Amylin analog: Pramlintide
- Dopamine – D2 receptor agonist: Bromocriptine
- Sodium-glucose cotransport-2 (SGLT-2) inhibitor: Dapagliflzine.
The sulfonyl urea is an antidiabetic drug.
The sulfonylurea consists of two generations, i.e.
lst generation: Tolbutamide and Chlorpropamide.
IInd generation: Glibenclamide, glipimide, glicazide and glimepiride.
Question 18. Classify The Oral Antidiabetic Drugs. Write In Brief The Mechanism Of Action, Adverse Effects, And Therapeutic Uses Of Biguanides.
Answer:
Classification Of Oral Antidiabetic Or Hypoglycemic Drugs
1. Enhance insulin secretion
- Sulfonylureas (KATP channel blockers)
- Ist Generation: Tolbutamide and chlorpropamide
- IInd Generation: Glibenclamide, glipizide, gliclazide and glimepiride
- Meglitinide/phenylalanine analogs: Repaglinide, Nateglinide
- Glucagon-like peptide-1 (GLP-1) receptor agonists: Exenatide, Liraglutide
- Dipeptidyl peptidase-4 (DPP- 4): Sitagliptin, Saxagliptin, Vildagliptin, Alogliptin, Linagliptin
2. Drugs overcoming insulin resistance
- Biguanides (AMPk activator): Phenformin, Metformin
- Thiazolidinediones (PPARγ activator): Rosiglitazone, Pioglitazone.
3. Miscellaneous antidiabetic drugs
- α-Glucosidase Inhibitor: Acarbose, Miglitol, Voglibose
- Amylin analog: Pramlintide
- Dopamine – D2 receptor agonist: Bromocriptine
- Sodium-glucose cotransport-2 (SGLT-2) inhibitor: Dapagliflzine.
Metformin is the only used biguanide that is used clinically.
Mechanism Of Action
- It suppresses hepatic gluconeogenesis and glucose output from the liver. Enhance insulin-mediated glucose disposal in muscle and fat.
- Retard intestinal absorption of glucose, other hexoses, amino acids, and vitamin B 12.
- It interferes with the mitochondrial respiratory chain and promotes peripheral glucose utilization by enhancing anaerobic glycolysis.
Adverse Effects
- Abdominal pain
- Anorexia
- Nausea
- Metallic taste
- Mild diarrhea
- Tiredness
- Loss of weight
- Skin rashes
- Lactic acidosis is the most serious complication and is rare with metformin
- Prolonged use can cause vitamin B12 deficiency.
Therapeutic Effects
Biguanides are used in obese mild diabetics, non-diabetic obese patients, and in patients allergic to sulfonylureas.
Question 19. Explain Why Glimepiride Is Used In The Treatment Of Diabetes Mellitus.
Answer:
Glimepiride is the second-generation sulphonylurea. It acts on so-called sulphonylurea receptors on the pancreatic β cell membrane and causes depolarization by reducing the conductance of ATP-sensitive K+ channels.
This enhances calcium influx degranulation and insulin release. That’s why glimepiride is used in the treatment of diabetes mellitus.
Question 20. Classify Antidiabetic Drugs. What Are The Adverse Effects Of Insulin?
Answer:
Diabetes mellitus is a chronic metabolic disorder that is characterized by hyperglycemia and altered metabolism of carbohydrates.
Diabetes mellitus is divided into two types, i.e. Type I insulin-dependent diabetes mellitus and Type II non-insulin diabetes mellitus.
Insulin is the antidiabetic drug used in the treatment of Type I diabetes mellitus and oral antidiabetic drugs or oral hypoglycemic drugs are used in the treatment of Type II diabetes mellitus.
Classification Of Antidiabetic Drugs
Various insulin preparations are based on the onset and duration of action.
Rapidly Acting Insulin Preparations
- It consists of insulin lispro, insulin aspart, insulin glulisine
- These insulins are in the form of clear solutions
- This insulin forms fewer hexamers.
- On giving subcutaneously they immediately dissociate in monomers and rapidly get absorbed.
- They get mixed with all types of insulin solutions.
- These insulin preparations are taken just before meals.
- They lower the risk of late postprandial hypoglycemia.
Short Acting Insulin
- These insulin preparations are short-acting and soluble.
- This insulin forms hexamers.
- On giving subcutaneously they are slowly absorbed.
- Their onset of actions occurs within 30 min and is administered 30 to 45 min before meals.
- They can be given IM and IV also.
- Regular insulin is a clear solution and can be mixed with all types of insulin preparations.
Intermediate Acting Insulin
- These insulins are complexed with protamine and zinc.
- On giving subcutaneously they dissociate slowly
- Their onset of action is delayed and the duration of action is 10 to 20 hours.
- Their solution is cloudy.
- They should be given once or twice daily subcutaneously.
Long-Acting Insulin
- These insulins should be given subcutaneously.
- They have a prolonged duration of action.
- They cannot be mixed with any other human insulin due to their acidic Ph.
- They should be avoided in pregnant patients.
- Glargine has a lower risk of nocturnal hypoglycemia and provides better-fasting blood glucose levels as compared to NPH insulin.
Insulin Detemir
- On giving subcutaneously it binds to albumin in the blood, and they have prolonged duration of action.
- They have minimal peak levels.
- It is given twice a day.
Insulin Preparations Based On Its Source
- Bovine insulin or Beef insulin: It differs from human insulin by three amino acid residues and is more antigenic to men.
- Porcine insulin or pig insulin: It differs from human insulin by one amino acid residue and is less immunogenic.
Both bovine and porcine insulin are antigenic so they are not used. - Human insulin: It is prepared by enzymatic modification of porcine insulin or DNA recombinant technology. This insulin is the least immunogenic. In this resistance to insulin and lipodystrophy at the site of injection is very rare.
Classification Of Antidiabetic Or Hypoglycemic Drugs
1. Enhance insulin secretion
- Sulfonylureas (KATP channel blockers)
- Ist Generation: Tolbutamide and chlorpropamide
- IInd Generation: Glibenclamide, glipizide, gliclazide and glimepiride
- Meglitinide/phenylalanine analogs: Repaglinide, Nateglinide
- Glucagon-like peptide-1 (GLP-1) receptor agonists: Exenatide, Liraglutide
- Dipeptidyl peptidase-4 (DPP- 4): Sitagliptin, Saxagliptin, Vildagliptin, Alogliptin, Linagliptin
2. Drugs overcoming insulin resistance
- Biguanides (AMPk activator): Phenformin, Metformin
- Thiazolidinediones (PPARγ activator): Rosiglitazone, Pioglitazone.
3. Miscellaneous antidiabetic drugs
- α-Glucosidase Inhibitor: Acarbose, Miglitol, Voglibose
- Amylin analog: Pramlintide
- Dopamine – D2 receptor agonist: Bromocriptine
- Sodium-glucose cotransport-2 (SGLT-2) inhibitor: Dapagliflzine.
Adverse Effects Of Insulin
Following are the adverse effects of insulin.
- Hypoglycemia is the most frequent and the most serious reaction to insulin.
Hypoglycemia can occur in any diabetic following inadvertent injection of large doses, by missing a meal, or by performing vigorous exercise. The
symptoms can be divided into those due to counterregulatory sympathetic stimulation—sweating, anxiety, palpitation, tremor; and those due to deprivation of the brain of its essential nutrient glucose (neuroglycopenia symptoms)—dizziness, headache, behavioral changes, visual disturbances, hunger, fatigue, weakness, muscular incoordination and sometimes falling. Generally, the reflex sympathetic symptoms occur before neuroglycopenia.
Finally, when blood glucose falls further (to < 40 mg/ dl) mental confusion, seizures, and coma occur. - Local reactions: Swelling, erythema, and stinging sometimes occur at the injection site, especially in the beginning. Localized lipodystrophy occurs in
the subcutaneous fat after long usage. - Allergy: This is infrequent and is due to contaminating proteins. It is very rare with human/highly purified insulins. Urticaria, angioedema, and anaphylaxis are the manifestations.
- Nonspecific adverse effects: These are headache, paresthesia, weight gain, nausea, diarrhea, vomiting, and constipation.
- Insulin resistance: The development of acute insulin resistance is due to trauma, surgery, psychological stress, etc. Chronic insulin resistance occurs in patients with the usage of prolonged conventional beef or pork insulin.
Question 21. Write Short Note On Pharmacological Actions Of Insulin.
Answer:
The following are the pharmacological actions of insulin:
- Carbohydrate metabolism: Insulin decreases blood glucose levels, inhibits glycogenolysis, inhibits gluconeogenesis, promotes glycogenesis in muscle and liver, and increases the rate of utilization of glucose.
- Protein metabolism: It promotes protein synthesis and inhibits protein breakdown.
- Fat metabolism: Insulin promote the synthesis of free fatty acids and triglyceride and inhibit lipolysis.
- It increases potassium entry into the cells.
- It decreases urea output from the liver.
Question 22. Write Short Note On Insulin Preparations And Adverse Effects Of Insulin Therapy.
Answer:
Insulin Preparations Based On Its Source
- Bovine insulin or Beef insulin: It differs from human insulin by three amino acid residues and is more antigenic to men.
- Porcine insulin or pig insulin: It differs from human insulin by one amino acid residue and is less immunogenic.
Both bovine and porcine insulin are antigenic so they are not used. - Human insulin: It is prepared by enzymatic modification of porcine insulin or DNA recombinant technology. This insulin is the least immunogenic. In this resistance to insulin and lipodystrophy at the site of injection is very rare.
Adverse Effects Of Insulin
Following are the adverse effects of insulin.
- Hypoglycemia is the most frequent and the most serious reaction to insulin.
Hypoglycemia can occur in any diabetic following inadvertent injection of large doses, by missing a meal, or by performing vigorous exercise. The
symptoms can be divided into those due to counterregulatory sympathetic stimulation—sweating, anxiety, palpitation, tremor; and those due to deprivation of the brain of its essential nutrient glucose (neuroglycopenia symptoms)—dizziness, headache, behavioral changes, visual disturbances, hunger, fatigue, weakness, muscular incoordination and sometimes falling. Generally, the reflex sympathetic symptoms occur before neuroglycopenia.
Finally, when blood glucose falls further (to < 40 mg/ dl) mental confusion, seizures, and coma occur. - Local reactions: Swelling, erythema, and stinging sometimes occur at the injection site, especially in the beginning. Localized lipodystrophy occurs in
the subcutaneous fat after long usage. - Allergy: This is infrequent and is due to contaminating proteins. It is very rare with human/highly purified insulins. Urticaria, angioedema, and anaphylaxis are the manifestations.
- Nonspecific adverse effects: These are headache, paresthesia, weight gain, nausea, diarrhea, vomiting, and constipation.
- Insulin resistance: The development of acute insulin resistance is due to trauma, surgery, psychological stress, etc. Chronic insulin resistance occurs in patients with the usage of prolonged conventional beef or pork insulin.
Question 23. Write A Short Note On the Indication Of Oral Hypoglycemic Drugs.
Answer:
Oral hypoglycemics are only indicated in Type II diabetes mellitus. They are best used in patients with.
- Age above 40 years at onset of disease.
- Obesity at the time of presentation.
- Duration of disease is less than 5 years when starting treatment.
- Fasting blood sugar < 200 mg/dl
- Insulin requirement < 40 units/day
- Nonketoacidosis or a history of it or any other complication.
- Sulfonylureas are used in the treatment of maturity-onset diabetes, insulin-resistant diabetes, and diabetes insipidus.
- Biguanides are used in obese mild diabetics, nondiabetic obese patients, and patients allergic to sulfonylureas.
- Meglitinides are used in type II diabetes mellitus for controlling postprandial hyperglycemia.
- Thiazolidinediones are used in combination with sulphonylureas or metformin in Type II diabetes mellitus.
- Alpha-glucosidase inhibitors are used in obese type II diabetes mellitus patients.
- Both the newer drugs i.e. GLP-1 receptor agonist and DPP-4 inhibitors are used in Type II diabetes mellitus patients.
Question 24. Write Short Note On Antidiabetic Drugs.
Answer:
Diabetes mellitus is a chronic metabolic disorder that is characterized by hyperglycemia and altered metabolism of carbohydrates.
Diabetes mellitus is divided into two types, i.e. Type I insulin-dependent diabetes mellitus and Type II non-insulin diabetes mellitus.
Insulin is the antidiabetic drug used in the treatment of Type I diabetes mellitus and oral antidiabetic drugs or oral hypoglycemic drugs are used in the treatment of Type II diabetes mellitus.
Antidiabetic Drugs Rapidly Acting Insulin Preparations
- It consists of insulin lispro, insulin aspart, insulin glulisine
- These insulins are in the form of clear solutions
- This insulin forms fewer hexamers.
- On giving subcutaneously they immediately dissociate in monomers and rapidly get absorbed.
- They get mixed with all types of insulin solutions.
- These insulin preparations are taken just before meals.
- They lower the risk of late postprandial hypoglycemia.
Antidiabetic Drugs Short Acting Insulin
- These insulin preparations are short-acting and soluble.
- This insulin forms hexamers.
- On giving subcutaneously they are slowly absorbed.
- Their onset of actions occurs within 30 min and is administered 30 to 45 min before meals.
- They can be given IM and IV also.
- Regular insulin is a clear solution and can be mixed with all types of insulin preparations.
Intermediate Acting Insulin
- These insulins are complexed with protamine and zinc.
- On giving subcutaneously they dissociate slowly
- Their onset of action is delayed and the duration of action is 10 to 20 hours.
- Their solution is cloudy.
- They should be given once or twice daily subcutaneously.
Antidiabetic Drugs Long-Acting Insulin
- These insulins should be given subcutaneously.
- They have a prolonged duration of action.
- They cannot be mixed with any other human insulin due to their acidic Ph.
- They should be avoided in pregnant patients.
- Glargine has a lower risk of nocturnal hypoglycemia and provides better-fasting blood glucose levels as compared to NPH insulin.
Antidiabetic Drugs Insulin Detemir
- On giving subcutaneously it binds to albumin in the blood, and they have prolonged duration of action.
- They have minimal peak levels.
- It is given twice a day.
Antidiabetic Drugs Insulin Preparations Based On Its Source
- Bovine insulin or Beef insulin: It differs from human insulin by three amino acid residues and is more antigenic to men.
- Porcine insulin or pig insulin: It differs from human insulin by one amino acid residue and is less immunogenic.
Both bovine and porcine insulin are antigenic so they are not used. - Human insulin: It is prepared by enzymatic modification of porcine insulin or DNA recombinant technology. This insulin is the least immunogenic. In this resistance to insulin and lipodystrophy at the site of injection is
Oral antidiabetic drugs lower blood glucose levels on oral administration.
Classification Of Antidiabetic Or Hypoglycemic Drugs
1. Enhance insulin secretion
- Sulfonylureas (KATP channel blockers)
- Ist Generation: Tolbutamide and chlorpropamide
- IInd Generation: Glibenclamide, glipizide, gliclazide and glimepiride
- Meglitinide/phenylalanine analogs: Repaglinide, Nateglinide
- Glucagon-like peptide-1 (GLP-1) receptor agonists: Exenatide, Liraglutide
- Dipeptidyl peptidase-4 (DPP- 4): Sitagliptin, Saxagliptin, Vildagliptin, Alogliptin, Linagliptin
2. Drugs overcoming insulin resistance
- Biguanides (AMPk activator): Phenformin, Metformin
- Thiazolidinediones (PPARγ activator): Rosiglitazone, Pioglitazone.
3. Miscellaneous antidiabetic drugs
- α-Glucosidase Inhibitor: Acarbose, Miglitol, Voglibose
- Amylin analog: Pramlintide
- Dopamine – D2 receptor agonist: Bromocriptine
- Sodium-glucose cotransport-2 (SGLT-2) inhibitor: Dapagliflzine.
Mechanism Of Action Sulphonylureas
Biguanides
- They suppress gluconeogenesis in the liver.
- They promote peripheral utilization of glucose.
- They inhibit intestinal absorption of glucose, amino acid, and vitamin B12.
Meglitinides
These drugs stimulate insulin release by closing ATP-sensitive potassium channels in β cells of islet of L Langerhans leading to depolarization and causing the release of insulin.
Thiazolidinediones
These drugs bind to nuclear peroxisome proliferator-activated receptor – γ which causes activation of insulin-responsive genes and sensitizes peripheral tissues to insulin which decreases blood glucose by:
- Increasing transport of glucose in muscle and adipose tissue
- By inhibiting liver gluconeogenesis
- By promoting lipogenesis.
α Glucosidase Inhibitors
These drugs lead to the reduction of intestinal absorption of carbohydrates by inhibiting enzyme α glucosidase and decreasing postprandial hyperglycemia.
Newer Drugs
- GLP-1 receptor agonist: It suppresses the release of glucagon and stimulates insulin secretion.
- DPP-4 inhibitor: It inhibits enzyme DPP-4 decreases the release of glucagon and increases insulin secretion.
Uses Of Oral Antidiabetic Drugs
- Sulfonylureas are used in the treatment of maturity-onset diabetes, insulin-resistant diabetes, and diabetes insipidus.
- Biguanides are used in obese mild diabetics, non-diabetic obese patients, and patients allergic to sulfonylureas.
- Meglitinides are used in type II diabetes mellitus for controlling postprandial hyperglycemia.
- Thiazolidinediones are used in combination with sulphonylureas or metformin in Type II diabetes mellitus.
- Alpha-glucosidase inhibitors are used in Obese type II diabetes mellitus patients
- Both the newer drugs, i.e. GLP-1 receptor agonist and DPP-4 inhibitors are used in Type II diabetes mellitus patients.
Question 25. Write Short Note On Newer Insulins.
Answer:
Novel long and short-acting insulin analogs, the so-called ‘designer insulins’, developed through genetic engineering in the 1990s, paved the way for more physiological insulin therapy.
- They were theoretically less problematic in terms of hypoglycemia and patient satisfaction.
- They made the treatment flexible, safer, and simpler. Newer insulins are faster-acting preprandial insulin or longer-acting basal insulin which provide a constant concentration with no peak increase in insulin level.
- Newer analogs exist as monomers and are absorbed much faster (insulin aspart or lispro)or absorbed very slowly (insulin glargine or detemir).
- The newer analogs have increased stability, less variability, and selective action which will help in developing individualized treatments suitable to specific patient characteristics and will improve glycemic control.
- Following are the newer insulins:
- Rapidly acting: Insulin lispro, insulin aspart, insulin glulisine
- Short-acting: Regular soluble insulin
- Intermediate-acting: NPH
- Long-acting: Insulin glargine, insulin detemir.
Rapidly Acting Insulin Preparations
- It consists of insulin lispro, insulin aspart, insulin glulisine
- These insulins are in the form of clear solutions
- This insulin forms fewer hexamers.
- On giving subcutaneously they immediately dissociate in monomers and rapidly get absorbed.
- They get mixed with all types of insulin solutions.
- These insulin preparations are taken just before meals.
- They lower the risk of late postprandial hypoglycemia.
Short Acting Insulin
- These insulin preparations are short-acting and soluble.
- This insulin forms hexamers.
- On giving subcutaneously they are slowly absorbed.
- Their onset of actions occurs within 30 min and is administered 30 to 45 min before meals.
- They can be given IM and IV also.
- Regular insulin is a clear solution and can be mixed with all types of insulin preparations.
Intermediate Acting Insulin
- These insulins are complexed with protamine and zinc.
- On giving subcutaneously they dissociate slowly
- Their onset of action is delayed and the duration of action is 10 to 20 hours.
- Their solution is cloudy.
- They should be given once or twice daily subcutaneously.
Long-Acting Insulin
- These insulins should be given subcutaneously.
- They have a prolonged duration of action.
- They cannot be mixed with any other human insulin due to their acidic Ph.
- They should be avoided in pregnant patients.
- Glargine has a lower risk of nocturnal hypoglycemia and provides better-fasting blood glucose levels as compared to NPH insulin.
Insulin Detemir
- On giving subcutaneously it binds to albumin in the blood, and they have prolonged duration of action.
- They have minimal peak levels.
- It is given twice a day.
Insulin Preparations Based On Its Source
- Bovine insulin or Beef insulin: It differs from human insulin by three amino acid residues and is more antigenic to men.
- Porcine insulin or pig insulin: It differs from human insulin by one amino acid residue and is less immunogenic.
Both bovine and porcine insulin are antigenic so they are not used. - Human insulin: It is prepared by enzymatic modification of porcine insulin or DNA recombinant technology. This insulin is the least immunogenic. In this resistance to insulin and lipodystrophy at the site of injection is
Question 26. Write the Difference Between Sulphonylureas And Biguanides.
Answer:
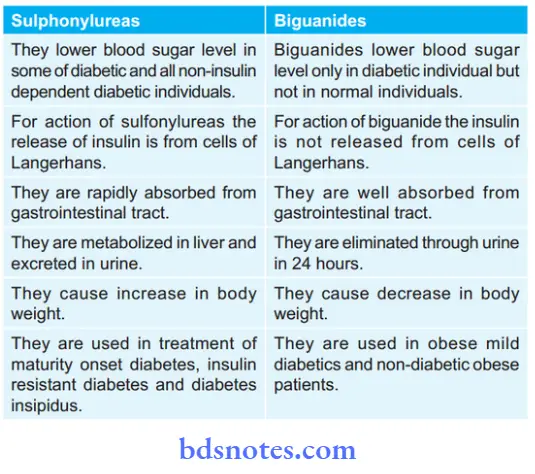
Following are the differences between sulphonylureas and biguanides:
Question 27. Classify Sulphonylureas. Describe Briefly Their Mechanism Of Action.
Answer:
Classification Of Sulphonylureas
- Ist generation: Tolbutamide and Chlorpropamide.
- IInd generation: Glibenclamide, glipimide, glicazide and glimepiride.
Mechanism Of Action
- Sulfonylureas also increase the sensitivity of peripheral tissues to insulin by increasing the number of insulin receptors.
- Sulfonylureas decreases the release of glucagon.
Question 28. Write Short Answer On Drugs For Treatment Of Type Ii Diabetes Mellitus.
Answer:
Oral antidiabetic drugs or oral hypoglycemic drugs are used in the treatment of type II diabetes mellitus.
0

Leave a Reply