Describe the mechanism of Coagulation. Write hemophilia under the following headings:
- Blood Coagulation Definition
- Blood Coagulation Clinical features
- Blood Coagulation Treatment
Answer. Coagulation is the spontaneous arrest of the bleeding.
Following are the factors which are involved in the mechanism of coagulation of blood:
Factor I—Fibrinogen
Factor II—Prothrombin
Factor III—Thromboplastin (Tissue factor)
Factor IV—Calcium ions
Factor V—Labile factor
Factor VI—Presence not approved
Factor VII—Stable factor
Factor VIII—Anti-hemophilic factor
Factor IX—Christmas factor
Factor X—Stuart-Prower factor
Factor XI—Plasma thromboplastin antecedent
Factor XII—Hegman factor
Factor XIII—Fibrin-stabilizing factor
Factor XIV—Prekallikrein
Factor XV—Kallikrein
Factor XVI—Platelet factor
Read And Learn More: General Medicine Question And Answers
Coagulation occurs in three stages
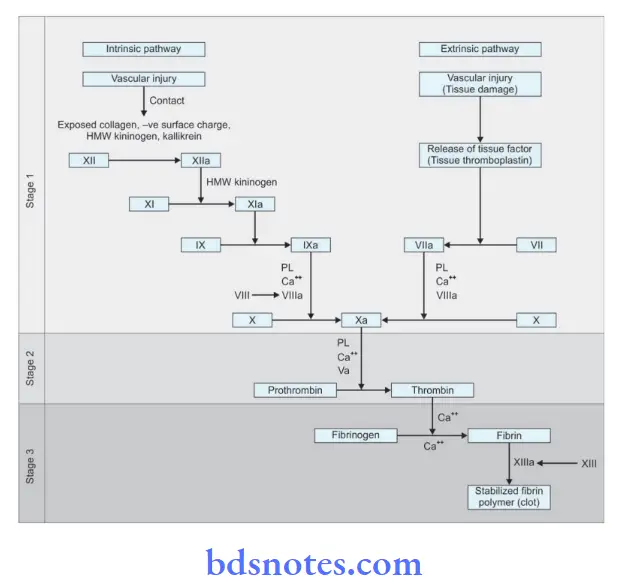
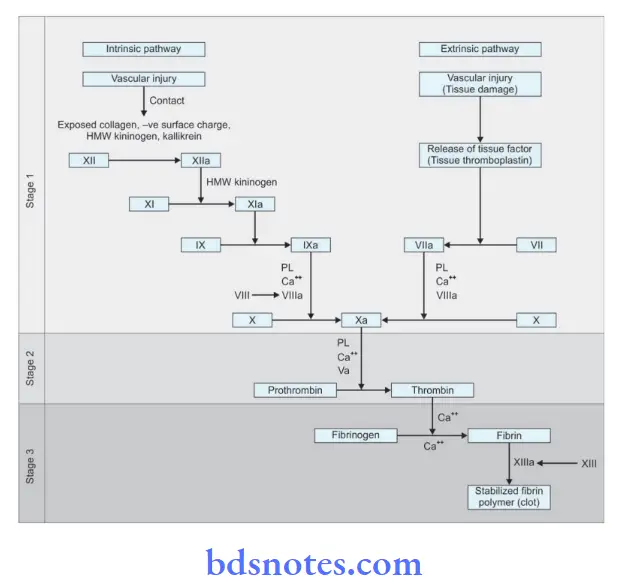
Mechanism of coagulation Blood coagulation occurs in three major stages:
- Stage 1: Activation of StuartPrower factor (formation of prothrombin activator)
- Stage 2: Formation of thrombin from prothrombin
- Stage 3: Formation of firing from fibrinogen
Coagulation Pathway – Activation Of Stuart-Prower Factor (Factor X)
- Activation of StuartPrower factor or factor X is the key to blood coagulation. Factor X is called a prothrombin activator as it activates prothrombin to form thrombin. Therefore, this process is also called prothrombin activation.
- This is achieved by two pathways: the intrinsic pathway and the extrinsic pathway.
Coagulation Intrinsic Pathway The intrinsic mechanism of prothrombin activation occurs in four steps:
Hemophilia Diagnosis
Step 1 (activation of factor XII) Activation of intrinsic pathway starts with contact of Hageman factor with a negatively charged surface or exposed collagen of the injured vessel wall.
- High molecular weight kininogen and kallikrein act as cofactors to facilitate the activation of factor XII
- Exposed collagen stimulates platelet adhesion and aggregation before initiating blood coagulation.
step 2 (activation of factor XI) Activated factor XII (XIIa) converts factor XI to its active form (XIa). This step is accelerated in the presence of high molecular weight kininogen.
step 3 (activation of factor IX ) Factor XIa then converts factor IX to IXa, which is accentuated by factor VIIa. Calcium accelerates this process.
step 4 (activation of factor X)
Coagulation Pathway
- The final step in the activation of the prothrombin activator is the activation of factor X. Factor IXa causes the activation of factor X to Xa, the activated Stuart power factor.
- The membrane phospholipid, calcium and activated factor VIII act as cofactors for the activation of the Stuart power factor is crucial in Stage 1.
- Formation of factor via is the key to the process of activation of factor X
Coagulation Extrinsic Pathway Extrinsic pathway of blood coagulation occurs in three steps:
Step 1 (release of tissue thromboplastin)
- Key to the clotting mechanism is the release of tissue thromboplastin from the injured tissue.
- As tissue thromboplastin is the tissue factor that is viewed as extrinsic to circulating blood, this system of blood coagulation is called an extrinsic system of clotting.
step 2 (activation of VII)
- Tissue thromboplastin converts factor VII to its active form (VIIa).
- This is the key step in the extrinsic mechanism.
- Factor VIIa directly activates not only factor X but also factor IX.
- Thus it also influences the intrinsic mechanism of activation of factor X.
Step 3 (activation of X) Factor VIIa converts X to Xa. This process is accelerated in the presence of calcium, platelet phospholipid, and tissue thromboplastin.
Formation of thrombin from Prothrombin
- This is the second stage of blood coagulation in which activated
- StuartPrower factor (Xa) converts prothrombin to thrombin, in the presence of platelet phospholipid, calcium, and activated factor V (Va).
- Factor Va acts as a cofactor for the acceleration of this process. Therefore, it is also called proaccelerin or accelerator globulin.
Formation of Fibrin from Fibrinogen This is the first stage of blood coagulation in which thrombin acts as an enzyme to convert firinogen to firin.
In this process, first, the fibrin monomers are formed and afterward, they are polymerized into a firing thread (blood clot).
This occurs in three steps:
- Proteolysis of soluble fibrinogen
- Polymerization of fibrin monomers
- Stabilization of firing polymer
Proteolysis of soluble Fibrinogen Fibrinogen has three domains: two peripheral (D) domains and one central (E) domain.
- Thrombin binds with the central domain and proteolytically releases two fibrinopeptides A and B from amino terminals of Aα and Bβ chains of each fibrinogen molecule.
- The release of firinopeptides leads to the formation of firin monomers.
Mechanism of firing stabilization
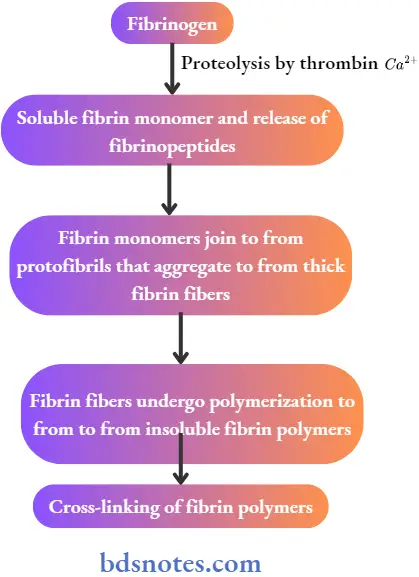
Polymerization of Fibrin Monomers Fibrin monomers join to form protofirils.
- About 15 to 20 protofibrils aggregate to form thick fibers of firing.
- Protofirils also branch out to form a meshwork of interconnected thick fibrin fibers. This is called the polymerization of fibrin monomers.
- Thrombin initiates the process of polymerization and simultaneously activates factor XIII.
- Factor XIIIa completes the process of polymerization.
Stabilization Of Fibrin Polymer Fibrin stabilizing factor (XIIIa) stabilizes the fibrin polymers by cross-linking them.
- Factor XIII is converted to XIIIa by thrombin.
- Calcium acts as a cofactor for this conversion.
- Covalent cross-linking of fibrin polymers provides adequate strength to the firing thread and to the fibrin meshwork.
- The stabilized firing meshwork is the blood clot.
- Red cells and platelets are trapped inside the fibrin meshwork to give the volume to the clot.
Definition of Hemophilia
Hemophilia is an inherited disorder that affects males and is transmitted by females. It is an X-linked recessive disorder caused by a deficiency of factor VIII.
It is a hereditary disorder of blood coagulation characterized by excessive hemorrhage due to increased coagulation time. It is of two types, i.e. hemophilia A and hemophilia B.
Hemophilia Clinical Features
- At birth: A Newborn with hemophilia is usually healthy, though bleeding from the cord and cephalohematoma may occur.
- In infants: Hemophilia is asymptomatic till 6 to 12 months when bruising becomes more obvious. Bleeding from the mouth is common.
- During childhood: In severely affected individuals, spontaneous bleeding may occur in joints and muscles, including the psoas muscle.
- In adults: The frequency of spontaneous bleeding decreases, but joints may already have been damaged. Intracranial hemorrhage is a lifethreatening complication. Spontaneous bleeds are common in mildly affcted individuals, but after injury bleeding occurs till appropriate therapy has begun.
Hemophilia Treatment
- It is done by fresh blood transfusion when bleeding is in a large mass.
- Factor VIII concentrate is employed in case of hemophilia A and factor IX concentrate is employed in case of hemophilia B.
- A hemophilic will require treatment before any dental procedure. Such a patient is managed by IV infusion cryoprecipitate or factor VIII combined with aminocaproic acid 4 to 6 g QDS.
- For any major surgery, periodontal surgery or extraction of a tooth hemophilic patient should be hospitalized.
- Infusion of factor VIII concentrate is given before surgery and is continued for 48 to 72 hours. Antibiotics should also be given to the patient.
Clinical Features, Pathogenesis, And Treatment Of Hemophilia
Coagulation is the spontaneous arrest of the bleeding. Following are the factors which are involved in the mechanism of coagulation of blood:
Factor I—Fibrinogen
Factor II—Prothrombin
Factor III—Thromboplastin (Tissue factor)
Factor IV—Calcium ions
Factor V—Labile factor
Factor VI—Presence not approved
Factor VII—Stable factor
Factor VIII—Anti-hemophilic factor
Factor IX—Christmas factor
Factor X—Stuart-Prower factor
Factor XI—Plasma thromboplastin antecedent
Factor XII—Hegman factor
Factor XIII—Fibrin-stabilizing factor
Factor XIV—Prekallikrein
Factor XV—Kallikrein
Factor XVI—Platelet factor
coagulation occurs in three stages
Hemophilia Management
- Local anesthesia is contraindicated. So intrapulpal anesthesia, and intraligamentary anesthesia should be used.
- Sedation with diazepam or NO2O2 sedation can be given.
- Endodontic procedures should be carried out and care should be taken not to do instrumentation beyond the apex. If hemorrhage is present, it should be controlled by 1:1000 aqueous epinephrine on paper point.
- Restorative treatments can be carried out by proper application of rubber dam to avoid trauma to the gingiva and other soft tissues.
- In case if rubber dam is not present an epinephrine-impregnated hemostatic cord is kept in the gingival sulcus before preparation of crown or inlay margin.
Hemophilia Diagnosis
- Complete dentures and removable partial dentures can be given to hemophilic patients and are well tolerated by them. The patient has to take care of proper maintenance of the hygiene of the prosthesis.
- Conservative periodontal treatment should be done rather than attempting periodontal surgeries.
- In case, oral surgical procedures are to be done local hemostatic agents should be used, pressure surgical packs should be employed, and sutures and topical thrombin should be used.
- After removal of the tooth, the socket is packed with a mechanical splint. Post-operative use of anti-fibrinolytic agents is used to support clot maintenance.
- In cases of Hemophilia A Human freezedried factor VIII concentrate or new recombinant factor VIII is used.
- In hemophilia B human dried factor IX concentrate is supplied as power which is to be mixed with distilled water and administered IV.

Leave a Reply