Head Injuries
Head injuries derive their importance because of the fact that many patients who die or who are disabled belong to the younger age groups. Head injuries account for 1% of all deaths, one-fourth of deaths due to trauma and they are responsible for half of all deaths from road traffic accidents. The majority of the patients are young, adult males.
Read And Learn More: Clinical Medicine And Surgery Notes
Head Injuries Classification
- Based on the clinical type
- Open
- Closed
- Based on the type of injury
- Blunt injury—acceleration, deceleration
- Missile injuries
- The term open head injury is used to denote a type of injury in which there is a fracture of the skull associated with a tear of the dura and arachnoid, resulting in cerebrospinal fluid leak either to the external environment or into one of the potentially infective areas in the base of the skull, e.g. CSF rhinorrhoea or otorrhoea.
- A closed head injury is one where there is no such leakage. The advantage of this classification is that it helps the treating physician to recognise a group of patients who are likely to develop an infective complication following the head injury and he can initiate measures to prevent it.
- Blunt injuries depending on the severity of impact can result in an open or closed head injury. Missile injuries tend to result in an open head injury most often. The brain is protected by a bony box which has a vault and base of the skull. The base of the skull in contrast to the vault is a rough terrain due to the various bony prominences, ridges and forantinae.
- This factor is important in causing extensive brain damage to the brain in acceleration/deceleration type of injuries. In addition to linear acceleration/deceleration, rotational acceleration is also capable of producing damage to the brain as the brain swirls about inside the skull, Such injuries result in maximal damage at interfaces between structures of different densities such as grey matter—white matter junctions.
Head Injuries Pathology
- The pathological changes due to trauma to the brain can be classified into primary and secondary
Primary lesions
- Diffuse neuronal damage
- Shearing lesions
- Contusions and lacerations
Secondary lesions
- Swelling
- Haemorrhage
- Extradural
- Subdural
- Intracerebral
- Infection
Primary Lesions
- Diffuse neuronal damage is the most constant feature of blunt injuries. Immediately after an injury, no changes may be seen.
- But changes begin after 14 hours of injury and maximum effects may last upto one week.
- Prolonged unconsciousness may follow injuries which produce only diffuse neuronal damage without any obvious macroscopic changes.
- Shearing lesions of the nerve fibres account for some severe injuries without any conspicuous changes to the naked eye examination of the brain (cerebral concussion).
- Wide-spread degeneration of white matter occurs without much changes in the paralysis of the nervous system cortex or brainstem. These patients have spasticity in all 4 limbs after injury and when they regain consciousness they are found to be severely demented.
- Contusion and lacerations are the obvious naked-eye changes seen after injuries and were thought to be the main injuries before diffuse neuronal damage and shearing lesions were described.
- Contusions are seen on the summit of the gyri which gets injured against the bone.
- The overlying pia is torn, and the blood seeps into the subarachnoid space. A bleeding conical vessel may result in the formation of an acute subdural haematoma or intracerebral haemorrhage.
- Brain oedema which develops surrounding the contusion and lacerations is the one that determines the outcome.
- Most often contusions are seen at the tips of the frontal and temporal lobes; under the surface of the frontal and temporal lobes; over the corpus callosum, superior and anterior surfaces of the cerebellum and the anterior surface of the brain stem.
Cerebral Concussion
- Temporary physiological paralysis of the nervous system
- Loss of consciousness
- Post-traumatic amnesia
- Recovery may be complete
- Some can develop complications
Primary Lesions
- Diffuse neuronal damage
- Cerebral contusion
- Cerebral laceration
Secondary Lesions Brain Swelling
- This is a vague term applied to an increase in brain bulk due to both oedema and venous congestion.
- It is aggravated by hypoxia or respiratory insufficiency which may be due to associated lung injury or obstruction to upper respiratory passages.
- Sometimes such a swelling can lead to severe brain compression which is difficult to relieve since there is no single mass lesion.
Intracranial Haemorrhage
Extradural or subdural haemorrhages may develop as a clean-cut secondary event, even though bleeding may have started at the time of injury. These cause compression of the brain, a secondary rise in intracranial pressure and can cause death if not detected and treated early.
Secondary Lesions
- Brain swelling
- Oedema
- Venous congestion
- Hypoxia
- Intracranial haemorrhage
- Extradural
- Subdural
- Infections
- Open head injury
- Generalised meningitis
- Subdural empyema
- Closed head injury
- Pott’s puffy tumour
- Open head injury
Secondary Lesions Infections
- All open head injuries are liable to result in intracranial infection either as generalised meningitis or focal infection such as subdural empyema or brain abscess, osteomyelitis of the skull.
- After closed head injuries, infection of a subpericranial blood clot may result in Pott’s puffy tumour.
- When infection supervenes an already injured brain, it may retard the recovery or may even lead to death. Hence, it becomes mandatory to treat all infections vigorously.
Cause Of Death In Head Injuries
- It is instructive to consider the pathological findings in fatal cases and to speculate the deaths which might have been prevented.
- For example, earlier, many deaths which had occurred due to aggravation of brain swelling due to hypoxia could have been prevented by ventilation and anti-oedema measures.
- It should be emphasised that the role of the treating physician is to anticipate and take appropriate measures to prevent the patient from succumbing to the secondary changes.
- In extensive primary damage to the brain, apart from supportive treatment, one may have to wait and hope.
- Extensive injury to vital areas like diencephalon, or patients with diffuse damage are not likely to survive. These are patients who are unconscious from the time of injury with bilateral, dilated, fixed pupils, flaccidity in all 4 limbs and autonomic disturbances.
- Sometimes a head injury associated with extensive injuries to the chest, abdomen or limbs by their sheer severity can cause death.
- Intracranial complications like haematomas, brain swelling, and infection and extracranial complications like chest injury/metabolic abnormalities if recognised and treated early can go a long way in saving the life of the patients.
Intracranial Haematoma
- Most of the head injuries are mild or minor and irrespective of treatment, the patient recovers on his own.
- All those who are unconscious, even if briefly, run the risk of respiratory obstruction.
- Some of the so-called trivially injured run the risk of developing an intracranial haematoma.
- Hence, all head injuries must be taken seriously. A complicated head injury is one where any of the secondary pathological changes may occur and threaten the life of the patient.
- An uncomplicated head injury is one where no such events occur. However, it could be a severe one where the unconsciousness is prolonged.
- These haematomas could develop in any one of the planes intracranially. Extradural (epidural), subdural, intracerebral haematoma, or a haemorrhagic contusion.
- The clinical presentation of these haematomas is due to either an increase in the intracranial pressure (or) due to signs of cerebral compression.
- In the case of acute subdural haematoma or intracerebral haematoma, the clinical picture and the outcome of treatment are also dependent on associated brain damage.
Extradural/Epidural Haematoma
- The clot collects between the dura and the inner table of the skull. A majority of them occur in the middle cranial fossa since injury to middle meningeal vessels (vein and artery) is the commonest cause.
- However, about 20–25% of the extradural haematomas can occur in the frontal, and parietal regions, at the vertex or in the posterior fossa.
- Injury to the dural venous sinuses or a large diploic venous channel are the other causes of the formation of a haematoma.
- Depending upon the source of bleeding the hematoma could collect rapidly (hyperacute type) or slowly over a period of a few hours to a few days and present as a chronic lesion.
- 60–80% of these patients have an associated fracture of the skull bone and only a few of them may present with classical symptoms with lucid interval. In the remaining patients, the initial picture can vary from an unconscious state to a fully conscious person with or without a history of post-traumatic amnesia.
- With the widespread availability and use of CT scans, the diagnosis has become much simpler nowadays. However, a few clinical features are worth mentioning.
1. Deteriorating Consciousness Level
- This is one of the hallmarks of the diagnosis of intracranial haematoma. The term lucid interval is used when a patient recovers from an initial period of unconscious state.
- Though in earlier days this was said to be associated with intracranial haematomas it can occur in other conditions like brain oedema, multiple constusions etc.
- To assess the consciousness level properly, instead of using vaguely defined terms like semiconscious, obtunded etc., the Glasgow coma score has been used widely, thereby avoiding observer errors in the observation of such patients.
- Restlessness in a previously quiet patient indicates increasing intracranial pressure, which again needs to be investigated or at the earliest appearance of focal neuronal deficit, a patient has to be taken up for exploratory boreholes.
- The progressive neurological deficit indicates cerebral compression and the manifestation may depend on the area of the brain affected.
2. Pupillary Abnormalities
- These are to be considered as late manifestations. It is due to pressure by the herniating temporal lobe on the ipsilateral third nerve at the tentorial hiatus.
- In the early stages due to irritation of the nerve, there is constriction.
- Due to the transient phenomenon, the early constriction often goes unnoticed and the patients are detected in the next stage of pupillary dilatation caused by paralysis of pupil-constrictor fibres in the third nerve. However, if the cerebral compression is unrelieved, this may go on to bilateral.
- Pupillary dilatation is due to ischaemia of the third nerve nucleus at the midbrain which is caused by pressure on the posterior cerebral artery. These series of pupillary changes due to paralysis of the third nerve have been termed Hutchinsonian pupils.
- The dilated pupil has a definite localising value that if at all an exploratory burr hole has been decided upon, it should be carried out on the side of the initially dilated pupil.
3. Autonomic Disturbances
- Bradycardia though said to be a definite sign, is a late and not an early sign.
- Initially, there may be a rise in the pulse rate (tachycardia) which may progress to bradycardia, when the systolic blood pressure increases. At times there may be a rise in the diastolic pressure also.
- These changes are brought about due to changes in cerebral blood flow as a consequence of increased intracranial pressure.
- Respirations become deep, with a slow rate (bradypnoea) and later patients may develop Cheyne-Stokes ventilation due to brainstem ischaemia.
- Local scalp swelling is seen in more than half of the cases. Thus, examination of the head for any such swelling becomes important.
- Some of these patients may have a stiff neck either due to increased intracranial pressure or due to associated injury to neck muscles.
- A mild fever may, at times, occur and this sometimes confuses the observer in which case the patients must be investigated with a definitive investigation like a CT scan or if not much time is available, one should not hesitate to proceed to exploratory burr holes or a trauma craniotomy flap has to be employed to rule out a haematoma.
- Though in adults, ‘SHOCK’ is a rare complication of head injury, in children with intracranial haematoma and associated cephalohaematomas, due to volume depletion ‘SHOCK’ may be encountered. Even in adults, if there is a large scalp injury which is not sutured immediately, shock can occur.
- Posterior fossa haematomas in any plane are dangerous because of the lesser space available for the haematomas as a result of which rapid brain stem compression can occur which may prove fatal.
- Though the availability of CT scans has made detection of these so-called unusual haematomas more frequent in a suspected case, even if facilities are not available, the treating physician should explore the posterior fossa, if the clinical features suggest haematoma, or if the skull X-rays show a fracture line extending across the occipital bone towards the foramen magnum.
Extradural/Epidural Haematoma Investigations
As has been pointed out earlier, the advent of a CT scan of the head has made the diagnosis easier and more specific, It should be emphasized that in the absence of a CT scan, if adequate clinical features point out to the possibility of an intracranial haematoma, the patient must be taken up immediately for an exploratory surgery rather than wait and allow him to develop irreversible brain stem damage.
Since 60–80% of patients with an intracranial haematoma have a skull bone fracture, immaterial consciousness level has to be observed for at least 24–48 hours.
Occasionally one may have to resort to old investigations like angiography not only to establish the haematoma but to rule out associated dural venous sinus injury, etc.
Treatment of Head Injuries in General
Resuscitation and Support
- Admission is indicated when
- Definite history of unconsciousness
- Fracture temporal bone
- A person who cannot be attended by the doctors immediately, i.e. no medical facilities nearby.

Indications For Skull Radiology
- Loss of consciousness
- Obvious depression on the skull
- Compound fracture
- Laceration or contusion of the scalp
- Focal neurological signs
2. Casualty reception
- Airway
- Mouth gag—to prevent the tongue from falling backwards.
- Endotracheal intubation with positive pressure ventilation. Hypoxia is an important cause of cerebral oedema which worsens the level of consciousness.
- General assessment of patient:
- To rule out abdominal injuries like splenic rupture.
- Haemot’horax—mayneedanintercostal tube.
- Long bone fractures.
- A general assessment of the degree of shock by pulse, BP monitoring and treatment.
- Neurological assessment by Glasgow–Coma Scale.
1. Eyes open
- Spontaneously 4
- To speech 3
- To pain 2
- None 1
2. Best verbal response
- Oriented 5
- Confused 4
- Inappropriate words 3
- Incomprehensible sounds 2
- None 1
3. Best motor response
- Obeys commands 6
- Localises the pain 5
- Withdrawal to pain 4
- Flexion to pain 3
- Extension to pain 2 (severe damage with an increase of ICP)
- None 1
The total score is 15; the minimum score is 3. Any patient who has a coma score of 7 or less than 7 is said to be in a coma.
2. Care of Unconscious
- Ryle’s tube aspiration or feeding
- Care of the eyes—padding
- Catheter for drainage of urine
- Change of position to avoid bed sores.
3. Surgical Treatment for Extradural Haematoma
- Immediate surgery for the removal of haematoma and relief of cerebral compression is a must.
- Extradural haematoma especially is a neurosurgical emergency and whether the patient lives or dies will depend upon the speed with which the compression is relieved.
- It is not an exaggeration to state that even if one has to do decompression with unsterile instruments, at the bedside it may be worth the effort.
- In every neurosurgeon’s career, at least once such an opportunity might have occurred and a live patient may justify the means employed.
- Once the consciousness is lost, pupil dilates, or decerebrate rigidity and periodic breathing develops it may be only a matter of few minutes that may be available to save the life of the patient and one should not wait and waste time.
- In the case of extradural haematoma, the outcome is dependent on the size of the haematoma and the stage at which the patient was taken up for surgery.
- In the case of acute subdural and intracerebral haematoma, it depends on associated brain damage.
- If the associated brain damage is very severe, patients succumb to the brain damage.
Miscellaneous Fracture Skull Anterior Fossa Fracture
- A fractured cribriform plate can result in CSF rhinorrhoea.
- Fracture may extend to the orbit—subconjunctival haemorrhage.
- Olfactory nerve involvement —partial anosmia.
- The optic nerve may be confused or fracture may involve the optic foramen
resulting in partial or total loss of vision. - Rarely 3rd nerve palsy gives rise to dilated pupil.
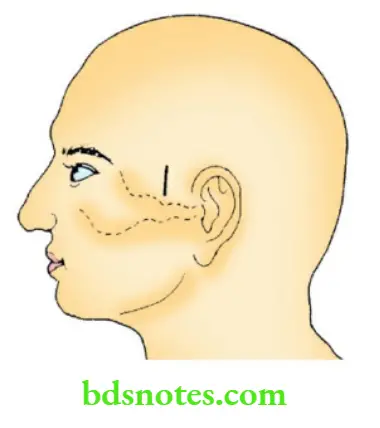
Extradural Haematoma
- 3 cm vertical incision immediately above the midpoint of zygoma
- Strip the pericranium
- Burr hole with Hudson’s brace
- Evacuate black-currant jelly clot
- Extend the burr-hole and control bleeding
- middle-meningeal artery by bipolar diathermy
- Dural hitch sutures to prevent stripping of dura
Middle Cranial Fossa Fracture
- Epistaxis due to fracture venous/sphenoid sinuses
- CSP from the ear: CSF with blood, hence does not clot
- 7th nerve palsy
- Rarely are 6th and 8th nerves also involved.
Posterior Cranial Fossa Fracture
- Extravasation of blood in the suboccipital region causes boggy swelling in
the nape of the neck - 9th, 10th, 11th cranial nerves may also be involved
- Battle’s sign: Discoloration of skin and collection of blood occur in the
region of the mastoid process.
Csf Rhinorrhoea
- There should be communication between the intradural cavity and the nose
(subarachnoid space). - It indicates a tear of the dura mainly in the basal region, and a fracture
involving paranasal sinuses —frontal, ethmoidal, and sphenoidal. - There is always an injury to a small portion of the brain. It (the portion of the brain) plugs the tear, preventing the dura from healing. Thus, the rhinorrhoea persists for many days.
- This leads to complications, i.e. infection and meningitis.
Csf Rhinorrhoea Treatment
- Prophylactic antibiotics.
- If the rhinorrhoea persists, repair of the dural defect alone (or) at times with a shunt procedure will be needed.
Pott’s Puffy Tumour
- This is a subperiosteal infection usually caused by osteomyelitis of the
underlying skull. - It is common in the frontal region and the frontal bone is commonly involved.
- The cause of infection is frontal sinusitis. Another common cause of infection of a subpericranial haematoma is following needle aspiration.
- It can also follow chronic suppurative otitis media.
- Pus collects in the subpericranial space and extradural plane, which
communicate with each other (dumb-bell type abscess). - It causes a boggy swelling in the frontal region and tenderness over the scalp.
- Pitting oedema over the scalp is conclusively called Pott’s puffy tumour.
- Severe headache, vomiting and blurring of vision should clinch the diagnosis.
Pott’s Puffy Tumour Treatment
- CT scan to confirm the diagnosis.
- A burr hole and aspiration of pus can be done followed by 6–8 weeks of antibiotics.
- In chronic cases, the wall of the abscess may have to be removed and the associated osteomyelitic skull bone requires a radical removal under cover of antibiotics which have to be given for 6–8 weeks period.
Chronic Subdural Haematoma
- Common in old people.
- Because of the shrinkage of the brain, the distance between the dura and the skull increases and due to minor trauma, cortical veins are torn resulting in a collection of blood.
- Bleeding is never progressive and the blood in the subdural space slowly compresses the brain causing features of raised ICT.
Chronic Subdural Haematoma Clinical Features
- Old aged patients
- History of minor trauma
- Bilateral headache
- Mental apathy
- Slowness
- Confusion—later alteration in the level of consciousness may progress to unconsciousness.
- Waxing and waning of the level of consciousness is seen in some patients; if such a history is elicited, one should always suspect chronic subdural haematoma.
Chronic Subdural Haematoma Diagnosis
CT scan or, if feasible, an MRI scan (cerebral angiography had been used and is still being used in some centres where access to the latest imaging facilities is not available) are the ideal investigations.
Chronic Subdural Haematoma Treatment
- Burr hole and drainage of the haematoma under local anaesthesia or under general anaesthesia occasionally is the often practised mode of treatment.
- At times, one may have to resort to two or more boreholes to ensure adequate evacuation.
- If the brain fails to expand and obliterate the cavity, especially in older people or persons with a very thick inner membrane, a large craniotomy and wide excision of the subdural membrane has to be carried out to remove the constricting effect.
- Adequate bed rest and plenty of fluid administration are also important postoperative measures.
Chronic Subdural Haematoma Outcome
Surgery offers good prospects for the treatment of benign brain tumours such as meningioma or pituitary adenoma, but the outcome of treatment of malignant tumours is still poor.

Leave a Reply