General Anesthetics
Question 1 Write A Short Note On Diethyl Ether.
Answer:
It is a highly volatile liquid and produces irritating vapors which are inflammable and explosive.
- Ether is an inhalational liquid.
- Ether is a potent anesthetic that produces good analgesia and marked muscle relaxation by reducing acetylcholine output from motor nerve endings.
- Ether is highly soluble in blood. Induction is prolonged and unpleasant with struggling, breadth holding, and marked respiratory secretions.
- Recovery is slow, and postanesthetic nausea, vomiting, and retching are marked.
- BP and respiration are generally well maintained because of reflux stimulation and high sympathetic tone. It does not sensitize the heart to adrenaline and is non-hepatoxic.
Read And Learn More: Pharmacology Question And Answers
Question 2. Discuss Ultrashort Anesthesia.
Answer:
Ultrashort anesthesia is anesthesia for a very short duration.
- Mainly short-acting baritones such as thiopentone sodium are used.
- Thiopentone sodium is an ultrashort-acting barbiturate.
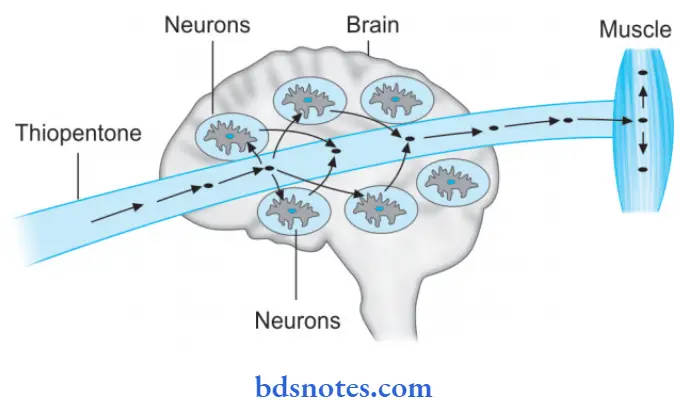
- During ultrashort anesthesia, thiopentone sodium is injected IV as 2.5% solution produces unconsciousness in 15 to 20 seconds.
- After a single IV dose, it rapidly enters highly perfused organs like the brain, liver, and heart and causes anesthesia. As the blood level of the drug falls rapidly, it diffuses out of the central nervous system in blood and then to the less perfused organs like skeletal muscle and adipose tissue. This redistribution causes the termination of drug action.
- Its undissociated form has high lipid solubility due to which it almost instantaneously enters the brain.
- Thiopentone is employed as the sole anesthetic for short operations which are not painful.
Question 3. Write Briefl On Halothane.
Or
Write A Short Note On Halothane.
Answer:
Halothane is a volatile, non-inflammable and non-irritant.
- Its induction and recovery are faster.
- It is a potent anesthetic.
- Halothane produces poor analgesia.
- Halothane causes a fall in BP, depression of myocardial contractility, and decreases heart rate. Respiratory depression is seen. It dilates bronchi and is preferred for asthmatics.
- Halothane sensitizes the myocardium to catecholamines and can precipitate arrhythmias.
- Halothane is expensive.
- It can cause hepatitis if it is repeatedly used.
- Halothane is non-pungent and is well tolerated. It is preferred for induction and maintenance in children.
- Adverse effects are hypotension, respiratory depression, hepatotoxicity, and arrhythmias.
- It is a potent anesthetic.
- It is not a good muscle relaxant or analgesic.
- Halothane causes a fall in BP, depression of myocardial contractility, and decreases heart rate. Respiratory depression is seen.
- It dilates bronchi and is preferred for asthmatics. Hepatitis can occur after repeated use. Recovery is smooth and quick.
Question 4. Write A Short Note On Ketamine.
Answer:
Ketamine is a general anesthetic that is given intravenously and is slowly acting drug.
- It causes dissociative anesthesia characterized by catatonia, amnesia, and analgesia without actual loss of consciousness.
- Ketamine acts by blocking N – methyl – D – aspartate type of glutamate receptors.
- It is the only anesthetic that produces cardiovascular stimulation as it causes sympathetic stimulation.
- It leads to bronchodilatation and is used in asthmatics.
- Ketamine mainly acts in cortical and subcortical areas.
Ketamine Pharmacokinetics
It is a highly lipid soluble drug that rapidly enters high perfusion organs, i.e. brain, liver, heart, etc. Later on, the drug redistributes to less perfused organs. Metabolism of the drug occurs in the liver and is excreted in urine and bile.
Ketamine Uses
- It is a useful anesthetic agent for poor-risk geriatric patients.
- It is used in patients with shock.
- In operations of head, neck, and face.
- In dressing for burn wounds.
- In asthmatics.
- In children.
Ketamine Adverse Effects
- It causes an ‘emergence phenomenon’ during recovery which is associated with disorientation, sensory and perceptual illusions, and vivid dreams.
- It increases the blood pressure and heart rate.
- It increases intracranial pressure.
- It increases intraocular pressure, so it is avoided in glaucoma.
Question 5. Define General Anesthesia. Enumerate Various General Anesthetic Agents. Describe The Advantages And Disadvantages Of Each General Anesthetic Agent.
or
Describe General Anesthetics Merits (Advantages) And Demerits (Disadvantages)
Answer:
General anesthesia is the process in which there is a reversible loss of all sensations and consciousness.
Enumeration Of Various Anesthetic Agents
- Inhalational:
- Gas: Nitric oxide, cyclopropane
- Liquids: Ether, halothane, isoflurane, desflurane, enflrane, savoflrane and methoxyflrane.
- Intravenous:
- Inducing agents: Thiopentone sodium, methohexitone, propofol, and etomidate
- Short-Acting Drugs:
- Benzodiazepines: Diazepam, lorazepam, midazolam.
- Dissociative anesthesia: Ketamine
- Opioid analgesia: Fentanyl.
Advantages Of Each General Anesthetic Agent
- General Anesthetic Agent Nitrous Oxide
- It is a good analgesic
- Postanesthetic nausea is absent
- It is non-toxic to the kidneys, liver, and brain
- It is cheap.
- General Anesthetic Agent Ether
- It is a good analgesic and produces marked muscle
- General Anesthetic Agent Relaxation.
- It maintains blood pressure and is nonhepatotoxic.
- It is cheap and can be given by open drop.
- It is safer in inexperienced hands.
- General Anesthetic Agent Halothane
- It is non-irritant and non-inflammable.
- Pharyngeal and laryngeal reflexes are abolished early and the cough is depressed which dilates the bronchi so it is used safely in asthmatics.
- Its action is rapid.
- It is used to promote deliberate hypotension.
- General Anesthetic Agent Isoflurane
- It is non-irritating and non-inflammable.
- It produces rapid induction and rapid recovery.
- It is safer in patients with myocardial ischemia.
- It does not provoke seizures and is used for nerve surgery.
- General Anesthetic Agent Desflurane
- Its induction and recovery are very fast.
- Patients can be discouraged a few hours after surgery.
- General Anesthetic Agent Thiopentone sodium
- It is used in short operations
- It has very rapid action
- It is used in rapid control of convulsions.
- General Anesthetic Agent Diazepam
- It has no postoperative nausea and vomiting.
- Involuntary movements are not stimulated.
- General Anesthetic Agent Ketamine
- It is good for hypovolemic patients.
- It should be used in angiographic, cardiac catheterization, and trauma surgery.
- It can be repeatedly used.
- It can be used in persons who do not want to lose consciousness during surgery.
- It is preferred in children and is suitable for burn dressing.
- General Anesthetic Agent Fentanyl
- It is good for burning dressing
- It does not cause postoperative pain.
- It is a good analgesic.
Disadvantages Of Each General Anesthetic Agent
- General Anesthetic Agent Nitrous Oxide
- It is a poor muscle relaxant
- It has low blood solubility.
- General Anesthetic Agent Ether
- Its induction is prolonged and unpleasant.
- Postanesthetic nausea, vomiting, and retching are marked.
- It has inflammable properties.
- General Anesthetic Agent Halothane
- It is not a good analgesic and is potent muscle relaxant.
- It produces Tachyarrhythmias.
- It is used during labor, prolongs labor, and increases postpartum blood loss.
- On repeated use it causes hepatitis.
- General Anesthetic Agent Isoflurane
- It increases heart rate.
- Respiration depression is prominent.
- Secretions are increased.
- It is expensive.
- General Anesthetic Agent Desflurane
- It induces coughing and causes laryngospasms.
- General Anesthetic Agent Thiopentone Sodium
- It has poor analgesic action.
- It is weak muscle relaxant.
- Cardiovascular collapse may occur.
- Laryngospasm occurs when respiratory secretions or other irritants are present.
- General Anesthetic Agent Diazepam
- It produces sedation, amnesia, and consciousness.
- It is a poor analgesic
- It is not preferred in endoscopies or angiographies.
- General Anesthetic Agent Ketamine
- It is not preferred for hypertension and ischemic heart disease.
- Emergence delirium, hallucinations*and involuntary movements occur.
- General Anesthetic Agent Fentanyl
- Nausea, vomiting, and itching are present during recovery.
- Assistance is required while giving anesthesia
- It may increase the tone of chest muscles.
Question 6. Explain The Pharmacological Basis For, Oxygen Is Always Used With Nitrous Oxide.
Answer:
Oxygen is always used with nitrous oxide to prevent diffusion hypoxia.
- The nitrous oxide having low blood solubility rapidly diffuses into the alveoli and dilutes the alveolar air-partial pressure of oxygen in the alveoli.
- The resultant hypoxia is called diffusion hypoxia.
- It is not of much consequence if the cardiopulmonary reserve is normal, but may be dangerous if it is low.
- It can be prevented by continuing 100% oxygen inhalation for a few minutes after discontinuation of nitrous oxide.
Question 7. Write A Short Note On Spinal Anesthesia.
Answer:
The local anesthetic is injected in the subarachnoid space between L2-3 or L3-4, i.e. below the Lower end of the spinal cord.
- The primary site of action is the nerve root in the cauda equina rather than the spinal cord.
- The lower abdomen and hind limbs are anesthetized and paralyzed.
- The drug solution could be hyperbaric or isobaric with CSF.
- Nerve roots rapidly take up and retain the local anesthetic solution, therefore, its concentration in CSF falls quickly after injection.
- The level of anesthesia does not change with the change of posture after 10 min. Also, higher segments are exposed to progressively lower concentrations of LA.
- The duration of spinal anesthesia depends on the drug used and its concentration.
- The addition of 0.2-0.4 mg of adrenaline to the LA prolongs spinal anesthesia by about 1/3rd when measured by the time taken for the level of sensory block to recede to LA.
Spinal Anesthesia Uses
Spinal anesthesia is used for operations on the lower limbs, pelvis, lower abdomen, prostatectomy, fracture setting, obstetric procedures, cesarean section, etc.
Complications Of Spinal Anesthesia
- Respiratory paralysis is rare.
- Hypotension can occur due to the blockade of sympathetic vasoconstrictor outflow to blood vessels; venous pooling and decreased return to the heart contribute more to the fall in BP than arteriolar dilatation.
- Headache is due to seepage of CSF; can be minimized by using a smaller bore needle.
- Septic meningitis: Due to infection introduced during lumbar puncture; incidence is very low.
- Nausea and vomiting: After abdominal operations due to reflexes initiated by traction on abdominal viscera.
Question 8. Classify General Anesthetics. Describe The Actions And Adverse Effects Of Halothane.
Answer:
Classification Of General Anesthetics
- Inhalational:
- Gas: Nitric Oxide, cyclopropane
- Liquids: Ether, halothane, isoflurane, desflurane, enflrane, savoflrane and methoxyflrane.
- Intravenous:
- Inducing agents: Thiopentone sodium, methohexitone, propofol, and etomidate
- Short-acting drugs:
- Benzodiazepines: Diazepam, lorazepam, midazolam
- Dissociative anesthesia: Ketamine
- Opioid analgesia: Fentanyl.
Action Of Halothane
Halothane causes general anesthesia due to its actions on multiple ion channels, which ultimately depresses nerve conduction, breathing, and cardiac contractility.
Its immobilizing effects have been attributed to its binding to potassium channels in cholinergic neurons. Halothane’s effect is also likely due to binding to NMDA and calcium channels, causing hyperpolarization.
Adverse Effects Of Halothane
- Cardiac arrhythmias are very common during halothane anesthesia. Ventricular arrhythmias occur more frequently than with other volatile anesthetics.
- Hepatic necrosis, also known as “Halothane hepatitis” occurs rarely but fatalities have been reported.
- Severe hepatotoxicity occurs more frequently after repeated exposure to halothane.
- Eosinophilia has been reported in conjunction with halothane-induced hepatotoxicity.
- Malignant hyperpyrexia has occasionally been reported with halothane.
- Halothane has a depressant effect on the respiratory and cardiovascular systems and the following undesirable effects have been reported, i.e.
- Respiratory depression
- Hypotension
- Bradycardia
- Skeletal muscle relaxation
- Postoperative nausea, vomiting, and shivering.
Question 9. Give A Brief Account Of Preanesthetic Medication.
Or
Write Briefl On Preanesthetic Medication.
Or
Write Short Note On Preanesthetic Medication.
Answer:
Following are the aims and preanesthetic drugs fulfilling them which make anesthesia more pleasant and safe:
- For reducing anxiety and apprehension: Benzodiazepines such as diazepam, lorazepam, etc. are given due to their sedative, amnesic, calming, and anxiolytic effects along with the wide margin of safety.
- For preventing vagal bradycardia and to decrease salivary secretions caused by anesthetics: Antimuscarinic drugs, i.e. atropine or glycopyrrolate prevent vagal bradycardia and hypotension.
These drugs also cause the prevention of laryngospasm by decreasing respiratory secretions. Glycopyrrolate is given as it is potent and does not produce CNS side effects and causes less tachycardia. - To relieve pre and postoperative pain: Opioid analgesics such as morphine, pethidine or fentanyl relieve pain, but opioids have side effects such as respiratory depression, hypotension, nausea, vomiting, constipation, biliary spasm, and bronchospasm in asthmatics. Diclofenac can also be given.
- For antiemesis: Metoclopramide, domperidone, or ondansetron can be given to control vomiting. Metoclopramide leads to extrapyramidal symptoms and acute dystonias. Ondansetron is commonly used as it produces side effects very rarely.
- Prevention of acid secretion and stress ulcer: H2 blocker i.e. ranitidine or proton pump inhibitor, i.e. omeprazole decreases gastric acid secretion and
aspiration pneumonia before prolonged surgery. - For accelerating gastric emptying before emergency surgery: In such cases, metoclopramide or domperidone can be used.
These are the prokinetic drugs that increase the tone of the lower esophageal sphincter and accelerate gastric emptying, this also leads to the prevention of aspiration pneumonia.
Question 10. Explain The Pharmacological Basis Of The Use Of Atropine In Preanesthetic Medication.
Or
Explain Why Atropine Is Used As Preanesthetic Medication?
Answer:
Atropine has been used primarily to reduce salivary and bronchial secretions.
Their main aim of use is to prevent vagal bradycardia and hypotension and prophylaxis of laryngospasm which is precipitated by respiratory secretions.

Leave a Reply