Gangrenem Definition
Macroscopic death of tissue with superadded putrefaction. It affects the limbs (Figs 14.8 and 14.9), intestines, appendix, etc. In this chapter differential diagnosis of causes of gangrene of the limbs is considered.
Pregangrene
Rest pain, colour changes at rest and at exercises, oedema, hyperaesthesia, and skin ulcerations are due to inadequate blood supply to the limb. These changes are described as gangrenous changes in the limb.

Classification Of Gangrene
- Cardiovascular causes
- TAO
- Atherosclerotic gangrene
- Acute embolic gangrene
- Syphilitic gangrene
- Raynaud’s disease
- Cervical rib
- Vasculitis syndrome
- Polycythaemia
- Neurological causes
- Hemiplegia, paraplegia, bedsore.
- Traumatic gangrene
- Direct—thrombosis; indirect—crushing injuries
- Physical causes
- Sun rays, radiation, corrosive acids
- Drugs—Ergotamine
- Diabetic gangrene
- Acute infective gangrene
- Boil, carbuncle, cancrum oris, gas gangrene.
Read And Learn More: Clinical Medicine And Surgery Notes
Clinical Features Of Gangrene
- A part which is gangrenous is a dead portion of the body. It has no arterial pulsations, venous return or capillary filling.
- It has no sensation.
- The colour initially will be pale and later it changes to dusky grey and finally black. The black colour is due to the disintegration of haemoglobin and the formation of iron sulphide.

- The gangrenous part has to be treated by surgical excision or debridement, which may amount to either disarticulation of the toe or even an amputation.
- The gram-positive, gram-negative and anaerobic organisms multiply in this segment and can produce septicaemia. Thus, this may precipitate multi-organ failure such as renal failure, adult respiratory distress syndrome (ARDS), etc.
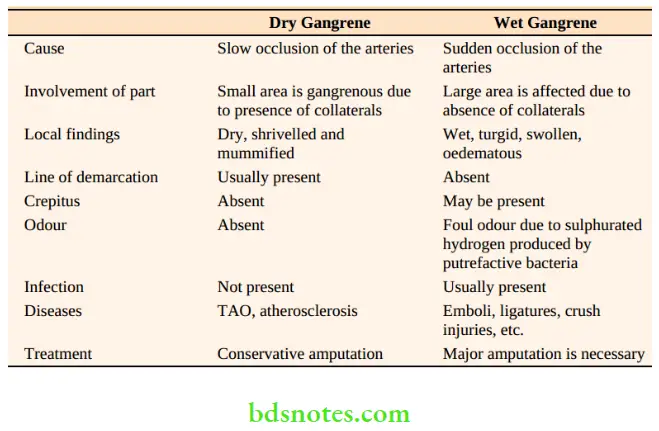
Clinical Features Of Gangrene Clinical types
Basically, there are two types.
- Dry gangrene
- Wet gangrene
Special Types of Gangrene
Cancrum oris
- It is an extensive ulcerative disease of cheek mucosa occurring in malnourished children.
- Precipitating factors are:
- Malnourishment
Signs Of Gangrene
- Loss of pulsation
- Loss of colour
- Loss of temperature
- Loss of sensation
- Loss of function
- Major diseases like diphtheria, whooping cough, typhoid, measles, kala azar, etc.

- As a result of these factors opportunistic organisms like Vincent’s organisms – Borrelia vincentii and fusiformis multiply and cause multiple ulcers, erosions, and later fibrosis.
- As the disease progresses sometimes the whole thickness of the cheek may be lost.
Treatment of cancrum oris
- Ryle’s tube-feeding
- Improve the nutrition
- Appropriate antibiotics: Metronidazole 400 mg three times a day for 7–10 days.
- Reconstructive surgery may be necessary later.
Complications of cancrum oris
- Fibrosis causes restriction of the movement of the jaw.
- Sept 3, toxaemia and death.
Acrocyanosis
- It is also called hereditary cold extremities
- Persistent cyanotic discolouration of hands when exposed to cold is a feature.
- This is brought about by intermittent spasms of small peripheral vessels — commonly affecting hands, rarely feet also.
- Generally, it is mild and nonprogressive.
Drug Abuse And Gangrene
- Abuse of drugs is an important cause of gangrene in the modern day.
- Inadvertent injection of drugs into an artery, results in thrombosis of the artery resulting in acute ischaemia —commonly in the femoral artery.
- Emergency treatment in symptomatic cases includes heparinisation, and infusion of dextran.
- In severe cases, emergency angiography and intra-arterial thrombolysis is considered.
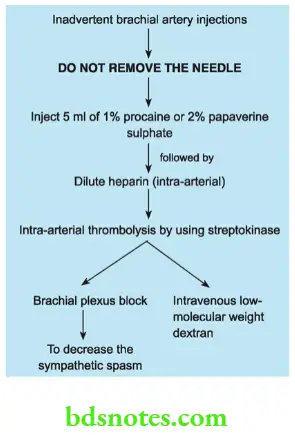
Iatrogenic Drug-induced Gangrene
- Inadvertent intra-arterial injection of thiopentone into one of the high divisions of the brachial artery (congenital anomaly), usually the ulnar, will result in severe burning and blanching of the hand.
- If this complication is noticed following steps (measures) have to be taken immediately.

Ergot And Gangrene
- Ergot preparations are used by patients with migraine over a long period.
- Ergotamine gangrene occurs in those who eat bread infected with claviceps purpurea.
Example: Dwellers on the shores of the Mediterranean Sea and the Russian Steppes.
Clinical Examination Case Of Upper Limb Ischemia Patient Data
1. Name age and sex: Younger patients may have cervical rib and vasculitis syndromes as possible causes. Middle-aged and young male smokers may be having TAO affecting the upper limb. Older patients may have embolic causes.
Presenting complaints
- Do you have any pain? Generally, pain is a serious complaint in the vast majority of cases. Some may complain of unbearable pain— typically a vascular in origin. Aching pain in the forearm also may be a presenting complaint.
- When did you notice these ulcers or black patches? The sudden development of colour changes including black patches suggests an embolic phenomenon. Some patients present with gangrenous patches of skin or subcutaneous tissue. Gangrene affects distal parts such as fingers and nail beds. To find out the possible source of emboli ask the following questions: Did you have chest pain? If present it could be related to valvular heart disease such as mitral stenosis or following a myocardial infarction a few months back.

- The patient may show similar gangrene patches in the feet or other limb which has developed slowly. In such cases, it is most likely due to TAO.
- If any ulcer is present find out the duration and how it is caused. It is usually precipitated by minor trauma and it occurs in the most distal part of the body such as the tip of the fingers. Ischaemic ulcers are deep and very painful.
- A history of coldness, numbness, paraesthesia and colour changes indicate chronic ischaemia. Excessive sweating is a vasomotor symptom.
- History of any swelling in the lower neck or any dull pain in the lower neck suggests cervical rib.
- Tingling and numbness, or paraesthesia in the distribution of C8, T1. Suggest features of ulnar nerve paralysis or weakness (lower nerve root involvement, mainly first thoracic nerve due to paralysis of interosseus muscles, wasting of hypothenar muscles. It includes sensory disturbances and motor disturbances (performing fine action—writing, buttoning, etc.).


Personal history
In men, a history of smoking should be asked for. Smokers have an increased incidence of arterial occlusive disorders.
Inspection
- Of hand, fingers and entire upper limb: Look for evidence of ulcer or gangrene. If present describe them. Look for evidence of muscle wasting, e.g. small muscle wasting— Loss of hypothenar muscle eminence may be due to ulnar nerve compression caused by a cervical rib. Look for evidence of chronic ischemia of the upper limb like ridging of nails, loss of pulp space, muscle wasting, etc
- Look for any prominent veins and oedema which may be caused by axillary vein thrombosis.
- In acute embolic gangrene, veins are empty.
- Mention muscle wasting/limb girth
- Look for any swelling in the neck which may be pulsatile, for example. cervical rib with pseudoaneurysm, etc.
Common Causes Of Weakness Of Small Muscles
- Cervical rib
- Carpal tunnel syndrome
- Cervical disc (central protrusion)
- Cervical spondylitis
- Chronic disease—Leprosy
Palpation
- For any loss of sensation, tenderness and muscle wasting.
- Palpate brachial artery and radial artery
- Tests for thoracic outlet syndrome.
- Neck: Bony mass or prominence caused by a cervical rib. It will be bony hard and fixed.
- If a pulsatile swelling is found, mention whether it is transmitted or expansile
- Any other mass — Lymph nodal mass.
Auscultation
Prominent subclavian artery pulsation is due to the cervical rib lifting the cervical rib. Bruit is due to post-stenotic dilatation.
Evidence of Nerve Weakness
Ulnar nerve involvement may suggest cervical rib as a cause of gangrene.
Examination of regional lymph nodes
Enlargement of axillary lymph nodes can be due to infection associated with gangrene.
Examination of peripheral vessels in all other limbs
- Upper limb involvement in addition to lower limb involvement is common in TAO patients (Buerger’s disease).
- Gross thickening of vessels in elderly patients may suggest atherosclerosis.

Leave a Reply