Diseases Of The Endocrine System
Question 1. Write a short note on acromegaly.
Answer. If the excess of growth hormone occurs after the fusion of epiphysis, then enlargement of acral parts, i.e. hands, fingers, feet, and toes occurs leading to an increase in their width rather than length.
Acromegaly Etiology
- In 95% of cases, it is a pituitary adenoma.
- Excessive secretion of growth hormone-releasing hormone from carcinoid tumors and adrenal tumors.
- Excessive growth hormonesecreting pancreatic islet cell tumors.
- As a part of multiple endocrine neoplasia type I.
Clinical Features Of Acromegaly
- General: Fatigue, weight gain, heat intolerance, increased sweating
- Skin changes: Thickening of skin. Skin is coarse and greasy, perspiration, hypertrichosis
- Soft tissues: Thickening of lips and nose, macroglossia, increase in heel pad, hypertrophy of muscular system in initial stages, mammary hyperplasia.
- Skeletal changes: Arthropathy of joints; Enlargement of hands, feet, supraorbital ridges, facial bones; prognathism is present; spacing apart of teeth; thick clavicles; Changes in the spine, i.e. Osteoporosis, Kyphosis, lordosis, and scoliosis; carpel-tunnel syndrome; prominent ridges and furrows on the skull; Large frontal and maxillary sinus
- Cardiovascular: Hypertension, cardiac failure or acromegalic cardiomyopathy, coronary artery disease, Arrythmias
- Respiratory: Deep voice due to enlargement of larynx, Lungs enlarge proportionately with thorax
- Ophthalmologic: Visual field defects are present such as bitemporal hemianopia or scotomas
- Metabolic: Impaired glucose tolerance is present.
- Malignancy: Prevalence of malignant disease, i.e. probability of colonic cancer increased.
Read And Learn More: General Medicine Question And Answers
Investigations Of Acromegaly
- Radiography:
- Xray Skull shows enlarged sella turcica, enlarged frontal sinus, increased thickness of the skull,macrognathia, and wide space teeth.
- There is arrowhead tufting of finger tips
- Heel pad sign: Heel pad > 23mm thick.
- CT scan: A large adenoma is easily seen on a CT scan taken after IV contrast.
- MRI: Sagittl’s view is useful in identifying the relationship between suprasellar and infrasellar structures.
- Biochemical diagnosis:
- Growth hormone levels are increased.
- Glucose tolerance test: It is the accepted diagnostic method for measuring glucose and growth hormone.
In healthy individuals growth hormone is undetectable during the test. - Insulin-like growth factor-I (IGF–I) levels: Growth hormone stimulates the production of IGF–I predominantly in the liver. IGFI levels assess disease activity in acromegalics, reflecting overall growth hormone secretion.
Management Of Acromegaly
- Surgical: Surgery is the treatment of choice. Surgical removal of tumors is done by trans-sphenoidal route followed by radiotherapy.
- Radiotherapy: It is advised when initial attempts at surgery do not reduce growth hormone levels to 5 MU/L.
Implantation of radioactive isotope. Yttium-90 causes a major reduction in growth hormone levels. - Medical therapy:
- Bromocriptine 20-30 mg/day orally in divided doses is given.
- Octreotide decreases the growth hormone levels.
Its dose is 100 µg TDS and can be increased up to 1500 µg/day.
Sandostatin: LAR is a sustained-release formulation of octreotide. It is given as 30 mg IM for 6 weeks which decreases growth hormone levels and also decreases pituitary tumor size. - Growth hormone receptor antagonist, i.e.
Pegvisomant is given S C at 40 mg/day followed by self-administration of 10mg/day. Liver function needs monitoring.
Question 2. Outline the management of thyrotoxicosis.
Answer. The management of thyrotoxicosis is divided into four parts as follows:
General Management Of Thyrotoxicosis:
- Allow the patient to take mental and physical rest.
- Maintain the nutrition of the patient by giving a nutritious diet.
- If the patient is anxious alprazolam 0.25 to 0.5 mg BD is given.
Drug Therapy Of Thyrotoxicosis:
- Anti-thyroid drugs such as carbimazole, i.e. 40 to 60 mg/day, methimazole, i.e. 100 to 150 mg 8 hourly, and propylthiouracil, i.e. 300 to 450 mg/ day can be given depending on the severity of the disease.
Drugs should be gradually decreased for 4 to 8 weeks based on FT4 levels. When FT4 levels are normal, carbimazole 5 to 15 mg/day or propylthiouracil 50 mg/day is given.
Drugs can be given for 1 to 2 years by regular checking of FT4 and TSH levels. - For symptomatic relief, betablockers such as propanolol 80–160 mg daily are given.
It is given for 2 to 3 weeks along with anti-thyroid treatment.
It relieves symptoms such as anxiety, tremors, and tachycardia. - Dexamethasone 8 mg/day may be used to inhibit the conversion of T4 to T3 in severe forms of thyrotoxicosis.
- Lithium carbonate 300–450 mg TDS inhibits thyroid hormone secretion temporarily in patients who are allergic to iodides and thioamides.
- Potassium perchlorate 500 mg BD inhibits iodine uptake by the thyroid gland. It is combined with thioamides.
- Surgery: Subtotal thyroidectomy is done in severely affcted cases.
- Before surgery patient should be made euthyroid by beta blockers and anti-thyroid drugs.
- Two weeks before the surgery drugs should be stopped and lugol iodine is given to reduce the vascularity.
- Radioiodine treatment: Radioactive iodine, i.e. 131I leads to the destruction of thyroid cells and is given with antithyroid drugs to prevent thyroid storm.
- Antithyroid drugs must be stopped for a minimum of 3 to 5 days before 131I to allow uptake of isotope 555 MBq to ablate the thyroid.
- High doses are needed for large goiter in severely thyrotoxic patients.
Question 3. Write a short note on Grave’s disease.
Answer. Grave’s disease is an autoimmune disease caused by the production of autoantibodies that stimulate thyroid-stimulating hormone receptors on the thyroid cell membrane resulting in excessive synthesis and secretion of thyroid hormone.
Risk Factors Of Grave’s Disease
- Genetic susceptibility: The role of hereditary factors is evidenced by increased incidence of other autoimmune disorders in members of patient’s families.
- Emotional stress
- Gender: Females are more prone than men (7 to 10:1) ratio.
- Pregnancy: iodinecontaining drugs
- Iodine and drugs: Amiodarone and iodinecontaining contrast media may precipitate Graves’ disease.
- Irradiation, e.g. radioactive iodine for multinodular goiter.
Symptoms Of Grave’s Disease
- Weight loss with increased appetite
- Heat intolerance and sweating
- Fatigue and weakness
- Hyperactivity, irritability, dysphoria, insomnia
- Dyspnea
- Oligomenorrhea, loss of libido
- Diarrhea/Defecation hyper defecation
- Polyuria
Signs Of Grave’s Disease
- Tremor, hyper-reflxia
- Tachycarclia, atrial firillation in elderly
- Warm moist skin
- Lid retraction, lid lag (causing a stare)
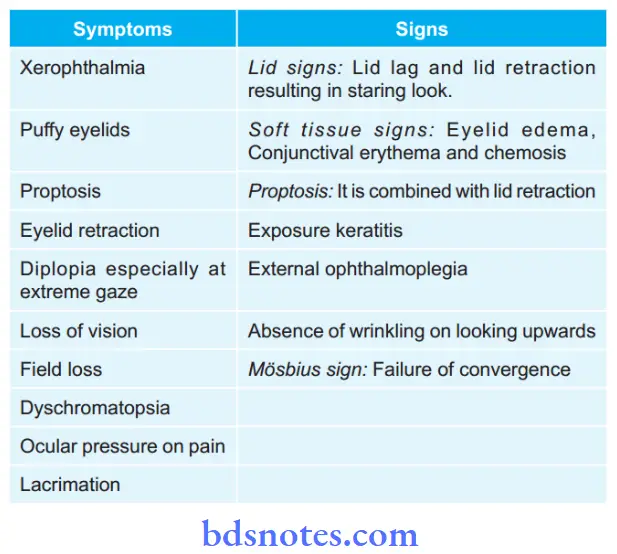
- Thyroid ophthalmopathy is a specific feature of Grave’s disease for which signs and symptoms are as follows:
Investigations Of Grave’s Disease
- T3 and T4 both are elevated.
- Low TSH or become undetectable
- 131I uptake is increased, i.e. greater than 35% at 5 hours
- Serum cholesterol is low
- ECG shows tachycardia, arrhythmias, STT changes
- Ultrasonography of the thyroid shows different goiter
Treatment For Discomfort
- Artificial tears should be given for the day, i.e. methylcellulose is given.
- Simple eye ointment should be given for the night
- Patients should use dark glasses with side frames.
- No smoking
Medical Therapy of Grave’s Disease
- Reduction of morning lid edema by sleeping on the bed with its head slightly raised.
- Prednisolone 60 mg daily is given.
- Anti-thyroid drugs such as carbimazole i.e. 40–60 mg/day, methimazole, i.e. 100–150 mg 8 hourly, and propylthiouracil, i.e. 300–450 mg/day can be given depending on the severity of the disease.
- Drugs should be gradually decreased for 4 to 8 weeks based on FT4 levels.
- When FT4 levels are normal carbimazole 5–15 mg/day or propylthiouracil 50mg/day is given.
- Drugs can be given for 1–2 years by regular checking of FT4 and TSH levels.
- For symptomatic relief beta-blockers such as propanolol 80–160 mg daily is given.
- It is given for 2–3 weeks along with anti thyroid treatment.
- It relieves symptoms such as anxiety, tremors, and tachycardia.
- Radioactive iodine, i.e. 131I leads to the destruction of thyroid cells and is given with antithyroid drugs.
Surgery Of Grave’s Disease
- Subtotal thyroidectomy is done in severely affcted cases.
- Before surgery patient should be made euthyroid by beta blockers and antithyroid drugs.
- Two weeks before the surgery drugs should be stopped and lugol iodine is given to reduce the vascularity.
Question 4. Write a short note on hyperthyroidism.
Answer. Hyperthyroidism is defined as increased secretion of thyroid hormone with an increase in levels of T3 and T4.
Etiology Of Hyperthyroidism
Common causes:
- Grave’s disease
- Toxic nodular goiter
- Multinodular
- Solitary nodule
Less common:
- Thyroiditis
- Druginduced
- Factitious
- Iodine excess
Rare:
- Pituitary or ectopic TSH
- Thyroid carcinoma
Clinical Features Of Hyperthyroidism
- Goiter is present, i.e. either diffuse or nodular.
- Gastrointestinal features: Vomiting, diarrhea, and weight loss
- Cardiovascular features: Arrhythmia, i.e. atrial fibrillation, dyspnea, wide pulse pressure
- Dermatological manifestations: Clubbing, loss of hair, palms becoming red, increased sweating
- Reproductive features: Amenorrhea, infertility, abortion, impotence
- Ophthalmological features: Exophthalmos, Diplopia, lid retraction, staring look, excessive watering from eyes
- Neuromuscular features: Tremors in hand, psychosis, irritability, restlessness, nervousness, high tendon reflexes
- Miscellaneous: Fatigue, polydipsia, heat tolerance
Investigations Of Hyperthyroidism
- Serum TSH level is decreased and is the initial diagnostic test. Normal TSH levels exclude clinical hyperthyroidism.
- Serum total and unbound (free) T3 and T4 are increased in hyperthyroidism.
- In some cases, only T3 levels are raised whereas T4 is normal (T3 toxicosis).
- TSHR antibody levels are increased in about 75% of cases.
ESR may be increased in subacute thyroiditis. - The uptake of radioactive iodine by the thyroid is increased in Graves’ disease and toxic nodular goiter, whereas it is low in subacute thyroiditis.
- Ultrasonography of the thyroid gland reveals diffuse enlargement of thyroid gland which helps in diffrentiating
- Graves’ disease from nodular goiter.
Drug Therapy for hyperthyroidism
- Anti-thyroid drugs such as carbimazole, i.e. 40–60 mg/day, methimazole, i.e. 100–150 mg 8 hourly, and propylthiouracil, i.e. 300–450 mg/day can be given depending on the severity of the disease.
Drugs should be gradually decreased for 4–8 weeks based on FT4 levels.
When FT4 levels are normal carbimazole 5–15 mg/day or propylthiouracil 50 mg/day is given.
Drugs can be given for 1–2 years by regular checking of FT4 and TSH levels. - For symptomatic relief betablockers such as propanolol 80–160 mg daily is given.
It is given for 2–3 weeks along with anti-thyroid treatment.
It relieves symptoms such as anxiety, tremors, and tachycardia. - Dexamethasone 8 mg/day may be used to inhibit the conversion of T4–T3 in severe forms of thyrotoxicosis.
- Lithium carbonate 300–450 mg TDS inhibits thyroid hormone secretion temporarily in patients who are allergic to iodides and thioamides.
- Potassium perchlorate 500 mg BD inhibits iodine uptake by the thyroid gland. It is combined with thioamides.
Surgery Of Hyperthyroidism
- Subtotal thyroidectomy is done in severely affcted cases. Before surgery, the patient should be made euthyroid by beta blockers and antithyroid drugs.
- Two weeks before the surgery drugs should be stopped and lugol iodine is given to reduce the vascularity.
Radioactive Iodine Of Hyperthyroidism
- Radioactive iodine, i.e. 131I leads to the destruction of thyroid cells and is given with antithyroid drugs to prevent thyroid storm.
- Antithyroid drugs must be stopped for a minimum of 3–5 days before 131I to allow uptake of isotope 555MBq to ablate the thyroid.
- High doses are needed for large goiters in severely thyrotoxic patients.
Question 5. Write a short note on myxedema.
Answer. Myxedema is a clinical condition resulting from decreased circulating levels of T3 and T4.
It is characterized by the deposition of mucinous material causing swelling of the skin and subcutaneous tissue.
Clinical Features Of Myxedema
- General: There is tiredness, somnolence, weight gain, cold intolerance, and goiter.
- Skin and subcutaneous tissue: Coarse dry skin, puffiness of face with malar flush, baggy eyelids with swollen edematous appearance of supraclavicular regions, neck, and lack of hand and feet.
- Cardiovascular and respiratory features: Bradycardia, angina, cardiac failure, pericardial effusion, and pleural effusion.
- Neuromuscular features: Aches and pains, cerebellar syndrome with slurred speech and ataxia, muscle cramps, and stiffness.
- Gastrointestinal features: Constipation and ascites
- Developmental: Growth and mental retardation
- Reproductive system: Infertility, menorrhagia, hyperprolactemia, and galactorrhea.
Investigation Of Myxedema
- Serum T3 and T4 are decreased.
- Serum TSH level is high
- Creatinine level increases
- Serum cholesterol level is increased
- BMR is low
- Iodine uptake by the thyroid is poor
- ECG can show bradycardia, low amplitude of QRS and
STT changes. - The blood picture shows macrocytic anemia.
- Xray chest can be normal or show cardiomegaly.
- Photomotogram reveals delayed ankle jerk.
Management Of Myxedema
- In patients with myxedema, adequate ventilation is maintained along with electrolyte balance and slow warming.
- The principle of therapy is the replacement of deficient thyroid hormones.
- Treatment of myxedema is the lifelong replacement of thyroid hormones by Lthyroxine.
- The initial starting dosage is 50–100 µg daily as a single dose on an empty stomach in the morning for the first 3 to 4 weeks.
- After some time, the dosage can be increased to 150 µg/day.
- Adjustment of the final dosage should be done after assessing
- TSH levels.
- The maximum dosage of L–thyroxine is 300 µg/day.
- In geriatric patients or patients suffering from ischemic heart disease, a low dose of L–thyroxine 25 µg/day can be started and is increased after assessing the levels of TSH.
- Since the plasma half-life of L–thyroxine is 7 days so increase and decrease in dose should be done at an interval of 2 weeks.
Question.6. Describe clinical manifestations and management of myxedema.
Or
Write a short note on the treatment of myxedema.
Answer.
Clinical Manifestations Of Myxedema
- Cold intolerance
- Thickness and dryness of skin and hair
- Swelling of hands and face
- Change in shape of face
- Thickening of lips is present
- Non-pitting edema is present
- There is a yellowish discoloration of the skin.
- Hoarseness of voice is present.
- There is a decrease or loss of sweating
- Loss of hair on the outer third of the eyebrows.
- Slow pulse/bradycardia.
Management Of Myxedema
- In patients with myxedema, adequate ventilation is maintained along with electrolyte balance and slow warming.
- The principle of therapy is the replacement of deficient thyroid hormones.
- Treatment of myxedema is the lifelong replacement of thyroid hormones by Lthyroxine.
- The initial starting dosage is 50–100 µg daily as a single dose on an empty stomach in the morning for the first 3 to 4 weeks.
After some time, the dosage can be increased to 150 µg/day. - Adjustment of final dosage should be done after assessing TSH levels.
- The maximum dosage of L–thyroxine is 300 µg/day.
- In geriatric patients or patients suffering from ischemic heart disease, a low dose of L–thyroxine 25 µg/day can be started and is increased after assessing the levels of TSH.
- Since the plasma half-life of L–thyroxine is 7 days so increase and decrease in dose should be done at an interval of 2 weeks.
Question 7. Describe the clinical and diagnostic features of myxedema.
Answer.
Clinical Features Of Myxedema
- General: There is tiredness, *somnolence, weight gain, cold intolerance, and goiter.
- Skin and subcutaneous tissue: Coarse dry skin, puffiness of the face with malar flush, baggy eyelids with swollen edematous appearance of supraclavicular regions, neck, and lack of hand and feet.
- Cardiovascular and respiratory features: Bradycardia, angina, cardiac failure, pericardial effusion, and pleural effusion.
- Neuromuscular features: Aches and pains, cerebellar syndrome with slurred speech and ataxia, muscle cramps, and stiffness.
- Gastrointestinal features: Constipation and ascites
- Developmental: Growth and mental retardation
- Reproductive system: Infertility, menorrhagia, hyperprolactemia, and galactorrhea.
Diagnosis is based on the Clinical signs of the patient and the investigations
Clinical Signs Of Myxedema
- Cold intolerance
- Thickness and dryness of skin and hair,
- Swelling of hands and face
- Change in shape of face
- Thickening of lips is present
- Non-pitting edema is present
- There is a yellowish discoloration of the skin.
- Hoarseness of voice is present.
- There is a decrease or loss of sweating
- Loss of hair on the outer third of the eyebrows.
- Slow pulse/bradycardia.
Investigations Of Myxedema
- Thyroid function test: There is a reduction in T3 and T4 levels and a rise in serum thyroidstimulating hormone which indicates primary hypothyroidism.
- Reduction in T3 and T4 levels with TSH levels below normal range is secondary hypothyroidism.
- Serum cholesterol: It is raised in primary thyroid failure. The fall in serum level is more than 50 mg/100 mL.
- Tendon reflex duration is prolonged.
- In ECG bradycardia, low voltage complexes and flattened or inverted Twaves are present.
Question 8. Write a short note on hypothyroidism.
Or
Write in brief on hypothyroidism.
Or
Write signs and symptoms of hypothyroidism.
Or
Write all clinical features of hypothyroidism.
Or
Write clinical features, diagnosis, and management of hypothyroidism.
Or
Discuss clinical features, complications, investigations, and treatment of hypothyroidism.
Answer. Hypothyroidism is defined as a clinical condition caused by a low level of circulating thyroid hormones.
Types Of Hypothyroidism
- Primary: When the cause lies in the thyroid
- Secondary: When hypothyroidism occurs due to disease of the anterior pituitary.
Symptoms Of Hypothyroidism
- Feeling of tiredness
- Weight gain
- Cold intolerance
- Hoarseness of voice and lethargy
- Somnolence
- Goiter
- Hyperlipidemia.
Signs Of Hypothyroidism
- Skin and subcutaneous tissues: Dry skin, puffiness of face with malar flush, baggy eyelids, alopecia, vitiligo
- Cardiovascular: Bradycardia, angina, heart failure
- Respiratory: Pericardial effusion, pleural effusion
- Psychiatric: Depression and psychosis
- Neuromuscular: Ache and pain, cerebellar ataxia, myalgia, delayed relaxation of reflexes, carpal tunnel syndrome
- Gastrointestinal: Constipation, ascites, ileus
- Hematological: Iron defiiency anemia, macrocytic anemia, pernicious anemia, normochromic normocytic anemia
- Reproductive: Infertility, impotence, menorrhagia
- Development: Growth retardation, mental retardation, and delayed puberty.
Investigations Of Hypothyroidism
- Serum T3 and T4 levels are low.
- Serum TSH level is high in primary hypothyroidism and low in secondary hypothyroidism.
- Serum cholesterol levels are high.
- ECG shows bradycardia, low amplitude of QRS, and STT changes.
- The blood picture shows macrocytic anemia.
- Xray chest can be normal or show cardiomegaly
Treatment Of Hypothyroidism
- Treatment of hypothyroidism is lifelong.
- Thyroid hormones are replaced by Lthyroxine
- The initial starting dosage is 50–100 µg daily empty stomach a single dose in the morning for the first 3 to 4 weeks.
Later dose is increased to 150 µg daily. - Final dose adjustment is done by TSH levels. TSH levels are maintained in the normal range by increasing the dosage.
- The maximum dose of L-thyroxine is 300 µg.
Complications Of Hypothyroidism Untreated hypothyroidism can lead to a number of health problems:
- Goiter: Constant stimulation of the thyroid to release more hormones may cause the gland to become larger — a condition known as goiter.
- Hashimoto’s thyroiditis is one of the most common causes of goiter.
- Although generally not uncomfortable, a large goiter can affect appearance and may interfere with swallowing or breathing.
- Heart problems: Hypothyroidism may also be associated with an increased risk of heart disease, primarily because high levels of lowdensity lipoprotein (LDL) cholesterol the “bad” cholesterol — can occur in people with an underactive thyroid.
- Even subclinical hypothyroidism, a mild or early form of hypothyroidism in which symptoms have not yet developed, can cause an increase in total cholesterol levels and impair the pumping ability of the heart.
- Hypothyroidism can also lead to an enlarged heart and heart failure.
- Mental health issues: Depression may occur early in hypothyroidism and may become more severe over time. Hypothyroidism can also cause slowed mental functioning.
- Peripheral neuropathy: Longterm uncontrolled hypothyroidism can cause damage to peripheral nerves the nerves that carry information from the brain and spinal cord to the rest of the body.
Signs and symptoms of peripheral neuropathy may include pain, numbness and tingling in the area affcted by the nerve damage.
It may also cause muscle weakness or loss of muscle control. - Myxedema: This rare, lifethreatening condition is the result of longterm, undiagnosed hypothyroidism.
- Its signs and symptoms include intense cold intolerance and drowsiness followed by profound lethargy and unconsciousness.
- A myxedema coma may be triggered by sedatives, infection, or other stress on your body.
- If an individual shows signs or symptoms of myxedema, he/she needs immediate emergency medical treatment.
- Infertility: Low levels of thyroid hormone can interfere with ovulation, which impairs fertility.
- In addition, some of the causes of hypothyroidism — such as autoimmune disorders — can also impair fertility.
- Birth defects: Babies born to women with untreated thyroid disease may have a higher risk of birth defects than babies born to healthy mothers.
- These children are also more prone to serious intellectual and developmental problems.
- Infants with untreated hypothyroidism present at birth are at risk of serious problems with both physical and mental development.
- But if this condition is diagnosed within the first few months of life, the chances of normal development are excellent.
Question 9. Discuss thyroid function tests.
Answer. A laboratory thyroid profile includes measurement of
- Serum T4
- Resin T3 uptake
- T4 binding ratio
- Free T4 index
- Thyroid-stimulating hormone.
Serum t4
- Measured total serum T4 reflects hormone which both binds to thyroidbinding globulin and free hormone.
- The normal range of serum T4 is 5–11.5 µg/DL. Hence, changes in either free hormone level or concentration in thyroidbinding globulin will alter total serum T4 but not affect free hormone level.
- Therefore, increased secretion of thyroidbinding globulin increases total serum T4 whereas a decrease in TBG lowers total serum T4.
Resin T3 Uptake
- It reflects the thyroid-binding globulin concentration and is reported as a percentage, i.e. 25 to 35%.
- A present amount of radioactive T3 is added to the patient’s sample of serum.
- Radioactive T3 binds to all liable binding sites on thyroid-binding globulin and leftover is bound to resin and is measured.
T4 Binding ratio
- The resin T3 uptake is converted to the T4 binding ratio by dividing the measured resin T3 uptake by reference serum mean resin T3 uptake which is 30%.
- The resin T3 uptake and T4 binding ratio are low and high in hypothyroidism and hyperthyroidism, respectively.
Free t4 Index
- It represents a calculated free T4 hormone concentration. It is calculated by multiplying the total serum T4 by the T4 binding ratio.
- The free T4 index is low and high in hypothyroidism and hyperthyroidism.
Thyroid-stimulating hormone (TSH)
- It is secreted from the anterior pituitary and has a negative feedback relationship with circulating T4 and T3.
- It is the single best test for diagnosing primary hypothyroidism and hyperthyroidism.
- In the former condition, serum TSH is increased and in the latter condition, it is decreased.
Question.10.Write briefly on Addison’s disease.
Answer. Addison’s disease or primary hypoadrenalism results from the destruction of the adrenal cortex by a variety of pathological processes.
Addison’s Disease Etiology
- It is caused due to autoimmune adrenalitis.
- Infections, i.e. TB, cytomegalovirus, and fungal infection associated with AIDS.
- By tumors
- Inherited disorders, i.e. adrenoleukodystrophies and familial isolated glucocorticoid defiiency.
Clinical Features Of Addison’s Disease
- Pigmentation of skin and mucus membrane: There is bluish-black discoloration of lips, gums, and the posterior aspect of the palate.
- Gastrointestinal symptoms: Anorexia, nausea and vomiting.
- Constipation with intermittent diarrhea, achlorhydria, and abdominal pain
- Cardiovascular system: Postural hypotension, and faintness may result. Dyspnea is also present.
- Muscular system: Muscular weakness and wasting with creatinuria. Sometimes cramps in muscles are present.
- Mental and nervous: Muscle weakness and lassitude (exhaustion) are the first symptoms to appear. Loss of memory and drowsiness.
- Genital system: Impotence and *amenorrhea are present.
- Renal system: Renal function is impaired and the excretion of urine is diminished.
Investigation Of Addison’s Disease
- Serum sodium and chloride levels are decreased
- The blood sugar level is decreased
- Blood urea increases
- Urine secretion of chloride is increased.
- Urinary secretion decreases
- BMR is decreased
- Abdominal X-ray shows calcification of the adrenal gland.
Treatment Of Addison’s Disease
- Cortisone substitution: Hydrocortisone 20 mg TDS for 72 hours. For maintenance, the dose is 20 mg in the morning and 10 mg in the evening.
- Aldosterone substitution: Fludrocortisone 50 μg BD is started.
- Salt: Patients with diarrhea or profuse sweating should be given an additional 3–6 gm of sodium chloride daily.
Question.11. Write a short note on thyrotoxicosis (Clinical features).
Answer.
Clinical Features Of Thyrotoxicosis
- Goiter is present, i.e. either diffuse or nodular.
- Gastrointestinal features: Vomiting, diarrhea, and weight loss
- Cardiovascular features: Arrhythmia, i.e. atrial fibrillation, dyspnea, wide pulse pressure
- Dermatological manifestations: Clubbing, loss of hair, palms becoming red, increased sweating
- Reproductive features: Amenorrhea, infertility, abortion, impotence
- Ophthalmological features: Exophthalmos, Diplopia, lid retraction, staring look, excessive watering from eyes
- Neuromuscular features: Tremors in hand, psychosis, irritability, restlessness, nervousness, high tendon reflexes
- Miscellaneous: Fatigue, polydipsia, heat tolerance
Question.12.Describe the clinical findings of hyperthyroidism.
Or
Describe the clinical findings, diagnosis, and management of hyperthyroidism.
Answer.
Clinical Features Of Hyperthyroidism
- Goiter is present, i.e. either diffuse or nodular.
- Gastrointestinal features: Vomiting, diarrhea, and weight loss
- Cardiovascular features: Arrhythmia, i.e. atrial fibrillation, dyspnea, wide pulse pressure
- Dermatological manifestations: Clubbing, loss of hair, palms becoming red, increased sweating
- Reproductive features: Amenorrhea, infertility, abortion, impotence
- Ophthalmological features: Exophthalmos, Diplopia, lid retraction, staring look, excessive watering from eyes
- Neuromuscular features: Tremors in hand, psychosis,irritability, restlessness, nervousness, high tendon reflexes
- Miscellaneous: Fatigue, polydipsia, heat tolerance
Drug Therapy for hyperthyroidism
- Anti-thyroid drugs such as carbimazole, i.e. 40–60 mg/day, methimazole, i.e. 100–150 mg 8 hourly, and propylthiouracil, i.e. 300–450 mg/day can be given depending on the severity of the disease.
Drugs should be gradually decreased for 4–8 weeks based on FT4 levels.
When FT4 levels are normal carbimazole 5–15 mg/day or propylthiouracil 50 mg/day is given.
Drugs can be given for 1–2 years by regular checking of FT4 and TSH levels. - For symptomatic relief betablockers such as propanolol 80–160 mg daily is given.
It is given for 2–3 weeks along with anti-thyroid treatment.
It relieves symptoms such as anxiety, tremors, and tachycardia. - Dexamethasone 8 mg/day may be used to inhibit the conversion of T4–T3 in severe forms of thyrotoxicosis.
- Lithium carbonate 300–450 mg TDS inhibits thyroid hormone secretion temporarily in patients who are allergic to iodides and thioamides.
- Potassium perchlorate 500 mg BD inhibits iodine uptake by the thyroid gland. It is combined with thioamides.
Diagnosis Of Hyperthyroidism
The case with signs like exophthalmos, tremors, tachycardia, and thyroid enlargement and symptoms, i.e. sweating, intolerance to heat, restlessness, increased appetite, diarrhea, and weight loss can be diagnosed as hyperthyroidism. In an anxiety state, the hands are cold and moist while in hyperthyroidism, they are warm and moist.
- Thyroid function test: There are raised T3 and T4 levels.
- Diagnosis is solely based on investigations.
- Serum TSH level is decreased and is the initial diagnostic test. Normal TSH levels exclude clinical hyperthyroidism.
- Serum total and unbound (free) T3 and T4 are increased in hyperthyroidism.
- In some cases, only T3 levels are raised whereas T4 is normal (T3 toxicosis).
- TSHR antibody levels are increased in about 75% of cases.
ESR may be increased in subacute thyroiditis. - The uptake of radioactive iodine by the thyroid is increased in Graves’ disease and toxic nodular goiter, whereas it is low in subacute thyroiditis.
- Ultrasonography of the thyroid gland reveals diffuse enlargement of the thyroid gland which helps differentiating
- Graves’ disease from nodular goiter.
Question 13. Write a short note on the parathyroid hormone.
Answer. Parathyroid hormone is secreted by the chief cells of the parathyroid gland.
Action Of Parathyroid Hormone
- The primary function of parathyroid hormone is to maintain the blood calcium level within the range of 9 to 11 mg.
- Parathyroid hormone maintains blood calcium levels by acting on bone, kidney, and GIT; by increasing the resorption of calcium from bones, by decreasing the excretion of calcium through kidneys, by increasing absorption of calcium through GIT.
- The increased activity of parathyroid glands leads to excessive secretion of parathormone which leads to the disorder known as hyperparathyroidism and decreased synthesis of parathormone is called hypoparathyroidism.
Question 14. Write a short note on thyrotoxicosis.
Or
Write a short answer on thyrotoxicosis.
Answer.
Hyperthyroidism is defined as an increased secretion of thyroid hormone with an increase in levels of T3 and T4.
Etiology Of Thyrotoxicosis
Common causes:
- Grave’s disease
- Toxic nodular goiter
- Multinodular
- Solitary nodule
Less common:
- Thyroiditis
- Druginduced
- Factitious
- Iodine excess
Rare:
- Pituitary or ectopic TSH
- Thyroid carcinoma
Clinical Features Of Thyrotoxicosis
- Goiter is present, i.e. either diffuse or nodular.
- Gastrointestinal features: Vomiting, diarrhea, and weight loss
- Cardiovascular features: Arrhythmia, i.e. atrial fibrillation, dyspnea, wide pulse pressure
- Dermatological manifestations: Clubbing, loss of hair, palms becoming red, increased sweating
- Reproductive features: Amenorrhea, infertility, abortion, impotence
- Ophthalmological features: Exophthalmos, Diplopia, lid retraction, staring look, excessive watering from eyes
- Neuromuscular features: Tremors in hand, psychosis,irritability, restlessness, nervousness, high tendon reflexes
- Miscellaneous: Fatigue, polydipsia, heat tolerance
Investigations Of Thyrotoxicosis
- Serum TSH level is decreased and is the initial diagnostic test. Normal TSH levels exclude clinical hyperthyroidism.
- Serum total and unbound (free) T3 and T4 are increased in hyperthyroidism.
- In some cases, only T3 levels are raised whereas T4 is normal (T3 toxicosis).
- TSHR antibody levels are increased in about 75% of cases.
- ESR may be increased in subacute thyroiditis.
- The uptake of radioactive iodine by the thyroid is increased in Graves’ disease and toxic nodular goiter, whereas it is low in subacute thyroiditis.
- Ultrasonography of the thyroid gland reveals diffuse enlargement of the thyroid gland which helps differentiate.
- Graves’ disease from nodular goiter.
Drug Therapy Of Thyrotoxicosis
- Anti-thyroid drugs such as carbimazole, i.e. 40–60 mg/day, methimazole, i.e. 100–150 mg 8 hourly, and propylthiouracil, i.e. 300–450 mg/day can be given depending on the severity of the disease.
- Drugs should be gradually decreased for 4–8 weeks based on FT4 levels. When FT4 levels are normal carbimazole 5–15 mg/day or propylthiouracil 50 mg/day is given.
- Drugs can be given for 1–2 years by regular checking of FT4 and TSH levels.
- For symptomatic relief betablockers such as propanolol 80–160 mg daily is given.
- It is given for 2–3 weeks along with anti-thyroid treatment.
- It relieves symptoms such as anxiety, tremors, and tachycardia.
- Dexamethasone 8 mg/day may be used to inhibit the conversion of T4–T3 in severe forms of thyrotoxicosis.
- Lithium carbonate 300–450 mg TDS inhibits thyroid hormone secretion temporarily in patients who are allergic to iodides and thioamides.
- Potassium perchlorate 500 mg BD inhibits iodine uptake by the thyroid gland. It is combined with thioamides.
Surgery Of Thyrotoxicosis
- Subtotal thyroidectomy is done in severely affcted cases. Before surgery, the patient should be made euthyroid by beta blockers and antithyroid drugs.
- Two weeks before the surgery drugs should be stopped and lugol iodine is given to reduce the vascularity.
Radioactive Iodine Of Thyrotoxicosis
- Radioactive iodine, i.e. 131I leads to the destruction of thyroid cells and is given with antithyroid drugs to prevent thyroid storm.
- Antithyroid drugs must be stopped for a minimum of 3–5 days before 131I to allow uptake of isotope 555MBq to ablate the thyroid.
- High doses are needed for large goiters in severely thyrotoxic patients.
Question.15. Write a short note on investigations in a case of Cushing’s syndrome.
Answer. Cushing’s syndrome is caused by the excessive production of cortisol.
Investigations Of Cushing’s Syndrome
- Urinary excretion of 11 oxysteroids and 17 ketosteroids is increased.
Dexamethasone suppression test showing failure of significant plasma cortisol suppression favors adrenal tumor as the cause. - Glucose tolerance tests such as diabetes.
- Xray chest for evidence of thymic carcinoma.
- Xray skull for pituitary edema is not helpful since a pituitary basophilic adenoma does not expand and so sella turcica and glenoid processes are normal.
- Xray dorsal spine may show the collapse of vertebrae producing a fish spine appearance.
- IV *pyelography for adrenocortical tumor. *Perirenal insufflation, *tomography, USG and CT scan, and MRI to detect adrenal hyperplasia.
Question.16. Write in brief clinical features and management of thyroid nodules.
Answer. The term “thyroid nodule” refers to any abnormal growth that forms a lump in the thyroid gland.
Clinical Features Of Thyroid Nodules
- Voice hoarseness
- The rapid increase in size, there are compressive symptoms such as dyspnea or dysphagia
- Lymphadenopathy
- Sudden, unexplained weight loss
- Nervousness
- Rapid or irregular heartbeat.
Management Of Thyroid Nodules Surgery should be performed in the following instances:
- Reaccumulation of the nodule despite 3 to 4 repeated FNACs
- Size in excess of 4 cm
- Complex cyst on thyroid ultrasound (showing solid and cystic components)
- Compressive symptoms
- Signs of malignancy (vocal cord dysfunction, lymphadenopathy)
Oral thyroxine therapy suppresses pituitary secretion of thyroidstimulating hormone, thereby removing an important growth factor for thyroid follicle cells.

Leave a Reply