Drugs Used In Respiratory System
Question 1. Write A Short Note On Cough Expectorant.
Answer:
Cough expectorants or mucokinetics are drugs that increase bronchial secretion or reduce its viscosity, facilitating its removal by coughing.
Types Of Cough Expectorants
- Bronchial secretion enhancers: Sodium or potassium citrate, potassium iodide, guaifenesin, balsam of Tolu, vasaka, ammonium chloride.
- Mucolytics: Bromhexine, ambroxol, acetylcysteine, carbocisteine.
Bronchial Secretion Enhancers
Sodium or potassium citrate: They increase bronchial secretion by salt-action.
Potassium iodide: It is secreted by bronchial glands and can irritate airway mucosa. Its chronic use can affect thyroid function. It is not used now.
Guaifenesin, vasaka, and Tolu balsam: They enhance the bronchial secretion and mucociliary function while being secreted by tracheobronchial glands.
Read And Learn More: Pharmacology Question And Answers
Ammonium chloride: Ammonium salts are nauseating and reflexly increase respiratory secretions.
Mechanism Of Action
Side Effects
Nausea, vomiting, and bronchospasm.
Mucolytics
Bromhexine
- It is a derivative of the alkaloid vaccine which is obtained from the adhatoda vasica.
- It is a potent mucolytic and microkinetic.
- It is capable of inducing thin copious bronchial secretion.
Mechanism Of Action
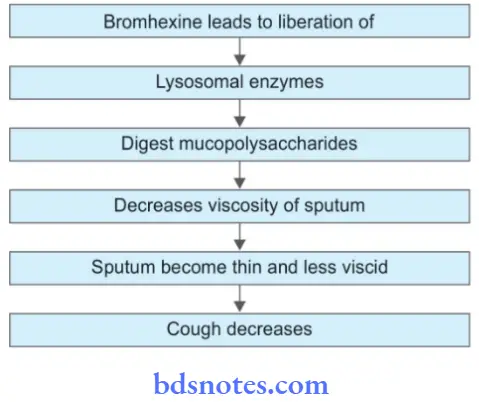
Side Effects: Rhinorrhea, lacrimation, gastric irritation, and hypersensitivity.
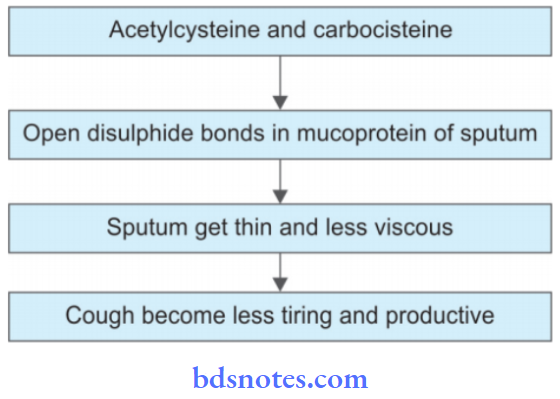
Acetylcysteine And Carbocisteine
These are the mucolytics that are used as aerosols in the treatment of cough.
Question 2. Write A Short Note On Bromhexine.
Answer:
- It is a derivative of the alkaloid vaccine which is obtained from the adhatoda vasica.
- It is a potent mucolytic and mucokinetic.
- It is capable of inducing thin copious bronchial secretion.
Mechanism Of Action
Side Effects
- Rhinorrhea
- Lacrimation
- Gastric irritation
- Hypersensitivity.
Question 3. Give A Description Of The Central Cough Suppressant.
Or
Write A Short On Antitussive Drugs.
Answer:
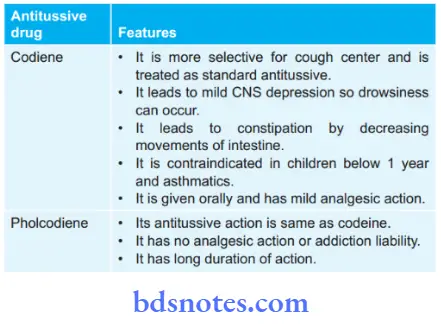
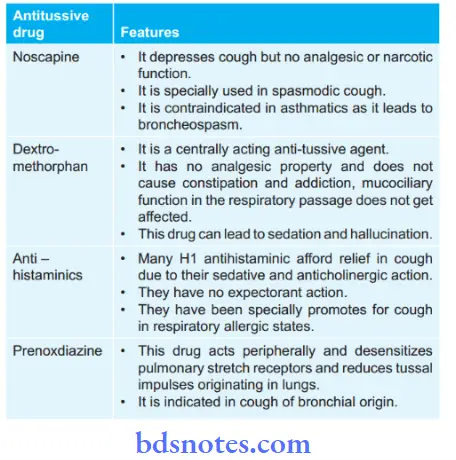
Central cough suppressant is also known as antitussive.
Antitussive: These drugs act on CNS and raise the threshold of the cough center or act peripherally in the respiratory tract to reduce tussive impulse or both these actions.
Classification
- Opioids: Codeine, pholcodine, ethylmorphine.
- Nonopioids: Noscapine, dextromethorphan, chlophedianol.
- Antihistaminic: Diphenhydramine, chlorpheniramine, and promethazine.
- Peripherally acting: Prenoxdiazine.
Question 4. Write A Short Note On Salbutamol.
Answer:
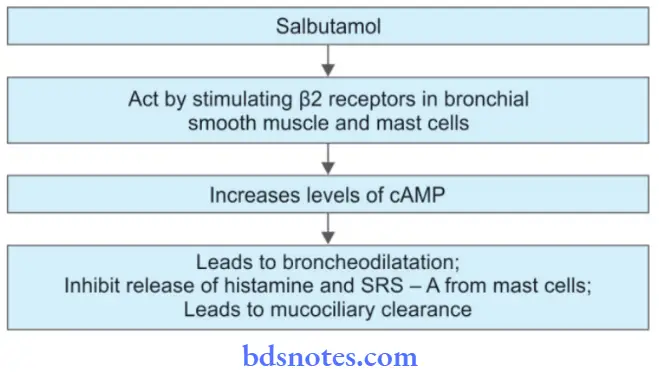
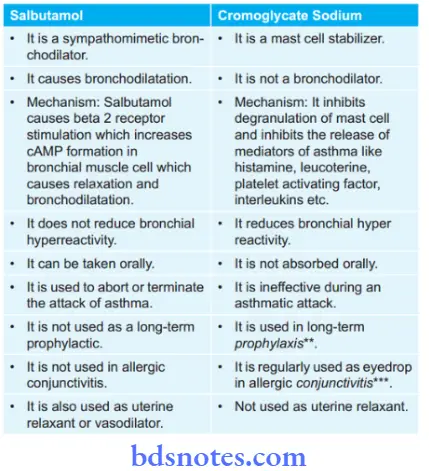
Salbutamol is a sympathomimetic bronchodilator.
Inhaled salbutamol produces bronchodilatation in 5 min and its action last for 2 to 4 hours.
Mechanism Of Action
 Pharmacological Actions
Pharmacological Actions
- It leads to bronchodilatation.
- It causes relaxation of the pregnant uterus.
- It leads to the dilatation of blood vessels that supply skeletal muscles.
- Salbutamol promotes hepatic glycogenolysis and the uptake of potassium in cells.
Therapeutic Uses
- Bronchial asthma as it causes bronchodilatation.
- It delays premature labor.
- It is useful in hyperkalemia as it increases the uptake of potassium ions in cells.
Side Effects
- Cardiac side effects such as tachycardia and palpitation are less prominent.
- Muscle tremors
- Presence of restlessness, nervousness, throat irritation, and ankle edema.
- Hyperglycemia can occur in diabetics.
Question 5. Compare The Action And Uses Of Salbutamol And Cromoglycate Sodium.
Answer:
Question 6. Write A Short Note On Bronchodilators.
Or
Write A Short Note On Bronchodilators In Bronchial Asthma.
Or
Write Short Note On Bronchodilator Drugs.
Answer:
Bronchodilators are used in the treatment of bronchial asthma.
The following are the bronchodilators:
1. Sympathomimetics:
- Selective β2 adrenergic agonists: Salbutamol, Terbutaline, Bambuterol, Salmeterol, Formoterol, Ephedrine
- Non-selective: Adrenaline
2. Methylxanthines: Theophylline, aminophylline, cholinetheophyllinate, hydroxyethyl theophylline, Theophylline ethanolate of piperazine, doxophylline
3. Anticholinergics: Ipratropium bromide, tiotropium bromide.
Sympathomimetics
- Selective β2 adrenergic agonists act by stimulating β2 receptors in bronchial smooth muscles and mast cells and increasing cAMP formation which leads to
bronchodilatation, inhibit the release of histamine SRS-A from mast cells and promote mucociliary clearance.
Selective β2 adrenergic agonists are the first-line drugs for bronchial asthma. On inhalation, these drugs are very well tolerated. - Non-selective sympathomimetics, i.e. adrenaline. Adrenaline produces prompt and powerful bronchodilatation by acting through β2 adrenergic receptors. Its
use is declining these days due to its dangerous side effects.
Methylxanthines
- Theophylline and aminophylline cause inhibition of phosphodiesterase and prevent degradation of cAMP and cGMP. This causes an increase in the accumulation of intracellular cAMP which leads to bronchodilatation,
inhibit the release of histamine SRS-A from mast cells and promote mucociliary clearance. - Methylxanthines potentiate the effect of sympathomimetics i.e. increases bronchodilatation and cardiac stimulation.
- Methylxanthines have a narrow margin of safety i.e. they can lead to tachycardia, palpitation, hypotension, and sometimes sudden death due to cardiac arrhythmia.
- Theophylline is given by oral route while aminophylline is given by slow IV infusion.
Anticholinergics
- Anticholinergics selectively block the effects of acetylcholine in bronchial smooth muscle and lead to bronchodilatation but these drugs have no effect on mucociliary clearance.
- Anticholinergics have less effect on bronchial asthma as compared to sympathomimetic drugs.
- They are administered through an inhalational route.
- In acute severe asthma combination of ipratropium bromide along with β2 adrenergic agonists provide more prolonged bronchodilatation.
Question 7. Write Pharmacological Basis For Use Of Selective β2 Agonist For Bronchial Asthma.
Answer:
Selective β2 agonist activates β2 adrenoceptors present on airway smooth muscle and enhances the release of cAMP by activating the adenyl cyclase enzyme.
The mast cells have β2 adrenergic receptors that also respond to them.
So these drugs relax the smooth muscle of the airway and inhibit the release of bronchoconstriction chemical mediators from the mast cells and increase mucociliary transport by increasing ciliary activity.
Question 8. Explain Why Salbutamol Is Preferred Over Ephedrine In Asthma.
Answer:
Salbutamol is fastest acting bronchodilator with a peak effect in 10 minutes while ephedrine is slow in onset, has low efficacy, and has frequent side effects.
That’s why salbutamol is preferred over ephedrine in asthma.
Question 9. Explain why salbutamol is preferred over isoprenaline in the treatment of asthma.
Answer:
- Bronchial airways contain β2 receptors which are responsible for producing bronchodilation. Salbutamol is a selective β2 agonist which is usually administered by the inhalational route during an acute asthmatic attack. Therefore, it produces bronchodilation and improves airflow without having any prominent adverse effect on other systems.
In comparison, isoprenaline is a non-selective β receptor agonist exerting its action on both β1 and β2 receptors, though, it can dilate the bronchus (due to β2 agonism), its additional action on the β1 receptors can lead to tachycardia and even fatal arrhythmias at high doses. - Salbutamol can be given by inhalational route whereas isoprenaline is given by IV route. Therefore the risk of extrapulmonary adverse effects due to β2 agonism like tremors and hypoglycemia more with isoprenaline as compared to salbutamol.
Question 10. Write A Short Note On Montelukast.
Answer:
It is a leukotriene antagonist.
Mechanism Of Action
Montelukast competitively antagonizes (blocks) CysLT1 receptor-mediated bronchoconstriction, increased vascular permeability, and recruitment of eosinophils.
Indications
Prophylactic therapy in mild to moderate asthma. In asthmatic patients, bronchodilatation, reduced sputum eosinophil count, suppression of bronchial inflammation, and hyperreactivity are noted.
In aspirin-induced asthma.
Side Effects
- Headache and rashes.
- Churg-Strauss syndrome.
Question 11. Classify Drugs Used For The Treatment Of Bronchial Asthma And Discuss Inhalational Corticosteroids.
Answer:
Classification Of Drugs Used For Treatment Of Bronchial Asthma
1. Bronchodilators
- Sympathomimetics:
- Selective β2 adrenergic agonists: Salbutamol, terbutaline, bambuterol, salmeterol, formoterol, ephedrine
- Non-selective: Adrenaline
- Methylxanthines: Theophylline, aminophylline, choline theophylline, hydroxyethyl theophylline, theophylline ethanolate of piperazine, doxophylline
- Anticholinergics: Ipratropium bromide, tiotropium bromide
2. Leucotriene antagonists: Montelukast, Zafilukast
3. Mast cell stabilizer: Sodium cromoglycate, Ketotifen
4. Corticosteroids
- Systemic: Hydrocortisone, prednisolone, and other
- Inhalational: Beclomethasone dipropionate, budesonide, flticasone propionate, flnisolide, ciclesonide
5. Anti-IgE antibody: Omalizumab.
Inhalational Corticosteroids
- Inhalational corticosteroids are beclomethasone dipropionate, budesonide, fluticasone propionate, flnisolide, ciclesonide.
- Inhaled glucocorticoids, i.e. beclomethasone, budesonide, fluticasone, and ciclesonide are the prophylactic agents in bronchial asthma. Ciclesonide is added later on. Ciclesonide is a prodrug and gets activated by esterases in bronchial epithelium.
- Since airway inflammation is present in early mild disease and bronchial remodeling starts developing from the beginning, it is advocated that inhaled steroids are the first step for all asthma patients.
- Inhaled steroids suppress bronchial inflammation, increase peak expiratory flow rate and reduce the need to rescue β2 agonist inhalation, and prevent episodes of acute asthma.
- Adverse effects of inhalational steroids are hoarseness of voice, dysphonia, sore throat, and asymptomatic or symptomatic oropharyngeal candidiasis. These side effects are reduced by using a spacer and rinsing the mouth after each dose.
- Inhaled steroids along with long-acting β agonists have synergistic action and are used in bronchial asthma and COPD. They are also used in moderate and severe persistent asthma. Examples are Fluticasone + Salmeterol, Budesonide + Formoterol.
Question 12. Classify Drugs Used In Treatment Of Bronchial Asthma.
Answer:
Classification Of Drugs Used For Treatment Of Bronchial Asthma
1. Bronchodilators
- Sympathomimetics:
- Selective β2 adrenergic agonists: Salbutamol, Terbutaline, Bambuterol, Salmeterol, Formoterol, Ephedrine
- Non-selective: Adrenaline
- Methylxanthines: Theophylline, aminophylline, choline theophylline, hydroxyethyl theophylline, theophylline ethanolate of piperazine, doxophylline
- Anticholinergics: Ipratropium bromide, tiotropium bromide
2. Leucotriene antagonists: Montelukast, zafilukast
3. Mast cell stabilizer: Sodium cromoglycate, ketotifen
4. Corticosteroids
- Systemic: Hydrocortisone, Prednisolone, and other
- Inhalational : Beclomethasone dipropionate, Budesonide, Fluticasone propionate, Flunisolide, Ciclesonide
5. AntiIgE antibody: Omalizumab

Leave a Reply