Drugs Used In Congestive Heart Failure Congestive Heart Failure
Congestive heart failure (CHF) is a chronic progressive condition that affects the pumping power of your heart muscles. Cardiac failure is the inability of the heart to pump blood effectively at a rate that meets the needs of metabolizing tissues.
- This occurs due to reduced contractility of the cardiac muscles, especially those of the ventricles, which cause a decrease in cardiac output, increasing the blood volume of the heart.
- As a result, systemic blood pressure and renal blood flow are both reduced, which often leads to the development of edema in the lower extremities and the lung (pulmonary edema) as well as renal failure.
Types of CHF
- Left-sided CHF is the most common type of CHF. It occurs when the left ventricle doesn’t properly pump blood out to the body. As the condition progresses, fluid can build up in the lungs, which makes breathing difficult. There are two types of left-sided heart failure:
- Systolic heart failure occurs when the left ventricle fails to contract normally. This reduces the level of force available to push blood into circulation.
- Diastolic failure or diastolic dysfunction happens when the muscle in the left ventricle becomes stiff. Because it can no longer relax, the heart can’t quite fill with blood between beats.
- Right-sided CHF occurs when the right ventricle has difficulty pumping blood to the lungs. Blood backs up in blood vessels, which causes fluid retention in the lower extremities, abdomen, and other vital organs.
- It’s possible to have left-sided and right-sided CHF at the same time. Usually, the disease starts on the left side and then travels to the right when left untreated.
Read and Learn More Medicinal Chemistry II Notes
Drugs Used In Congestive Heart Failure
Drugs that increase the force of contraction allow greater amounts of blood to be distributed throughout the body and, in turn, reduce the symptoms associated with CHF.
Most of the positive inotropic agents show their effects on the force of contraction by modifying the coupling mechanism involved in the myocardial contractile process.
Cardiac Glycosides
Cardiac glycosides have both beneficial and toxic effects on the heart. Digoxin is one of the oldest compounds used in cardiovascular medicine.
Chemistry of the Cardiac Glycosides Cardiac glycosides are composed of two portions the sugar moiety and the non-sugar (aglycone) moiety.
- Aglycones- The aglycone portion of the cardiac glycosides is a steroid nucleus containing 4 rings A, B, C, and D. Rings A and C-D are cis fused, whereas rings B-C have a trans configuration.
- The cardiac glycosides include two distinct classes of compounds the cardenolides and the bufadienolides.
- These differ in the substitutions at the C-17 position; where the cardenolides possess an unsaturated butyrolactone ring, the bufadienolides, possess a six-membered lactone ring with two conjugated double bonds.
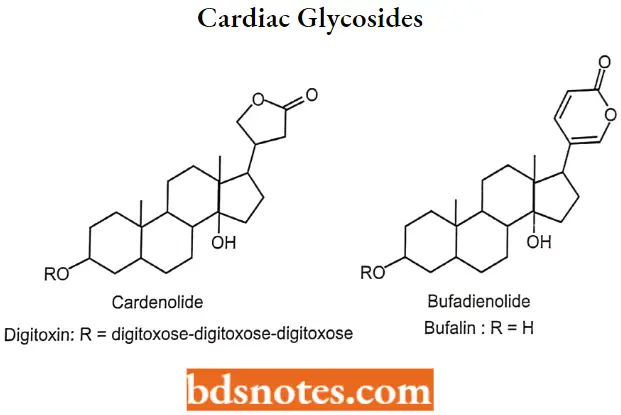
Glycone or Sugar moiety – Hydroxyl group of aglycone at the 3 position is conjugated with sugar moiety via 1,4- glucosidic linkage. Commonly found sugar moieties are 1-rhamnose, d-digitoxose, d-glucose, and d-cymarose. These sugars existin β- conformation.
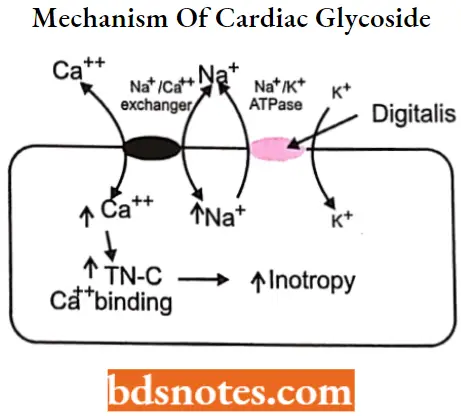
Cardiac Glycosides MOA: Cardiac glycosides show a positive inotropic effect. They inhibit the membrane-bound Na+/K+– adenosine triphosphatase (Na+/K+ ATPase) pump which is responsible for sodium/potassium exchange.
- Normally, these Na+/K+-ATPase pumps move potassium ions in and sodium ions out of the myocardium. At the resting state, sodium is located outside the cell.
- On membrane depolarization, Na+ goes inside, leading to an immediate elevation of the action potential.
- Increased intracellular sodium stimulates the influx of Ca2++ which is represented by the plateau region of the cardiac action potential. The influx of calcium causes the efflux of potassium out of the myocardial membrane.
- The Na+/K+ exchange is an energy-dependent process and is catalyzed by the enzyme Na+/K+– ATPase.
Cardiac glycosides inhibit this enzyme, due to which less amount of sodium is exchanged with potassium which in turn results in increased intracellular calcium. Elevated intracellular calcium concentration causes an increase in myocardial contraction.
Digoxin
A cardiotonic glycoside obtained mainly from Digitalis lanata; it consists of three sugars and the aglycone digoxigenin. Digoxin has positive inotropic and negative chronotropic activity.
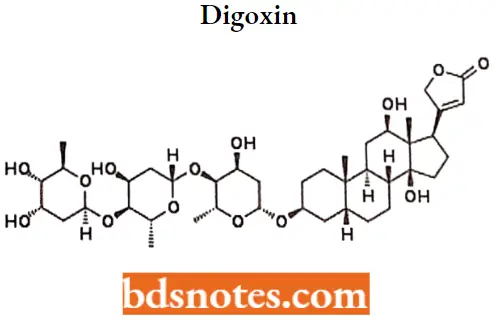
Dlgoxin MOA: Digoxin inhibits the Na+/K+-ATPase membrane pump, increasing intracellular sodium and calcium concentrations. Increased intracellular concentrations of calcium may promote the activation of contractile proteins (For Example., actin, and myosin).
Dlgoxin Metabolism: Hepatic (but not dependent upon the cytochrome P-450 system). The end metabolites, which include 3 b-digoxigenin, 3-keto-digoxigenin, and their glucuronide and sulfate conjugates, are polar and are postulated to be formed via hydrolysis, oxidation, and conjugation.
Dlgoxin Uses: It is used to control ventricular rate in atrial fibrillation and in the management of congestive heart failure with atrial fibrillation.
- Its use in congestive heart failure and sinus rhythm is less certain. The margin between toxic and therapeutic doses is small.
- Digoxin is usually given orally, but can also be given by 4 injections in urgent situations. The half-life is about 3b hours for patients with normal renal function.
Toxicity
In mild to moderate toxicity, the common symptoms are anorexia, nausea and vomiting, muscular weakness, bradycardia, and ventricular premature contractions. The nausea is a result of the excitation of the chemoreceptor trigger zone in the medulla.
- In severe toxicity, the common symptoms are blurred vision, disorientation, diarrhea, ventricular tachycardia, and AV block, which can progress into ventricular fibrillation.
- It is usually accepted that the toxicity of the cardiac glycosides results from inhibition of the Na+/K+-ATPase pump, which results in increased intracellular levels of Ca2+.
- Hypokalemia (decreased potassium), which can be induced by co-administration of thiazide diuretics, glucocorticoids, or by other means, can be an important factor in initiating a toxic response.
Digitoxin
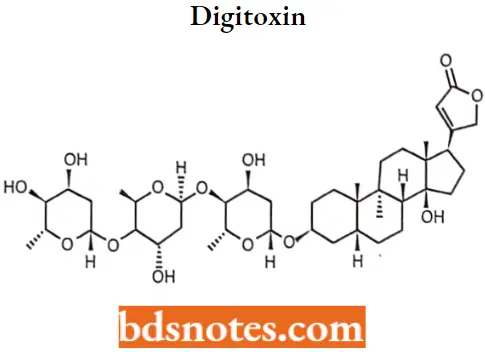
Digitoxin MOA: Digitoxin inhibits the Na-K-ATPase membrane pump, increasing intracellular sodium and calcium concentrations. Increased intracellular concentrations of calcium may promote the activation of contractile proteins (For Example., actin, and myosin).
Digitoxin also acts on the electrical activity of the heart, increasing the slope of phase 4 depolarization, shortening the action potential duration, and decreasing the maximal diastolic potential.
Digitoxin Uses: For the treatment and management of congestive cardiac insufficiency, arrhythmias, and heart failure.
Digitoxin is sometimes used in place of digoxin. It has a longer half-life than digoxin. It is eliminated via the liver, so could be used in patients with poor or erratic kidney function.
Toxicity
Toxic effects, which are similar to those of digoxin namely; anorexia, nausea, vomiting, diarrhea, confusion, visual disturbances, and cardiac arrhythmias are longer lasting.
Nesiritide
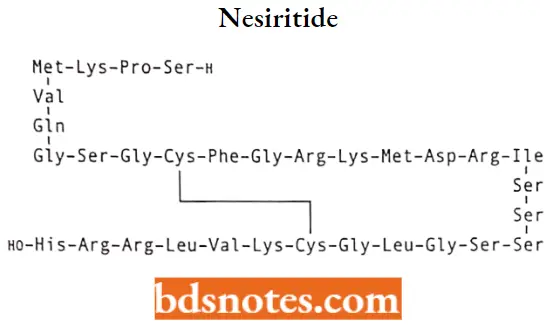
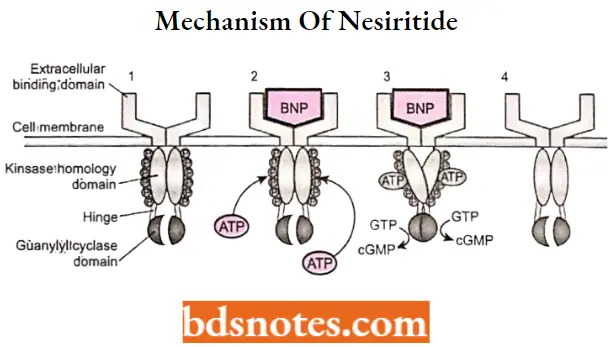
Nesiritide MOA: Nesiritide is a recombinant human B (brain)-type natriuretic peptide (rhBNP) that exerts a direct vasodilator}ÿ effect on arterial and venous blood vessels, along with potent natriuretic and diuretic effects on the kidney.
- These effects result from the binding of rhBNP to natriuretic peptide receptors A and B on vascular smooth muscle cells, endothelial cells, and kidneys.
- And adrenal gland; inhibition of peripheral vascular sympathetic neurotransmission; and inhibition of the renin-angiotensin-aldosterone pathway.
- Binding to natriuretic peptide receptors A and B activates guanylyl cyclase, resulting in an intracellular rise in cGMP. cGMP regulates vascular smooth muscle relaxation via a decrease in intracellular calcium
Nesiritide Metabolism: Nesiritide undergoes proteolytic cleavage of the peptide by endopeptidases, such as neutral endopeptidase, which are present on the vascular lumenal surface.
Nesiritide Uses: For the intravenous treatment of patients with acutely decompensated congestive heart failure who have dyspnea at rest or with minimal activity.
Nesiritide Adverse effect: Symptomatic hypotension has been reported in approximately 4% of adult patients receiving nesiritide.
- Careful blood pressure monitoring is therefore advised, and nesiritide is not recommended in adults with baseline systolic blood pressure less than 100 mm Hg.
- Nesiritide may decrease renal function in patients with severe CHF whose kidney function is dependent on renin-angiotensin-aldosterone function.
Bosentan
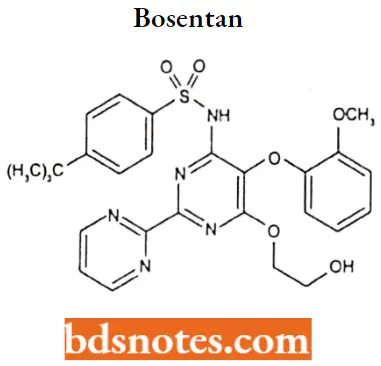
Bosentan IUPAC name: 4-tert-butyl-N-[6-(2-hydroxyethoxy)-5-(2-methoxyphenoxy)-2-(pyrimidin-2-yl) pyrimidin-4-yl] benzene-1-sulfonamide.
Bosentan MOA: Endothelin-1 (ET-1) is a neurohormone, the effects of which are mediated by binding to ETA and ETB receptors in the endothelium and vascular smooth muscle.
- ET-1 concentrations are elevated in the plasma and lung tissue of patients with pulmonary arterial hypertension, suggesting a pathogenic role for ET-1 in this disease.
- Bosentan is a specific and competitive antagonist at endothelin receptor types ETA and ETB– Bosentan has a slightly higher affinity for ETA receptors than for ETB receptors.
Bosentan Metabolism: Bosentan is metabolized in the liver by the cytochrome P450 enzymes CYP2C9 and CYP3A4 (and possibly CYP2C19), producing three metabolites, one of which, Ro 48-5033, is pharmacologically active and may contribute 10 to 20% to the total activity of the parent compound.
Bosentan Uses: Used in the treatment of pulmonary arterial hypertension (PAH), to improve exercise ability and to decrease the rate of clinical worsening (in patients with WHO Class 3 or 4 symptoms).
Bosentan Adverse effects: The most common side effect was headache of mild to moderate intensity, nausea, and vomiting, but no serious adverse events. Mild decreases in blood pressure and increases in heart rate were observed.
Tezosentan
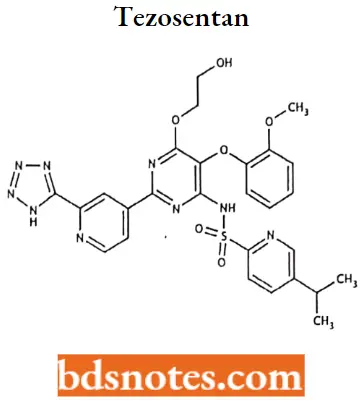
Tezosentan IUPAC name: N-[6-(2-hydroxyethoxy)-5-(2-methoxyphenoxy)-2-[2-(2H-1,2,3,4-tetrazol-5-yl) pyridin-4-yl] pyrimidin-4-yl] -5-(propan-2-yl) pyridine-2-sulfonamide.
Tezosentan MOA: Tezosentan is an intravenous and non-selective ETA and ETB receptor antagonist. It acts as a vasodilator and was designed as a therapy for patients with acute heart failure.
Tezosentan Uses: Investigated for use or treatment in congestive heart failure, liver disease, and heart disease.
Drugs Used In Congestive Heart Failure Multiple Choice Questions And Answers
Question 1. Cardiac glycosides inhibit which of the following?
- Na-H-ATPase
- Na-K-ATPase
- Na-H-Symporter
- All of the above
Answer: 2. Na-K-ATPase
Question 2. Ncsiritlde is metabolized by proteolytic cleavage of the peptide by ________
- Exopepticwses
- Lipase
- Endopeptidases
- Pepsin
Answer: 3. Endopeptidases
Question 3. Clinical efficacy of digitalis glycosides is based on _________
- Decreased transmission through the AV node
- Increased myocardial contractility
- Both
- Neither
Answer: 3. Both
Question 4. Cardiac output is directly dependent upon _________
- Peripheral vascular resistance
- Intravascular blood volume
- Heart rate alone
- Heart rate and stroke volume
Answer: 4. Heart rate and stroke volume
Question 5. Component of digitalis responsible for Na/K ATPase binding ________
- Genin or aglycone moiety
- Sugar residues
- Steroid component
- All of the above
Answer: 1. Genin or aglycone moiety
Question 6. The most common symptom of heart failure.
- Tachycardia
- Oliguria
- Hepatomegaly
- Dyspnea
Answer: 4. Dyspnea
Question 7. Clinical efficacy of digitalis glycosides is based on _________
- Decreased transmission through the AV node
- Increased myocardial contractility
- Both
- All of the above
Answer: 3. Both
Question 8. Primarily excreted in the urine; digitalis glycosides with half-life of 16 days.
- Digoxin
- Digitoxin
- Both
- None of the above
Answer: 1. Digoxin
Question 9. Inhibitors of Na/K ATPase used in the management of CHF.
- Enalapril
- Digoxin
- Minoxidil
- Amrinone
Answer: 2. Digoxin
Question 10. The mechanism by which vasodilators improve myocardial performance in CHF.
- Increase heart rate
- Promote diuresis
- Reduce afterload
- Reduce pulmonary blood flow
Answer: 3. Reduce afterload
Question 11. Which of the following is an intravenous endothelin receptor antagonist?
- Tezosentan
- Digoxin
- Nesiritide
- Digitoxin
Answer: 4. Digitoxin
Drugs Used In Congestive Heart Failure Short Questions And Answers
Question 1. Explain the different types of CHF
Answer:
- Left-sided CHF is the most common type of CHF. It occurs when the left ventricle doesn’t properly pump blood out to the body. As the condition progresses, fluid can build up in the lungs, which makes breathing difficult. There are two types of left-sided heart failure:
- Systolic heart failure occurs when the left ventricle fails to contract normally. This reduces the level of force available to push blood into circulation.
- Diastolic failure or diastolic dysfunction, happens when the muscle in the left ventricle becomes stiff. Because it can no longer relax, the heart can’t quite fill with blood between beats.
- Right-sided CHF occurs when the right ventricle has difficulty pumping blood to the lungs. Blood backs up in blood vessels, which causes fluid retention in the lower extremities, abdomen, and other vital organs.
- It’s possible to have left-sided and right-sided CHF at the same time. Usually, the disease starts on the left side and then travels to the right when left untreated.
Question 2. Write the mechanism of action of cardiac glycosides.
Answer:
Cardiac glycosides show a positive inotropic effect. They inhibit the membrane-bound Na+/K+- adenosine triphosphatase (Na+/K+ ATPase) pump which is responsible for sodium/potassium exchange.
- Normally, these Na+/K+-ATPase pumps move potassium ions in and sodium ions out of the myocardium. At the resting state, sodium is located outside the cell. On membrane depolarization, Na+ goes inside, leading to an immediate elevation of the action potential.
- Increased intracellular sodium stimulates the influx of Ca2++ which is represented by the plateau region of the cardiac action potential.
- The influx of calcium causes the efflux of potassium out of the myocardial membrane. The Na+/K+ exchange is an energy-dependent process and is catalyzed by the enzyme Na+/K+-ATPase.
- Cardiac glycosides inhibit this enzyme, due to which less amount of sodium is exchanged with potassium which in turn results in increased intracellular calcium. Elevated intracellular calcium concentration causes an increase in myocardial contraction.
Question 3. Write the mechanism of action of Nesiritide
Answer:
Nesiritideis a recombinant human B (brain)-type natriuretic peptide (rhBNP) that exerts a direct vasodilatory effect on arterial and venous blood vessels, along with potent natriuretic and diuretic effects on the kidney.
- These effects result from the binding of rhBNP to natriuretic peptide receptors A and B on vascular smooth muscle cells, endothelial cells, kidney, and adrenal gland; inhibition of peripheral vascular sympathetic neurotransmission; and inhibition of the renin-angiotensin-aldosterone pathway.
- Binding to natriuretic peptide receptors A and B activates guanylyl cyclase, resulting in an intracellular rise in cGMP. cGMP regulates vascular smooth muscle relaxation via a decrease in intracellular calcium.
Question 4. Write the uses of Tezosentan and bosentan.
Answer:
Tezosentan uses– Investigated for use or treatment in congestive heart failure, liver disease, and heart disease.
Bosentan uses– Used in the treatment of pulmonary arterial hypertension (PAH), to improve exercise ability and to decrease tire rate of clinical worsening (in patients with WHO Class 3 or 4 symptoms).

Leave a Reply