Diseases Of Skin
Question.1. Name the vesiculobullous lesions of oral cavity.
Describe etiology, histopathology, and clinical features of oral lichen planus.
Or
Write short answer on clinical features and histology of lichen planus
Answer.
Vesiculobullous Lesions
Fitzpatrick Classification
- According to Anatomical Plane:
- Intraepidermal Blister Granular Layer
- Pemphigus foliaceus
- Frictional blisters
- Staphylococcus scalded syndrome.
- Spinous Layer
- Eczematous dermatitis
- Secondary to heat and cold
- Herpes virus infection
- Familial benign pemphigus
- Suprabasal
- Pemphigus vulgaris
- Pemphigus vegetans
- Darier’s disease
- Basal layer
- Erythema multiforme
- Toxic epidermal necrolysis
- Lupus erythematosus
- Lichen planus
- Epidermolysis bullosa simplex
- Intraepidermal Blister Granular Layer
Read And Learn More: Oral Pathology Question And Answers
- DermalEpidermal Junction Zone:
- Lamina lucida
- Bullous pemphigoid
- Cicatrical pemphigoid
- Epidermolysis bullosa junctional
- Below basal lamina
- Erythema multiforme
- Epidermolysis bullosa dystrophica
- Lamina lucida
Vesiculobullous lesions
- Primary Blistering:
- Pemphigus
- Bullous pemphigoid
- Cicatrical pemphigoid
- Epidermolysis bullosa acqusita.
- Secondary blistering:
- Contact
- Erythema multiform
- Toxic epidermal necrolysis.
- Infection:
- Varicella zoster
- Herpes simplex
- Bullous impetigo.
- Systemic disease:
- Infection cutaneous emboli
- Metabolic
- Diabetic with bullae
- Porphyria cutanea tarda.
Oral Lichen Planus
Lichen planus is also known as lichen ruber planus.
- It is a precancerous condition
- Lichen planus is a common mucocutaneous disease which arises due to an abnormal immunological reaction and the disease has some tendency to undergo malignant transformation.
Oral Lichen Planus Etiology
- Immunology:
- Due to cell-mediated immune response
- Due to autoimmunity
- Immunodeficiency.
- Genetic factors: Lichen planus is reported in families, twins, husband and wife.
- Infectious: By spirochete.
- Drugs and chemicals: It is responsible for the lichenoid reaction.
- Psychogenic factors: Stress results, nervousness with emotional upset, overwork and some form of mental strain.
- Habit: Chewing of tobacco, betel nut and smoking.
Clinical Features Of Oral Lichen Planus
- It occurs among middle-aged and elderly people.
- There is slight predilection for the females.
- Lichen planus can involve several areas of oral cavity.
Oral lesion: Mucosal surface of buccal mucosa, vestibule,tongue, lips, flor of mouth, palate and gingiva. - Patient may report with burning sensation of oral mucosa.
- Oral lesion is characterized by radiating white and gray velvety thread-like papules in linear, angular or retiform arrangement, tiny white elevated dots are present at the intersection of white lines known as “Wickhm’s striae”.
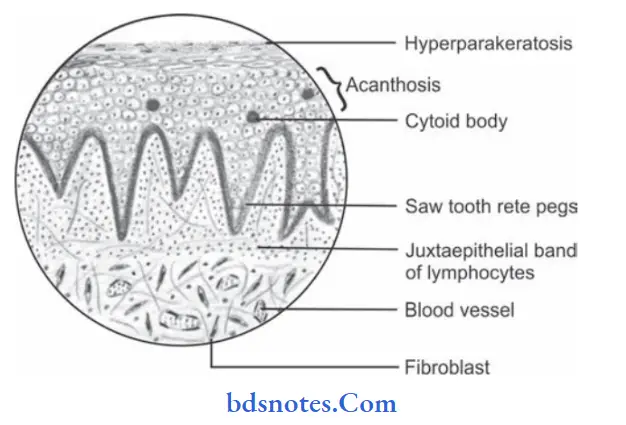
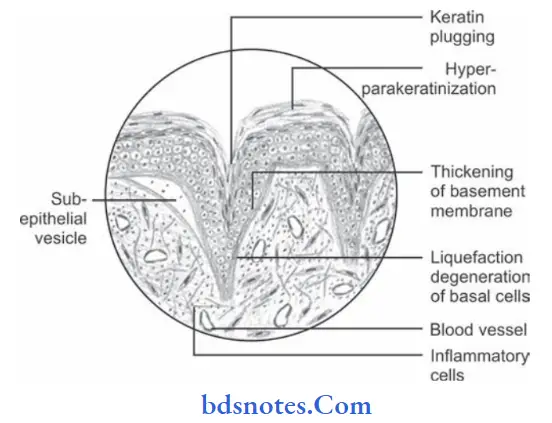
Histopathology Of Oral Lichen Planus
- Overlying surface epithelium exhibits hyperorthokeratinization or hyperparakeratinization or both.
- Acanthosis of spinal cell layer is present.
- Shortened and pointed rete pegs of epithelium which produces “Saw tooth” appearance.
- Intercellular edema in spinous cell layer is present.
- There is presence of necrosis or liquefaction degeneration of basal cell layer of epithelium.
- Few rounded or ovoid, amorphous eosinophilic bodies are present which are known as “Civatt bodies”.
- These civatt bodies represent dead keratinocytes or other necrotic epithelial components which are transported to connective tissue for phagocytosis.
- Chronic inflammatory cell infiltration is present in juxta epithelial lesion.
Question 2. Enumerate vesiculobullous lesions and describe pemphigus.
Answer.
Pemphigus
Pemphigus is a group of vesiculobullous lesion of skin and mucous membrane which is characterized by formation of intraepithelial vesicles or bulla causing separation of epithelium.
Clinical Features Of Pemphigus
- It occurs during 4th, 5th and 6th decades of life and is more prevalent among the females.
- Rapidly developing vesicle or bulla on several areas of skin and mucous membrane which contain clear fluid initially but later on there is formation of pus.
- Vesicle ruptures very soon and leaves painful, erythematous ulcers that bleed profusely.
- Gentle traction or oblique pressure on and affected area around the lesion causes stripping of the normal skin or mucous membrane which is known as “Nikolsky’s Sign”.
- Patient may die due to dehydration and septicemia.
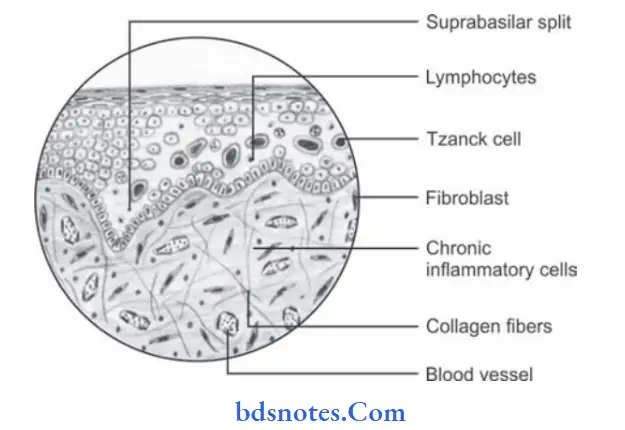
Histopathology Of Pemphigus
- Formation of vesicle or bulla within the epithelium that result in supra basilar split.
- Following the suprabasal split the basal cell layer remains attached to lamina propria and appears as row of “Tomb Stone”.
- Loss of intracellular bridges and collection of edema flid results in acantholysis within spinous cell layer which causes disruption of prickle cell layer.
- As result of acantholysis, clumps of large hyperchromatic epithelial cells lying free within the vesicular fluid, these desquamated cells are round and smooth in appearance and are known as Tzanck cells.
- Small number of PMNs and lymphocytes may be found.
Treatment Of Pemphigus
- High dose of steroids
- Immunosuppressive agents
- Antibiotics to prevent secondary infection.
- Fluid and electrolyte balance must be strictly maintained.
Question.3. Write short note on erythema multiforme.
Answer. Erythema multiforme is an acute inflammatory dermatological disorder that involves skin, mucous membrane,s and sometimes internal organs.
Etiology Of Erythema multiforme
- Infection: TB, herpes simplex.
- Drug hypersensitivity: Barbiturates, sulphonamides, salicylates.
- Hyperimmune reaction: Due to formation of antigen-antibody complex against submucosal and derma blood vessels.
Types Of Erythema multiforme
- EM minor or erythema multiforme minor.
It represents the localized eruption of skin with mild or no mucosal involvement. - EM major or erythema multiforme major or Steven Johnson syndrome (SJS)
It is more severe mucosal and skin disease and is potentially lifethreatening disorder.
Clinical Features Of Erythema multiforme
- It occurs between the age of 15 to 40 years and males are more commonly affected.
- Rapidly developing erythematous macules, papules, vesicle or bulla appear symmetrically over hand and arm, legs and feet, face and neck.
- Classical dermal lesions of erythema multiforme which often appear on extremities are called “Bull’s eye”.
- Vesicles of mucosal surface are short lived and become eroded or ulcerated and bleed profusely.
- Patient also develops tracheobronchial ulceration and pneumonia.
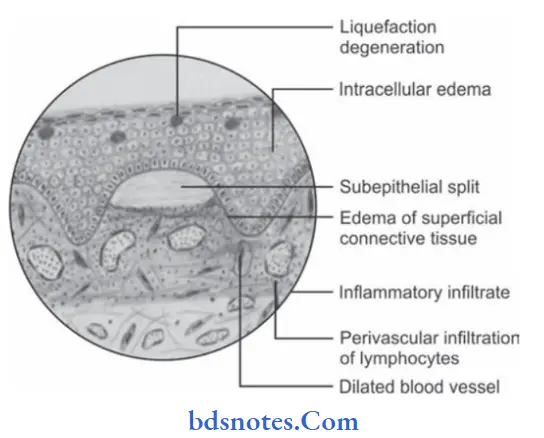
Histopathology Of Erythema multiforme
- It usually consists of acanthosis, intercellular or intracellular edema, and necrosis of epithelium.
- Vesicles may form within epithelium or at epithelial connective tissue junction.
- Subepithelial connective tissue shows edema and perivascular infiltration of lymphocytes and macrophages.
Treatment For Of Erythema multiforme
Topical and systemic steroid therapy coupled with antibiotic.
Question.4. Define premalignancy. Enumerate the premalignant lesions and conditions. Describe in detail lichen planus.
Answer. Premalignancy is an altered state of tissue which often has but not always has high potential to undergo malignant transformation.
Enumeration Of Premalignant Lesion
Premalignant lesion is defied as “A morphologically altered tissue in which cancer is more likely to occur than its apparently normal counterparts”. For example:
- Leukoplakia
- Erythroplakia
- Mucosal changes associated with smoking habits
- Carcinoma in situ
- Bowen disease
- Actinic keratosis, Actinic cheilitis and Actinic elastosis.
Enumeration Of Premalignant Condition
Premalignant condition is defied as “A generalized state or condition associated with significantly increased risk for cancer
development”. For example:
- Syphilis
- OSMF
- Oral lichen planus
- Sideropenic dysplasia
- Dyskeratosis congenita
- Lupus erythematosus.
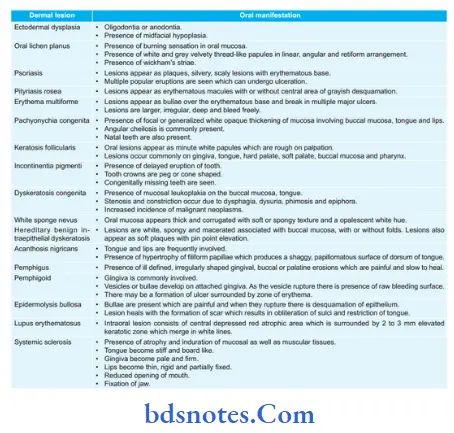
Question.5. Write short note on oral manifestations of hereditary ectodermal dysplasia.
Answer. Ectodermal dysplasia is a hereditary disorder characterized by defective formation of ectodermal structures, i.e. teeth, nail, sweat glands, sebaceous glands and hair follicles.
Oral Manifestations Of Ectodermal dysplasia
- Anodontia and oligodontia
- Frequent malformation of any teeth in both deciduous and permanent teeth. Incisors appear to be conical, tapered or pointed while molars look narrow.
- Salivary glands including intraoral accessory glands are sometimes hypoplastic in this disease which leads to xerostomia.
- Patient have pharyngitis with dysphagia and there is hoarseness of voice.
- Alveolar process does not develop in absence of teeth, there is a reduction from normal vertical dimension resulting in protuberant lips
- Palatal arch is high and at times patient exhibits cleft palate.
Question.6.Define vesicle and bulla. Describe in detail etiopathogenesis, clinical features, histopathology and investigations of pemphigus vulgaris.
Answer. Vesicle is defined as a superficial blister which is 5 mm or less in diameter and is usually filled with clear fluid.
Bulla is defined as a larger blister which is greater than 5 mm in diameter.
Pemphigus vulgaris is an autoimmune, intraepithelial blistering disease affecting the skin and mucous membrane and is mediated by circulating autoantibodies directed against keratinocyte cell surfaces.
Etiopathogenesis
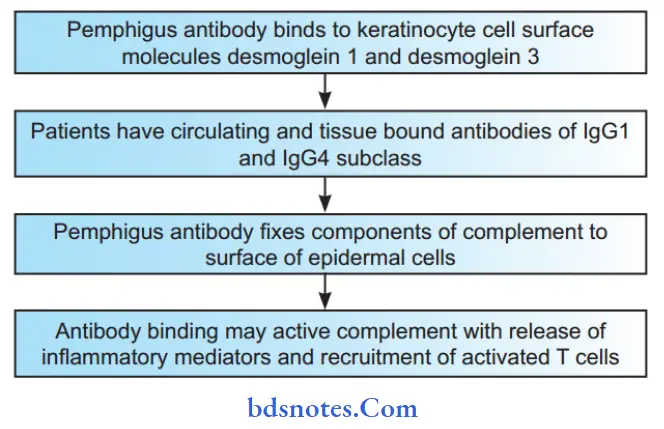
Protease Theory
According to protease theory deposition of autoantibody within the epithelium induces the proteolytic activity by activating tissue plasminogen.
This inturn generate proteolytic enzyme called plasmin which destroy desmosomes.
Investigations
- Incisional/punch biopsy of the involved area should be done and is histopathologically examined.
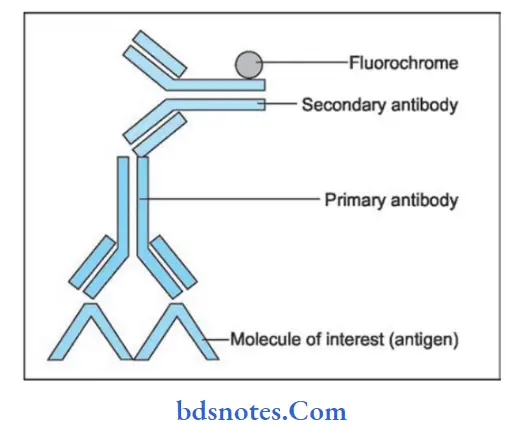
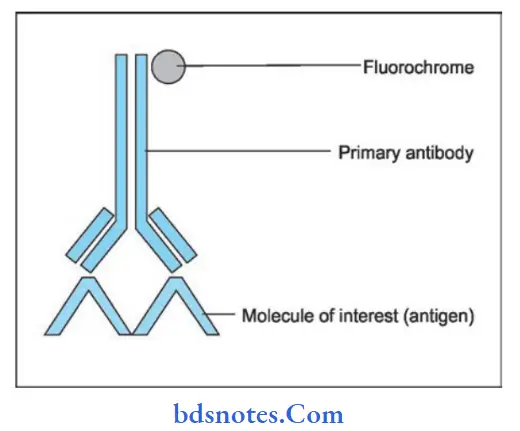
- Immunofluorescent testing: Direct immunofluorescence testing is done to demonstrate the presence of immunoglobulins, predominantly IgG but sometimes in combination with C3, IgA and IgM, in the intercellular spaces or intercellular substance in either oral epithelium or clinically normal epithelium adjacent to lesion.
- Indirect immunofluorescence: This is accomplished basically by incubating normal animal or human mucosa with serum from the patient suspected of having the disease and adding the fluorescein-conjugated human antiglobulin.
A positive reaction in the tissue indicates presence of circulating immunoglobulin antibodies.
Question.7. Enumerate the mucocutaneous lesions of oral cavity.
Describe in detail Pemphigus.
Or
Enumerate mucocutaneous lesions. Describe in detail Pemphigus.
Answer.
Mucocutaneous Lesions of Oral Cavity
Genodermatosis
- Darier’s disease
- White sponge nevus
- Hereditary benign intraepithelial dyskeratosis
- PeutzJeghers syndrome
- Pachyonychia congenita
- Dyskeratosis congenita
- Pseudoxanthoma elasticum
Non-infective Disease
- Vesicular
- Bullous pemphigoid
- Benign mucous membrane pemphigoid
- Pemphigus
- Erythema multiforme
- Lichen planus
- Epidermolysis bullosa
- NonVesicular
- Geographic Tongue
- Lichen planus
- Collagen Disorders
- Wegener’s granulomatosis
- Midline lethal granuloma
- Polyarteritis nodosa
- Scleroderma
- Lupus erythematosus
- Vasculitis
- Degenerative Disorder
- OSMF
- Amyloidosis
- Solar elastosis
- Pigmentation
- Anemia
- Albert syndrome
- Addison’s disease
- Racial pigmentation
- Endocrinopathy
Question.8. Write short note on Steven-Johnson syndrome.
Answer. StevenJohnson syndrome is a severe bullous form of erythema multiforme with widespread involvement typically including skin, oral cavity, eyes and genitalia.
- Skin lesions: The cutaneous lesions in this mucocutaneous ocular disease are those of erythema multiforme although they are commonly hemorrhagic and are often vesicular or bullous.
- Oral mucous membrane lesions: Lesions are extremely painful and severe.
Mucosal vesicles or bullae occur which rupture and leave surfaces covered with white or yellow exudates.
Erosions of pharynx are common. Lips may exhibit ulceration with bloody crusting and are painful. - Eye lesions: It consist of photophobia, conjunctivitis,corneal ulceration and panophthalmitis. Blindness may result.
- Genital lesions: There is non-specific urethritis, balanitis, vaginal ulcers.
Question.9. Write notes on discoid lupus erythematosus.
Answer. Discoid lupus erythematosus remain confined to the mucosa and skin.
Etiology
- Genetic susceptibility
- Autoimmune: Patient develops antibodies to their own cells.
- Endocrine: Common in pregnant ladies.
Clinical Features
- It is seen during 3rd and 4th decades of life.
- Female predilection is present with ratio of 5:1.
- Lesion appears as circumscribed slightly elevated white patch surrounded by erythematous halo.
- Skin lesions are slightly elevated. They are purple or red macules and are covered by gray or yellow scales.
- As removal of scale is done it result in carpet track extension.
There is presence of butterfly-shaped distribution over malar region at bridge of nose.
Oral Manifestations
- Tongue, buccal mucosa, vermilion border of lip are most common involved oral sites.
- Patient complains of burning and tenderness in the involved area.
- Lesion begin as erythematous area with induration and white spots. At times pain is felt in ulcerated area with crusting and bleeding. Scale formation is absent.
- Fine white striae are seen radiating from the margins.
- Lips show erythematous area which is surrounded by keratotic border.
Histopathology
- It is characterized by hyperkeratosis with keratotic plugging.
- There is presence of atrophy of rete pegs.
- Presence of liquefaction degeneration of basal layer of cells.
- Perivascular infiltration of lymphocytes is present and their collection at about dermal appendages.
- Basophilic degeneration of collagen and elastic fiers is present.
- Hyalinization is also seen.
- Edema and fibrinoid change is present beneath the epithelium.
Treatment
Corticosteroids along with immunosuppressant drugs is the choice.
Question.10.Describe in brief Tzanck cells.
Answer. Tzanck cell is a term given to a free flating epithelial cell in any intraepithelial vesicle.
Tzanck cells are seen in mainly two diseases, i.e.
1. Pemphigus vulgaris
2. Herpes simplex infection
Tzanck Cells In Pemphigus Vulgaris
Pemphigus consists of vesicle or bulla formation in spinous layer of epithelium just above basal cell layer which leads to suprabasilar split.
Prevesicular edema weaken intercellular junctions and intercellular bridges between epithelial cells break and the epithelial cells fell apart which is known as acantholysis, due to this clumps of epithelial cells found free on the vesicular space.
These loose cells are characterized by degenerative changes such as hyperchromatic staining and swelling of nuclei, cells become round in shape, these cells are known as tznck cells.
Tzanck Cells In Herpes Simplex Infection
Herpes simplex virus mainly affects the epithelial cells. Infected epithelial cells undergo ballooning degeneration and show following features such as acantholysis, nuclear clearing, and enlargement of nucleus.
These acantholytic epithelial cells are known as tznck cells.
Question.11. Write in detail on genodermatosis.
Answer. Genodermatoses are genetically determined skin conditions.
- Some of the genodermatoses are characterized particularly by alteration in normal keratinization process and are known as genokeratosis.
Following are the genodermatosis:
- Darier’s disease
- White sponge nevus
- Hereditary benign intraepithelial dyskeratosis
- PeutzJeghers syndrome
- Pachyonychia congenita
- Pseudoxanthoma elasticum
- Porokeratosis
- Warty dyskeratoma.
Darier’s Disease Of Genodermatoses
It is also known as keratosis follicularis.
Clinical Features Of Genodermatoses
- It occurs during childhood or in adults.
- Initially, there is presence of papules over the skin which is red in color later on they become purple brown or gray in color.
- Changes in nails are also seen such as splintering, longitudinal streaking and fisuring.
- White papule occurs in oral cavity over hard and soft palate, tongue and gingiva. It is rough on palpation.
Histopathology Of Genodermatoses
- Histopathology reveals hyperkeratosis, papillomatosis,acanthosis and benign dyskeratosis.
- Benign dyskeratosis show typical cells, i.e. corps ronds and grains
- Corps ronds: These cells are larger than normal squamous cells and have round homogeneous basophilic nucleus with dark eosinophilic cytoplasm and distinct cell membrane. They are seen in granular layer and superfiial spinous cell layer.
- Grains: Small, elongated, parakeratotic cells present in keratin layer.
White Sponge Nevus Of Genodermatoses
It is also known as Cannon’s disease.
Clinical Features Of Genodermatoses
- It occurs most commonly at birth and its intensity increases till puberty.
- It is seen on buccal mucosa, gingiva and palate.
- It appears as thick, corrugated, soft textured, white opalescent line.
- White or keratotic area could be removed by rubbing and normal looking epithelium is seen.
Histopathology Of Genodermatoses
- Histopathologically epithelium shows hyper parakeratosis and acanthosis.
- Cells of spinous layer show intracellular edema.
- Parakeratin plugging is seen which is projecting deep in spinous cell layer.
Hereditary benign intraepithelial Dyskeratosis
- It is also known as Witkop-Von Sallmann syndrome.
Clinical Features
- It occurs commonly in children.
- Most commonly it involves eyes. In oral cavity it is seen in flor of mouth, buccal mucosa, tongue and palate.
- It appears as spongy, white macerated area.
Histopathology
Histologically thick epithelium is seen with hydropic degeneration.
Dyskeratotic cells are seen, i.e. round, eosinophilic, waxy appearing cells are seen.
Peutz-Jeghers Syndrome
It is also known as hereditary intestinal polyposis syndrome.
Features
In it there is pigmentation of face and oral cavity.
Adenocarcinoma can occur in gastric, duodenum, and colon.
Histopathology
Histologically acanthosis of epithelium is seen with elongation of rete ridges.
Pachyonychia Congenita
It is also known as JadassohnLewandowsky syndrome.
Clinical Features
- It occur in neonates.
- It is seen on nails, palms, hands and feet.
- There is thickening of nail present, thickening increase toward free border of nail bed and get filled with yellow keratotic debris which leads to the projection of nail upward at free border.
- Hairs are sparse and corneal dyskeratosis is seen.
- Bullae are seen over the feet.
Histopathology
Histopathology of skin and mucous membrane showing acanthosis, parakeratosis and hyperkeratosis.
Pseudoxanthoma Elasticum
It leads to the degeneration of elastic fiers and make them susceptible for calcium.
Clinical Features
- It occurs at age of 13 years.
- Yellow papules are seen over the skin near neck, mouth, axilla.
- Skin surrounding the mouth give hound dog appearance.
- Lower lip is affected inside oral cavity.
Porokeratosis
It is also known as Mibelli’s disease.
Clinical Features
- This disease occurs in childhood.
- Male predilection is present.
- It is seen commonly in face, neck, extremities and genitalia.
- Lesion appear as crateriform keratotic papule which later on form elevated plaque.
- Plaque from it margins is surrounded by raised border of epidermis.
- Nails of patient get thick and ridged.
- In oral cavity lesion is seen in upper lip and palate.
Histopathology
- Histologically elevated horny margin of the lesion show hyperkeratosis and acanthosis with deep groove filed with parakeratin and absence of underlying granular layer. This forms cornoid lamella.
- Central portion of the lesion show epithelial atrophy.
Warty Dyskeratoma
It is also known as isolated Darier’s disease.
Clinical Features
- The disease occur in older age.
- Male predilection is present.
- Lesions are seen on scalp, neck, face and over the upper part of chest.
- Lesion present as elevated nodule which is umblicated.
- Borders of lesion are raised.
- Color of lesion is not specifi and it varies from brown or yellow to black or grey.
- Orally lesion occurs very rarely and if present it can be seen as whitish area with central depression over it.
Histopathology
- Histopathologically intraoral lesions show central orthokeratin or parakeratin core below which epithelium show suprabasilar separation which result in cleft like space having acantholytic and dyskeratotic cells.
- Connective tissue papillae have single layer of basal cells.
- Underlying connective tissue show non-specific chronic inflammatory infiltrate.
Question.12. Write in brief on ectodermal dysplasia.
Answer. Term ectodermal dysplasia is a group of inherited diseases in which two or more ectodermal structures fails to develop.
- Disease can be autosomal dominant or autosomal recessive or it can be Xlinked too.
- Most common ectodermal dysplasia is hereditary hypohidrotic ectodermal dysplasia.
Clinical Features Of Ectodermal Dysplasia
- Male predominance is seen.
- Patient is characterized by hypotrichosis, hypohydrosis and at times anhydrosis.
- Patient has characteristic saddle nose.
- Fine and sparse hair are seen on eyebrows and eyelashes
- Periocular skin has fie wrinkles with hyperpigmentation.
- Frontal bossing is commonly present.
- Nails appear dystrophic and britte.
- Skin of the patient remains dry and there is absence or partial presence of sweat glands. Due to this patient cannot perspire and his heat regulation is disturbed which lead to increased temperature of patient.
Histopathology Of Ectodermal Dysplasia
Histopathology of skin reveals following features:
- There is reduction in number of sweat glands, hair follicles and sebaceous glands.
- Epidermis is thin and flattened.
- Eccrine sweat glands are few or poorly developed.
- In oral histopathology, salivary glands show ectasia of ducts and inflammatory changes.
Treatment Of Ectodermal Dysplasia
- Condition is genetic so it is noncurable.
- Prosthetic rehabilitation of patient should be done by complete dentures, RPDs or fied dentures.
- Dental implants can also be considered.
Question.13.Write short note on CREST syndrome.
Answer. It is considered to be a mild variant of systemic sclerosis.
The term CREST is an acronym for:
C Calcinosis Cutis
R- Raynaud’s phenomenon
E Esophageal dysfunction
S Sclerodactyly
T Telangiectasia.
Clinical Features Of CREST
- Female predilection is present.
- It most commonly occurs during sixth or seventh decades of life.
- Signs of the disease develop from months to years.
- Calcinosis cutis: It is characterized by deposition of calcium beneath the skin in form of nodules which are 0.5 to 2 cm in size and are movable, multiple and are nontender.
- Raynaud’s phenomenon: It is seen when patient’s hand or feet are exposed to cold.
Characteristic clinical sign is blanching of digits which appear whitish in color because of vasospasm.
After few minutes extremity become blue in color because of venous stasis.
As area get warm it gives duskyred hue which indicates of return of hyperemic blood flow.
With all this presence of throbbing pain is there. - Esophageal dysfunction: It is present because of deposition of abnormal collagen in esophageal submucosa.
- Sclerodactyly: In this fingers get stiff skin becomes smooth and shiny.
- Flexure of fingers occurs resulting in claw deformity.
- Telangiectasia: In this bleeding from superficial dilated vessels is seen.
Question.14.Write short note on direct and indirect immunofluorescence.
Answer. Direct and indirect immunofluorescence are the techniques which are used to detect immune-mediated or immunobullous diseases.
Direct immunofluorescence
It is the diagnostic method which is used for detection of autoantibodies which are bound to patient’s tissue.
Method
- Frozen section of patient’s tissue is placed over a slide.
- Tissue is incubated with fluoresceinconjugated goat antihuman antibodies.
- Antibodies bind to the human immunoglobulin site.
- Excess of antibodies are washed with buffred normal saline.
- Section is viewed under ultraviolet microscope.
Indirect Immunofluorescence
It is the diagnostic method which is used for detection of antibodies which are present in blood.
Method
- Frozen section of monkey’s esophagus is placed over a slide and is incubated with patient’s serum.
- Excess serum is washed off
- Apply fluorescent conjugated anti-human Ig antibodies.
- Wash of excess antibody.
- Section is viewed under ultraviolet microscope.
Question.15. Describe etiopathogenesis of lichen planus.
Answer. Following are the etiopathogenesis of lichen planus:
- Oral lichen planus is a T cell-mediated autoimmune disease in which cytotoxic CD8 + T cells trigger the apoptosis of oral epithelial cells.
The CD8 + lesional T cells may recognize the antigen associated with major histocompatibility complex (MHC) class I on keratinocytes.
After antigen recognition and activation, CD8 + cytotoxic T cells may trigger keratinocyte apoptosis.
Activated CD8 + T Cells may release cytokines that attract additional lymphocytes. - As per the recent studies in psychoneuroimmunology psychosomatic stress results in the autoimmunity reactions and this leads to lichen planus.
Question.16. What are vesiculobullous lesions. Describe in detail pemphigus.
Answer. Vesicles are the superficial blisters which are 5 mm or less in diameter and are usually filled with clear fluids.
Bulla is a large blister which is greater than 5 mm in diameter.
The lesions which consist of vesicles or bullae are known as vesiculobullous lesions.
Question 17. Enumerate dermal lesions with oral manifestation.
Describe systemic lupus erythematosus in detail.
Or
Enumerate the dermal diseases with oral manifestation.
Describe the etiology, clinical and histopathological features of systemic lupus erythematosus in detail with diagram. Give its treatment plan.
Answer. Enumeration of dermal lesions with oral manifestations
Systemic lupus erythematosus
It is an autoimmune disease which is characterized by autoantibodies, immune complex formation as well as dysregulation of immune system which causes damage to any organ of body.
Etiology Of Lupus Erythematosus
- Genetic predisposition: Higher incidence of autoantibodies is seen in blood relations of patient.
- Viral infection
- Hormones, i.e. increase estrogen level in pregnancy.
- Autoimmune: Antibodies are developed towards one’s own body cells.
Pathogenesis Of Lupus Erythematosus
Antibodies are produced in reaction to exposure of normally unexposed self-antigens.
Dysregulation of immune system leads to excessive production of antibodies against DNA, ribosomes,other nuclear antigens, platelet, erythrocytes, leucocytes and various tissue specifi antigens which causes tissue damage.
Clinical Features Of Lupus Erythematosus
- It occurs during 30 years of age in females and 40 years of age in males.
- Female predilection is seen. Female to male ratio is 2:1
- Most common sites affected are face, neck, upper arm,shoulders. Disease is characterized by repeated remission and exacerbations over these sites.
- Patient complained of pain and fever in joints and muscles.
Itching or burning sensation is also present along with the areas of hyperpigmentation. Symptoms aggravate under exposure to sunlight. - The characteristic sign of the disease is presence of erythematous patches over the face which coalesce to form roughly symmetrical pattern over the cheeks and across the bridge of nose, this is known as butterfly distribution. In the kidney fibrinoid thickening of glomerular capillaries produces characteristic wire loops, this leads to renal insufficiency.
- In the heart there is presence of typical endocarditis involving valves along with fibrinoid degeneration of epicardium and myocardium.
Oral Manifestations Of Lupus Erythematosus
- Buccal mucosa, lip, and palate are most commonly affected.
- Patient complaints of presence of burning sensation in the mouth. Xerostomia is also seen.
- Lesions have very much similarity to lesions of discoid lupus except that they are hyperemic, edematous and extension of lesion is pronounced. Tendency for bleeding and petechiae is more as well as superfiial ulcerations surrounded by red halo are also present.
- Intraoral lesion consists of central depressed red atrophic area which is surrounded by 2 to 3 mm elevated keratotic zone which merge in white lines.
Histopathology Of Lupus Erythematosus
- In systemic lupus erythematosus, areas of epithelial atrophy are present with absence of keratinization.
- There is presence of liquefactive degeneration of basal cell layer.
- There is presence of edema of subepithelial connective tissue with dilatation of vessels.
- In systemic lupus erythematosus degenerative areas and collagen disturbances are more prominent.
- Inflammatory features are less common.
Laboratory Findings Of Lupus Erythematosus
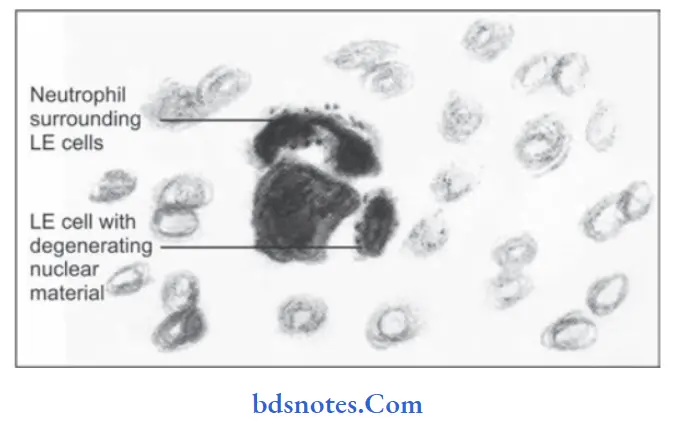
- LE cell inclusion phenomenon is used in which there is addition of blood serum from a person who is suspected to the buff coat of normal blood.
If patient is suffering from systemic lupus erythematosus, typical LE cells will appear. The test consists of rosett of neutrophils surrounding pale nuclear mass. - There is also presence of anemia, leucopenia, thrombocytopenia and elevated ESR and serum gamma globulin level with positive Coombs test.
- Lupus band test is positive, i.e. there is deposition of IgG, IgM or complement component at epidermal dermal junction or basement membrane zone of skin.
Treatment Of Lupus Erythematosus
- Exposure to sunlight should be avoided.
- Patient should be kept on systemic corticosteroid therapy.
- NSAIDs should also be given to combat the symptoms.
Question.18. Describe pathogenesis, clinical manifestations, and histopathological features of oral lichen planus.
Answer. Pathogenesis
- Oral lichen planus is a T cell-mediated autoimmune disease in which cytotoxic CD8 + T cells trigger the apoptosis of oral epithelial cells.
The CD8 + lesional T cells may recognize the antigen associated with major histocompatibility complex (MHC) class I on keratinocytes.
After antigen recognition and activation, CD8 + cytotoxic T cells may trigger keratinocyte apoptosis.
Activated CD8 + T Cells may release cytokines that attract additional lymphocytes. - As per the recent studies in pschyoneuro-immunology, psychosomatic stress results in the autoimmunity reactions and this leads to lichen planus.

Leave a Reply