Diseases Of Cardiovascular System
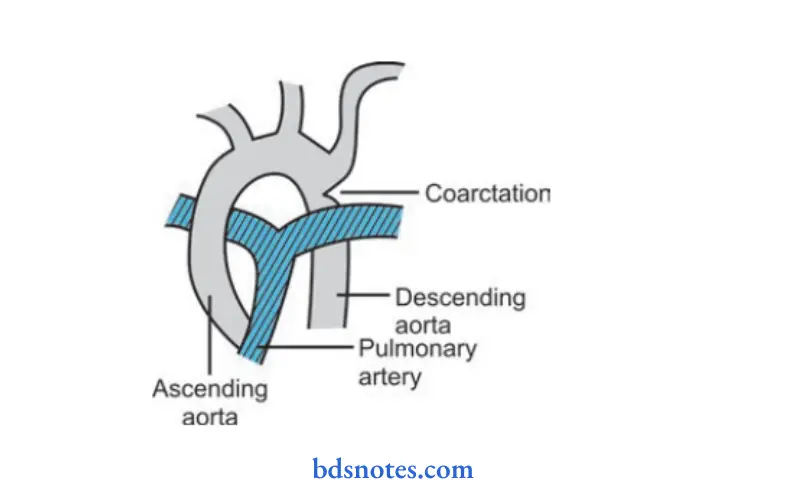
Question.1. Write short note on coarctation of aorta.
Answer. Coarctation of aorta is defied as the narrowing of aorta at or distal to the subclavian artery.
Clinical Features Coarctation Of Aorta.
- In uncomplicated cases the onlysymptoms are *intermittent claudication, pain, weakness and dyspnea on running.
- Headache and nose bleed
- Hypertension in upper limb
- Physical examination shows weak or impalpable femorals in comparison to strong radial acting pulsation.
- Heart size remains normal with left ventricular forcible apex.
- On auscultation:
- S1 is accentuated
- S2 normal splittng delayed A2
- S3 with left ventricular filing
- S4 with hypertension.
Read And Learn More: General Medicine Question And Answers
Investigation Coarctation Of Aorta.
- ECG: It shows left axis deviation representing left ventricular failure.
- X-ray: Normal sized heart with prominent ascending aorta.
- Barium swallow shows characteristic E sign.
- Aortography: Show usually short narrow segment.
Treatment Coarctation Of Aorta.
- Medical management consists of control of congestive cardiac failure in infancy.
- Defiitive management is operative.
- Operation can be done at any age, but lowest risk is between 1–10 years.
- Resection of narrow segment is done in operation.
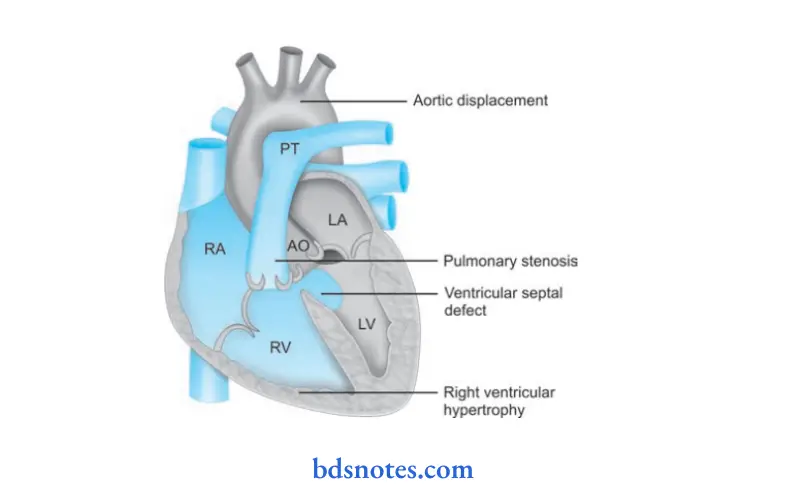
Question 2. Write short note on tetralogy of Fallot.
Answer. It is the commonest cyanotic congenital heart disease in children above the age of 2 years.
It is characterized by four constituents:
- Ventricular septal defect.
- Pulmonary stenosis
- Overriding or dextroposed aorta
- Right ventricular hypertrophy.
Clinical Features tetralogy of Fallot.
- The chief complaint is development of *anoxic spells. The anoxic spells are dangerous for children and can occur many times.
- It occurs prominently after walking up or following exertion.
- Children start crying, become dyspneic, blue than before and may loose consciousness. Convulsions may occur.
- Frequency varies from once in a few days to numerous attcks everyday.
- Each spell is lifethreatening.
Physical signs tetralogy of Fallot.
- Cyanosis
- Clubbing of figer and toes
- Growth is stunted
- Ejection systolic murmur is present at pulmonary area.
- ECG may show right ventricular hypertrophy
- Second sound may show delayed splittng
- In Xray chest boot shaped heart is seen
- Echocardiography shows that aorta is not juxtaposed with intraventricular septum.
Complications tetralogy of Fallot.
- Syncope
- Cerebral abscess
- Stroke due to cerebral thrombosis
- Subacute infective endocarditis
- Sudden death
Treatment tetralogy of Fallot.
It is divided into two stages:
1. Management of anoxic spells
2. Defiitive treatment.
Management of anoxic spells tetralogy of Fallot.
- Knee chest position
- Humidifid oxygen / moist oxygen
- Morphine: 0.1 to 0.2 mg / kg subcutaneous inj.
- Correction of acidosis if pH < 7.1 by giving sodium bicarbonate IV
- Propranolol 0.1 gm / kg IV during spells and then 0.5 to 1
mg / kg 4 to 6 hourly orally. - Vasopressor: Methoxamine IM or IV
- Correct anemia
- Consider operation.
Defiitive Treatment tetralogy of Fallot.
It is operative. Operative treatment is of two varieties, i.e.
papillative and defiitive.
Question 3. Outline the management of congestive cardiac failure.
Answer. The management of cardiac failure aims to restore balance between metabolic demands of the body and person heart’s ability to meet these demands.
- Rest: Complete bed rest is the key stone of management. When the patient is dyspneic, bed rest is given with the head end of bed raised to 45°.
The legs should be kept below the pelvis to prevent the flid present in legs to return to vascular system and precipitate pulmonary edema. - Diet: Basic aim is to restrict sodium in the diet.
Quantity of salt intake per day should not exceed 0.5 gm.
Salt substitutes may be used to make diet more palatable. - Diuretics: In cardiac failure there is always sodium and water retention.
Hence, diuretics are given to increase sodium extraction.
Furosemide 40 to 80 mg orally produces effct in 4 to 6 hours and on IV administration of furosemide 40 to 100 mg produces its effct in 20 minutes. Spironolactone which is potassium sparing diuretic is given 25 mg orally 4 times a day which removes the symptoms like hypokalemia due to action of furosemide.
Triamterene or amiloride hydrochloride is given along with spironolactone. - Digitalis: It increases the force of myocardial contraction and decreases work of heart.
The commonly used drug is digoxin which is administered orally 0.25 mg BD.
For rapid digitalization digoxin 0.5–0.75 mg is given slow IV over a period of 5 to 10 minutes under electrocardiographic control. - Sympathomimetic amines: Dopamine at low doses of 3 to 5 μg / kg / min increases contractility of heart.
- Vasodilators: Sodium nitroprusside in the dose of 5 to 10 μg / min have balance dilator effct.
Besides this hydralazine, nitrates and ACE inhibitors are used. - Inodilator levosimendan: This is a calcium channel sensitizer. It has positive inotropic and vasodilator effct.
It is given IV with loading dose of 6–12µg/kg/ min over 10 min followed by infusion 0.05 to 2 µg/ kg/min infusion. - Oxygen: It is given via Woulfe’s botte at rate of 5 to 8 lts/min.
Miscellaneous drugs: Tranquilizers such as diazepam 2 to 5 mg TDS are given to reduce anxiety. - Cardiac re-synchronization therapy or biventricular pacing: It is used in patients with symptomatic refractory cardiac failure with conduction abnormality or left bundle branch block.
This therapy involves pacing the right atrium, right ventricle and left ventricle to improve synchrony of the cardiac chambers. - Left ventricular assist device: Devices such as intraaortic balloon pump, impella device, heartmate, thoratic are considered when medical management fails.
They are usually used as a bridge to cardiac transplant.
Question 4. Describe the management of acute left ventricular failure.
Answer.
Management Acute Left Ventricular Failure.
First aim of treatment is to fid and remove the precipitating cause, i.e. arrhythmia or an intercurrent infection.
- Patient should be kept in sitting position, with legs hanging along side of the bed, i.e. upright posture should be maintained.
- Diet: Salt free diet is given till left ventricular failure improves and later on restricted salt diet is given.
- Sedatives: Morphine should be given in doses of 5 to 10 mg along with an antiemetic, i.e. metaclopramide 10mg I.V. and repeat the drug as soon as desired.
- Oxygen: About 60% of oxygen is given by facemask under positive pressure. It should be given as 6 to 8 L/min through Wolfe’s botte.
- Loop diuretics: Furosemide 40 to 100 mg IV should be given.
- IV sodium nitroprusside 20 to 30µg/min or IV nitroglycerin should be given in patients whose systolic blood pressure is more than 100 mm Hg.
Digitalis: If digoxin is not used previously, the three fourth of full dose, i.e. 0.5 to 1mg is given as IV dose. - Bronchodilators: Attmes aminophylline or theophylline in dose of 250 to 500 mg I.V. decreases brochoconstriction.
- In cases of severe left ventricular failure inotropes can be given.
- If all the above measures failed then rotating tourniquet should be applied to extremities.
- Intra-aortic balloon counterpulsation: It is used in acute left ventricular failure during cardiac procedures or cardiac repairs.
Question 5. Outline the management of essential hypertension.
Or
Describe briefl management of hypertension.
Answer.
Management systemic hypertension.
Nonpharmacological treatment
1. Salt restriction: Modest sodium restriction 2.4 gm sodium or 6 gm NaCl is effctive in controlling hypertension.
2. Weight reduction: In overweight persons, reduction of 1 kg may reduce 1.6 to 1.3 mm Hg of blood pressure
3. Stop smoking: Smoking raises BP. It is an independent and most important reversible coronary risk factor.
4. Diet:
Lactovegetarian diet and high intake of poly unsaturated fih oils have high potassium levels and lower blood pressure by:
- Increased sodium extraction
- Decreased sympathetic activity
- Decreased renninangiotensin secretion and direct dilatation of removal of renal arteries
- Adequate calcium and magnesium intake should be maintained in diet
5. Limit of alcohol intake is done
6. Various forms of relaxation like yoga, biofeedback and psychotherapy lower the blood pressure
7. Regular exercise, relaxation exercise.
Pharmacological therapy
1. Diuretics: Commonly used diuretics are hydrochlorothiazide 100 mg per day, chlorthalidone 50–100 mg/day.
The reduced potassium levels in body results in hypokalemia, potassium supplements have to be given in people on longterm diuretic therapy.
Potassium sparing diuretics, i.e. spironolactone 25 mg TDS is given.
2. Beta-blockers: Propranolol was used extensively as effctive antihypertensive drug. The dose administered as 40–160 mg/day.
3. Calcium channel blockers: Nifedipine 16 to 20 mg BD is administered. Side effects are headache, dizziness, flshing.
Drug is contraindicated in acute myocardial infarction, cardiogenic shock, pregnancy and is used with caution in diabetics and edema.
Felodipine sulfate 5 to 10 mg/day is effctive in mild to moderate hypertension.
Amlodipine 5 to 10 gm is effective and is safe in hypertensives.
4. ACE inhibitors:
- Enalapril maleate 5 mg OD is given.
- Captopril in combination with diuretics or a betablocker. 25 gm TDS of captopril is administered. It is considered safe in asthmatics and diabetics.
- Ramipril 2.5 mg daily is used to reduce hypertension.
5. Alpha-1 adrenergic blockers: Prazosin is commonly used drug. Dose is 0.5 mg TDS.
6. Vasodilators: Diazoxide and sodium nitroprusside are given as IV dosage.
Question 6. Describe briefly management of acute myocardial infarction.
Or
Outline the management of acute myocardial infarction.
Answer. The management of myocardial infarction is divided into two parts:
1. Early management.
2. Late management.
Early Management acute myocardial infarction.
- Aspirin 150–300 mg to be chewed earliest.
- Sublingual glyceryl trinitrate 0.4–1 mg, to be repeated, if necessary
- Oxygen through nasal cannula at a rate of 2–4 L/min.
- Procure IV line and take blood samples for glucose, lipids and complete haemogram.
- Record 12lead ECG.
- Pain may be relieved by IV morphine (5 mg) plus metoclopramide as an antimetic (10 mg).
- IV betablockers (metoprolol 5 mg every 2–5 minutes for 3 doses) for ongoing chest pain, hypertension and tachycardia provided there is no contraindication.
- Thrombolysis should be done.
- If PTCA is planned, give GP IIb/IIIa inhibitor
- After admission immediately shift the patient to ICU or
ICCU
In Hospital treatment acute myocardial infarction.
Hospitalization and strict Bed rest
- Hospitalize the patient and advice strict bed rest. As early as the patient is hospitalized, the bettr it is.
- Patient should be strictly admittd in ICCU.
Analgesia acute myocardial infarction.
- IV morphine sulphate 10 mg and an anti emetic, i.e. cyclizine 50 mg is given through I.V. cannula.
- The drug is repeated depending on the response till complete analgesia is received and patient feels bettr.
Anti-platelet drugs acute myocardial infarction.
Low dose aspirin, i.e. 75 to 150 mg and clopidogrel 300 mg stat and then 75 mg orally daily is given.
Oxygen therapy acute myocardial infarction.
Inhalation of oxygen increases arterial partial pressure of oxygen, so there is increase in the concentration of oxygen gradient which is responsible for diffusionn of oxygen in ischemic myocardium from adjacent better perfused areas. This is given by facemask or nasal prongs for a day or two after infarction.
Thrombolysis acute myocardial infarction.
- Coronary thrombolysis helps to restore patency of coronary artery preserves left ventricular function and improves survival.
- The choice of drug for thrombolysis is less important than the speed of treatment.
- Streptokinase, 1.5 million units in 100 mL of saline given in an intravenous infusion over 1 hour, is a widely accepted method.
It is a cheap, but being antigenic, sometimes, may cause serious allergic manifestations.
Hence, it can be used once and therapy is changed if the patient requires second thrombolysis within few years.
Alteplase (tissue Plasminagen activator (tPa)
- It is a potent firinolytic drug but is expensive.
- It is less antigenic and does not cause hypotension.
- The current tPA regimen given over 90 minutes (bolus dose of 15 mg followed by 50 mg over 30 minutes and then 35 mg over next 60 minutes) is widely accepted. The other drugs include reteplase given in double dose regime i.e.
10 million units over 2–3 minute followed by another dose of 10 million units after 30 minutes.
Tenectaplase given as bolus dose of 53 mg/kg over 10 seconds. Both reteplase and tenectaplase are known as bolus firinolytics.
Angioplasty
Immediate angioplasty of infarct related artery is safe and is effctive alternative to thrombolysis. It is done in the patients in whom the hazards of thrombolysis is high.
Anti-coagulants
- Subcutaneous heparin, i.e. 7,500 units twice a day for 7–10 days or till discharge of patient from the hospital can be employed.
In patients who do not receive thrombolytic therapy to prevent venous thrombosis. - Patients who receive thrombolytic therapy (tPA) should receive immediate and full doses of heparin (10,000 U bolus plus, l000 U hourly).
Beta-adrenergic Blockers
Acute betaadrenoreceptors blockade intravenous atenolol (5–l0 mg given over 5 minutes) or metoprolol (5–15 mg given over 5 minutes) relieves pain, reduces arrhythmias, salvages myocardium and improves short term mortality in patients who present within l2 hours of onset of pain.
Nitrates and other agents
Sublingual glyceryl trinitrate 0.4 mg is useful in threatened infarction.
Sedatives
Diazepam 5mg for three to four times a day is effctive. It is given for few days.
Diet
- For fist 4 to 5 days low calorie diet which is divided into multiple meals is given.
- If heart failure is present restrict the salt.
- From second week, food should be increased in amount.
Lipid lowering agent
Atorvastatin is given to reduce the LDL levels.
Late Management acute myocardial infarction.
1. Risk stratifiation and further investigations: Prognosis of patient survived after myocardial infarction depends on degree of myocardial damage, any residual ischemia and presence of ventricular arrhythmias.
2. Life style modifiation:
- Stop smoking
- Diet control
- Regular exercise.
3. Secondary prevention
- Antiplatelet agents, i.e. aspirin
- Lipid lowering agents
- Betablockers and ACEI in congestive cardiac failure and hypertension.
- Control of blood sugar in diabetes.
4. Rehabilitation and after care:
- Physical activities should be restricted for 4 to 6 weeks since infarct takes 4–6 weeks to become replaced with firous tissue.
- Gradual mobilization and return to work over 6 weeks.
When there are complications, the regimen has to be modifid accordingly. - Exercise within the limits set by angina and tiredness will do no harm but much good. Same limits apply to sexual activity.
- Control of obesity, regular exercises, cessation of smoking, adoption of a less frenetic way of life and control of plasma lipids by diets and drugs.
- Complications should be managed. Pain relief, reassurance, rest and correction of hypokalemia play a major role in prevention of arrhythmias.
Routine drug therapy acute myocardial infarction.
- Low dose aspirin, i.e. 75 to 150 mg daily and is continued indefiitely.
- Beta-adrenergic blocker should be given for 4 to 6 weeks if there is no contraindication.
- ACE inhibitor, i.e. captopril 25 mg TID or ramipril 2.5 to 5 mg BD
- Lipid lowering agent atorvastatin is given to lower the LDL levels.
Question 7. Enumerate the complications and outline the management of acute myocardial infarction.
Answer.
Enumeration of complications of Myocardial Infarction
1. Immediate
1. Arrhythmias and conduction disturbances
- Sinus bradycardia
- Ventricular ectopics
- Ventricular tachycardia
- Ventricular firillation
- Idioventricular rhythm
- Atrial firillation
- Heart block
2. Post-myocardial angina can occur in 50% patients occur.
3. Acute circulatory failure.
4. Pericarditis
5. Mechanical complications include:
- Papillary muscle dysfunction or rupture
- Rupture of interventricular septum
- Rupture of ventricle
6. Mural thrombosis and embolism
7. Sudden death
2. Late complications:
- Postmyocardial infarction syndrome (Dressler’s syndrome)
- Ventricular aneurysm.
Management acute myocardial infarction.
The management of myocardial infarction is divided into two parts:
1. Early management.
2. Late management.
Early Management acute myocardial infarction.
- Aspirin 150–300 mg to be chewed earliest.
- Sublingual glyceryl trinitrate 0.4–1 mg, to be repeated, if necessary
- Oxygen through nasal cannula at a rate of 2–4 L/min.
- Procure IV line and take blood samples for glucose, lipids and complete haemogram.
- Record 12lead ECG.
- Pain may be relieved by IV morphine (5 mg) plus metoclopramide as an antimetic (10 mg).
- IV betablockers (metoprolol 5 mg every 2–5 minutes for 3 doses) for ongoing chest pain, hypertension and tachycardia provided there is no contraindication.
- Thrombolysis should be done.
- If PTCA is planned, give GP IIb/IIIa inhibitor
- After admission immediately shift the patient to ICU or
ICCU
In Hospital treatment
Hospitalization and strict Bed rest
- Hospitalize the patient and advice strict bed rest. As early as the patient is hospitalized, the bettr it is.
- Patient should be strictly admittd in ICCU.
Analgesia
- IV morphine sulphate 10 mg and an anti emetic, i.e. cyclizine 50 mg is given through I.V. cannula.
- The drug is repeated depending on the response till complete analgesia is received and patient feels bettr.
Anti-platelet drugs
Low dose aspirin, i.e. 75 to 150 mg and clopidogrel 300 mg stat and then 75 mg orally daily is given.
Oxygen therapy
Inhalation of oxygen increases arterial partial pressure of oxygen, so there is increase in the concentration of oxygen gradient which is responsible for diffusionn of oxygen in ischemic myocardium from adjacent better perfused areas. This is given by facemask or nasal prongs for a day or two after infarction.
Thrombolysis
- Coronary thrombolysis helps to restore patency of coronary artery preserves left ventricular function and improves survival.
- The choice of drug for thrombolysis is less important than the speed of treatment.
- Streptokinase, 1.5 million units in 100 mL of saline given in an intravenous infusion over 1 hour, is a widely accepted method.
It is a cheap, but being antigenic, sometimes, may cause serious allergic manifestations.
Hence, it can be used once and therapy is changed if the patient requires second thrombolysis within few years.
Alteplase (tissue Plasminagen activator (tPa)
- It is a potent firinolytic drug but is expensive.
- It is less antigenic and does not cause hypotension.
- The current tPA regimen given over 90 minutes (bolus dose of 15 mg followed by 50 mg over 30 minutes and then 35 mg over next 60 minutes) is widely accepted. The other drugs include reteplase given in double dose regime i.e.
10 million units over 2–3 minute followed by another dose of 10 million units after 30 minutes.
Tenectaplase given as bolus dose of 53 mg/kg over 10 seconds. Both reteplase and tenectaplase are known as bolus firinolytics.
Angioplasty
Immediate angioplasty of infarct related artery is safe and is effctive alternative to thrombolysis. It is done in the patients in whom the hazards of thrombolysis is high.
Anti-coagulants
- Subcutaneous heparin, i.e. 7,500 units twice a day for 7–10 days or till discharge of patient from the hospital can be employed.
In patients who do not receive thrombolytic therapy to prevent venous thrombosis. - Patients who receive thrombolytic therapy (tPA) should receive immediate and full doses of heparin (10,000 U bolus plus, l000 U hourly).
Beta-adrenergic Blockers
Acute betaadrenoreceptors blockade intravenous atenolol (5–l0 mg given over 5 minutes) or metoprolol (5–15 mg given over 5 minutes) relieves pain, reduces arrhythmias, salvages myocardium and improves short term mortality in patients who present within l2 hours of onset of pain.
Nitrates and other agents
Sublingual glyceryl trinitrate 0.4 mg is useful in threatened infarction.
Sedatives
Diazepam 5mg for three to four times a day is effctive. It is given for few days.
Diet
- For fist 4 to 5 days low calorie diet which is divided into multiple meals is given.
- If heart failure is present restrict the salt.
- From second week, food should be increased in amount.
Lipid lowering agent
Atorvastatin is given to reduce the LDL levels.
Late Management
1. Risk stratifiation and further investigations: Prognosis of patient survived after myocardial infarction depends on degree of myocardial damage, any residual ischemia and presence of ventricular arrhythmias.
2. Life style modifiation:
- Stop smoking
- Diet control
- Regular exercise.
3. Secondary prevention
- Antiplatelet agents, i.e. aspirin
- Lipid lowering agents
- Betablockers and ACEI in congestive cardiac failure and hypertension.
- Control of blood sugar in diabetes.
4. Rehabilitation and after care:
- Physical activities should be restricted for 4 to 6 weeks since infarct takes 4–6 weeks to become replaced with firous tissue.
- Gradual mobilization and return to work over 6 weeks.
When there are complications, the regimen has to be modifid accordingly. - Exercise within the limits set by angina and tiredness will do no harm but much good. Same limits apply to sexual activity.
- Control of obesity, regular exercises, cessation of smoking, adoption of a less frenetic way of life and control of plasma lipids by diets and drugs.
- Complications should be managed. Pain relief, reassurance, rest and correction of hypokalemia play a major role in prevention of arrhythmias.
Routine drug therapy
- Low dose aspirin, i.e. 75 to 150 mg daily and is continued indefiitely.
- Beta-adrenergic blocker should be given for 4 to 6 weeks if there is no contraindication.
- ACE inhibitor, i.e. captopril 25 mg TID or ramipril 2.5 to 5 mg BD
- Lipid lowering agent atorvastatin is given to lower the LDL levels.
Question 8. Describe the clinical features, diagnosis and treatment of acute myocardial infarction.
Or
Describe the clinical features of acute myocardial infarction.
Answer. Acute myocardial infarction is defied as irreversible damage to myocardium of heart as a result of occlusive thrombus due to rupture of atherosclerotic plaque in coronary artery.
Clinical Features acute myocardial infarction.
Symptoms: acute myocardial infarction.
- Pain: Chest pain is more common and is severe in comparison to angina.
Pain is severe with pallor and peculiar facial expression.
Pain is described as tightness, heaviness and constriction. - Anxiety: It is common and occurs when there is fear of impending death.
- Nausea and vomiting.
- Breathlessness due to fall in cardiac output.
- Collapse or syncope due to arrhythmia and profound hypertension.
Signs: acute myocardial infarction.
1. Signs of sympathetic activation
- Pallor
- Sweating
- Tachycardia.
2. Signs of vagal stimulation
- Vomiting
- Bradycardia.
3. Signs of impaired myocardial function
- Hypotension and oligouria
- Narrow pulse pressure
- Raised jugular venous pressure
- Third heart sound
- Quite fist heart sound
- Lung crepitations.
4. Signs oftissue damage: Fever and arrhythmia
5. Signs of complications:
- Due to mitral regurgitation
- Due to pericarditis.
- Ventricular ectopic beats
- Ventricular tachycardia
- Heart blocks.
Diagnosis acute myocardial infarction.
Diagnosis of acute myocardial infarction is based on history, characteristics symptoms and signs and investigations.
Investigations acute myocardial infarction.
1. Electrocardiography:
1. ECG is the specific method for confirming the
diagnosis.
2. Typical changes are seen in leads which faces the infracted area. These changes are:
- Elevation of STsegment
- Pathologic Qwaves appear.
- T waves may become tall and peaked in very early myocardial infarction.
T waves are transient and last for a few hours only. - In contrast to transmural lesions, partial thickness or subendothelial infarction causes ST/T wave changes without Qwaves or prominent ST elevation.
- Changes in the ECG are seen which evolve in predictable fashion over next few days to weeks.
2. Blood test:
1. Plasma biochemical markers:
Myocardial infarction leads to detectable rise in the plasma concentration of various enzymes and proteins that are normally concentrated within the cardiac cells.
Plasma enzymes (cardiac injury enzymes) are as follows:
- Creatine kinase (CK).
- Aspartate aminotransferase (AST).
- Lactate dehydrogenase (LDH).
- Myoglobin
- Troponins (troponin I and troponin T)
2. Creatine kinase starts to rise at 4–6 hours and it peaks by about 12 hours and falls to normal in 48–72 hours.
Myocardial isoenzyme of creatine kinase is more specifi. It is useful for diagnosis of early myocardial infarction.
3. Aspartate aminotransferase (AST) starts to rise at about 12 hours and reaches a peak on the fist or second day and returns on third and fourth day.
4. Lactate dehydrogenase (LDH) starts to rise after 12 hours, reaches a peak after 2–3 days and may remain elevated for a week.
Rise in the value of LDH I (anisoenzyme of LDH) is a more sensitive indicator of myocardial infarction than total LDH.
It is useful in diagnosis for patients who present several days after myocardial infarction.
5. Cardiac troponins are cardiac troponinT (cTnT) and cardiac troponinI (cTnI). Sensitivity of troponins is similar to that of isoenzymes of creatine kinase.
Moreover, cTnT remains elevated for 100 to 200 hours after acute myocardial infarction and therefore, it may have particular utility in the evaluation of patients who present suffiently long episode after the pain in chest.
- Leukocytosis with a peak on fist day.
- ESR is raised which may remain raised for some days.
- Creactive protein is elevated.
6. Chest X-ray: It can detect acute pulmonary edema or congestion. It is also helpful to detect pericardial effsion, cardiomegaly, etc.
7. Radionuclide scanning: It shows site of necrosis and the extent of impairment of ventricular function.
8. Echocardiography: This is done for regional wall motion abnormality and ejection fraction.
Treatment acute myocardial infarction.
The management of myocardial infarction is divided into two parts:
1. Early management.
2. Late management.
Early Management acute myocardial infarction.
- Aspirin 150–300 mg to be chewed earliest.
- Sublingual glyceryl trinitrate 0.4–1 mg, to be repeated, if necessary
- Oxygen through nasal cannula at a rate of 2–4 L/min.
- Procure IV line and take blood samples for glucose, lipids and complete haemogram.
- Record 12lead ECG.
- Pain may be relieved by IV morphine (5 mg) plus metoclopramide as an antimetic (10 mg).
- IV betablockers (metoprolol 5 mg every 2–5 minutes for 3 doses) for ongoing chest pain, hypertension and tachycardia provided there is no contraindication.
- Thrombolysis should be done.
- If PTCA is planned, give GP IIb/IIIa inhibitor
- After admission immediately shift the patient to ICU or
ICCU
In Hospital treatment acute myocardial infarction.
Hospitalization and strict Bed rest
- Hospitalize the patient and advice strict bed rest. As early as the patient is hospitalized, the bettr it is.
- Patient should be strictly admittd in ICCU.
Analgesia acute myocardial infarction.
- IV morphine sulphate 10 mg and an anti emetic, i.e. cyclizine 50 mg is given through I.V. cannula.
- The drug is repeated depending on the response till complete analgesia is received and patient feels bettr.
Anti-platelet drugs acute myocardial infarction.
Low dose aspirin, i.e. 75 to 150 mg and clopidogrel 300 mg stat and then 75 mg orally daily is given.
Oxygen therapy acute myocardial infarction.
Inhalation of oxygen increases arterial partial pressure of oxygen, so there is increase in the concentration of oxygen gradient which is responsible for diffusionn of oxygen in ischemic myocardium from adjacent better perfused areas. This is given by facemask or nasal prongs for a day or two after infarction.
Thrombolysis acute myocardial infarction.
- Coronary thrombolysis helps to restore patency of coronary artery preserves left ventricular function and improves survival.
- The choice of drug for thrombolysis is less important than the speed of treatment.
- Streptokinase, 1.5 million units in 100 mL of saline given in an intravenous infusion over 1 hour, is a widely accepted method.
It is a cheap, but being antigenic, sometimes, may cause serious allergic manifestations.
Hence, it can be used once and therapy is changed if the patient requires second thrombolysis within few years.
Alteplase (tissue Plasminagen activator (tPa)
- It is a potent firinolytic drug but is expensive.
- It is less antigenic and does not cause hypotension.
- The current tPA regimen given over 90 minutes (bolus dose of 15 mg followed by 50 mg over 30 minutes and then 35 mg over next 60 minutes) is widely accepted. The other drugs include reteplase given in double dose regime i.e.
10 million units over 2–3 minute followed by another dose of 10 million units after 30 minutes.
Tenectaplase given as bolus dose of 53 mg/kg over 10 seconds. Both reteplase and tenectaplase are known as bolus firinolytics.
Angioplasty
Immediate angioplasty of infarct related artery is safe and is effctive alternative to thrombolysis. It is done in the patients in whom the hazards of thrombolysis is high.
Anti-coagulants
- Subcutaneous heparin, i.e. 7,500 units twice a day for 7–10 days or till discharge of patient from the hospital can be employed.
In patients who do not receive thrombolytic therapy to prevent venous thrombosis. - Patients who receive thrombolytic therapy (tPA) should receive immediate and full doses of heparin (10,000 U bolus plus, l000 U hourly).
Beta-adrenergic Blockers
Acute betaadrenoreceptors blockade intravenous atenolol (5–l0 mg given over 5 minutes) or metoprolol (5–15 mg given over 5 minutes) relieves pain, reduces arrhythmias, salvages myocardium and improves short term mortality in patients who present within l2 hours of onset of pain.
Nitrates and other agents
Sublingual glyceryl trinitrate 0.4 mg is useful in threatened infarction.
Sedatives
Diazepam 5mg for three to four times a day is effctive. It is given for few days.
Diet
- For fist 4 to 5 days low calorie diet which is divided into multiple meals is given.
- If heart failure is present restrict the salt.
- From second week, food should be increased in amount.
Lipid lowering agent
Atorvastatin is given to reduce the LDL levels.
Late Management acute myocardial infarction.
1. Risk stratifiation and further investigations: Prognosis of patient survived after myocardial infarction depends on degree of myocardial damage, any residual ischemia and presence of ventricular arrhythmias.
2. Life style modifiation:
- Stop smoking
- Diet control
- Regular exercise.
3. Secondary prevention
- Antiplatelet agents, i.e. aspirin
- Lipid lowering agents
- Betablockers and ACEI in congestive cardiac failure and hypertension.
- Control of blood sugar in diabetes.
4. Rehabilitation and after care:
- Physical activities should be restricted for 4 to 6 weeks since infarct takes 4–6 weeks to become replaced with firous tissue.
- Gradual mobilization and return to work over 6 weeks.
When there are complications, the regimen has to be modifid accordingly. - Exercise within the limits set by angina and tiredness will do no harm but much good. Same limits apply to sexual activity.
- Control of obesity, regular exercises, cessation of smoking, adoption of a less frenetic way of life and control of plasma lipids by diets and drugs.
- Complications should be managed. Pain relief, reassurance, rest and correction of hypokalemia play a major role in prevention of arrhythmias.
Routine drug therapy acute myocardial infarction.
- Low dose aspirin, i.e. 75 to 150 mg daily and is continued indefiitely.
- Beta-adrenergic blocker should be given for 4 to 6 weeks if there is no contraindication.
- ACE inhibitor, i.e. captopril 25 mg TID or ramipril 2.5 to 5 mg BD
- Lipid lowering agent atorvastatin is given to lower the LDL levels.
Question 9. Write short note on angina pectoris.
Or
Describe clinical features, diagnosis and management of angina pectoris.
Answer. Angina pectoris is a symptom complex caused by transient myocardial ischemia and constitutes a clinical syndrome rather than a disease.
Types
- Stable
- Unstable
- Nocturnal
- Prinzmetal’s
- Postinfarction angina
Etiology
Acute myocardial ischemia occurs when myocardial oxygen demand exceeds supply in following:
- Coronary atherosclerotic narrowing (most cases).
- Nonatherosclerotic coronary artery disease—Coronary spasm, coronary thromboembolism, congenital anomalies, coronary vasculitis.
- Valvalar heart disease — Aortic stenosis and/or aortic regurgitation, mitral stenosis with pulmonary hypertension, mitral valve prolapse.
- Pulmonary hypertension.
- Systemic hypertension.
- Hvpertrophic or dilated cardiomyopathy.
- Anemia—from tachycardia and reduction in O2 availability.
Precipitating causes
- Physical exertion
- Heavy metal
- Exposure to cold
- Emotion and excitement
- Hyperinsulinism in diabetic patients
- Other causes: Straining at stools, bathing, sexual intercourse,micturition
Clinical Features angina pectoris
symptoms angina pectoris
1. Anginal pain:
- Site: Most often over middle or lower sternum or over left precordium, at times in epigastrium. Sometimes discomfort is located only in left shoulder or left upper arm, occasionally in lower jaw and rarely in interscapular area.
- Radiation of pain: May spread to right or left arm or both neck or jaw. Occasionally, pain starts in the wrist, upper arms or face and then spreads to the chest.
- Character: Vicelike constriction or choking. Sometimes only pressure or burning pain, rarely mere weakness of one or both arms. An important characteristic is its constancy, the pain being steady while it lasts.
- Duration: Most commonly l to 4 minutes. It may force patient to stop walking.
- Provocation: By effrt specially like walking against the wind or up a climb, hurrying after meals or unaccustomed exercise at times due to excitement anger, and fear. In advanced cases, pain is provoked by lying down (angina decubitus) or stooping.
- Relief with sublingual nitroglycerine.
2. Dyspnea: If it occurs before the pain suggests severe ventricular disease.
3. Other symptoms:
- Choking sensation in throat or feeling of impending doom.
- Belching or passage of fltus or polyuria after an attck.
- Dizziness, faintness or rarely syncope
- If pain is severe sweating and nausea.
Signs angina pectoris
1. At time, no signs are present.
2. Signs ofLV dysfunction: Atrial or third heart sound.
3. Dysfunction of papillary muscle: It can lead to transient mitral regurgitation in case of ischemia.
4. Signs associated with risk factors:
- Hypertension.
- Hyperlipidemia—Arcus senilis, xanthelasma, or cholesterol deposits along tendons and in skin of palms and buttcks.
- Obesity
- Diabetes and its accompaniments.
5. During the attck—pallor and sweating with rise of BP often tachycardia.
Pressure on carotid sinus may produce slowing of pulse and cessation of pain.
Diagnosis angina pectoris
Investigations angina pectoris
- Resting ECG: ECG changes of myocardial ischemia are reflcted in ST-T waves. Occassionally, there is flttning of T waves in some lead in patient with angina.
- Exercise ECG or stress test: With continuous ECG monitoring and intermittent BP recording is performed with a treadmill or bicycle ergometer. Standardized protocols are used (e.g. Bruce protocol), enabling performance to be assessed in same patient at diffrent times and workload at onset of symptoms or ECG changes to be determined.
An exercise ECG is abnormal, if there is horizontal or downsloping ST segment depression of 0.1 mm or more in any lead. - Myocardial perfusion scintigraphy: The isotope cardiovascular stress (usually thallium201 or technetium—99 m) is injected at peak exercise and images taken with a camera immediately or shortly after exercise and compared with rest images taken a few hours later following a second injection of tracer.
Areas of myocardial ischemia are identifid by reduced isotopic uptake in the same anatomical distribution stress images but not resting images (reversible defect). - Coronary angiography: It is done before angioplasty or coronary bypass surgery.
Management angina pectoris
- It is divided into three phases:
- General measures.
- Pharmacological treatment.
- Invasive treatment.
General Measures angina pectoris
- Do not smoke
- Aim at ideal body weight
- Take regular exercise
- Avoid severe exertion, vigorous exercise and exercise in cold weather
- Take sublingual nitrate before taking exertion that may induce angina.
Pharmacological treatment angina pectoris
Following agents are used with successful outcome.
1. Antiplatelet agents:
- Aspirin is used usually in dose of 75–150 mg daily.
- Clopidogrel is used along with or without aspirin at dose of 75 mg daily.
2. Anti-anginal agents:
- Sublingual glycertrinitrate effctively abort anginal attack by causing coronary vasodilatation and reducing preload and cardiac output.
- Beta-blockers improve cardiac effiency and reduce oxygen consumption. Cardioselective agents such as atenolol 25 to 50 mg, metoprolol 200 mg daily can be used.
- Calciumchannel antagonists, i.e. amlodipine, lacidipine. They are the vasodilators and lowers myocardial oxygen demand by reducing blood
pressure and myocardial contractility. - Potassiumchannel opener, i.e. nicorandil has atrial and venous dilatation property which does not exhibit tolerance.
Invasive treatment angina pectoris
- *Percutaneous coronary *intervention or percutaneous transluminal coronary *angioplasty is done.
- Coronary artery bypass grafting is done.
Question 10. Outline the management of angina pectoris.
Answer.
Angina pectoris is a symptom complex caused by transient myocardial ischemia and constitutes a clinical syndrome rather than a disease.
Types
- Stable
- Unstable
- Nocturnal
- Prinzmetal’s
- Postinfarction angina
Etiology
Acute myocardial ischemia occurs when myocardial oxygen demand exceeds supply in following:
- Coronary atherosclerotic narrowing (most cases).
- Nonatherosclerotic coronary artery disease—Coronary spasm, coronary thromboembolism, congenital anomalies, coronary vasculitis.
- Valvalar heart disease — Aortic stenosis and/or aortic regurgitation, mitral stenosis with pulmonary hypertension, mitral valve prolapse.
- Pulmonary hypertension.
- Systemic hypertension.
- Hvpertrophic or dilated cardiomyopathy.
- Anemia—from tachycardia and reduction in O2 availability.
Precipitating causes angina pectoris
- Physical exertion
- Heavy metal
- Exposure to cold
- Emotion and excitement
- Hyperinsulinism in diabetic patients
- Other causes: Straining at stools, bathing, sexual intercourse,micturition
Clinical Features angina pectoris
symptoms angina pectoris
1. Anginal pain:
- Site: Most often over middle or lower sternum or over left precordium, at times in epigastrium. Sometimes discomfort is located only in left shoulder or left upper arm, occasionally in lower jaw and rarely in interscapular area.
- Radiation of pain: May spread to right or left arm or both neck or jaw. Occasionally, pain starts in the wrist, upper arms or face and then spreads to the chest.
- Character: Vicelike constriction or choking. Sometimes only pressure or burning pain, rarely mere weakness of one or both arms. An important characteristic is its constancy, the pain being steady while it lasts.
- Duration: Most commonly l to 4 minutes. It may force patient to stop walking.
- Provocation: By effrt specially like walking against the wind or up a climb, hurrying after meals or unaccustomed exercise at times due to excitement anger, and fear. In advanced cases, pain is provoked by lying down (angina decubitus) or stooping.
- Relief with sublingual nitroglycerine.
2. Dyspnea: If it occurs before the pain suggests severe ventricular disease.
3. Other symptoms:
- Choking sensation in throat or feeling of impending doom.
- Belching or passage of fltus or polyuria after an attck.
- Dizziness, faintness or rarely syncope
- If pain is severe sweating and nausea.
Signs angina pectoris
1. At time, no signs are present.
2. Signs ofLV dysfunction: Atrial or third heart sound.
3. Dysfunction of papillary muscle: It can lead to transient mitral regurgitation in case of ischemia.
4. Signs associated with risk factors:
- Hypertension.
- Hyperlipidemia—Arcus senilis, xanthelasma, or cholesterol deposits along tendons and in skin of palms and buttcks.
- Obesity
- Diabetes and its accompaniments.
5. During the attck—pallor and sweating with rise of BP often tachycardia.
Pressure on carotid sinus may produce slowing of pulse and cessation of pain.
Diagnosis angina pectoris
Investigations angina pectoris
- Resting ECG: ECG changes of myocardial ischemia are reflcted in ST-T waves. Occassionally, there is flttning of T waves in some lead in patient with angina.
- Exercise ECG or stress test: With continuous ECG monitoring and intermittent BP recording is performed with a treadmill or bicycle ergometer. Standardized protocols are used (e.g. Bruce protocol), enabling performance to be assessed in same patient at diffrent times and workload at onset of symptoms or ECG changes to be determined.
An exercise ECG is abnormal, if there is horizontal or downsloping ST segment depression of 0.1 mm or more in any lead. - Myocardial perfusion scintigraphy: The isotope cardiovascular stress (usually thallium201 or technetium—99 m) is injected at peak exercise and images taken with a camera immediately or shortly after exercise and compared with rest images taken a few hours later following a second injection of tracer.
Areas of myocardial ischemia are identifid by reduced isotopic uptake in the same anatomical distribution stress images but not resting images (reversible defect). - Coronary angiography: It is done before angioplasty or coronary bypass surgery.
Management angina pectoris
- It is divided into three phases:
- General measures.
- Pharmacological treatment.
- Invasive treatment.
General Measures angina pectoris
- Do not smoke
- Aim at ideal body weight
- Take regular exercise
- Avoid severe exertion, vigorous exercise and exercise in cold weather
- Take sublingual nitrate before taking exertion that may induce angina.
Pharmacological treatment angina pectoris
Following agents are used with successful outcome.
1. Antiplatelet agents:
- Aspirin is used usually in dose of 75–150 mg daily.
- Clopidogrel is used along with or without aspirin at dose of 75 mg daily.
2. Anti-anginal agents:
- Sublingual glycertrinitrate effctively abort anginal attack by causing coronary vasodilatation and reducing preload and cardiac output.
- Beta-blockers improve cardiac effiency and reduce oxygen consumption. Cardioselective agents such as atenolol 25 to 50 mg, metoprolol 200 mg daily can be used.
- Calciumchannel antagonists, i.e. amlodipine, lacidipine. They are the vasodilators and lowers myocardial oxygen demand by reducing blood
pressure and myocardial contractility. - Potassiumchannel opener, i.e. nicorandil has atrial and venous dilatation property which does not exhibit tolerance.
Invasive treatment angina pectoris
- *Percutaneous coronary *intervention or percutaneous transluminal coronary *angioplasty is done.
- Coronary artery bypass grafting is done.
Question 11. Describe briefl Marfan’s syndrome.
Answer. It is a genetic metabolic disorder of connective tissue.
Etiology
Disease is caused by defect in manufacture of firillin molecules in extracellular matrix.
Clinical Features Marfan’s syndrome.
- Patient is tall and slender.
- The inheritance is autosomal dominant.
- Extremities especially fingers and toes are long and thin.
- Muscles are Markedly *hypotonic and joints are *hyper extensible.
- The main cause of *morbidity and *mortality is related to CVS. There is aortic aneurysm (localized abnormal dilatation of blood vessel usually an artery due to congenital defect or weakness in wall of vessel) and other valve abnormalities mainly mitral incompetence.
- Death is due to rupture of aneurysm.
- There is presence of flt feet, *stooped shoulders and dislocation of optic lens.
Management Marfan’s syndrome.
- Betablockers are given to prevent *aneurysmal rupture.
- Treatment of complication: Aneurysm* can be operatively treated by using dacron mesh or graft.
- Valvular defects are treated accordingly by either repair or replacement.
Question 12. Enumerate causes of continuous murmurs.
Answer A continuous murmur is one which begins in systole and continues through the second heart sound into part or whole of diastole.
Causes of continuous murmurs are as follows:
- Patent ductus arteriosus
- Aortopulmonary window
- Ruptured sinus of valsalva into the right side of the heart
- Surgically produced shunts in TOP—BlalockTaussig shunt
- Coarctation of aorta
- Coronary/pulmonary/systemic A-V fitula
- Aortic stenosis and aortic regurgitation
- Ventricular septal defect with aortic regurgitation
- Venous hum
- Mammary souff
- Anomalous origin of left coronary artery from pulmonary artery
Question 13. Describe briefl complete heart block.
Answer. Complete heart block is also known as third degree heart block or complete AV block
Etiology
1. Congenital:
- Usually associated with ventricular septal defect,rarely isolated.
2. Acquired:
Rheumatic heart disease
- Acute infections—rheumatic fever, diphtheria
- Drugs—Digitalis, quinidine
- Calcifi aortic stenosis.
- Trauma (penetrating).
- Surgical procedures: After correction of ventricular septal defect, or following insertion of prosthetic valves or removal of hypertrophied septum in
hypertrophic cardiomyopathy. - Cardiomyopathy (particularly infitrative).
- Syphilitic heart disease.
- Infitrative masses: Sarcoidosis, tubercles, abscesses from endocarditis, gummas, tumors, amyloidosis, hemochromatosis.
- Collagendiseases: Rheumatoid arthritis, dermatomyositis.
- Fistulae: Sinus of Valsalva aneurysm rupturing into right atrium.
- Unknown cause: Idiopathic firosis.
Clinical Features Marfan’s syndrome.
Symptoms Marfan’s syndrome.
- Due to low cardiac output: Lassitude, fatigue, light headedness, and especially during exercise syncope.
- Symptoms of vertebrobasilar insuffiency and congestive heart failure may be precipitated.
- Due to increased stroke volume: Uncomfortable awareness of heart beat, or slow palpitation, if block is intermittnt.
- Due to transient circulatory arrest: Stokes-Adams attcks Symptoms depend on duration of standstill of circulation: About 5 seconds—giddiness and faintness, about 10 seconds—convulsions.
- Convulsions and incontinence may suggest epilepsy, but in transient asystole pallor is often striking, patient flshes during recovery, and consciousness is regained very rapidly; though some permanent impairment of cerebral function may occur after long or repeated episodes.
Signs Marfan’s syndrome.
- Slow and regular heart rate: At 30 to 50 beats per minute,which does not usually increase signifiant with physical activity or exercise.
- Raised Jugular venous pressure: ‘a’ waves may be seen in the neck unrelated to ventricular beats.
- Cannon waves: Giant ‘a’ waves which are transmittd in the neck when the atrium contracts against a closed tricuspid valve.
- Variation in intensity ofFirst heart sound: First heart sound is loudest when the interval between the preceding atrial beat and the ventricular beat is short, it is faintest when the interval is long.
From time to time, there is a sharp accentuation of the fist sound at the apex (cannon sound). - Tide pulse pressure: Due to increased systolic pressure and low diastolic pressure. This gives rise to water hammer pulse and capillary pulsation.
- Cardiac enlargement: Due to increased stroke volume, hyperdynamic cardiac impulse.
- Systolic ejection murmur: Loudest in 2nd and 3rd left interspaces adjacent to the sternal edge, and due to increased velocity of blood flw associated with increased stroke volume.
- Atrial sounds: They may be heard in constant relation to fist and second heart sounds.
- Apical diastolic flw murmur: It is occasional.
- ECG: There is no relation between atrial and ventricular complexes. The duration of QRS is normal.
Management Marfan’s syndrome.
In acute complete av Block
Acute onset of complete AV block occurs in acute myocardial infarction, i.e. in inferior myocardial infarction and anterior myocardial infarction.
Complete AV Block with Inferior Myocardial Infarction
- Complete AV block occurs usually in acute inferior wall infarction but are transient and less troublesome.
No treatment is needed in such patients who are well and hemodynamically stable. If in such cases, clinical deterioration occurs, then atropine 0.6 mg IV can be given as a bolus and repeated, if necessary.
If this treatment fails, then a temporary pacemaker may be inserted.
In most of the patients, heart block disappears under 7–10 days.
Complete AV Block with Anterior Myocardial Infarction
- This occurs less commonly, is dangerous and carry poor prognosis.
Asystole commonly occurs in such cases and lead to mortality.
If patients develop asystole, atropine 0.6 mg IV given as bolus and repeated, if needed. Temporary pacemaker is inserted immediately. Isoprenaline infusion, i.e.
1 to 5 mg in 500 mL of 5% dextrose should be started at minimum rate to produce a satisfactory heart rhythm till temporary pacemaker is inserted. - Ifblockisduetodrugtoxicity, strictlystoptheoffndingdrug.
Chronic complete av block
A permanent pacemaker is indicated in patients having asymptomatic Mobit type II complete heart block because it can improve their prognosis.
Question 14. Enumerate the causes of massive cardiomegaly.
Answer. The causes of massive cardiomegaly are:
- Hypertrophic cardiomyopathy and dilated
*cardiomyopathy - Congenital insuffiency of tricuspid valve
- Pediatric anesthesia
- Nonuniform pulmonary artery perfusion
- Idiopathic arterial calcifiation in childhood.
- Cyanosis
- Alveolar hemorrhage syndrome with renal involvement
- Rheumatic fever
- Pericardial effsion
- Ebstein anomaly.
Question 15. Describe briefly verapamil.
Answer. Verapamil is a Class IV anti arrhythmic agent and an anti hypertensive drug.
Mechanism of action verapamil.
- It leads to coronary dilatation and decreases myocardial oxygen consumption.
- It interferes with the inward displacement of calcium and delays conduction within the AV node.
Dosage verapamil.
40 or 80 mg TDS orally
Or
5 mg to 10 mg IV paroxysmal atrial tachycardia.
Side effects verapamil.
- Constipation
- Hypotension
- Vertigo
- Nervousness
Indications verapamil.
- In supraventricular tachycardias such as atrial tachycardia
and atrial firillation - In premature heart beats
- In ischemic heart disease such as angina
- In hypertension
Question 16. Describe briefl captopril.
Answer. Captopril is an ACE inhibitor.
Mechanism of action captopril.
- Drug prevent the conversion of angiotensin I into angiotensin II by inhibiting angiotensin converting enzyme thus preventing action of angiotensin II, i.e. vasoconstriction and aldosterone synthesis and causes fall in blood pressure.
- Captopril metabolizes bradykinin which is a potent vasodilator.
It increases bradykinin levels causing vasodilatation.
Adverse effects captopril.
It causes hypotension, hyperkalemia, dry persistent cough, loss of taste sensation, urticaria, angiedema, pruritus, skin rash, agranulocytosis, proteinuria, renal insuffiency
Uses captopril
- Captopril is first line drug to be used in treatment of hypertension. The captopril is more effective in renovascular hypertension.
- It decreases preload and afterload in cardiac heart failure.
- In diabetics, it improves renal function.
- Captopril is used in myocardial infarction and also causes reduction in motility.
Dose captopril.
It is given 25 mg TDS increased every week upto a maximum of 450 mg/day
Question 17. Describe clinical features, investigation and treatment of left ventricular failure.
Or
Write short note on left ventricular failure.
Answer.
Left ventricular failure is defied as failure to maintain an effctive ventricular output for a given pulomonary venous or left atrial pressure or can do so only at the expense of an elevated left atrial filing pressure.
Causes left ventricular failure.
1. Left ventricular outflw obstruction:
- Systemic hypertension
- Aortic valvular stenosis
- Idiopathic hypertrophic subaortic stenosis
- Coarctation of aorta
2. Left ventricular inflw obstruction:
- Mitral stenosis
- Left atrial myxoma
- Endomyocardial firosis with stif left ventricle
3. Left ventricular volume overload:
- Mitral valve prolapsed
- Mitral regurgitation
- Aortic regurgitation (rheumatic and nonrheumatic)
- Ventricular septal defect
- Patent ductus arteriosus
- High output states
- Papillary muscle dysfunction
4. Reduced left ventricular contractility:
- Cardiomyopathy predominantly involving left
ventricle - Anterior wall myocardial infarction
- Left ventricle endocarditis
Clinical Features left ventricular failure.
- Progressive dyspnea is the earliest sign of left heart failure.
- Presence of orthopnea due to increase in venous return during recumbent position.
- Attcks of breathlessness which occur at night and awaken the patient, i.e. paroxysmal nocturnal dyspnea.
- In severe heart failure there is a periodic respiration in which periods of hyperpnea alternate with apnea, i.e.
CheyneStokes respiration. - Presence of dry cough which is disturbing.
- Presence of oliguria and nocturia.
- Presence of tachypnea because of stif congested lungs and there is also presence of tachycardia because of hypoxia created due to pulmonary congestion.
- Presence of fatigue and weakness.
- Cerebral symptoms are present, i.e. altered mental state, diffilty in concentration, memory impairment, headache, insomnia and anxiety
Physical Findings left ventricular failure.
- Extremities can be cold or pale.
- There is presence of tachycardia and rapid pulse rate.
- Presence of profuse sweating
- Presence of tachypnea, i.e. increased respiratory rate
- There is low pulse volume or pulsus alternans can be present.
- Presence of central cyanosis.
- Third heart sound can be heard.
- There is presence of basal pulmonary rales or crackles.
- Presence of an expiratory wheezing.
- Presence of oliguria.
- Hydrothorax or pleural effsion is present.
- Presence of anxiety and depression.
- Urine can be ofhigh specifi gravity and shows proteinuria.
- Presence of massive cardiomegaly.
Investigations left ventricular failure.
1. Electrocardiogram:
- Presence of left ventricular hypertrophy and left atrial hypertrophy in patients having aortic valvular diseases as well as mitral regurgitation.
- Presence of STT changes in patients having disease of myocardium.
2. Chest X-ray:
- Presence of enlargement of cardiac shadow.
- Presence of pulmonary venous congestion which extends from hilum to periphery.
- There is presence of Kerley’s lines because of interstitial edema.
3. Echocardiogram:
- Increase in the left ventricular dimensions
- Left ventricular end diastolic pressure or volume of both can be high
- Increase in the cardiac output and stroke volume
- There is reduction in ejection fractions
4. Other tests:
Monitor blood urea and other electrolytes
Treatment left ventricular failure.
- First aim of treatment is to fid and remove the precipitating cause, i.e. arrhythmia or an intercurrent infection.
- Patient should be kept in sitting position, with legs hanging alongside of the bed, i.e. upright posture should be maintained.
- Diet: Saltfree diet is given till left ventricular failure improves and later on restricted salt diet is given.
- Sedatives: Morphine should be given in doses of 5 to 10 mg along with an antiemetic, i.e. metoclopramide 10 mg IV and repeat the drug as soon as desired.
- Oxygen: About 60% of oxygen is given by facemask under positive pressure. It should be given as 6 to 8 lts / min through Wolfe’s botte.
- Loop diuretics: Furosemide 40–100 mg IV should be given.
- IV sodium nitroprusside 20–30 µg/min or IV nitroglycerine should be given in patients whose systolic blood pressure is more than 100 mm of Hg.
- Digitalis: If digoxin is not used previously, the three fourth of full dose, i.e. 0.5 to 1 mg is given as IV dose.
- Bronchodilators: At times, aminophylline or theophylline in dose of 250 to 500mg IV decreases bronchoconstriction.
- In cases of severe left ventricular failure, inotropes can be given.
- If all the above measures failed, then rotating tourniquet should be applied to extrimities.
- Intra-aortic balloon counterepulsation: It is used in acute left ventricular failure during cardiac procedures or cardiac repairs.
Question 18. Describe briefl acute pulmonary edema.
Answer. The term acute pulmonary edema refers to collection of flid into alveoli its wall and alveolar sac due to an acute increase in left atrial pressure.
Causes left acute pulmonary edema.
1. Cardiogenic:
- Left ventricular failure
- Myocardial infarction
- Mitral stenosis
- Pulmonary infarction
- Cardiac arrhythmia.
2. Non-cardiogenic:
- Fluid overload
- Shock
- Inhalation of gastric acid (Mendelson’s syndrome)
- High altitude pulmonary edema.
Clinical Features acute pulmonary edema.
- Feeling of *oppression in chest
- Acute and distressing dyspnea
- Short cough and pink frothy sputum, sometimes blood tinged flid from mouth and nose.
- Sweat and feeble pulse.
- Fall of temperature.
Management acute pulmonary edema.
- Bed rest is provided as the sittng position tends to reduce
venous return. - Oxygen is provided
- Inj. Morphine 15 mg subcutaneously is given.
- Inj. Furosemide 80 mg IV relieves pulmonary edema.
If patient has not received digoxin during last fortnight - Inj. Digoxin (0.5. to 1 mg) is given.
- Inj. Aminophylline 0.24 gm slow IV in 10 min is effctive.
- Patients not responding above regimen IV nitroprusside
20–30 unit g per minute is given.
Question 19. Discuss etiology, clinical features, diagnosis and management of acute myocardial infarction.
Answer. Acute myocardial infarction is defied as irreversible damage to myocardium of heart as a result of occlusive thrombus due to rupture of atherosclerotic plaque in coronary artery.
Etiology
- The most important cause of myocardial infarction is coronary atherosclerosis.
- Obesity and hypertension
- Cigarett smoking
- Diabetes mellitus
- Sedentary life cycle (A life cycle involving litte exercise,even of at least strenuous type)
- Dyslipidemia, i.e. increased levels of LDL.
- Hereditary susceptibility
Clinical Features acute myocardial infarction.
Symptoms: acute myocardial infarction.
- Pain: Chest pain is more common and is severe in comparison to angina.
Pain is severe with pallor and peculiar facial expression.
Pain is described as tightness, heaviness and constriction. - Anxiety: It is common and occurs when there is fear of impending death.
- Nausea and vomiting.
- Breathlessness due to fall in cardiac output.
- Collapse or syncope due to arrhythmia and profound hypertension.
Signs: acute myocardial infarction.
1. Signs of sympathetic activation
- Pallor
- Sweating
- Tachycardia.
2. Signs of vagal stimulation
- Vomiting
- Bradycardia.
3. Signs of impaired myocardial function
- Hypotension and oligouria
- Narrow pulse pressure
- Raised jugular venous pressure
- Third heart sound
- Quite fist heart sound
- Lung crepitations.
4. Signs oftissue damage: Fever and arrhythmia
5. Signs of complications:
- Due to mitral regurgitation
- Due to pericarditis.
- Ventricular ectopic beats
- Ventricular tachycardia
- Heart blocks.
The management of myocardial infarction is divided into two parts:
1. Early management.
2. Late management.
Early Management acute myocardial infarction.
- Aspirin 150–300 mg to be chewed earliest.
- Sublingual glyceryl trinitrate 0.4–1 mg, to be repeated, if necessary
- Oxygen through nasal cannula at a rate of 2–4 L/min.
- Procure IV line and take blood samples for glucose, lipids and complete haemogram.
- Record 12lead ECG.
- Pain may be relieved by IV morphine (5 mg) plus metoclopramide as an antimetic (10 mg).
- IV betablockers (metoprolol 5 mg every 2–5 minutes for 3 doses) for ongoing chest pain, hypertension and tachycardia provided there is no contraindication.
- Thrombolysis should be done.
- If PTCA is planned, give GP IIb/IIIa inhibitor
- After admission immediately shift the patient to ICU or ICCU
In Hospital treatment acute myocardial infarction.
Hospitalization and strict Bed rest
- Hospitalize the patient and advice strict bed rest. As early as the patient is hospitalized, the bettr it is.
- Patient should be strictly admittd in ICCU.
Analgesia acute myocardial infarction.
- IV morphine sulphate 10 mg and an anti emetic, i.e. cyclizine 50 mg is given through I.V. cannula.
- The drug is repeated depending on the response till complete analgesia is received and patient feels bettr.
Anti-platelet drugs acute myocardial infarction.
Low dose aspirin, i.e. 75 to 150 mg and clopidogrel 300 mg stat and then 75 mg orally daily is given.
Oxygen therapy acute myocardial infarction.
Inhalation of oxygen increases arterial partial pressure of oxygen, so there is increase in the concentration of oxygen gradient which is responsible for diffusionn of oxygen in ischemic myocardium from adjacent better perfused areas. This is given by facemask or nasal prongs for a day or two after infarction.
Thrombolysis acute myocardial infarction.
- Coronary thrombolysis helps to restore patency of coronary artery preserves left ventricular function and improves survival.
- The choice of drug for thrombolysis is less important than the speed of treatment.
- Streptokinase, 1.5 million units in 100 mL of saline given in an intravenous infusion over 1 hour, is a widely accepted method.
It is a cheap, but being antigenic, sometimes, may cause serious allergic manifestations.
Hence, it can be used once and therapy is changed if the patient requires second thrombolysis within few years.
Alteplase (tissue Plasminagen activator (tPa)
- It is a potent firinolytic drug but is expensive.
- It is less antigenic and does not cause hypotension.
- The current tPA regimen given over 90 minutes (bolus dose of 15 mg followed by 50 mg over 30 minutes and then 35 mg over next 60 minutes) is widely accepted. The other drugs include reteplase given in double dose regime i.e.
10 million units over 2–3 minute followed by another dose of 10 million units after 30 minutes.
Tenectaplase given as bolus dose of 53 mg/kg over 10 seconds. Both reteplase and tenectaplase are known as bolus firinolytics.
Angioplasty
Immediate angioplasty of infarct related artery is safe and is effctive alternative to thrombolysis. It is done in the patients in whom the hazards of thrombolysis is high.
Anti-coagulants
- Subcutaneous heparin, i.e. 7,500 units twice a day for 7–10 days or till discharge of patient from the hospital can be employed.
In patients who do not receive thrombolytic therapy to prevent venous thrombosis. - Patients who receive thrombolytic therapy (tPA) should receive immediate and full doses of heparin (10,000 U bolus plus, l000 U hourly).
Beta-adrenergic Blockers
Acute betaadrenoreceptors blockade intravenous atenolol (5–l0 mg given over 5 minutes) or metoprolol (5–15 mg given over 5 minutes) relieves pain, reduces arrhythmias, salvages myocardium and improves short term mortality in patients who present within l2 hours of onset of pain.
Nitrates and other agents
Sublingual glyceryl trinitrate 0.4 mg is useful in threatened infarction.
Sedatives
Diazepam 5mg for three to four times a day is effctive. It is given for few days.
Diet
- For fist 4 to 5 days low calorie diet which is divided into multiple meals is given.
- If heart failure is present restrict the salt.
- From second week, food should be increased in amount.
Lipid lowering agent
Atorvastatin is given to reduce the LDL levels.
Late Management acute myocardial infarction.
1. Risk stratifiation and further investigations: Prognosis of patient survived after myocardial infarction depends on degree of myocardial damage, any residual ischemia and presence of ventricular arrhythmias.
2. Life style modifiation:
- Stop smoking
- Diet control
- Regular exercise.
3. Secondary prevention
- Antiplatelet agents, i.e. aspirin
- Lipid lowering agents
- Betablockers and ACEI in congestive cardiac failure and hypertension.
- Control of blood sugar in diabetes.
4. Rehabilitation and after care:
- Physical activities should be restricted for 4 to 6 weeks since infarct takes 4–6 weeks to become replaced with firous tissue.
- Gradual mobilization and return to work over 6 weeks.
When there are complications, the regimen has to be modifid accordingly. - Exercise within the limits set by angina and tiredness will do no harm but much good. Same limits apply to sexual activity.
- Control of obesity, regular exercises, cessation of smoking, adoption of a less frenetic way of life and control of plasma lipids by diets and drugs.
- Complications should be managed. Pain relief, reassurance, rest and correction of hypokalemia play a major role in prevention of arrhythmias.
Routine drug therapy acute myocardial infarction.
- Low dose aspirin, i.e. 75 to 150 mg daily and is continued indefiitely.
- Beta-adrenergic blocker should be given for 4 to 6 weeks if there is no contraindication.
- ACE inhibitor, i.e. captopril 25 mg TID or ramipril 2.5 to 5 mg BD
- Lipid lowering agent atorvastatin is given to lower the LDL levels.
Question 20. Describe clinical diagnosis of subacute bacterial endocarditis. How will you confim diagnosis?
Or
Write short note on diagnosis of infective endocarditis.
Answer. For clinical diagnosis of subacute bacterial endocarditis,there is a criteria given by Duke, i.e. Duke’s criteria.
Duke’s criteria for clinical diagnosis of saBe
Major criteria subacute bacterial endocarditis
- Blood culture: Positive blood culture with typical infective endocarditis microorganisms (Viridans streptococci, S. bovis, HAECK group or community acquired S. aureus orenterococci)
- Endocardial involvement: New regurgitation murmur,positive ECG for SABE.
Minor criteria subacute bacterial endocarditis
- Predisposing cardiac or IV drug abuse.
- Fever
- Vascular phenomenon: Emboli, mycotic aneurysms, petechiae
- Immunologic phenomenon: Glomerulonephritis and rheumatoid factor.
- Echocardiogram: Consistent with infective endocarditis, but not meeting major criteria.
- Microbiology: Positive blood cultures, but not meeting major criteria, serological evidence of active infection with possible microorganisms.
Confimation of Diagnosis subacute bacterial endocarditis
The confimation is of three types, i.e:
1. Definite:
- Pathology or bacteriology of vegetations.
Or - Both major criteria
Or - One major and three minor criteria
Or - Five minor criteria
2. Possible:
Neither defiite nor rejected
3. Rejected:
- Firm alternative diagnosis
Or - Resolution on less than four days of antibiotics.
Question 21. Write short note on malignant hypertension.
Answer. Malignant hypertension is a complication of hypertension characterized by very elevated blood pressure and organ damage in eyes, brain, lung and kidneys.
It diffrs form other complication of hypertension in that it is accomplished by *papilledema.
Systolic and diastolic blood pressure are usually greater than 240 and 140 mm Hg.
Malignant hypertension is an hypertensive emergency.
Etiology
- Drugs, i.e. cocaine, betablockers and oral contraceptives
- Alcohol
- Atherosclerosis
- Chronic diabetes mellitus
- Renal failure.
Clinical Features acute rheumatic mitral stenosis.
- Chest pain is present
- Dyspnea
- Neurological defect
- Angina and myocardial infarction
- Pulmonary edema
- Headache
- Cerebral hemorrhage or infarction
- Visual disturbance
- *Hypertensive encephalopathy
- Gastrointestinal symptoms, i.e. nausea and vomiting.
- Oligurea.
Diagnosis acute rheumatic mitral stenosis.
- Complete blood count
- Coagulation profie
- Electrolyte profie
- Urine output and electrolytes
- TSH
- Renal function test
- Chest radiograph
- Head CT scan
- ECG to see ischemia and infarction.
Treatment acute rheumatic mitral stenosis.
Since malignant hypertension is a medical emergency, it requires immediate treatment.
- Most effective agent for blood pressure reduction in an emergency is controlled IV infusion of sodium nitroprusside, i.e. 0.3 to 1.0 µg/kg/min.
- Alternatively diazoxide 300 mg I.V. or enalaprilat 1.25 mg IV is given rapidly and anti-hypertensive effct is noted under 1 to 3 min.
The same dose is repeated when pressure begins to elevate. - Chewing a nefiipine l0 mg capsule is often suffient to give a graded reduction in blood pressure.
- Bed rest should be given to the patient.
- Sedation by IV diazepam is given.
- A potent diuretic, i.e. IV frusemide 40 mg stat can also be given.
Question 22. Describe the etiology, clinical features, complication and management of acute myocardial infarction.
Answer.
Acute myocardial infarction is defied as irreversible damage to myocardium of heart as a result of occlusive thrombus due to rupture of atherosclerotic plaque in coronary artery.
Etiology
- The most important cause of myocardial infarction is coronary atherosclerosis.
- Obesity and hypertension
- Cigarett smoking
- Diabetes mellitus
- Sedentary life cycle (A life cycle involving litte exercise,even of at least strenuous type)
- Dyslipidemia, i.e. increased levels of LDL.
- Hereditary susceptibility
The management of myocardial infarction is divided into two parts:
1. Early management.
2. Late management.
Early Management acute myocardial infarction.
- Aspirin 150–300 mg to be chewed earliest.
- Sublingual glyceryl trinitrate 0.4–1 mg, to be repeated, if necessary
- Oxygen through nasal cannula at a rate of 2–4 L/min.
- Procure IV line and take blood samples for glucose, lipids and complete haemogram.
- Record 12lead ECG.
- Pain may be relieved by IV morphine (5 mg) plus metoclopramide as an antimetic (10 mg).
- IV betablockers (metoprolol 5 mg every 2–5 minutes for 3 doses) for ongoing chest pain, hypertension and tachycardia provided there is no contraindication.
- Thrombolysis should be done.
- If PTCA is planned, give GP IIb/IIIa inhibitor
- After admission immediately shift the patient to ICU or
ICCU
In Hospital treatment acute myocardial infarction.
Hospitalization and strict Bed rest
- Hospitalize the patient and advice strict bed rest. As early as the patient is hospitalized, the bettr it is.
- Patient should be strictly admittd in ICCU.
Analgesia acute myocardial infarction.
- IV morphine sulphate 10 mg and an anti emetic, i.e. cyclizine 50 mg is given through I.V. cannula.
- The drug is repeated depending on the response till complete analgesia is received and patient feels bettr.
Anti-platelet drugs acute myocardial infarction.
Low dose aspirin, i.e. 75 to 150 mg and clopidogrel 300 mg stat and then 75 mg orally daily is given.
Oxygen therapy acute myocardial infarction.
Inhalation of oxygen increases arterial partial pressure of oxygen, so there is increase in the concentration of oxygen gradient which is responsible for diffusionn of oxygen in ischemic myocardium from adjacent better perfused areas. This is given by facemask or nasal prongs for a day or two after infarction.
Thrombolysis acute myocardial infarction.
- Coronary thrombolysis helps to restore patency of coronary artery preserves left ventricular function and improves survival.
- The choice of drug for thrombolysis is less important than the speed of treatment.
- Streptokinase, 1.5 million units in 100 mL of saline given in an intravenous infusion over 1 hour, is a widely accepted method.
It is a cheap, but being antigenic, sometimes, may cause serious allergic manifestations.
Hence, it can be used once and therapy is changed if the patient requires second thrombolysis within few years.
Alteplase (tissue Plasminagen activator (tPa)
- It is a potent firinolytic drug but is expensive.
- It is less antigenic and does not cause hypotension.
- The current tPA regimen given over 90 minutes (bolus dose of 15 mg followed by 50 mg over 30 minutes and then 35 mg over next 60 minutes) is widely accepted. The other drugs include reteplase given in double dose regime i.e.
10 million units over 2–3 minute followed by another dose of 10 million units after 30 minutes.
Tenectaplase given as bolus dose of 53 mg/kg over 10 seconds. Both reteplase and tenectaplase are known as bolus firinolytics.
Angioplasty
Immediate angioplasty of infarct related artery is safe and is effctive alternative to thrombolysis. It is done in the patients in whom the hazards of thrombolysis is high.
Anti-coagulants
- Subcutaneous heparin, i.e. 7,500 units twice a day for 7–10 days or till discharge of patient from the hospital can be employed.
In patients who do not receive thrombolytic therapy to prevent venous thrombosis. - Patients who receive thrombolytic therapy (tPA) should receive immediate and full doses of heparin (10,000 U bolus plus, l000 U hourly).
Beta-adrenergic Blockers
Acute betaadrenoreceptors blockade intravenous atenolol (5–l0 mg given over 5 minutes) or metoprolol (5–15 mg given over 5 minutes) relieves pain, reduces arrhythmias, salvages myocardium and improves short term mortality in patients who present within l2 hours of onset of pain.
Nitrates and other agents
Sublingual glyceryl trinitrate 0.4 mg is useful in threatened infarction.
Sedatives
Diazepam 5mg for three to four times a day is effctive. It is given for few days.
Diet
- For fist 4 to 5 days low calorie diet which is divided into multiple meals is given.
- If heart failure is present restrict the salt.
- From second week, food should be increased in amount.
Lipid lowering agent
Atorvastatin is given to reduce the LDL levels.
Late Management acute myocardial infarction.
1. Risk stratifiation and further investigations: Prognosis of patient survived after myocardial infarction depends on degree of myocardial damage, any residual ischemia and presence of ventricular arrhythmias.
2. Life style modifiation:
- Stop smoking
- Diet control
- Regular exercise.
3. Secondary prevention
- Antiplatelet agents, i.e. aspirin
- Lipid lowering agents
- Betablockers and ACEI in congestive cardiac failure and hypertension.
- Control of blood sugar in diabetes.
4. Rehabilitation and after care:
- Physical activities should be restricted for 4 to 6 weeks since infarct takes 4–6 weeks to become replaced with firous tissue.
- Gradual mobilization and return to work over 6 weeks.
When there are complications, the regimen has to be modifid accordingly. - Exercise within the limits set by angina and tiredness will do no harm but much good. Same limits apply to sexual activity.
- Control of obesity, regular exercises, cessation of smoking, adoption of a less frenetic way of life and control of plasma lipids by diets and drugs.
- Complications should be managed. Pain relief, reassurance, rest and correction of hypokalemia play a major role in prevention of arrhythmias.
Routine drug therapy acute myocardial infarction.
- Low dose aspirin, i.e. 75 to 150 mg daily and is continued indefiitely.
- Beta-adrenergic blocker should be given for 4 to 6 weeks if there is no contraindication.
- ACE inhibitor, i.e. captopril 25 mg TID or ramipril 2.5 to 5 mg BD
- Lipid lowering agent atorvastatin is given to lower the LDL levels.
Enumeration of complications of Myocardial Infarction
1. Immediate
1. Arrhythmias and conduction disturbances
- Sinus bradycardia
- Ventricular ectopics
- Ventricular tachycardia
- Ventricular firillation
- Idioventricular rhythm
- Atrial firillation
- Heart block
2. Post-myocardial angina can occur in 50% patients occur.
3. Acute circulatory failure.
4. Pericarditis
5. Mechanical complications include:
- Papillary muscle dysfunction or rupture
- Rupture of interventricular septum
- Rupture of ventricle
6. Mural thrombosis and embolism
7. Sudden death
2. Late complications:
- Postmyocardial infarction syndrome (Dressler’s syndrome)
- Ventricular aneurysm.
Management acute myocardial infarction.
The management of myocardial infarction is divided into two parts:
1. Early management.
2. Late management.
Early Management acute myocardial infarction.
- Aspirin 150–300 mg to be chewed earliest.
- Sublingual glyceryl trinitrate 0.4–1 mg, to be repeated, if necessary
- Oxygen through nasal cannula at a rate of 2–4 L/min.
- Procure IV line and take blood samples for glucose, lipids and complete haemogram.
- Record 12lead ECG.
- Pain may be relieved by IV morphine (5 mg) plus metoclopramide as an antimetic (10 mg).
- IV betablockers (metoprolol 5 mg every 2–5 minutes for 3 doses) for ongoing chest pain, hypertension and tachycardia provided there is no contraindication.
- Thrombolysis should be done.
- If PTCA is planned, give GP IIb/IIIa inhibitor
- After admission immediately shift the patient to ICU or ICCU
In Hospital treatment
Hospitalization and strict Bed rest
- Hospitalize the patient and advice strict bed rest. As early as the patient is hospitalized, the bettr it is.
- Patient should be strictly admittd in ICCU.
Analgesia
- IV morphine sulphate 10 mg and an anti emetic, i.e. cyclizine 50 mg is given through I.V. cannula.
- The drug is repeated depending on the response till complete analgesia is received and patient feels bettr.
Anti-platelet drugs
Low dose aspirin, i.e. 75 to 150 mg and clopidogrel 300 mg stat and then 75 mg orally daily is given.
Oxygen therapy
Inhalation of oxygen increases arterial partial pressure of oxygen, so there is increase in the concentration of oxygen gradient which is responsible for diffusionn of oxygen in ischemic myocardium from adjacent better perfused areas. This is given by facemask or nasal prongs for a day or two after infarction.
Thrombolysis
- Coronary thrombolysis helps to restore patency of coronary artery preserves left ventricular function and improves survival.
- The choice of drug for thrombolysis is less important than the speed of treatment.
- Streptokinase, 1.5 million units in 100 mL of saline given in an intravenous infusion over 1 hour, is a widely accepted method.
It is a cheap, but being antigenic, sometimes, may cause serious allergic manifestations.
Hence, it can be used once and therapy is changed if the patient requires second thrombolysis within few years.
Alteplase (tissue Plasminagen activator (tPa)
- It is a potent firinolytic drug but is expensive.
- It is less antigenic and does not cause hypotension.
- The current tPA regimen given over 90 minutes (bolus dose of 15 mg followed by 50 mg over 30 minutes and then 35 mg over next 60 minutes) is widely accepted. The other drugs include reteplase given in double dose regime i.e.
10 million units over 2–3 minute followed by another dose of 10 million units after 30 minutes.
Tenectaplase given as bolus dose of 53 mg/kg over 10 seconds. Both reteplase and tenectaplase are known as bolus firinolytics.
Angioplasty
Immediate angioplasty of infarct related artery is safe and is effctive alternative to thrombolysis. It is done in the patients in whom the hazards of thrombolysis is high.
Anti-coagulants
- Subcutaneous heparin, i.e. 7,500 units twice a day for 7–10 days or till discharge of patient from the hospital can be employed.
In patients who do not receive thrombolytic therapy to prevent venous thrombosis. - Patients who receive thrombolytic therapy (tPA) should receive immediate and full doses of heparin (10,000 U bolus plus, l000 U hourly).
Beta-adrenergic Blockers
Acute betaadrenoreceptors blockade intravenous atenolol (5–l0 mg given over 5 minutes) or metoprolol (5–15 mg given over 5 minutes) relieves pain, reduces arrhythmias, salvages myocardium and improves short term mortality in patients who present within l2 hours of onset of pain.
Nitrates and other agents
Sublingual glyceryl trinitrate 0.4 mg is useful in threatened infarction.
Sedatives
Diazepam 5mg for three to four times a day is effctive. It is given for few days.
Diet
- For fist 4 to 5 days low calorie diet which is divided into multiple meals is given.
- If heart failure is present restrict the salt.
- From second week, food should be increased in amount.
Lipid lowering agent
Atorvastatin is given to reduce the LDL levels.
Late Management
1. Risk stratifiation and further investigations: Prognosis of patient survived after myocardial infarction depends on degree of myocardial damage, any residual ischemia and presence of ventricular arrhythmias.
2. Life style modifiation:
- Stop smoking
- Diet control
- Regular exercise.
3. Secondary prevention
- Antiplatelet agents, i.e. aspirin
- Lipid lowering agents
- Betablockers and ACEI in congestive cardiac failure and hypertension.
- Control of blood sugar in diabetes.
4. Rehabilitation and after care:
- Physical activities should be restricted for 4 to 6 weeks since infarct takes 4–6 weeks to become replaced with firous tissue.
- Gradual mobilization and return to work over 6 weeks.
When there are complications, the regimen has to be modifid accordingly. - Exercise within the limits set by angina and tiredness will do no harm but much good. Same limits apply to sexual activity.
- Control of obesity, regular exercises, cessation of smoking, adoption of a less frenetic way of life and control of plasma lipids by diets and drugs.
- Complications should be managed. Pain relief, reassurance, rest and correction of hypokalemia play a major role in prevention of arrhythmias.
Routine drug therapy
- Low dose aspirin, i.e. 75 to 150 mg daily and is continued indefiitely.
- Beta-adrenergic blocker should be given for 4 to 6 weeks if there is no contraindication.
- ACE inhibitor, i.e. captopril 25 mg TID or ramipril 2.5 to 5 mg BD
- Lipid lowering agent atorvastatin is given to lower the LDL levels.
Acute myocardial infarction is defied as irreversible damage to myocardium of heart as a result of occlusive thrombus due to rupture of atherosclerotic plaque in coronary artery.
Clinical Features acute myocardial infarction.
Symptoms: acute myocardial infarction.
- Pain: Chest pain is more common and is severe in comparison to angina.
Pain is severe with pallor and peculiar facial expression.
Pain is described as tightness, heaviness and constriction. - Anxiety: It is common and occurs when there is fear of impending death.
- Nausea and vomiting.
- Breathlessness due to fall in cardiac output.
- Collapse or syncope due to arrhythmia and profound hypertension.
Signs: acute myocardial infarction.
1. Signs of sympathetic activation
- Pallor
- Sweating
- Tachycardia.
2. Signs of vagal stimulation
- Vomiting
- Bradycardia.
3. Signs of impaired myocardial function
- Hypotension and oligouria
- Narrow pulse pressure
- Raised jugular venous pressure
- Third heart sound
- Quite fist heart sound
- Lung crepitations.
4. Signs oftissue damage: Fever and arrhythmia
5. Signs of complications:
- Due to mitral regurgitation
- Due to pericarditis.
- Ventricular ectopic beats
- Ventricular tachycardia
- Heart blocks.
Diagnosis acute myocardial infarction.
Diagnosis of acute myocardial infarction is based on history, characteristics symptoms and signs and investigations.
Investigations acute myocardial infarction.
1. Electrocardiography:
1. ECG is the specific method for confirming the
diagnosis.
2. Typical changes are seen in leads which faces the infracted area. These changes are:
- Elevation of STsegment
- Pathologic Qwaves appear.
- T waves may become tall and peaked in very early myocardial infarction.
T waves are transient and last for a few hours only. - In contrast to transmural lesions, partial thickness or subendothelial infarction causes ST/T wave changes without Qwaves or prominent ST elevation.
- Changes in the ECG are seen which evolve in predictable fashion over next few days to weeks.
2. Blood test:
1. Plasma biochemical markers:
Myocardial infarction leads to detectable rise in the plasma concentration of various enzymes and proteins that are normally concentrated within the cardiac cells.
Plasma enzymes (cardiac injury enzymes) are as follows:
- Creatine kinase (CK).
- Aspartate aminotransferase (AST).
- Lactate dehydrogenase (LDH).
- Myoglobin
- Troponins (troponin I and troponin T)
2. Creatine kinase starts to rise at 4–6 hours and it peaks by about 12 hours and falls to normal in 48–72 hours.
Myocardial isoenzyme of creatine kinase is more specifi. It is useful for diagnosis of early myocardial infarction.
3. Aspartate aminotransferase (AST) starts to rise at about 12 hours and reaches a peak on the fist or second day and returns on third and fourth day.
4. Lactate dehydrogenase (LDH) starts to rise after 12 hours, reaches a peak after 2–3 days and may remain elevated for a week.
Rise in the value of LDH I (anisoenzyme of LDH) is a more sensitive indicator of myocardial infarction than total LDH.
It is useful in diagnosis for patients who present several days after myocardial infarction.
5. Cardiac troponins are cardiac troponinT (cTnT) and cardiac troponinI (cTnI). Sensitivity of troponins is similar to that of isoenzymes of creatine kinase.
Moreover, cTnT remains elevated for 100 to 200 hours after acute myocardial infarction and therefore, it may have particular utility in the evaluation of patients who present suffiently long episode after the pain in chest.
- Leukocytosis with a peak on fist day.
- ESR is raised which may remain raised for some days.
- Creactive protein is elevated.
6. Chest X-ray: It can detect acute pulmonary edema or congestion. It is also helpful to detect pericardial effsion, cardiomegaly, etc.
7. Radionuclide scanning: It shows site of necrosis and the extent of impairment of ventricular function.
8. Echocardiography: This is done for regional wall motion abnormality and ejection fraction.
Treatment acute myocardial infarction.
The management of myocardial infarction is divided into two parts:
1. Early management.
2. Late management.
Early Management acute myocardial infarction.
- Aspirin 150–300 mg to be chewed earliest.
- Sublingual glyceryl trinitrate 0.4–1 mg, to be repeated, if necessary
- Oxygen through nasal cannula at a rate of 2–4 L/min.
- Procure IV line and take blood samples for glucose, lipids and complete haemogram.
- Record 12lead ECG.
- Pain may be relieved by IV morphine (5 mg) plus metoclopramide as an antimetic (10 mg).
- IV betablockers (metoprolol 5 mg every 2–5 minutes for 3 doses) for ongoing chest pain, hypertension and tachycardia provided there is no contraindication.
- Thrombolysis should be done.
- If PTCA is planned, give GP IIb/IIIa inhibitor
- After admission immediately shift the patient to ICU or
ICCU
In Hospital treatment acute myocardial infarction.
Hospitalization and strict Bed rest
- Hospitalize the patient and advice strict bed rest. As early as the patient is hospitalized, the bettr it is.
- Patient should be strictly admittd in ICCU.
Analgesia acute myocardial infarction.
- IV morphine sulphate 10 mg and an anti emetic, i.e. cyclizine 50 mg is given through I.V. cannula.
- The drug is repeated depending on the response till complete analgesia is received and patient feels bettr.
Anti-platelet drugs acute myocardial infarction.
Low dose aspirin, i.e. 75 to 150 mg and clopidogrel 300 mg stat and then 75 mg orally daily is given.
Oxygen therapy acute myocardial infarction.
Inhalation of oxygen increases arterial partial pressure of oxygen, so there is increase in the concentration of oxygen gradient which is responsible for diffusionn of oxygen in ischemic myocardium from adjacent better perfused areas. This is given by facemask or nasal prongs for a day or two after infarction.
Thrombolysis acute myocardial infarction.
- Coronary thrombolysis helps to restore patency of coronary artery preserves left ventricular function and improves survival.
- The choice of drug for thrombolysis is less important than the speed of treatment.
- Streptokinase, 1.5 million units in 100 mL of saline given in an intravenous infusion over 1 hour, is a widely accepted method.
It is a cheap, but being antigenic, sometimes, may cause serious allergic manifestations.
Hence, it can be used once and therapy is changed if the patient requires second thrombolysis within few years.
Alteplase (tissue Plasminagen activator (tPa)
- It is a potent firinolytic drug but is expensive.
- It is less antigenic and does not cause hypotension.
- The current tPA regimen given over 90 minutes (bolus dose of 15 mg followed by 50 mg over 30 minutes and then 35 mg over next 60 minutes) is widely accepted. The other drugs include reteplase given in double dose regime i.e.
10 million units over 2–3 minute followed by another dose of 10 million units after 30 minutes.
Tenectaplase given as bolus dose of 53 mg/kg over 10 seconds. Both reteplase and tenectaplase are known as bolus firinolytics.
Angioplasty
Immediate angioplasty of infarct related artery is safe and is effctive alternative to thrombolysis. It is done in the patients in whom the hazards of thrombolysis is high.
Anti-coagulants
- Subcutaneous heparin, i.e. 7,500 units twice a day for 7–10 days or till discharge of patient from the hospital can be employed.
In patients who do not receive thrombolytic therapy to prevent venous thrombosis. - Patients who receive thrombolytic therapy (tPA) should receive immediate and full doses of heparin (10,000 U bolus plus, l000 U hourly).
Beta-adrenergic Blockers
Acute betaadrenoreceptors blockade intravenous atenolol (5–l0 mg given over 5 minutes) or metoprolol (5–15 mg given over 5 minutes) relieves pain, reduces arrhythmias, salvages myocardium and improves short term mortality in patients who present within l2 hours of onset of pain.
Nitrates and other agents
Sublingual glyceryl trinitrate 0.4 mg is useful in threatened infarction.
Sedatives
Diazepam 5mg for three to four times a day is effctive. It is given for few days.
Diet
- For fist 4 to 5 days low calorie diet which is divided into multiple meals is given.
- If heart failure is present restrict the salt.
- From second week, food should be increased in amount.
Lipid lowering agent
Atorvastatin is given to reduce the LDL levels.
Late Management acute myocardial infarction.
1. Risk stratifiation and further investigations: Prognosis of patient survived after myocardial infarction depends on degree of myocardial damage, any residual ischemia and presence of ventricular arrhythmias.
2. Life style modifiation:
- Stop smoking
- Diet control
- Regular exercise.
3. Secondary prevention
- Antiplatelet agents, i.e. aspirin
- Lipid lowering agents
- Betablockers and ACEI in congestive cardiac failure and hypertension.
- Control of blood sugar in diabetes.
4. Rehabilitation and after care:
- Physical activities should be restricted for 4 to 6 weeks since infarct takes 4–6 weeks to become replaced with firous tissue.
- Gradual mobilization and return to work over 6 weeks.
When there are complications, the regimen has to be modifid accordingly. - Exercise within the limits set by angina and tiredness will do no harm but much good. Same limits apply to sexual activity.
- Control of obesity, regular exercises, cessation of smoking, adoption of a less frenetic way of life and control of plasma lipids by diets and drugs.
- Complications should be managed. Pain relief, reassurance, rest and correction of hypokalemia play a major role in prevention of arrhythmias.
Routine drug therapy acute myocardial infarction.
- Low dose aspirin, i.e. 75 to 150 mg daily and is continued indefiitely.
- Beta-adrenergic blocker should be given for 4 to 6 weeks if there is no contraindication.
- ACE inhibitor, i.e. captopril 25 mg TID or ramipril 2.5 to 5 mg BD
- Lipid lowering agent atorvastatin is given to lower the LDL levels.
Question.37. Write management of acute coronary thrombosis and its prevention.
Answer. It is the formation of blood clot in coronary artery.
Management acute coronary thrombosis
- Thrombolytic agents are used, i.e. streptokinase
- Antiplatelet drugs, i.e. heparin and aspirin
- Anticoagulants, i.e. warfarin
- Platelet glycoprotein receptor antagonist, i.e. abciximab
- When a thrombus is large and life-threatening, surgical removal is done.
Prevention acute coronary thrombosis
- Deep breathing exercise of patient in bed.
- Slight elevation of foot part of bed for bed fast patients.
- Exercise of extremities while on bed
- Maintenance of hydration
- Correction of cardiac failure.
Question.38. Describe the etiology, clinical features, complications and management of acute myocardial infarction.
Answer. Acute myocardial infarction is defied as irreversible damage to myocardium of heart as a result of occlusive thrombus due to rupture of atherosclerotic plaque in coronary artery.
Etiology
- The most important cause of myocardial infarction is atherosclerosis.
- Obesity and hypertension
- Cigarett smoking
- Diabetes mellitus
- Sedentary life cycle.
- Dyslipidemia.
Clinical Features acute myocardial infarction.
Symptoms: acute myocardial infarction.
- Pain: Chest pain is more common and is severe in comparison to angina.
Pain is severe with pallor and peculiar facial expression.
Pain is described as tightness, heaviness and constriction. - Anxiety: It is common and occurs when there is fear of impending death.
- Nausea and vomiting.
- Breathlessness due to fall in cardiac output.
- Collapse or syncope due to arrhythmia and profound hypertension.
Signs: acute myocardial infarction.
1. Signs of sympathetic activation
- Pallor
- Sweating
- Tachycardia.
2. Signs of vagal stimulation
- Vomiting
- Bradycardia.
3. Signs of impaired myocardial function
- Hypotension and oligouria
- Narrow pulse pressure
- Raised jugular venous pressure
- Third heart sound
- Quite fist heart sound
- Lung crepitations.
4. Signs oftissue damage: Fever and arrhythmia
5. Signs of complications:
- Due to mitral regurgitation
- Due to pericarditis.
- Ventricular ectopic beats
- Ventricular tachycardia
- Heart blocks.
Enumeration of complications of Myocardial Infarction
1. Immediate
1. Arrhythmias and conduction disturbances
- Sinus bradycardia
- Ventricular ectopics
- Ventricular tachycardia
- Ventricular firillation
- Idioventricular rhythm
- Atrial firillation
- Heart block
2. Post-myocardial angina can occur in 50% patients occur.
3. Acute circulatory failure.
Management acute myocardial infarction.
The management of myocardial infarction is divided into two parts:
1. Early management.
2. Late management.
Early Management acute myocardial infarction.
- Aspirin 150–300 mg to be chewed earliest.
- Sublingual glyceryl trinitrate 0.4–1 mg, to be repeated, if necessary
- Oxygen through nasal cannula at a rate of 2–4 L/min.
- Procure IV line and take blood samples for glucose, lipids and complete haemogram.
- Record 12lead ECG.
- Pain may be relieved by IV morphine (5 mg) plus metoclopramide as an antimetic (10 mg).
- IV betablockers (metoprolol 5 mg every 2–5 minutes for 3 doses) for ongoing chest pain, hypertension and tachycardia provided there is no contraindication.
- Thrombolysis should be done.
- If PTCA is planned, give GP IIb/IIIa inhibitor
- After admission immediately shift the patient to ICU or
ICCU
Question.39. Write short note on treatment of acute myocardial infarction.
Answer.
In Hospital treatment acute myocardial infarction.
Hospitalization and strict Bed rest
- Hospitalize the patient and advice strict bed rest. As early as the patient is hospitalized, the bettr it is.
- Patient should be strictly admittd in ICCU.
Analgesia acute myocardial infarction.
- IV morphine sulphate 10 mg and an anti emetic, i.e. cyclizine 50 mg is given through I.V. cannula.
- The drug is repeated depending on the response till complete analgesia is received and patient feels bettr.
Anti-platelet drugs acute myocardial infarction.
Low dose aspirin, i.e. 75 to 150 mg and clopidogrel 300 mg stat and then 75 mg orally daily is given.
Oxygen therapy acute myocardial infarction.
Inhalation of oxygen increases arterial partial pressure of oxygen, so there is increase in the concentration of oxygen gradient which is responsible for diffusionn of oxygen in ischemic myocardium from adjacent better perfused areas. This is given by facemask or nasal prongs for a day or two after infarction.
Thrombolysis acute myocardial infarction.
- Coronary thrombolysis helps to restore patency of coronary artery preserves left ventricular function and improves survival.
- The choice of drug for thrombolysis is less important than the speed of treatment.
- Streptokinase, 1.5 million units in 100 mL of saline given in an intravenous infusion over 1 hour, is a widely accepted method.
It is a cheap, but being antigenic, sometimes, may cause serious allergic manifestations.
Hence, it can be used once and therapy is changed if the patient requires second thrombolysis within few years.
Alteplase (tissue Plasminagen activator (tPa)
- It is a potent firinolytic drug but is expensive.
- It is less antigenic and does not cause hypotension.
- The current tPA regimen given over 90 minutes (bolus dose of 15 mg followed by 50 mg over 30 minutes and then 35 mg over next 60 minutes) is widely accepted. The other drugs include reteplase given in double dose regime i.e.
10 million units over 2–3 minute followed by another dose of 10 million units after 30 minutes.
Tenectaplase given as bolus dose of 53 mg/kg over 10 seconds. Both reteplase and tenectaplase are known as bolus firinolytics.
Angioplasty
Immediate angioplasty of infarct related artery is safe and is effctive alternative to thrombolysis. It is done in the patients in whom the hazards of thrombolysis is high.
Anti-coagulants
- Subcutaneous heparin, i.e. 7,500 units twice a day for 7–10 days or till discharge of patient from the hospital can be employed.
In patients who do not receive thrombolytic therapy to prevent venous thrombosis. - Patients who receive thrombolytic therapy (tPA) should receive immediate and full doses of heparin (10,000 U bolus plus, l000 U hourly).
Beta-adrenergic Blockers
Acute betaadrenoreceptors blockade intravenous atenolol (5–l0 mg given over 5 minutes) or metoprolol (5–15 mg given over 5 minutes) relieves pain, reduces arrhythmias, salvages myocardium and improves short term mortality in patients who present within l2 hours of onset of pain.
Nitrates and other agents
Sublingual glyceryl trinitrate 0.4 mg is useful in threatened infarction.
Sedatives
Diazepam 5mg for three to four times a day is effctive. It is given for few days.
Diet
- For fist 4 to 5 days low calorie diet which is divided into multiple meals is given.
- If heart failure is present restrict the salt.
- From second week, food should be increased in amount.
Lipid lowering agent
Atorvastatin is given to reduce the LDL levels.
Late Management acute myocardial infarction.
1. Risk stratifiation and further investigations: Prognosis of patient survived after myocardial infarction depends on degree of myocardial damage, any residual ischemia and presence of ventricular arrhythmias.
2. Life style modifiation:
- Stop smoking
- Diet control
- Regular exercise.
3. Secondary prevention
- Antiplatelet agents, i.e. aspirin
- Lipid lowering agents
- Betablockers and ACEI in congestive cardiac failure and hypertension.
- Control of blood sugar in diabetes.
4. Rehabilitation and after care:
- Physical activities should be restricted for 4 to 6 weeks since infarct takes 4–6 weeks to become replaced with firous tissue.
- Gradual mobilization and return to work over 6 weeks.
When there are complications, the regimen has to be modifid accordingly. - Exercise within the limits set by angina and tiredness will do no harm but much good. Same limits apply to sexual activity.
- Control of obesity, regular exercises, cessation of smoking, adoption of a less frenetic way of life and control of plasma lipids by diets and drugs.
- Complications should be managed. Pain relief, reassurance, rest and correction of hypokalemia play a major role in prevention of arrhythmias.
Routine drug therapy acute myocardial infarction.
- Low dose aspirin, i.e. 75 to 150 mg daily and is continued indefiitely.
- Beta-adrenergic blocker should be given for 4 to 6 weeks if there is no contraindication.
- ACE inhibitor, i.e. captopril 25 mg TID or ramipril 2.5 to 5 mg BD
- Lipid lowering agent atorvastatin is given to lower the LDL level
Question.40. Describe etiology, diagnostic criteria and prophylaxis of acute rheumatic fever.
Answer.
Etiology
- Predisposing causes:
Age should be 5 to 15 years.
Sex has equal incidence - Genetic factors: Family incidence known.
- Social and economic factors: Dampness, overcrowding and under nutrition increases incidence.
- Idiosyncrasy is presumably a factor since 3% of people are involved in streptococcal epidemics develop rheumatic fever.
Diagnosis of rheumatic fever is made by ‘Jones criteria’ which is as follows:
Major criteria Rheumatic Fever
1. Carditis: Rheumatic Fever
- It is pancarditis involving endocardium, myocardium and pericardium.
- It manifests as breathlessness, palpitation and chest pain.
- Tachycardia, cardiomegaly and new or change murmurs
- Aortic regurgitation in 50% cases.
- Pericarditis produces frictional rub and pericardial tenderness.
- Cardiac failure due to myocardial infarction.
2. Sydenham’s chorea: Rheumatic Fever
- Late neurological manifestations that occurs at least three months after the episode of acute rheumatic fever when all signs disappear.
- More common in female.
- It is characterized by involuntary dancing movements of hands, feet or face.
3. Polyarthritis: Rheumatic Fever
- Early feature of illness is non-specifi.
- It is characterized by acute painful symmetric and migratory inflmmation of large joints.
- Classical presentation is acute migratory polyarthritis.
Pain and swelling in involved joints subside or disappear as newer joints get affcted.
4. Erythema marginatum: Rheumatic Fever
Red macules which fade in center, but remain red at the edges and occur mainly on trunk and proximal extremities on face.
5. Subcutaneous nodules: Rheumatic Fever
They are small, dense, firm, painless and are best felt over tendons and bones.
- Nodules appear more than 3 weeks after onset ofother manifestations.
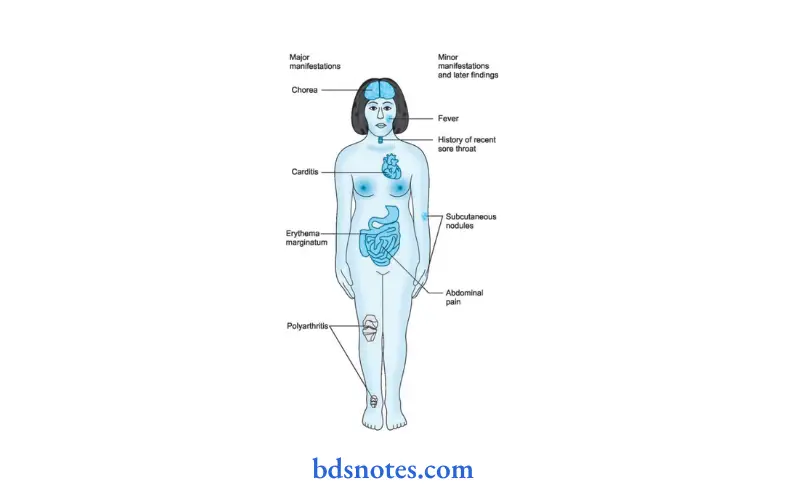
Clinical Rheumatic Fever
- Fever
- Arthralgia
- Previous history of rheumatic fever or rheumatic heart disease.
Laboratory Rheumatic Fever
- Acute phase reactants (leucokytosis, raised ESR, C reactive protein)
- Prolonged PR interval in ECG.
Essential criteria Rheumatic Fever
Evidence for recent streptococcal infection as evidenced by:
1. Increase in ASO titer
- > 333 Todd units (in children).
- > 250 Todd units (in adults).
- Positive throat culture for streptococcal infection
- Recent history of scarlet fever.
Confirmation of Diagnosis Rheumatic Fever
Result is based on Presence of two or more major criterias or one major and two minor criteria, in the presence of essential criteria, is required to diagnose acute rheumatic fever.
Management Acute Rheumatic Fever.
1. Treatment of acute attck: Rheumatic Fever
- Bed rest is important to reduce joint pain and cardiac workload.
Duration of bed rest is guided by markers of inflmmation like temperature,
WBC count and ESR. - Benzathine penicillin 1.2 mu IM 4 hourly. If patient is allergic to penicillin, erythromycin 40–50 mg / kg for ten days is given.
- Aspirin usually relieves symptom of arthritis rapidly.
A starting dose of60 mg/kg body weight per day is given divided into 6 doses.
The dose may be increased to 120 mg / kg body weight.
This dose may produce severe symptoms like vomiting, tachypnea and acidosis. Aspirin is given till ESR comes to normal. - Corticosteroids like prednisolone produces rapid symptomatic relief than aspirin and is indicated in cases with severe arthritis or carditis.
Prednisolone is given in doses of 1.2 mg / kg body weight till ESR comes to normal
2. Secondary prevention: Rheumatic Fever
To prevent further attck of rheumatic fever, longterm prophylaxis is needed.
- Benzathine penicillin 1.2 mu IM is injected at the interval of 21 days.
Further attck is unusual after the age of 21 years and treatment can be stopped. - To prevent chances of endocarditis prophylactic antibiotic therapy should be given.
Question.41. Write short note on prehypertension and its management.
Answer. Prehypertension is considered to be blood pressure readings with a systolic pressure from 120–139 mm Hg or a diastolic pressure from 80–89 mm Hg.
Readings greater than or equal to 140 / 90 mm Hg are considered hypertension.
prehypertension Symptoms
Prehypertension is often asymptomatic (without symptoms) at the time of diagnosis. Only extremely elevated blood pressure (malignant hypertension) can, in rare cases, cause headaches, visual changes, fatigue, or dizziness, but these are nonspecifi symptoms which can occur with many other conditions.
Thus, blood pressures above normal can go undiagnosed for a long period of time.
prehypertension Management
Depending on one’s blood pressure and risk factors for heart disease, one may only need to make a few lifestyle adjustments.
Here are some strategies to help manage prehypertension:
- Lose weight, if one is overweight. Being overweight increases the risk of high blood pressure.
However, losing weight can lower high blood pressure.
Studies show that modest weight loss can prevent hypertension by 20% in overweight people with prehypertension. - Exercise regularly: Exercise helps to lose weight. Exercise also helps in lowering blood pressure.
- Eat plenty offruits, vegetables, whole grains, fih, and low-fat dairy: Studies show high blood pressure can be lowered and prevented with the DASH diet.
This diet is low in sodium and high in potassium, magnesium, calcium,protein, and fier. - Cut back on dietary salt / sodium: A diet high in sodium (salt) can increase blood pressure.
A lowsodium diet can lower high blood pressure or prevent it.
Aim for less than 2,300 milligrams of sodium daily (about 1 teaspoon of table salt). - Eat foods low in saturated and transfat and cholesterol.
Diets high in saturated fat (meats and highfat dairy), transfat (some margarine, snack foods, and pastries) and cholesterol (organ meats, highfat dairy, and egg yolks) may lead to obesity, heart disease, and cancer. - Eat a plant-based or vegetarian diet: Add highprotein soy foods to your diet. Increase servings of fruits and vegetables by adding one serving at a time.
You can add a serving of fruit at lunchtime.
Then add a serving of vegetables at dinner. - Drink only in moderation: Drinking excess alcohol can increase blood pressure. Limit drinking to not more than two drinks a day for men, and one drink a day for women.
Question.42. Write management of unstable angina pectoris.
Or
Write management of unstable angina.
Answer.
1. To control acute disease and stabilize the thrombotic process:
- Hospitalization – to facilitate rapid adjustments in therapy which are usually required.
- Oxygen administration and sedation.
- Therapy with beta blockers and calcium antagonists.
- Sublingual nitrates for immediate relief.
- IV nitrates – IV Nitroglycerin 3-10 µg / min if patient does not sette on above therapy. IV nitrates produce hypotension and regular BP measurements are required and dose is increased.
- Aspirin 325 mg. OD and Clopidogrel 75 mg / day or Prasugrel 10 mg / day.
- Anticoagulation with heparin. Dose 60 U / kg IV bolus followed by 12 U / kg / hr infusion. Low molecular heparin superior to unfractionated heparin in dose of 1 mg / kg 12 hourly subcutaneous.
- Glycoprotein IIb / IIIa receptor inhibitors – which block the receptors that lead to platelet aggregation
- Eptifiatide 180 µg / kg IV bolus followed by 2 µg / kg / min. infusion.
- Tirofian 0.4 pg / kg / min over 30 mins, followed by 0.1 µg / min. infusion.
- Abciximab 0.25 mg / kg IV bolus followed by 0.125 µg / kg / min. infusion.
2. Longterm management of underlying coronary artery disease—with revascularization procedures.
Question.43. Describe types, etiology, sign, symptoms, investigations and outline treatment of infective endocarditis.
Or
Write short note on infective endocarditis.
Or
Describe risk factors clinical features, diagnosis and treatment of infective endocarditis.
Or
Discuse etiology, Clinical feature and treatment of infective endocarditis.
Answer. Infective endocarditis is an illness caused by microbial infection of the cardiac endothelial surface.
Types infective endocarditis
- Acute bacterial endocarditis: Caused by virulent organisms and run its course over days to weeks.
- Subacute bacterial endocarditis: Caused by organisms of low virulence and run its course over weeks to months.
- Non-bacterial thrombotic endocarditis: Sterile vegetations occur in this type.
- Surgical endocarditis: May follow any type of surgery and is caused by Staphylococcus epidermidis.
Etiology
- Generally, the microorganisms attck an already damaged heart.
- The microorganisms responsible are Streptococcus viridans, S.
- faecalis and Staphylococcus aureus. Below given are all the heart defects which lead to infective endocarditis.
Relatively High risk
- Prosthetic heart valves.
- Aortic valve disease
- Mitral regurgitation + stenosis
- Congenital heart disease
- Previous infective endocarditis.
Intermediate risk
- Mitral valve prolapse
- Mitral stenosis
- Tricuspid valve disease
- Pulmonary valve disease
- Asymmetrical septal hypertrophy
- Calcifi aortic sclerosis
- Nonvalvular intracardiac prosthetic implants
Very low risk
- Atrial septal defect
- Atherosclerotic plaques
- Post myocardial infarction thrombi, atrial thrombi and ventricular aneurysms
- Syphilitic aortitis
- Cardiac pacemakers
- Surgically corrected cardiac lesions (without prosthetic implants)
Signs infective endocarditis
1. Signs of infection:
- Fever: Variable, low grade.
- Anaemia: Yellow muddy discoloration of skin.
- Clubbing: of figers and toes occurs early.
- Splenomegaly: after about 6 weeks of illness. Sudden enlargement with tenderness and rub if infarction of spleen. Rarely gross splenomegaly.
- Arthralgia: Sudden transient pain in joints without any effsion.
2. Cardiac signs:
Murmur:
- Organic heart murmur: due to valvular defect or congenital cardiovascular lesions.
- Development of new murmurs: due to perforation of ventricular septum, rupture of sinus of Valsalva, acute mitral regurgitation or acute aortic regurgitation.
- Absence ofmurmur:
- Endocarditis involving mural thrombus complicating healed myocardial infarction.
- Early acute endocarditis involving previously normal valve.
- Tricuspid endocarditis when it exists, may be murmur free.
- Cardiac failure—may occur due to toxic myocarditis.
Systemic embolism: infective endocarditis
1. Arterial:
- Cerebral producing hemiplegia or mycotic aneurysms which may subsequently rupture.
- Renal causing colic and hematuria.
- Retinal with disturbing vision.
- Of mesenteric arteries causing acute abdominal pain; splenic infarction with sudden local pain and perhaps friction.
- Peripheral vessel resulting in gangrene of an extremity. Early prosthetic valve endocarditis.
2. Pulmonary: Recurrent pneumonitis (infective emboli cause abscesses) and arterial rupture.
Immunological:
Thenar and hypothenar eminences:
- Osler’s nodes: Tender, peasized nodules on pads of figers and toes. Often pale in the centre
- May occur in crops. Fade after few days usually without breaking down or leaving any residue.
- Either due to minute emboli in superficial terminal vessels or due to vasculitis.
Laneway lesions: Large nontender macules on palms and soles.
Skin and mucous membranes:
- Petechial hemorrhages in palpebral conjunctivae, buccal and pharyngeal mucous membrane.
- Subungual: Splinter hemorrhages
- Finger and toe tips: Osler’s nodes
- Retina-Roth spots: Lesions with a white centre and red edge. Boatshaped hemorrhage
- Renal: Glomerulonephritis leading to kidney failure.
Symptoms infective endocarditis
- Patient with a known cardiac ailment may start complaining of vague ill health, fatigue, weakness and a lowgrade fever.
- There is presence of pain and marked aches all over the body.
Investigations infective endocarditis
- Blood cultures: In absence of recent or concurrent antibiotic therapy, the fist 3 random blood cultures (2–4 hours apart) are positive in most patients, and blood culture is positive by third day in 90%.
- Urine: Microscopic hematuria most common fiding. Slight albuminuria and hyaline and granular casts also found.
- Hematology: Normocytic. normochromic anemia, usually mild. May be raised ESR and raised Creactive protein.
- Chest radiograph: May be diagnostic in right sided endocarditis, with multiple shadows visible due to an embolic pneumonia.
- ECG: Myocardial infarction seen on ECG may be due to coronary embolism, and a conduction defect may be due to development of an aortic root abscess.
- Echocardiography: Higher sensitivity in identifying vegetation with Transoesophageal echocardiography as compared to transthoracic echocardiography.
Vegetations: An echodense structure attched to the valve or its supporting structures, or lying in the track of a turbulent jet, which is irregular in shape.
Leaflt perforation is best seen as regurgitant jet on color flw mapping.
Annular and periprosthetic echolucent spaces (abscesses) and fitula formation. - Chest X-ray: Shows evidence of cardiomegaly and heart failure.
Treatment infective endocarditis
Treatment during disease Process Sub-Acute Bacterial Endocarditis
- It is mainly antimicrobial treatment. Along with source of infection symptoms are removed as soon as possible.
- Antibiotics should preferably be bactericidal.
- Antibiotics should be administered parenterally to achieve high serum concentration since the vegetation is avascular.
- Therapy is generally of prolonged duration.
- Selection of antibiotics should be based on culture report and minimum inhibitory concentration (MIC) values.
- Empirical therapy may be initiated in acute severe cases after drawing blood samples for culture.
The antibiotics are later changed based on sensitivity reports, if necessary. - Treatment of infective endocarditis should be prompt and adequate.
The list of antibiotics commonly used, their dosage and indications are given below in table.
Antimicrobial therapy for Infective endocarditis
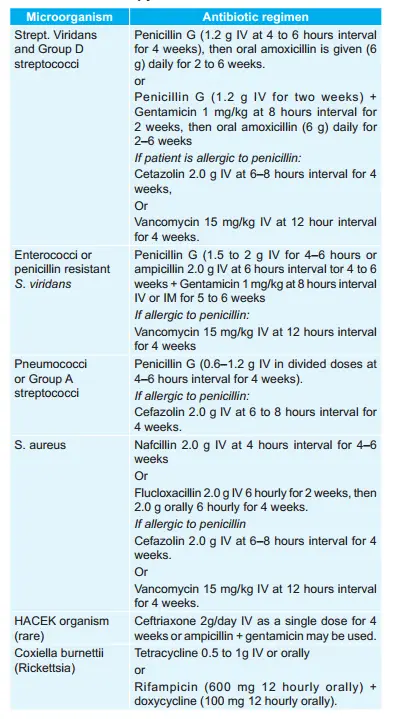
Prophylaxis against Infective endocarditis
Patients with valvular and congenital heart disease who are at high or moderate risk of endocarditis should receiveprophylactic antibiotics before undergoing any procedure which may cause bacteremia.
Antibiotic regimen for prophylaxis of endocarditis in adults at moderate or highrisk is as follows:
1. Oral cavity, respiratory tract, or esophageal procedures (in patients at highrisk, administer a half dose after the initial dose).
- Standard regimen: Amoxicillin 2.0 g oral 1 hour before procedure.
- Inability to take oral medication of standard regimen:
Ampicillin 2.0 g IV or IM within 30 min of procedure. - If patient is allergic to penicillin:
Clarithromycin 500 mg or azithromycin 500 mg orally l hour before procedure.
Or
Cephalexin or cefadroxil 2 g orally 1 hour before procedure
Or
Clindamycin 600 mg oral l hour before procedure - If patient is allergic to penicillin and is unable to take oral medication
Clindamycin 600 mg I.V. 30 min before procedure.
Or
Cefazolin 1.0 g I.V. or IM 30 min before procedure.
2. Genitourinary and gastrointestinal tract procedures:
- In high risk patients: Ampicillin 2g IM or IV + gentamycin 1.5 mg/kg IV or IM within 30 min of starting the procedure followed by ampicillin
- In high-risk patients allergic to penicillin: Vanacomycin 1g IV over 1 to 2 hour + gentamycin 1.5 mg/kg IV or IM combination is given within 30 min of starting the procedure.
- In moderate risk patients: Amoxicillin 2.0 g oral 1 hour before procedure Or ampicillin or amoxicillin 2.0 g IV or IM within 30 min of procedure.
- In moderate riskpatients allergic to penicillin: Vancomycin 1g IV over 1 to 2 hours completed within 30 min of starting procedure.
Question.44. Describe etiology, diagnostic criteria, complications and management of rheumatic fever.
Answer.
Etiology
- Predisposing causes:
Age should be 5 to 15 years.
Sex has equal incidence - Genetic factors: Family incidence known.
- Social and economic factors: Dampness, overcrowding and under nutrition increases incidence.
- Idiosyncrasy is presumably a factor since 3% of people are involved in streptococcal epidemics develop rheumatic fever.
Major criteria Rheumatic Fever
1. Carditis: Rheumatic Fever
- It is pancarditis involving endocardium, myocardium and pericardium.
- It manifests as breathlessness, palpitation and chest pain.
- Tachycardia, cardiomegaly and new or change murmurs
- Aortic regurgitation in 50% cases.
- Pericarditis produces frictional rub and pericardial tenderness.
- Cardiac failure due to myocardial infarction.
2. Sydenham’s chorea: Rheumatic Fever
- Late neurological manifestations that occurs at least three months after the episode of acute rheumatic fever when all signs disappear.
- More common in female.
- It is characterized by involuntary dancing movements of hands, feet or face.
3. Polyarthritis: Rheumatic Fever
- Early feature of illness is non-specifi.
- It is characterized by acute painful symmetric and migratory inflmmation of large joints.
- Classical presentation is acute migratory polyarthritis.
Pain and swelling in involved joints subside or disappear as newer joints get affcted.
4. Erythema marginatum: Rheumatic Fever
Red macules which fade in center, but remain red at the edges and occur mainly on trunk and proximal extremities on face.
5. Subcutaneous nodules: Rheumatic Fever
They are small, dense, firm, painless and are best felt over tendons and bones.
- Nodules appear more than 3 weeks after onset ofother manifestations.
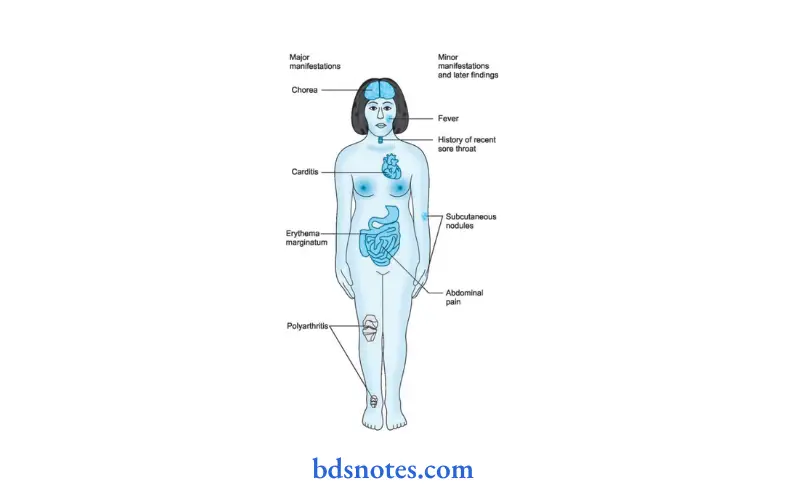
Management Acute Rheumatic Fever.
1. Treatment of acute attck: Rheumatic Fever
- Bed rest is important to reduce joint pain and cardiac workload.
Duration of bed rest is guided by markers of inflmmation like temperature,
WBC count and ESR. - Benzathine penicillin 1.2 mu IM 4 hourly. If patient is allergic to penicillin, erythromycin 40–50 mg / kg for ten days is given.
- Aspirin usually relieves symptom of arthritis rapidly.
A starting dose of60 mg/kg body weight per day is given divided into 6 doses.
The dose may be increased to 120 mg / kg body weight.
This dose may produce severe symptoms like vomiting, tachypnea and acidosis. Aspirin is given till ESR comes to normal. - Corticosteroids like prednisolone produces rapid symptomatic relief than aspirin and is indicated in cases with severe arthritis or carditis.
Prednisolone is given in doses of 1.2 mg / kg body weight till ESR comes to normal
2. Secondary prevention: Rheumatic Fever
To prevent further attck of rheumatic fever, longterm prophylaxis is needed.
- Benzathine penicillin 1.2 mu IM is injected at the interval of 21 days.
Further attck is unusual after the age of 21 years and treatment can be stopped. - To prevent chances of endocarditis prophylactic antibiotic therapy should be given.
Complications infective endocarditis
Inflmmation caused by rheumatic fever may last for a few weeks to several months. In some cases, the inflmmation may cause longterm complications.
Rheumatic heart disease is permanent damage to the heart caused by the inflmmation of rheumatic fever. Problems are most common with the valve between the two left chambers of the heart (mitral valve), but the other valves may be affcted.
The damage may result in one of the following conditions:
- Valve stenosis: This condition is a narrowing of the valve,which results in decreased blood flw.
- Valve regurgitation: This condition is a leak in the valve,which allows blood to flw in the wrong direction.
- Damage to heart muscle: The inflmmation associated with rheumatic fever can weaken the heart muscle, resulting in poor pumping function.
Damage to the mitral valve, other heart valves or other heart tissues can cause problems with the heart later in life.
Resulting conditions may include:
- Atrial firillation, an irregular and chaotic beating of the upper chambers of the heart (atria).
- Heart failure, an inability of the heart to pump enough blood to the body.
Question.45.Write the diffrence between cardiac and non-cardiac chest pains.
Answer.
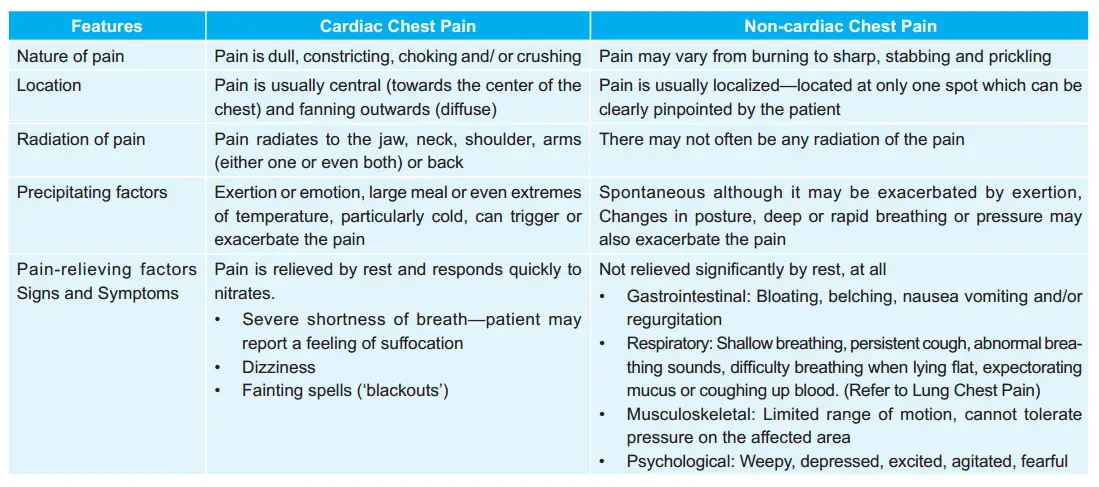
Question.46. Give defiition, etiology, sign and symptoms, investigation and treatment of congestive cardiac failure.
Or
Write clinical features, investigations and treatment of congestive cardiac failure.
Answer. It is defied as a pathophysiologic state when heart is not able to maintain its cardiac output to meet the demands of metabolizing tissues or can do so only at the expense of elevating filing pressures.
In congestive cardiac failure, patient has features of both right and leftsided heart failure.
Etiology
Left-sided Failure congestive cardiac failure.
1. Myocardial damage:
- Myocardial infarction
- Myocarditis
- Cardiomyopathy
- Cardiac depressant drugs.
2. Increased load:
- Hypertension
- Mitral and aortic valve disease
- Cardiac arrhythmias
- Over transfusion.
Right-sided Failure congestive cardiac failure.
1. Pulmonary hypertension:
- Secondary to left heart failure
- Chronic lung disease
- Pulmonary embolism
- Lefttoright shunts.
- Primary pulmonary hypertension.
- Right ventricular infarction.
- Pulmonary and tricuspid valve disease
- Isolated right ventricular cardiomyopathy.
Signs and symptoms/ clinical Features congestive cardiac failure.
Left-sided Failure congestive cardiac failure.
- Common respiratory signs are tachypnea (increased rate of breathing) and increased work of breathing (non-specifi signs of respiratory distress).
Rales or crackles, heard initially in the lung bases, and when severe, throughout the lung filds suggest the development of pulmonary edema (flid in the alveoli). Cyanosis which suggests severe hypoxemia, is a late sign of extremely severe pulmonary edema. - Additional signs indicating left ventricular failure include a laterally displaced apex beat (which occurs, if the heart is enlarged) and a gallop rhythm (additional heart sounds) may be heard as a marker of increased blood flw, or increased intracardiac pressure.
Heart murmurs may indicate the presence of valvular heart disease, either as a cause (e.g. aortic stenosis) or as a result (e.g. mitral regurgitation) of the heart failure. - Backward failure of the left ventricle causes congestion of the pulmonary vasculature, and so the symptoms are predominantly respiratory in nature.
- Patient will have dyspnea (shortness of breath) on exertion and in severe cases, dyspnea at rest.
- Increasing breathlessness on lying flt, called orthopnea, occurs. It is often measured in the number of pillows required to lie comfortably, and in severe cases, the patient may resort to sleeping while sittng up.
- Another symptom of heart failure is paroxysmal nocturnal dyspnea a sudden night time attck of severe breathlessness, usually several hours after going to sleep.
- Easy fatigability and exercise intolerance are also common complaints related to respiratory compromise.
- Cardiac asthma or wheezing may occur.
- Compromise of left ventricular forward function may result in symptoms of poor systemic circulation such as dizziness, confusion and cool extremities at rest.
Right-sided Failure congestive cardiac failure.
- Physical examination may reveal pittng peripheral edema, ascites, and hepatomegaly.
- Jugular venous pressure is frequently assessed as a marker of flid status, which can be accentuated by eliciting hepatojugular reflx.
- Backward failure of the right ventricle leads to congestion of systemiccapillaries. Thisgenerates excessflid accumulation in the body.
This causes swelling under the skin (termed peripheral edema or anasarca) and usually affects the dependent parts of the body fist (causing foot and ankle swelling in people who are standing up, and sacral edema in people who are predominantly lying down). - Nocturia (frequent night time urination) may occur when flid from the legs is returned to the bloodstream while lying down at night.
- In progressively severe cases, ascites (flid accumulation in the abdominal cavity causing swelling) and hepatomegaly (enlargement of the liver) may develop.
- Signifiant liver congestion may result in impaired liver function, and jaundice and even coagulopathy (problems of decreased blood clottng) may occur.
Investigation congestive cardiac failure.
- Electrocardiogram (ECG): This will reveal arrhythmias, ventricular hypertrophy and myocardial ischemia.
- Chest X-ray: This will show enlargement of heart, peripheral lung congestion, presence of Kerley’s lines, pulmonary edema, hydrothorax, pulmonary hypertension, double atrial shadow in mitral valve disease and calcifiation of valves.
- Echocardiogram: In this ultrasound is used to image the heart muscle, valve structures, and blood flw pattrns.
The echocardiogram is very helpful in diagnosing heart muscle weakness.
In addition, the test can suggest possible causes for the heart muscle weakness (for example, prior heart attck, and severe valve abnormalities).
Virtually all patients in whom the diagnosis of congestive heart failure is suspected should ideally undergo echocardiography early in their assessment. - Nuclear medicine studies assess the overall pumping capability of the heart and examine the possibility of inadequate blood flw to the heart muscle.
- BNP or B-type natriuretic peptide level: This level can vary with age and gender but is typically elevated from heart failure and can aid in the diagnosis, and can be useful in following the response to treatment of congestive heart failure.
- Blood urea and electrolytes: It is done for hypokalemia,hyponatremia and renal failure,
Treatment congestive cardiac failure.
- Rest: Complete bed rest is the key stone of management.
When the patient is dyspneic, bed rest is given with the head end of bed raised to 45°.
The legs should be kept below the pelvis to prevent the flid present in legs to return to vascular system and precipitate pulmonary edema. - Diet: Basic aim is to restrict sodium in the diet. Quantity of salt intake per day should not exceed 0.5 gm.
Salt substitutes may be used to make diet more palatable. - Diuretics: In cardiac failure, there is always sodium and water retention. Hence, diuretics are given to increase sodium extraction.
Furosemide 40–80 mg orally produces effct in 4–6 hours and on IV administration of furosemide 40–100 mg produces its effct in 20 minutes.
Spironolactone which is potassium sparing diuretic is given 25 mg orally 4 times a day which removes the symptoms such as hypokalemia due to action of furosemide.
Triamterene or amiloride hydrochloride is given along with spironolactone. - Digitalis: It increases the force of myocardial contraction and decreases work of heart. The commonly used drug is digoxin which is administered orally 0.25 mg BD.
For rapid digitalization digoxin 0.5–0.75 mg is given slow IV over a period of 5–10 minutes under electrocardiographic control. - Sympathomimetic amines: Dopamine at low doses of 3–5 μg/kg / min increases contractility of heart.
- Vasodilators: Sodium nitroprusside in the dose of 5–10 μg/min have balance dilator effct. Besides this hydralazine,nitrates and ACE inhibitors are used.
- Inodilator levosimendan: This is a calcium channel sensitizer.
It has positive inotropic and vasodilator effct.
It is given IV with loading dose of 6–12µg/kg/min over 10 min followed by infusion 0.05 to 2 µg/kg/min infusion. - Oxygen: It is given via Woulfe’s bottle at rate of 5–8 L/min.
- Miscellaneous drugs: Tranquilizers such as diazepam 2 to 5mg TDS are given to reduce anxiety.
- Cardiac re-synchronization therapy or biventricular pacing: It is used in patients with symptomatic refractory cardiac failure with conduction abnormality or Left Bundle Branch Block.
This therapy involves pacing the right atrium, right ventricle and left ventricle to improve synchrony of thecardiac chambers. - Left ventricular assist device: Devices such as Intraaortic balloon pump, Impella device, HeartMate, Thoracic are considered when medical management fails. They are usually used as a bridge to cardiac transplant.
Question.47. Write on management of cardiac arrest.
Answer. Cardiac arrest is defied as sudden failure of heartresulting in inadequate cerebral circulation.
Management cardiac arrest.
1. Basic life support or Basic cardiac life support
Maintain the airway, breathing and circulation simultaneously as rapidly as possible as follows:
- Airway: Airway must be patent. If any of the foreign body is suspected, the patient must be rolled on one side and 4–5 forceful blows must be delivered rapidly between the shoulder blades with the heel of the hand.
Now keep the patient in supine position and abdominal thrusts in an upward direction are given to the patient just below the xiphisternum.
After the foreign body is excluded, patient should be kept in supine position as he may require external cardiac massage and artifiial respiration.
The patient’s head should be lifted with one hand under the neck and the other hand pressing the forehead so that the head is tilted backwards to keep the upper airway patent. - Breathing: Once the patency of airway is maintained, and if breathing is inadequate, artifiial ventilation must be given. With the above position, the patient’s nostrils must be sealed with thumb and index figer and mouthtomouth respiration must be given to the patient.
This is done by taking a deep inspiration and exhaling in the patient’s mouth and then the patient is allowed to exhale passively.
Continue this procedure at the rate of 16-18/min. In hospitals, an Ambu bag is used. - Circulation: With the patient in supine position, neck extended and legs elevated a sudden sharp thrust is given on the chest wall.
This may restore the effctive beating of the heart especially, if the cardiac arrest is due to cardiac standstill.
In absence of response, external cardiac massage is given.
2. Advanced Cardiac Life Support (ACLS)
As the basic life support is maintained an ECG must be taken to determine whether the cause of cardiac arrest is ventricular asystole or ventricular firillation.
1. If it is ventricular asystole, while electric methods of treatment like external cardiac pacemaker are made available, the following drugs are given;
- Epinephrine (Adrenaline): 1 mL of 1:1000 epinephrine is given intravenous followed by a bolus of dextrose.
- Calcium: 10 mL calcium gluconate 10% is injected IV or sometimes intracardiac. It is rarely used.
- Sodium bicarbonate: 10 mL of 7.5% sodium bicarbonate is infused slowly intravenously to correct metabolic acidosis. This is also rarely used.
- Vasopressors: Norepinephrine 1:1000 is initially given in the dose of 2 mL and later repeated, if hypotension persists.
2. lf it is ventricular firillation the following drugs are used in addition:
- Lignocaine: 50–100 mg is injected intravenously as a bolus and may be repeated after 15–20 min.
- Propranolol: 5–10 mg may be given intravenously as an antiarrhythmic agent.
- Bretylium tosylate: It is given as 5 to 10mg/kg IV
2. Specifi measures cardiac arrest.
- For ventricular asystole: If cardiac arrest persists in spite of the above measures, external cardiac pacing is done.
If this is negative or required for a long period, internal cardiac pacemaker is inserted. - For ventricular firillation: If the above drugs do not immediately revert the cardiac rhythm, or if ventricular firillation is recurrent inspite of the above measures a direct current (DC) shock is given to the heart with 200 joules.
It should be repeated, if required after a few minutes with 300 V Joules and then up to 400 Joules.
3. Management after successful resuscitation in an unconscious patient
- Endotracheal Intubation with controlled ventilation should be continued with the help of a ventilator to keep the partial pressure of oxygen at 100 mm Hg and partial pressure of carbon dioxide at 30-40 mm Hg.
- Blood pressure must be maintained at 10mm Hg systolic, if required with the help of vasopressors like dopamine.
- Acid-base and flid electrolyte balance should be maintained.
- Mannitol 350 to 500 mL I.V. or dexamethasone 4 mg 6 to 8 hourly I.V. should be given in presence of cerebral edema.
- Phenytoin sodium, diazepam or phenobarbitone should be given if there are convulsions.
- Aspiration pneumonia should be prevented by appropriate antibiotics.
Question.48. Write in brief sign, symptoms and treatment of rheumatic fever.
Or
Write signs and symptoms of acute rheumatic fever.
Answer. It is an acute, recurrent, inflmmatory disease mainly of children typically occurring 1 to 5 weeks after Group A streptococcal infection.
Symptoms rheumatic fever
- Pyrexia of unknown origin.
- Arthralgia, i.e. pain in joints. Pain in joints is fleting and migratory.
Signs rheumatic fever
Carditis rheumatic fever
- It is pancarditis involving endocardium, myocardium and pericardium.
- It manifests as breathlessness, palpitation and chest pain.
tachycardia, cardiomegaly and new or change murmurs. - Aortic regurgitation in 50% cases.
- Pericarditis produces frictional rub and pericardial tenderness.
- Cardiac failure due to myocardial infarction.
Sydenham’s chorea rheumatic fever
- Late neurological manifestations that occurs at least three months after the episode of acute rheumatic fever when all signs disappear.
- More common in female.
- It is characterized by involuntary dancing movements of hands, feet or face.
Arthritis rheumatic fever
- Early feature of illness and is non-specifi.
- It is characterized by acute painful symmetric and migratory inflmmation of large joints.
Erythema Marginatum rheumatic fever
Red macules which fade in center but remain red at the edges and occur mainly on trunk and proximal extremities on face.
Subcutaneous nodules
- They are small, dense and fim and painless and are best felt over tendons and bones.
- Nodules appear more than 3 weeks after onset of other manifestations.
Respiratory rheumatic fever
Epistaxis is an atypical manifestation.
Gastrointestinal rheumatic fever
Mild gastroenteritis is present. Repeated vomiting spells are present.
Question.49. Write in brief sign, symptoms and treatment of hypertension.
Answer. Hypertension refers to increase in the blood pressure.
Symptoms hypertension.
1. General: Presence of headache, dizziness, palpitation and easy fatigability
2. Symptoms referable to systemic vascular involvement:
- Epistaxis
- Hematuria
- Blurring of vision or sudden blindness
- Dyspnea on exertion
- Anginal chest pain
- Palpitations
- Transient ischemic episodes leading to weakness or paralysis
- Hypertensive encephalopathy
- Tinnitus
- Syncope
3. Symptoms related to underlying disease:
- Edema and puff face due to acute nephritis
- Weight gain, hirsutism, truncal obesity due to Cushing’s syndrome
- Weight loss, tremors, palpitation and sweating due to hyperthyroidism or pheochromocytoma
- Joint pain, bronchospasm and peripheral vascular disease symptoms due to polyarteritis nodosa.
Signs hypertension.
- Moon’s face, buffalo hump and truncal obesity in Cushing’s syndrome.
- Presence of puff face, rough skin, obesity in myxedema
- Tremors, tachycardia, exophthalmos, thyroid dermopathy and goiter in hyperthyroidism
- Prognathism, clubbed hand, coarse features in acromegaly
- Palpable kidney lump in polycystic kidney
- Bruit over abdominal aorta.
- Undiagnosed fever and recurrent urinary infections in chronic pyelonephritis.
Question.50. Write short note on congestive cardiac failure.
Or
Write sign and symptoms of congestive cardiac failure.
Or
Describe in brief congestive cardiac failure
Answer.
Answer. It is defied as a pathophysiologic state when heart is not able to maintain its cardiac output to meet the demands of metabolizing tissues or can do so only at the expense of elevating filing pressures.
In congestive cardiac failure, patient has features of both right and leftsided heart failure.
Etiology
Left-sided Failure congestive cardiac failure.
1. Myocardial damage:
- Myocardial infarction
- Myocarditis
- Cardiomyopathy
- Cardiac depressant drugs.
2. Increased load:
- Hypertension
- Mitral and aortic valve disease
- Cardiac arrhythmias
- Over transfusion.
Right-sided Failure congestive cardiac failure.
1. Pulmonary hypertension:
- Secondary to left heart failure
- Chronic lung disease
- Pulmonary embolism
- Lefttoright shunts.
- Primary pulmonary hypertension.
- Right ventricular infarction.
- Pulmonary and tricuspid valve disease
- Isolated right ventricular cardiomyopathy.
Signs and symptoms/ clinical Features congestive cardiac failure.
Left-sided Failure congestive cardiac failure.
- Common respiratory signs are tachypnea (increased rate of breathing) and increased work of breathing (non-specifi signs of respiratory distress).
Rales or crackles, heard initially in the lung bases, and when severe, throughout the lung filds suggest the development of pulmonary edema (flid in the alveoli). Cyanosis which suggests severe hypoxemia, is a late sign of extremely severe pulmonary edema. - Additional signs indicating left ventricular failure include a laterally displaced apex beat (which occurs, if the heart is enlarged) and a gallop rhythm (additional heart sounds) may be heard as a marker of increased blood flw, or increased intracardiac pressure.
Heart murmurs may indicate the presence of valvular heart disease, either as a cause (e.g. aortic stenosis) or as a result (e.g. mitral regurgitation) of the heart failure. - Backward failure of the left ventricle causes congestion of the pulmonary vasculature, and so the symptoms are predominantly respiratory in nature.
- Patient will have dyspnea (shortness of breath) on exertion and in severe cases, dyspnea at rest.
- Increasing breathlessness on lying flt, called orthopnea, occurs. It is often measured in the number of pillows required to lie comfortably, and in severe cases, the patient may resort to sleeping while sittng up.
- Another symptom of heart failure is paroxysmal nocturnal dyspnea a sudden night time attck of severe breathlessness, usually several hours after going to sleep.
- Easy fatigability and exercise intolerance are also common complaints related to respiratory compromise.
- Cardiac asthma or wheezing may occur.
- Compromise of left ventricular forward function may result in symptoms of poor systemic circulation such as dizziness, confusion and cool extremities at rest.
Right-sided Failure congestive cardiac failure.
- Physical examination may reveal pittng peripheral edema, ascites, and hepatomegaly.
- Jugular venous pressure is frequently assessed as a marker of flid status, which can be accentuated by eliciting hepatojugular reflx.
- Backward failure of the right ventricle leads to congestion of systemiccapillaries. Thisgenerates excessflid accumulation in the body.
This causes swelling under the skin (termed peripheral edema or anasarca) and usually affects the dependent parts of the body fist (causing foot and ankle swelling in people who are standing up, and sacral edema in people who are predominantly lying down). - Nocturia (frequent night time urination) may occur when flid from the legs is returned to the bloodstream while lying down at night.
- In progressively severe cases, ascites (flid accumulation in the abdominal cavity causing swelling) and hepatomegaly (enlargement of the liver) may develop.
- Signifiant liver congestion may result in impaired liver function, and jaundice and even coagulopathy (problems of decreased blood clottng) may occur.
Investigation congestive cardiac failure.
- Electrocardiogram (ECG): This will reveal arrhythmias, ventricular hypertrophy and myocardial ischemia.
- Chest X-ray: This will show enlargement of heart, peripheral lung congestion, presence of Kerley’s lines, pulmonary edema, hydrothorax, pulmonary hypertension, double atrial shadow in mitral valve disease and calcifiation of valves.
- Echocardiogram: In this ultrasound is used to image the heart muscle, valve structures, and blood flw pattrns.
The echocardiogram is very helpful in diagnosing heart muscle weakness.
In addition, the test can suggest possible causes for the heart muscle weakness (for example, prior heart attck, and severe valve abnormalities).
Virtually all patients in whom the diagnosis of congestive heart failure is suspected should ideally undergo echocardiography early in their assessment. - Nuclear medicine studies assess the overall pumping capability of the heart and examine the possibility of inadequate blood flw to the heart muscle.
- BNP or B-type natriuretic peptide level: This level can vary with age and gender but is typically elevated from heart failure and can aid in the diagnosis, and can be useful in following the response to treatment of congestive heart failure.
- Blood urea and electrolytes: It is done for hypokalemia,hyponatremia and renal failure,
Treatment congestive cardiac failure.
- Rest: Complete bed rest is the key stone of management.
When the patient is dyspneic, bed rest is given with the head end of bed raised to 45°.
The legs should be kept below the pelvis to prevent the flid present in legs to return to vascular system and precipitate pulmonary edema. - Diet: Basic aim is to restrict sodium in the diet. Quantity of salt intake per day should not exceed 0.5 gm.
Salt substitutes may be used to make diet more palatable. - Diuretics: In cardiac failure, there is always sodium and water retention. Hence, diuretics are given to increase sodium extraction.
Furosemide 40–80 mg orally produces effct in 4–6 hours and on IV administration of furosemide 40–100 mg produces its effct in 20 minutes.
Spironolactone which is potassium sparing diuretic is given 25 mg orally 4 times a day which removes the symptoms such as hypokalemia due to action of furosemide.
Triamterene or amiloride hydrochloride is given along with spironolactone. - Digitalis: It increases the force of myocardial contraction and decreases work of heart. The commonly used drug is digoxin which is administered orally 0.25 mg BD.
For rapid digitalization digoxin 0.5–0.75 mg is given slow IV over a period of 5–10 minutes under electrocardiographic control. - Sympathomimetic amines: Dopamine at low doses of 3–5 μg/kg / min increases contractility of heart.
- Vasodilators: Sodium nitroprusside in the dose of 5–10 μg/min have balance dilator effct. Besides this hydralazine,nitrates and ACE inhibitors are used.
- Inodilator levosimendan: This is a calcium channel sensitizer.
It has positive inotropic and vasodilator effct.
It is given IV with loading dose of 6–12µg/kg/min over 10 min followed by infusion 0.05 to 2 µg/kg/min infusion. - Oxygen: It is given via Woulfe’s bottle at rate of 5–8 L/min.
- Miscellaneous drugs: Tranquilizers such as diazepam 2 to 5mg TDS are given to reduce anxiety.
- Cardiac re-synchronization therapy or biventricular pacing: It is used in patients with symptomatic refractory cardiac failure with conduction abnormality or Left Bundle Branch Block.
This therapy involves pacing the right atrium, right ventricle and left ventricle to improve synchrony of thecardiac chambers. - Left ventricular assist device: Devices such as Intraaortic balloon pump, Impella device, HeartMate, Thoracic are considered when medical management fails. They are usually used as a bridge to cardiac transplant.
Question.51.Describe the defiition, etiology, clinical features,diagnostic criteria and management of acute rheumatic fever.
Or
Discuss, etiology, clinical features, diagnostic criteria and management of acute rheumatic fever.
Answer.
Symptoms rheumatic fever
- Pyrexia of unknown origin.
- Arthralgia, i.e. pain in joints. Pain in joints is fleting and migratory.
Signs rheumatic fever
Carditis rheumatic fever
- It is pancarditis involving endocardium, myocardium and pericardium.
- It manifests as breathlessness, palpitation and chest pain.
tachycardia, cardiomegaly and new or change murmurs. - Aortic regurgitation in 50% cases.
- Pericarditis produces frictional rub and pericardial tenderness.
- Cardiac failure due to myocardial infarction.
Sydenham’s chorea rheumatic fever
- Late neurological manifestations that occurs at least three months after the episode of acute rheumatic fever when all signs disappear.
- More common in female.
- It is characterized by involuntary dancing movements of hands, feet or face.
Arthritis rheumatic fever
- Early feature of illness and is non-specifi.
- It is characterized by acute painful symmetric and migratory inflmmation of large joints.
Erythema Marginatum rheumatic fever
Red macules which fade in center but remain red at the edges and occur mainly on trunk and proximal extremities on face.
Subcutaneous nodules
- They are small, dense and fim and painless and are best felt over tendons and bones.
- Nodules appear more than 3 weeks after onset of other manifestations.
Respiratory rheumatic fever
Epistaxis is an atypical manifestation.
Gastrointestinal rheumatic fever
Mild gastroenteritis is present. Repeated vomiting spells are present.
Clinical Manifestations Acute Rheumatic Fever.
- Prodromal phase: Tonsillitis or sore throat 1 to 4 weeks prior to onset of acute rheumatic fever. Besides this anorexia, pallor, fatigability and nervous irritability is present.
- Latent phase: When antibodies to preceding streptococcal infection are produced.
- Phase of onset of rheumatic fever/mode of onset.
Arthritis and fever 2–3 weeks after infection. - Cardiac symptoms 3–6 weeks after infection is fist to draw attntion.
- Abdominal symptoms: Abdominal pain and tenderness, nausea, vomiting, fever and leukocytosis.
- Pyrexia of unknown origin
- Typhoid or inflenzal mode of onset with fever
- Nodules of skin lesion.
Treatment of acute rheumatic Fever
- Bed rest is important to reduce joint pain and cardiac workload.
Duration of bed rest is guided by markers of inflmmation like temperature, WBC count and ESR. - Benzathine penicillin 1.2 mu IM 4 hourly.
If patient is allergic to penicillin, erythromycin 40–50 mg / kg for ten days is given. - Aspirin usually relieves symptom of arthritis rapidly.
A starting dose of 60 mg / kg body weight per day is given divided into 6 doses.
The dose may be increased to 120 mg / kg body weight.
This dose may produce severe symptoms like vomiting, tachypnea and acidosis is given till ESR comes to normal. - Corticosteroids like prednisolone produces rapid symptomatic relief than aspirin and is indicated in cases with severe arthritis or carditis.
Prednisolone is given in doses of 1.2 mg / kg body weight till ESR comes to normal.
Question.52. Write short note on congenital heart disease.
Answer. Congenital heart diseases are the abnormalities of heart and great vessels due to defective development in the prenatal period.
Classification congenital heart disease
1. Acyanotic:
- Acyanotic with left to right shunt:
- Atrial septal defect (ASD)
- Ventricular septal defect (VSD)
- Patent ductus arteriosus
- Aortopulmonary window
- Common complete atrioventricular canal.
2. Acyanotic without shunt:
- Pulmonary stenosis
- Endocardial cushion effcts
- Aortic stenosis
- Coarctation of aorta.
3. Cyanotic:
- Complete transposition of great vessels
- Persistent truncus arteriosus
- Tetralogy of Fallot
- Ebstein’s anomaly with righttoleft shunt
- Common atrium.
Etiology
- Patent Ductus arteriosus: Maternal cause, Patau’s syndrome
- Atrial septal defect: Rubella virus, Noonan’s syndrome, HoltOram syndrome, Down syndrome, Patau’s syndrome,
- Ventricular septal defect: Alcohol, HoltOram syndrome,
- Down’s syndrome, Edward’s syndrome.
- Tricuspid atresia: Alcohol
- Fallot’s Tetralogy: Down’s syndrome, lesions associated with 22q11 deletions.
Features of various congenital Heart diseases
- Central cyanosis and digital clubbing is present in transposition of great vessels and tetralogy of Fallot.
- Growth retardation as well as intellectual impairment is present in all congenital heart diseases.
- Syncope is present in severe right or left ventricular outflw tract obstruction.
Short stature is commonly seen in patients with congenital heart disease.
Question.53. Describe JNC VII criteria for hypertension. Write in brief investigations and outline treatment.
Answer. JNC VII criterias is the 7th report of the Joint National Committe on Prevention Detection, Evaluation and Treatment of High Blood Pressure.
Jnc vII criteria for Hypertensio
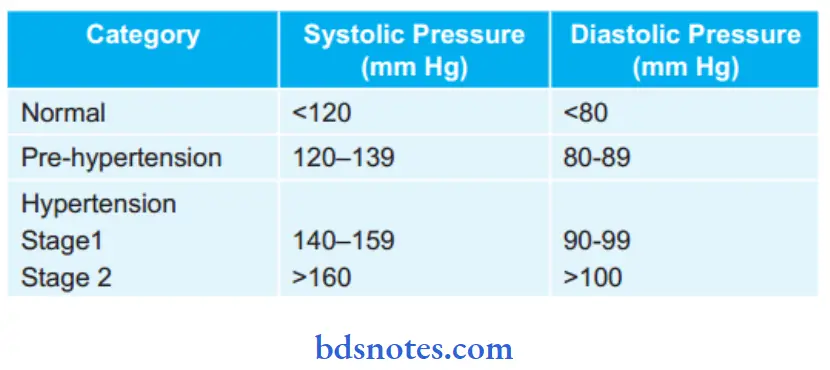
Hypertension should be based on average of two or more readings taken at each of two or more visits after initial reading.
Investigations criteria for hypertension
1. Routine tests: criteria for hypertension
- Urinalysis: Detection of proteinuria and microscopic hematuria may indicate some degree of renal arteriolar necrosis and nephrosclerosis, or underlying intrinsic renal disease such as polycystic kidneys, chronic pyelonephritis or glomerulonephritis.
- Serum biochemistry: High sodium and low potassium may suggest primary hyperaldosteronism.
- Urea and creatinine: High levels suggest a degree of renal impairment due to hypertension, or that underlying renal disease is the cause for hypertension.
- Lipid and glucose concentrations: To judge cardiovascular risk status for each patient.
- ECG: Detection of left ventricular hypertrophy and strain pattrn is an important adverse prognostic indicator.
2. Special tests: criteria for hypertension
- Intravenous pyelogram and renal ultrasound, if renal disease is present.
- Renal arteriography for renal artery stenosis
- Plasma rennin activity and aldosterone for Conn syndrome
- Angiography / MRI for coarctation of aorta.
Treatment criteria for hypertension
Management criteria for hypertension
Nonpharmacological treatment
1. Salt restriction: Modest sodium restriction 2.4 gm sodium or 6 gm NaCl is effctive in controlling hypertension.
2. Weight reduction: In overweight persons, reduction of 1 kg may reduce 1.6 to 1.3 mm Hg of blood pressure
3. Stop smoking: Smoking raises BP. It is an independent and most important reversible coronary risk factor.
4. Diet: Lactovegetarian diet and high intake of poly unsaturated fih oils have high potassium levels and lower blood pressure by:
- Increased sodium extraction
- Decreased sympathetic activity
- Decreased renninangiotensin secretion and direct dilatation of removal of renal arteries
- Adequate calcium and magnesium intake should be maintained in diet
5. Limit of alcohol intake is done
6. Various forms of relaxation like yoga, biofeedback and psychotherapy lower the blood pressure
7. Regular exercise, relaxation exercise.
Pharmacological therapy criteria for hypertension
1. Diuretics: Commonly used diuretics are hydrochlorothiazide 100 mg per day, chlorthalidone 50–100 mg/day.
The reduced potassium levels in body results in hypokalemia, potassium supplements have to be given in people on longterm diuretic therapy.
Potassium sparing diuretics, i.e. spironolactone 25 mg TDS is given.
2. Beta-blockers: Propranolol was used extensively as effctive antihypertensive drug. The dose administered as 40–160 mg/day.
3. Calcium channel blockers: Nifedipine 16 to 20 mg BD is administered. Side effects are headache, dizziness, flshing.
Drug is contraindicated in acute myocardial infarction, cardiogenic shock, pregnancy and is used with caution in diabetics and edema.
Felodipine sulfate 5 to 10 mg/day is effctive in mild to moderate hypertension.
Amlodipine 5 to 10 gm is effective and is safe in hypertensives.
4. ACE inhibitors:
- Enalapril maleate 5 mg OD is given.
- Captopril in combination with diuretics or a betablocker. 25 gm TDS of captopril is administered. It is considered safe in asthmatics and diabetics.
- Ramipril 2.5 mg daily is used to reduce hypertension.
5. Alpha-1 adrenergic blockers: Prazosin is commonly used drug. Dose is 0.5 mg TDS.
6. Vasodilators: Diazoxide and sodium nitroprusside are given as IV dosage
Question.54. Describe aetiology, clinical features and management of coronary artery disease.
Answer. Coronary artery diseases are also known as ischaemic heart disease.
Following are the coronary artery diseases:
- Angina pectoris
- Acute myocardial infarction
- Sudden cardiac death.
Aetiology of coronary artery diseases
1. Atherosclerotic coronary artery disease
2. Other coronary artery diseases:
- Coronary artery spasm
- Coronary arteritis
- Embolism
- Coronary AV malformation
3. Valvular diseases:
- Aortic stenosis and regurgitation
- Mitral valve prolapse
4. Other cardiac diseases:
- Hypertrophic cardiomyopathy
- Collagen disease
- Syphilis
5. Increased demands:
- Thyrotoxicosis
- Anemia
- Beriberi
Clinical Features coronary artery disease
- Angina pectoris: Refer to Ans 22 of same chapter.
- Acute myocardial infarction: Refer to Ans 21 of same chapter
- Sudden cardiac arrest: In this, a person with good health fall ill and die suddenly within minutes and few hours.
- Absence of pulses
- On auscultation, cardiac impulse is not present.
- Extremities are cold
- Cessation of respiration of patient
- Blood pressure is not measurable.
Management coronary artery disease
- Angina pectoris: Refer to Ans 22 of same chapter.
- Acute myocardial infarction: Refer to Ans 19 of same chapter
- Sudden cardiac arrest: Refer to Ans 47 of same chapter.
Question.56.Write management of atrial firillation.
Answer. It is the most common sustained tachyarrhythmia seen in patients.
Management f atrial firillation.
- Ventricular rate is reduced by giving digoxin. Digoxin 0.5 mg IV slowly is given. After this, patient is kept on oral digitalis therapy, i.e. 0.25 mg twice daily.
- Antiarrhythmic drugs such as propranolol is given IV at a rate of 1 mg every 5 min followed by maintenance of oral dose of 20–40 mg three times a day.
- Underlying causes such as thyrotoxicosis and acute chest infections should be treated to maintain normal sinus rhythm.
- Anticoagulant therapy should be given in patients with chronic atrial firillation.
- Defirillation should be done. A DC shock of 100 joules restore normal sinus rhythm.
Question.57. Write short note on prophylaxis for infective endocarditis.
Answer.
Sub-acute bacterial endocarditis is defied as infection and inflmmation of inner lining of heart including heart valves.
It also includes infection at the site congenital heart anomaly.
Clinical Manifestations infective endocarditis.
- General: Presence of nausea, fever, anorexia, weight loss, night sweat and weakness.
- Cardiovascular system: Tachycardia, cardiac murmur, conduction defect and cardiac failure.
- Blood vessels: Loss of peripheral pulse.
- Central nervous system: Headache, hemiplegia or monoplegia and toxic encephalopathy.
- Lungs: Pleuritic pain and hemoptysis Nails: Osler’s nodes, clubbing of finger and splinter hemorrhage.
- Skin: Purpuric spot and petechial hemorrhage.
- Eyes: Roth’s spot and subconjunctival hemorrhage.
- Kidney: Hematuria and glomerulonephritis
- Spleen: Splenomegaly is present
- Blood: Anemia is present
Pathogenesis infective endocarditis.

Investigations infective endocarditis.
1. Blood culture: In absence of recent or concurrent antibiotic therapy, the fist 3 random blood cultures are positive in most patients, and blood culture is positive by third day in 90%.
2. Urine: Microscopic hematuria is the most common fiding.
Slight albuminuria and hyaline and granular casts also found.
3. Hematology: Normocytic normochromic anemia, usually mild. May be raised ESR and raised Creactive protein.
4. Chest radiograph: May be diagnostic in right sided endocarditis, with multiple shadows visible due to an embolic pneumonia.
5. ECG: Myocardial infarction seen on ECG may be due coronary embolism, and a conduction defect may be due to development of an aortic root abscess.
6. Echocardiography: Higher sensitivity in identifying vegetation with transesophageal echocardiography as compared to transthoracic echocardiography.
- Vegetations: An echodense structure attched to the valve or its supporting structures, or lying in the track of a turbulent jet, which is irregular in shape.
- Leaflt perforation is best seen as regurgitant jet on color flw mapping.
- Annular and periprosthetic echolucent spaces (abscesses) and fitula formation.
7. Chest X-ray: Shows evidence of cardiomegaly and heart failure.
Management infective endocarditis.
Management is divided into three parts:
- Treatment during disease process
- Prophylaxis
- Indication for cardiac surgery.
Treatment during disease Process infective endocarditis.
- It is mainly antimicrobial treatment. Along with source of infection symptoms are removed as soon as possible.
- Antibiotics should preferably be bactericidal.
- Antibiotics should be administered parenterally to achieve high serum concentration since the vegetation is avascular.
- Therapy is generally of prolonged duration.
- Selection of antibiotics should be based on culture report and minimum inhibitory concentration (MIC) values.
- Empirical therapy may be initiated in acute severe cases after drawing blood samples for culture.
The antibiotics are later changed based on sensitivity reports, if necessary. - Treatment of infective endocarditis should be prompt and adequate.
The list of antibiotics commonly used, their dosage and indications are given below in table.
Antimicrobial therapy for Infective endocarditis
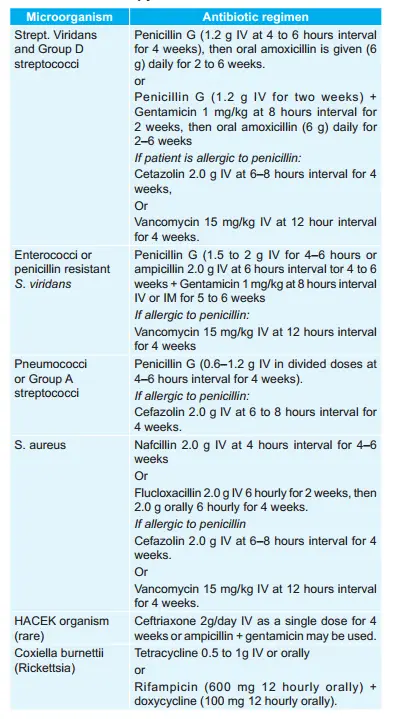
Prophylaxis against Infective endocarditis
Patients with valvular and congenital heart disease who are at high or moderate risk of endocarditis should receiveprophylactic antibiotics before undergoing any procedure which may cause bacteremia.
Antibiotic regimen for prophylaxis of endocarditis in adults at moderate or highrisk is as follows:
1. Oral cavity, respiratory tract, or esophageal procedures (in patients at highrisk, administer a half dose after the initial dose).
- Standard regimen: Amoxicillin 2.0 g oral 1 hour before procedure.
- Inability to take oral medication of standard regimen:
Ampicillin 2.0 g IV or IM within 30 min of procedure. - If patient is allergic to penicillin:
Clarithromycin 500 mg or azithromycin 500 mg orally l hour before procedure.
Or
Cephalexin or cefadroxil 2 g orally 1 hour before procedure
Or
Clindamycin 600 mg oral l hour before procedure - If patient is allergic to penicillin and is unable to take oral medication
Clindamycin 600 mg I.V. 30 min before procedure.
Or
Cefazolin 1.0 g I.V. or IM 30 min before procedure.
2. Genitourinary and gastrointestinal tract procedures:
- In high risk patients: Ampicillin 2g IM or IV + gentamycin 1.5 mg/kg IV or IM within 30 min of starting the procedure followed by ampicillin
- In high-risk patients allergic to penicillin: Vanacomycin 1g IV over 1 to 2 hour + gentamycin 1.5 mg/kg IV or IM combination is given within 30 min of starting the procedure.
- In moderate risk patients: Amoxicillin 2.0 g oral 1 hour before procedure Or ampicillin or amoxicillin 2.0 g IV or IM within 30 min of procedure.
- In moderate riskpatients allergic to penicillin: Vancomycin 1g IV over 1 to 2 hours completed within 30 min of starting procedure.
Indication for cardiac surgery
- Heart failure due to valve damage
- Failure of antibiotic therapy, i.e. in fungal endocarditis
- Large vegetation on left sided heart valves with evidence or highrisk of systemic emboli.
- Abscess formation
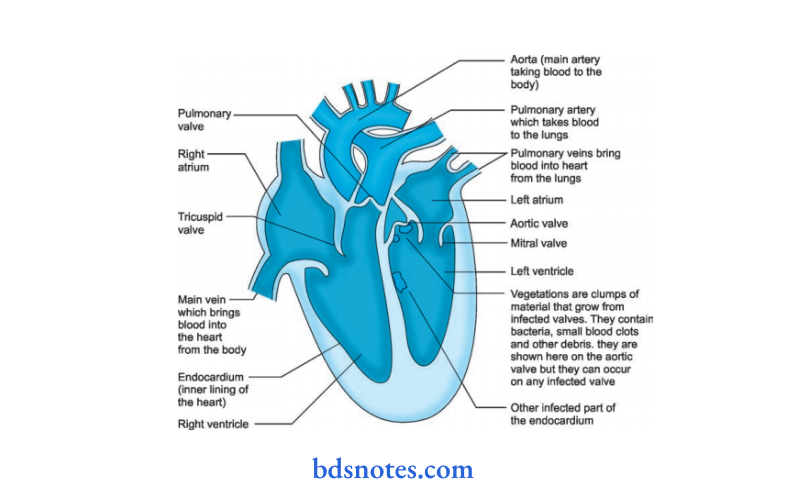
Question.58. Describe clinical features of rheumatic fever and diagnosis of carditis with strategy of prophylaxis.
Answer.
It is an acute inflmmatory disease which occurs due to infection by group A hemolytic streptococci which involves heart, joint, skin and nervous system which develops as autoimmune reaction to infecting organism.
Etiology
- Predisposing causes:
Age should be 5 to 15 years.
Sex has equal incidence - Genetic factors: Family incidence known.
- Social and economic factors: Dampness, overcrowding and under nutrition increases incidence.
- Idiosyncrasy is presumably a factor since 3% of people are involved in streptococcal epidemics develop rheumatic fever.
Clinical Manifestations rheumatic fever
- Prodromal phase: Tonsillitis or sore throat 1 to 4 weeks prior to onset of acute rheumatic fever. Besides this anorexia, pallor, fatigability and nervous irritability is present.
- Latent phase: When antibodies to preceding streptococcal infection are produced.
- Phase of onset of rheumatic fever/mode of onset.
Arthritis and fever 2–3 weeks after infection. - Cardiac symptoms 3–6 weeks after infection is fist to draw attntion.
- Abdominal symptoms: Abdominal pain and tenderness, nausea, vomiting, fever and leukocytosis.
- Pyrexia of unknown origin
- Typhoid or inflenzal mode of onset with fever
- Nodules of skin lesion.
Treatment of acute rheumatic Fever
- Bed rest is important to reduce joint pain and cardiac workload.
Duration of bed rest is guided by markers of inflmmation like temperature, WBC count and ESR. - Benzathine penicillin 1.2 mu IM 4 hourly.
If patient is allergic to penicillin, erythromycin 40–50 mg / kg for ten days is given. - Aspirin usually relieves symptom of arthritis rapidly.
A starting dose of 60 mg / kg body weight per day is given divided into 6 doses.
The dose may be increased to 120 mg / kg body weight.
This dose may produce severe symptoms like vomiting, tachypnea and acidosis is given till ESR comes to normal. - Corticosteroids like prednisolone produces rapid symptomatic relief than aspirin and is indicated in cases with severe arthritis or carditis.
Prednisolone is given in doses of 1.2 mg / kg body weight till ESR comes to normal.
The term acute pulmonary edema refers to collection of flid into alveoli its wall and alveolar sac due to an acute increase in left atrial pressure.
Causes rheumatic fever
1. Cardiogenic:
- Left ventricular failure
- Myocardial infarction
- Mitral stenosis
- Pulmonary infarction
- Cardiac arrhythmia.
2. Non-cardiogenic:
- Fluid overload
- Shock
- Inhalation of gastric acid (Mendelson’s syndrome)
- High altitude pulmonary edema.
Clinical Features rheumatic fever
- Feeling of *oppression in chest
- Acute and distressing dyspnea
- Short cough and pink frothy sputum, sometimes blood tinged flid from mouth and nose.
- Sweat and feeble pulse.
- Fall of temperature.
Management rheumatic fever
- Bed rest is provided as the sittng position tends to reduce
venous return. - Oxygen is provided
- Inj. Morphine 15 mg subcutaneously is given.
- Inj. Furosemide 80 mg IV relieves pulmonary edema.
If patient has not received digoxin during last fortnight - Inj. Digoxin (0.5. to 1 mg) is given.
- Inj. Aminophylline 0.24 gm slow IV in 10 min is effctive.
- Patients not responding above regimen IV nitroprusside 20–30 unit g per minute is given.
Management Acute Rheumatic Fever.
1. Treatment of acute attck: Rheumatic Fever
- Bed rest is important to reduce joint pain and cardiac workload.
Duration of bed rest is guided by markers of inflmmation like temperature,
WBC count and ESR. - Benzathine penicillin 1.2 mu IM 4 hourly. If patient is allergic to penicillin, erythromycin 40–50 mg / kg for ten days is given.
- Aspirin usually relieves symptom of arthritis rapidly.
A starting dose of60 mg/kg body weight per day is given divided into 6 doses.
The dose may be increased to 120 mg / kg body weight.
This dose may produce severe symptoms like vomiting, tachypnea and acidosis. Aspirin is given till ESR comes to normal. - Corticosteroids like prednisolone produces rapid symptomatic relief than aspirin and is indicated in cases with severe arthritis or carditis.
Prednisolone is given in doses of 1.2 mg / kg body weight till ESR comes to normal
2. Secondary prevention: Rheumatic Fever
To prevent further attck of rheumatic fever, longterm prophylaxis is needed.
- Benzathine penicillin 1.2 mu IM is injected at the interval of 21 days.
Further attck is unusual after the age of 21 years and treatment can be stopped. - To prevent chances of endocarditis prophylactic antibiotic therapy should be given
Question.59. Write short note on PTCA.
Answer. Percutaneous transluminal coronary angioplasty (PTCA) is a minimally invasive procedure to open up blocked coronary arteries, allowing blood to circulate unobstructed to the heart muscle.
In PTCA, balloon dilatation of coronary stenosis is done.
Method Percutaneous transluminal coronary angioplasty (PTCA)
Procedure of doing PTCA is commenced by passing a guide wire under floroscopic control, this wire positions the balloon dilatation centre at level of stenosis, now balloon dilatation of the stenotic segment is carried out for maintaining the circulation all through.
Indications
- This method provides complete or partial revascularization in cases of stable angina pectoris, unstable angina pectoris or myocardial infarction.
- It is indicated in patients with recurrent angina after coronary artery bypass grafting (CABG).
Complications Percutaneous transluminal coronary angioplasty (PTCA)
- Blood vessel occlusion can occur by thrombosis.
- Recurrent angina pectoris
- Restenosis can occur.
Question.60. Describe risk factors, clinical features, diagnosis and treatment of myocardial infarction.
Or
Describe clinical features, diagnosis, primary care,treatment and complications of acute myocardial infarction.
Answer.
Acute myocardial infarction is defied as irreversible damage to myocardium of heart as a result of occlusive thrombus due to rupture of atherosclerotic plaque in coronary artery.
Clinical Features myocardial infarction.
Symptoms: myocardial infarction.
- Pain: Chest pain is more common and is severe in comparison to angina.
Pain is severe with pallor and peculiar facial expression.
Pain is described as tightness, heaviness and constriction. - Anxiety: It is common and occurs when there is fear of impending death.
- Nausea and vomiting.
- Breathlessness due to fall in cardiac output.
- Collapse or syncope due to arrhythmia and profound hypertension.
Signs: myocardial infarction.
1. Signs of sympathetic activation
- Pallor
- Sweating
- Tachycardia.
2. Signs of vagal stimulation
- Vomiting
- Bradycardia.
3. Signs of impaired myocardial function
- Hypotension and oligouria
- Narrow pulse pressure
- Raised jugular venous pressure
- Third heart sound
- Quite fist heart sound
- Lung crepitations.
4. Signs oftissue damage: Fever and arrhythmia
5. Signs ofcomplications:
- Due to mitral regurgitation
- Due to pericarditis.
- Ventricular ectopic beats
- Ventricular tachycardia
- Heart blocks.
Diagnosis myocardial infarction.
Diagnosis of acute myocardial infarction is based on history, characteristics symptoms and signs and investigations.
Investigations myocardial infarction.
1. Electrocardiography:
1. ECG is the specific method for confirming the diagnosis.
2. Typical changes are seen in leads which faces the infracted area. These changes are:
- Elevation of STsegment
- Pathologic Qwaves appear.
- T waves may become tall and peaked in very early myocardial infarction.
T waves are transient and last for a few hours only. - In contrast to transmural lesions, partial thickness or subendothelial infarction causes ST/T wave changes without Qwaves or prominent ST elevation.
- Changes in the ECG are seen which evolve in predictable fashion over next few days to weeks.
2. Blood test:
1. Plasma biochemical markers:
Myocardial infarction leads to detectable rise in the plasma concentration of various enzymes and proteins that are normally concentrated within the cardiac cells.
Plasma enzymes (cardiac injury enzymes) are as follows:
- Creatine kinase (CK).
- Aspartate aminotransferase (AST).
- Lactate dehydrogenase (LDH).
- Myoglobin
- Troponins (troponin I and troponin T)
2. Creatine kinase starts to rise at 4–6 hours and it peaks by about 12 hours and falls to normal in 48–72 hours.
Myocardial isoenzyme of creatine kinase is more specifi. It is useful for diagnosis of early myocardial infarction.
3. Aspartate aminotransferase (AST) starts to rise at about 12 hours and reaches a peak on the fist or second day and returns on third and fourth day.
4. Lactate dehydrogenase (LDH) starts to rise after 12 hours, reaches a peak after 2–3 days and may remain elevated for a week.
Rise in the value of LDH I (anisoenzyme of LDH) is a more sensitive indicator of myocardial infarction than total LDH.
It is useful in diagnosis for patients who present several days after myocardial infarction.
5. Cardiac troponins are cardiac troponinT (cTnT) and cardiac troponinI (cTnI). Sensitivity of troponins is similar to that of isoenzymes of creatine kinase.
Moreover, cTnT remains elevated for 100 to 200 hours after acute myocardial infarction and therefore, it may have particular utility in the evaluation of patients who present suffiently long episode after the pain in chest.
- Leukocytosis with a peak on fist day.
- ESR is raised which may remain raised for some days.
- Creactive protein is elevated.
6. Chest X-ray: It can detect acute pulmonary edema or congestion. It is also helpful to detect pericardial effsion, cardiomegaly, etc.
7. Radionuclide scanning: It shows site of necrosis and the extent of impairment of ventricular function.
8. Echocardiography: This is done for regional wall motion abnormality and ejection fraction.
Treatment myocardial infarction.
The management of myocardial infarction is divided into two parts:
1. Early management.
2. Late management.
Early Management myocardial infarction.
- Aspirin 150–300 mg to be chewed earliest.
- Sublingual glyceryl trinitrate 0.4–1 mg, to be repeated, if necessary
- Oxygen through nasal cannula at a rate of 2–4 L/min.
- Procure IV line and take blood samples for glucose, lipids and complete haemogram.
- Record 12lead ECG.
- Pain may be relieved by IV morphine (5 mg) plus metoclopramide as an antimetic (10 mg).
- IV betablockers (metoprolol 5 mg every 2–5 minutes for 3 doses) for ongoing chest pain, hypertension and tachycardia provided there is no contraindication.
- Thrombolysis should be done.
- If PTCA is planned, give GP IIb/IIIa inhibitor
- After admission immediately shift the patient to ICU or
ICCU
In Hospital treatment
Hospitalization and strict Bed rest
- Hospitalize the patient and advice strict bed rest. As early as the patient is hospitalized, the bettr it is.
- Patient should be strictly admittd in ICCU.
Analgesia
- IV morphine sulphate 10 mg and an anti emetic, i.e. cyclizine 50 mg is given through I.V. cannula.
- The drug is repeated depending on the response till complete analgesia is received and patient feels bettr.
Anti-platelet drugs
Low dose aspirin, i.e. 75 to 150 mg and clopidogrel 300 mg stat and then 75 mg orally daily is given.
Oxygen therapy
Inhalation of oxygen increases arterial partial pressure of oxygen, so there is increase in the concentration of oxygen gradient which is responsible for diffusionn of oxygen in ischemic myocardium from adjacent better perfused areas. This is given by facemask or nasal prongs for a day or two after infarction.
Thrombolysis
- Coronary thrombolysis helps to restore patency of coronary artery preserves left ventricular function and improves survival.
- The choice of drug for thrombolysis is less important than the speed of treatment.
- Streptokinase, 1.5 million units in 100 mL of saline given in an intravenous infusion over 1 hour, is a widely accepted method.
It is a cheap, but being antigenic, sometimes, may cause serious allergic manifestations.
Hence, it can be used once and therapy is changed if the patient requires second thrombolysis within few years.
Alteplase (tissue Plasminagen activator (tPa)
- It is a potent firinolytic drug but is expensive.
- It is less antigenic and does not cause hypotension.
- The current tPA regimen given over 90 minutes (bolus dose of 15 mg followed by 50 mg over 30 minutes and then 35 mg over next 60 minutes) is widely accepted. The other drugs include reteplase given in double dose regime i.e.
10 million units over 2–3 minute followed by another dose of 10 million units after 30 minutes.
Tenectaplase given as bolus dose of 53 mg/kg over 10 seconds. Both reteplase and tenectaplase are known as bolus firinolytics.
Angioplasty
Immediate angioplasty of infarct related artery is safe and is effctive alternative to thrombolysis. It is done in the patients in whom the hazards of thrombolysis is high.
Anti-coagulants
- Subcutaneous heparin, i.e. 7,500 units twice a day for 7–10 days or till discharge of patient from the hospital can be employed.
In patients who do not receive thrombolytic therapy to prevent venous thrombosis. - Patients who receive thrombolytic therapy (tPA) should receive immediate and full doses of heparin (10,000 U bolus plus, l000 U hourly).
Beta-adrenergic Blockers
Acute betaadrenoreceptors blockade intravenous atenolol (5–l0 mg given over 5 minutes) or metoprolol (5–15 mg given over 5 minutes) relieves pain, reduces arrhythmias, salvages myocardium and improves short term mortality in patients who present within l2 hours of onset of pain.
Nitrates and other agents
Sublingual glyceryl trinitrate 0.4 mg is useful in threatened infarction.
Sedatives
Diazepam 5mg for three to four times a day is effctive. It is given for few days.
Diet
- For fist 4 to 5 days low calorie diet which is divided into multiple meals is given.
- If heart failure is present restrict the salt.
- From second week, food should be increased in amount.
Lipid lowering agent
Atorvastatin is given to reduce the LDL levels.
Late Management
1. Risk stratifiation and further investigations: Prognosis of patient survived after myocardial infarction depends on degree of myocardial damage, any residual ischemia and presence of ventricular arrhythmias.
2. Life style modifiation:
- Stop smoking
- Diet control
- Regular exercise.
3. Secondary prevention
- Antiplatelet agents, i.e. aspirin
- Lipid lowering agents
- Betablockers and ACEI in congestive cardiac failure and hypertension.
- Control of blood sugar in diabetes.
4. Rehabilitation and after care:
- Physical activities should be restricted for 4 to 6 weeks since infarct takes 4–6 weeks to become replaced with firous tissue.
- Gradual mobilization and return to work over 6 weeks.
When there are complications, the regimen has to be modifid accordingly. - Exercise within the limits set by angina and tiredness will do no harm but much good. Same limits apply to sexual activity.
- Control of obesity, regular exercises, cessation of smoking, adoption of a less frenetic way of life and control of plasma lipids by diets and drugs.
- Complications should be managed. Pain relief, reassurance, rest and correction of hypokalemia play a major role in prevention of arrhythmias.
Routine drug therapy
- Low dose aspirin, i.e. 75 to 150 mg daily and is continued indefiitely.
- Beta-adrenergic blocker should be given for 4 to 6 weeks if there is no contraindication.
- ACE inhibitor, i.e. captopril 25 mg TID or ramipril 2.5 to 5 mg BD
- Lipid lowering agent atorvastatin is given to lower the LDL levels.
Enumeration of complications of Myocardial Infarction
1. Immediate
1. Arrhythmias and conduction disturbances
- Sinus bradycardia
- Ventricular ectopics
- Ventricular tachycardia
- Ventricular firillation
- Idioventricular rhythm
- Atrial firillation
- Heart block
2. Post-myocardial angina can occur in 50% patients occur.
3. Acute circulatory failure.
4. Pericarditis
5. Mechanical complications include:
- Papillary muscle dysfunction or rupture
- Rupture of interventricular septum
- Rupture of ventricle
6. Mural thrombosis and embolism
7. Sudden death
2. Late complications:
- Postmyocardial infarction syndrome (Dressler’s syndrome)
- Ventricular aneurysm.
Management Myocardial Infarction
The management of myocardial infarction is divided into two parts:
1. Early management.
2. Late management.
Early Management
- Aspirin 150–300 mg to be chewed earliest.
- Sublingual glyceryl trinitrate 0.4–1 mg, to be repeated, if necessary
- Oxygen through nasal cannula at a rate of 2–4 L/min.
- Procure IV line and take blood samples for glucose, lipids and complete haemogram.
- Record 12lead ECG.
- Pain may be relieved by IV morphine (5 mg) plus metoclopramide as an antimetic (10 mg).
- IV betablockers (metoprolol 5 mg every 2–5 minutes for 3 doses) for ongoing chest pain, hypertension and tachycardia provided there is no contraindication.
- Thrombolysis should be done.
- If PTCA is planned, give GP IIb/IIIa inhibitor
- After admission immediately shift the patient to ICU or
ICCU
In Hospital treatment
Hospitalization and strict Bed rest
- Hospitalize the patient and advice strict bed rest. As early as the patient is hospitalized, the bettr it is.
- Patient should be strictly admittd in ICCU.
Analgesia
- IV morphine sulphate 10 mg and an anti emetic, i.e. cyclizine 50 mg is given through I.V. cannula.
- The drug is repeated depending on the response till complete analgesia is received and patient feels bettr.
Anti-platelet drugs
Low dose aspirin, i.e. 75 to 150 mg and clopidogrel 300 mg stat and then 75 mg orally daily is given.
Oxygen therapy
Inhalation of oxygen increases arterial partial pressure of oxygen, so there is increase in the concentration of oxygen gradient which is responsible for diffusionn of oxygen in ischemic myocardium from adjacent better perfused areas. This is given by facemask or nasal prongs for a day or two after infarction.
Thrombolysis
- Coronary thrombolysis helps to restore patency of coronary artery preserves left ventricular function and improves survival.
- The choice of drug for thrombolysis is less important than the speed of treatment.
- Streptokinase, 1.5 million units in 100 mL of saline given in an intravenous infusion over 1 hour, is a widely accepted method.
It is a cheap, but being antigenic, sometimes, may cause serious allergic manifestations.
Hence, it can be used once and therapy is changed if the patient requires second thrombolysis within few years.
Alteplase (tissue Plasminagen activator (tPa)
- It is a potent firinolytic drug but is expensive.
- It is less antigenic and does not cause hypotension.
- The current tPA regimen given over 90 minutes (bolus dose of 15 mg followed by 50 mg over 30 minutes and then 35 mg over next 60 minutes) is widely accepted. The other drugs include reteplase given in double dose regime i.e.
10 million units over 2–3 minute followed by another dose of 10 million units after 30 minutes.
Tenectaplase given as bolus dose of 53 mg/kg over 10 seconds. Both reteplase and tenectaplase are known as bolus firinolytics.
Angioplasty
Immediate angioplasty of infarct related artery is safe and is effctive alternative to thrombolysis. It is done in the patients in whom the hazards of thrombolysis is high.
Anti-coagulants
- Subcutaneous heparin, i.e. 7,500 units twice a day for 7–10 days or till discharge of patient from the hospital can be employed.
In patients who do not receive thrombolytic therapy to prevent venous thrombosis. - Patients who receive thrombolytic therapy (tPA) should receive immediate and full doses of heparin (10,000 U bolus plus, l000 U hourly).
Beta-adrenergic Blockers
Acute betaadrenoreceptors blockade intravenous atenolol (5–l0 mg given over 5 minutes) or metoprolol (5–15 mg given over 5 minutes) relieves pain, reduces arrhythmias, salvages myocardium and improves short term mortality in patients who present within l2 hours of onset of pain.
Nitrates and other agents
Sublingual glyceryl trinitrate 0.4 mg is useful in threatened infarction.
Sedatives
Diazepam 5mg for three to four times a day is effctive. It is given for few days.
Diet
- For fist 4 to 5 days low calorie diet which is divided into multiple meals is given.
- If heart failure is present restrict the salt.
- From second week, food should be increased in amount.
Lipid lowering agent
Atorvastatin is given to reduce the LDL levels.
Late Management
1. Risk stratifiation and further investigations: Prognosis of patient survived after myocardial infarction depends on degree of myocardial damage, any residual ischemia and presence of ventricular arrhythmias.
2. Life style modifiation:
- Stop smoking
- Diet control
- Regular exercise.
3. Secondary prevention
- Antiplatelet agents, i.e. aspirin
- Lipid lowering agents
- Betablockers and ACEI in congestive cardiac failure and hypertension.
- Control of blood sugar in diabetes.
4. Rehabilitation and after care:
- Physical activities should be restricted for 4 to 6 weeks since infarct takes 4–6 weeks to become replaced with firous tissue.
- Gradual mobilization and return to work over 6 weeks.
When there are complications, the regimen has to be modifid accordingly. - Exercise within the limits set by angina and tiredness will do no harm but much good. Same limits apply to sexual activity.
- Control of obesity, regular exercises, cessation of smoking, adoption of a less frenetic way of life and control of plasma lipids by diets and drugs.
- Complications should be managed. Pain relief, reassurance, rest and correction of hypokalemia play a major role in prevention of arrhythmias.
Routine drug therapy
- Low dose aspirin, i.e. 75 to 150 mg daily and is continued indefiitely.
- Beta-adrenergic blocker should be given for 4 to 6 weeks if there is no contraindication.
- ACE inhibitor, i.e. captopril 25 mg TID or ramipril 2.5 to 5 mg BD
- Lipid lowering agent atorvastatin is given to lower the LDL levels.
Risk Factors
- Family history of heart disease
- Patient history of heart disease
- Diabetes or elevated blood glucose even in nondiabetics
- Hypertension
- Advanced age
- High lipoprotein lipids
- Stress, smoking, sedentary lifestyle, compulsive personality
- Poor diet, i.e. high sodium, high fat, high intake of alcohol;low intake of B complex vitamin, calcium, magnesium and potassium; low intake of fruit and vegetables
- Obesity.
Primary care
- Aspirin 150–300 mg to be chewed earliest.
- Sublingual glyceryltrinitrate 0.4–1 mg, to be repeated, if necessary
- Oxygen through nasal cannula at a rate of 2–4 L/min.
- Procure IV line and take blood samples for glucose, lipids and complete hemogram.
- Record 12lead ECG.
- Pain may be relieved by IV morphine (5 mg) plus metoclopramide as an antimetic (10 mg).
- IV betablockers (metoprolol 5 mg every 2–5 minutes for 3 doses) for ongoing chest pain, hypertension and tachycardia provided, there is no contraindication.
- Thrombolysis should be done.
- If PTCA is planned, give GP IIb/IIIa inhibitor
- After admission, immediately shift the patient to ICU or ICCU
Question.61 Write clinical features, risk factors, diagnosis and management of ischemic heart disease.
Answer. Ischemic heart disease occurs whenever there is an imbalance between myocardial oxygen demand and its supply.
Clinical Features Ischemic Heart Disease
- Presence of asymptomatic ischemia.
- Angina—Stable or unstable
- Ischemic cardiomyopathy
- Acute myocardial infarction
- Cardiac arrest
- Arrythmias or conduction defects
- Sudden cardiac death
- Asymptomatic coronary artery disease detected on routine medical check up.
Risk Factors Ischemic Heart Disease
- Age: As age advances chances of occurrence of coronary artery diseases increases. It is due to cumulative effcts of multiple risk factors overtime.
- Diet: Diet rich in fat, sugar, cholesterol leads to formation of athroma and this leads to coronary artery diseases.
Genetic: Positive family history of sudden death, myocardial infarction, angina are points to genetic predisposition. - Personality: In persons having traits of aggressiveness, ambition and competitiveness chances of occurrence of coronary artery diseases increases.
Smoking: Persons who smoke are susceptible for coronary artery diseases because of nicotine and carbon monoxide. - Diabetes mellitus: Due to diabetes athroma may develop in early age and patient is suffring from asymptomatic coronary artery disease.
- Obesity: It is associated with increased levels of serum cholesterol, blood pressure, serum triglycerides and serum insulin which lead to coronary artery disease.
- Physical activity: Persons who does not undergo regular physical activities such as brisk walking or exercise have chances for coronary artery diseases.
Diagnosis Ischemic Heart Disease
In angina Pectoris
- Resting ECG: ECG changes of myocardial ischemia are reflcted in S-T waves. Occasionally, there is flttning of Twaves in some lead in patient with angina.
- Exercise ECG orStress test: Withcontinuous ECG monitoring and intermittntBP recordingis performed witha treadmill or bicycle ergometer.
Standardised protocols are used (e.g. Bruce protocol), enabling performance to be assessed in same patient at diffrent times and work load at onset of symptoms or ECG changes to be determined. An exercise ECG is abnormal, if there is horizontal or downsloping ST segment depression of 0.1 mm or more in any lead. - Myocardial perfusion scintigraphy: The isotope cardiovascular stress (usually thallium201 or technetium—99 m) is injected at peak exercise and images taken with a camera immediately or shortly after exercise and compared with rest images taken a few hours later following a second injection of tracer.
Areas of myocardial ischemia are identifid by reduced isotopic uptake in the same anatomical distribution stress images but not resting images (reversible defect). - Coronary angiography: It is done before angioplasty or coronary bypass surgery.
In acute Myocardial Infarction Ischemic Heart Disease
Diagnosis of acute myocardial infarction is based on history, characteristics symptoms and signs and investigations.
Investigations Ischemic Heart Disease
1. Electrocardiography:
- ECG is the specific method for confirming the diagnosis.
- Typical changes are seen in leads which faces the infracted area. These changes are:
- Elevation of ST segment
- Pathologic Q—waves appear.
- T waves may become tall and peaked in very early myocardial infarction.
T waves are transient and last for a few hours only. - In contrast to transmural lesions, partial thickness or subendothelial infarction causes ST/T wave changes without Q waves or prominent ST elevation.
- Changes in the ECG are seen which evolve in predictable fashion over next few days to weeks.
2. Blood test:
1. Plasma biochemical markers:
Myocardial infarction leads to detectable rise in the plasma concentration of various enzymes and proteins that are normally concentrated within the cardiac cells.
Plasma enzymes (cardiac injury enzymes) are as follows:
- Creatine kinase (CK).
- Aspartate aminotransferase (AST).
- Lactate dehydrogenase (LDH).
- Myoglobin
- Troponins (troponin I and troponin T)
- Creatine kinase starts to rise at 4–6 hours and it peaks by about 12 hours and falls to normal in 48–72 hours. Myocardial isoenzyme of creatine kinase is more specifi. It is useful for diagnosis of early myocardial infarction.
- Aspartate aminotransferase (AST) starts to rise at about 12 hours and reaches a peak on the fist or second day and returns on third and fourth day.
- Lactate dehydrogenase (LDH) starts to rise after 12 hours, reaches a peak after 2–3 days and may remain elevated for a week.
Rise in the value of LDH I (an isoenzyme of LDH) is a more sensitive indicator of myocardial infarction than total LDH.
It is useful in diagnosis for patients who present several days after myocardial infarction. - Cardiac troponins are cardiac troponinT (cTnT) and cardiac troponinI (cTnI). Sensitivity of troponins is similar to that of isoenzymes of creatine kinase. Moreover, cTnT remains elevated for 100–200 hours after acute myocardial infarction and therefore, it may have particular utility in the evaluation of patients who present suffiently long episode after the pain in chest.
2. Leucocytosis with a peak on fist day.
3. ESR is raised, which may remain raised for some days.
4. C-reactive protein is elevated.
5. Chest X-ray: It can detect acute pulmonary edema or congestion. It is also helpful to detect pericardial effsion, cardiomegaly, etc.
6. Radionuclide scanning: It shows site of necrosis and the extent of impairment of ventricular function.
7. Echocardiography: This is done for regional wall motion abnormality and ejection fraction.
Management Ischemic Heart Disease
Angina pectoris is a symptom complex caused by transient myocardial ischemia and constitutes a clinical syndrome rather than a disease.
Types
- Stable
- Unstable
- Nocturnal
- Prinzmetal’s
- Postinfarction angina
Etiology
Acute myocardial ischemia occurs when myocardial oxygen demand exceeds supply in following:
- Coronary atherosclerotic narrowing (most cases).
- Nonatherosclerotic coronary artery disease—Coronary spasm, coronary thromboembolism, congenital anomalies, coronary vasculitis.
- Valvalar heart disease — Aortic stenosis and/or aortic regurgitation, mitral stenosis with pulmonary hypertension, mitral valve prolapse.
- Pulmonary hypertension.
- Systemic hypertension.
- Hvpertrophic or dilated cardiomyopathy.
- Anemia—from tachycardia and reduction in O2 availability.
Precipitating causes
- Physical exertion
- Heavy metal
- Exposure to cold
- Emotion and excitement
- Hyperinsulinism in diabetic patients
- Other causes: Straining at stools, bathing, sexual intercourse,micturition
Clinical Features Ischemic Heart Disease
symptoms Ischemic Heart Disease
1. Anginal pain:
- Site: Most often over middle or lower sternum or over left precordium, at times in epigastrium. Sometimes discomfort is located only in left shoulder or left upper arm, occasionally in lower jaw and rarely in interscapular area.
- Radiation of pain: May spread to right or left arm or both neck or jaw. Occasionally, pain starts in the wrist, upper arms or face and then spreads to the chest.
- Character: Vicelike constriction or choking. Sometimes only pressure or burning pain, rarely mere weakness of one or both arms. An important characteristic is its constancy, the pain being steady while it lasts.
- Duration: Most commonly l to 4 minutes. It may force patient to stop walking.
- Provocation: By effrt specially like walking against the wind or up a climb, hurrying after meals or unaccustomed exercise at times due to excitement anger, and fear. In advanced cases, pain is provoked by lying down (angina decubitus) or stooping.
- Relief with sublingual nitroglycerine.
2. Dyspnea: If it occurs before the pain suggests severe ventricular disease.
3. Other symptoms:
- Choking sensation in throat or feeling of impending doom.
- Belching or passage of fltus or polyuria after an attck.
- Dizziness, faintness or rarely syncope
- If pain is severe sweating and nausea.
Signs Ischemic Heart Disease
1. At time, no signs are present.
2. Signs ofLV dysfunction: Atrial or third heart sound.
3. Dysfunction of papillary muscle: It can lead to transient mitral regurgitation in case of ischemia.
4. Signs associated with risk factors:
- Hypertension.
- Hyperlipidemia—Arcus senilis, xanthelasma, or cholesterol deposits along tendons and in skin of palms and buttcks.
- Obesity
- Diabetes and its accompaniments.
5. During the attck—pallor and sweating with rise of BP often tachycardia.
Pressure on carotid sinus may produce slowing of pulse and cessation of pain.
Diagnosis Ischemic Heart Disease
Investigations Ischemic Heart Disease
- Resting ECG: ECG changes of myocardial ischemia are reflcted in ST-T waves. Occassionally, there is flttning of T waves in some lead in patient with angina.
- Exercise ECG or stress test: With continuous ECG monitoring and intermittent BP recording is performed with a treadmill or bicycle ergometer. Standardized protocols are used (e.g. Bruce protocol), enabling performance to be assessed in same patient at diffrent times and workload at onset of symptoms or ECG changes to be determined.
An exercise ECG is abnormal, if there is horizontal or downsloping ST segment depression of 0.1 mm or more in any lead. - Myocardial perfusion scintigraphy: The isotope cardiovascular stress (usually thallium201 or technetium—99 m) is injected at peak exercise and images taken with a camera immediately or shortly after exercise and compared with rest images taken a few hours later following a second injection of tracer.
Areas of myocardial ischemia are identifid by reduced isotopic uptake in the same anatomical distribution stress images but not resting images (reversible defect). - Coronary angiography: It is done before angioplasty or coronary bypass surgery.
Management Ischemic Heart Disease
- It is divided into three phases:
- General measures.
- Pharmacological treatment.
- Invasive treatment.
General Measures Ischemic Heart Disease
- Do not smoke
- Aim at ideal body weight
- Take regular exercise
- Avoid severe exertion, vigorous exercise and exercise in cold weather
- Take sublingual nitrate before taking exertion that may induce angina.
Pharmacological treatment Ischemic Heart Disease
Following agents are used with successful outcome.
1. Antiplatelet agents:
- Aspirin is used usually in dose of 75–150 mg daily.
- Clopidogrel is used along with or without aspirin at dose of 75 mg daily.
2. Anti-anginal agents:
- Sublingual glycertrinitrate effctively abort anginal attack by causing coronary vasodilatation and reducing preload and cardiac output.
- Beta-blockers improve cardiac effiency and reduce oxygen consumption. Cardioselective agents such as atenolol 25 to 50 mg, metoprolol 200 mg daily can be used.
- Calciumchannel antagonists, i.e. amlodipine, lacidipine. They are the vasodilators and lowers myocardial oxygen demand by reducing blood
pressure and myocardial contractility. - Potassiumchannel opener, i.e. nicorandil has atrial and venous dilatation property which does not exhibit tolerance.
Invasive treatment Ischemic Heart Disease
- *Percutaneous coronary *intervention or percutaneous transluminal coronary *angioplasty is done.
- Coronary artery bypass grafting is done.
The management of myocardial infarction is divided into two parts:
1. Early management.
2. Late management.
Early Management Ischemic Heart Disease
- Aspirin 150–300 mg to be chewed earliest.
- Sublingual glyceryl trinitrate 0.4–1 mg, to be repeated, if necessary
- Oxygen through nasal cannula at a rate of 2–4 L/min.
- Procure IV line and take blood samples for glucose, lipids and complete haemogram.
- Record 12lead ECG.
- Pain may be relieved by IV morphine (5 mg) plus metoclopramide as an antimetic (10 mg).
- IV betablockers (metoprolol 5 mg every 2–5 minutes for 3 doses) for ongoing chest pain, hypertension and tachycardia provided there is no contraindication.
- Thrombolysis should be done.
- If PTCA is planned, give GP IIb/IIIa inhibitor
- After admission immediately shift the patient to ICU or
ICCU
In Hospital treatment Ischemic Heart Disease
Hospitalization and strict Bed rest
- Hospitalize the patient and advice strict bed rest. As early as the patient is hospitalized, the bettr it is.
- Patient should be strictly admittd in ICCU.
Analgesia Ischemic Heart Disease
- IV morphine sulphate 10 mg and an anti emetic, i.e. cyclizine 50 mg is given through I.V. cannula.
- The drug is repeated depending on the response till complete analgesia is received and patient feels bettr.
Anti-platelet drugs Ischemic Heart Disease
Low dose aspirin, i.e. 75 to 150 mg and clopidogrel 300 mg stat and then 75 mg orally daily is given.
Oxygen therapy Ischemic Heart Disease
Inhalation of oxygen increases arterial partial pressure of oxygen, so there is increase in the concentration of oxygen gradient which is responsible for diffusionn of oxygen in ischemic myocardium from adjacent better perfused areas. This is given by facemask or nasal prongs for a day or two after infarction.
Thrombolysis Ischemic Heart Disease
- Coronary thrombolysis helps to restore patency of coronary artery preserves left ventricular function and improves survival.
- The choice of drug for thrombolysis is less important than the speed of treatment.
- Streptokinase, 1.5 million units in 100 mL of saline given in an intravenous infusion over 1 hour, is a widely accepted method.
It is a cheap, but being antigenic, sometimes, may cause serious allergic manifestations.
Hence, it can be used once and therapy is changed if the patient requires second thrombolysis within few years.
Alteplase (tissue Plasminagen activator (tPa)
- It is a potent firinolytic drug but is expensive.
- It is less antigenic and does not cause hypotension.
- The current tPA regimen given over 90 minutes (bolus dose of 15 mg followed by 50 mg over 30 minutes and then 35 mg over next 60 minutes) is widely accepted. The other drugs include reteplase given in double dose regime i.e.
10 million units over 2–3 minute followed by another dose of 10 million units after 30 minutes.
Tenectaplase given as bolus dose of 53 mg/kg over 10 seconds. Both reteplase and tenectaplase are known as bolus firinolytics.
Angioplasty Ischemic Heart Disease
Immediate angioplasty of infarct related artery is safe and is effctive alternative to thrombolysis. It is done in the patients in whom the hazards of thrombolysis is high.
Anti-coagulants Ischemic Heart Disease
- Subcutaneous heparin, i.e. 7,500 units twice a day for 7–10 days or till discharge of patient from the hospital can be employed.
In patients who do not receive thrombolytic therapy to prevent venous thrombosis. - Patients who receive thrombolytic therapy (tPA) should receive immediate and full doses of heparin (10,000 U bolus plus, l000 U hourly).
Beta-adrenergic Blockers Ischemic Heart Disease
Acute betaadrenoreceptors blockade intravenous atenolol (5–l0 mg given over 5 minutes) or metoprolol (5–15 mg given over 5 minutes) relieves pain, reduces arrhythmias, salvages myocardium and improves short term mortality in patients who present within l2 hours of onset of pain.
Nitrates and other agents Ischemic Heart Disease
Sublingual glyceryl trinitrate 0.4 mg is useful in threatened infarction.
Sedatives Ischemic Heart Disease
Diazepam 5mg for three to four times a day is effctive. It is given for few days.
Diet Ischemic Heart Disease
- For fist 4 to 5 days low calorie diet which is divided into multiple meals is given.
- If heart failure is present restrict the salt.
- From second week, food should be increased in amount.
Lipid lowering agent Ischemic Heart Disease
Atorvastatin is given to reduce the LDL levels.
Late Management Ischemic Heart Disease
1. Risk stratifiation and further investigations: Prognosis of patient survived after myocardial infarction depends on degree of myocardial damage, any residual ischemia and presence of ventricular arrhythmias.
2. Life style modifiation:
- Stop smoking
- Diet control
- Regular exercise.
3. Secondary prevention
- Antiplatelet agents, i.e. aspirin
- Lipid lowering agents
- Betablockers and ACEI in congestive cardiac failure and hypertension.
- Control of blood sugar in diabetes.
4. Rehabilitation and after care:
- Physical activities should be restricted for 4 to 6 weeks since infarct takes 4–6 weeks to become replaced with firous tissue.
- Gradual mobilization and return to work over 6 weeks.
When there are complications, the regimen has to be modifid accordingly. - Exercise within the limits set by angina and tiredness will do no harm but much good. Same limits apply to sexual activity.
- Control of obesity, regular exercises, cessation of smoking, adoption of a less frenetic way of life and control of plasma lipids by diets and drugs.
- Complications should be managed. Pain relief, reassurance, rest and correction of hypokalemia play a major role in prevention of arrhythmias.
Routine drug therapy Ischemic Heart Disease
- Low dose aspirin, i.e. 75 to 150 mg daily and is continued indefiitely.
- Beta-adrenergic blocker should be given for 4 to 6 weeks if there is no contraindication.
- ACE inhibitor, i.e. captopril 25 mg TID or ramipril 2.5 to 5 mg BD
- Lipid lowering agent atorvastatin is given to lower the LDL levels.
Question.62. Write short answer on jugular venous pulse.
Answer. Jugular venous pulse is an important physical sign of cardiovascular disease.
This pulse is examined for pressure and wave forms.
Procedure of measuring jugular venous pulse
This is examined y reclining the patient against pillows at 450 angle, neck muscles should be relaxed, upper level of pulsation of an internal jugular vein is seen, though vein may itself be not visible.
In a normal person, jugular venous pulsation in above said position remains either behind the clavicle or below it and rarely extends beyond 2 to 3 cm above sternal angle.
Waveforms of jugular venous pulse
Waveform of jugular venous pulse in patient of sinus rhythm is:
- ‘a’ wave occur due to atrial systole. This is absent in atrial firillation but becomes large in tricuspid stenosis, right ventricle hypertrophy and pulmonary hypertension.
- ‘c’ wave corresponds to tricuspid closure ‘v’ wave result from building of pressure in right atrium during ventricular systole when tricuspid valve is closed.
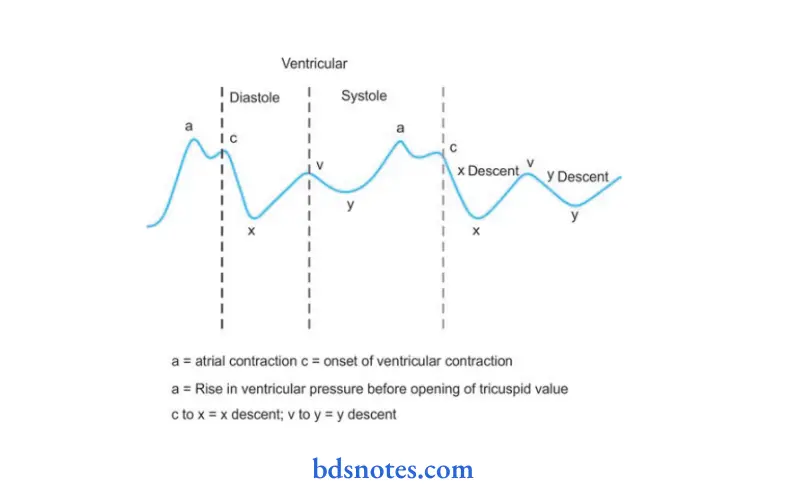
- This wave becomes prominent in tricuspid regurgitation or congestive heart failure.
- All the above mention three waves i.e. a, c and v waves are known as positive waves.
- There are two more waves present beside these which are known as negative waves or descents i.e. x and y descents.
- ‘x’ descent correspond with atrial relaxation and downward displacement of tricuspid valve at the time of ventricular systole. It is prominent in constrictive pericarditis.
- Following the summit of ‘v’ wave, negative ‘y’ descent is produced by opening of tricuspid valve and rapid flw of blood in right ventricle.
- Prominent ‘y’ descent occurs in constructive pericarditis and congestive heart failure along with ‘v’ wave, so it is collectively known as prominent ‘v’ wave and ‘y’ descent.
- Slow ‘y’ descent occurs in tricuspid stenosis where ‘a’ wave is prominent.
- Giant ‘a’ wave is a large sharp systolic wave seen in venous pulse during forcible contraction of right ventricle against closed tricuspid valve.
It is seen in complete heart block, atrioventricular dissociation and junctional rhythm.
Question.63. Write short answer on beta blockers.
Answer. These drugs inhibit responses mediated by the adrenergic β blockers.
Classifiation Beta Blockers.
- Cardioselective (β1): Metoprolol, atenolol, acebutolol.
- β2 selective: Butoxamine.
- Nonselective (β1+ β2): Propranolol, nadolol, sotalol, timolol.
Actions Beta Blockers
- Heart: These drugs decreases force of contraction, decreases AV conduction, decreases heart rate, decreases automaticity of myocardial fiers thus cardiac output is decreased.
- Blood vessels: On prolong administration BP falls in hypertensives.
- Respiratory system: It causes increase of bronchoconstriction in asthmatics.
- Eye: β-blockers decrease aqueous humor secretion.
Adverse Reactions Beta Blockers
- CVS: Bradycardia, heart block and can precipitate heart failure.
- Respiratory system: these drugs can precipitate bronchial asthma.
- CNS: Disturbed sleep, fatigue, hallucination and mental depression.
- Muscular weakness and tiredness
- Abrupt withdrawal can cause angina or frank myocardial infarction.
Contraindications Beta Blockers
- They are contraindicated in asthmatics and COPD.
- They are contraindicated in patients of Prinzmetal angina.
- They are contraindicated in peripheral vascular disease.
- They are contraindicated in patients with low cardiac reserve.
- They are contraindicated in diabetic who are taking oral antidiabetic drugs as they delay recovery from hypoglycemia.
Uses or Indications of β Blockers
- Hypertension: β blockers are used to treat all the grades of hypertension.
They are also indicated in angina, myocardial infarction and cardiac arrhythmias. - In prophylaxis of angina and myocardial infarction: β blockers decreases oxygen demand of myocardium and decreases the heart rate.
These drugs reduces the frequency of angina attcks.
They are indicated in acute phase of myocardial infarction so that they limit the size of infarct. - In cardiac arrhythmias: They are indicated in atrial arrhythmias i.e. atrial fibrillation, atrial flutter and paroxysmal supraventricular tachycardia.
- Congestive cardiac failure: Chronic usage of β blockers reducec rate of mortality during chronic heart failure.
- Pheochromocytoma: These drugs control cardiac manifestations produced by pheochromocytoma.
- Glaucoma: They decrease intraocular pressure by decreasing secretion of aqueous humor. Timolol is the choice of drug.
- In prophylaxis of migraine: They decreases the frequency of migraine headache.
- Hyperthyroidism: Sign and symptoms of hyperthyroidism decreases due to blockade of β receptors.
- Essential tremors: Propranolol provides relief in tremors.
- Anxiety: It acts as antianxiety drug.
- Alcohol withdrawl: Propranolol provides benefi in alcohol withdrawl.
- Dissecting aortic aneurysm: β blockers reduce cardiac contractility as well as development of pressure during systole.
Question.64. Write short answer on calcium channel blocker.
Answer. Following are the calcium channel blockers:
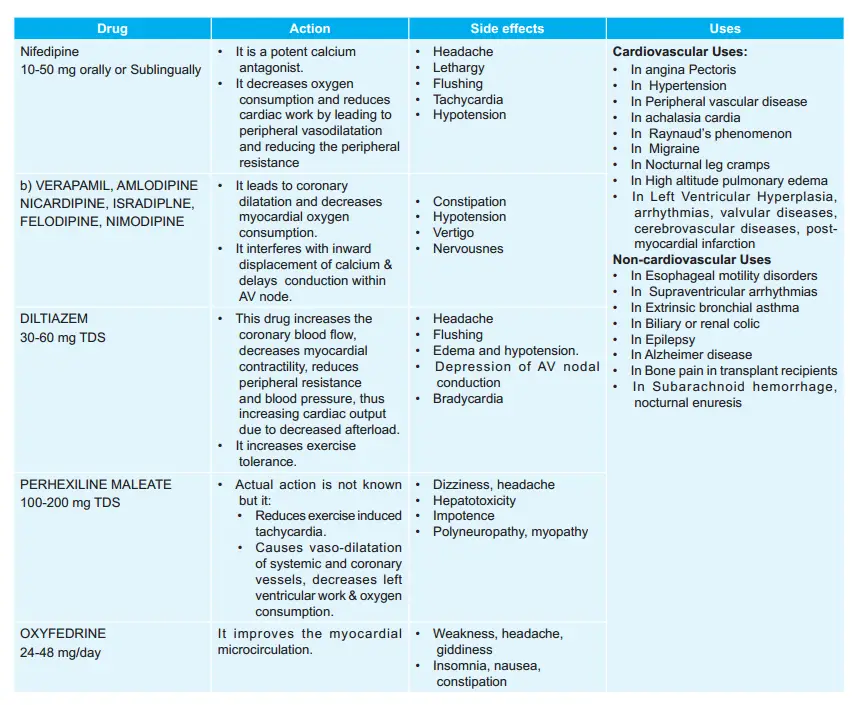

Leave a Reply