Diseases Of Blood And Blood Forming Organs
Question.1. Write short note on pernicious anemia.
Answer. Pernicious anemia is a type of a chronic progressive, megaloblastic anemia of adults and is caused by a deficiency of intrinsic factors in stomach.
Etiology
- Due to impaired absorption of vitamin B12: This occurs due to the atrophy of gastric mucosa which results in lack of secretion of intrinsic factor.
- As autoimmune reaction to gastric parietal cells or intrinsic factor.
- Strict vegetariAns suffr from vitamin B12 deficiency as it is present only in eggs, meat, and milk.
- Malabsorption of vitamin B12 due to inadequate gastric production or defective functioning of intrinsic factor.
- Various other causes which lead to the deficiency of vitamin B12 are gastrectomy, celiac disease, Crohn’s disease, alcoholism, prolong usage of drugs, i.e. proton pump inhibitors, colchicines.
Clinical Features
- Generalized weakness, palpitation, nausea, vomiting, anorexia, diarrhea and dyspnea.
- Patients have smooth, dry, and yellow skin.
- Neurological manifestation includes tingling sensation in hand and feet, paresthesia of extremities due to peripheral nerve degeneration.
- Glossitis, glossodynia (painful tongue) and glossopyrosis (itching and burning tongue).
- Tongue appears beefy red in color.
- Sometimes loss of papilla produces a bald appearance of tongue.
- Sometimes hyperpigmentation occurs in mucosa.
- Inflmmation and burning sensation surround entire oral mucosa.
Read And Learn More: Oral Pathology Question And Answers
Histopathology
- Oral epithelial cells become enlarged and show hyperchromatic nuclei with prominent nucleoli along with serrated nuclear membrane.
- Epithelium becomes atrophic.
- There is presence of subepithelial chronic inflmmatory cell infitration.
Laboratory Findings
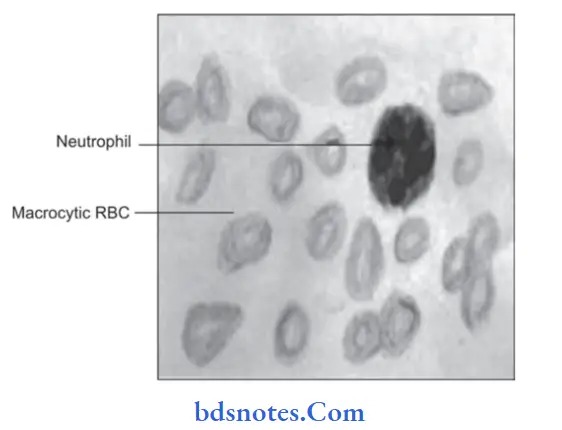
- Macrocytosis is commonly seen.
- Red blood cell count is decreased, at times it is 10 lakh/cubic mm of blood.
- Mild to moderate thrombocytopenia is also seen.
- MCV, MCH, MCHC concentration is normal
- Howell jolly bodies and cabot rings are present.
- Neutrophils are hypersegmented.
- Buccal scrapings show nuclear abnormalities
- Schilling test show vitamin B12 deficiency.
- Serum lactate dehydrogenase is markedly increased while serum potassium, cholesterol and skeletal alkaline phosphatase are often decreased.
- Bone marrow is hypercellular and show trilineage differentiation.
- Erythroid precursors are large and oval. Nucleus is large and contains coarse motley chromatin clumps giving checkboard appearance.
Treatment
IM injection of vitamin B12 is given.
Question.2. Write notes on aplastic anemia.
Answer. It is a rare disorder characterized by the peripheral blood pancytopenia (anemia, leukopenia and thrombocytopenia) associated with bone marrow suppression.
Etiology
- Drug and chemicals: Common drugs which can cause aplastic anemia are benzene derivatives, chloramphenicol,penicillin, sulfonamides and anticancer drugs.
- Infections: Patients with bacterial disease such as tuberculosis and viral infections like hepatitis and infection mononucleosis can cause pancytopenia.
- Radiation: Longterm exposure to continuous radiation has lead to development of aplastic anemia.
- Other causes: Pregnancy and thymoma can cause aplastic anemia.
Clinical Features
- It is more common in young adults and elderly individuals.
- Marked pallor of skin and petechiae.
- Numbness and tingling of extremities.
- Generalized edema of body (anasarca).
- Fever and infections occur due to neutropenia.
- Spontaneous gingival bleeding and epistaxis.
- Multiple areas of ulceration in oral mucosa.
Treatment
Blood transfusion, splenectomy and bone marrow transplant.
Question.3. Write notes on sickle cell anemia.
Or
Write short note on sickle cell anemia.
Answer. It is an autosomal dominant disorder.
- In sickle cell anemia the erythrocytes assume crescent shape and undergo lysis.
Clinical Features
- It is more common in females.
- Malaise, weakness and jaundice with yellow sclera.
- Pallor, loss of appetite and muscular rigidity.
- Fever, pain in abdomen and back in joints.
- Swelling in joints, hand and feet.
- There may be delayed eruption and hypoplasia of dentition.
- There is presence of mongoloid faces with high cheek bones and bimaxillary prognathism.
Radiographic Features
- Skull radiographs reveals multiple small spicules (small needle shaped body) across calvarium, which produces “Hair-on-end” appearance.
- IOPA reveals “Step ladder” like trabeculae between contagious and posterior teeth.
- Increased osteoporosis and hyperplasia of bone marrow.
Treatment
No specific treatment.
Oxygen and blood transfusion in serious situation.
Question.4. Write notes on purpura.
Answer. It is defined as purplish discoloration of skin and mucous membrane due to subcutaneous and submucus extravasation of blood.
Clinical Features
- Purpura commonly occurs among adults below 40 years and females are more commonly affcted.
- Sudden spontaneous occurrence of petechiae (small pin point hemorrhage under skin or mucosa), ecchymoses or hematomas in skin and mucous membrane.
- Bleeding spots on skin or mucosal surface which do not blanch on pressure.
- Women may have heavy menses or bleeding between periods.
- Spontaneous gingival bleeding is present.
- Bleeding into TMJ results in pain and trismus.
Treatment
- Steroid therapy and repeated blood transfusions.
- Splenectomy and immunosuppressive drug therapy is required.
Question.5. Write short note on hemophilia.
Answer. Hemophilia is a potentially fatal inherited bleeding disorder characterized by the profuse hemorrhage due to defiiency of clottng factors.
Types
- Hemophilia A or classic hemophilia: In this factor VIII defiiency is present.
- Hemophilia B or christmas disease: In this factor IX deficiency is present.
- von Willebrand’s disease: In this factor VIII defiiency is present along with defective platelet function.
Clinical Features
- Disease is mostly characterized by the easy bruising and prolongs bleeding particularly often accidental, surgical and dental trauma.
- Spontaneous bleeding into subcutaneous tissue or internal orgAns leads to recurrent soft tissue hematoma formation.
- Gastric hemorrhage may occur in case of gastric ulcer.
Joint problems occur due to degenerative changes in joint structures, osteoporosis and muscle atrophy. - Severe hemorrhage from gingival tissue after dental extraction.
- Slight trauma may lead to hematoma formation in tongue,lips and palate.
- Hemophilic patient has high caries index and severe periodontal disease.
Treatment
- Immediate transfusion of factor VIII or IX concentrate is primary treatment.
- Patient need transfusion in every 12 hours until bleeding stops.
- Analgesic and corticosteroids reduce joint pain and swelling.
- In mild hemophilia, use of IV desmopressin is done.
Question.6. Write short note on oral manifestations of leukemia.
Answer. Following are the oral manifestations of leukemia Patient has got gingival hyperplasia which is the constant feature of leukemia.
- Gingiva become boggy, edematous and deep red and bleed easily.
- Gingival swelling is present due to leukemic infitration.
- Purpuric lesions of oral mucosa analogus to cutaneous ecchymosis may also be seen.
- Loosening of teeth due to necrosis of PDL is present.
- Destruction of alveolar bone is seen.
- Crusting of lips is also seen.
Question.7. Write short note on Plummer-Vinson syndrome.
Answer. Plummer-Vinson syndrome is also known as Paterson-Brown-Kelly syndrome.
Plummer-Vinson syndrome consists of following features i.e. dysphagia, iron deficiency anemia,koilonychia and glossitis.
Clinical Features
- It is seen in middle aged women.
- Patient has characteristic asthenic appearance.
- Esophageal webs are present which leads to dysphagia.
- Tongue is smooth and red.
- Angular cheilitis is also seen.
- Nails of the patient are spoon-shaped.
Diagnosis
- Clinical diagnosis reveals all the above-mentioned features.
- During blood examination picture of iron deficiency anemia is present.
- Biopsy reveals atrophy of epithelium, lamina propria as well as muscles.
Management
- Iron deficiency anemia should be corrected by giving hematinics to the patient.
- Esophageal dilatation should be done.
Question.8.Define and classify anemia. Describe iron deficiency anemia.
Or
Write in detail on iron deficiency anemia.
Or
Write short note on iron deficiency anemia.
Or
Define anemia. Describe iron deficiency anemia in detail.
Answer. Anemia is defined as abnormal reduction in number of circulating RBCs, quantity of hemoglobin and the volume of packed red cells in a given unit of blood.
Classification of Anemia
Etiological classification of anemia (By Lea and Febiger 1981)
- Loss of blood
- Acute posthemorrhagic anemia
- Chronic posthemorrhagic anemia.
- Excessive destruction of red blood corpuscles
-
- Extracorpuscular causes
- Antibodies
- Infections like malaria
- Splenic sequestration and destruction
- Associated diseases like lymphomas
- Drugs, chemical and physical agents
- Trauma to RBC.
- Extracorpuscular causes
- Intracorpuscular hemolytic diseases
-
- Hereditary
- Disorders of glycolysis
- Faulty synthesis or maintenance of reduced glutathione.
- Qualitative or quantitative abnormalities in the synthesis of globulin
- Abnormalities in RBC membrane
- Erythropoietic porphyria
- Acquired
- Paroxysmal nocturnal hemoglobinuria
- Lead poisoning.
- Hereditary
-
- Impaired blood production resulting from deficiency of substances essential for erythropoiesis
- Iron deficiency
- Deficiency of various B vitamins: Vitamin B12 and folic acid (pernicious anemia and megaloblastic anemia); pyridoxine responsive anemia
- Protein deficiency
- Possibly ascorbic acid deficiency
- Inadequate production of mature erythrocytes
- Deficiency of erythroblast
- Atrophy of bone marrow: Aplastic anemia
- Chemical or physical agents
- Hereditary
- Idiopathic.
- Isolated erythroblastopenia
- Thymoma
- Chemical agents
- Antibodies.
- Atrophy of bone marrow: Aplastic anemia
- Infiltration of bone marrow
- Leukemia, lymphomas
- Multiple myeloma
- Carcinoma, Sarcoma
- Myelofibrosis.
- Endocrine abnormalities
- Myxedema
- Addison’s disease
- Pituitary insufficiency
- Sometimes hyperthyroidism.
- Chronic renal failure
- Chronic inflammatory disease
- Infectious
- Deficiency of erythroblast
Noninfectious including granulomatous and collagen disease.
Cirrhosis of liver.
Morphological Classification of Anemia
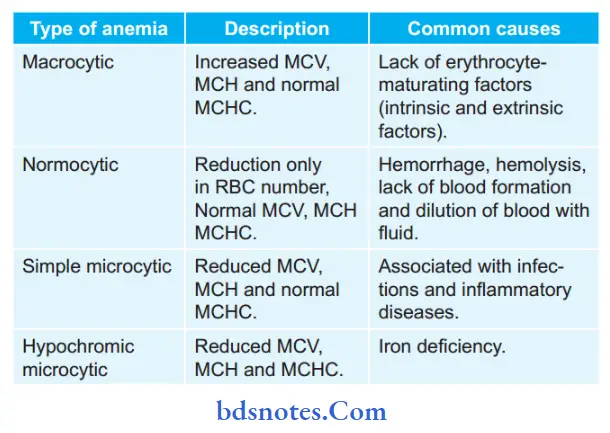
MCV = Mean corpuscular volume
MCH = Mean corpuscular hemoglobin
MCHC = Mean corpuscular hemoglobin concentration.
Iron Deficiency Anemia
Iron deficiency anemia results due to a deficiency of iron in the body.
Etiology
- Exogenous Cause: It is due to dietary deficiency
- Endogenous Cause:
- Absorption Defect as occurs in.
- Histamine, i.e. fast achlorhydria.
- Gastric operations, i.e. total gastrectomy and partial gastrectomy.
- Eterogeneous:
- Unusual hurry in the passage of chyme.
- Abnormality in absorbing mucosa.
- Transport Defect, i.e. atransferrinemia.
- Loss in Iron from Body:
- Loss due to hemorrhage in peptic ulcer, hiatus hernia, Ca stomach, Ca colon and hookworm manifestation.
- Excessive menstrual bleeding.
- Excessive excretion.
- Increased Requirement of Iron in pregnancy and lactation.
- Absorption Defect as occurs in.
Clinical Features
- Females are more commonly affected during 4th and 5th decades.
- Patient complains of lack of concentration, tiredness,headache, presence of tingling sensations over extremities.
- Nails of the patient become britte and nail bed becomes spoon shaped which is also known as koilonychia.
- Patients feel difficulty in swallowing. This is also termed as dysphagia.
- Pigmentation can be seen over the dorsum of hand and metacarpophalangeal joint which is also known as knuckle pigmentation.
- Plummer-Vinson syndrome is associated with iron defi ciency anemia and other features are dysphagia, koilonychia and glossitis.
Oral Manifestations
- Presence of pallor of oral mucosa as well as gingiva.
- Atrophy of oral mucosa is present. This is seen on tongue and buccal mucosa.
- Glossodynia, i.e. pain in the tongue and glossopyrosis, i.e.reddening of tongue is present.
- Atrophy of filiform and fungiform papillae is present giving tongue a bald or smooth or glistening appearance.
- Presence of cracking and fisuring is seen at corner of mouth suggestive of angular cheilitis.
- At times aphthous ulcers are also seen.
Laboratory Diagnosis
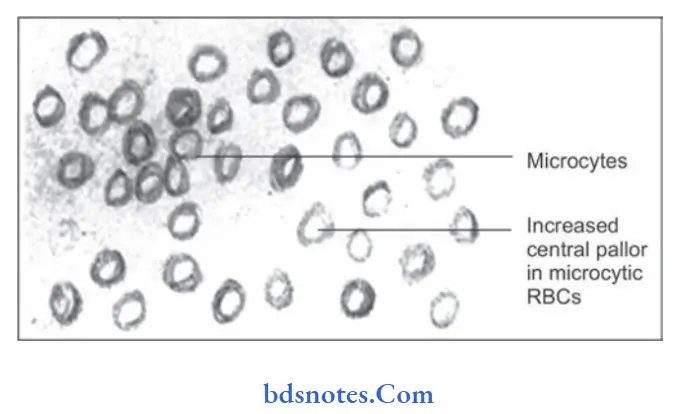
- Examination of peripheral blood picture shows:
- Chromicity: Hypochromia of RBC
- Central pallor increased
- Anisochromia present
- Size: Microcytic anisocytotic
- Shape: Poikilocytosis often present, pear shaped tailed variety of RBC, elliptical form common.
- Target cell: Present
- Reticulocytes: Present
- Osmotic fragility: Slightly decreased
- ESR: Seldom elevated
- Chromicity: Hypochromia of RBC
- RBC count is between 3,000,000 to 4,000,000 cells per cubic mm of blood.
- Presence of low serum iron and ferritin with an elevated total iron binding capacity.
- Hemoglobin level is at 4 mg/dL or below it.
- MCV, MCH, and MCHC are decreased.
Treatment
- Patient should be kept on oral iron therapy. Ferrous fumarate or ferrous sulphate should be given to the patient.
300 mg tablet should be given 3 to 4 times a day for six months duration.
Question.9.Classify gingival hyperplasia and describe leukemia.
Answer.
Classifiation of Gingival Hyperplasia
On basis of etiological factors and pathologic changes
- Inflammatory enlargement
- Chronic
- Acute
- Drug-Induced Enlargement
- Enlargement associated with systemic disease
- Conditional enlargement
- Pregnancy
- Puberty
- Vitamin C deficiency
- Plasma cell gingivitis
- Non-specifi conditioned enlargement (Pyogenic granuloma)
- Systemic diseases causing gingival enlargement
- Leukemia
- Granulomatous disease (E.g. Wegner’s Granulo matosis, sarcoidosis)
- Conditional enlargement
- Neoplastic Enlargement
- Benign tumors
- Malignant tumors.
- False Enlargement.
Using the criteria of location and distribution gingival enlargement is designated as follows:
- Localized: Gingival enlargement limited to one or more teeth.
- Generalized: Involving the gingiva throughout the mouth.
- Marginal: Confied to marginal gingiva.
- Papillary: Confied to interdental papilla.
- Diffse: Involving the marginal and attched papillae.
- Discrete: Isolated sessile or pedunculated tumor like enlargement.
On basis of degree of gingival enlargement
Grade 0: No sign of gingival enlargement.
Grade I: Enlargement confimed to interdental papilla.
Grade II: Enlargement involves papilla and marginal gingiva.
Grade III: Enlargement covers three quarters or more of the crown.
Leukemia
Leukemia is a disease which is characterized by overproduction of
WBCs which are present in circulating blood in an immature form.
Types of Leukemia
- Acute
- Chronic
Etiology
- Chromosomal abnormality: Presence of an abnormal chromosome, e.g. Philadelphia chromosome.
- Exposure to high doses of radiation therapy.
- Exposure to certain chemicals, e.g. phenyl butazone and benzene.
- Myeloproliferative disorders like polycythemia vera.
- Congenital or genetic abnormalities.
- Presence of primary immune defiiency
- Infection with human leukocyte virus.
Acute Leukemia
Classification of Acute Leukemia (FAB Classifiation)
1. Acute myeloblastic leukemia (AMD)
- M0: Minimally differentiated: Myeloblasts lack defiite cytologic and cytochemical features but have myeloid lineage antigens.
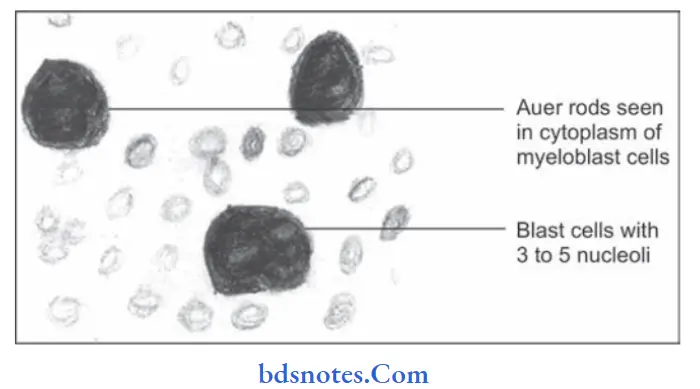
- M1: AML without maturation: Myeloblasts
predominate with distant nucleoli, few granules or Auer rods are present. - M2: AML with maturation: Myeloblasts with promyelocytes predominate and Auer rods may be present.
- M3: Acute promyelocytic leukemia: Hypergranular promyelocytes often with multiple Auer rods are seen.
- M4: Acute myelomonocytic leukemia: Mature cells of both myeloid and monocytic series in peripheral blood; myeloid cells resemble M2
- M5: Acute monocytic leukemia: Promonocytes or undiffrentiated blast.
- M6: Acute erythroleukemia: Erythroblast predominate;myeloblasts and promyelocytes also increased
- M7: Acute megakaryocytic leukemia: Pleomorphic undiffrentiated blast cells predominate and react with antiplatelet antibodies.
2. Acute lymphoblastic leukemia
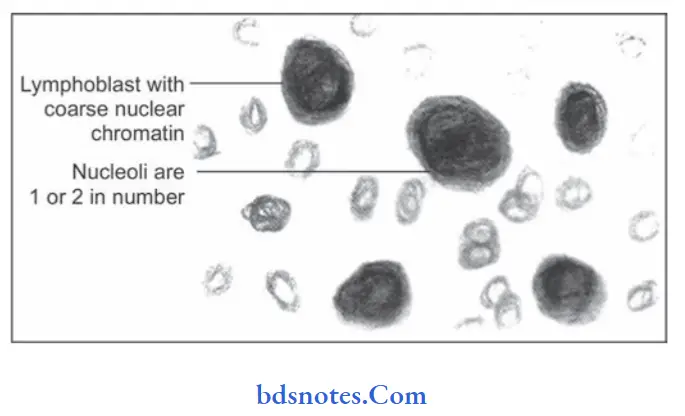
- L1: Acute lymphoblastic (Seen in children): Homogeneous small lymphoblasts; scanty cytoplasm,regular round nuclei, inconspicuous nucleoli.
- L2: Acute lymphoblastic (Seen in adults): Heterogeneous lymphoblasts; variable amount of
cytoplasm, irregular or cleft nuclei, large nucleoli. - L3: Burkitts type (Uncommon): Large homogenus lymphoblasts; nuclei are round to oval, prominent nucleoli, cytoplasmic vacuolation.
Clinical Features
Acute leukemias are more common in children and adults from 1st to 4th decades of life.
Clinical features are due to:
- Bone marrow failure
- Anemia is seen leading to pallor, lethargy and dyspnea.
- Pyrexia is present.
- Bleeding manifestations are present, such as spontaneous bruises, petechiae, bleeding from gingiva.
- Infections of multiple organs are present.
- Organ infiltration
- Presence of pain and tenderness in bones.
- Enlargement of tonsils is present.
- Lymphadenopathy is seen.
- Hepatomegaly and splenomegaly are common findings.
- Chloroma or granulocytic sarcoma is a localized tumor mass occurring over the skin or orbit by local infiltration of tissues by leukemic cells.
Oral Manifestations
- Bleeding from gingiva is present. Gingiva becomes boggy,edematous and red in color.
- Presence of paresthesia of lower lip.
- Crustation over lips is seen.
- Mobility of permanent teeth is present.
- Oral mucosa appears pale with ulceration along with petechiae and ecchymosis.
Laboratory Findings
- Anemia: It is normochromic in type, moderate reticulocytes are seen, few nucleated red cells.
- Thrombocytopenia: Platelet count is below 50,000/µl of blood.
- WBC count: It ranges from subnormal to markedly elevated. It is 1,00,000/µl of blood in advanced cases. Leucocytes in peripheral blood are blast cells.
- Bone marrow examination shows hypercellularity. Bone marrow is packed with leukemic blast cells. Erythropoietic cells are reduced. Megaloblastic features and ring sideroblasts are present.
Chronic leukemia
These are hematologic malignancies in which predominant leukemic cells are initially well differentiated. They are of two
types:
1. Chronic myeloid leukemia
2. Chronic lymphocytic leukemia
Chronic myeloid leukemia
It consists of large leukemic cells and diffrentiated WBCs in bone marrow.
Clinical Features
- It occurs during 3rd and 4th decades of life.
- Splenomegaly is present.
- Patient complains of loss of weight, abdomen prominence.
- Presence of anemia leads to weakness, fatigue and dyspnea.
- Petechiae and ecchymosis is seen.
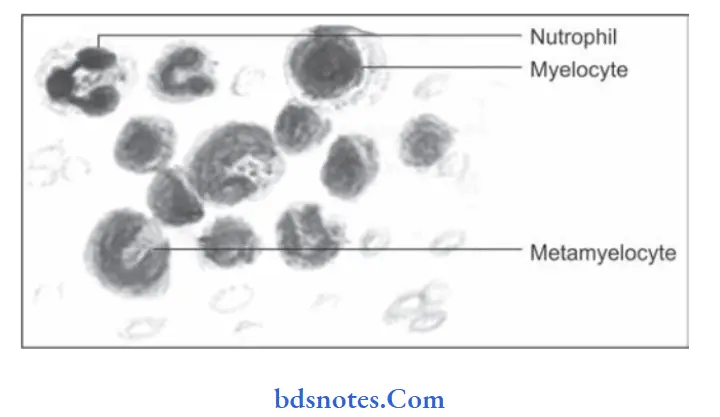
Laboratory Findings
- Anemia is normocytic and normochromic type.
- Marked leucocytosis is present, i.e. 2,00,000 cells/µl.
- There is increased proportion of basophils.
- Bone marrow shows hypercellularity with total or partial replacement of fat spaces by proliferating myeloid cells.
Chronic lymphocytic leukemia
It is the malignancy of mature B cells.
Clinical Features
- It occurs during 4th decade of life.
- Male predilection is seen.
- Features of anemia are seen, i.e. weakness, fatigue and dyspnea.
- Lymphadenopathy is commonly present.
- Hepatomegaly and splenomegaly is commonly seen.
- Hemorrhagic manifestations are common.
Oral Manifestations
- Gingival hypertrophy is present. Ulceration of gingiva with necrosis is present.
- Tongue is dark and swollen.
- Presence of mobility of teeth is seen.
- Necrosis of PDL is seen.
- Alveolar bone destruction is also present.
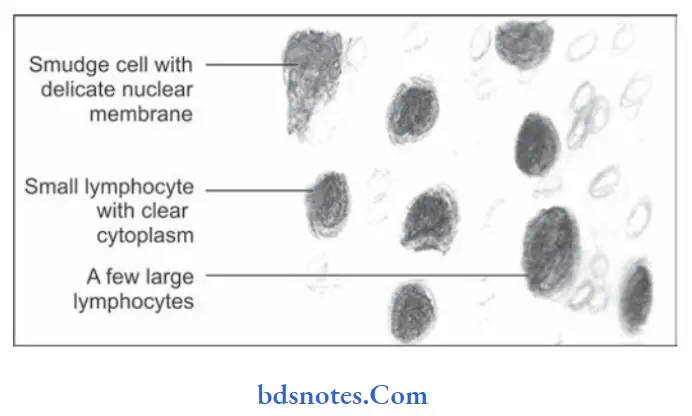
Laboratory Findings
- Anemia is mild to moderate and is normocytic normochromic type.
- Marked leucocytosis is present.
- Leucocytes are mature small lymphocytes.
- Platelet count is normal or moderately reduced.
Treatment
Chemotherapeutic drugs, radiation therapy and corticosteroids which leads to prolong remission and cures in some forms of disease.
Question.10. Write short note on erythroblastosis fetalis.
Answer. Erythroblastosis fetalis is a hemolytic anemia of newborns secondary to blood incompatibility mainly Rh factor between the mother and fetus.
Currently this disorder is uncommon due to use of anti antigen gamma globulin at delivery in mothers with Rh-negative blood.
Pathogenesis
It occurs due to the inheritance by the fetus of a blood factor from Rh positive father which act as foreign antigen to Rh negative mother.
Transplacental leak of RBCs from fetus to mother leads to immunization of mother and formation of antibodies which are transferred back to fetus transplacentally, this leads to fetal hemolysis.
Clinical Features
- Features depend on the severity of hemolysis, if it is severe child is stillborn or dead.
- Alive born child suffer from anemia with pallor, jaundice, compensatory erythropoiesis, i.e. medullary and extramedullary and edema.
Oral Manifestations
- Deposition of blood pigments in enamel and dentin of neonate which produces green, brown or blue hue.
- Enamel hypoplasia can also be present.
- A ring-like defect is present at incisal edges of deciduous anterior teeth and middle portion of deciduous cuspid and fist molar crown known as Rh hump.
Histopathology
Ground section of the affected teeth shows positive test for bilirubin.
Laboratory Findings
- RBC count at birth is from 1000000 cells/cu mm to normal level.
- Peripheral smear shows normoblasts or nucleated red cells.
- High bilirubin level.
- Direct Coombs test on cord blood is positive.
Treatment
No treatment is needed as the condition affects only deciduous teeth and not the permanent teeth.

Leave a Reply