Differential Diagnosis Of Periapical Radiolucencies
Question 1. Give differential diagnosis of periapical radiolucencies.
or
Describe in detail the differential diagnosis for periapical radiolucencies.
Answer. Lesions representing as periapical radiolucencies
True Periapical Radiolucent Lesions
That are truly in contact with the apex of the tooth.
- Pulpoperiapical radiolucencies
- Periapical granuloma
- Radicular cyst
- Periapical scar
- Periapical abscess
- Surgical defect
- Osteomyelitis
- Hyperplasia of sinus mucosa
- Periapical cemental dysplasia
- Acute apical periodontitis
- Traumatic bone cyst
- Dentigerous cyst
- Non-radicular cyst
- Benign and Malignant tumors including secondary metastatic deposits
- Giant cell granuloma
- Lymphoreticular tumors of bone
Read And Learn More: Oral Radiology Question And Answers
False (Anatomic Periapical Radiolucencies)
Produced by anatomic cavities or lytic bony lesions that do not contact the apex of tooth.
These radiolucent shadows are shifted from periapex by taking additional periapical radiographs at different angles:
- Mental foramen
- Focal osteoporotic bone marrow defects
- Dental papilla
- Incisive foramen
- Maxillary sinus
- About 30–60% of bone loss must have occurred for a change to be detected on radiographs.
Differential Diagnosis
- Periapical granuloma
- Periapical scar: Here involved tooth shows appearance of filing of root canal.
- Cementoma: During osteolytic stage of cementoma the tooth becomes vital while in granuloma tooth becomes non-vital.
- Radicular cyst: During FNAC straw-colored fluid is not obtained from periapical granuloma while straw color fluid is seen in cyst.
- Periapical cyst or radicular cyst
- Periapical granuloma: During FNAC straw-colored fluid is obtained from cyst while in granuloma flid is not present. Borders of cyst are hyperostotic.
- Periapical cementoma: During early stages, involved tooth is vital in granuloma while it is non-vital in cyst.
- Lateral periodontal cyst: When site ofthe radicular cyst is same as for lateral periodontal cyst, the confusion can be eliminated as the involved tooth is vital in lateral periodontal cyst while it is non-vital in periapical cyst.
- Traumatic bone cyst: Occurs mostly in mandible, while it is not true for periapical cyst.
- Periodontal abscess: Associated tooth is vital in abscess and bone loss is seen.
- Non-radicular cyst
- Primordial Cyst: No history of extraction of tooth is depicted by the patient in primordial cyst. Seen in younger individuals and in posterior region of mandible.
- Keratocyst: Size ofthe cyst is much greater as compared to residual cyst. Residual cyst is unilocular while the keratocyst can be multilocular. Seen in posterior region of mandible.
- Ameloblastoma: Larger in size and can be multilocular. Diameter of ameloblastoma is much greater than residual cyst.
- Periapical abscess
- Periodontal abscess: Periodontal abscess is mostly associated with periodontal pocket and pain. The involved tooth is vital.
- Foramina: In foramina, lamina dura appears to be intact while it is not intact in abscess.
- Marrow space: While taking radiograph, if marrow space get imposed with apex of root, continuity of lamina dura should be detected.
- Periapical osteofirosis: This is associated with the vital tooth while abscess is associated with non-vital tooth.
- Osteomyelitis
- Paget’s disease: In this, almost all the bones except few are affcted while in osteomyelitis affcted bone is involved.
- Eosinophilic granuloma: In osteomyelitis, margins are poor while margins are well defied in eosinophilic granuloma as compared to osteomyelitis.
- Acute apical periodontitis
- Radicular cyst: Tooth is non-vital in radicular cyst while it is vital in periodontitis.
- Periapical abscess: It is not associated with periodontal pocket while periodontitis is associated with pocket formation. Associated tooth is non-vital in periapical abscess, while it is vital in acute apical periodontitis.
- Periapical cemental dysplasia
- Pulpoperiapical lesions: Radiolucent area involving most commonly the lower incisors and is not associated with dental caries but it can be suspected as periapical cemental dysplasia. Mostly pulpoperiapical lesions are associated with the dental caries.
- Ossifying firoma: Seen in younger individuals and is seen most commonly in premolar area while periapical cemental dysplasia is most commonly associated with the incisor area.
- Atraumatic bone cyst: This is extensive in size as compared to periapical cemental dysplasia. Atraumatic bone is mostly seen in younger individuals.
- Cementoblastoma: Seen commonly in mandibular molar or premolar area.
- Traumatic bone cyst
- Radicular cyst: Tooth associated with the traumatic bone cyst is vital while the tooth associated with radicular cyst is non-vital.
- Ameloblastoma: Radiographic appearance in traumatic bone is unilocular while it is multilocular in ameloblastoma.
- Central giant cell granuloma: In traumatic bone cyst the internal bony septae are absent while in central giant cell granuloma internal bony septae are present.
- Eosinophilic granuloma: Traumatic bone cyst, is corticated while eosinophilic granuloma is non-corticated.
- Dentigerous cyst
- Adenomatoid odontogenic tumor: The lesion is associated more commonly with maxillary anterior region while dentigerous cyst is associated with impacted canines and third molars.
- Ameloblastoma: Ameloblastoma is multilocular. Ameloblastoma extends laterally away from tooth while dentigerous cyst encircles the tooth.
- Odontogenic keratocyst: OKC does not undergo bony expansion and also not resorb teeth and is placed more apical to the tooth as compared to dentigerous cyst.
- Radicular cyst: In primary teeth, it gives appearance of dentigerous cyst. So it is mandatory to look for caries in such cases.
- Giant cell granuloma
- Ameloblastoma: It is multilocular, seen in middle age, more susceptible in posterior aspect while giant cell granuloma is unilocular, seen in younger age and is more susceptible in premolar area.
- Traumatic bone cyst: Expansion of bony cortex is not present in traumatic bone cyst while it is seen in giant cell granuloma.
- Odontogenic myxoma: Associated with the impacted tooth and on radiographic examination, it is multilocular while giant cell granuloma is not associated with impacted tooth and is mostly unilocular.
Question 2. Enumerate and discuss in detail periapical radiolucencies.
or
Write short note on periapical radiolucencies.
Answer.
Periapical Radiolucencies
True Periapical Radiolucent Lesions
That are truly in contact with the apex of the tooth
- Pulpoperiapical radiolucencies:
- Periapical granuloma
- Radicular cyst
- Periapical scar
- Periapical abscess
- Surgical defect
- Osteomyelitis
- Hyperplasia of sinus mucosa
- Periapical cemental dysplasia
- Acute apical periodontitis
- Traumatic bone cyst
- Dentigerous cyst
- Non-radicular cyst
- Benign and malignant tumors including secondary metastatic deposits
- Giant cell granuloma
- Lymphoreticular tumors of bone.
False (anatomic Periapical Radiolucencies)
Produced by anatomic cavities or lytic bony lesions that do not ncontact the apex of the tooth.
These radiolucent shadows are shiftd from the periapex by taking additional periapical radiographs at different angles:
- Mental foramen
- Focal osteoporotic bone marrow defects
- Dental papilla
- Incisive foramen
- Maxillary sinus
About 30–60% of bone loss must have occurred for a change to be detected on radiographs.
Periapical Granuloma
It is a localized mass of chronic granulation tissue formed in response to infection.
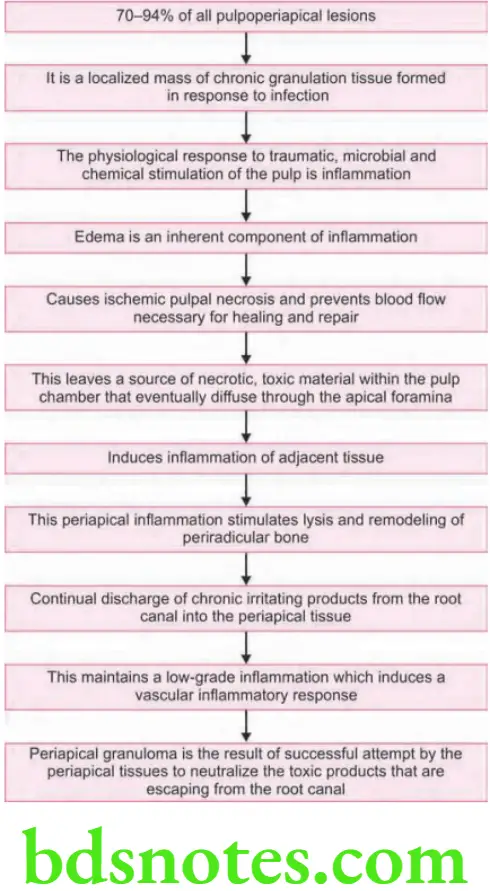
Pathogenesis
- The physiological response to traumatic, microbial and chemical stimulation of the pulp is inflammation.
- Edema is an inherent component of inflammation.
- Edema produces compression of apical blood vessels, causes ischemic pulpal necrosis and prevents blood flow necessary for healing and repair.
- This leaves a source of necrotic, toxic material with in the pulp chamber that eventually diffuse through the apical foramina.
- Induces inflammation of adjacent tissue.
- This periapical inflammation stimulates lysis and remodeling of periradicular bone.
- Continuous discharge of chronic irritating products from the root canal into the periapical tissue.
- This maintains a low-grade inflammation which induces a vascular inflammatory response.
- Periapical granuloma is the result of successful attempt by the periapical tissues to neutralize the toxic products that are escaping from the root canal.
Periapical Radiolucencies Clinical Features
- Tooth is often asymptomatic.
- Previous history of prolonged sensitivity to heat or cold
- Deep caries, a deep restoration or history of trauma.
- Tooth is oftn tender to percussion (because the apical PDL contains inflmed granulation tissue).
- Fail to react to thermal or electrical stimulation (because the pulp is nonvital).
Periapical Radiolucencies Radiographic Features
- Earliest sign: Thickened PDL space at the root apex.
- Well-circumscribed radiolucency: somewhat rounded and surrounding the apex of the tooth.
- Thin radiopaque hyperostotic border.
Periapical Radiolucencies Microscopic Features
- Proliferating endothelial cells, capillaries, young firoblasts, collagen, chronic inflammatory cells, lymphocytes, plasma cells, macrophages.
- Nests of odontogenic epithelium, Russell bodies, foam cells, cholesterol cleft.
- More inflmmation is seen in center of the lesion.
- At periphery: Fibrosis (healing) is seen.
Periapical Radiolucencies Treatment
- Extraction of the involved tooth.
- Root canal therapy (with or without apicoectomy).
- If left untreated, it may undergo transformation to periapical cyst.
Periapical Radiolucencies Periapical (Radicular) Cyst
- 2nd most common pulpoperiapical lesions.
- About 6–17% to 25.9 percent of all pulpoperiapical lesions.
- Inflmmatory cyst.
- Origin in cell rest of malassez, PDL cells which are remnants of Hertwig root sheath.
- About 58% of lateral incisors are involved.
- Deciduous teeth—molars are involved.
- Diameter > 1.6 cm.
- Expansion of cortical plates.
- Initially bony hard to palpation.
- Later rubbery and fluctuant: cortical plate becomes thinned (Crackling sound, crepitus).
Periapical Radiolucencies Microscopic Features
- Lumen surrounded by epithelial lining on a connective tissue wall.
- Periphery: Fibrous.
- Inner region: granulation tissue, chronic inflmmatory cells, foam cells, Russell bodies, cholesterol clefts. Aspiration—straw-colored flid.
- Cholesterol cleft—shiny granules.
Periapical Radiolucencies Differential Diagnosis
- Periapical granuloma
- Periapical scar
- Periapical cemento-osseous dysplasia
- Traumatic bone cyst
- Malignancy.
Periapical Radiolucencies Management
- Root canal treatment.
- 1–3 months recall.
- If extraction is indicated—periapical area should be curetted and microscopic examination should be done.
- Large radicular cysts—surgical enucleation, marsupialization, decompression.
- Sequential postsurgical radiographs should be taken to ensure that lesion is regressing.
- Average healing time for cyst of > 10 mm diameter is 2½ years.
- Incomplete removal—formation of residual cyst.
Periapical scar
- About 2–5% of all periapical radiolucent lesions.
- Composed of dense firous tissue.
- Situated at periapex of pulpless/endodontically treated tooth.
- It represents a previous periapical granuloma, cyst of abscess whose healing has terminated in the formation of dense scar tissue (cicatrix) rather than bone.
- Few spindle-shaped firoblasts.
- Collagen bundles show an advanced degree of hyalinization.
- Well-circumscribed radiolucency.
- Resembles periapical granuloma or cyst but is smaller than these entities.
- Tooth is asymptomatic.
- Radiolucency remains constant in size or shrinks slightly.
- Common site—anterior region of maxilla
- No treatment is required, if asymptomatic root canal filed tooth.
Periapical Abscess
- About 2% of all pathologic periapical radiolucencies.
- Primary or neoteric abscess (acute apical periodontitis, acute periapical abscess).
- Virulent bacteria rapidly spread to the periapical tissues and cause an acute periodontitis.
- Tooth is very sensitive.
- Onset and course of the infection are so sudden that resorption of bone has not yet occurred.
- Apical inflammation forces the tooth slightly from its socket due to which there is increased PDL space around the entire root.
Microscopic Features
- Central region of necrosis containing polymorphonuclear leukocytes surrounded by an inflamed connective tissue wall.
- Chronic resolving abscess—lymphocytes, plasma cells, macrophages and granulation tissue.
Periapical Radiolucencies Clinical Features
- Affcted tooth: Deep restoration, caries, resorption at the apex.
- Tooth is painful on percussion.
- High to bite.
- Does not respond to electric pulp test.
- Abscess may penetrate the cortical plate and from a space infection.
Periapical Radiolucencies Surgical Defect
- About 3% of all periapical radiolucencies.
- It is seen periapically aftr root resection procedures.
- Tooth is usually asymptomatic.
- Small depression in the mucosa over the apical area.
- Rounded, smoothly contoured and has well-defined borders.
- Usually < 1 cm in diameter.
- Periodic radiographic examination shows reduction in size of the radiolucency.
Periapical Radiolucencies Osteomyelitis
- Infection of bone involving all the three components: Periosteum, cortex and bone marrow
- Mandible is more commonly involved as compared to maxilla
- Offending tooth contains nonvital pulp, previously associated with an acute or chronic periapical abscess
- Basal bone is involved
Acute Osteomyelitis
- Similar to acute primary alveolar abscess, since onset and course is rapid and bone resorption has not occurred
- Chronic osteomyelitis
- Low-grade infection of bone
- Ifuntreated follows a protracted course ofbone destruction
- Mandible is most commonly involved
- Offnding tooth contains nonvital pulp
- Previously associated with acute or chronic periapical abscess
- Periapical radiolucency is somewhat rounded with poorly defied and ragged borders
- Such an appearance results from irregular extensions of the inflmmation and infection through marrow spaces and channels in the bone.
Microscopic Features
- Identical to that produced by chronic alveolar abscess
- Necrotic tissue containing polymorphonuclear leukocytes and regions of granulation tissue
- More dead bone (spicules with empty lacunae).
Differential Diagnosis
- Chronic alveolar abscess
- Paget’s disease
Periapical Radiolucencies Treatment
- Removal of involve tooth
- Curettage of socket
- Antibiotics
- Incision and drainage, if require
- Surgical sequestrectomy, saucerization and recontouring.
Periapical cemento-osseous dysplasia
(Periapical Cementoma, Periapical Osteofiroma)
Most common firo-cemento-osseous lesion
Reactive lesion of PDL origin
- Three stages of development
- Early (osteolytic or firoblastic) stage is radiolucent
- Intermediate stage: Radiolucent area containing radiopaque foci
- Mature stage: Well-defied solid homogeneous radiopacity surrounded by thin radiolucent border
Clinical Features
- Somewhat round radiolucencies with well-defied borders
- Associated teeth have vital pulp
- Blacks are more commonly affcted than whites
- About 80% lesions occur in women
- Seldom seen before 4th decade
- About 90% of lesions occur in mandible
- Most frequently involved site
- Periapical region of mandibular incisors
- Lesions may be solitary or multiple, are completely asymptomatic
- Seldom exceed 1 cm in diameter
Differential Diagnosis Of Periapical cemento-Osseous Dysplasia
- Anatomic radiolucency
- Pulpoperiapical radiolucency
- Associated with pulp disease or pulp death
- Traumatic bone cyst: Found in a younger age group
- Mandibular premolar or molar teeth
- Focal cemento-osseous dysplasia:
- Mandibular premolar or molar teeth
- Margins are not so discrete
- Cemento-ossifying firoma:
- Occurs at apices of vital teeth
- Younger people, premolar region
- Cementoblastoma (early stage):
- Occurs at the periapices of the mandibular molars.
- It characteristically extends higher or the roots.
Periapical Radiolucencies Periodontal Disease
- Advanced periodontal bone loss involving one tooth more severely than the teeth immediately adjacent to it.
- The entire bony support of the involved tooth may be destroyed, and the tooth may appear floating in radiolucency.
- Diagnosis can be made by probing the periodontal pockets. Placing gutt-percha points in the pockets to their full depths and then taking radiographs can demonstrate pocket depth relative to the root length.
- Affected teeth are quite mobile and sensitive to percussion.
- Teeth are vital, unless concomitant endodontic lesion is present.
- Treatment: Extraction
- The soft tissue most be curetted from apical region and sent for microscopic examination.
Traumatic Bone cyst
Simple/solitary Bone cyst
- False cyst of bone as it does not have an epithelial lining.
- Etiology is unknown but may be associated with trauma.
- Age: Under 20 years
- Site: Mandible, particularly the premolar/molar region above the mandibular canal, rarely anterior maxilla
- Size: Variable up to several centimeters in diameter.
- Shape: Monolocular, irregular, but the upper border arches up between the roots of the teeth producing the ‘scalloped appearance’
- Outline: Smooth and moderately well defied.
- Radiodensity: Uniformly radiolucent
- Effects: Adjacent teeth—vital with intact lamina dura minimal or no displacement, very rarely resorbed
- Minimal or no expansion of jaw:
- Aspiration—usually fruitless, but in some cases may reveal serosanguineous fluid, small quantity of blood, or a serum-like fluid.
- Microscopic examination—shows scanty tissue, which is loose or fibrous connective tissue containing some hemosiderin.
Periapical Radiolucencies Differential Diagnosis
- Radicular cyst: Pulps are nonvital
- Periapical cemento-osseous dysplasia: Seldom more than 0.7cm. Occurs over 30 years of age. Predilection for lower incisors periodic radiographs show the maturational stages of radiolucent periapical cemento-osseous dysplasia. Traumatic bone cyst is larger than 1 cm under 25 years Premolar/molar area.
- Median mandibular cyst: Occurs in the midline of lower jaw associated teeth are vital causes separation of teeth. Midline of lower jaw associated with teeth are vital.
Periapical Radiolucencies Management
The treatment of choice is to open the area surgically, establish the diagnosis of traumatic bone cyst, remove the tissue debris present, curette the walls of the bony cavity to induce bleeding. After the clot has organized, bone will fil the defect. A careful follow-up is necessary to confim healing.
Dentigerous cyst
- 2nd most common odontogenic cyst
- Pericoronal radiolucency is projected over the apex of neighboring tooth.
- In circumferential or lateral dentigerous cyst, the radiolucency may project over the apex of the same tooth.
Nonradicular cyst
- Nonradicular cyst may be projected over the apices of teeth
- Most common are:
- Incisive canal cyst
- Midplatine cyst
- Median mandibular cyst
- Primordial cyst
- With the exception of primordial cysts, these occur in specific regions of the jaw bones.
- Changing the angle at which the radiograph is taken frequently projects the radiolucent image of the nonodontogenic cyst away from the superimposed apices, this diffrentiates it from pulpoperiapical pathologies.
- Associated teeth are vital.
- If a cyst-like radiolucency larger than 2 cm in diameter is present over the apex of a vital maxillary incisor and can be projected away from the apex by changing the horizontal angulation of a second radiograph, most likely diagnosis is incisive canal cyst.
- If a cystic area at the periapex of a maxillary fist molar on a periapical fim is shown on an occlusal film to involve the whole palate, and if all the maxillary teeth are vital, the most appropriate diagnosis is mid palatine cyst.
Periapical Radiolucencies Malignant Tumor
Malignant tumors may be found as a single periapical radiolucency mimicking a more common benign lesion; early malignant lesions at the apices seldom present with features that suggest their identity. Therefore biopsy is mandatory for periapical lesions that do not respond to endodontic therapy, are surgical cases or are otherwise suspect:
- Squamous cell carcinoma
- Malignant tumor of the minor salivary glands
- Metastatic tumors
- Osteolytic sarcoma
- Chondrosarcoma
- Melanoma
- Fibrosarcoma
- Reticular cell sarcoma
- Multiple myeloma
- Malignant periapical radiolucencies may produce the following images
- Well-defied periapical radiolucency
- Poorly defied periapical radiolucency
- Large, ragged, well-defied radiolucent tumor
- Root resorption and band-like widening of PDL spaces.
Periapical Radiolucencies Features
- Middle and old age
- Pain may be a feature
- Teeth may be vital
- If the tumor is advanced, there may be migration, loosening, tipping, and spreading of teeth
- Gingival bleeding
- Paresthesia or anesthesia
- Advanced lesions may show expansion of jaw
- The advanced lesions are readily recognized as malignancies. The earlier lesions present a problem
- Periodic clinical and radiographic examination
- If root resection is performed the tissue recovered from the periapical region should be sent for microscopic study.
Question 3. Enumerate various periapical lesions. discuss in detail the clinical and radiographic findings of any two periapical lesions.
or
Classify and enumerate only (do not discuss) the various radiographically observable periapical lesion.
Answer.
Periapical Lesions
- Periapical granuloma: For clinical and radiographic features.
- Radicular cyst or periapical cyst.
Clinical Features of Radicular cyst
- Incidence: Radicular cyst constitutes about 50% or more among all types of jaw cysts.
- Age: Mostly third, fourth and fit decade of life.
- Sex: More common among males.
- Site: The cyst can occur in relation to any tooth of either jaw, but maxilla (60%) is more commonly affcted than mandible (40%).
- Involved toothisalwaysnon-vitaland canbe easilydetected by the presence of caries, fractures or discolorations, etc. Moreover, the affcted tooth does not respond to thermal electric pulp testing.
- Cyst becomes more symptomatic as there is acute exacerbation of the periapical inflmmation.
- Larger lesions on the other hand, oftn produce a slow enlarging, bony hard swelling, of the jaw with expansion and distortion of the cortical plates or disturbance in occlusion mostly of the regional teeth; maxillary lesions may cause either buccal or palatal cortical expansions whereas the mandibular lesions oftn cause buccal or labial expansions and rarely the lingual expansions.
- Severe bone destruction by the cystic lesion results in thinning of the cortical plates and it may produce a “springiness” of the jawbone when digital pressure is applied.
- There may be presence of flctuations in case the bone is completely eroded by a large cyst.
- These lesions clinically appear blue as they lie close to the overlying epithelium since the bone has been completely resorbed.
- Pain may be present in the cyst, if it is secondarily infected and it may result in the development of either intraoral or extraoral pus-discharging sinuses.
- On rare occasions, there may be occurrence of paresthesia or pathological fractures in the bone, etc.
- Occasionally, radicular cysts can be multiple in numbers, occurring in relation to several teeth or in relation to several roots of a multirooted tooth.
- A radicular cyst may persist in the jaw aftr the attched tooth has been extracted; such cyst is often called a ’residual cyst’. These cysts frequently cause swelling in the dentulous jaws and they regress slowly and spontaneously.
- In some cases, radicular cysts may develop at the opening of a large accessory pulp canal on the lateral aspect of the tooth root; and these cysts are often termed as ’lateral radicular cysts’.
- If the cyst is secondarily infected it leads to the formation of an abscess, which is called “cyst abscess”.
Radiographic Features of Radicular cyst
- It appears as a rounded or pear-shaped radiolucency at the apex of nonsensitive tooth or with nonvital tooth.
- Radiolucency is more than 1.5 cm in diameter but usually less than 3 cm in diameter. It has got well-defied outline with thin hyperostotic borders.
- Margins: In uncomplicated cases, margins are smooth, corticated and cortex is usually well-defined, welletched and continuous, except in some cases, there may be window formation. There is also thin white line surrounding the margins of bone cavity. This thin layer of cortical bone is almost always present unless suppuration supervenes in the cyst.
- Image of radiopaque borders is continuous with lamina dura around the associated tooth. Infection may cause the borders to become less distinct.
- Radicular cysts of long duration may cause resorption of roots.
- Adjacent teeth are usually displaced and rarely resorbed. There is also buccal expansion and involves maxillary area than displacement of antrum occurs.
Question 4. Enumerate various lesions which present as periapical radiolucencies and discuss anyone in detail.
Answer.
Periapical Granuloma
Pathogenesis
Flow chart in next column representing the pathogenesis.
Clinical Features
- Tooth is often asymptomatic.
- Previous history of prolonged sensitivity to heat or cold.
- Deep caries, a deep restoration or history of trauma.
- Tooth is often tender to percussion.
- Fail to react to thermal or electrical stimulation (because the pulp is nonvital).
Radiographic Features
- Earliest sign: Thickened PDL space at the root apex
- Well-circumscribed radiolucency: Somewhat rounded and surrounding the apex of the tooth
- Thin radiopaque hyperostotic border.
Microscopic Features
- Proliferating endothelialcells, capillaries, young firoblasts, collagen, chronic inflammatory cells, lymphocytes, plasma cells, macrophages.
- Nests of odontogenic epithelium, Russell bodies, foam cells, cholesterol cleft.
- More inflammation is seen in center of the lesion.
- At periphery, Fibrosis (healing) is seen.
Treatment
- Extraction of the involved tooth.
- Root canal therapy (with or without apicoectomy).
- If left untreated, it may undergo transformation to periapical cyst.
Question 5. Write short note on differential diagnosis for radiolucent lesion in maxillary anterior region.
Answer.
Radiolucent Lesion in Maxillary Anterior Region
- Periapical granuloma
- Radicular cyst
- Periapical scar
- Periapical abscess
- Surgical defect
- Osteomyelitis
- Acute apical perodontitis
- Traumatic bone cyst
- Dentigerous cyst
- Giant cell granuloma
Question 6. Write short note on periapical cyst.
Answer. Periapical cyst is also known as radicular cyst.
It appears as a well defied unilocular radiolucency with thin hyperostotic borders. The cyst is associated with a non-vital tooth.
Clinical Features of Radicular cyst
- Incidence: Radicular cyst constitutes about 50% or more among all types of jaw cysts.
- Age: Mostly third, fourth and fit decade of life.
- Sex: More common among males.
- Site: The cyst can occur in relation to any tooth of either jaw, but maxilla (60%) is more commonly affcted than mandible (40%).
- Involved toothisalways non-vitaland canbeeasilydetected by the presence of caries, fractures or discolorations, etc. Moreover, the affcted tooth does not respond to thermal electric pulp testing.
- Cyst becomes more symptomatic as there is acute exacerbation of the periapical inflmmation.
- Larger lesions on the other hand, oftn produce a slow enlarging, bony hard swelling, of the jaw with expansion and distortion of the cortical plates or disturbance in occlusion mostly of the regional teeth; maxillary lesions may cause either buccal or palatal cortical expansions whereas the mandibular lesions oftn cause buccal or labial expansions and rarely the lingual expansions.
- Severe bone destruction by the cystic lesion results in thinning of the cortical plates and it may produce a “springiness” of the jawbone when digital pressure is applied.
- There may be presence of flctuations in case the bone is completely eroded by a large cyst.
- These lesions clinically appear blue as they lie close to the overlying epithelium since the bone has been completely resorbed.
- Pain may be present in the cyst, if it is secondarily infected and it may result in the development of either intraoral or extraoral pus-discharging sinuses.
- On rare occasions, there may be occurrence of paresthesia or pathological fractures in the bone, etc.
- Occasionally, radicular cysts can be multiple in numbers, occurring in relation to several teeth or in relation to several roots of a multirooted tooth.
- A radicular cyst may persist in the jaw aftr the attched tooth has been extracted; such cyst is often called a ’residual cyst’. These cysts frequently cause swelling in the dentulous jaws and they regress slowly and spontaneously.
- In some cases, radicular cysts may develop at the opening of a large accessory pulp canal on the lateral aspect of the tooth root; and these cysts are oftn termed as ’lateral radicular cysts’.
- If the cyst is secondarily infected it leads to the formation of an abscess, which is called “cyst abscess”.
Radiographic Features of Radicular Cyst
- It appears as a rounded or pear-shaped radiolucency at the apex of nonsensitive tooth or with nonvital tooth.
- Radiolucency is more than 1.5 cm in diameter but usually less than 3 cm in diameter. It has got well-defied outline with thin hyperostotic borders.
- Margins: In uncomplicated cases, margins are smooth, corticated and cortex is usually well-defined, welletched and continuous, except in some cases, there may be window formation. There is also thin white line surrounding the margins of bone cavity. This thin layer of cortical bone is almost always present unless suppuration supervenes in the cyst.
- Image of radiopaque borders is continuous with lamina dura around the associated tooth. Infection may cause the borders to become less distinct.
- Radicular cysts of long duration may cause resorption of roots.
- Adjacent teeth are usually displaced and rarely resorbed. There is also buccal expansion and involves maxillary area than displacement of antrum occurs.
Differential Diagnosis
- Periapical granuloma: During FNAC, straw-colored fluid is obtained from cyst while in granuloma fluid is not present. Borders of cyst are hyperostotic.
- Periapical cementoma: During early stages, involved tooth is vital in granuloma while it is non-vital in cyst.
- Lateral periodontal cyst: When site of the radicular cyst is same as for lateral periodontal cyst, the confusion can be eliminated as the involved tooth is vital in lateral periodontal cyst while it is non-vital in periapical cyst.
- Traumatic bone cyst: Occurs mostly in mandible, while it is not true for periapical cyst.
- Periodontal abscess: Associated tooth is vital in abscess and bone loss is seen.
Question 7. Write short note on radiographic features of periapical granuloma.
Answer. Following are the radiographic features of periapical granuloma:
- Periapical area is radiolucent with loss of lamina dura.
- Radiolucency is of variable size at the apex of tooth, diameter is usually less than 1.5 cm.
- Lesion may or may not have well defied border, which can or cannot be hyperostotic.
- Presence of loss of lamina dura and periapical bone known as “periapical rarefying osteitis”.
- Involved tooth can show a deep restoration, extensive caries, fracture or a narrow pulp canal with non-vital pulp.

Leave a Reply