Diabetes Mellitus
Question 1. Discuss etiopathogenesis, clinical features, diagnosis, and complications of diabetes mellitus.
Or
Write a short note on complications of diabetes mellitus.
Or
Discuss etiopathogenesis and complications of type 2 diabetes mellitus. Enumerate its complications.
Or
Write in short on diabetes mellitus.
Or
Write a short note on diabetes mellitus.
Answer:
Diabetes mellitus is a heterogeneous metabolic disorder characterized by the common feature of chronic hyperglycemia with disturbance of carbohydrate, fat, and protein metabolism.
Diabetes mellitus is classified into two types:
- Type 1 Diabetes Mellitus: It is also called insulin-dependent or juvenile-onset diabetes.
- Type 2 Diabetes Mellitus: It is also called non-insulin-dependent diabetes mellitus or maturity-onset diabetes mellitus.
Etiopathogenesis
Type 1: Diabetes Mellitus
The basic phenomenon is the destruction of a cell mass, usually leading to absolute insulin deficiency.
- Genetic Susceptibility:
- Identical twins: If one twin has type I diabetes mellitus there is about a 50% chance of the second twin developing it.
- Susceptibility gene on HLA region in chromosome 6.
- Autoimmune Factors:
- Presence of Islet cell antibodies against insulin.
- Occurrence of lymphocytic infiltrate in and around pancreatic islets termed insulitis.
- CD8 +T cell-mediated selective destruction of b cells.
- Autoimmune diseases like Graves’ disease, Addison’s disease, and Hashimoto’s thyroiditis.
Read And Learn More: Pathology Question And Answers
Environmental Factors:
- Certain viral infections, i.e. mumps, measles, etc.
- Experimental induction with chemicals.
- Geographic and seasonal variations.
Type 2: Diabetes Mellitus
- Genetic Factors:
- Identical Twins: 80% chance of developing diabetes if one twin has diabetes mellitus.
- If both parents are diabetic the risk in offspring rises to 50%.
- Constitutional Factors:
- Obesity
- Hypertension
- Low physical activity.
- Insulin resistance
- Impaired glucose utilization
- Receptor and post-receptor defects
- Decreased insulin secretion
- Due to amylin
- Due to the glucose toxicity of islets.
- Due to lipotoxicity.
These above factors lead to increased hepatic glucose synthesis and cause hyperglycemia which leads to Type 2 diabetes mellitus.
Clinical Features of Diabetes Mellitus
Type 1: Diabetes Mellitus
- It occurs at an early age generally below the age of 35 years.
- The onset of symptoms is often abrupt.
- Patient has polyuria, polydypsia and polyphagia.
- Patients are not obese and have generally progressive loss of weight.
- Patients are prone to develop metabolic complications such as ketoacidosis.
Type 2: Diabetes Mellitus
- It occurs in middle age or beyond, usually above the age of 40.
- The onset of symptoms is slow.
- Patients are asymptomatic.
- Patients are obese and have unexplained weakness and loss of weight.
- Metabolic complications such as ketoacidosis are present.
Complications of Diabetes
Both types of diabetes mellitus may develop complications which are divided into two major groups:
- Acute metabolic conditions
- Late systemic complication.
Acute Metabolic Complications
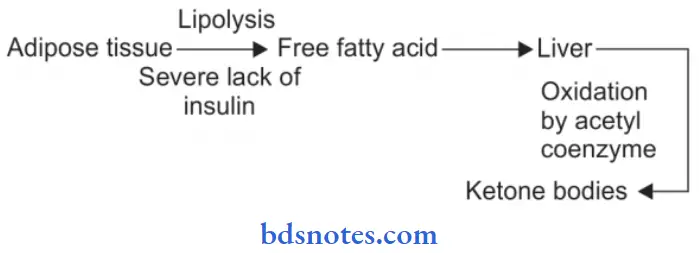
- Diabetic ketoacidosis: Ketoacidosis is almost exclusively a complication of type I diabetes mellitus. It can be developed in severe insulin deficiency.
Clinically the condition is characterized by anorexia, nausea, vomiting, deep and fast breathing, confusion, and coma.
- Hyperosmolar non-kinetic comma: It is usually a complication of type 2 diabetes mellitus. It is caused by severe dehydration resulting from sustained hyperglycemic diuresis.
- Blood sugar is extremely high and plasma osmolarity is high.
- Thrombolytic and bleeding complications are frequent due to the high viscosity of blood.
- Hypoglycemic episode: It may develop in patients with type 1 diabetes mellitus.
- It may result in excessive administration of insulin, missing a meal, or due to stress.
- It is harmful as they produce permanent brain damage and also results in worsening diabetic control and rebound hyperglycemia.
Late Systemic Complications
1. Atherosclerosis: Both Type 1 and Type 2 diabetes mellitus cause atherosclerosis. The process of atherosclerosis accelerated in patients with diabetes.
Various contributory factors for atherosclerosis are hyperlipidemia, reduced HDL levels, nonenzymatic glycosylation, increase platelet adhesiveness, obesity, and hypertension in diabetes.
Atherosclerosis can lead to coronary artery disease, silent myocardial infarction, cerebral stroke, and gangrene of the toe and feet.
2. Diabetic microangiopathy: This is characterized by the thickening of the basement membrane of small blood vessels and capillaries of different organs and tissues, i.e. skin, skeletal muscle, eye, and kidney.
A similar type of basement membrane-like material is deposited in non-vascular tissues, i.e. peripheral nerves, renal tubules, and Bowman’s capsule.
Diabetic microangiopathy occurs due to recurrent hyperglycemia which leads to increased glycosylation of hemoglobin and other proteins which causes thickening of the basement membrane.
3. Diabetic nephropathy: Involvement of the renal system is an important complication of diabetes mellitus.
Renal complications develop early and frequently in Type 1 diabetes mellitus as compared to type 2 diabetes mellitus.
Various clinical syndromes are associated with diabetic nephropathy, i.e. asymptomatic proteinuria, nephrotic syndrome, renal failure, and hypertension.
Cardiovascular diseases are 40 times more common in patients with end-stage renal disease in diabetes mellitus as compared to non-diabetics.
4. Diabetic neuropathy: It affects all the parts of the nervous system. Peripheral neuropathy is more characteristic. Pathologic changes are segmental demyelination, Schwann cell injury, and axonal damage.
5. Diabetic retinopathy: It is an important cause of blindness. This complication develops in more than 60% of diabetic patients.
Other ocular complications of diabetes mellitus are glaucoma, cataract, and corneal disease. Risk is greater in Type 1 diabetes mellitus as compared to type 2 diabetes mellitus.
6. Infections: Diabetes leads to the susceptibility of infections i.e. tuberculosis, pneumonia, pyelonephritis, otitis, carbuncles, and diabetic ulcers. It occurs due to impaired leucocyte functions, reduced cellular immunity, poor blood supply, and hyperglycemia.
Diagnosis of Diabetes Mellitus
- Urine testing: Urine tests are cheap and convenient. They are tested for the presence of glucose and ketones.
- Glucosuria:
- Benedict’s qualitative test detects any reducing test in urine.
- Dipstick Test: More sensitive and glucose-specific test, a method is based on enzyme coated paper strip which turns purple when dipped in urine containing glucose.
- Ketonuria: The test for ketone bodies in urine is required for assessing the severity of diabetes.
- Dipstick Test: More sensitive and glucose-specific test, a method is based on enzyme coated paper strip which turns purple when dipped in urine containing glucose.
- Benedict’s qualitative test detects any reducing test in urine.
- Glucosuria:
- Single blood sugar estimation: For diagnosis of diabetes, blood sugar determination is absolutely necessary.
- A fasting plasma glucose value above 126 mg/dl is certainly indicative of diabetes.
- Oral glucose tolerance test:
- An individual with a fastening value of random glucose higher than 126 mg/dl and a 2-hour value after 75 gm oral glucose higher than 200 mg/dl is labeled as diabetic.
- In a symptomatic case, the random blood glucose value above 200 mg/dl is diagnosed as diabetes.
Question 2. Discuss in brief laboratory diagnosis of diabetes mellitus.
Or
Write short notes on diagnostic tests of diabetes mellitus.
Or
Write a brief on investigating methods in the diagnosis of diabetes mellitus.
Answer:
Diabetes Mellitus Urine Testing
These tests are cheap and convenient but the diagnosis of diabetes cannot be based on urine testing alone since there may be false-positives and false-negative results. They can be used in population screening surveys. Urine is tested for the presence of glucose and ketones.
1. Glucosuria
- Benedict’s qualitative test detects any reducing substance in the urine and is not specific for glucose. A more sensitive and glucose-specific test is the dipstick method based on enzyme coated paper strip which turns purple when dipped in urine containing glucose. Besides diabetes mellitus, glucosuria may also occur in certain other conditions such as—renal glycosuria, alimentary (lag storage) glucosuria, and many metabolic disorders. However, two of these conditions—renal glucosuria and alimentary glucosuria, require further elaboration.
- Renal glucosuria: Next to diabetes, the most common cause of glucosuria is the reduced renal threshold for glucose. In such cases, although the blood glucose level is below 180 mg/dl glucose still appears regularly and consistently in the urine due to lowered renal threshold.
- Alimentary (lag storage) glucosuria: A rapid and transitory rise in blood glucose levels above the normal renal threshold may occur in some individuals after a meal. During this period, glucosuria is present.
2. Ketonuria
Tests for ketone bodies in the urine are required for assessing the severity of diabetes and not for the diagnosis of diabetes. However, if both glucosuria and ketonuria are present, the diagnosis of diabetes is almost certain.
- Rothera’s test (nitroprusside reaction) and strip test are conveniently performed for the detection of ketonuria.
Diabetes Mellitus Single Blood Sugar Estimation
For the diagnosis of diabetes, blood sugar determinations are absolutely necessary. Currently used are O—toluidine, Somogyi—Nelson, and glucose oxidase methods.
Whole blood or plasma may be used but whole blood values are 15% lower than plasma values. A grossly elevated single determination of plasma glucose may be sufficient to make the diagnosis of diabetes.
A fasting plasma glucose value above 126 mg/dl is indicative of diabetes.
Diabetes mellitus Screening by Fasting Glucose Test
Fasting plasma glucose determination is a screening test for type 2 diabetes mellitus. It is recommended that all individuals above 45 years of age must undergo a screening fasting glucose test every 3 years.
Diabetes Mellitus Oral Glucose Tolerance Test
It is performed principally for patients with borderline fasting plasma glucose values (i.e. between 100 and 140 mg/dl).
The patient who is scheduled for an oral glucose tolerance test is instructed to eat a high carbohydrate diet for at least 3 days prior to the test and come after an overnight fast on the day of the test.
A fasting blood sugar sample is first drawn. Then 75 gm of glucose dissolved in 300 mL of water is given. Blood and urine specimens are collected at half-hour intervals for at least 2 hours.
Blood or plasma glucose content is measured and urine is tested for glucosuria to determine the approximate renal threshold for glucose.
Diabetes mellitus Other Test
A few other tests are sometimes performed in specific conditions in diabetics and for research purposes:
- Glycosylated hemoglobin (HbA1c): Measurement of blood glucose level in diabetics suffers from variation due to dietary intake of the previous day. Long-term objective assessment of the degree of glycemic control is better monitored by measurement of glycosylated hemoglobin (HbA1C), a minor hemoglobin component present in normal persons (normal range 4–6%). This is because the non-enzymatic glycosylation of hemoglobin takes place over 90-120 days, the lifespan of red blood cells. HbA1C assay, therefore, gives an estimate of diabetic control and compliance for the preceding 3-4 months.
- Glycated albumin: This is used to monitor the degree of hyperglycemia during the previous 1-2 weeks when HbA1C can not be used.
- Extended GTT: The oral GTT is extended to 3-4 hours for the appearance of symptoms of hyperglycemia. It is a useful test in cases of reactive hypoglycemia of early diabetes.
- Intravenous GTT: This test is performed in persons who have intestinal malabsorption or in postgastrectomy cases.
- Cortisoneprimed GTT: This provocative test is a useful investigative aid in cases of potential diabetics.
- Islet autoantibodies: Glutamic acid decarboxylase and islet cell cytoplasmic antibodies may be used as a marker for type I DM.
Question 3. Write in short about diabetic nephropathy.
Answer:
Diabetic nephropathy means renal involvement in diabetes mellitus which is the complication of diabetes mellitus.
Diabetic nephropathy constitutes four types of renal lesions:
- Diabetic glomerulosclerosis
- Diffuse glomerulosclerosis
- Nodular glomerulosclerosis.
- Vascular lesions
- Diabetic pyelonephritis
- Tubular lesions.
Diabetic Glomerulosclerosis
Glomerular lesions in diabetes mellitus are common and account for the majority of abnormal findings referable to the kidney. Pathogenesis of these lesions in diabetes mellitus is explained by following sequential changes, i.e. glomerular hypertension → Renal hyperperfusion → Deposition of proteins in the mesangium → Glomerulosclerosis → Renal failure.
- Diffuse glomerulosclerosis:
- Diffuse glomerular lesions are the most common.
- There is the involvement of all parts of the glomeruli.
- Pathologic changes consist of thickening of the GBM and diffuse increase in the mesangial matrix with the mild proliferation of mesangial cells. Various exudative lesions such as capsular hyaline drops and firing caps may also be present.
- Nodular glomerulosclerosis:
- Nodular lesions of diabetic glomerulosclerosis are also called as Kimmezlstiel-Wilson (KW) lesions or intercapillary glomerulosclerosis.
- These lesions are specific for juvenile—onset diabetes or islet cell antibody—positive diabetes mellitus.
- The pathologic changes consist of one or more nodules in a few or many glomeruli. Nodule is an ovoid or spherical, laminated, hyaline, acellular mass located within a lobule of the glomerulus.
Diabetic nephropathy Vascular Lesions
Atheroma of renal arteries is very common and severe in diabetes mellitus. Hyaline arteriolosclerosis affecting the afferent and efferent arterioles of the glomeruli is also often severe in diabetes.
These vascular lesions are responsible for renal ischemia that results in tubular atrophy and interstitial fibrosis.
Diabetic Pyelonephritis
Poorly-controlled diabetics are particularly susceptible to bacterial infections. Papillary necrosis (necrotizing papillitis) is an important complication of diabetes that may result in acute pyelonephritis.
Tubular Lesions (Armani-Ebstein Lesions)
In untreated diabetics who have extremely high blood sugar levels, the epithelial cells of proximal convoluted tubules develop extensive glycogen deposits appearing as vacuoles.
These are called Armanni-Ebstein lesions. The tubules return to normal on control of the hyperglycemic state.
Question 4. Write a short note on the glucose tolerance test.
Answer:
It is also known as an oral glucose tolerance test.
Instruction to Patient Before Going for Glucose Tolerance Test
The patient who is scheduled for a glucose tolerance test is instructed to eat a high-carbohydrate diet for at least 3 days prior to the test and come after an overnight fast on the day of the test (for at least 8 hours).
Tolerance Test Sample
- A fasting blood sugar sample is first drawn.
- Then 75 gm of glucose dissolved in 300 mL of water is given.
- Blood and urine specimens are collected at half-hour intervals for at least 2 hours.
Tolerance Test Analysis
Blood or plasma glucose content is measured and tested for glucosuria to determine the approximate renal threshold for glucose. Venous whole blood concentrations are 15% lower than plasma glucose values.
Tolerance Test Results
- Individuals with a fasting value of plasma glucose higher than 126 mg/dl and a 2-hour value after 75 gm glucose higher than 200 mg /dL are labeled as diabetics.
- In a symptomatic case, the random blood glucose value above 200 mg/dl is diagnosed as diabetes mellitus.
- The normal cut-off value for fasting blood glucose is considered 110 mg/dl. Cases with fasting blood glucose values between 110 and 126 mg/dl are considered as impaired fasting glucose tolerance (IGT); these cases are at increased risk of developing diabetes later and therefore kept under observation for repeating the test.
- During pregnancy, however, a case of IGT is treated as diabetic.
Question 5. Write on urinary ketone bodies and their test.
Answer:
Whenever there is inadequate carbohydrate in the diet or a defect in carbohydrate metabolism body metabolizes an increasing amount of fatty acids.
Due to this intermediary products such as ketone bodies increase in blood. Ketone bodies are excreted through urine.
- Ketonuria occurs in diabetes mellitus.
- Detection of ketonuria in diabetes mellitus is necessary to assess the severity of the disease and also to change insulin dosage.
Test for Urinary Ketone Bodies
Rothera Test
- Principle
- Nitroprusside used in this test reacts with acetone and acetoacetic acid in the presence of alkali to produce the purple-colored compound.
- Procedure
- Transfer 5 mL of urine to the test tube using a Pasteur pipette.
- Add 1 gm of Rothera powder mixture and mix well.
- Layer over the urine 1 to 2 mL of concentrated ammonium hydroxide.
- Observe a pink-purple ring at the interface.
Observation
- The appearance of a pink-purple ring is suggestive of ketone bodies.
Dumn and Shipley’s Method
Procedure
- Take two test tubes and label them T & C.
- Add a pinch of a mixture of sodium nitroprusside, ammonium sulfate, and anhydrous sodium carbonate in both test tubes.
- In a tube labeled T add one drop of urine.
- In a tube labeled C add one drop of distilled water.
- Observe the color of the reaction mixture after 5 min.
Observation
Presence of violet color is suggestive of ketone bodies.

Leave a Reply