Developmental Disorders Of Teeth And Jaw Question And Answers
Question 1. Write short note on anodontia.
Answer. Anodontia is defined as the condition in which there is congenital absence of teeth in oral cavity.
Anodontia Etiology
The causes of anodontia are:
- Hereditary factor.
- Environmental factor.
- Familial factor.
- Syndrome associated.
- Radiation injury to the developing tooth germ.
Types of Anodontia
- Complete anodontia: There is congenital absence of all the teeth.
- Partial anodontia: Congenital absence of one or few teeth.
Anodontia can also be divided into following types:
-
- True anodontia: It occurs due to failure of development or formation of tooth in jaw bone.
- Pseudo anodontia: It refers to the condition in which teeth are present within the jaw bone but are not clinically visible in the mouth, as they have not erupted, e.g. impacted teeth.
- False anodontia: It is the condition in which teeth are missing in the oral cavity because of their previous extraction.
Complete Anodontia
- It is the condition in which there is neither any deciduous tooth nor any permanent tooth present in the oral cavity.
- It is usually seen in association with hereditary ectodermal dysplasia. A complete anodontia is a common feature of hereditary ectodermal dysplasia, however, in many cases cuspids are present in this disease.
- Complete anodontia occurs among children those who have received high doses of radiation to the jaws as infants for therapeutic reasons.
Partial Anodontia
- It is a common phenomenon and is characterized by congenital absence of one or few teeth.
- In partial anodontia any tooth can be congenitally missing.
- Third molars are most frequently observed as congenitally missing teeth.
- Mandibular first molar and the mandibular lateral incisor are least likely to be missing.
Read And Learn More: Oral Medicine Question And Answers
Question 2. Write short note on enamel hypoplasia.
Answer.
Enamel Hypoplasia
It is defined as an incomplete or defective formation of organic enamel matrix.
Enamel hypoplasia is of two types, i.e.
- Acquired enamel hypoplasia.
- Environmental enamel hypoplasia.
Hypoplasia Acquired Enamel
Factors Associated with Acquired Enamel Hypoplasia
There are two types of factors which are associated with acquired enamel hypoplasia:
- Hypoplasia Local factors:
- Local factors are infection, trauma, radiotherapy
- Idiopathic factors.
- When local infection or trauma causes damage to ameloblasts cells during odontogenesis, then it may lead to defect in enamel formation in isolated permanent tooth. This is known as focal enamel hypoplasia.
- Focal enamel hypoplasia is caused due to periapical spread of infection from a carious deciduous tooth or trauma to the deciduous tooth, the permanent tooth bud affected in this process is known as Turner’s tooth.

2. Environmental or systemic factors:
Systemic or environmental disturbances in the functioning of ameloblasts at specific period of time during odontogenesis of teeth manifests as horizontal line of small pits or grooves on enamel surfaces. This line on tooth surface indicates zone of enamel hypoplasia and corresponds to time of development and duration of insult. Following are the various factors which lead to systemic or environmental disturbances:
Prenatal period: The prenatal infections are rubella, syphilis.
- There is presence of internal disease
- There are excess fluoride ions.
Hypoplasia Neonatal period: During this period, enamel hypoplasia is caused due to:
- Hemolytic disease of newborn
- Birth injury
- Premature delivery
- Prolong labor
- Low birth weight.
Hypoplasia Postnatal period: During this period enamel hypoplasia is due to:
- Severe childhood infection
- Prolong fever due to infectious disease in childhood
- Nutritional deficiency
- Hypocalcemia
- Rickets
- Celiac disease.
Environmental Enamel Hypoplasia
In it, either primary or permanent dentition is involved.
Both enamel and dentin are affected.
Enamel Hypoplasia Causes
- Nutritional deficiency
- Exanthematous diseases
- Congenital syphilis
- Hypocalcemia
- Birth injury, prematurity, Rh-incompatibility
- Local infection/trauma
- Ingestion of chemicals.
Enamel Hypoplasia Types
- Mild: Few small grooves, pits or fissures in enamel surface.
- Moderate: Deep pits arranged horizontally across the tooth.
- Severe: Considerable portion of enamel may be lost.
Enamel Hypoplasia Clinical Features
- Usually pitting type of hypoplasia is seen in deficiency of vitamin A, C and during tooth formation.
- In case of congenital syphilis, incisors show Hutchinson’s teeth characterized by screw driven-shaped incisor and mulberry molars characterized by irregular enamel on the occlusal surface of the crown.
- Presence of Turner’s teeth in local infection.
Enamel Hypoplasia Management
- Since teeth which are affected with enamel hypoplasia are more susceptible for dental caries as compared to the normal teeth. Restoration should be confined to area of involvement.
- In severe enamel hypoplasia chrome steel crown is given. Severe forms need composite restoration or full ceramic crown.
- If sensitivity is present, desensitizing paste is prescribed.
- In mild hypoplastic molars, pit and fissures are placed over occlusal surface and 6 months re-evaluation is done.
- In patients with more demineralization, affected enamel should be removed and tooth should be restored with composite.
- Reduction of tooth and crown placement can also be done.
- In severe cases extraction can be done.
- In anterior teeth, porcelain veneers or zirconia crowns are indicated.
Question 3. Write short note on Dentinogenesis imperfecta.
Answer. Dentinogenesis imperfecta is also known as hereditary opalescent dentin or Capadepont’s teeth.
Dentinogenesis imperfecta Classification
- Shield Type 1: Dentinogenesis imperfecta always occur with osteogenesis imperfecta. As per Witkop it is known as dentinogenesis imperfecta.
- Shield Type 2: Dentinogenesis imperfecta which is not associated with osteogenesis imperfecta. As per Witkop it is known as hereditary opalescent dentin.
- Shield Type 3: It has got shell teeth appearance and multiple pulp exposure. As per Witkop it is known as Brandywine type.
Dentinogenesis imperfecta Clinical Features
Dentinogenesis imperfecta Clinical Features Shield Type 1
- Presence of multiple bone fractures, hyperextensible joints, blue sclera and there is progressive deafness.
- Deciduous teeth are affected more commonly as compared to permanent teeth.
- Color of teeth ranges from blue to brownish violet to yellow brown.
- Enamel is lost and dentition undergoes rapid attrition.
- Scalloping of DEJ is absent. Teeth are shorter in size. In some of the cases total crown loss is present.
- In anterior teeth, crown is of square shaped but both mesial and distal borders are curved.
- In posterior teeth, both bicuspids and molars become flat and normal circumferential curves get accentuated because of this, teeth show bulbous appearance. Neck of the teeth narrows down.
Dentinogenesis imperfecta Clinical Features Shield Type 2
Features are same as Shield Type I but they are severe in form and are not associated with osteogenesis imperfecta.
Dentinogenesis imperfecta Clinical Features Shield Type 3
- In this both permanent and deciduous dentition are affected.
- Here the thickness of enamel is normal while dentin is very thin.
- Tooth has opalescent color, crown is bell shaped and there is multiple pulp exposure.
Dentinogenesis imperfecta Radiographic Features
- Affected teeth shows cervical constriction and impart bulbous appearance.
- Pulp chamber is either partially or completely obliterated. Root canals can be absent or thread like.
- There is presence of periapical radiolucency without any pulpal involvement and widening of periodontal ligament space.
- In some of the cases radicular part of pulp cavities is narrow but pulp chamber consists of bulbous expansion which terminates at a point deep to occlusal aspect, this resembles as flame shape.
- In Brandywine type, tooth enamel is normal but dentin is thin and pulp chambers are enormous. Teeth look like as shell teeth. Root of tooth is very short.
Dentinogenesis imperfecta Management
- Overdenture can be given to the patient and affected teeth should be restored by glass ionomer cement.
- Anteriorly porcelain jacket crown and posteriorly cast metal crown can be given.
Question 4. Write short note on cleidocranial dysostosis.
Answer. It is also called cleidocranial dysplasia or Marie and
Sainton disease.
Cleidocranial Dysostosis Etiology
- Hereditary: True dominant Mendelian characteristic.
- Genetic: There is incomplete penetration of the genetic trait. Defect in CBFA I gene chromosome.
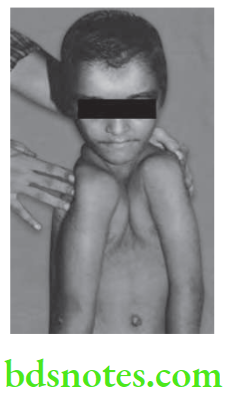
Cleidocranial Dysostosis Clinical Features
- The disease affects men and women with equal frequency.
- It primarily affects skull, clavicle and dentition.
- Head is brachycephalic or wide or short.
- Nasal bridge is depressed with broad base.
- In skull, fontanelles remain open or at least exhibit delayed closing.
- Lacrimal and zygotic bone remains underdeveloped.
- Sagittal suture is sunken and gives skull the flat appearance.
- Nasal bridge is depressed with broad base.
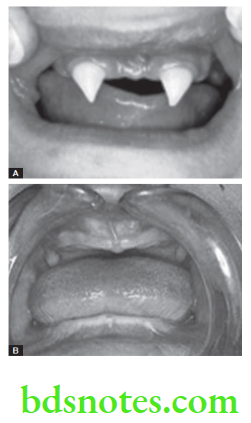
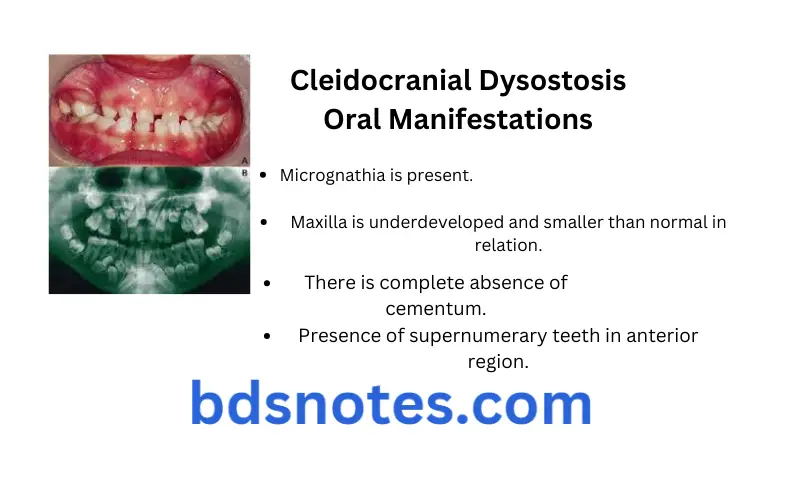
Cleidocranial Dysostosis Oral Manifestations
- Micrognathia is present.
- Maxilla is underdeveloped and smaller than normal in relation.
- Prolonged retention of primary dentition and delayed eruption of permanent dentition.
- There is complete absence of cementum.
- Presence of supernumerary teeth in anterior region.
- Roots of teeth are often short and thinner than normal.
- There is hypoplasia of enamel.
- High arch palate and cleft palate can be present.
Cleidocranial Dysostosis Radiographic Features
- Skull film reveals open sutures presence of wormian bones, wide cranium, delayed ossification of fontanelles.
- Evaluation of chest radiograph reveals the absence of clavicles.
- Jaws are flattened and there is overgrowth of cranial base: anteroposteriorly.
- Jaw examination reveals prolonged retention of primary dentition, multiple superanumerary teeth and small underdeveloped jaw.
- Roots of the teeth are short and thin.
Cleidocranial Dysostosis Management
- Not specific.
- Patient consists of supernumerary teeth which can be extracted, prosthetic replacement of teeth can be done.
- Unerupted tooth can be extracted orthodontically.
Question 5. Write short note on differential diagnosis of supernumerary teeth.
Answer. Following is the differential diagnosis of supernumerary teeth:
- Cleidocranial dysplasia: When viewed radiographically, numerous supernumerary teeth present. Patients routinely have 10 or more supernumerary teeth that are producing crowding and preventing eruption of deciduous teeth. There is an obvious mixed dentition with this disorder.
- Gardner syndrome: The second differential diagnosis that is associated with numerous supernumerary teeth is Gardner syndrome (familial adenomatous polyposis). This syndrome involves multiple supernumerary teeth as well as osteomas. The presence of supernumerary teeth may not be as numerous as those found in cleidocranial dysplasia.
- Supernumerary teeth in non syndromic cases: These cases present without any known associated diseases or syndromes. The patients are thought to have a genetic propensity toward supernumerary teeth.

Leave a Reply